Suture material Surgical suture is a medical device



- Slides: 54
Suture material Surgical suture is a medical device used to hold body tissues together after an injury or surgery. It generally consists of a needle with an attached length of thread. A number of different shapes, sizes, and thread materials have been developed over its millennia of history
» » Through many millennia, various suture materials were used, debated, and remained largely unchanged. Needles were made of bone or metals such as silver, copper, and aluminum bronze wire. Sutures were made of plant materials (flax, hemp and cotton) or animal material (hair, tendons, arteries, muscle strips and nerves, silk, catgut). African cultures used thorns, and others used ant (Dorylus )sutures by coaxing insects to bite wound edges with their jaws and subsequently twisting off the insects' heads. [1] The earliest reports of surgical suture date back to 3000 BC in ancient Egypt, and the oldest known suture is in a mummy from 1100 BC. The first detailed description of a wound suture and the suture materials used in it is by the Indian sage and physician Sushruta, written in 500 BCE. The Greek "father of medicine" Hippocrates described rudimentary suture techniques, as did the later Roman Aulus Cornelius Celsus. The 2 nd-century Roman physician Galen has been credited as the first to describe gut sutures, [1] or alternatively the 10 th-century Andalusian surgeon al-Zahrawi. Al. Zahrawi reportedly discovered the dissolving nature of catgut when his lute's strings were eaten by a monkey. The manufacturing process involved harvesting sheep intestines, the so called catgut suture, and was similar to that of strings for violins, guitar, and tennis racquets. Joseph Lister introduced great change in suturing technique (as in all surgery) when he endorsed the routine sterilization of all suture threads. He first attempted sterilization with the 1860 s "carbolic catgut, " and chromic catgut followed two decades later. Sterile catgut was finally achieved in 1906 with iodine treatment. [1] The next great leap came in the twentieth century. The chemical industry drove production of the first synthetic thread in the early 1930 s, which exploded into production of numerous absorbable and non-absorbable synthetics. The first synthetic absorbable was based on polyvinyl alcohol in 1931. Polyesters were developed in the 1950 s, and later the process of radiation sterilization was established for catgut and polyester. Polyglycolic acid was discovered in the 1960 s and implemented in the 1970 s. [1] Today, most sutures are made of synthetic polymer fibers. Silk and gut sutures are the only materials still - though rarely - in use from ancient times. In fact, gut sutures have been banned in Europe and Japan owing to concerns regarding Bovine Spongiform Encephalopathy.

Feature of ideal suture material 1. Adequate tensile strength 2. Good knot holding property 3. Should be least reactive 4. Easy handling property 5. Should have less memory 6. Should be easily available and cost effective Memory= memory of suture material is recoiling tendency after removal from the packet
Classification » Absorbable Vs. Nonabsorbable » Monofilament Vs. Multifilament » Natural or Synthetic
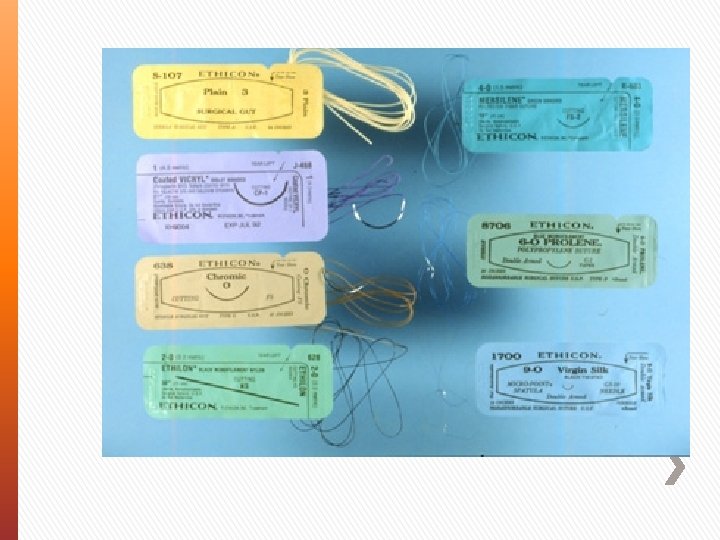
» Absorbable ˃ ˃ ˃ ˃ Catgut (plain & chromic), polyglycolic acid (Dexon), vicryl (polyglactic acid), Maxon (polyglyconate) PDS (poly Diaxanone suture material) Monocryl (polyglecaprone) Biosyn(glycomer) ˃ Used for deep tissues, membranes, & subcuticular skin closure » Non-Absorbable ˃ Silk, polypropylene(prolene), cotton, linen, polyester, nylon, stainless steel ˃ Used for skin (removed) & some deep structures (tendons, vessels, nerve repairs – not removed), herniorrhaphy, tenshion suturing
Absorbable Sutures » » » Internal Intradermal/ subcuticular Rarely on skin Circumcision Bowel anastmosis like gastrojejunostomy(vicryl)
Non-absorbable Suture » Primarily Skin ˃ Needs to be removed later » Stainless steel = exception ˃ Can be used internally + Ligature + Orthopedics ˃ Can be left in place for long periods
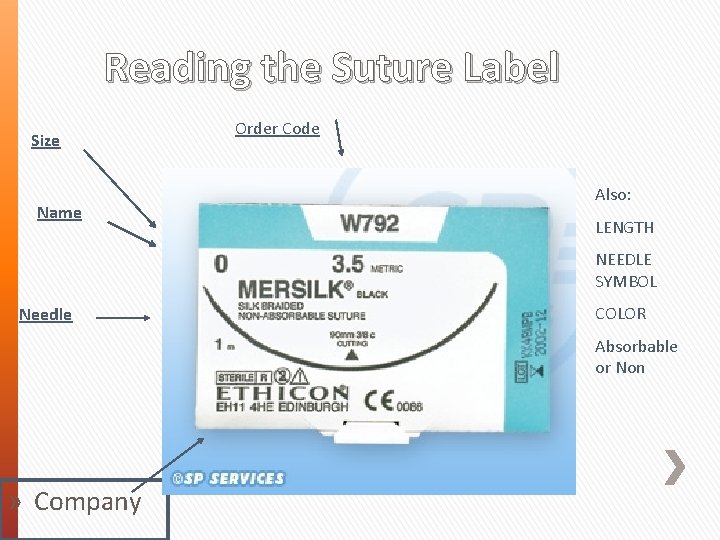
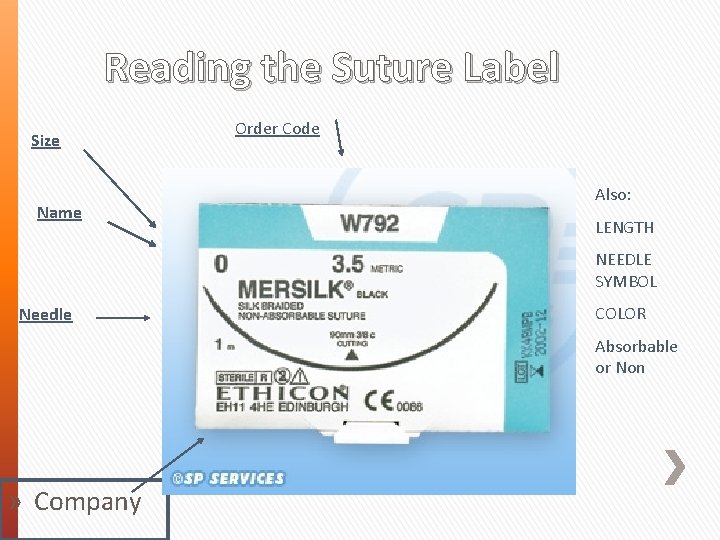
Reading the Suture Label Size Name Order Code Also: LENGTH NEEDLE SYMBOL Needle COLOR Absorbable or Non » Company
Absorbable Advantages Disadvantages » Broken down by body » Consideration of » No foreign body left wound support time » wound failure
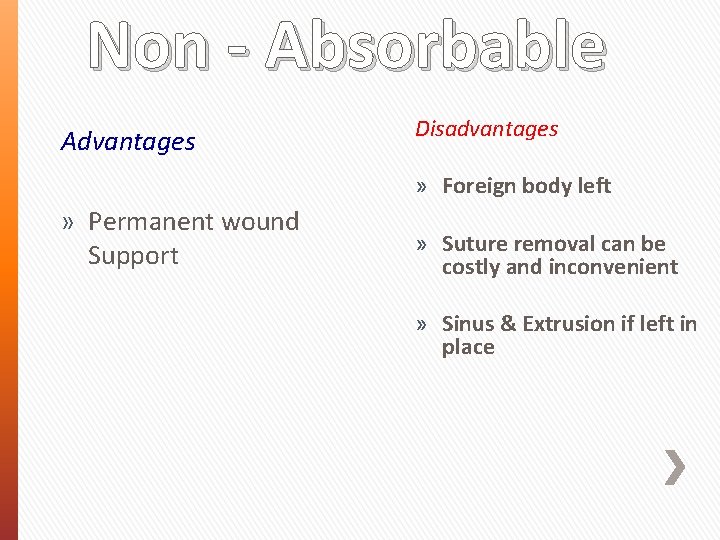
Non - Absorbable Advantages Disadvantages » Foreign body left » Permanent wound Support » Suture removal can be costly and inconvenient » Sinus & Extrusion if left in place
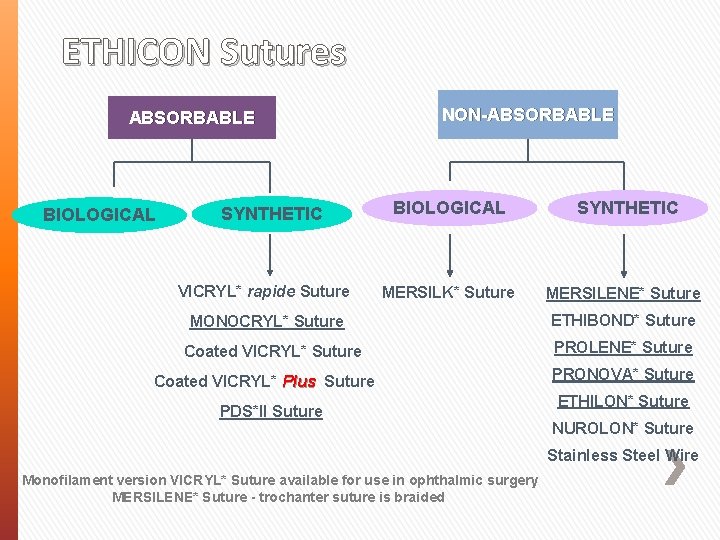
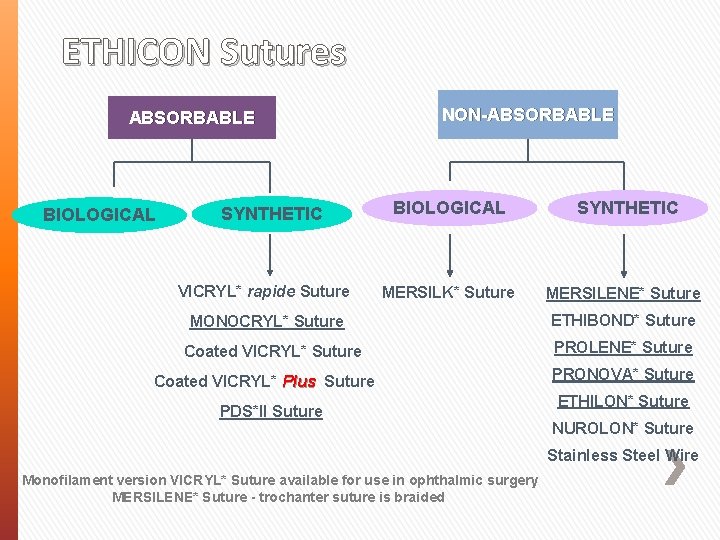
ETHICON Sutures ABSORBABLE BIOLOGICAL SYNTHETIC VICRYL* rapide Suture NON-ABSORBABLE BIOLOGICAL SYNTHETIC MERSILK* Suture MERSILENE* Suture MONOCRYL* Suture Coated VICRYL* Plus Suture PDS*II Suture ETHIBOND* Suture PROLENE* Suture PRONOVA* Suture ETHILON* Suture NUROLON* Suture Stainless Steel Wire Monofilament version VICRYL* Suture available for use in ophthalmic surgery MERSILENE* Suture - trochanter suture is braided
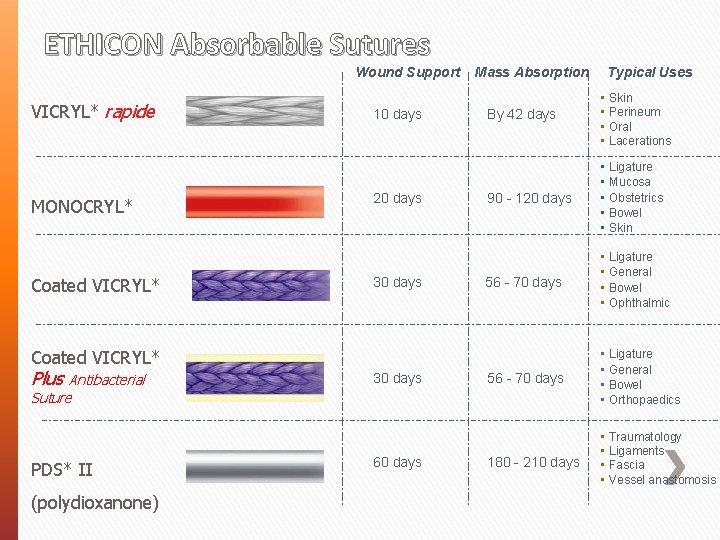
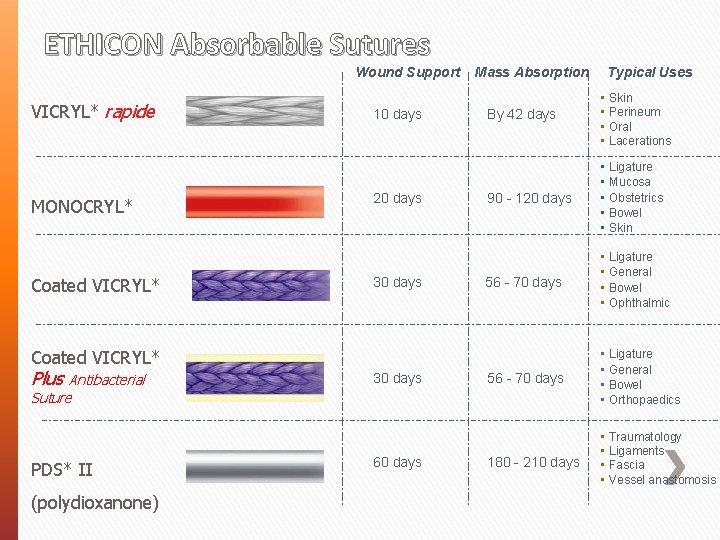
ETHICON Absorbable Sutures Wound Support VICRYL* rapide MONOCRYL* Coated VICRYL* 10 days 20 days 30 days Mass Absorption By 42 days • Skin • Perineum • Oral • Lacerations 90 - 120 days • Ligature • Mucosa • Obstetrics • Bowel • Skin 56 - 70 days • Ligature • General • Bowel • Ophthalmic 56 - 70 days • Ligature • General • Bowel • Orthopaedics 180 - 210 days • Traumatology • Ligaments • Fascia • Vessel anastomosis Coated VICRYL* Plus Antibacterial 30 days Suture PDS* II (polydioxanone) 60 days Typical Uses
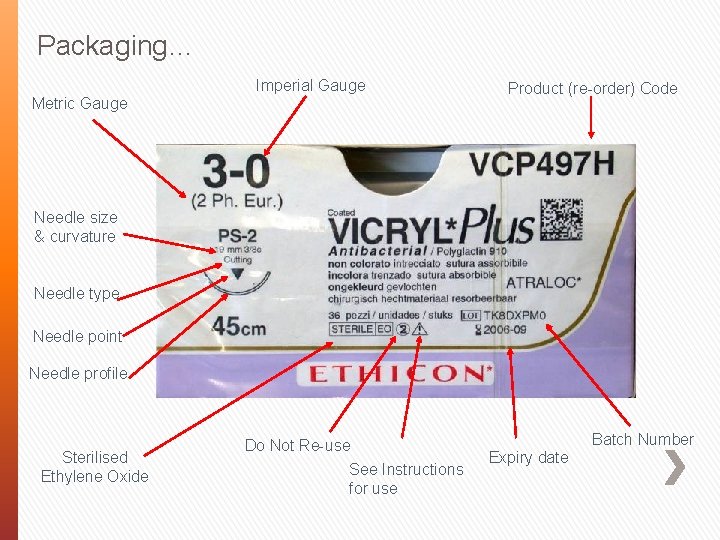
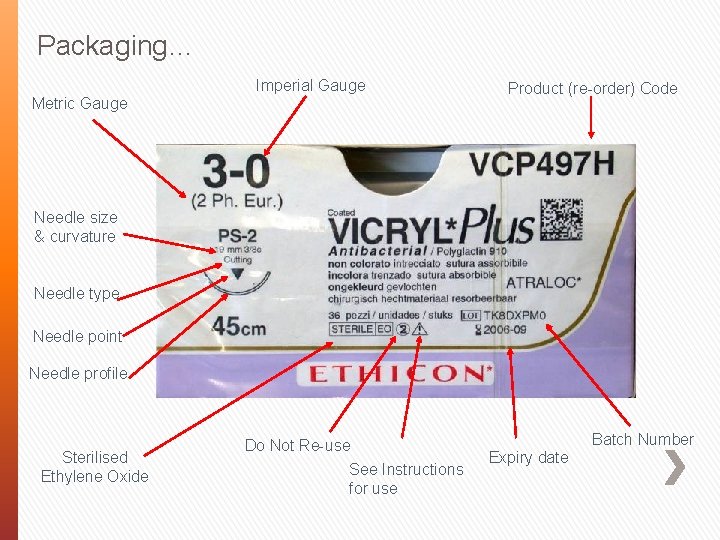
Packaging… Imperial Gauge Metric Gauge Product (re-order) Code Needle size & curvature Needle type Needle point Needle profile Sterilised Ethylene Oxide Do Not Re-use See Instructions for use Batch Number Expiry date
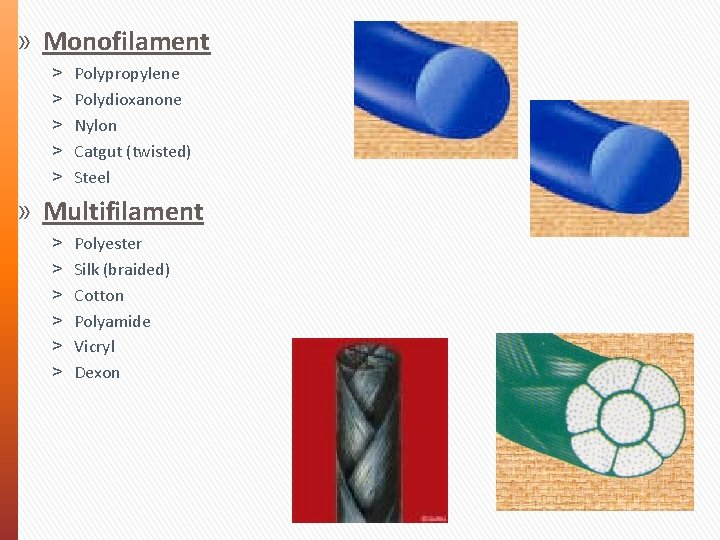
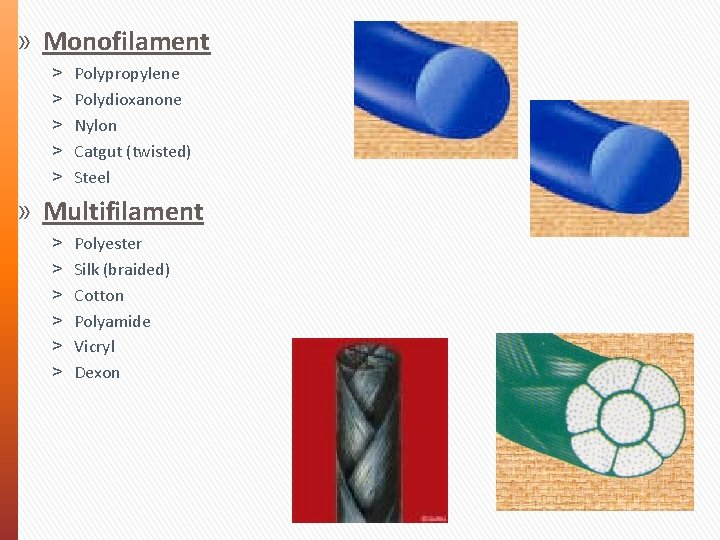
» Monofilament ˃ ˃ ˃ Polypropylene Polydioxanone Nylon Catgut (twisted) Steel » Multifilament ˃ ˃ ˃ Polyester Silk (braided) Cotton Polyamide Vicryl Dexon
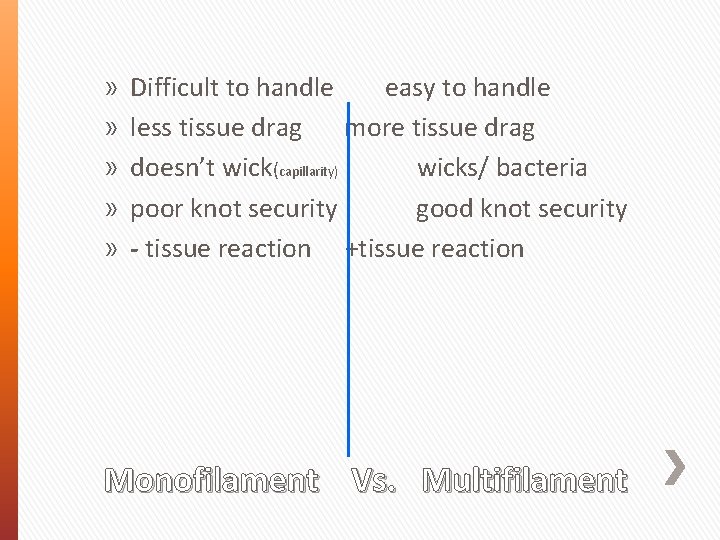
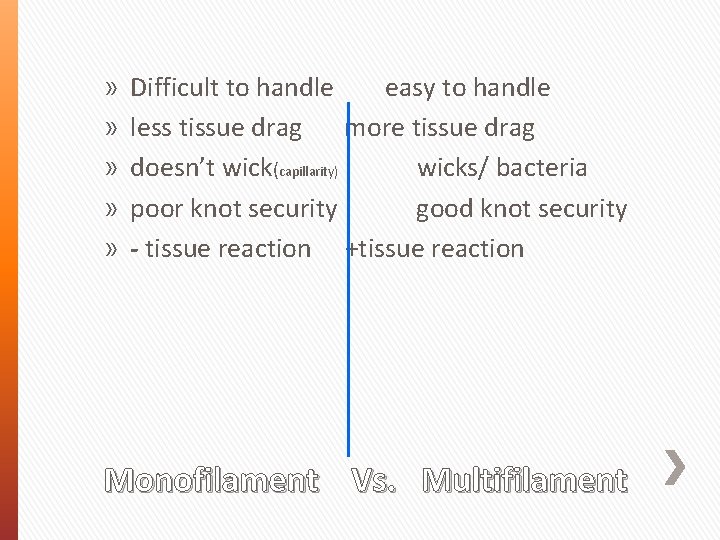
» » » Difficult to handle easy to handle less tissue drag more tissue drag doesn’t wick(capillarity) wicks/ bacteria poor knot security good knot security - tissue reaction +tissue reaction Monofilament Vs. Multifilament
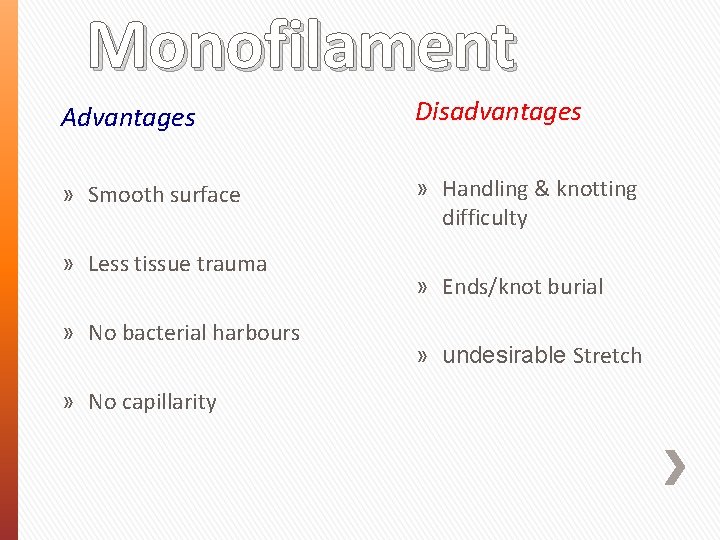
Monofilament Advantages Disadvantages » Smooth surface » Handling & knotting difficulty » Less tissue trauma » No bacterial harbours » No capillarity » Ends/knot burial » undesirable Stretch
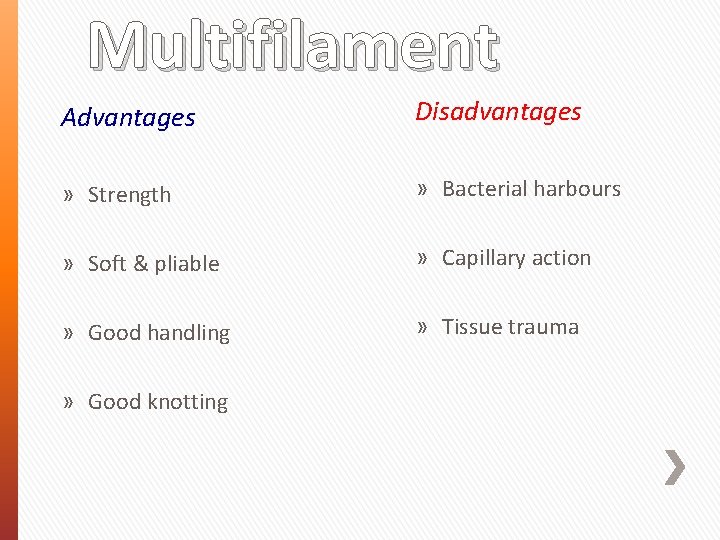
Multifilament Advantages Disadvantages » Strength » Bacterial harbours » Soft & pliable » Capillary action » Good handling » Tissue trauma » Good knotting
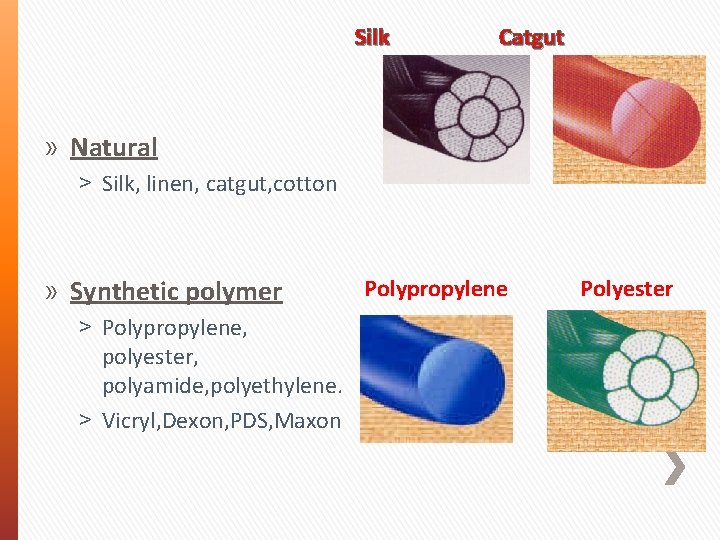
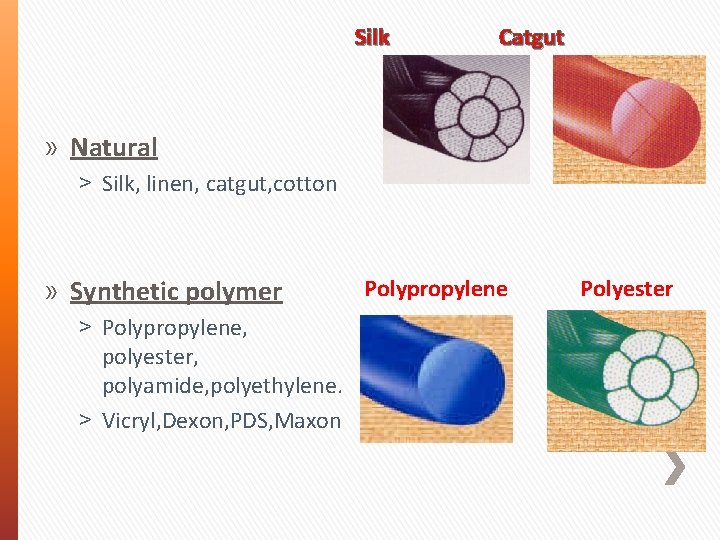
Silk Catgut » Natural ˃ Silk, linen, catgut, cotton » Synthetic polymer ˃ Polypropylene, polyester, polyamide, polyethylene. ˃ Vicryl, Dexon, PDS, Maxon Polypropylene Polyester
Natural Vs. Synthetic » Natural: ˃ ˃ Gut Chromic Gut Silk Collagen » All are absorbable
Gut/ Chromic Gut » Made of submucosa of small intestines » Multifilament » Breaks down by phagocytosis: inflammatory reaction common
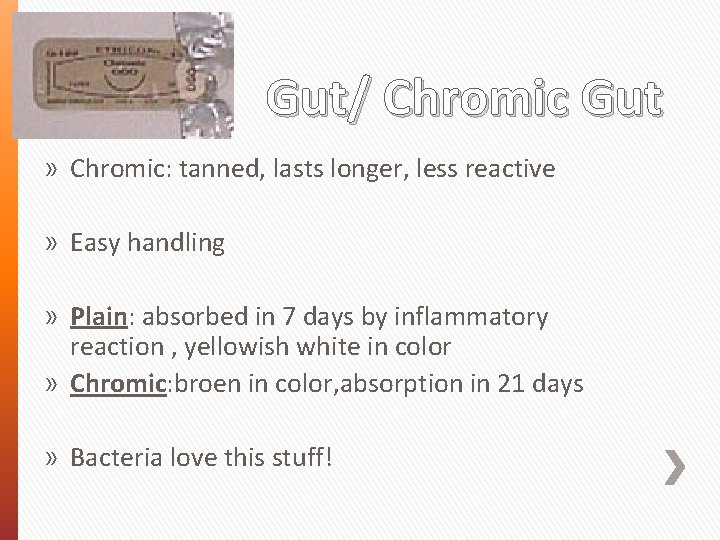
Gut/ Chromic Gut » Chromic: tanned, lasts longer, less reactive » Easy handling » Plain: absorbed in 7 days by inflammatory reaction , yellowish white in color » Chromic: broen in color, absorption in 21 days » Bacteria love this stuff!
Collagen and Silk » Natural sutures » VERY reactive, absorbable » Ophthalmic surgery only
Vicryl (Polyglactin 910) » Braided, multifilament, synthetic, absorbable » Stronger than gut: retains strength 90 days » Broken down by enzymes (hydrolysis), not phagocytosis. violet in color » Break-down products inhibit bacterial growth ˃ Can use in contaminated wounds, unlike other multifilaments
Dexon and PGA Polymer of glycolic acids Braided, synthetic, absorbable Creamy yellow in color Broken down by enzymes Both PGA and dexon have increased tissue drag, good knot security » Both are stronger than gut » » »
PDS (polydioxanone) » Monofilament (less drag, worse knot security – lots of “memory”) » Synthetic, absorbable » Very good tensile strength (better than gut, vicryl, dexon) which lasts months » Absorbed completely by 182 days
Maxon (polyglyconate) » » » Monofilament- memory Synthetic Absorbable Very little tissue drag Poor knot security Very strong
NONABSORBABLE SUTURES » Natural or Synthetic » Monofilament or multifilament

Silk » » » Natural Multifilament Braided , non absorable Derived from cocoon of silkworm Black in color It is coated suture material to reduce capillary action.
NYLON » » » Synthetic Mono or Multifilament Memory Very little tissue reaction Poor knot security
PROLENE(Polypropylene) » » » » Prolene, Surgilene Monofilament, Synthetic Blue in color High memory Won’t lose tensile strength over time Good knot security Very little tissue reaction
Stainless Steel » » » Monofilament Strongest ! Great knot security Difficult handling Can cut through tissues Very little tissue reaction, won’t harbor bacteria
Synthetic Advantages » Non-Absorbables are inert » Absorbables resemble natural substances » Absorption by hydrolysis » Predictable absorption » Strength Disadvantages » Monofilament handling is difficult
» Detail: » » Synthetic materials are man – made, produced by industrial processes. » • • Advantages Synthetic non-absorbable materials do not elicit tissue reaction as they are not absorbed. Synthetic absorbables are polymers which resemble sugars in their chemical structure, therefore they are eliminated easily. Absorption is by hydrolysis, which causes very little tissue reaction. This is in stark contrast to the biological group where absorption or suture breakdown is caused by enzymatic action. Hydrolysis takes place because water (or more correctly - interstitial fluid) interferes with the molecular bonds in the polymer chains which comprise these synthetic materials leading to their breakdown and elimination. Hydrolysis is also a much more predictable absorption method, allowing accurate forecasts of tensile strength retention. Finally, synthetic materials tend to be stronger than their biological equivalents for similar gauge sizes. Disadvantages The drawbacks of synthetic material tend to be related to their structure rather than their chemical composition. They can be more difficult to handle in the monofilament structure and at times, encapsulation can result in the suture being extruded or expelled by the body. • • » • •
Biological Advantages Disadvantages » Handling & knotting » Tissue reactions is more » Economy
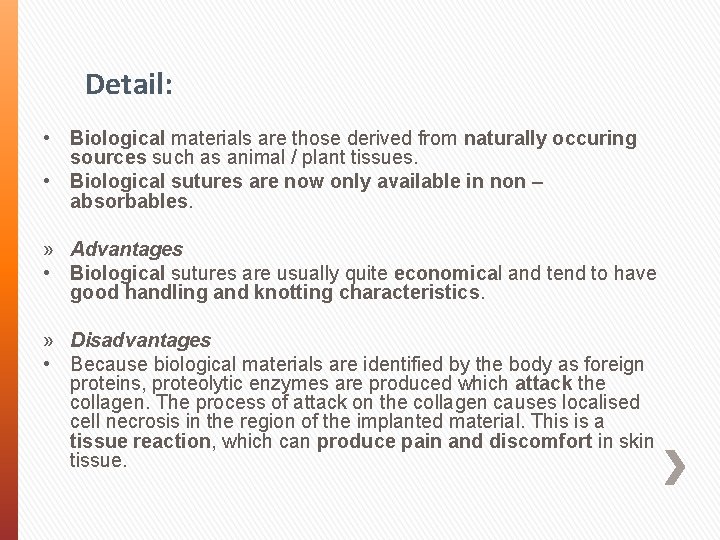
Detail: • Biological materials are those derived from naturally occuring sources such as animal / plant tissues. • Biological sutures are now only available in non – absorbables. » Advantages • Biological sutures are usually quite economical and tend to have good handling and knotting characteristics. » Disadvantages • Because biological materials are identified by the body as foreign proteins, proteolytic enzymes are produced which attack the collagen. The process of attack on the collagen causes localised cell necrosis in the region of the implanted material. This is a tissue reaction, which can produce pain and discomfort in skin tissue.
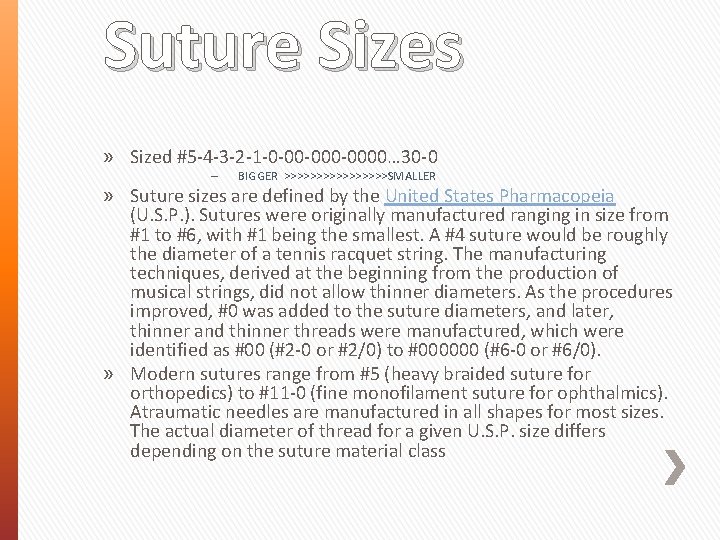
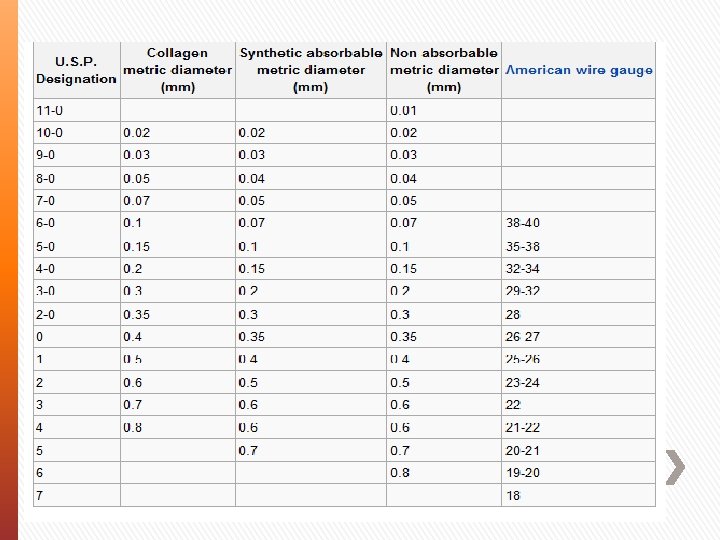
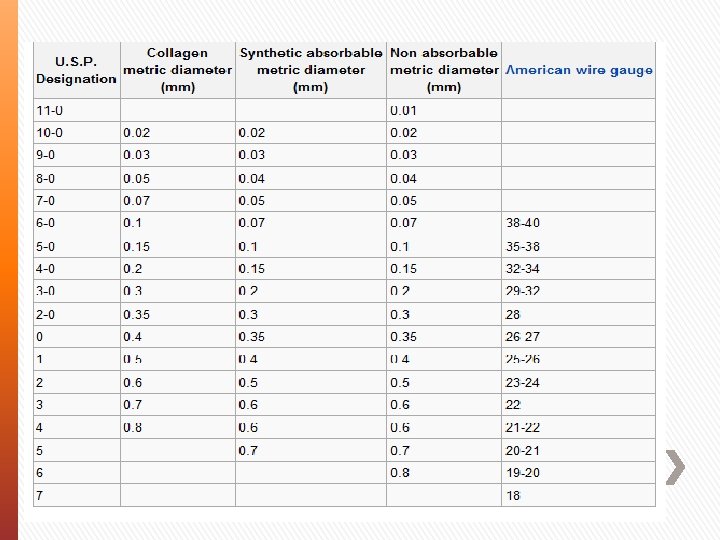
Suture Sizes » Sized #5 -4 -3 -2 -1 -0 -00 -0000… 30 -0 – BIGGER >>>>>>>>SMALLER » Suture sizes are defined by the United States Pharmacopeia (U. S. P. ). Sutures were originally manufactured ranging in size from #1 to #6, with #1 being the smallest. A #4 suture would be roughly the diameter of a tennis racquet string. The manufacturing techniques, derived at the beginning from the production of musical strings, did not allow thinner diameters. As the procedures improved, #0 was added to the suture diameters, and later, thinner and thinner threads were manufactured, which were identified as #00 (#2 -0 or #2/0) to #000000 (#6 -0 or #6/0). » Modern sutures range from #5 (heavy braided suture for orthopedics) to #11 -0 (fine monofilament suture for ophthalmics). Atraumatic needles are manufactured in all shapes for most sizes. The actual diameter of thread for a given U. S. P. size differs depending on the suture material class
Skin Staples » » » Very common in human medicine Expensive Very easy Very secure Very little tissue reaction Removal = ˃ Special tool required
Tissue Adhesive » Nexaband, Vetbond, and others » Little strength » Should not be placed between skin layers or inside body

Surgical Needles
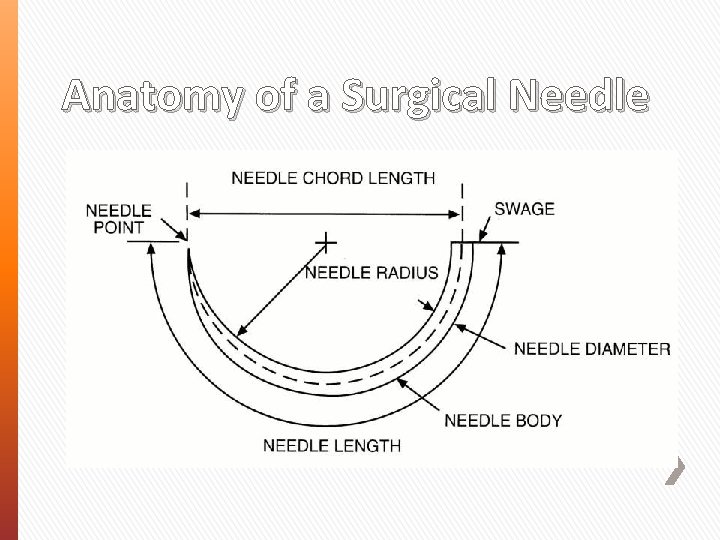
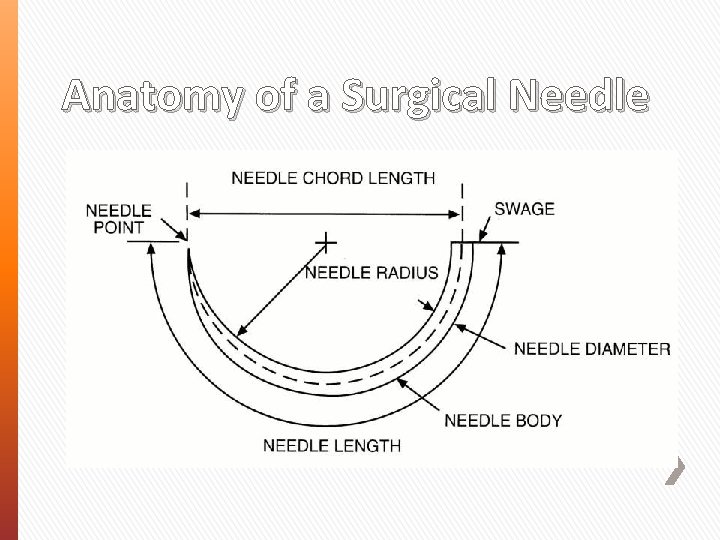
Anatomy of a Surgical Needle
Types of Needles » Eyed needles/ Traumatic needles ˃ More Traumatic ˃ Only thread through once ˃ Suture on a reel ˃ Tends to unthread itself easily
Types of Needles » Swaged-on needles/ Atraumatic needles ˃ Much less traumatic ˃ More expensive suture material ˃ Sterile
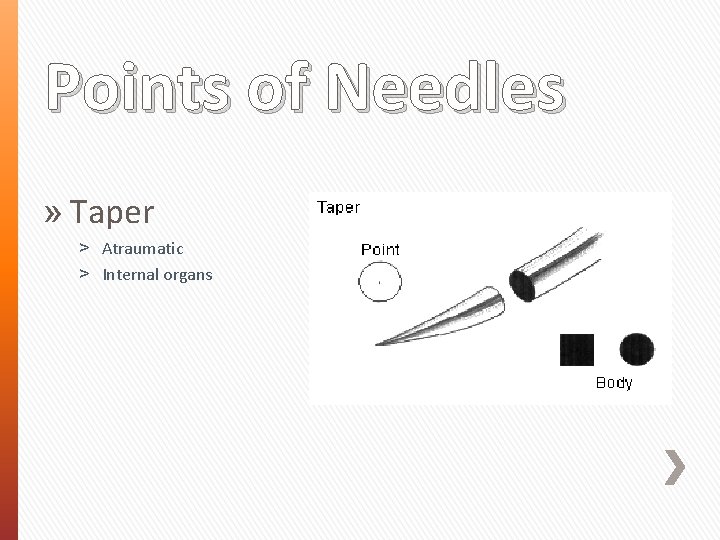
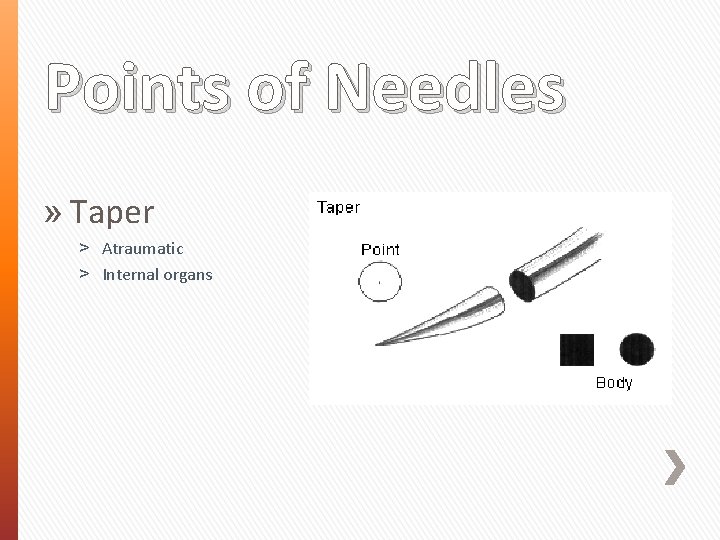
Points of Needles » Taper ˃ Atraumatic ˃ Internal organs
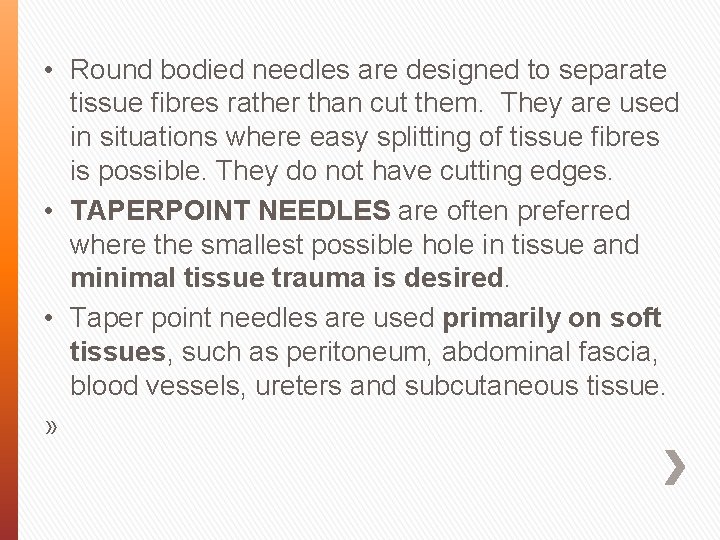
• Round bodied needles are designed to separate tissue fibres rather than cut them. They are used in situations where easy splitting of tissue fibres is possible. They do not have cutting edges. • TAPERPOINT NEEDLES are often preferred where the smallest possible hole in tissue and minimal tissue trauma is desired. • Taper point needles are used primarily on soft tissues, such as peritoneum, abdominal fascia, blood vessels, ureters and subcutaneous tissue. »
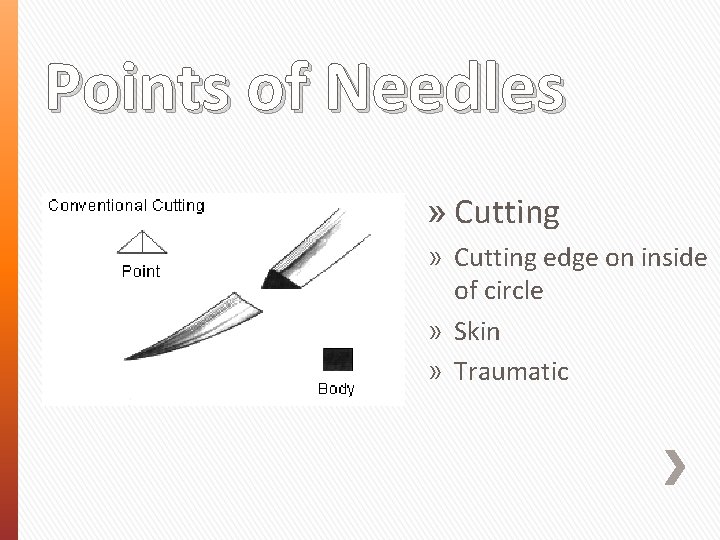
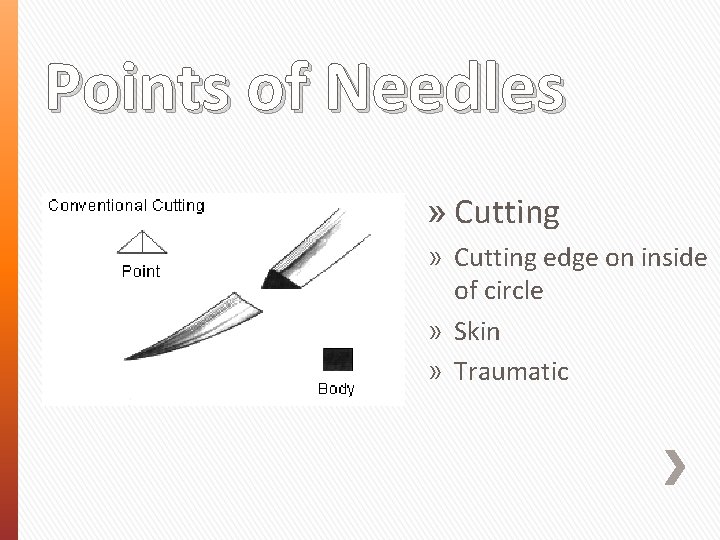
Points of Needles » Cutting edge on inside of circle » Skin » Traumatic
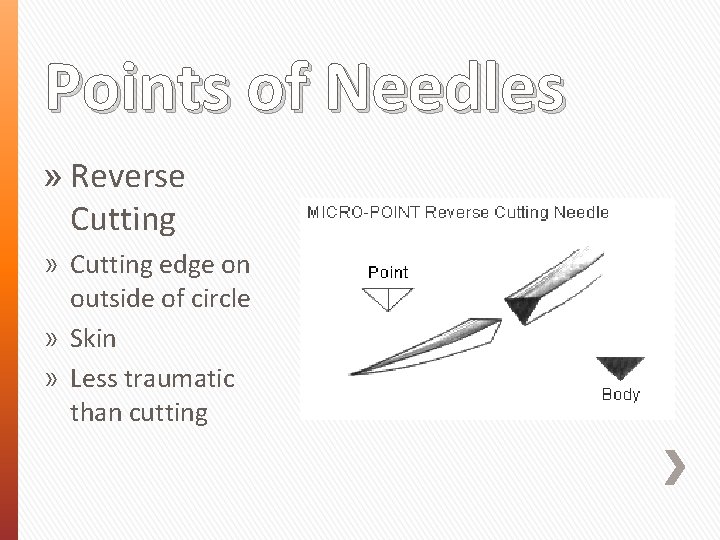
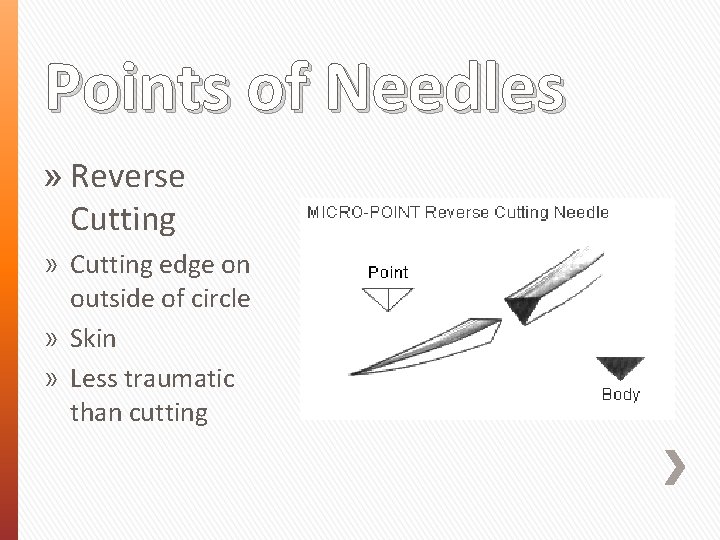
Points of Needles » Reverse Cutting » Cutting edge on outside of circle » Skin » Less traumatic than cutting
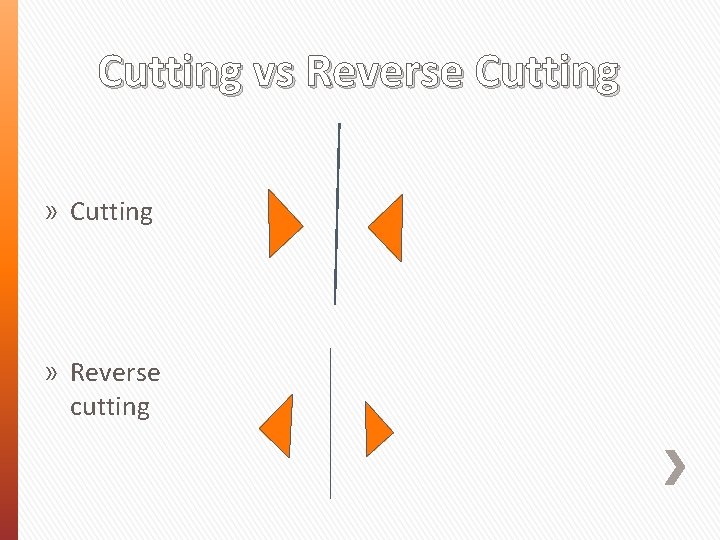
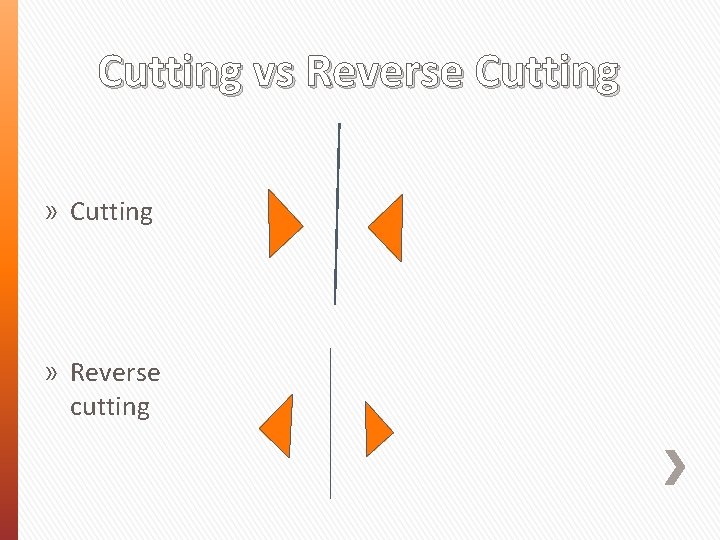
Cutting vs Reverse Cutting » Reverse cutting
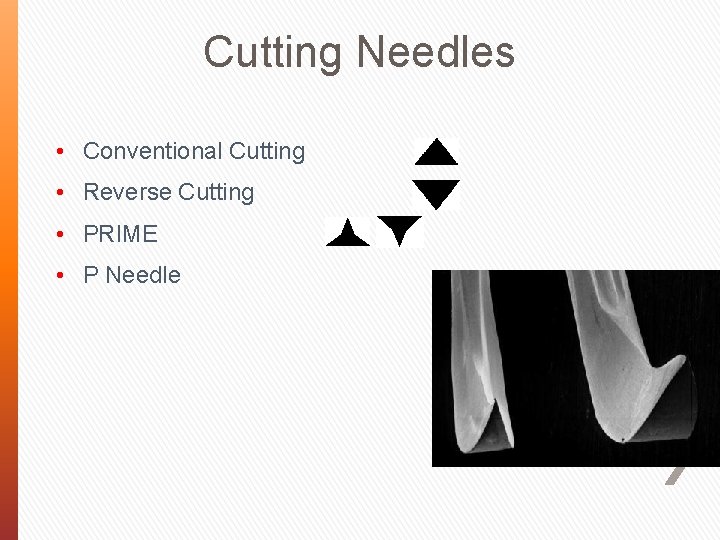
Cutting Needles • Conventional Cutting • Reverse Cutting • PRIME • P Needle
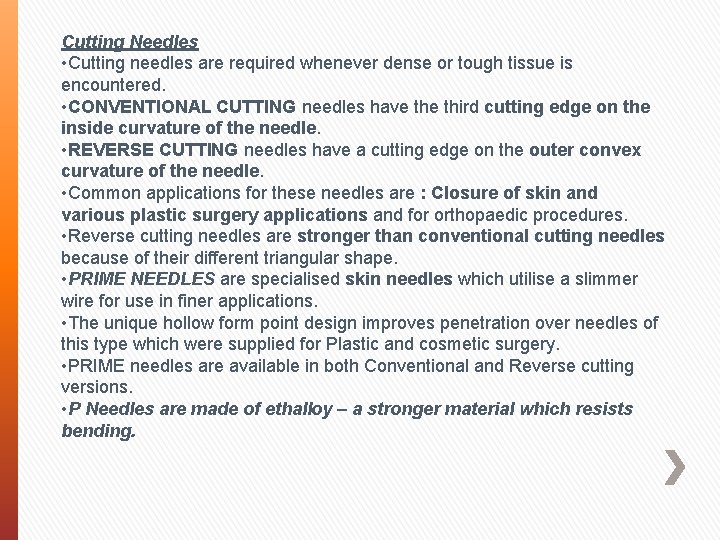
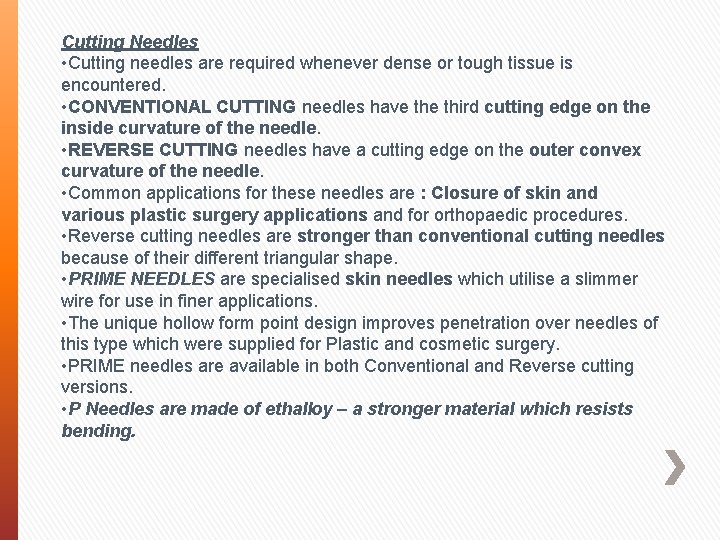
Cutting Needles • Cutting needles are required whenever dense or tough tissue is encountered. • CONVENTIONAL CUTTING needles have third cutting edge on the inside curvature of the needle. • REVERSE CUTTING needles have a cutting edge on the outer convex curvature of the needle. • Common applications for these needles are : Closure of skin and various plastic surgery applications and for orthopaedic procedures. • Reverse cutting needles are stronger than conventional cutting needles because of their different triangular shape. • PRIME NEEDLES are specialised skin needles which utilise a slimmer wire for use in finer applications. • The unique hollow form point design improves penetration over needles of this type which were supplied for Plastic and cosmetic surgery. • PRIME needles are available in both Conventional and Reverse cutting versions. • P Needles are made of ethalloy – a stronger material which resists bending.
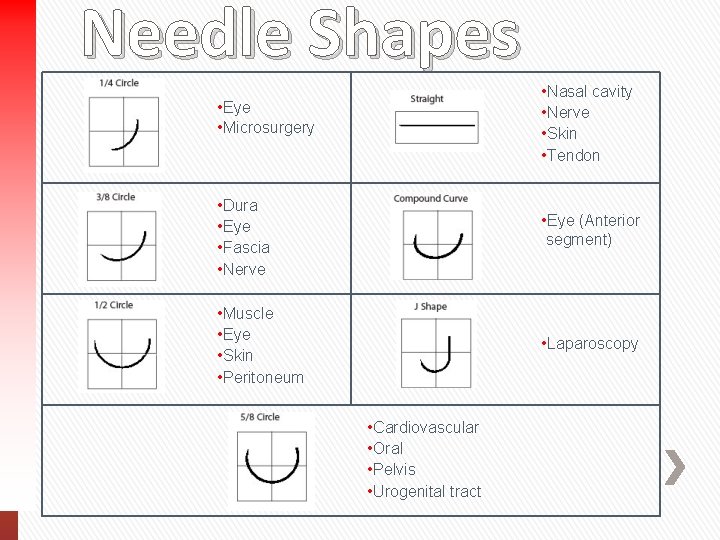
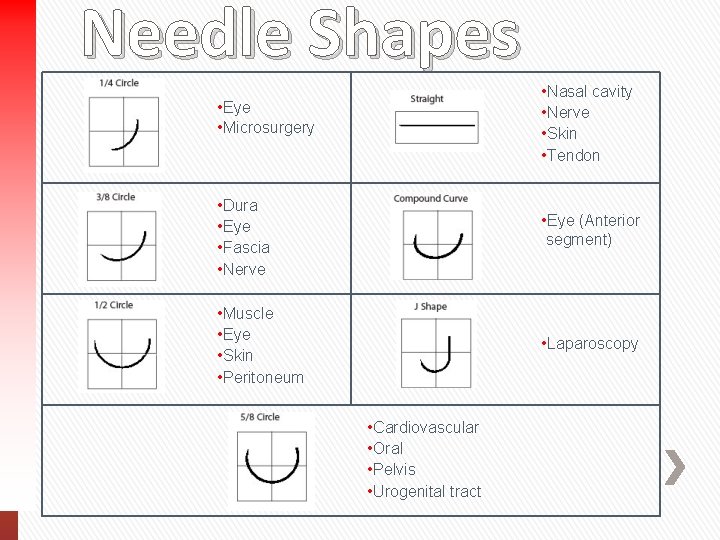
Needle Shapes • Eye • Microsurgery • Nasal cavity • Nerve • Skin • Tendon • Dura • Eye • Fascia • Nerve • Eye (Anterior segment) • Muscle • Eye • Skin • Peritoneum • Laparoscopy • Cardiovascular • Oral • Pelvis • Urogenital tract
• Needles are available in various shapes to accommodate the desired depth of bite and the desired "turnout" in specific tissue. The available shapes are shown on the slide. • Selection of the needle shape is dependent on the size and depth of the area to be sutured. Use of the 1/4 circle needle is often limited to ophthalmic and microsurgical procedures. • A commonly used curved needle is the 3/8 Circle. These needles can be easily manipulated in relatively large and superficial wounds such as closure of the dermis. • Because a large arc of manipulation is required, 3/8 Circle needles can be awkward or impossible to use in deep cavities such as the pelvis or in other small difficult to access locations. • A 1/2 Circle needle is relatively easy to use in these confined locations, although it requires more rotation of the wrist than a 3/8 circle. • The tip of a 1/2 circle needle can become obscured by tissue deep in the pelvic cavity for example. When this occurs the surgeon may have difficulty locating the point to reposition the needle holder and pull the needle through tissue. A 5/8 Circle needle may be useful in this situation, as may a 'J' needle. • Straight needles are generally used for skin and compound curved needles for Ophthalmics.
 Ram input or output device
Ram input or output device Conclusion of medical surgical nursing
Conclusion of medical surgical nursing Asepsis
Asepsis Ogden surgical medical society
Ogden surgical medical society What is medical asepsis
What is medical asepsis Bibliography of medical surgical nursing
Bibliography of medical surgical nursing Ideal suture
Ideal suture Suture material classification
Suture material classification Datum shift
Datum shift Material yield variance formula
Material yield variance formula Cultural relativism definition
Cultural relativism definition Whats cultural lag
Whats cultural lag Examples of non material culture
Examples of non material culture What is useful materials
What is useful materials Motorized material handling equipment
Motorized material handling equipment A tagout device is preferable to using a lockout device.
A tagout device is preferable to using a lockout device. Input device dan output device
Input device dan output device Gmdn udi
Gmdn udi Medical device academy
Medical device academy Medical device security conference
Medical device security conference Feasibility study medical device
Feasibility study medical device Medical devices software fmea
Medical devices software fmea Cdsco medical device classification
Cdsco medical device classification Vaporizer medical device
Vaporizer medical device Ecri umdns
Ecri umdns Medical device safety
Medical device safety Emergo medical device registration
Emergo medical device registration California medical license application
California medical license application Gbmc infoweb
Gbmc infoweb Difference between medical report and medical certificate
Difference between medical report and medical certificate Torrance memorial transitional care unit
Torrance memorial transitional care unit Cartersville medical center medical records
Cartersville medical center medical records Aappm
Aappm Surgical gown
Surgical gown Surgical sieve vitamin c
Surgical sieve vitamin c Betadine scrub and paint guidelines
Betadine scrub and paint guidelines Surgical education week
Surgical education week Microwave diathermy block diagram
Microwave diathermy block diagram Surgical audit cycle
Surgical audit cycle Proctologic position
Proctologic position Surgical metabolism
Surgical metabolism Surgical metabolism
Surgical metabolism Surgical planning laboratory
Surgical planning laboratory Surgical metabolism
Surgical metabolism A nurse floats to a busy surgical unit
A nurse floats to a busy surgical unit Surgical conscience
Surgical conscience Lyphadenitis
Lyphadenitis Care of critically ill surgical patient
Care of critically ill surgical patient Hibiclense
Hibiclense Avagard surgical scrub instructions
Avagard surgical scrub instructions Fascia stapler
Fascia stapler Chapter 27 patient safety and quality
Chapter 27 patient safety and quality Surgical team roles and responsibilities
Surgical team roles and responsibilities Prevention of vte in nonorthopedic surgical patients
Prevention of vte in nonorthopedic surgical patients Color coding of sutures
Color coding of sutures