The Special Senses Smell taste vision hearing and



- Slides: 48
The Special Senses • Smell, taste, vision, hearing and equilibrium • Housed in complex sensory organs
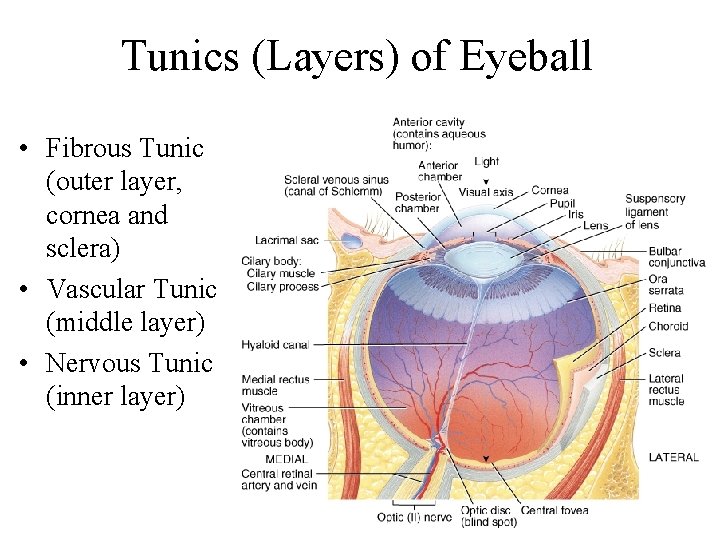
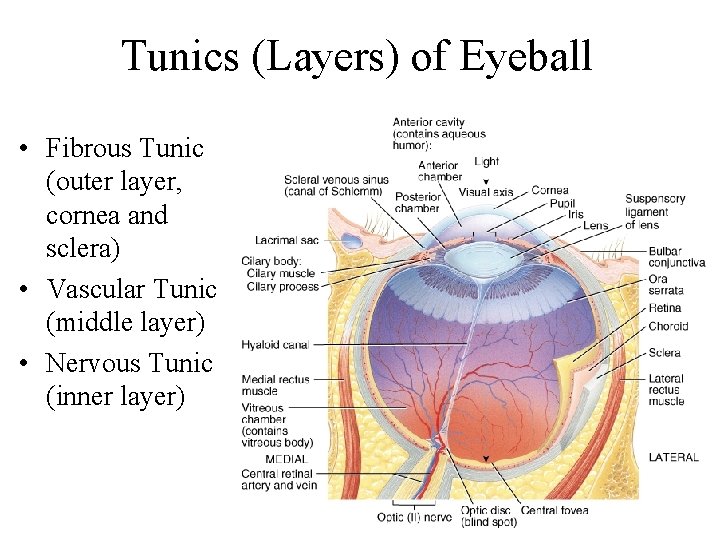
Tunics (Layers) of Eyeball • Fibrous Tunic (outer layer, cornea and sclera) • Vascular Tunic (middle layer) • Nervous Tunic (inner layer)
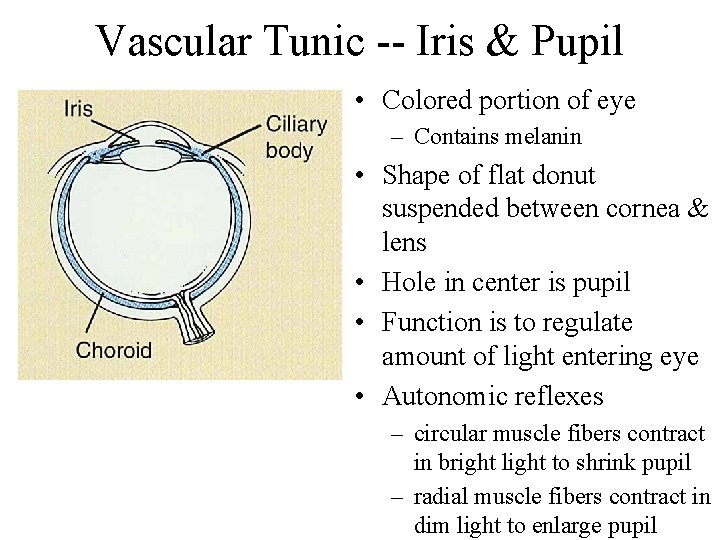
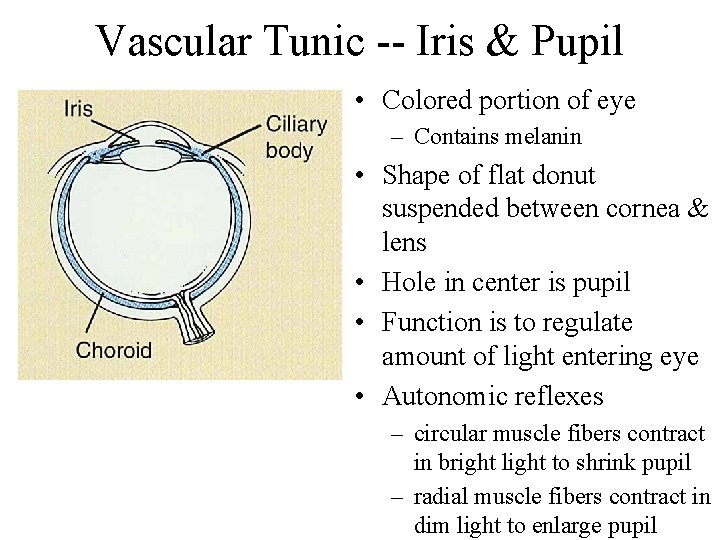
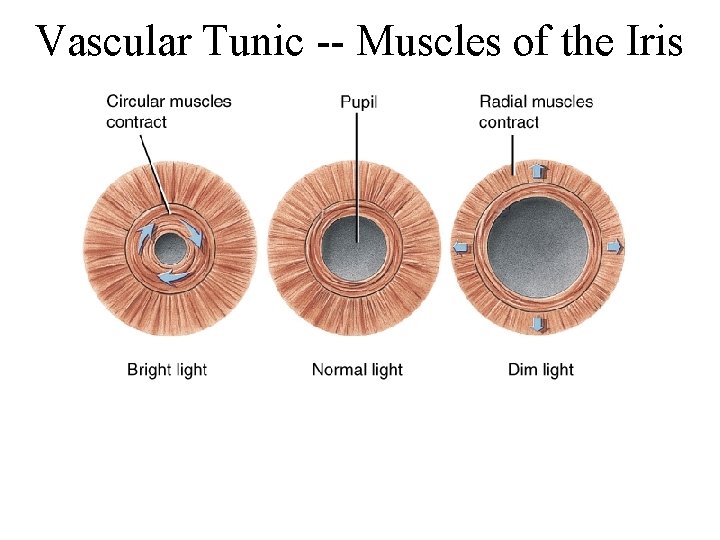
Vascular Tunic -- Iris & Pupil • Colored portion of eye – Contains melanin • Shape of flat donut suspended between cornea & lens • Hole in center is pupil • Function is to regulate amount of light entering eye • Autonomic reflexes – circular muscle fibers contract in bright light to shrink pupil – radial muscle fibers contract in dim light to enlarge pupil
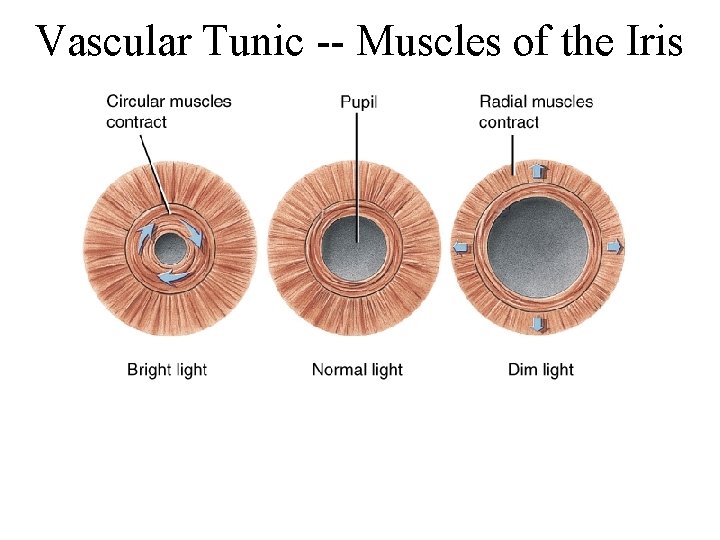
Vascular Tunic -- Muscles of the Iris
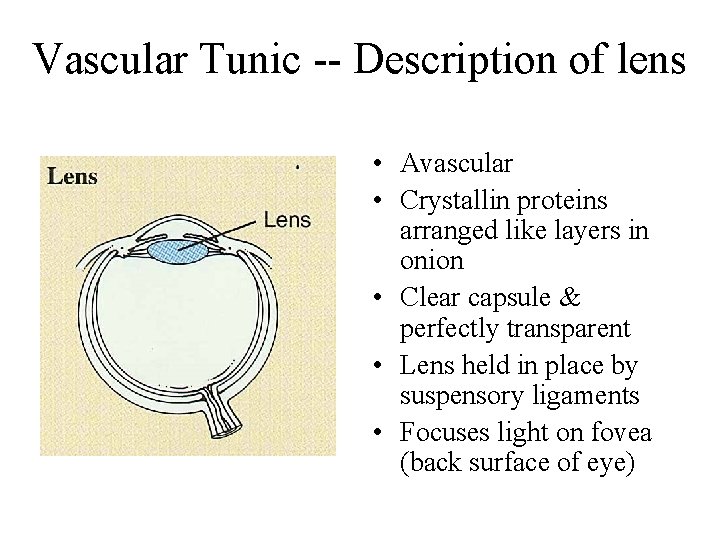
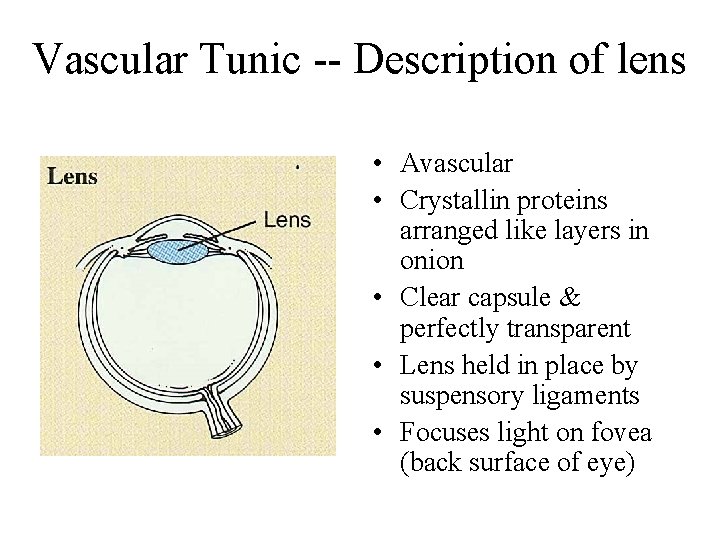
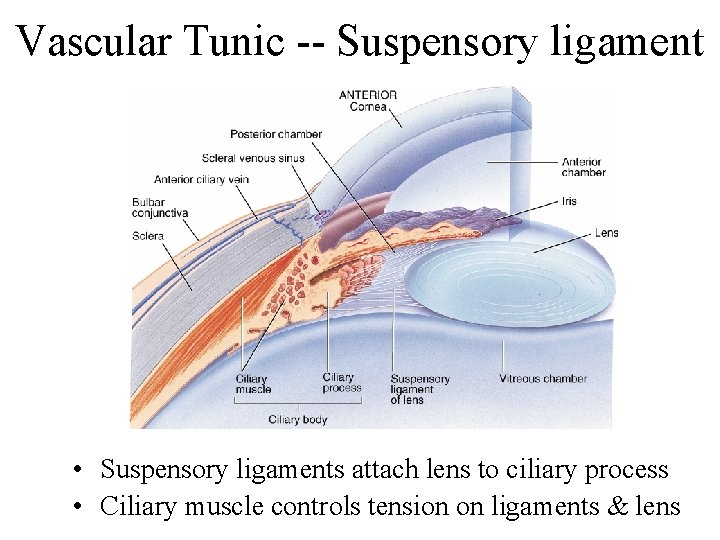
Vascular Tunic -- Description of lens • Avascular • Crystallin proteins arranged like layers in onion • Clear capsule & perfectly transparent • Lens held in place by suspensory ligaments • Focuses light on fovea (back surface of eye)
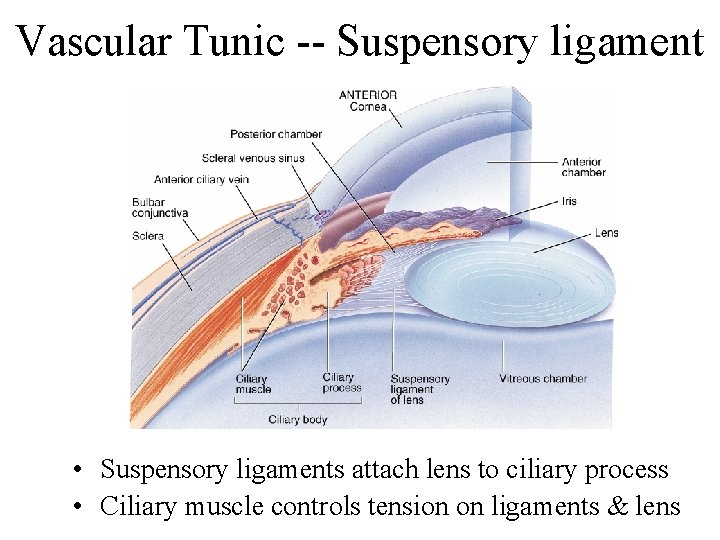
Vascular Tunic -- Suspensory ligament • Suspensory ligaments attach lens to ciliary process • Ciliary muscle controls tension on ligaments & lens
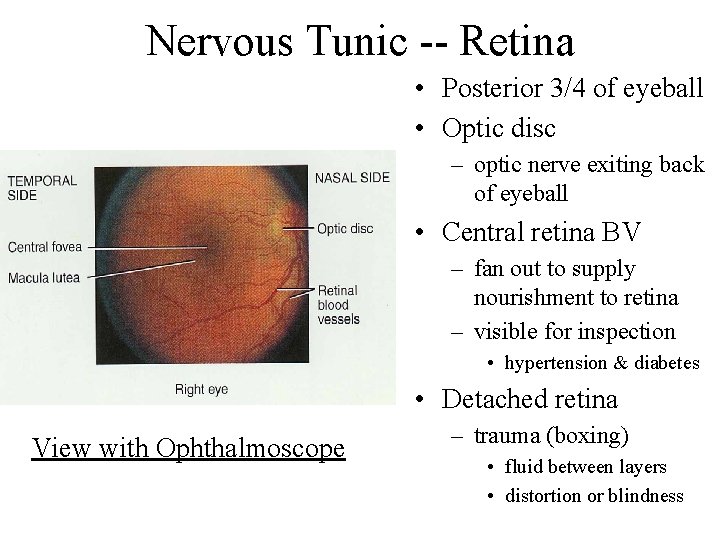
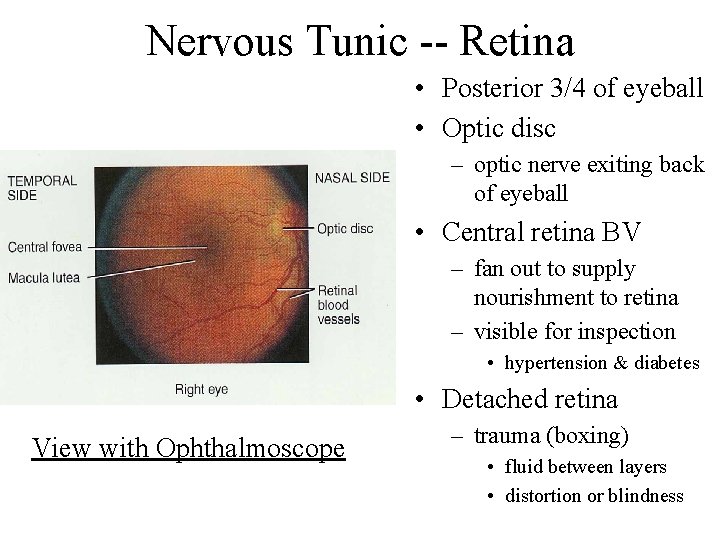
Nervous Tunic -- Retina • Posterior 3/4 of eyeball • Optic disc – optic nerve exiting back of eyeball • Central retina BV – fan out to supply nourishment to retina – visible for inspection • hypertension & diabetes • Detached retina View with Ophthalmoscope – trauma (boxing) • fluid between layers • distortion or blindness
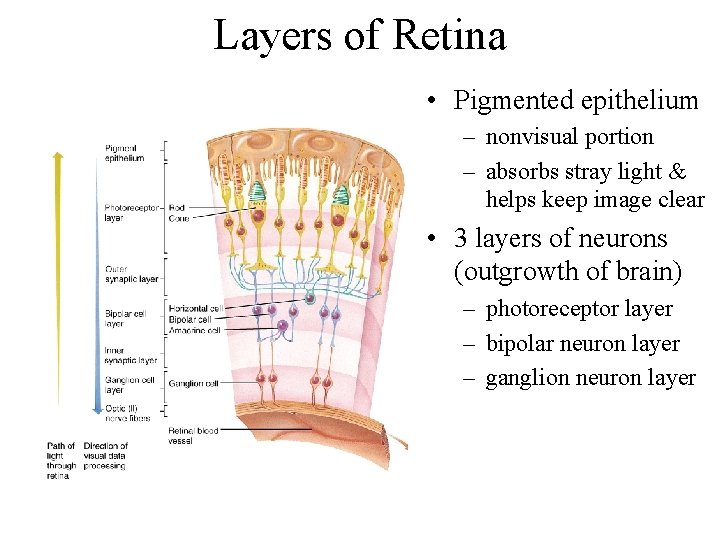
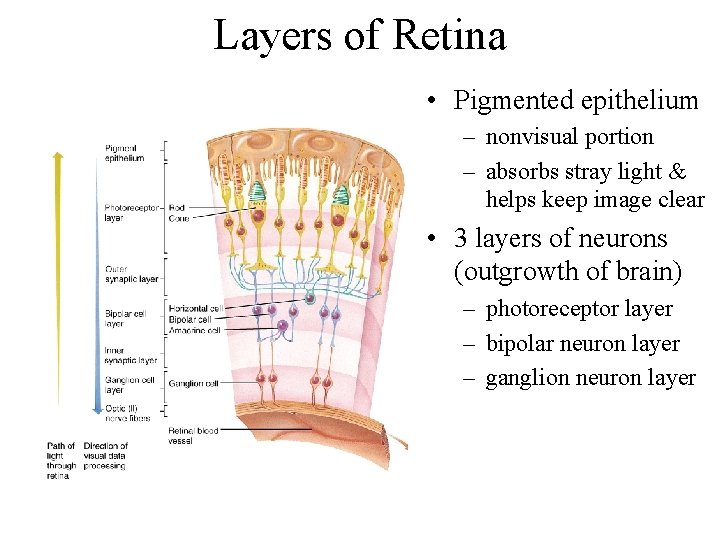
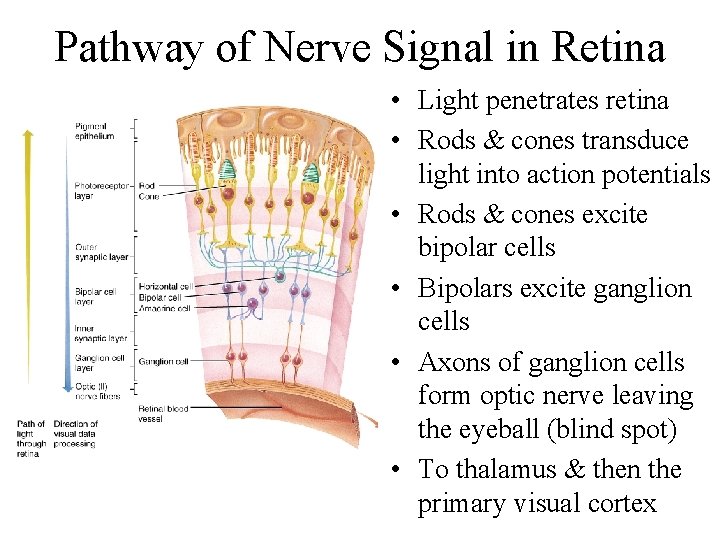
Layers of Retina • Pigmented epithelium – nonvisual portion – absorbs stray light & helps keep image clear • 3 layers of neurons (outgrowth of brain) – photoreceptor layer – bipolar neuron layer – ganglion neuron layer
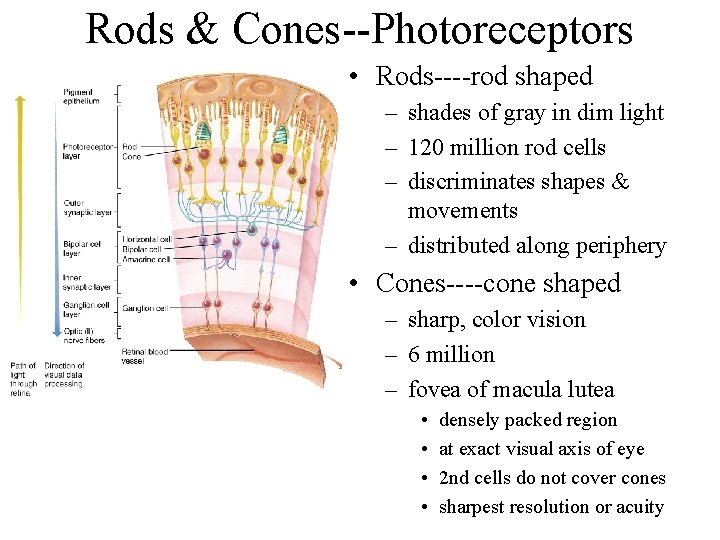
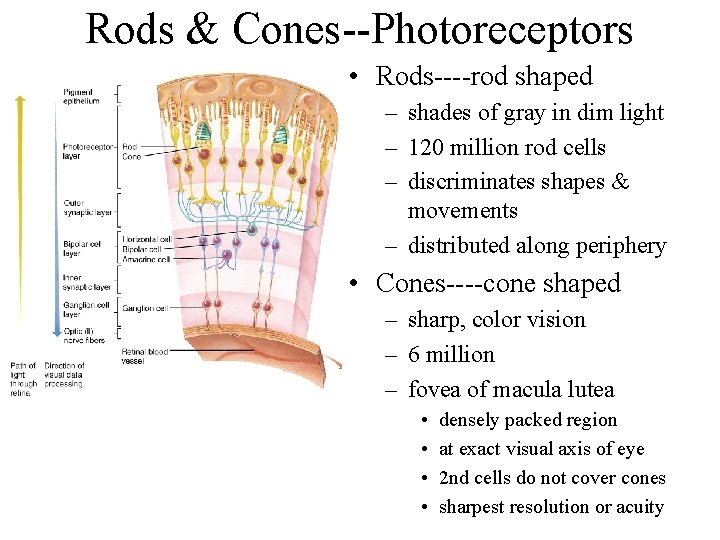
Rods & Cones--Photoreceptors • Rods----rod shaped – shades of gray in dim light – 120 million rod cells – discriminates shapes & movements – distributed along periphery • Cones----cone shaped – sharp, color vision – 6 million – fovea of macula lutea • • densely packed region at exact visual axis of eye 2 nd cells do not cover cones sharpest resolution or acuity
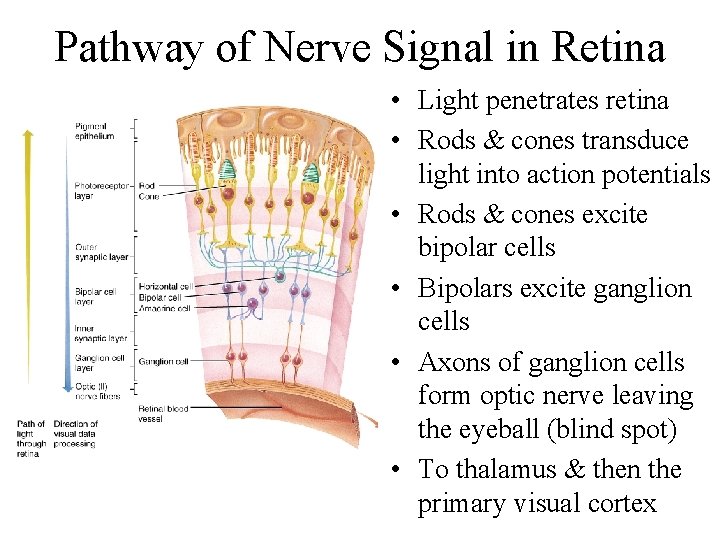
Pathway of Nerve Signal in Retina • Light penetrates retina • Rods & cones transduce light into action potentials • Rods & cones excite bipolar cells • Bipolars excite ganglion cells • Axons of ganglion cells form optic nerve leaving the eyeball (blind spot) • To thalamus & then the primary visual cortex
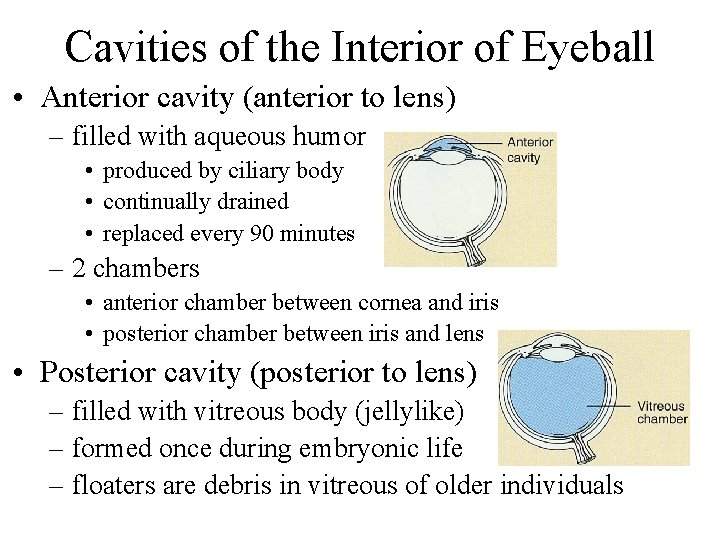
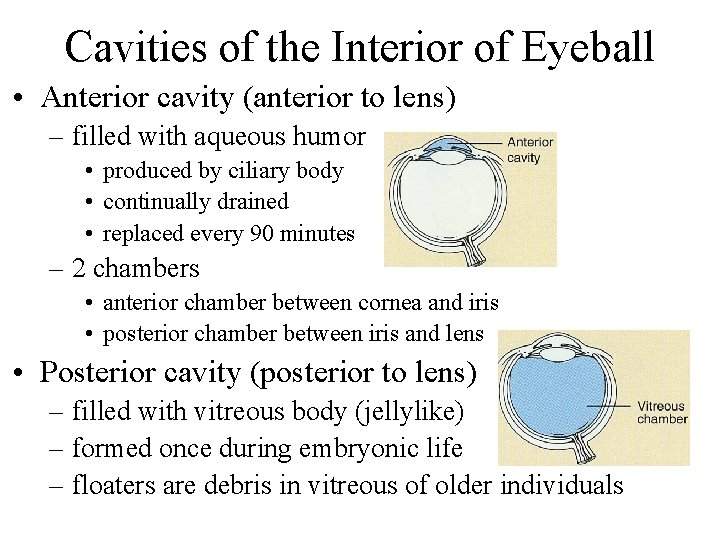
Cavities of the Interior of Eyeball • Anterior cavity (anterior to lens) – filled with aqueous humor • produced by ciliary body • continually drained • replaced every 90 minutes – 2 chambers • anterior chamber between cornea and iris • posterior chamber between iris and lens • Posterior cavity (posterior to lens) – filled with vitreous body (jellylike) – formed once during embryonic life – floaters are debris in vitreous of older individuals
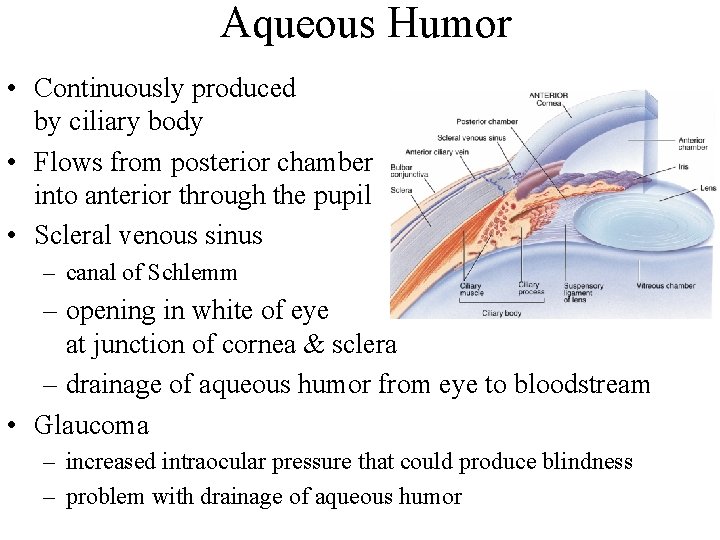
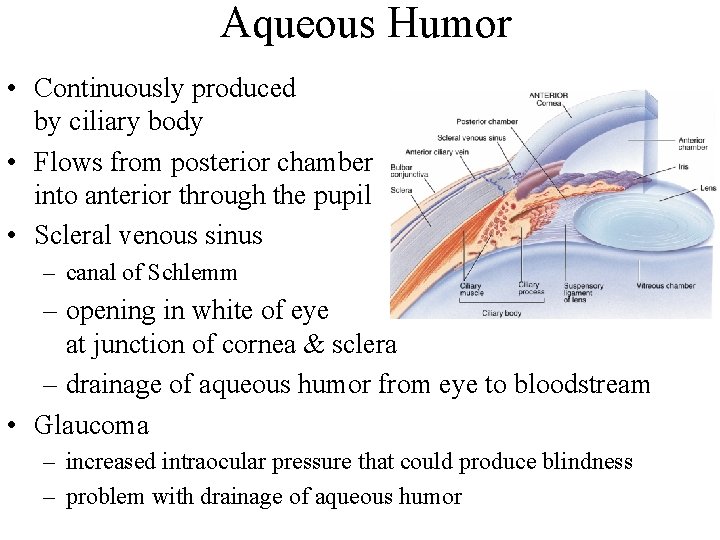
Aqueous Humor • Continuously produced by ciliary body • Flows from posterior chamber into anterior through the pupil • Scleral venous sinus – canal of Schlemm – opening in white of eye at junction of cornea & sclera – drainage of aqueous humor from eye to bloodstream • Glaucoma – increased intraocular pressure that could produce blindness – problem with drainage of aqueous humor
Major Processes of Image Formation • Refraction of light – by cornea & lens – light rays must fall upon the retina • Accommodation of the lens – changing shape of lens so that light is focused • Constriction of the pupil – less light enters the eye
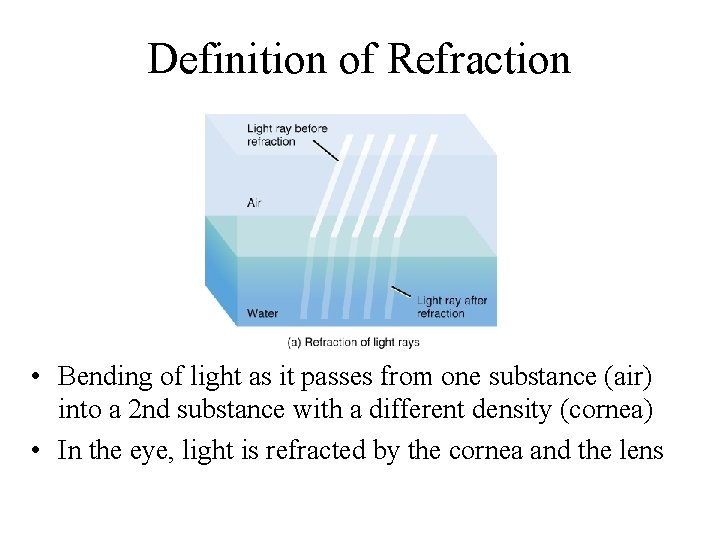
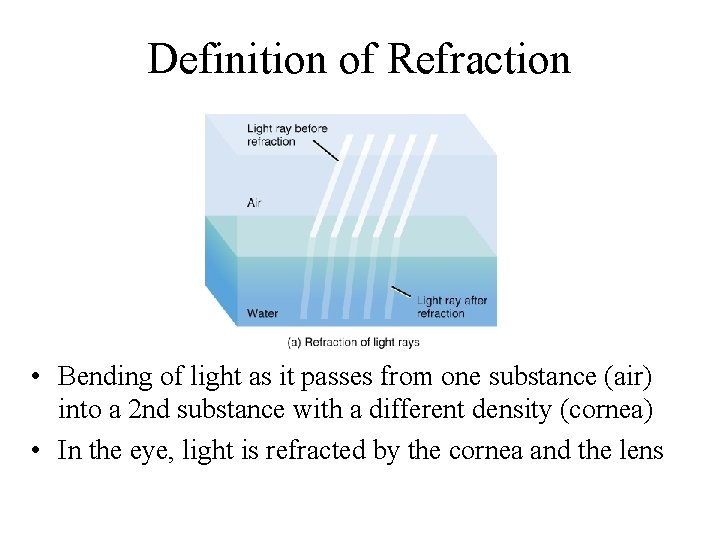
Definition of Refraction • Bending of light as it passes from one substance (air) into a 2 nd substance with a different density (cornea) • In the eye, light is refracted by the cornea and the lens
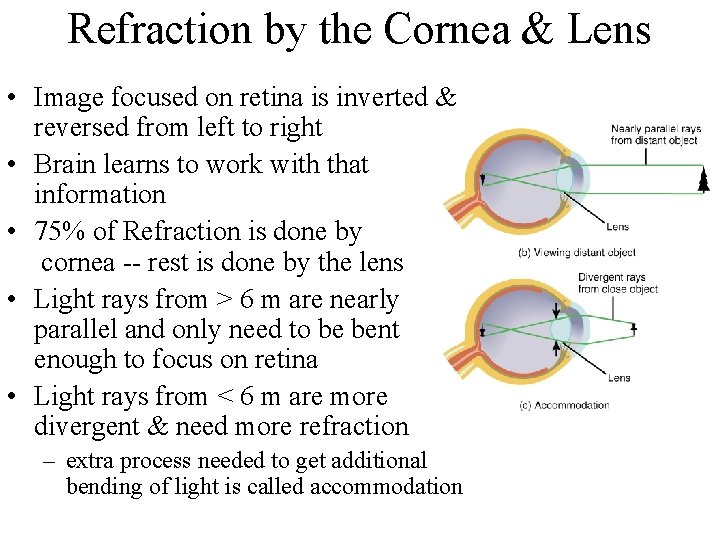
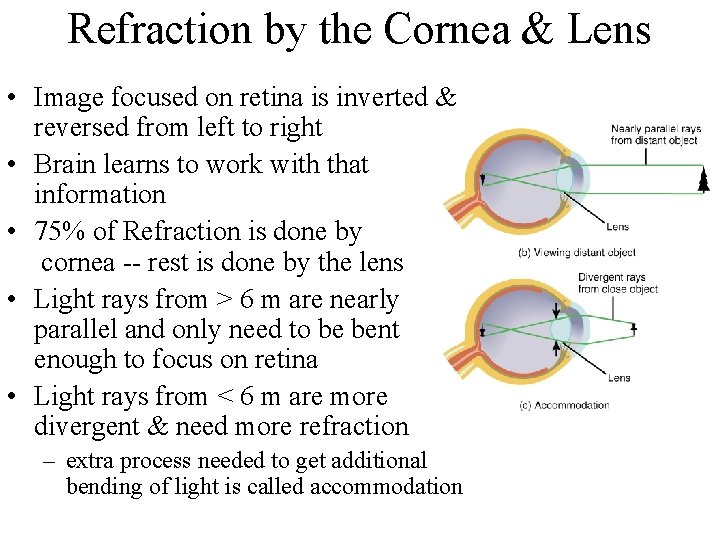
Refraction by the Cornea & Lens • Image focused on retina is inverted & reversed from left to right • Brain learns to work with that information • 75% of Refraction is done by cornea -- rest is done by the lens • Light rays from > 6 m are nearly parallel and only need to be bent enough to focus on retina • Light rays from < 6 m are more divergent & need more refraction – extra process needed to get additional bending of light is called accommodation

Accommodation & the Lens • Convex lens refract light rays towards each other • Lens of eye is convex on both surfaces • View a distant object – lens is nearly flat by pulling of suspensory ligaments • View a close object – ciliary muscle is contracted & decreases the pull of the suspensory ligaments on the lens – elastic lens thickens as the tension is removed from it – increase in curvature of lens is called accommodation
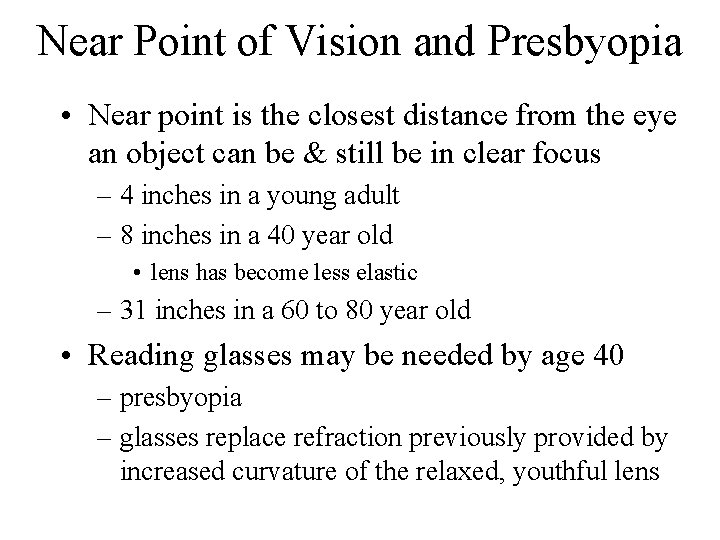
Near Point of Vision and Presbyopia • Near point is the closest distance from the eye an object can be & still be in clear focus – 4 inches in a young adult – 8 inches in a 40 year old • lens has become less elastic – 31 inches in a 60 to 80 year old • Reading glasses may be needed by age 40 – presbyopia – glasses replace refraction previously provided by increased curvature of the relaxed, youthful lens
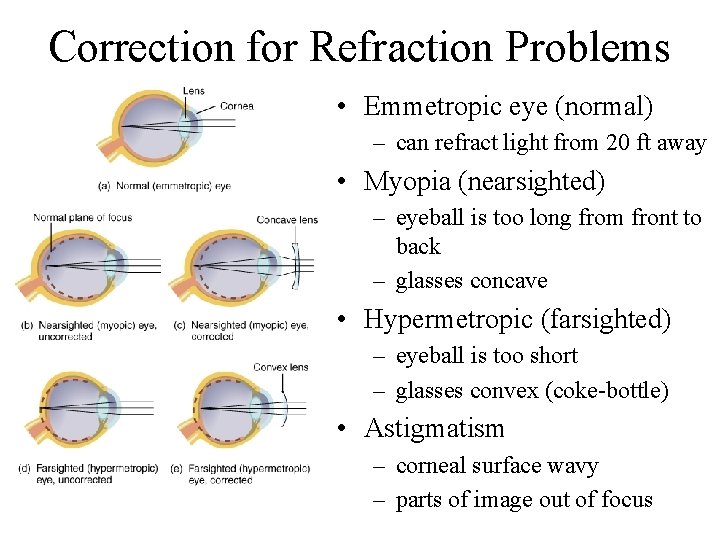
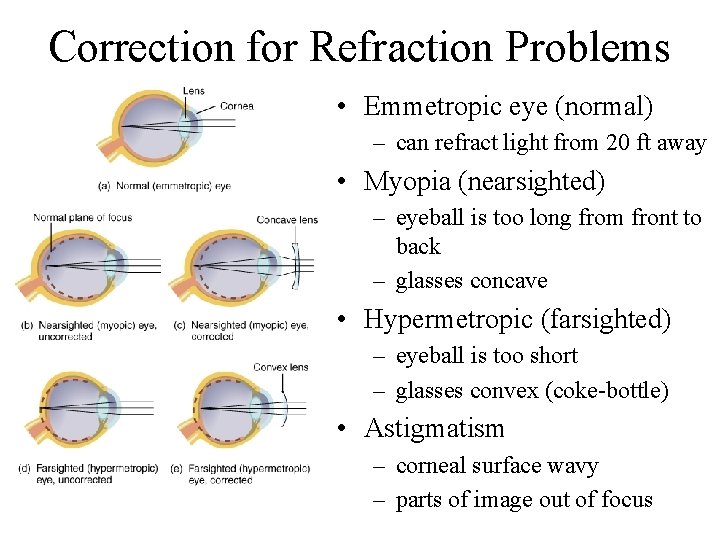
Correction for Refraction Problems • Emmetropic eye (normal) – can refract light from 20 ft away • Myopia (nearsighted) – eyeball is too long from front to back – glasses concave • Hypermetropic (farsighted) – eyeball is too short – glasses convex (coke-bottle) • Astigmatism – corneal surface wavy – parts of image out of focus
Convergence of the Eyes • Binocular vision in humans has both eyes looking at the same object • Allows for the perception of depth • As you look at an object close to your face, both eyeballs must turn inward. – convergence – required so that light rays from the object will strike both retinas at the same relative point – extrinsic eye muscles must coordinate this action
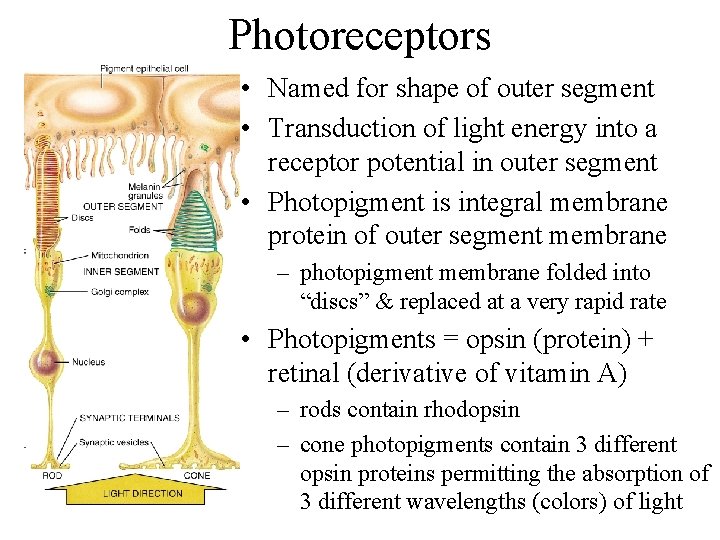
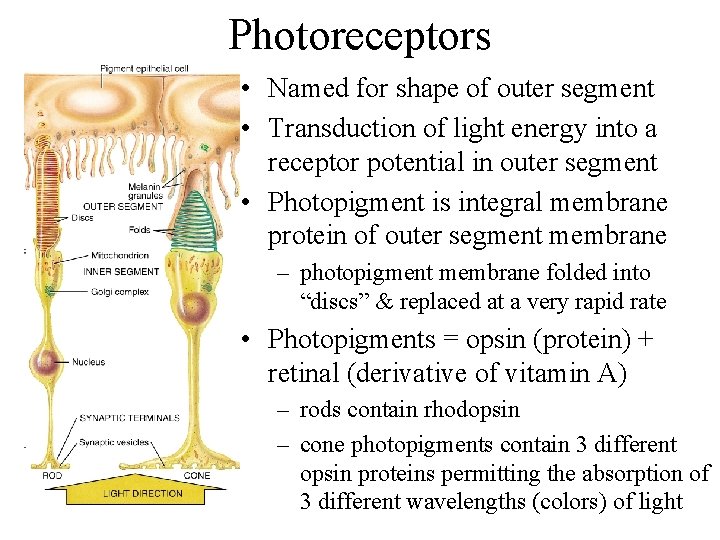
Photoreceptors • Named for shape of outer segment • Transduction of light energy into a receptor potential in outer segment • Photopigment is integral membrane protein of outer segment membrane – photopigment membrane folded into “discs” & replaced at a very rapid rate • Photopigments = opsin (protein) + retinal (derivative of vitamin A) – rods contain rhodopsin – cone photopigments contain 3 different opsin proteins permitting the absorption of 3 different wavelengths (colors) of light
Color Blindness & Night Blindness • Color blindness – inability to distinguish between certain colors – absence of certain cone photopigments – red-green color blind person can not tell red from green • Night blindness – difficulty seeing in low light – inability to make normal amount of rhodopsin – possibly due to deficiency of vitamin A

Photopigments • Isomerization – light cause cis-retinal to straighten & become transretinal shape – lead to production of receptor potential • Bleaching – enzymes separate the transretinal from the opsin – colorless final products • Regeneration – in darkness, an enzyme converts trans-retinal back to cis-retinal (resynthesis of a photopigment)
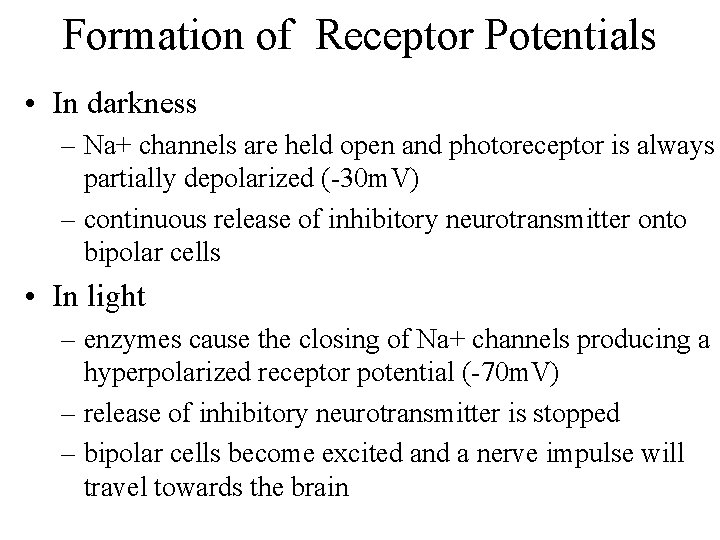
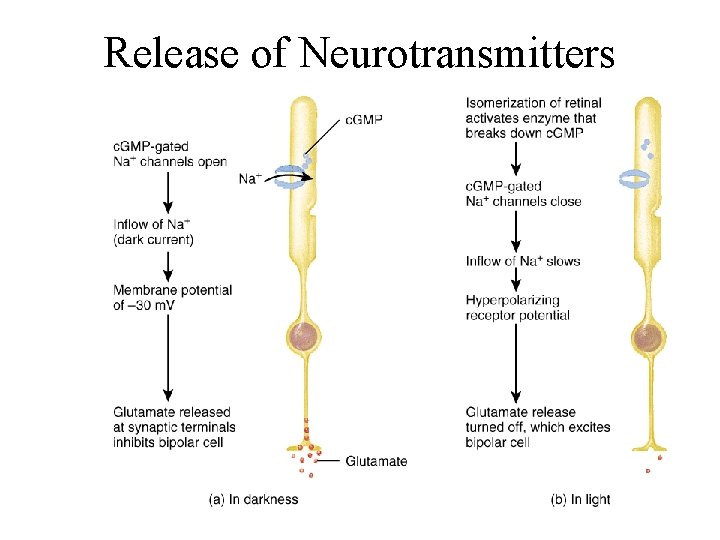
Formation of Receptor Potentials • In darkness – Na+ channels are held open and photoreceptor is always partially depolarized (-30 m. V) – continuous release of inhibitory neurotransmitter onto bipolar cells • In light – enzymes cause the closing of Na+ channels producing a hyperpolarized receptor potential (-70 m. V) – release of inhibitory neurotransmitter is stopped – bipolar cells become excited and a nerve impulse will travel towards the brain
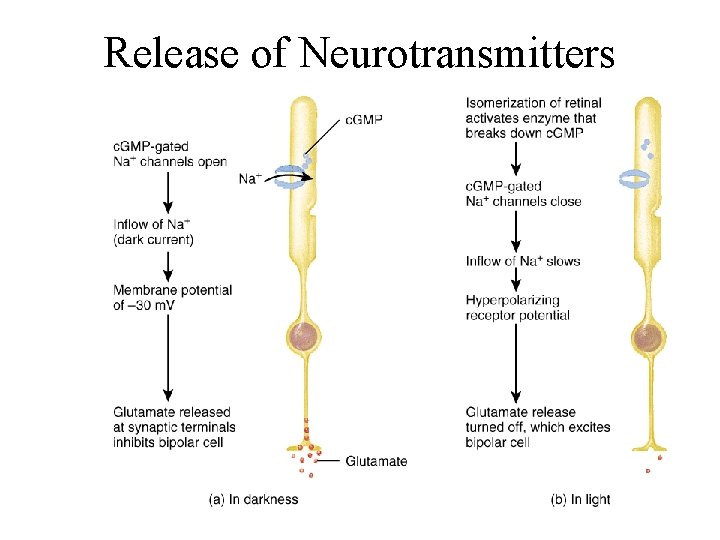
Release of Neurotransmitters
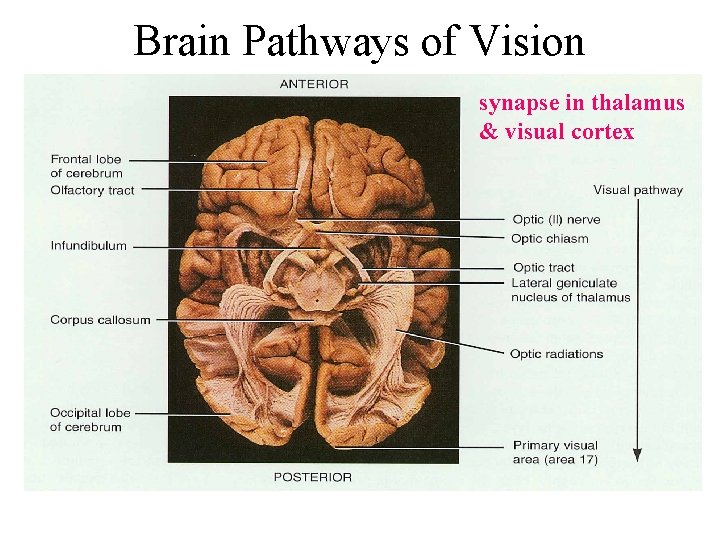
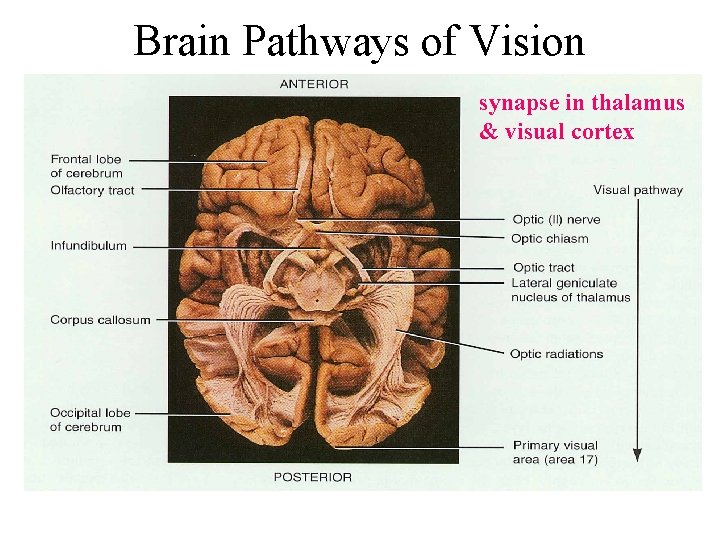
Brain Pathways of Vision synapse in thalamus & visual cortex
Processing of Image Data in the Brain • Visual information in optic nerve travels to – occipital lobe for vision – midbrain for controlling pupil size & coordination of head and eye movements – hypothalamus to establish sleep patterns based upon circadian rhythms of light and darkness
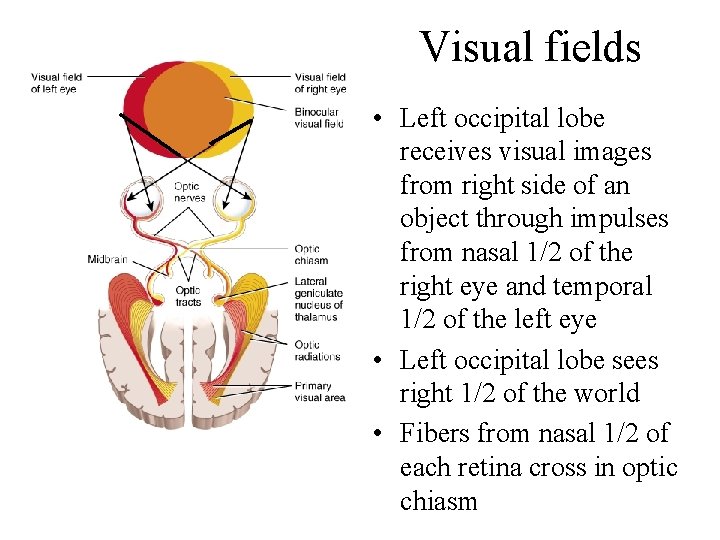
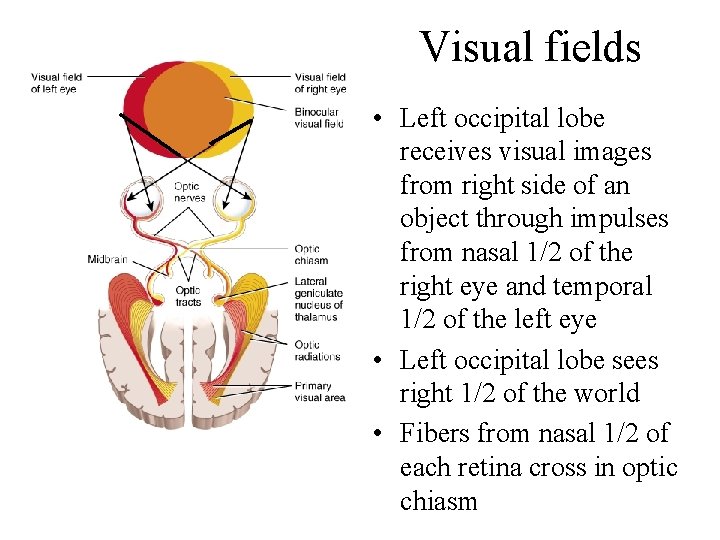
Visual fields • Left occipital lobe receives visual images from right side of an object through impulses from nasal 1/2 of the right eye and temporal 1/2 of the left eye • Left occipital lobe sees right 1/2 of the world • Fibers from nasal 1/2 of each retina cross in optic chiasm
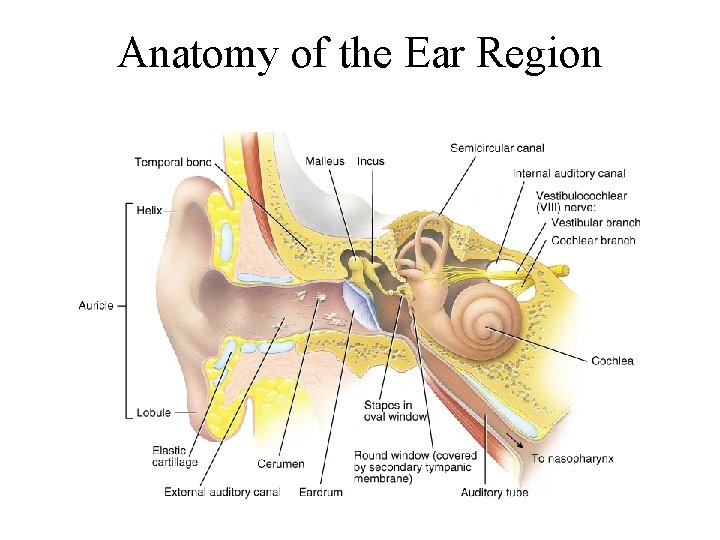
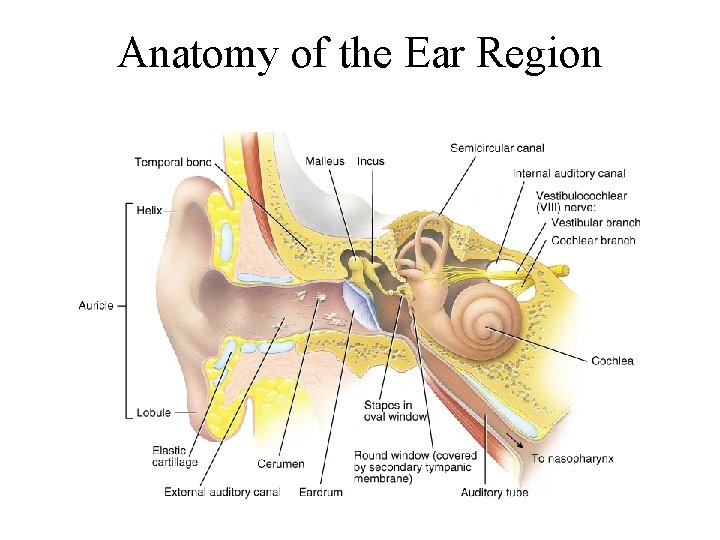
Anatomy of the Ear Region
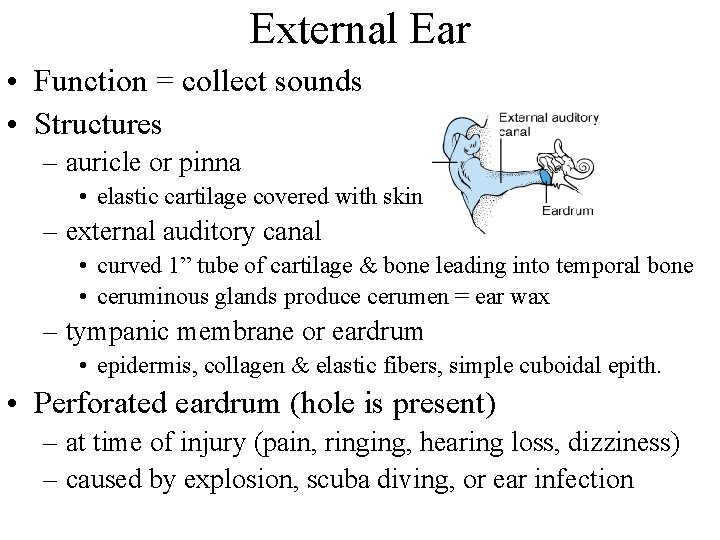
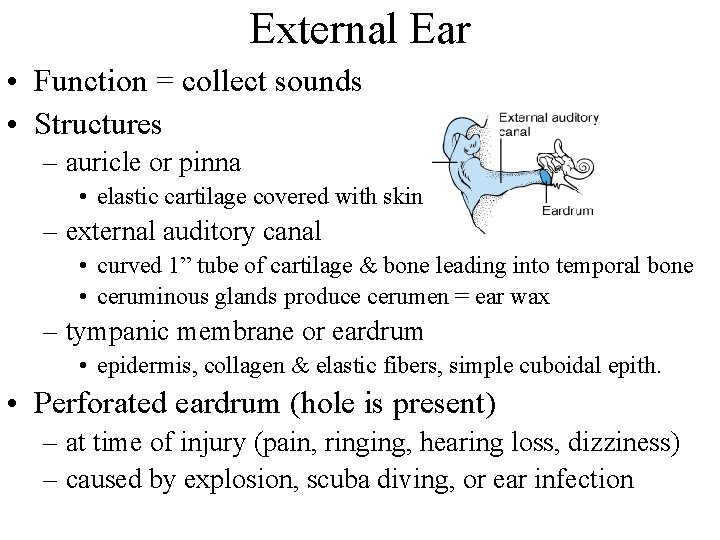
External Ear • Function = collect sounds • Structures – auricle or pinna • elastic cartilage covered with skin – external auditory canal • curved 1” tube of cartilage & bone leading into temporal bone • ceruminous glands produce cerumen = ear wax – tympanic membrane or eardrum • epidermis, collagen & elastic fibers, simple cuboidal epith. • Perforated eardrum (hole is present) – at time of injury (pain, ringing, hearing loss, dizziness) – caused by explosion, scuba diving, or ear infection
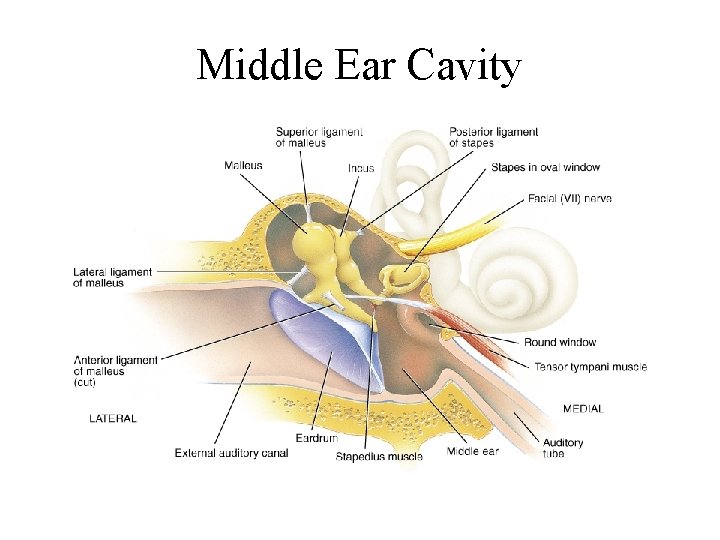
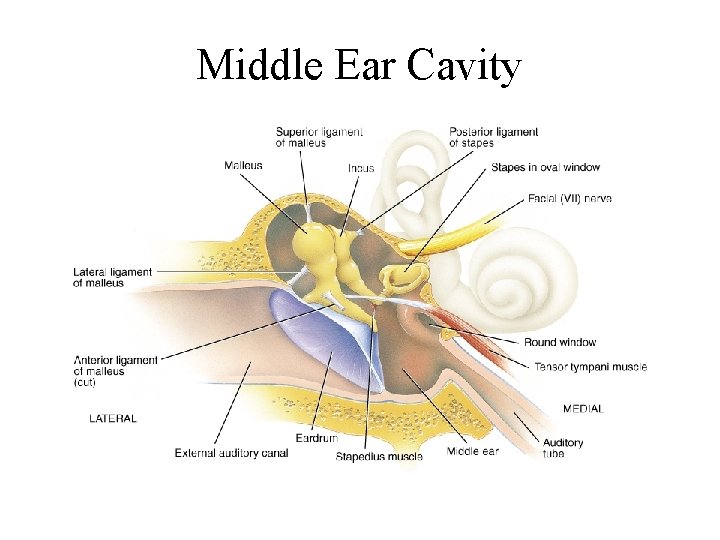
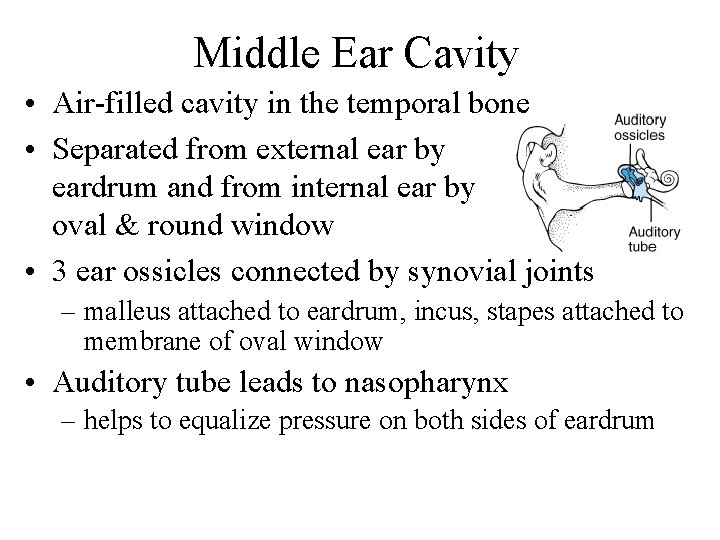
Middle Ear Cavity
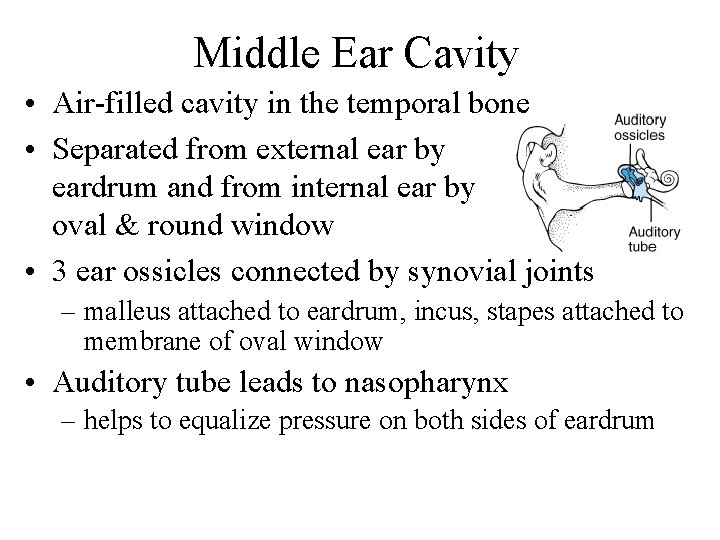
Middle Ear Cavity • Air-filled cavity in the temporal bone • Separated from external ear by eardrum and from internal ear by oval & round window • 3 ear ossicles connected by synovial joints – malleus attached to eardrum, incus, stapes attached to membrane of oval window • Auditory tube leads to nasopharynx – helps to equalize pressure on both sides of eardrum
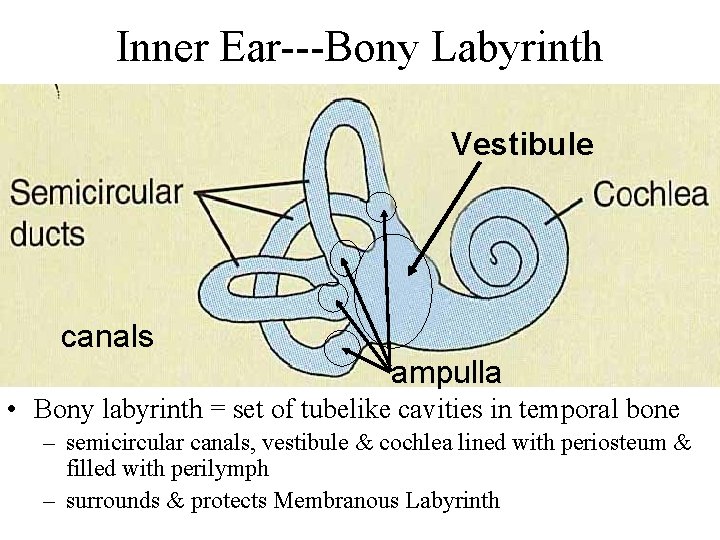
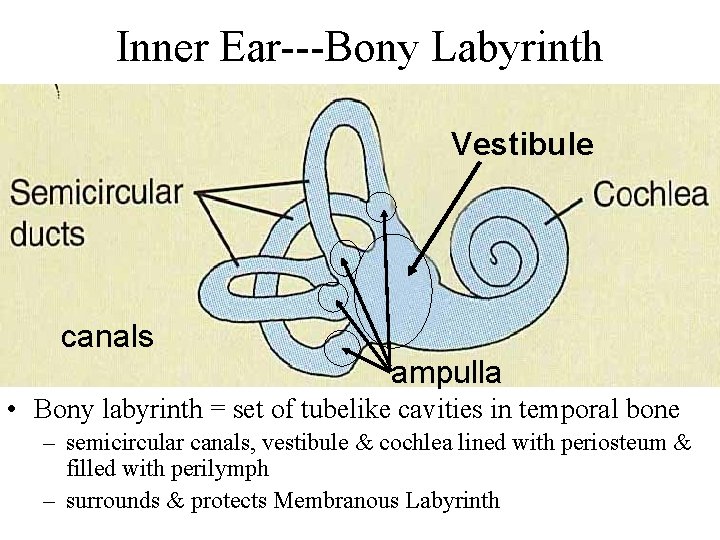
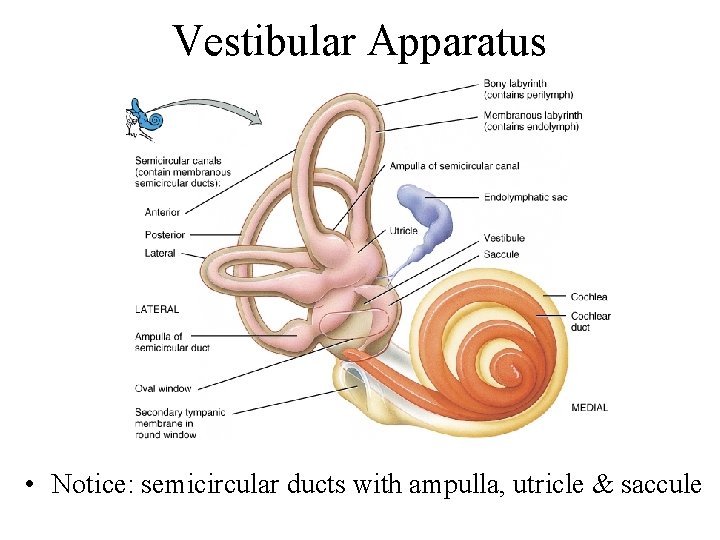
Inner Ear---Bony Labyrinth Vestibule canals ampulla • Bony labyrinth = set of tubelike cavities in temporal bone – semicircular canals, vestibule & cochlea lined with periosteum & filled with perilymph – surrounds & protects Membranous Labyrinth
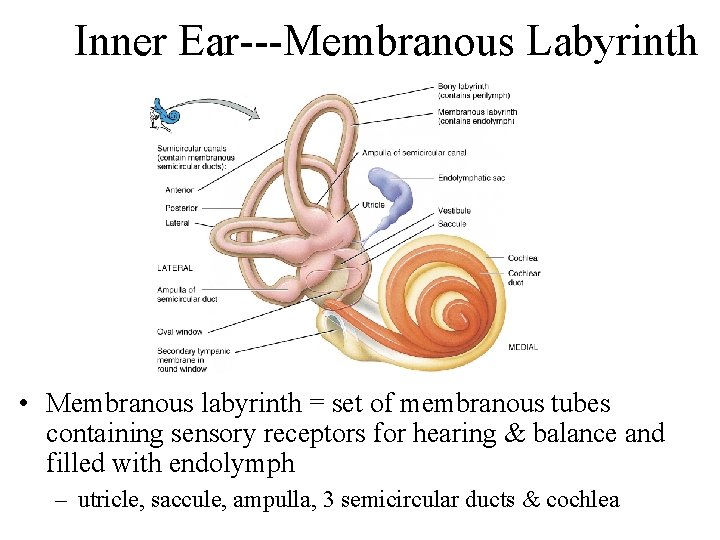
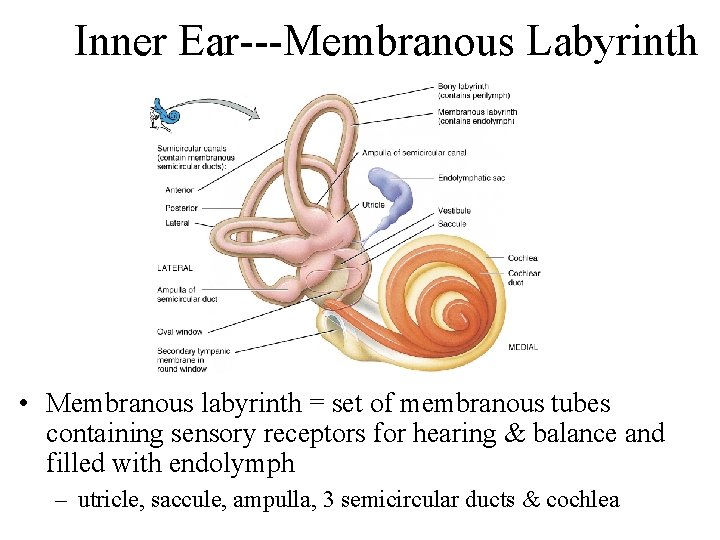
Inner Ear---Membranous Labyrinth • Membranous labyrinth = set of membranous tubes containing sensory receptors for hearing & balance and filled with endolymph – utricle, saccule, ampulla, 3 semicircular ducts & cochlea
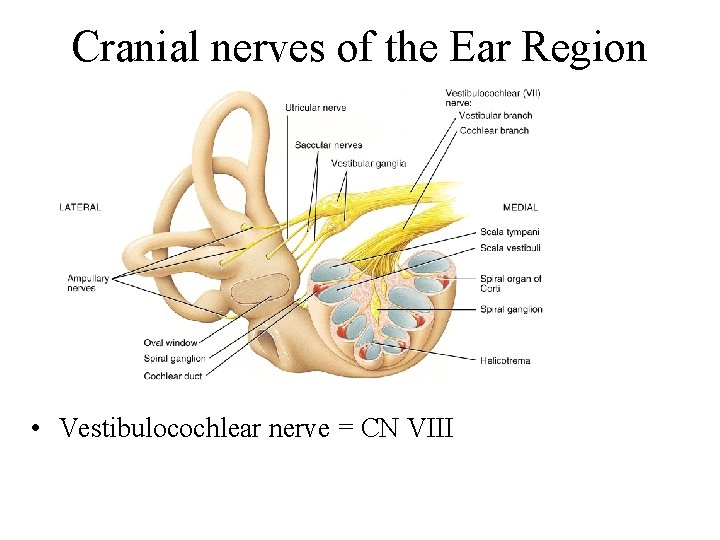
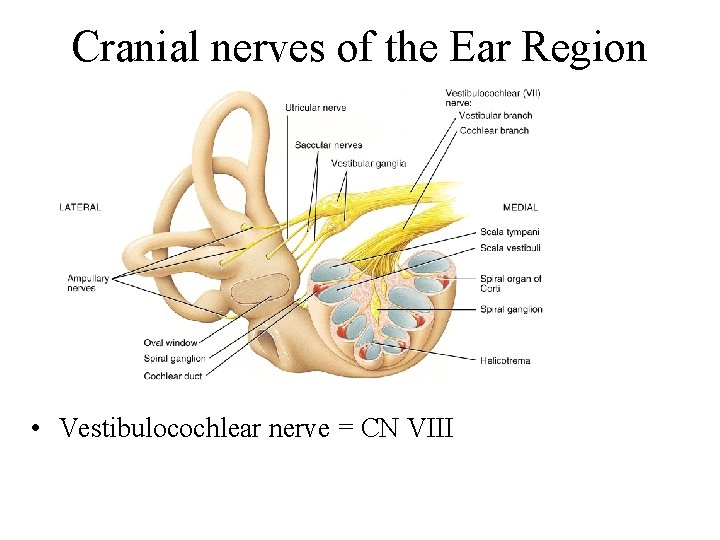
Cranial nerves of the Ear Region • Vestibulocochlear nerve = CN VIII
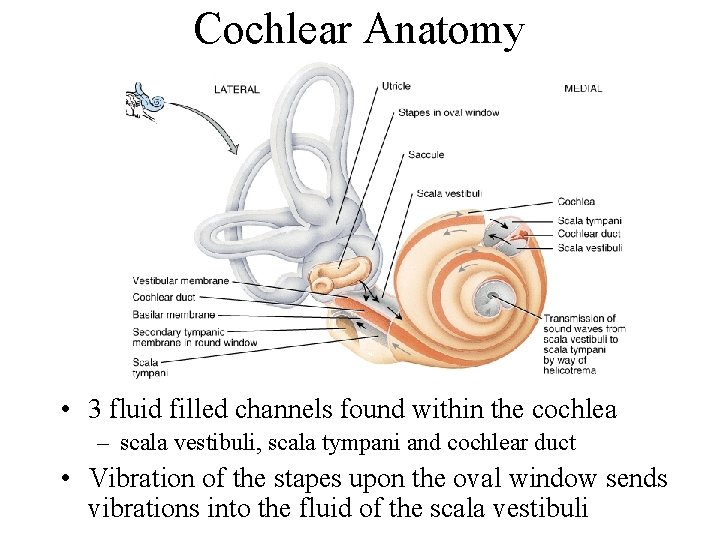
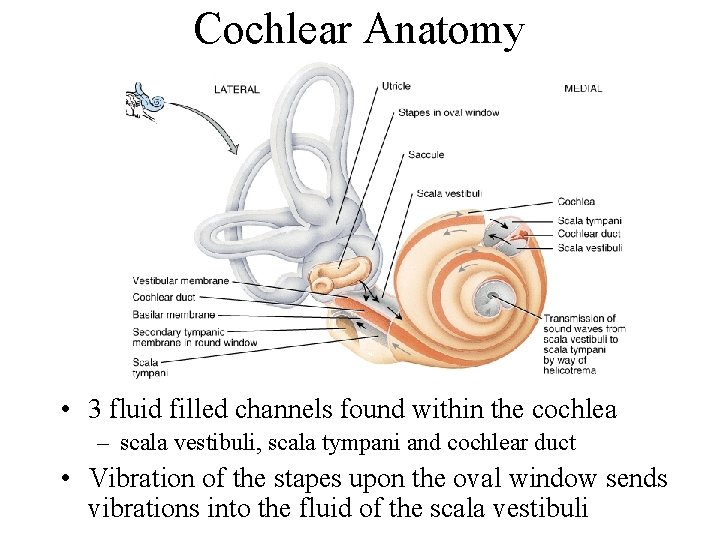
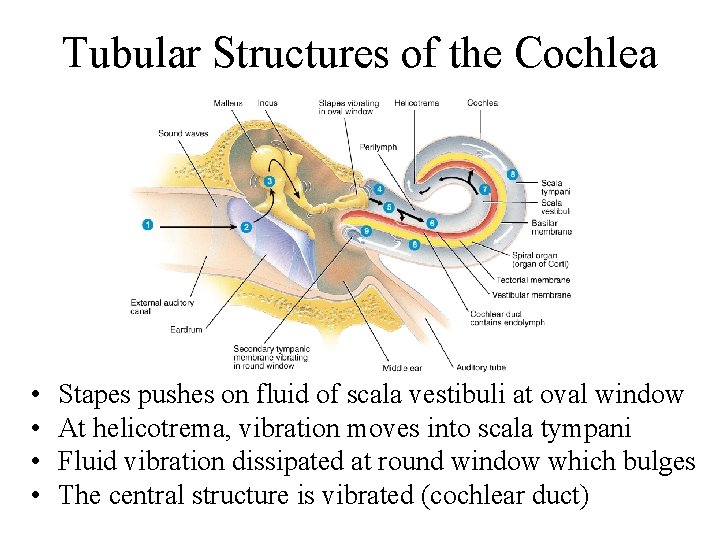
Cochlear Anatomy • 3 fluid filled channels found within the cochlea – scala vestibuli, scala tympani and cochlear duct • Vibration of the stapes upon the oval window sends vibrations into the fluid of the scala vestibuli
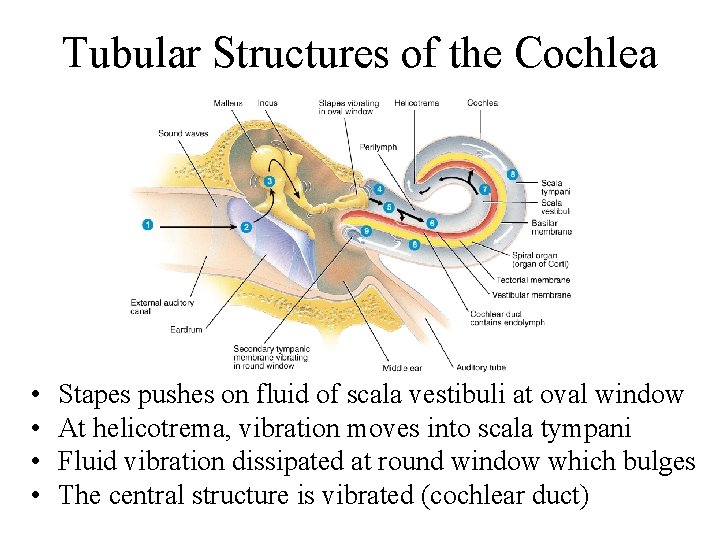
Tubular Structures of the Cochlea • • Stapes pushes on fluid of scala vestibuli at oval window At helicotrema, vibration moves into scala tympani Fluid vibration dissipated at round window which bulges The central structure is vibrated (cochlear duct)

Section thru one turn of Cochlea • Partitions that separate the channels are Y shaped – vestibular membrane above & basilar membrane below form the central fluid filled chamber (cochlear duct) • Fluid vibrations affect hair cells in cochlear duct
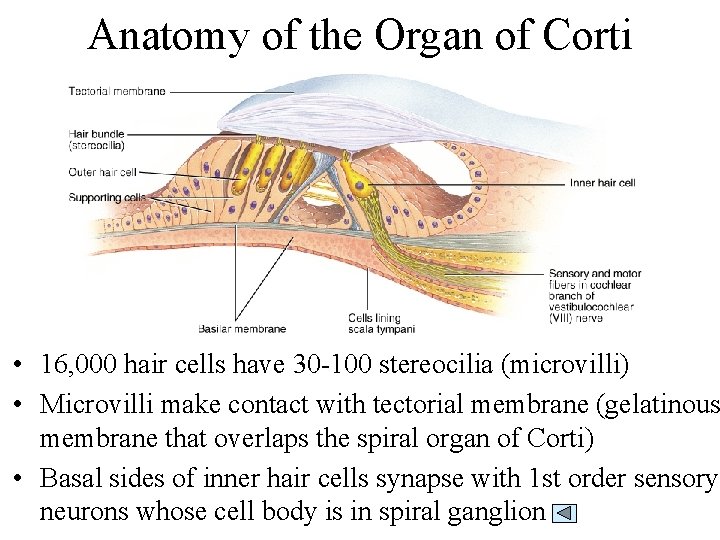
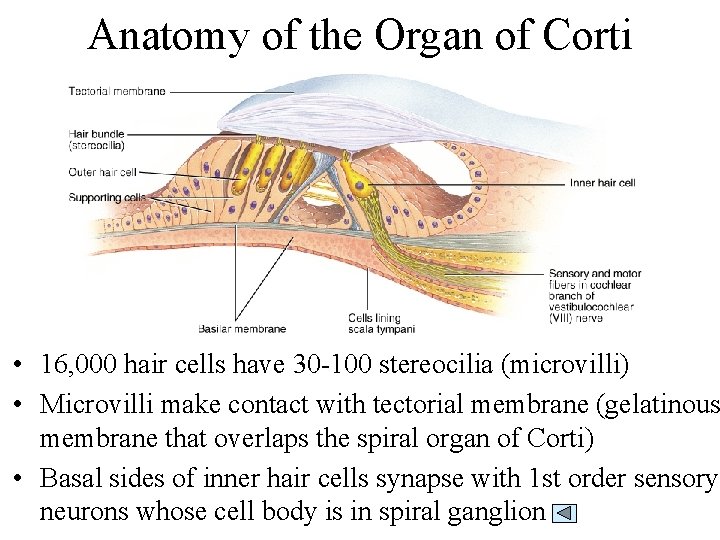
Anatomy of the Organ of Corti • 16, 000 hair cells have 30 -100 stereocilia (microvilli) • Microvilli make contact with tectorial membrane (gelatinous membrane that overlaps the spiral organ of Corti) • Basal sides of inner hair cells synapse with 1 st order sensory neurons whose cell body is in spiral ganglion
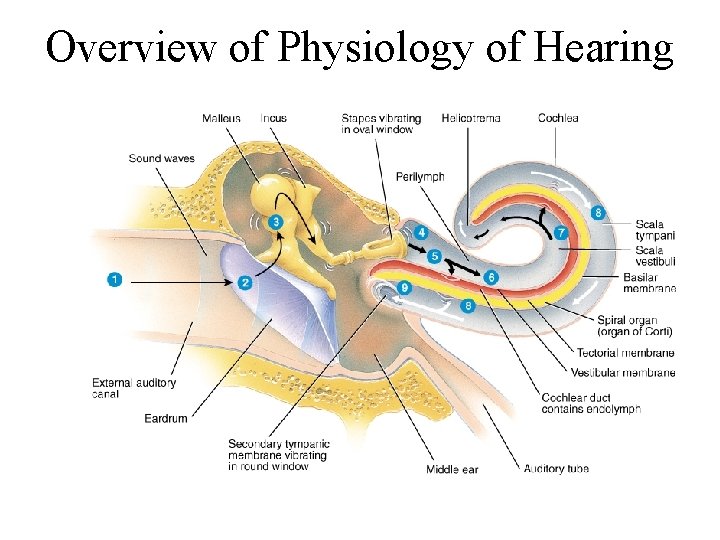
Physiology of Hearing • Auricle collects sound waves • Eardrum vibrates – slow vibration in response to low-pitched sounds – rapid vibration in response to high-pitched sounds • Ossicles vibrate since malleus attached to eardrum • Stapes pushes on oval window producing fluid pressure waves in scala vestibuli & tympani – oval window vibration 20 X more vigorous than eardrum • Pressure fluctuations inside cochlear duct move the hair cells against the tectorial membrane • Microvilli are bent producing receptor potentials
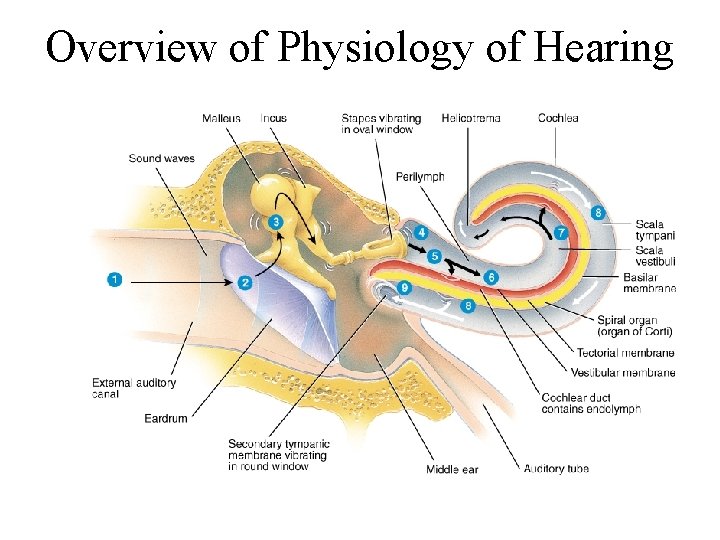
Overview of Physiology of Hearing
Hair Cell Physiology • Hair cells convert mechanical deformation into electrical signals • As microvilli are bent, mechanically-gated channels in the membrane let in K+ ions • This depolarization spreads & causes voltagegated Ca+2 channels at the base of the cell to open • Triggering the release of neurotransmitter onto the first order neuron – more neurotransmitter means more nerve impulses
Cochlear Implants • If deafness is due to destruction of hair cells • Microphone, microprocessor & electrodes translate sounds into electric stimulation of the vestibulocochlear nerve – artificially induced nerve signals follow normal pathways to brain • Provides only a crude representation of sounds
Physiology of Equilibrium (Balance) • Static equilibrium – maintain the position of the body (head) relative to the force of gravity – macula receptors within saccule & utricle • Dynamic equilibrium – maintain body position (head) during sudden movement of any type--rotation, deceleration or acceleration – crista receptors within ampulla of semicircular ducts
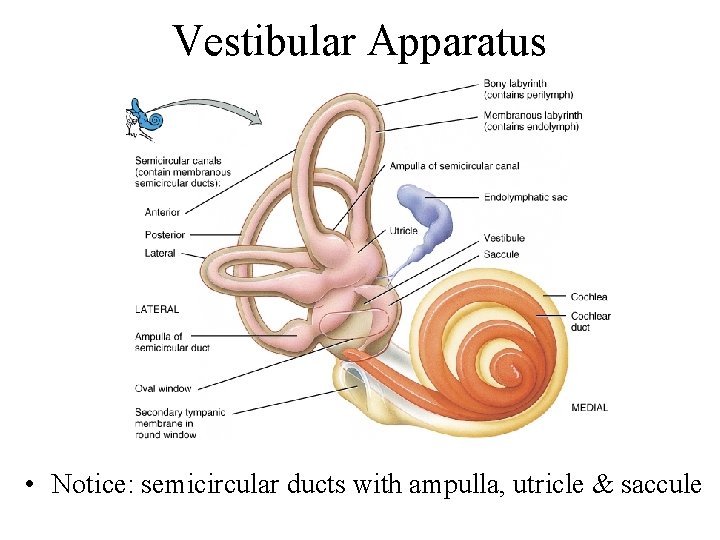
Vestibular Apparatus • Notice: semicircular ducts with ampulla, utricle & saccule
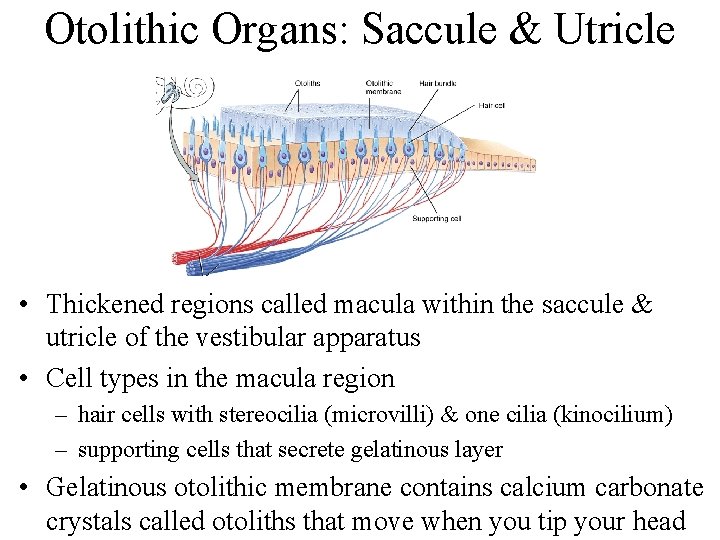
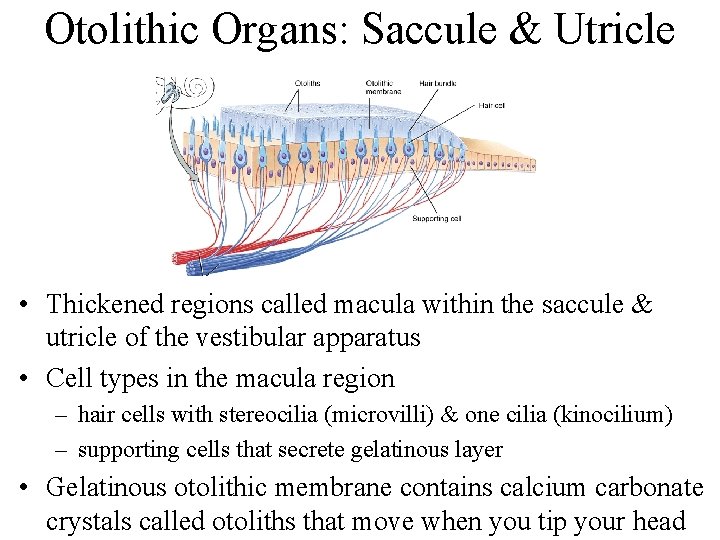
Otolithic Organs: Saccule & Utricle • Thickened regions called macula within the saccule & utricle of the vestibular apparatus • Cell types in the macula region – hair cells with stereocilia (microvilli) & one cilia (kinocilium) – supporting cells that secrete gelatinous layer • Gelatinous otolithic membrane contains calcium carbonate crystals called otoliths that move when you tip your head
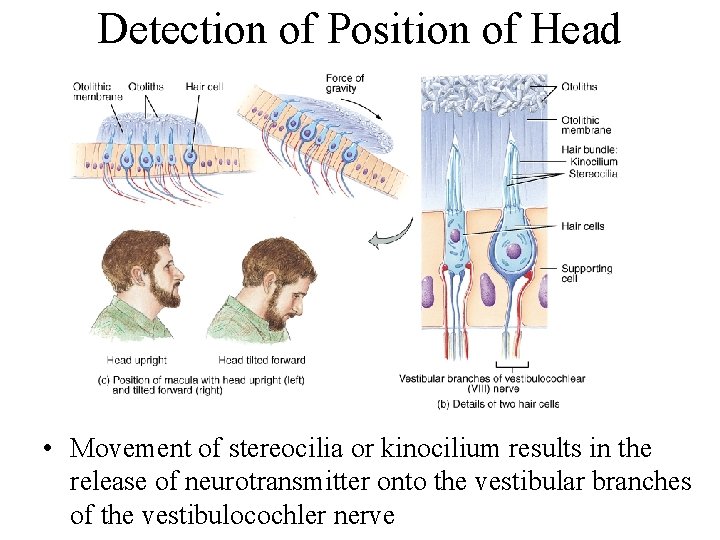
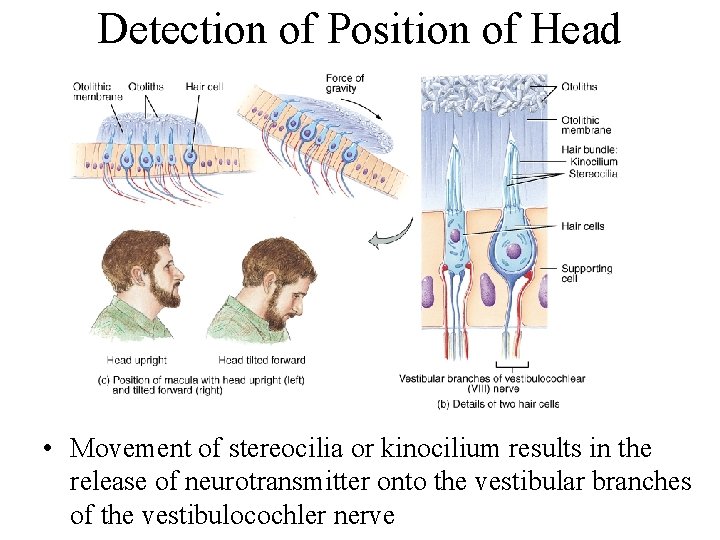
Detection of Position of Head • Movement of stereocilia or kinocilium results in the release of neurotransmitter onto the vestibular branches of the vestibulocochler nerve
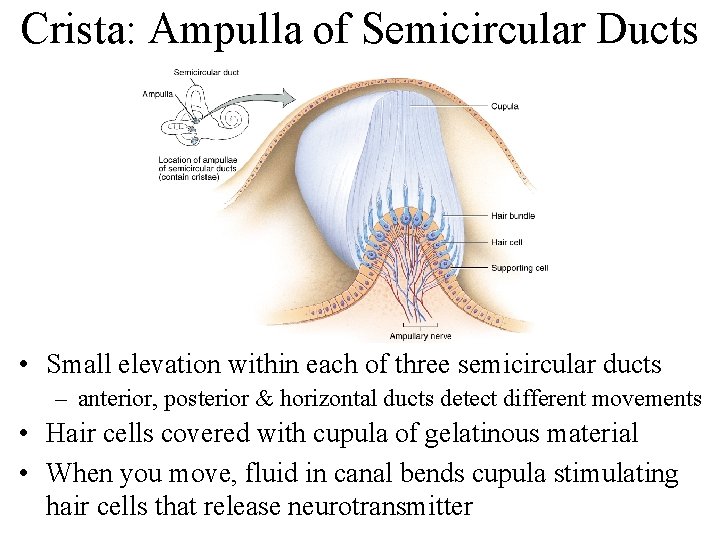
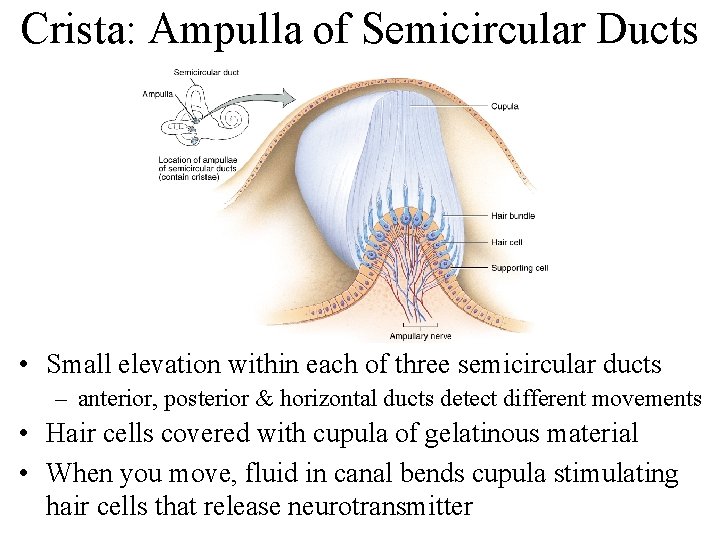
Crista: Ampulla of Semicircular Ducts • Small elevation within each of three semicircular ducts – anterior, posterior & horizontal ducts detect different movements • Hair cells covered with cupula of gelatinous material • When you move, fluid in canal bends cupula stimulating hair cells that release neurotransmitter
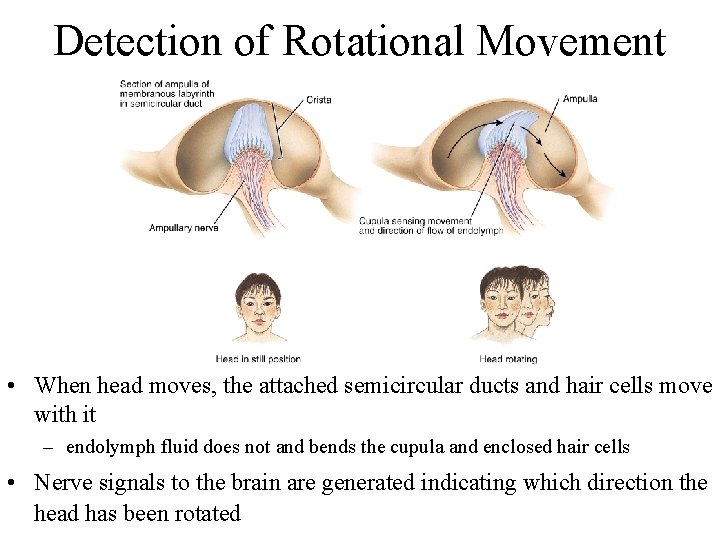
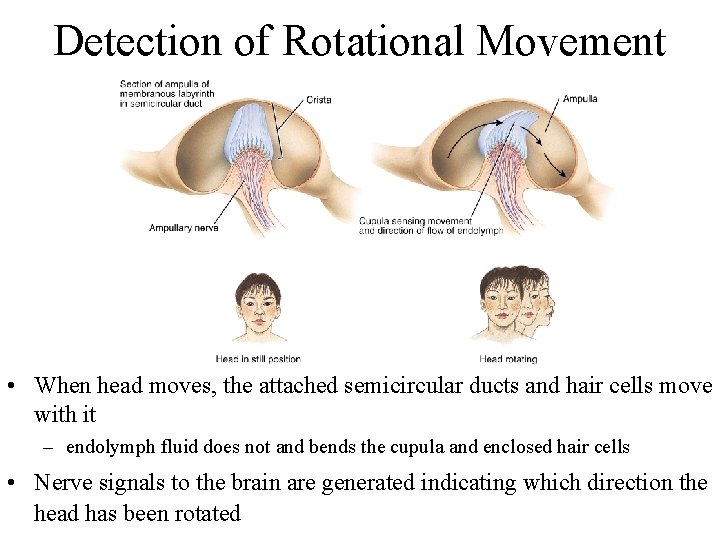
Detection of Rotational Movement • When head moves, the attached semicircular ducts and hair cells move with it – endolymph fluid does not and bends the cupula and enclosed hair cells • Nerve signals to the brain are generated indicating which direction the head has been rotated
 Beach side sight
Beach side sight The chemical senses taste and smell review worksheet
The chemical senses taste and smell review worksheet What is the difference between somatic and special senses
What is the difference between somatic and special senses Special vs general senses
Special vs general senses Flow chart of taste and smell
Flow chart of taste and smell 5 taste senses
5 taste senses Chapter 42 hearing speech and vision problems
Chapter 42 hearing speech and vision problems Chapter 10 somatic and special senses
Chapter 10 somatic and special senses Learning exercises chapter 11 medical terminology
Learning exercises chapter 11 medical terminology Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses Cn 3 nerve
Cn 3 nerve Ear bone structure
Ear bone structure Somatic senses
Somatic senses Special senses the eyes and ears
Special senses the eyes and ears The general and special senses chapter 9
The general and special senses chapter 9 Medico dental vision hearing
Medico dental vision hearing Bio 137
Bio 137 Anatomy labeled
Anatomy labeled The cones of the retina are coursera quiz answers
The cones of the retina are coursera quiz answers Chapter 17 special senses answer key
Chapter 17 special senses answer key Eye anatomy
Eye anatomy Special senses quiz
Special senses quiz Palpebral fissure
Palpebral fissure Signal conclusion
Signal conclusion Building vocabulary activity: the special senses
Building vocabulary activity: the special senses Building vocabulary activity: the special senses
Building vocabulary activity: the special senses Houses the receptors for hearing
Houses the receptors for hearing Emmentropia
Emmentropia Modiolus
Modiolus Chapter 15 special senses
Chapter 15 special senses Human vision vs computer vision
Human vision vs computer vision State-of-being verbs
State-of-being verbs Smell of apple
Smell of apple Talcum powder vs cornstarch
Talcum powder vs cornstarch Code smell
Code smell Code smells bloaters
Code smells bloaters Do owls have a sense of smell
Do owls have a sense of smell Once upon a time there was a boy named
Once upon a time there was a boy named How many miles away can a shark smell blood
How many miles away can a shark smell blood Postpartum hemorrhage treatment drugs
Postpartum hemorrhage treatment drugs What does carbonara smell like
What does carbonara smell like Grey discharge no smell
Grey discharge no smell Ester formation
Ester formation Melena smell
Melena smell Lochia assessment
Lochia assessment Colitas hotel california meaning
Colitas hotel california meaning Connotation of smell
Connotation of smell Tactile imagery
Tactile imagery Chemical and physical properties
Chemical and physical properties