TESTICULAR TUMORS INCIDENCE Testicular tumors are rare 1




- Slides: 34
TESTICULAR TUMORS


INCIDENCE • Testicular tumors are rare. • 1 – 2 % of all malignant tumors. • Most common malignancy in men in the 15 to 35 years age group. • Benign lesions represent a greater percentage of cases in children than in adults.
• Age - 3 peaks 2 – 4 yrs 20 – 40 yrs above 60 yrs • Testicular cancer is one of the few neoplasms associated with accurate serum markers.
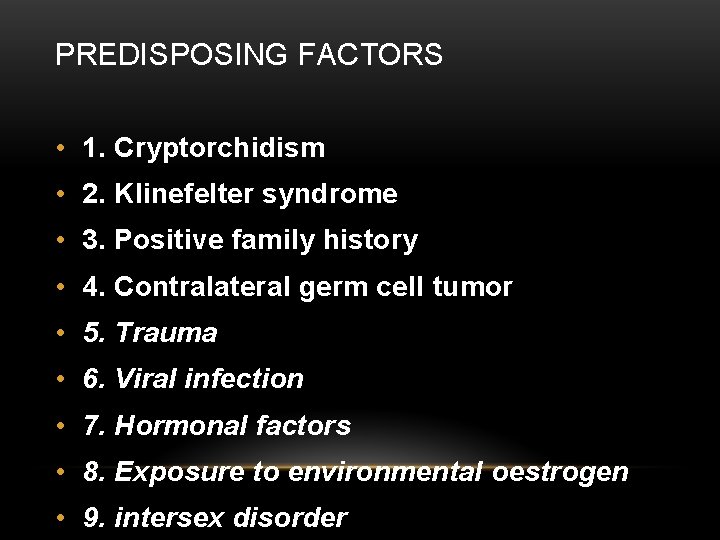
PREDISPOSING FACTORS • 1. Cryptorchidism • 2. Klinefelter syndrome • 3. Positive family history • 4. Contralateral germ cell tumor • 5. Trauma • 6. Viral infection • 7. Hormonal factors • 8. Exposure to environmental oestrogen • 9. intersex disorder
• Chromosomal abnormalities - loss of chromosome 11, 13, 18, abnormal chromosome 12 p.
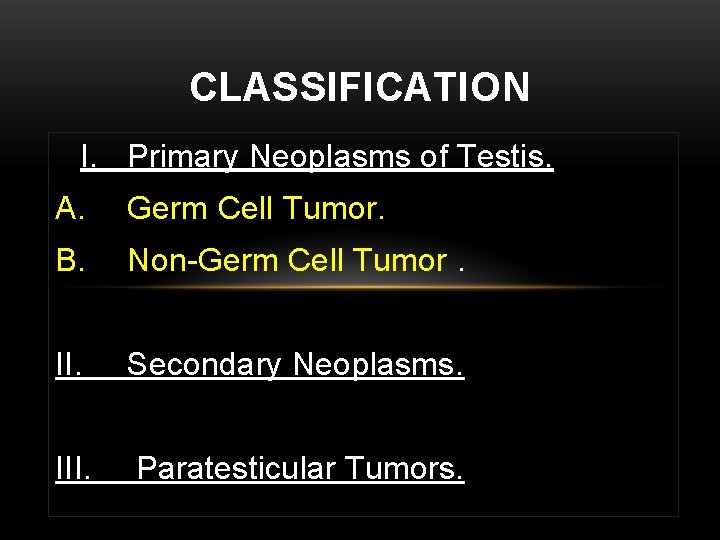
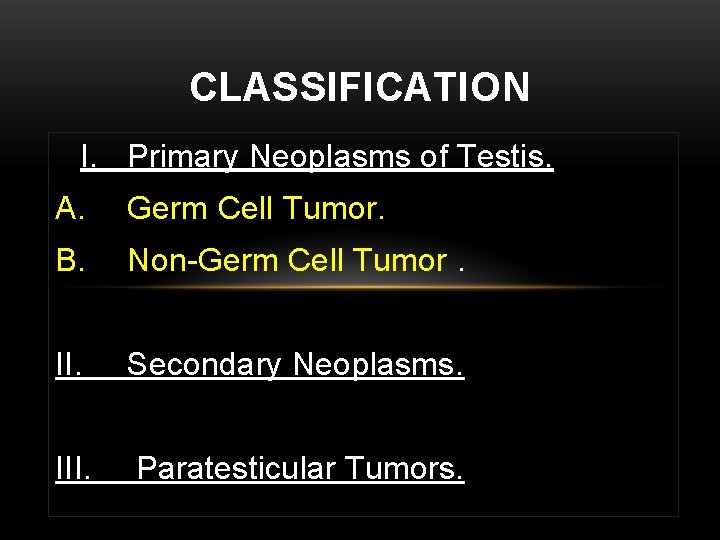
CLASSIFICATION I. Primary Neoplasms of Testis. A. Germ Cell Tumor. B. Non-Germ Cell Tumor. II. Secondary Neoplasms. III. Paratesticular Tumors.
• Germ Cell Tumor (GCT) arise from pluripotential cells, so a variety of elements may habitat in the primary tumor • More than half of GCTs contain more than one cell type and are therefore known as mixed GCTs
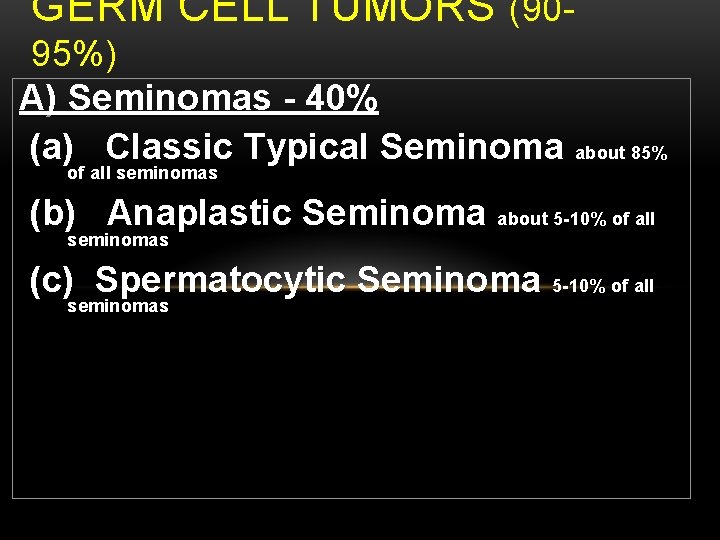
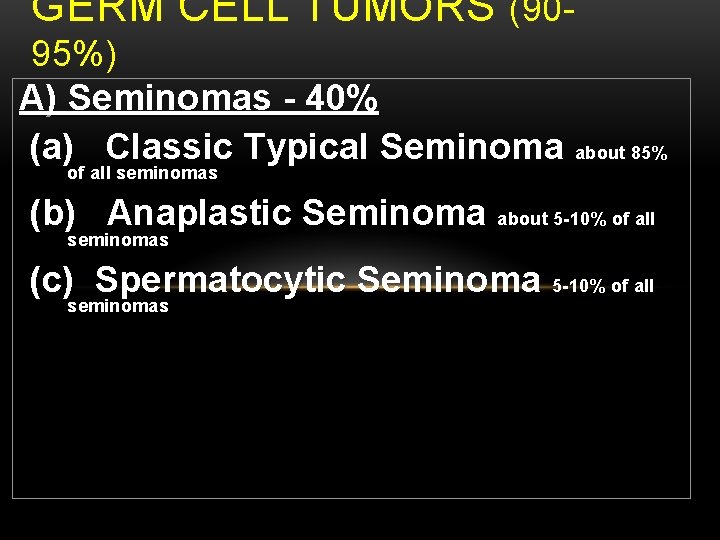
GERM CELL TUMORS (9095%) A) Seminomas - 40% (a) Classic Typical Seminoma about 85% of all seminomas (b) Anaplastic Seminoma about 5 -10% of all seminomas (c) Spermatocytic Seminoma 5 -10% of all seminomas
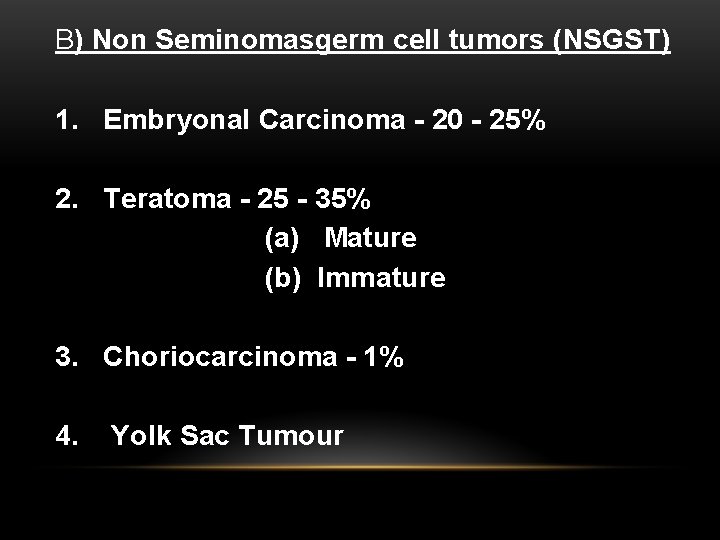
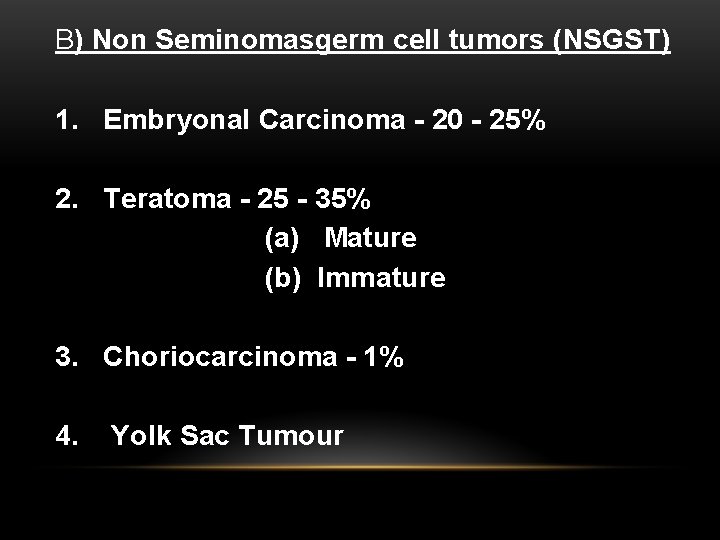
B) Non Seminomasgerm cell tumors (NSGST) 1. Embryonal Carcinoma - 20 - 25% 2. Teratoma - 25 - 35% (a) Mature (b) Immature 3. Choriocarcinoma - 1% 4. Yolk Sac Tumour
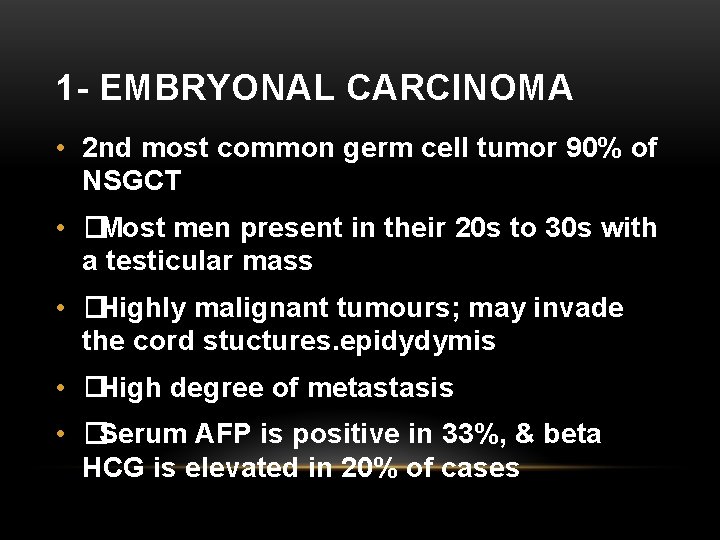
1 - EMBRYONAL CARCINOMA • 2 nd most common germ cell tumor 90% of NSGCT • �Most men present in their 20 s to 30 s with a testicular mass • �Highly malignant tumours; may invade the cord stuctures. epidydymis • �High degree of metastasis • �Serum AFP is positive in 33%, & beta HCG is elevated in 20% of cases
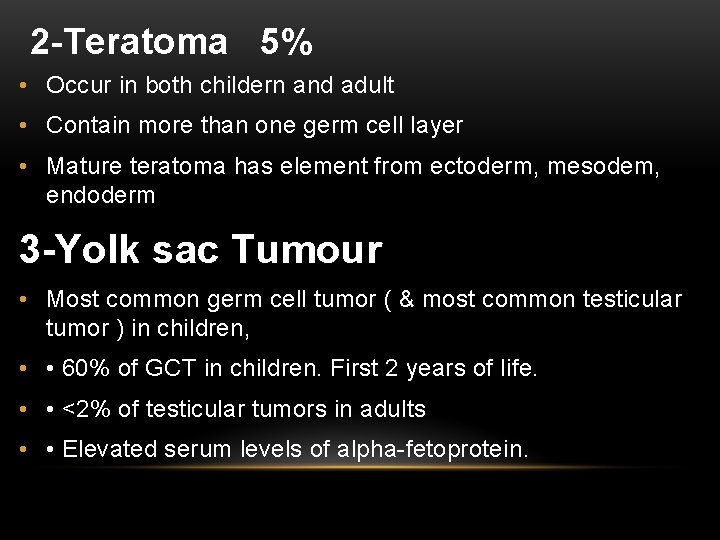
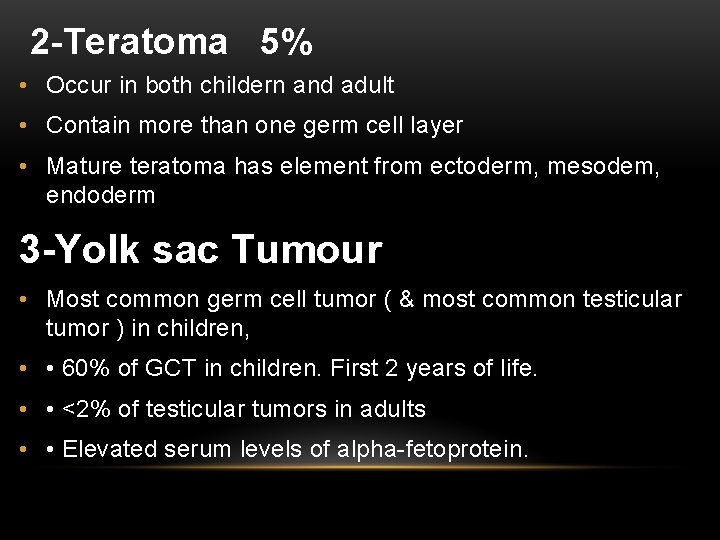
2 -Teratoma 5% • Occur in both childern and adult • Contain more than one germ cell layer • Mature teratoma has element from ectoderm, mesodem, endoderm 3 -Yolk sac Tumour • Most common germ cell tumor ( & most common testicular tumor ) in children, • • 60% of GCT in children. First 2 years of life. • • <2% of testicular tumors in adults • • Elevated serum levels of alpha-fetoprotein.
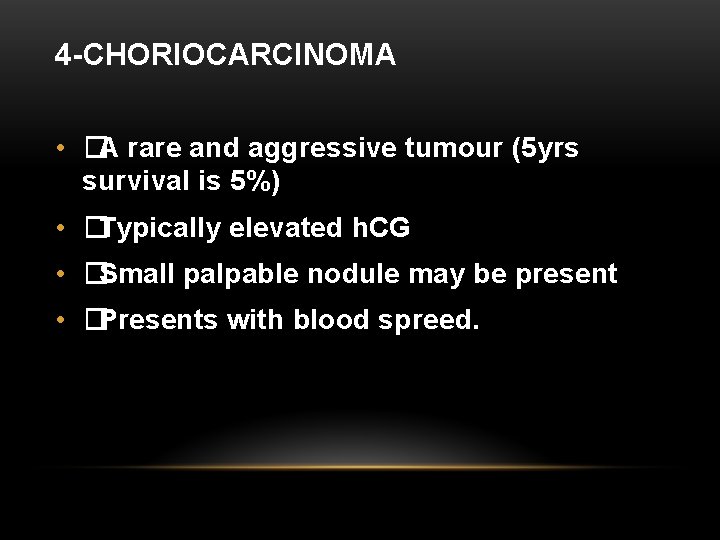
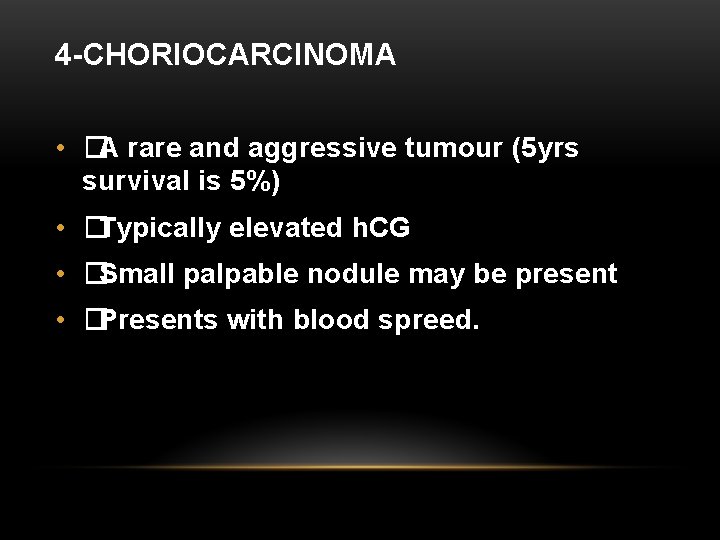
4 -CHORIOCARCINOMA • �A rare and aggressive tumour (5 yrs survival is 5%) • �Typically elevated h. CG • �Small palpable nodule may be present • �Presents with blood spreed.
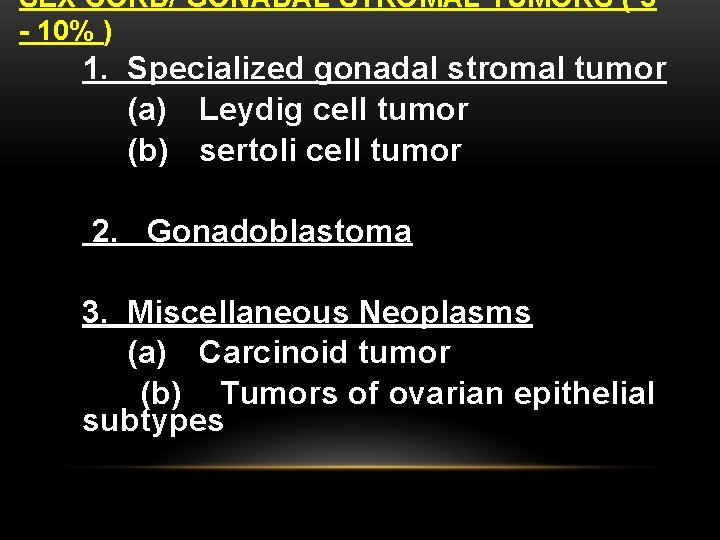
SEX CORD/ GONADAL STROMAL TUMORS ( 5 - 10% ) 1. Specialized gonadal stromal tumor (a) Leydig cell tumor (b) sertoli cell tumor 2. Gonadoblastoma 3. Miscellaneous Neoplasms (a) Carcinoid tumor (b) Tumors of ovarian epithelial subtypes
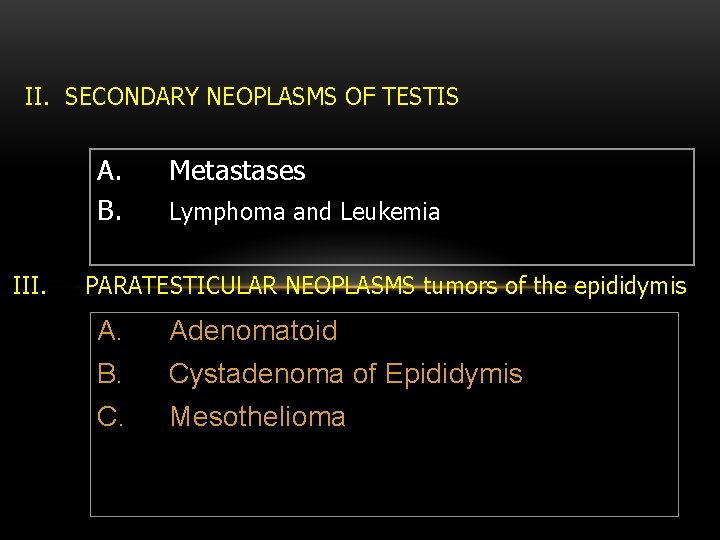
II. SECONDARY NEOPLASMS OF TESTIS A. B. III. Metastases Lymphoma and Leukemia PARATESTICULAR NEOPLASMS tumors of the epididymis A. Adenomatoid B. Cystadenoma of Epididymis C. Mesothelioma
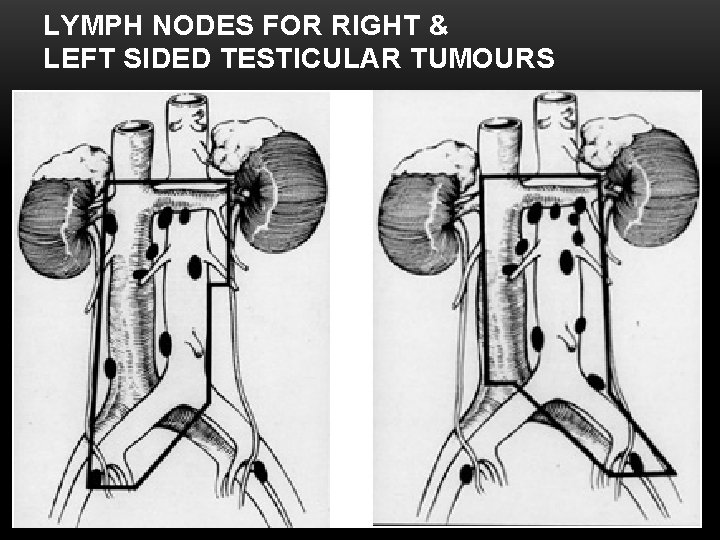
LYMPHATIC DRAINAGE • The primary drainage of the right testis is within the interaortocaval region. • Left testis drainage , the para-aortic region in the compartment bounded by the left ureter, the left renal vein, the aorta, and the origin of the inferior mesenteric artery. • Cross over from right to left is possible.
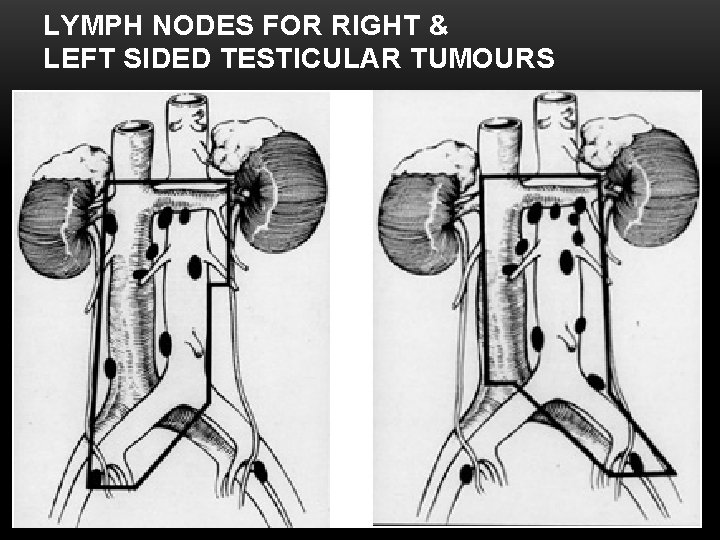
LYMPH NODES FOR RIGHT & LEFT SIDED TESTICULAR TUMOURS
LYMPHATIC DRAINAGE • Lymphatics of the epididymis drain into the external iliac chain. • Inguinal node metastasis may result from scrotal involvement by the primary tumor, prior inguinal or scrotal surgery, or retrograde lymphatic spread secondary to massive retroperitoneal lymph node deposits. • Testicular cancer spreads in a predictable and stepwise fashion, except choriocarcinoma. .
CLINICAL FEATURES • Painless Swelling (any firm to hard Testicular mass considered malignancy Until proved otherwise) • Dull Ache or Heaviness in the Lower Abdomen • 10% - Acute Scrotal Pain • 10% - Present with Metatstasis - Neck Mass / Cough / Anorexia / Vomiting / Back Ache/ Lower limb swelling • 5% - Gynecomastia • 2 nd hydrocele
PHYSICAL EXAMINATION • Examine contralateral normal testis. • Firm to hard fixed area within tunica albugenia is suspicious
DIFFERENTIAL DIAGNOSIS • Testicular torsion • Epididymitis, or epididymo-orchitis • Haematocele • Syphilitic gumma
SCROTAL ULTRASOUND • Ultrasonography of the scrotum is a rapid, reliable technique • Ultrasonography of the scrotum is basically an extension of the physical examination. • Hypoechoic area within the tunica albuginea is markedly suspicious for testicular cancer.

• Any patient with a solid, Firm Intratesticular Mass that cannot be Transilluminated should be regarded as Malignant unless otherwise proved.
IMAGING STUDIES • Chest X ray • CT abdomen – retroperitoneal nodes • MRI - No apparent advantage over CT
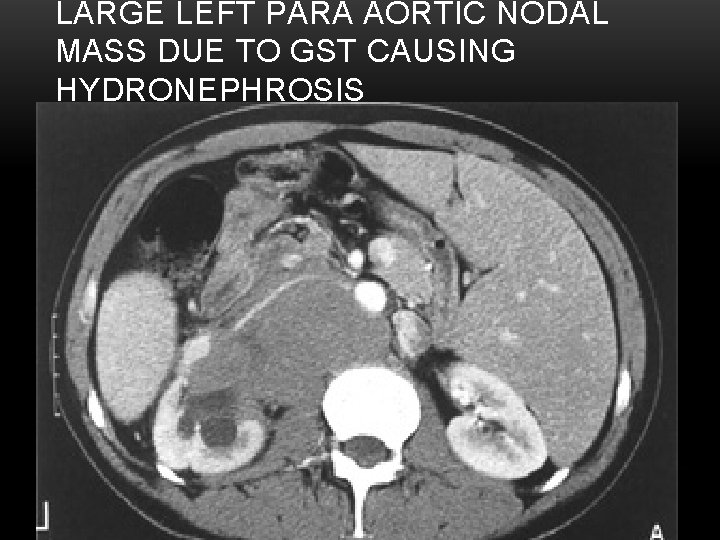
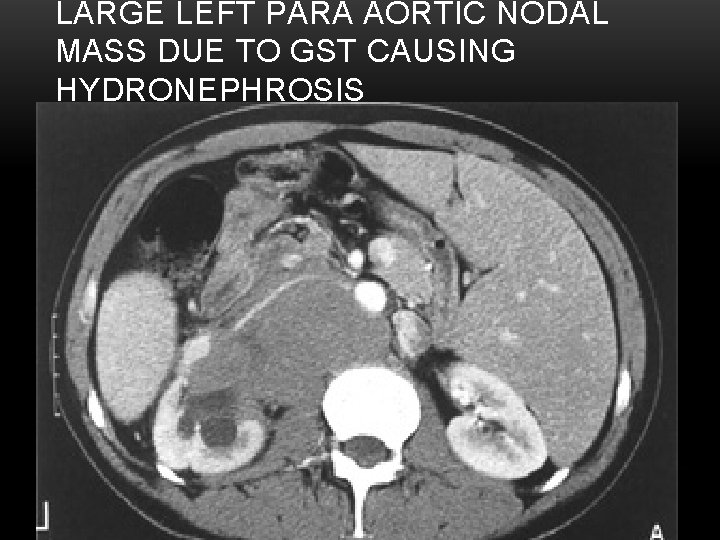
LARGE LEFT PARA AORTIC NODAL MASS DUE TO GST CAUSING HYDRONEPHROSIS
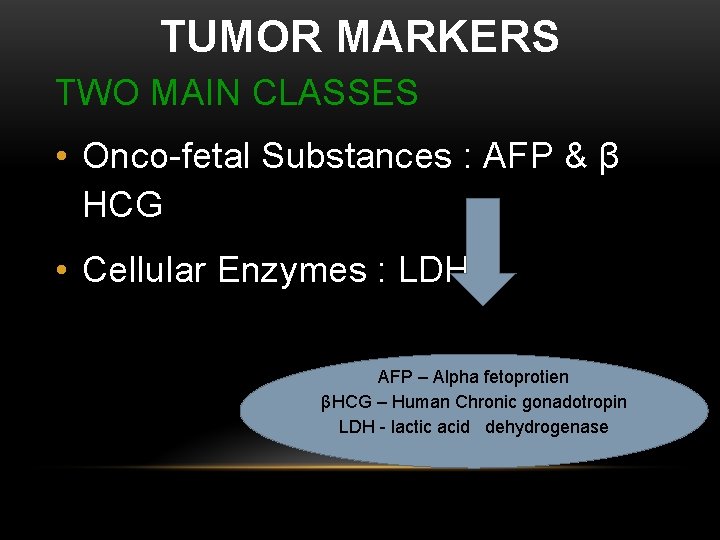
TUMOR MARKERS TWO MAIN CLASSES • Onco-fetal Substances : AFP & β HCG • Cellular Enzymes : LDH AFP – Alpha fetoprotien βHCG – Human Chronic gonadotropin LDH - lactic acid dehydrogenase
ROLE OF TUMOUR MARKERS • Helps in Diagnosis 80 to 85% Tumours have Positive Markers of Testicular • Most of Non-Seminomas have raised markers • Only 10 to 15% Non-Seminomas have normal marker level • After Orchidectomy if Markers Elevated means Residual Disease.
ROLE OF TUMOUR MARKERS • Negative Tumor Markers becoming positive on follow up usually indicates - Recurrence of Tumor • Markers become Positive earlier than imaging studies
AFP –( Alfafetoprotein) Present in NSGCTs and never found in pure seminoma or pure chorocarcenoima HCG – ( Human Chorionic Gonadotropin) Present mainly in Choriocarcinoma LDH – (Lactic dehydrogenese) Present in muscle may be seminoma (non spescific) elevated in
PRINCIPLES OF TREATMENT • INGUINAL ORCHIDECTOMY is Standard first line of therapy (Schevaso technique) Complete removal of ipsilateral epididymis and spermatic cord to the level of the internal inguinal ring. • Bulky Retroperitoneal Tumours or Metastatic Tumors Initially “DOWN-STAGED” with CHEMOTHERAPY
• Seminomas - Radio-Sensitive. • Non-Seminomas are Radio-Resistant and best treated by Surgery • Advanced Disease or Metastasis - Responds well to Chemotherapy

THANK YOU
 Teratoma
Teratoma Insidan region jh
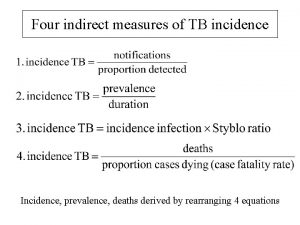
Insidan region jh Prevalence calculation formula
Prevalence calculation formula Prevalence vs incidence
Prevalence vs incidence Enneking
Enneking Exostosis
Exostosis Paresthiasis
Paresthiasis Local invasion
Local invasion Peter hino md
Peter hino md Odontogenic tumors
Odontogenic tumors Spinal cord tumors
Spinal cord tumors Adenocarcinoma
Adenocarcinoma Classification of tumors
Classification of tumors Response evaluation criteria in solid tumors (recist)
Response evaluation criteria in solid tumors (recist) Ameloblastoma rtg
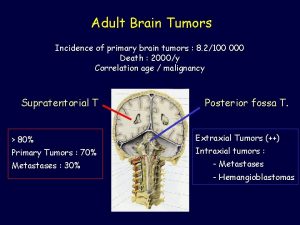
Ameloblastoma rtg Brain tumors
Brain tumors Intraductal papillary mucinous neoplasm
Intraductal papillary mucinous neoplasm Odontogenic tumors classification
Odontogenic tumors classification Chondrosarcoma
Chondrosarcoma Thyroid tumors
Thyroid tumors Chest wall tumors
Chest wall tumors Benign tumors in the uterus
Benign tumors in the uterus Caseating granuloma
Caseating granuloma Neoplasia testicular
Neoplasia testicular Diaphrosis
Diaphrosis Escroto
Escroto Percutaneous balloon pericardiotomy
Percutaneous balloon pericardiotomy Hormona antimulleriana valores normales 40 años
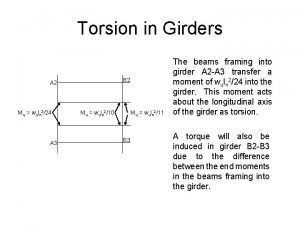
Hormona antimulleriana valores normales 40 años Mechanics of materials torsion
Mechanics of materials torsion Site:slidetodoc.com
Site:slidetodoc.com Lobes of prostate
Lobes of prostate Uretra
Uretra Testicular atrophy
Testicular atrophy Testicular detorsion maneuver
Testicular detorsion maneuver Plexo pampiniforme
Plexo pampiniforme