TEVAR Dissections and Aneurysms Christian Shults MD Assistant




































- Slides: 56
TEVAR: Dissections and Aneurysms Christian Shults, MD Assistant Professor, Georgetown School of Medicine Co-Director, Aortic Surgery Director Surgical Ablation Medstar Heart and Vascular Institute

Christian Shults, MD I have no relevant financial relationships




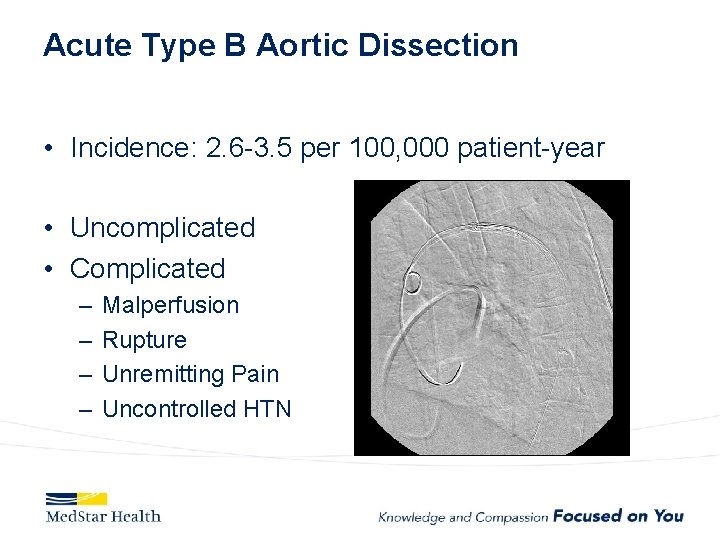
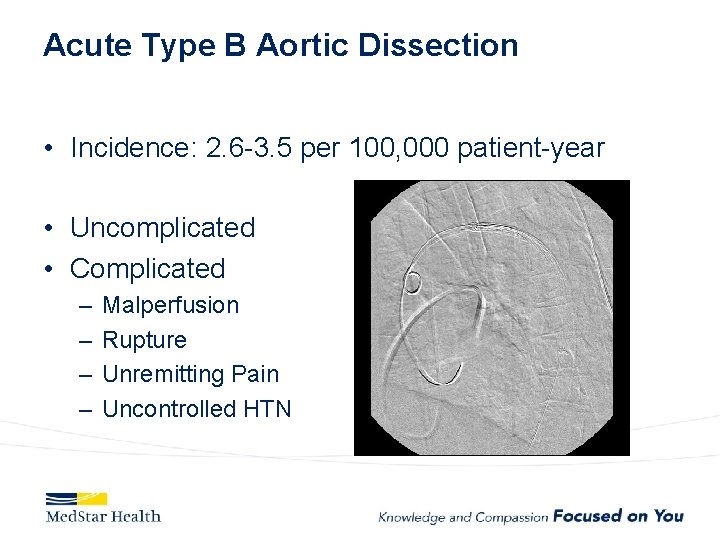
Acute Type B Aortic Dissection • Incidence: 2. 6 -3. 5 per 100, 000 patient-year • Uncomplicated • Complicated – – Malperfusion Rupture Unremitting Pain Uncontrolled HTN
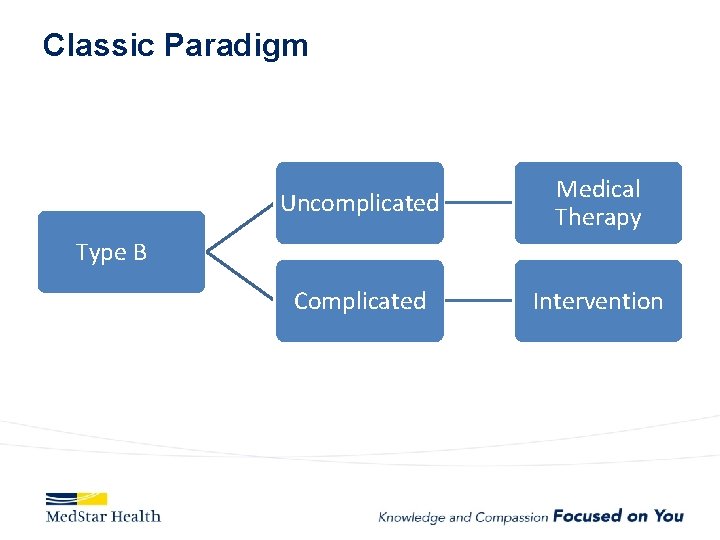
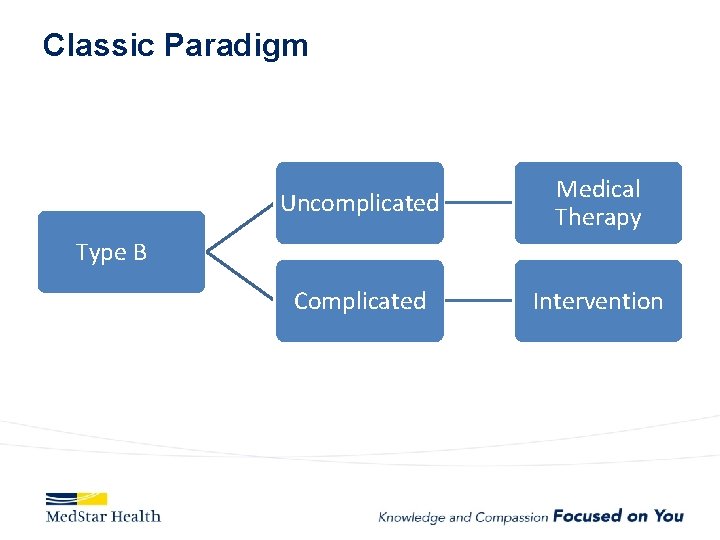
Classic Paradigm Uncomplicated Medical Therapy Complicated Intervention Type B
Uncomplicated – Medical Treatment • • • Labetalol Drip (SBP <120 mm. Hg) Nicardipine Drip Pain Control Serial Exams Labs (Creatinine, Base Deficit, Lactate) Follow up imaging (CTA @ Prior to Discharge, 1, 3, 6, 12 months)
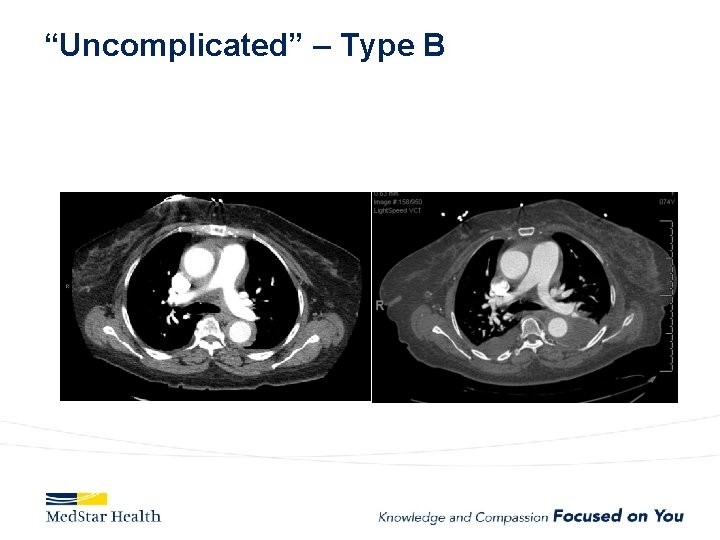
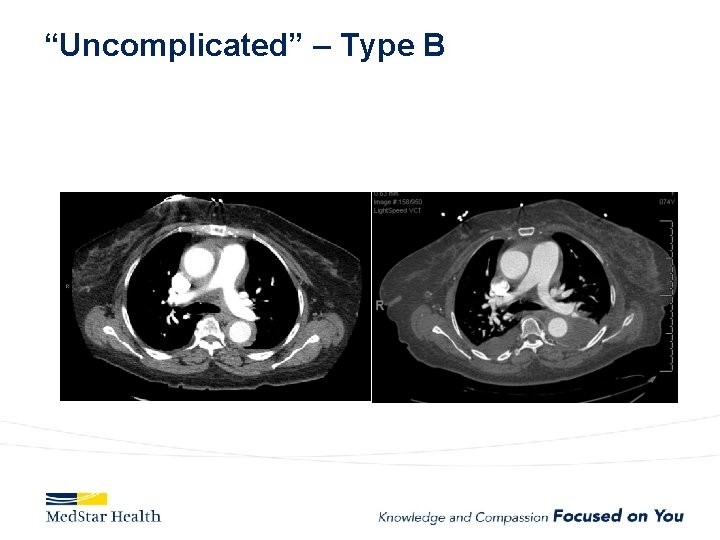
“Uncomplicated” – Type B
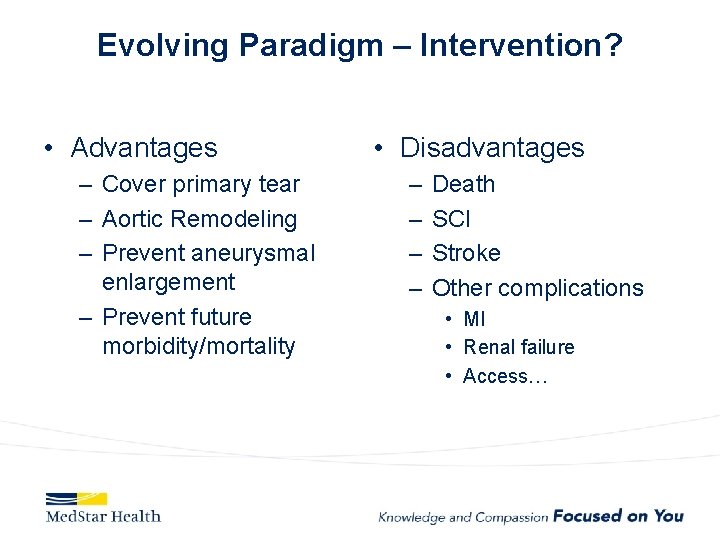
Evolving Paradigm – Intervention? • Advantages – Cover primary tear – Aortic Remodeling – Prevent aneurysmal enlargement – Prevent future morbidity/mortality • Disadvantages – – Death SCI Stroke Other complications • MI • Renal failure • Access…
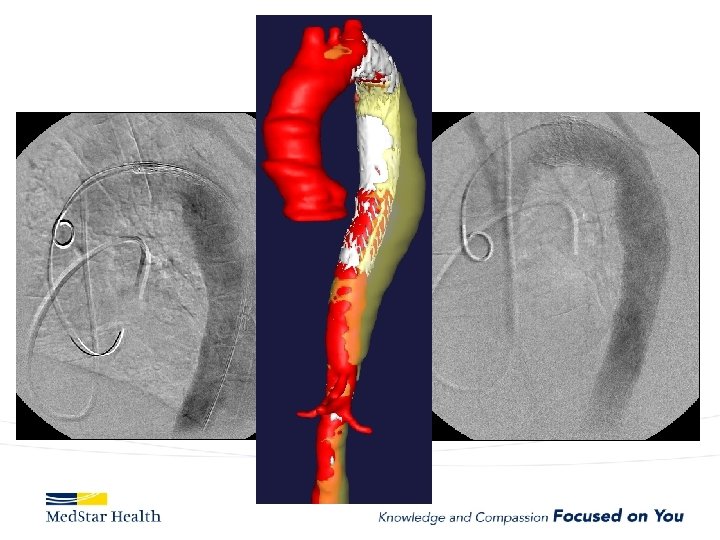
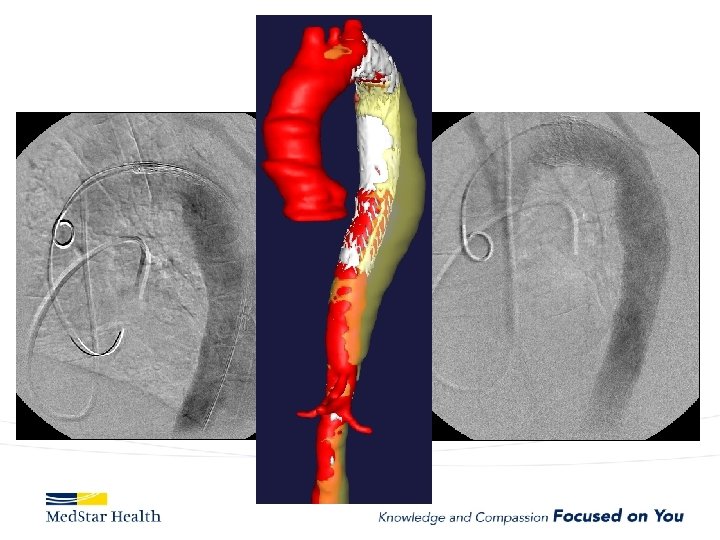
FL

Do We Treat? Who Do We Treat? How Do We Treat?

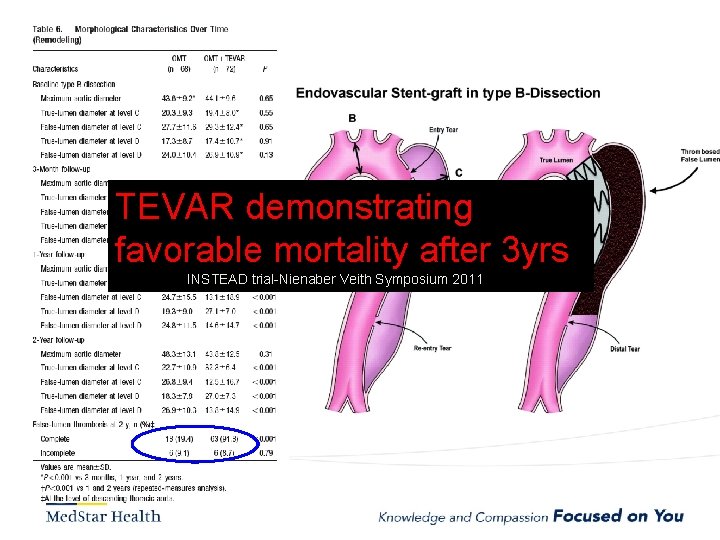
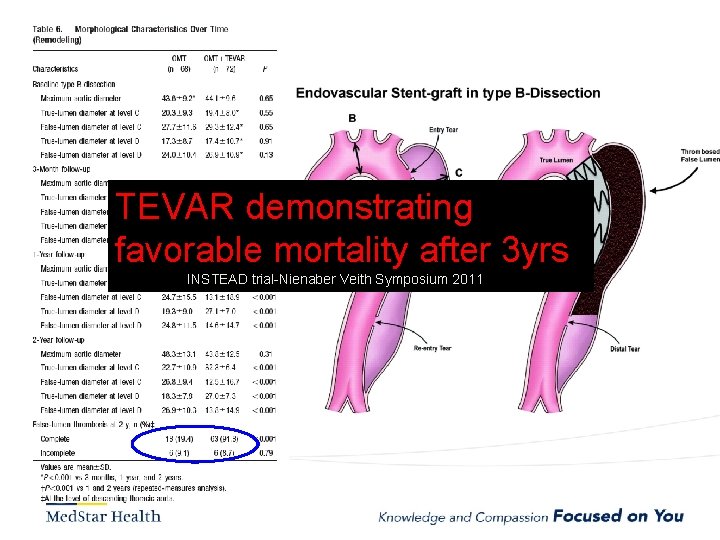
TEVAR demonstrating favorable mortality after 3 yrs INSTEAD trial-Nienaber Veith Symposium 2011
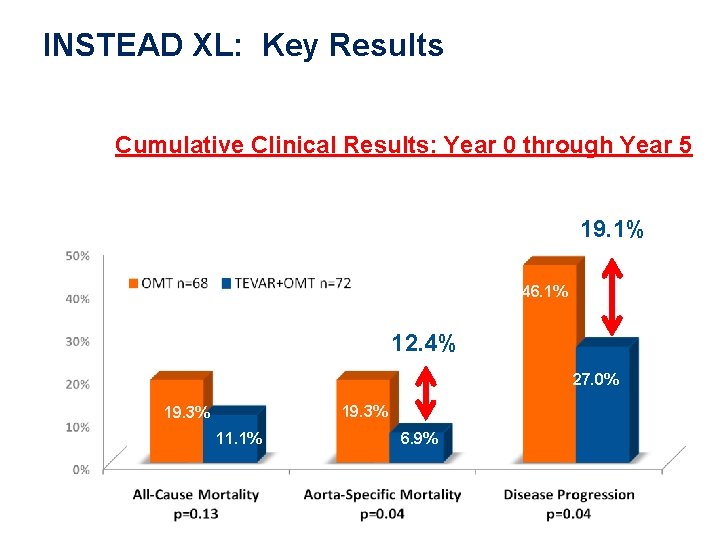
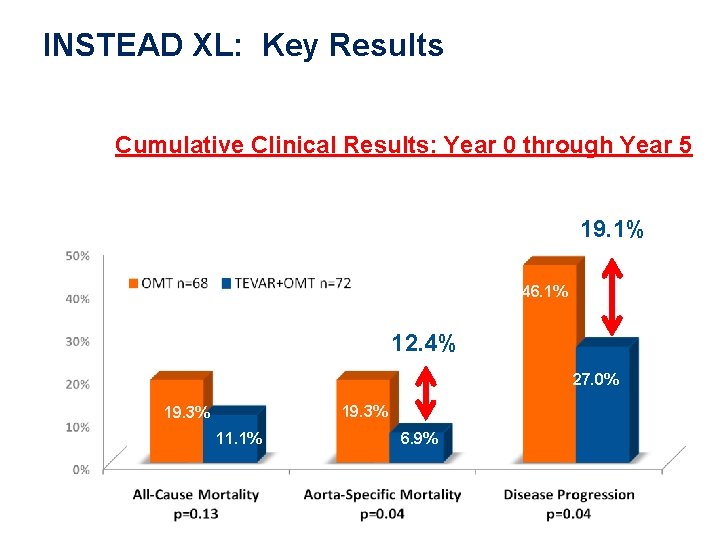
Clinical Evidence INSTEAD XL: Key Results Cumulative Clinical Results: Year 0 through Year 5 19. 1% 46. 1% 12. 4% 27. 0% 19. 3% 11. 1% 6. 9%
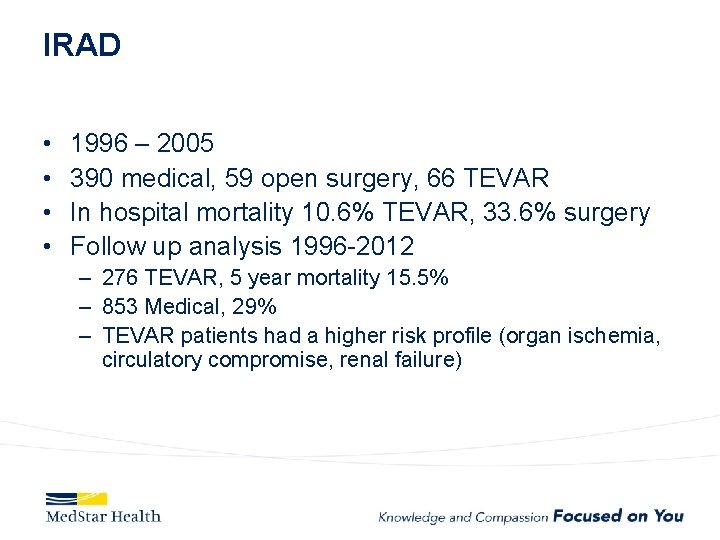
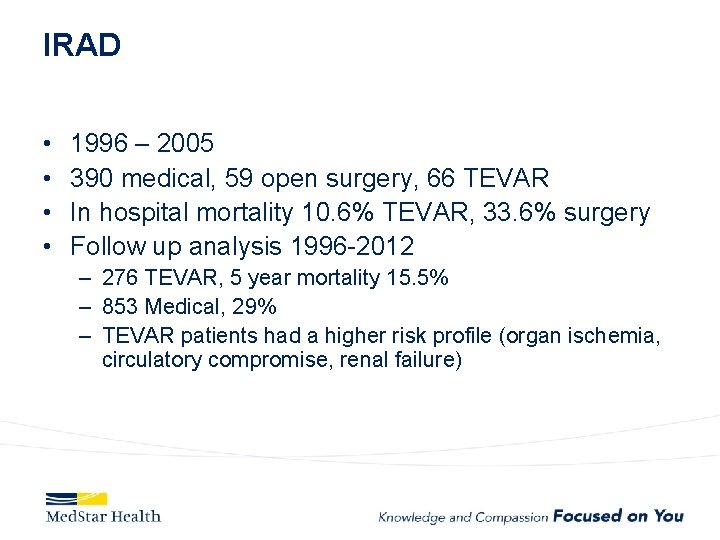
IRAD • • 1996 – 2005 390 medical, 59 open surgery, 66 TEVAR In hospital mortality 10. 6% TEVAR, 33. 6% surgery Follow up analysis 1996 -2012 – 276 TEVAR, 5 year mortality 15. 5% – 853 Medical, 29% – TEVAR patients had a higher risk profile (organ ischemia, circulatory compromise, renal failure)

Who Do We Treat?





How Do We Treat • Open repair-unacceptable morbidity and mortality • TEVAR – Improved morbidity and mortality – Coverage of primary entry tear – Additional coverage?

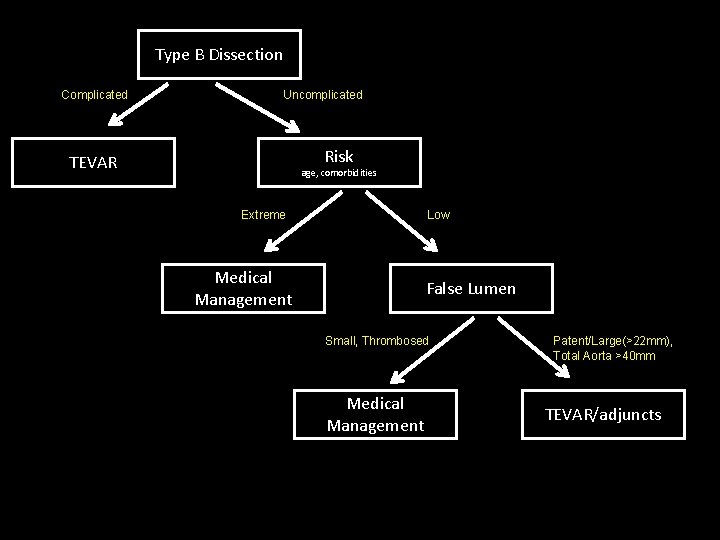
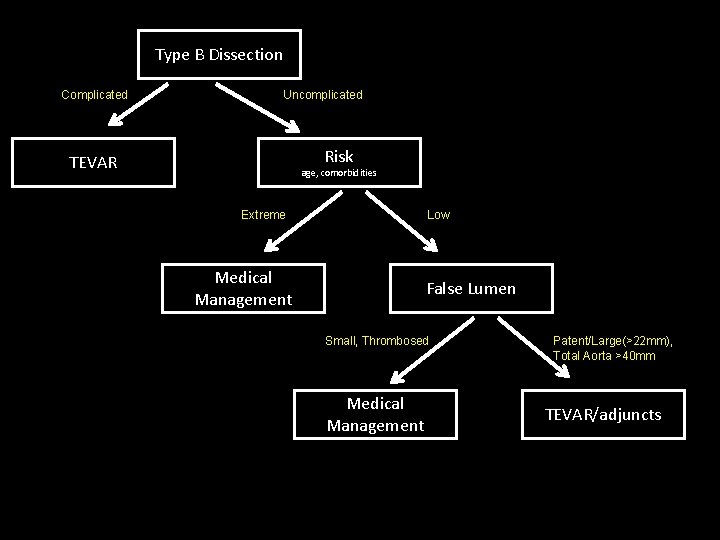
Type B Dissection Complicated Uncomplicated Risk TEVAR age, comorbidities Extreme Low Medical Management False Lumen Small, Thrombosed Medical Management Patent/Large(>22 mm), Total Aorta >40 mm TEVAR/adjuncts
Aneurysms • Descending – Obvious first choice assuming anatomically favorable • Ascending – IDE, Off label in high risk patient • Arch – Available in Europe, Under Trial in US • Thoraco – Available in Europe, Under Trial in US
Ascending Aorta • Currently off label unless in IDE • Challenges – Devices too long or too small for ascending – More complex terrain • Entire cardiac output • Valve/coronaries below • Inomminate above. – New Commercial Devices now available (shorter/tapered)
Current experience with ascending TEVAR JTCVS 2017 Nov 22, Roselli et al. 2006 to 2016 39 patients very high risk for open surgery – A dissection (12, 31%), – intramural hematoma (2, 5%), – pseudoaneurysm (22, 56%), – chronic dissection suture line entry tear (3, 8%). TEVAR in 36 Operative mortality 13%; 5 deaths all in Type A dissections Other complications: – stroke in 4 patients (10%), myocardial infarction in 2 patients (5%), tracheostomy in 2 patients (5%), and dialysis in 2 patients (5%).
• 30 days, 1 year, and 5 years overall survival: – 81%, 74%, and 64% • Freedom from reintervention: – 85%, 77%, and 68% • Significantly higher hazard of mortality with; – zone 0 A versus 0 C (P =. 020) – older age (P =. 026)
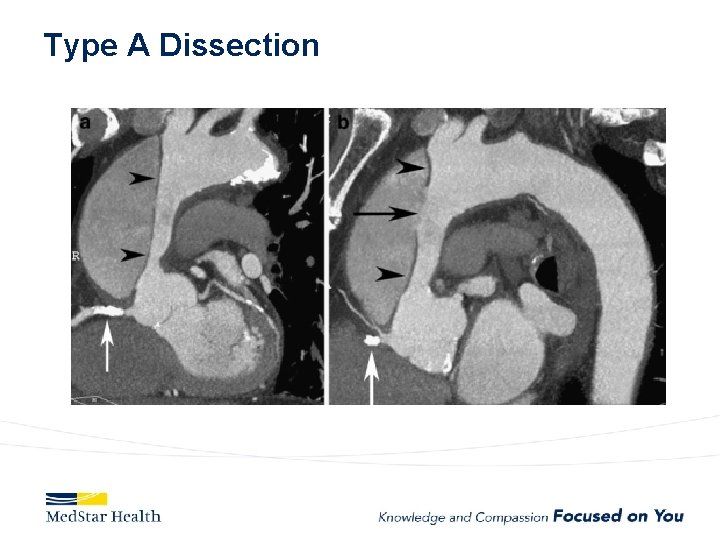
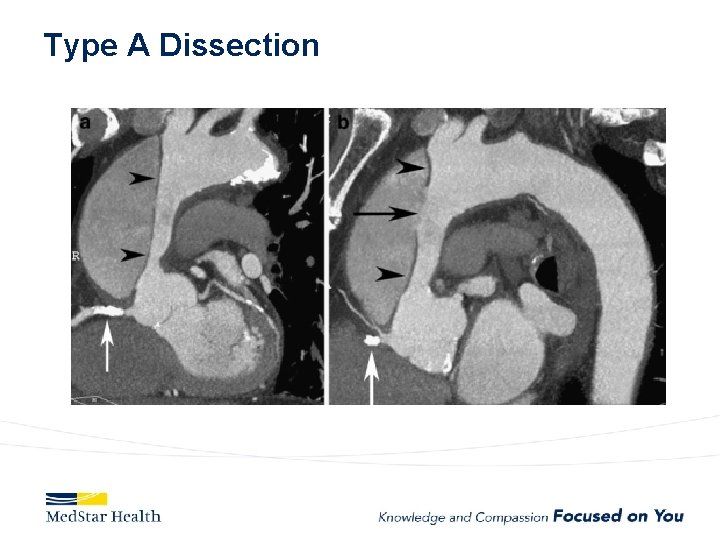
Type A Dissection















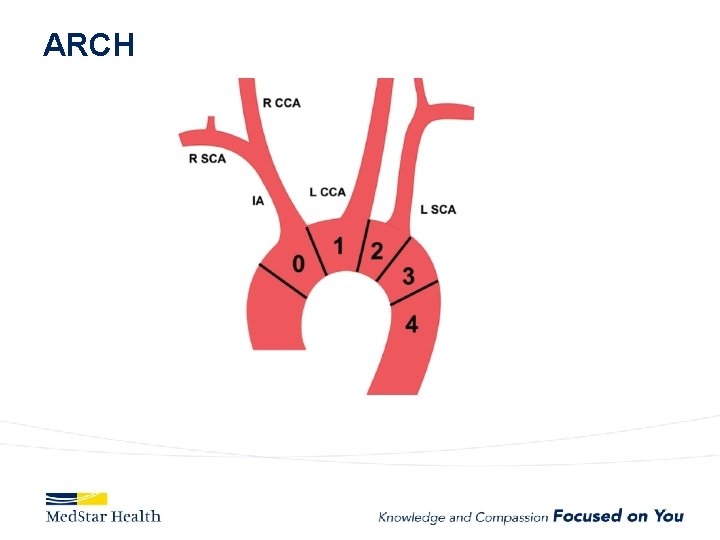
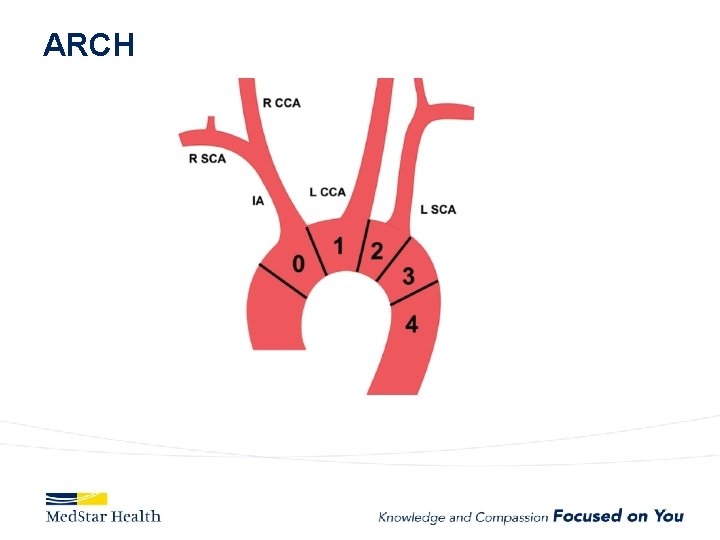
ARCH



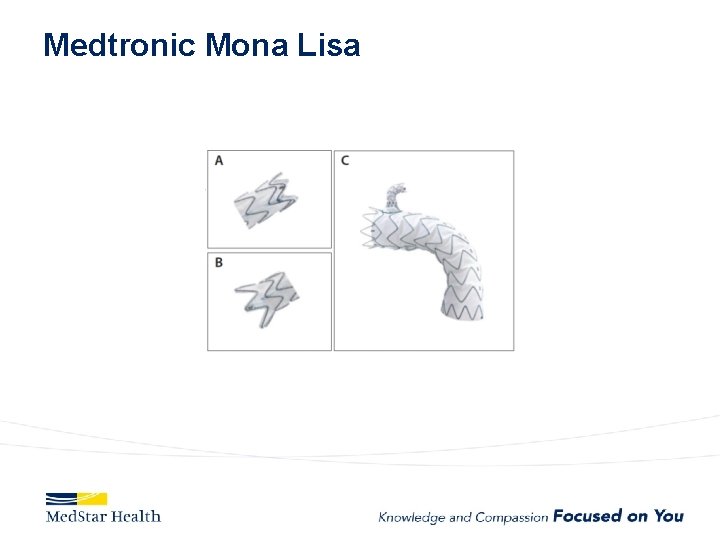
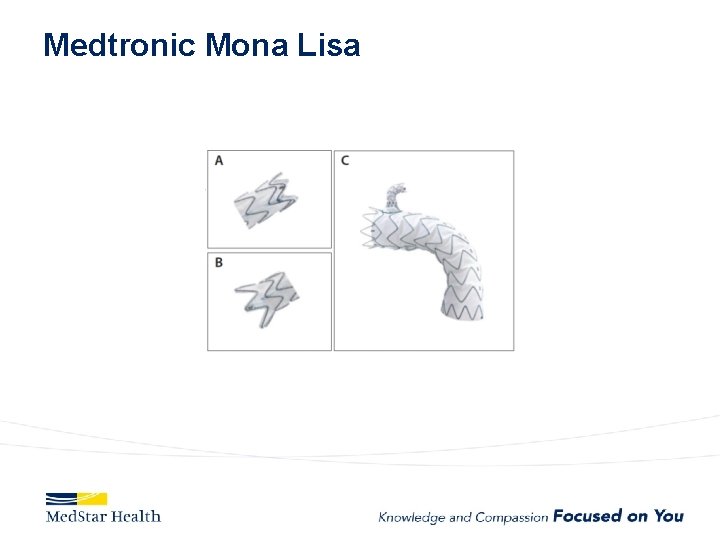
Medtronic Mona Lisa




Bolton
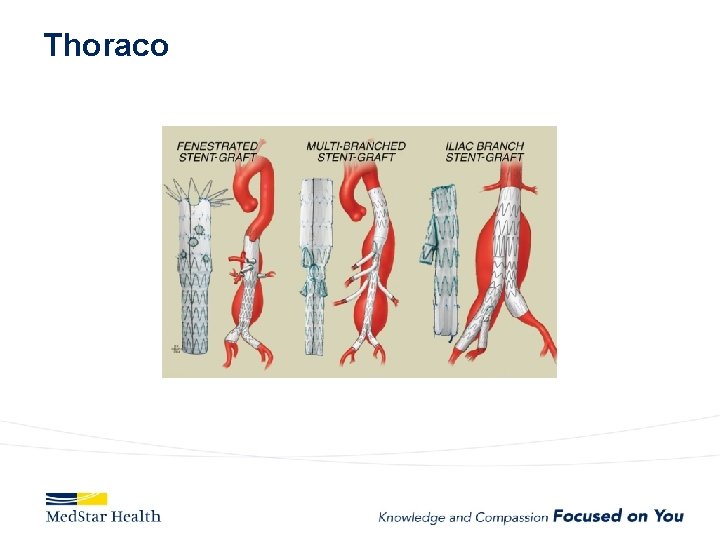
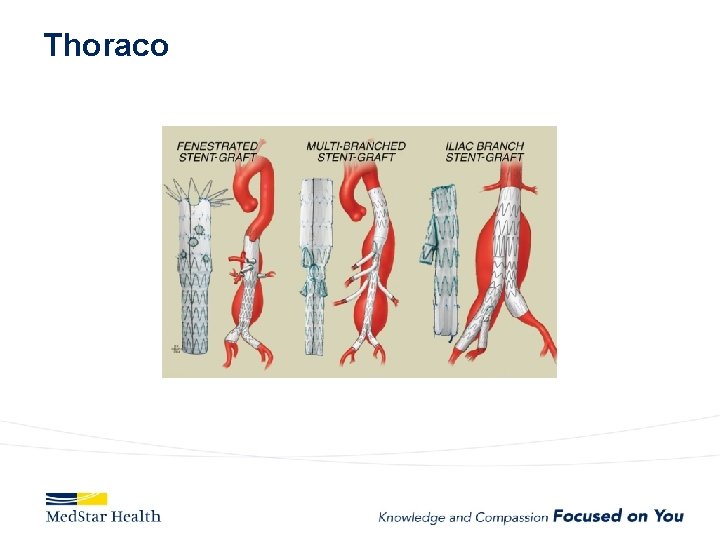
Thoraco
Conclusion • Indications for endovascular treatment of aortic disease are evolving • Devices are evolving as well • Future treatment will largely be endovascular
 What are the duties of assistant scorer?
What are the duties of assistant scorer? Dialogue clothes shop
Dialogue clothes shop When did you last questions
When did you last questions Printing and dyeing assistant
Printing and dyeing assistant Ethical and legal issues affecting the nursing assistant
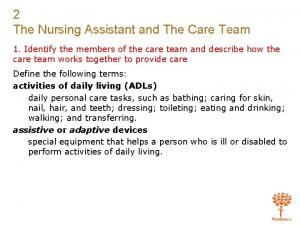
Ethical and legal issues affecting the nursing assistant 5 rights of delegation nursing examples
5 rights of delegation nursing examples Chapter 2 foundations of resident care
Chapter 2 foundations of resident care The signmaker's assistant quiz
The signmaker's assistant quiz As a laboratory assistant you measure chemicals
As a laboratory assistant you measure chemicals Chapter 2 dental assisting
Chapter 2 dental assisting Fujitsu alexa
Fujitsu alexa Medical assistant rop
Medical assistant rop Promotion from associate professor to professor
Promotion from associate professor to professor Assistant registrar ubd
Assistant registrar ubd Cisco configuration assistant (cca)
Cisco configuration assistant (cca) Kpu health care assistant
Kpu health care assistant Rearden commerce
Rearden commerce Cooperative interview questions
Cooperative interview questions Ibm software and support
Ibm software and support Hikvision recording assistant
Hikvision recording assistant Rog4d
Rog4d Cuhk salary scale 2020
Cuhk salary scale 2020 Function of district commissioner
Function of district commissioner Mrs rajlaxmi is working as the human resource consultant
Mrs rajlaxmi is working as the human resource consultant Cashflow assistant
Cashflow assistant Anwser
Anwser Attribute assistant arcmap
Attribute assistant arcmap Shop assistant good morning can i help you
Shop assistant good morning can i help you Head girl manifesto speech
Head girl manifesto speech The signmaker's assistant main idea
The signmaker's assistant main idea Mauritius police force hierarchy
Mauritius police force hierarchy Role of a teaching assistant
Role of a teaching assistant Palliative care assistant
Palliative care assistant Assistant manager career path
Assistant manager career path Siri dahl personal assistant
Siri dahl personal assistant How to email a professor
How to email a professor Patient safety assistant
Patient safety assistant Experimental design assistant
Experimental design assistant Cisco unified cm assistant console
Cisco unified cm assistant console Akshay kumar assistant
Akshay kumar assistant Arbitre assistant robot
Arbitre assistant robot Executive assistant conference 2019
Executive assistant conference 2019 Assistant secretary for aging
Assistant secretary for aging Danfoss alexa
Danfoss alexa Cisco personal communications assistant
Cisco personal communications assistant Dental assistant charting
Dental assistant charting Spiritual assistant
Spiritual assistant D-kefs scoring assistant
D-kefs scoring assistant Physician assistant kindergeneeskunde
Physician assistant kindergeneeskunde Laparoscopische cholecystectomie surgery assistant
Laparoscopische cholecystectomie surgery assistant Qcm validation formation assistant maternel
Qcm validation formation assistant maternel Junior assistant scoutmaster
Junior assistant scoutmaster Hello good afternoon teacher
Hello good afternoon teacher Good afternoon assistant
Good afternoon assistant University of new england physician assistant program
University of new england physician assistant program Telephone techniques chapter 14
Telephone techniques chapter 14 Veternary science
Veternary science