Sterilization and Disinfections Dr Saeed Naser Eldin Saeed

- Slides: 49
Sterilization and Disinfections Dr. Saeed Naser- Eldin Saeed
Sterilization Killing or destroying All forms of living microorganisms from objects. (bacteria and their spores). Sterilization is an absolute term means germ free objects. Disinfection: ◦ Is removing or reducing the number of the pathogenic microorganisms from objects. (Not absolute) ◦ Unable to destroy spores and some could not kill non enveloped viruses.
Methods used Physical methods. ◦ Chemical methods. ◦ Physical methods. ◦ Are more commonly used, simple, economical and reliable.
prevention of microbial growth: important in: • Food industry. • Health care: nosocomial infections. • Drinking water distribution systems • other industrial processes: e. g. , biofouling of oil pipeliness • The objective is to render the articles non infectious.
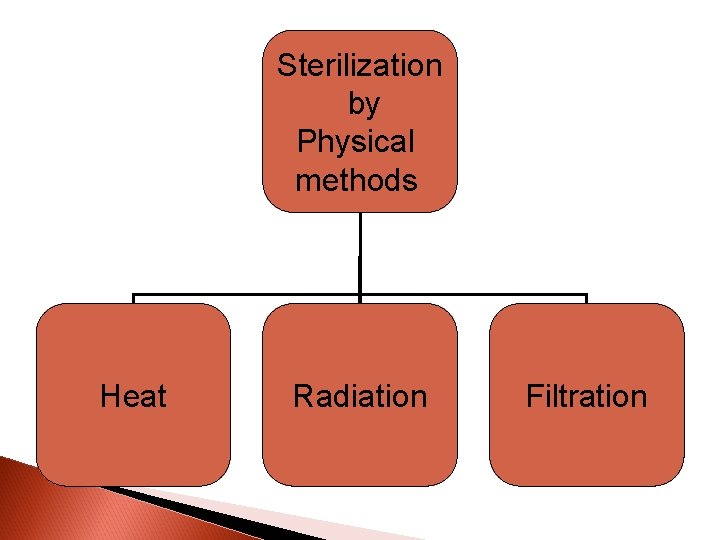
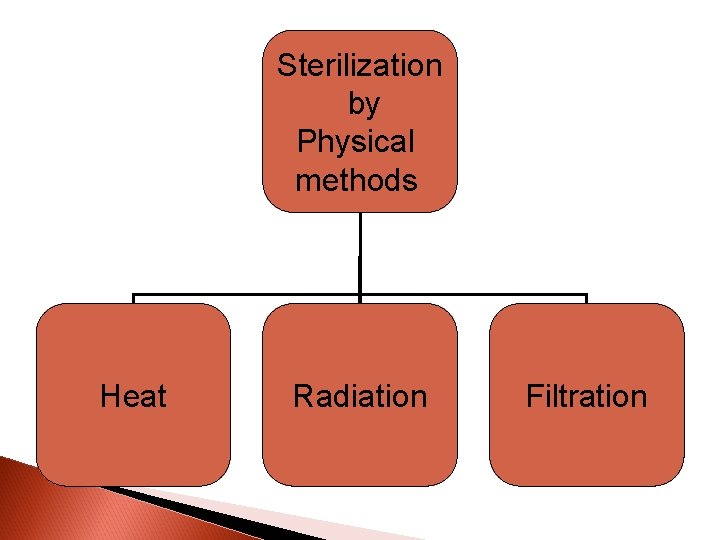
Sterilization by Physical methods Heat Radiation Filtration
Physical methods Heat: ◦ Exposure of the objects to heat will kills microbes by coagulation of protein, denaturation of enzymes and oxidation. Filtration: ◦ Sterilization through removing of microbes from fluids by exposing them to small size filter. This is used for heat sensitive fluids like serum, sugars and urea. Radiation: ◦ Exposure to radiation: This causes denaturation of proteins and enzymes.
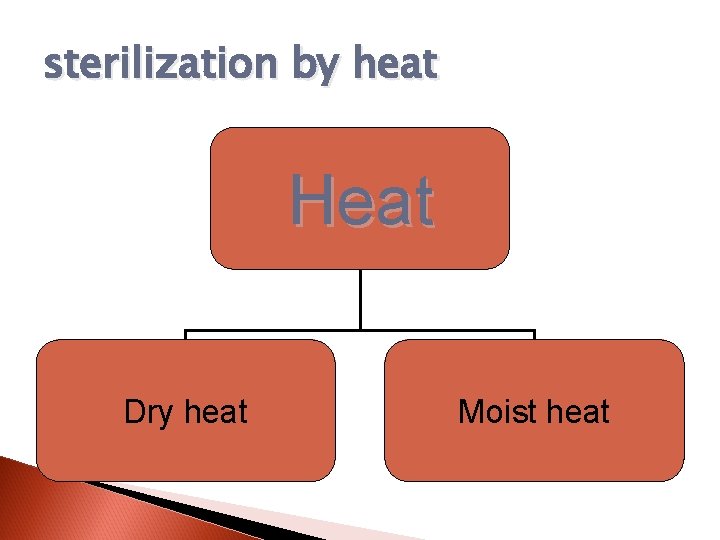
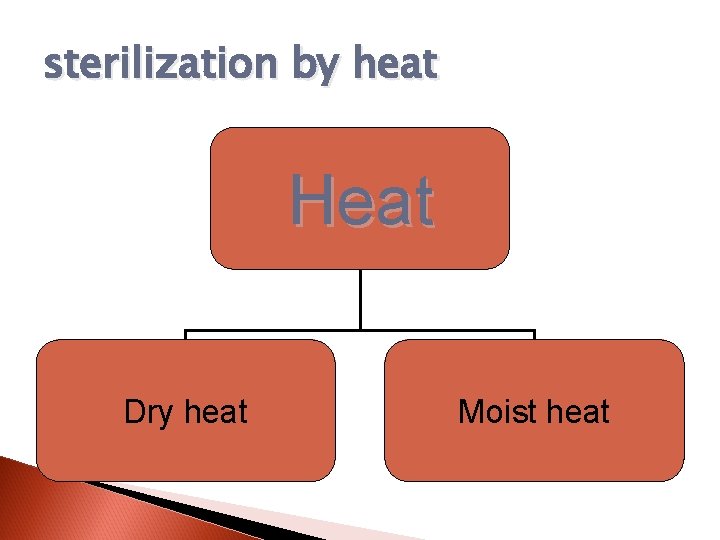
sterilization by heat Heat Dry heat Moist heat
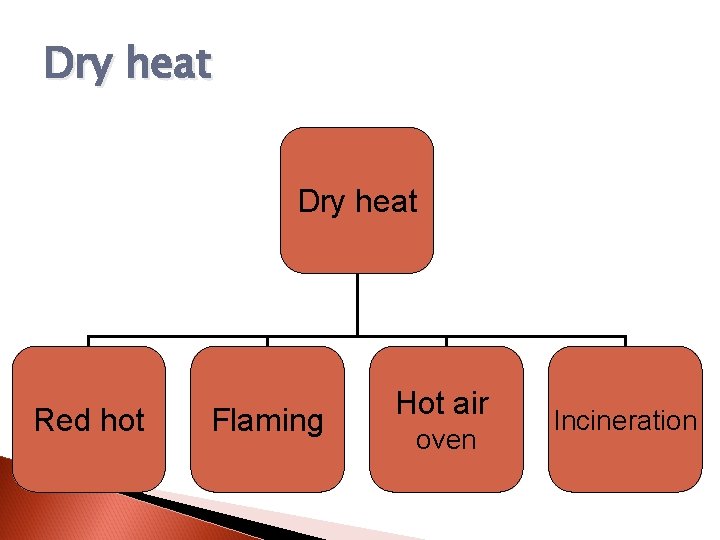
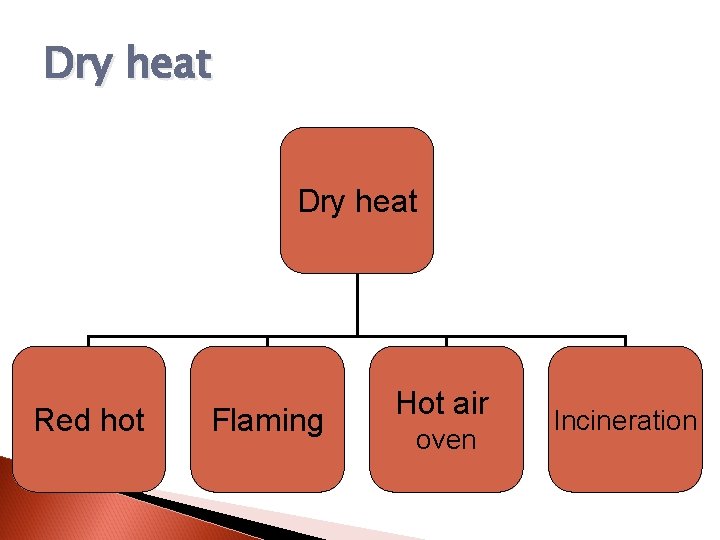
Dry heat Red hot Flaming Hot air oven Incineration
Red hot (Reddening) Exposure of wires and forceps to the Bunsen flame until it becomes red hot, then cooled down and used. Used for wire loop, straight wire, forceps, scalpels and metal rods.
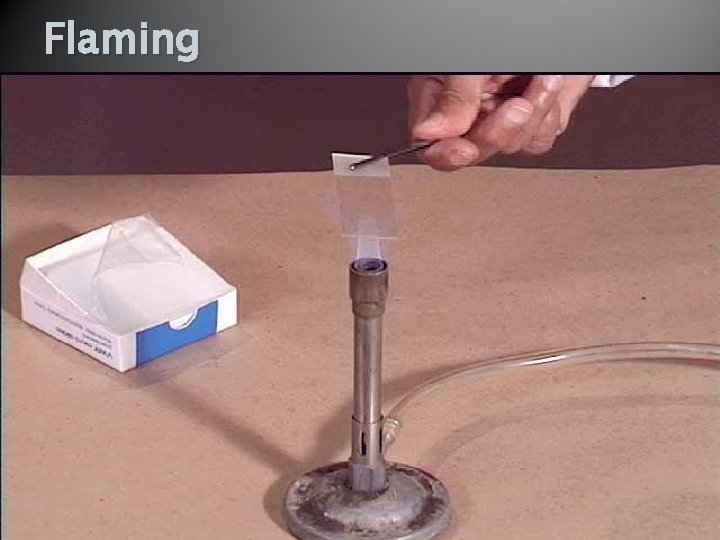
Flaming Slowly passing of objects to the Bunsen flame to reduce the number of microorganisms. The Bunsen flame give partially sterile area around it. This is used for sterilization of the mouth of bottle, flasks, containers and test tubes. it is also used for the preparation of smears, cultivation of bacteria ands. subculture
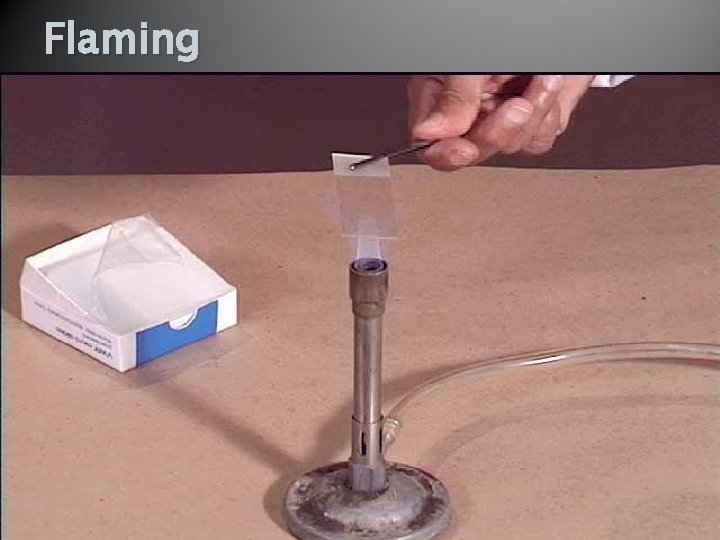
Flaming
Hot air oven This is a metal chamber (instruments) consists of a heater, thermometer, thermostat, perforated shelves, door and timer. It kills microbes by oxidation-reduction. There are certain thermal death points and Thermal death times for the articles to be sterilized: ◦ 160 C for 60 min. ◦ 170 C for 40 min. ◦ 180 C for 30 min.

oven for dry heat sterilization
Check the efficiency Bowei Dick test (Adhesive tabe). Browne’s tube No 3. (Red ----- green).
Incineration (Burnning) Is treating of an objects to heating over 250 until they become black. Done for used equipment.
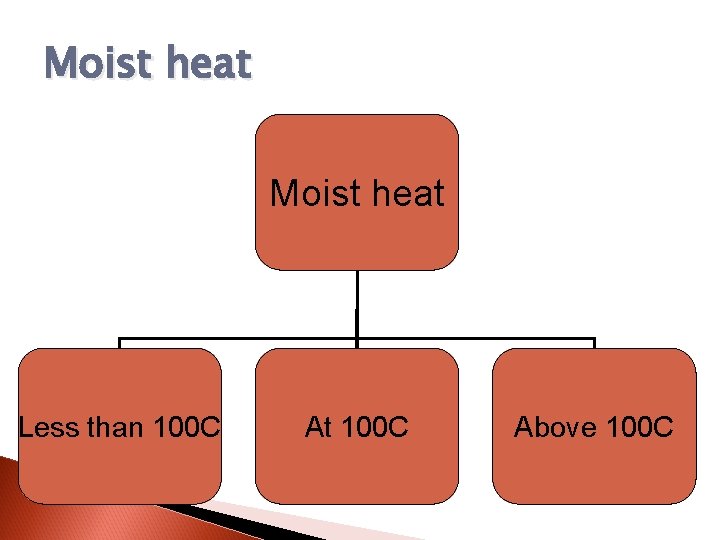
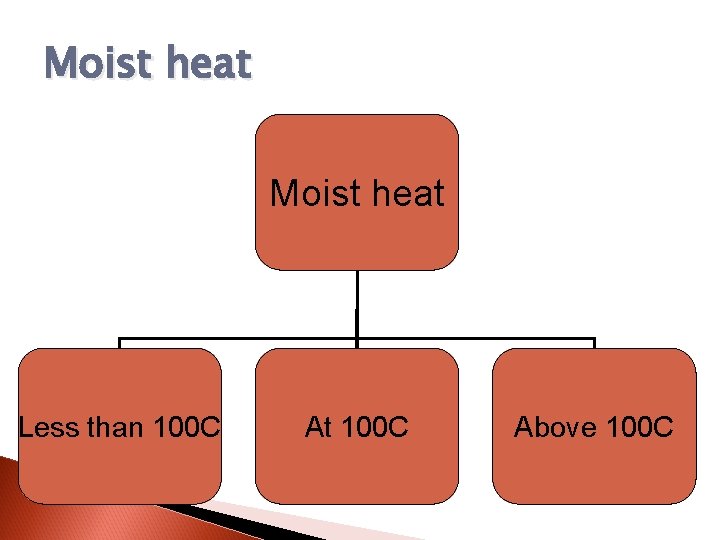
Moist heat Less than 100 C At 100 C Above 100 C
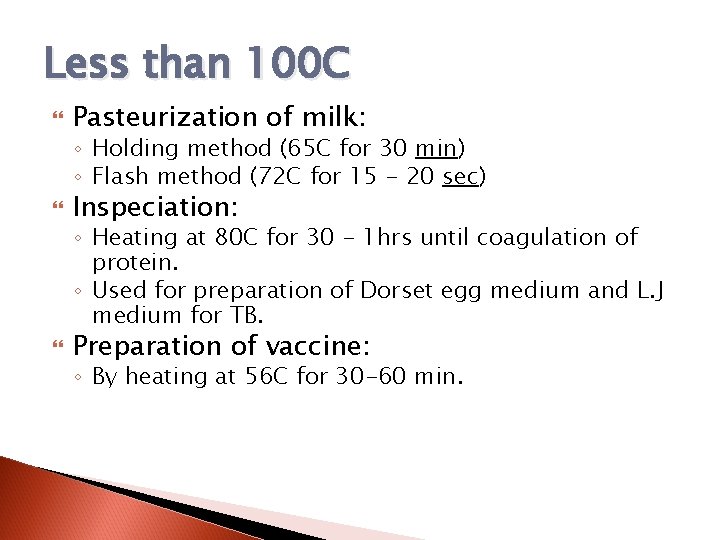
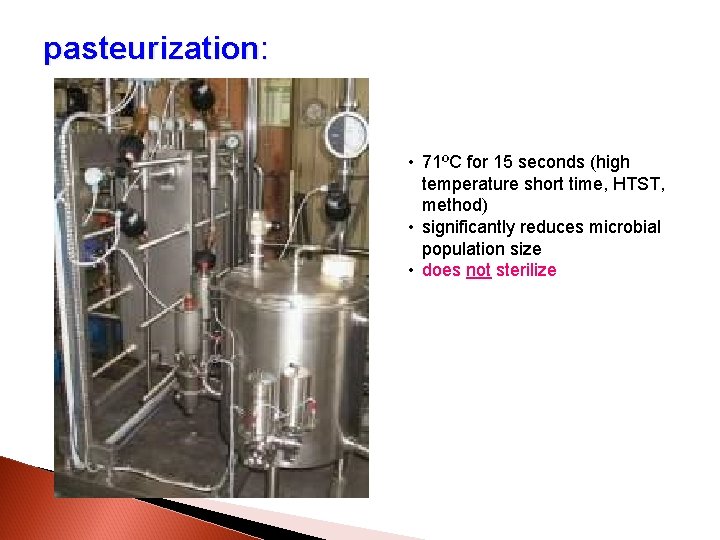
Less than 100 C Pasteurization of milk: ◦ Holding method (65 C for 30 min) ◦ Flash method (72 C for 15 - 20 sec) Inspeciation: ◦ Heating at 80 C for 30 - 1 hrs until coagulation of protein. ◦ Used for preparation of Dorset egg medium and L. J medium for TB. Preparation of vaccine: ◦ By heating at 56 C for 30 -60 min.
pasteurization: • 71ºC for 15 seconds (high temperature short time, HTST, method) • significantly reduces microbial population size • does not sterilize
At 100 C Steaming (Koch steamer): ◦ Single exposure of the microbe to steam at 100 C for 90 min (Shelves over the boiler). ◦ Tyndalization: Steaming at 100 C for 30 min for 3 successive days. 1 st day kill vegetative bacteria and germinate sporulated one ---- Put on the bench. 2 nd day kills all vegetative bacteria ---- Put on the bench. 3 rd day insure complete sterilization. Boiling (Inside the boiler, no shelves) ◦ At 100 C for 30 min.
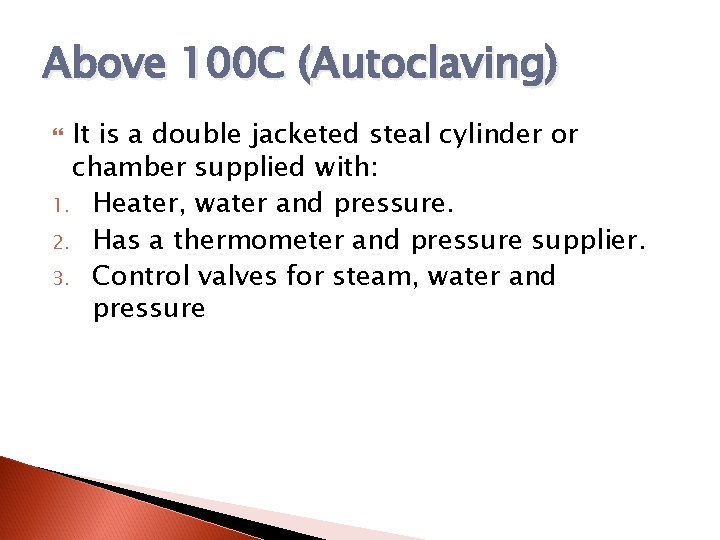
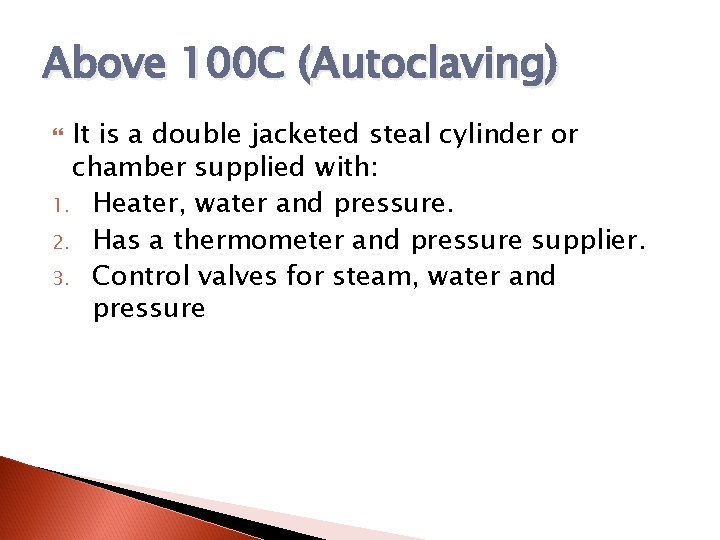
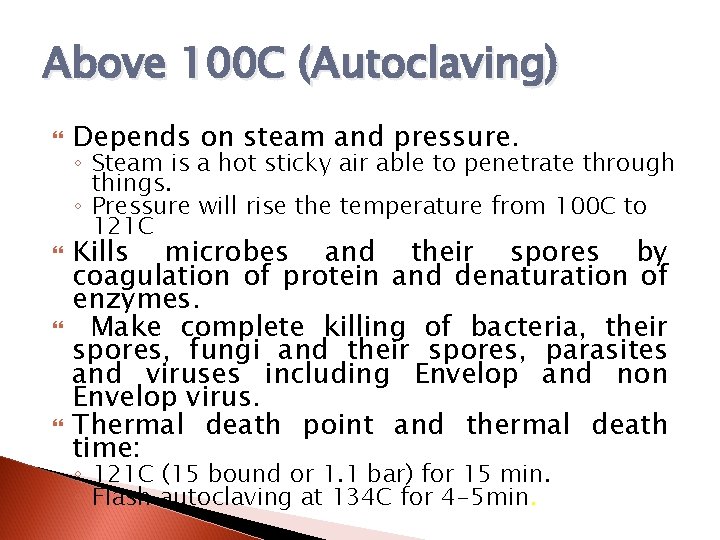
Above 100 C (Autoclaving) It is a double jacketed steal cylinder or chamber supplied with: 1. Heater, water and pressure. 2. Has a thermometer and pressure supplier. 3. Control valves for steam, water and pressure
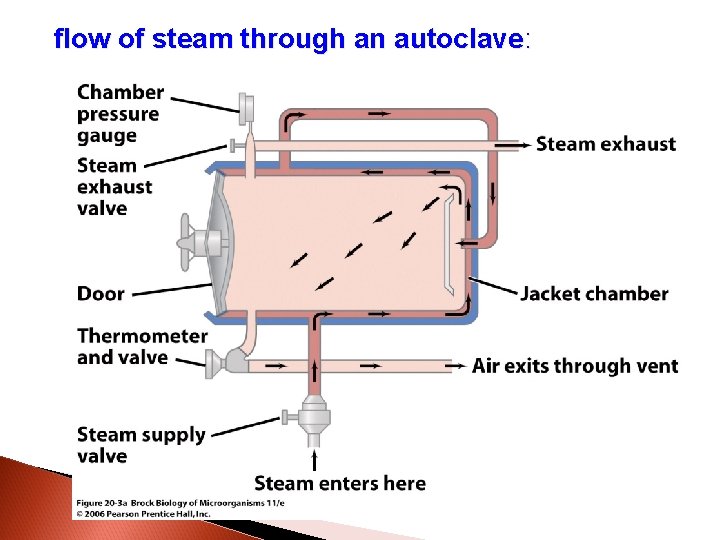
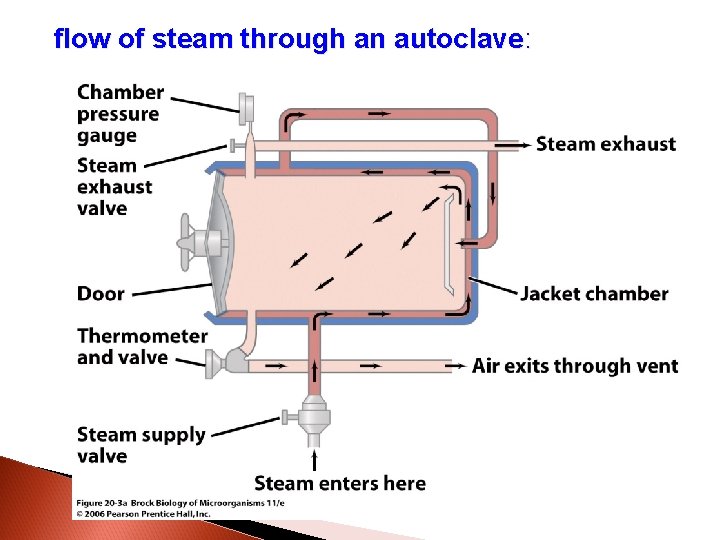
flow of steam through an autoclave:
Above 100 C (Autoclaving) Depends on steam and pressure. ◦ Steam is a hot sticky air able to penetrate through things. ◦ Pressure will rise the temperature from 100 C to 121 C Kills microbes and their spores by coagulation of protein and denaturation of enzymes. Make complete killing of bacteria, their spores, fungi and their spores, parasites and viruses including Envelop and non Envelop virus. Thermal death point and thermal death time: ◦ 121 C (15 bound or 1. 1 bar) for 15 min. ◦ Flash autoclaving at 134 C for 4 -5 min.
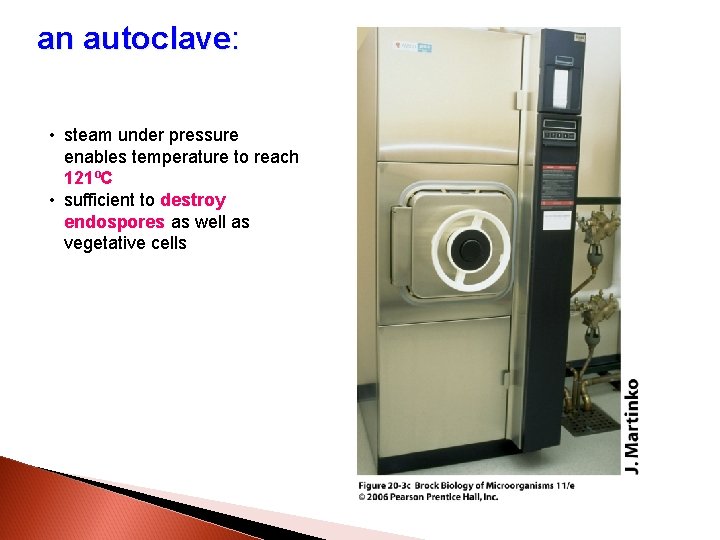
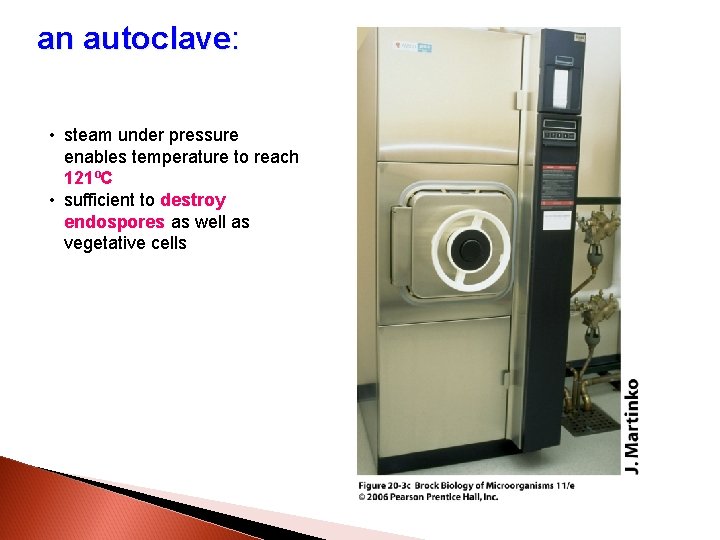
an autoclave: • steam under pressure enables temperature to reach 121ºC • sufficient to destroy endospores as well as vegetative cells
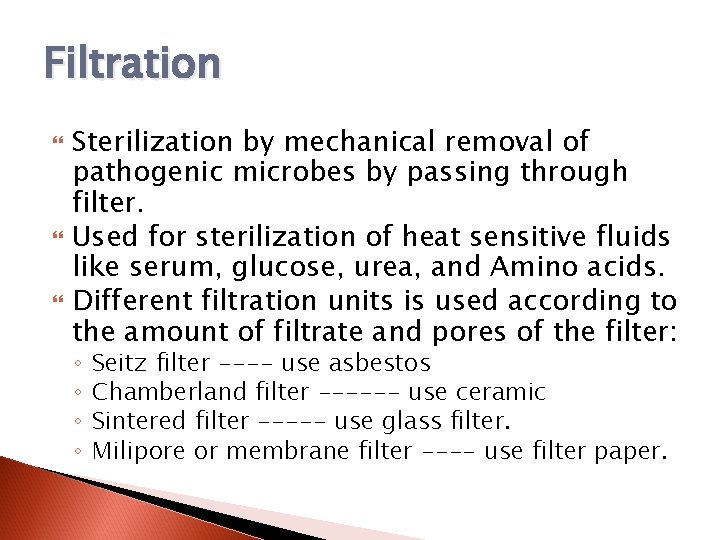
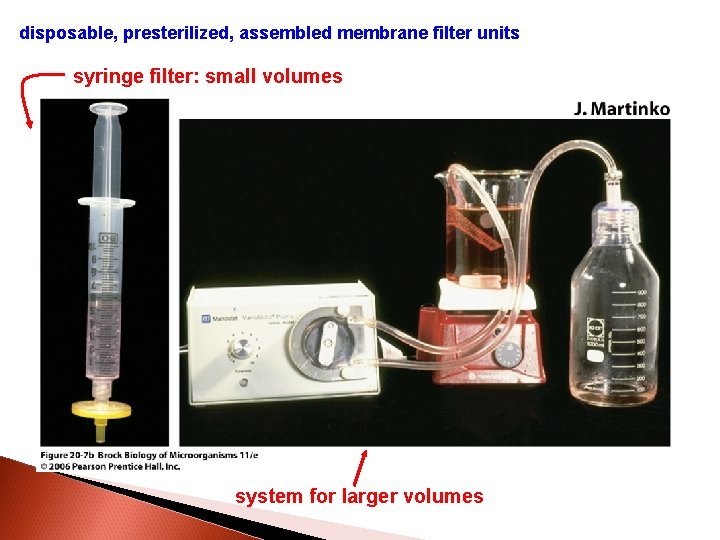
Filtration Sterilization by mechanical removal of pathogenic microbes by passing through filter. Used for sterilization of heat sensitive fluids like serum, glucose, urea, and Amino acids. Different filtration units is used according to the amount of filtrate and pores of the filter: ◦ ◦ Seitz filter ---- use asbestos Chamberland filter ------ use ceramic Sintered filter ----- use glass filter. Milipore or membrane filter ---- use filter paper.
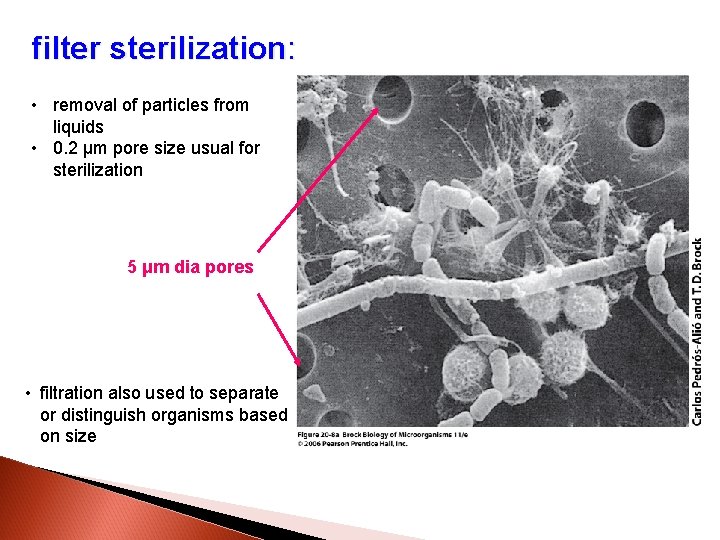
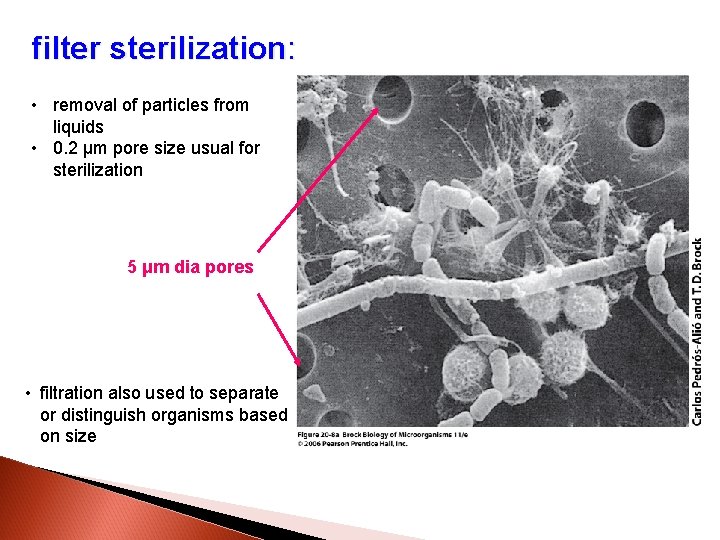
filter sterilization: • removal of particles from liquids • 0. 2 μm pore size usual for sterilization 5 μm dia pores • filtration also used to separate or distinguish organisms based on size
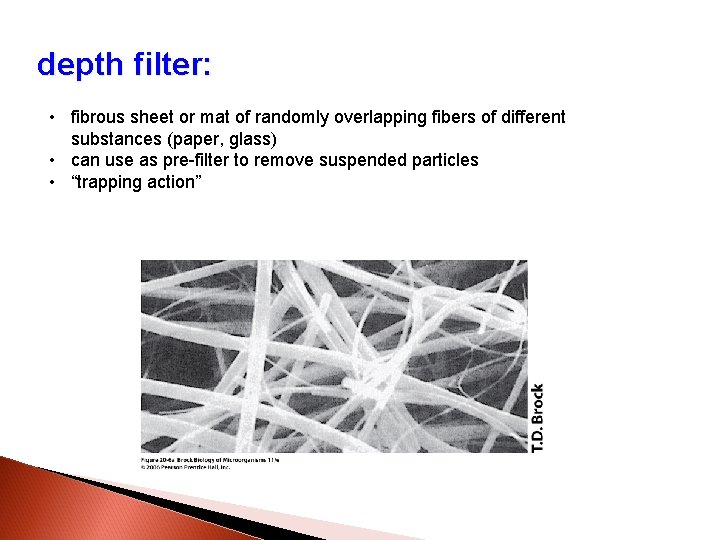
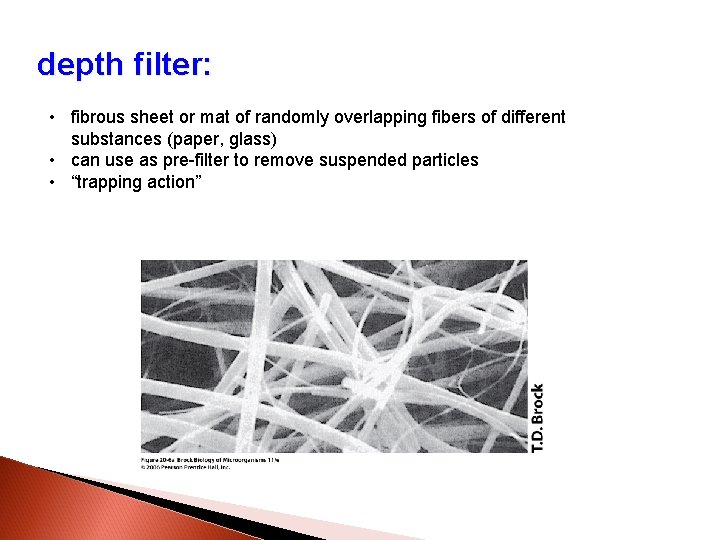
depth filter: • fibrous sheet or mat of randomly overlapping fibers of different substances (paper, glass) • can use as pre-filter to remove suspended particles • “trapping action”
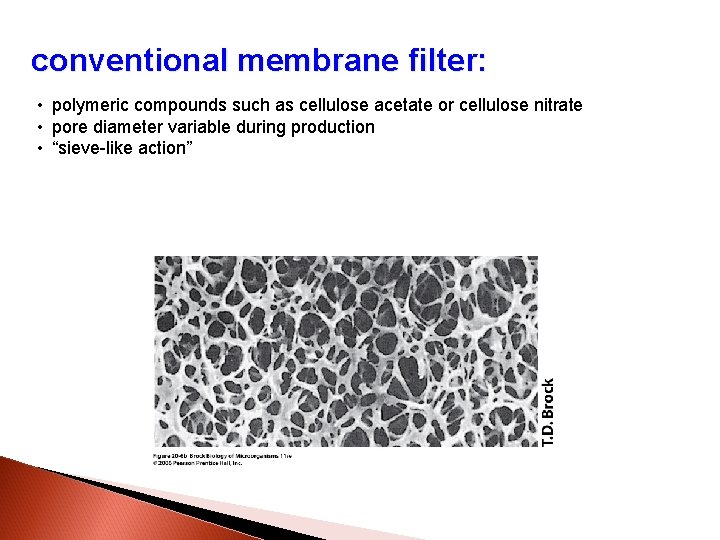
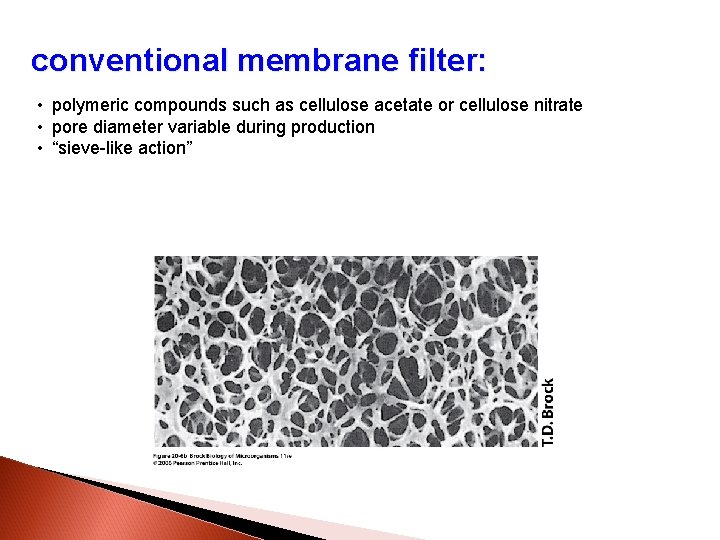
conventional membrane filter: • polymeric compounds such as cellulose acetate or cellulose nitrate • pore diameter variable during production • “sieve-like action”
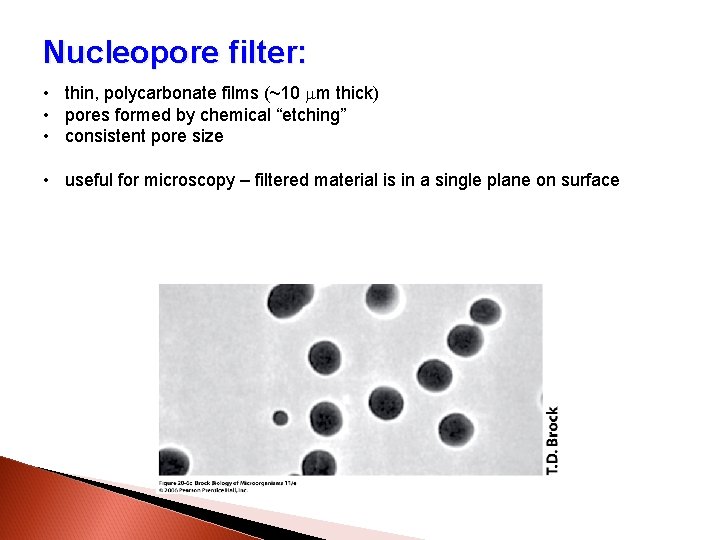
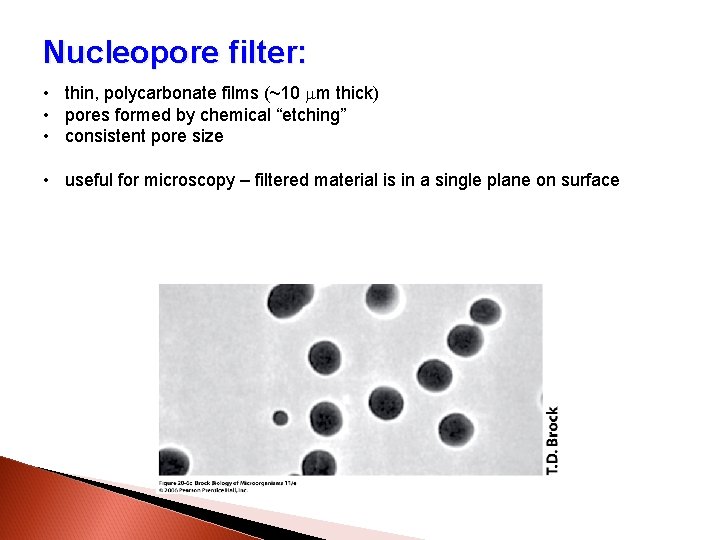
Nucleopore filter: • thin, polycarbonate films (~10 mm thick) • pores formed by chemical “etching” • consistent pore size • useful for microscopy – filtered material is in a single plane on surface
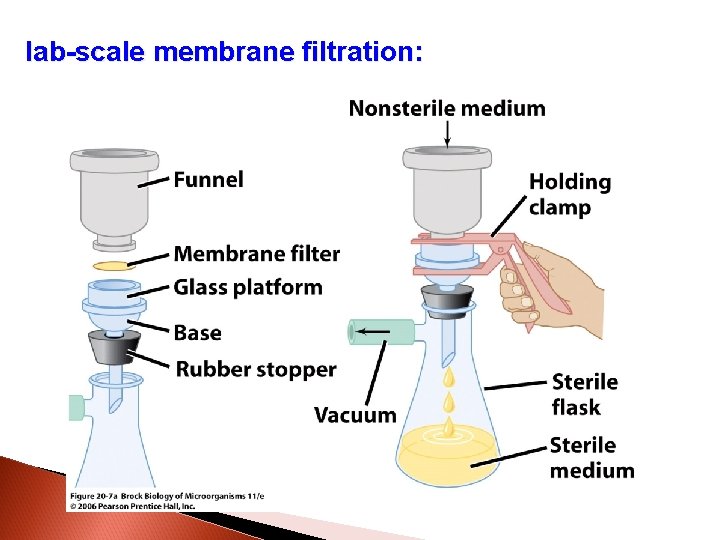
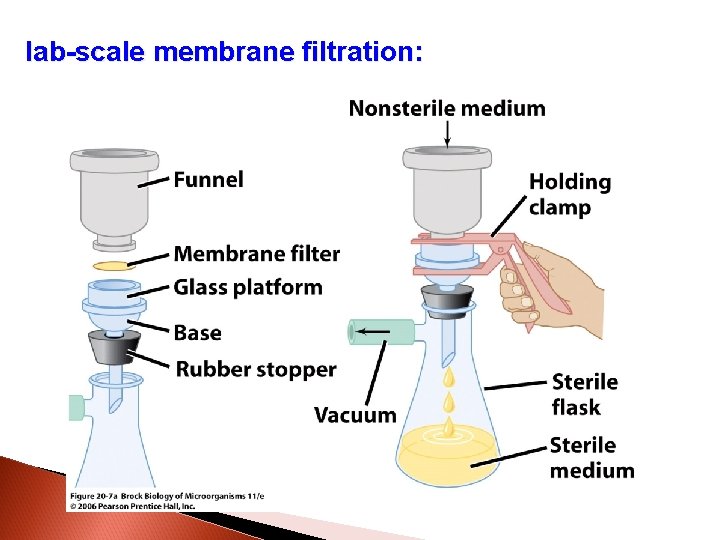
lab-scale membrane filtration:
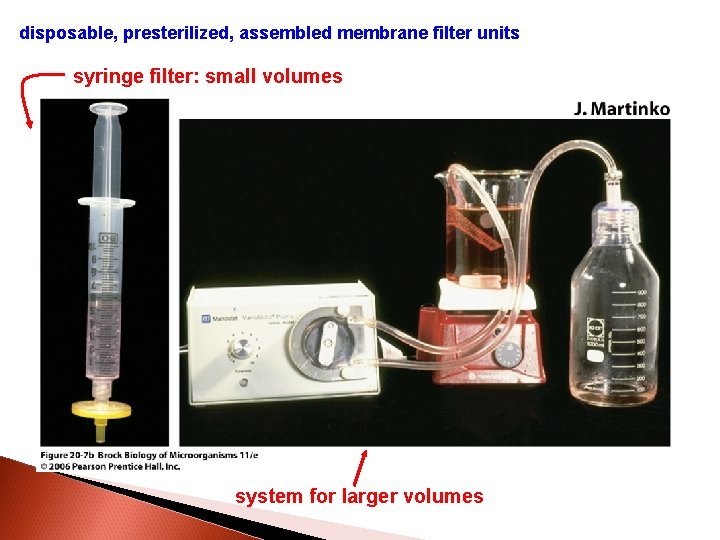
disposable, presterilized, assembled membrane filter units syringe filter: small volumes system for larger volumes
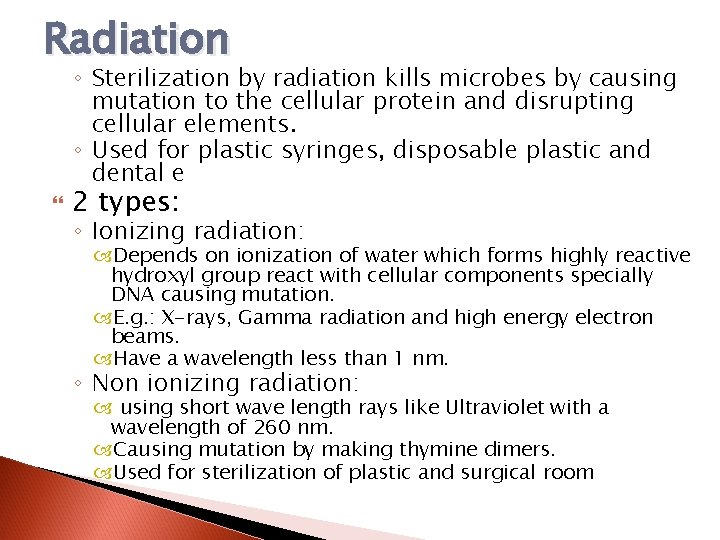
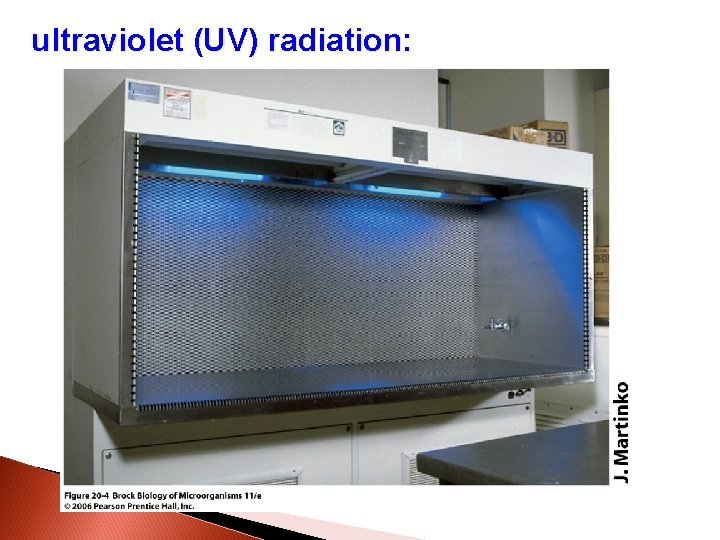
Radiation ◦ Sterilization by radiation kills microbes by causing mutation to the cellular protein and disrupting cellular elements. ◦ Used for plastic syringes, disposable plastic and dental e 2 types: ◦ Ionizing radiation: Depends on ionization of water which forms highly reactive hydroxyl group react with cellular components specially DNA causing mutation. E. g. : X-rays, Gamma radiation and high energy electron beams. Have a wavelength less than 1 nm. ◦ Non ionizing radiation: using short wave length rays like Ultraviolet with a wavelength of 260 nm. Causing mutation by making thymine dimers. Used for sterilization of plastic and surgical room
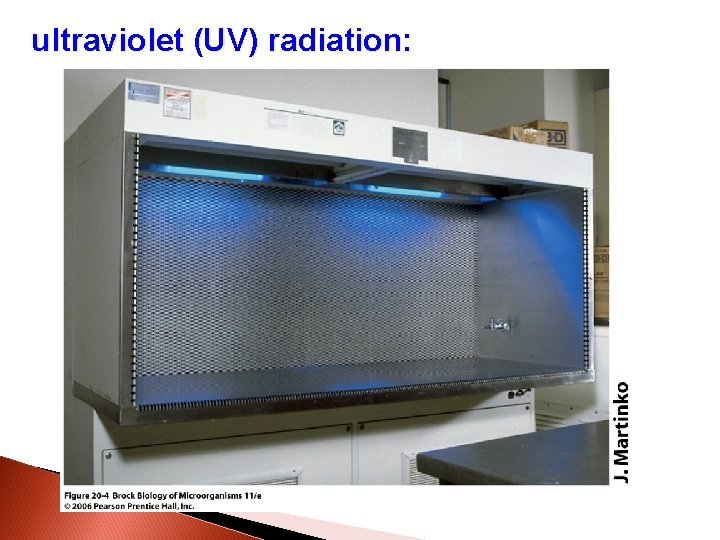
ultraviolet (UV) radiation:
Disinfection Chemical methods of sterilization
Disinfection: ◦ Is removing of pathogenic microorganism or reducing their number on the exposed area. ◦ Unable to destroy spores and some could not kill non envelop viruses. Factors affects disinfection action: ◦ ◦ ◦ ◦ Type of disinfecant used. Concentration of disinfectant. Type of microorganism. Number of microorganism. Time of exposure. Temperature. Presence of organic compound.
examples of modes of action: • alcohol - lipid solvent, protein denaturant • hydrogen peroxide (H 2 O 2) – oxidizing agent • triclosan (a phenolic) – disrupts cell membrane • chlorine gas – oxidizing agent • ethylene oxide – alkylating agent
1. Phenolic group of disinfectant: E. g. : Phenol crystal, Dittol, Lysol, Cresol. Injuring lipid containing plasma membrane leads to leakage of cellular contents. Remain active in the presence of organic materials, stable and persist for long period of time. Suitable for disinfecting pus, blood and sputum. Active against G+ve, G-ve, Mycobacterium & viruses.
2. Bisphenol: Contains 2 groups of phenol. Hexaclorophenol used for surgical and microbial control, Excessive use for infant could leads to neurologic damage. Triclosan found in antimicrobial soaps, inhibits an enzyme needed for synthesis of fatty acid which affects the integrity of plasma membrane.
3. Biguanides: E. g. : Chlorohexidine. Broad spectrum activity as disinfectant of skin and mucus membrane due to it is ability to bind to mucus membrane. Cause injury to plasma membrane.
4. Haloges: Iodine have broad spectrum activity to many bacteria, spores, fungi and some viruses, it binds to certain amino acids of enzyme and proteins. Iodophore (Betadine and Isodine) is non pigmented iodine comprise from iodine + organic materials to release the iodine slowly. Used for skin disinfection and wounds. Chlorine in shape of gas or solution combined with water to give HOCl (Oxidizing agents). Used for swimming pools, drinking water and sewage.
5. Alcohols: Causes denaturation of proteins, disrupt membrane and dissolve lipids. They able to act and Evaporate (Volatile). Used as skin disinfectant and in vein puncture in a concentration of 70%.
6. Heavy metals: Silver, mercury and copper Causes denaturation of proteins when bind to it. Silver nitrate is used as a droper to avoid opthalmia neontam by N. gonorrhoea. Silver sulfadiazine (Flamazine) is used in treating infection associated with burns. Copper sulfate is used to destroy green algae (effective in one part/million of water).
7. Dyes: Gention violet, Crystal violet and Eosine are very effective antiseptic.
8. Surface active agents: Soap and other detergent make mechanical remove of microbe by scrubbing of dead tissue so reduce their number. Quaternary ammonium compound are positively charged molecules kills G+ve bacteria. Affects plasma membrane and changes cell permiability. E. g. : Citerimide.
9. Aldehyde: E. g. : Formaldehyde and Gultraldehyde. Inactivate proteins by covalent cross-links with COOH, NH, OH and SH. Used for disinfect hospital instruments, benches and room.
10. Ethylene oxide gas: Used to sterilize plastics in closed chamber similar to autoclave. Denaturate proteins. Bacteriocidal, fungicidal and kills viruses. Used at high temperature 60 C for 4 -24 hrs. Carcinogenic.
11. Peroxygens: H 2 O 2 is an oxidizing agents kills many microbes especially who fail to produce catalase enzymes (Anaerobic bacteria). Used as disinfectant for gas gangrene. Ozone (O 3) also toxic for microbes and used instead of chlorine in treating drinking water.
Tests of Disinfectant activity: In-use test: ◦ Used to determine the proper disinfectant concentration to be used and to check if the used disinfectant is working properly or not: ◦ Take 1 ml from used disinfectant to 9 ml of nutrient broth. Immediately transfer 0. 02 ml into 10 different area of well dried nutrient agar. ◦ Incubate one plate at 37 C for 3 days and the other at R. T for 7 days. ◦ Growth in more than 5 drops- Failure of Disinfectant ◦ No growth ------- good disinfectant ◦ Growth in less than 5 drop --- success but needs increasing the concentration.
Continue…. . Phenol co-efficient test: ◦ Serial 2 fold dilution of both tested disinfectant and phenol are inoculated with Salmonella typhi and immediately re-subcultured on agar medium at 0 time, after 5 minutes and after 10 minutes. ◦ Good disinfectant gives real number after dividing the MIC of the disinfectant against the phenol. ◦ 4/2= 2 Good ◦ 2/4= ½ Bad disinfectant.
Continue…… Time killing assay: ◦ Used to determine the efficiency of disinfectant against bacteria during the times. ◦ Make serial dilution of disinfectant and subculture the commonly isolated bacteria and immediate culture on agar medium at 0 time, after 5 min and 10 min. ◦ Determine the last dilution of disinfectant that able to kill M. O in a shortest time. ◦ Use 4 X this concentration in your lab.