sterilization DEFINATIONS CLEANING It is a process which












- Slides: 49

sterilization
DEFINATIONS CLEANING - It is a process which removes visible contamination but does not necessarily destroy micro organisms. ASEPSIS -Term used to describe methods which prevent contamination of wounds and other sites
ØANTISEPSIS - It is the procedure or application of an antiseptic solution or an agent which inhibits the growth of microorganisms, while remaining in the contact with them. Ø DISINFECTION - it is a process which reduces the number of microorganisms to an acceptable level but may not inactive some viruses and bacterial spores. ØSTERLIZATION any process that effectively kills or eliminates transmissible agents (such as fungi, bacteria, viruses, spore forms, etc. ) from a surface, equipment, article of food or medication, or biological culture medium.
Ø Sanitizing - process of reducing the number of microorganisms Ø Decontamination - process that removes pathogenic microorganisms from an object to make it safe to handle.
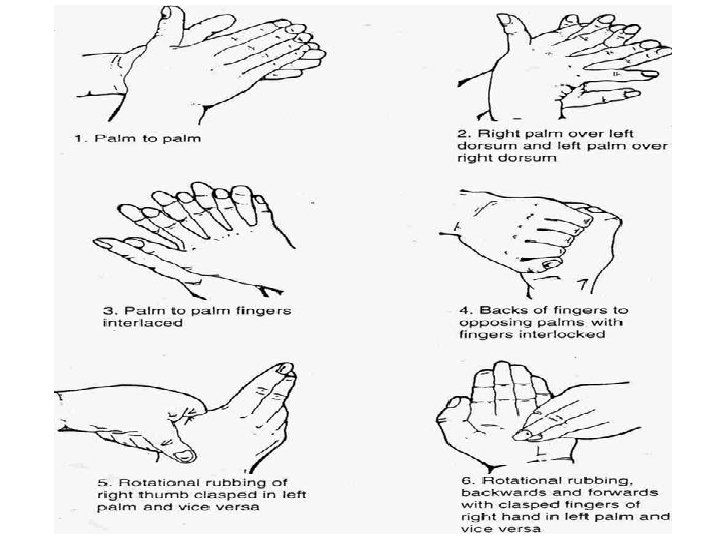
HAND WASHING • Three types of hand washing– Social hand washing – Clinical hand washing – Surgical hand washing
Social hand washing • Recommended following Øsocial-type contact with clients Øafter covering a cough or sneeze. • A plain liquid soap is often used.
Clinical hand washing • A clinical hand wash is used before clinical procedures on clients, when a client is being managed in isolation, or in outbreak situations. • An anti-microbial soap, containing an antiseptic agent, is used.
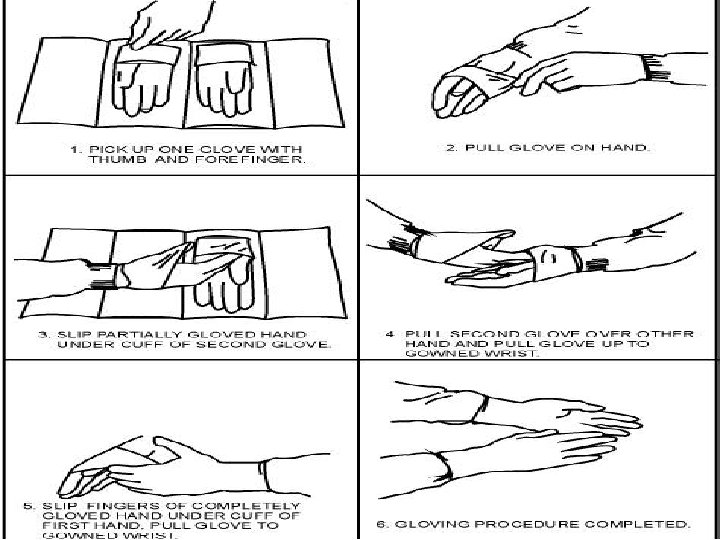
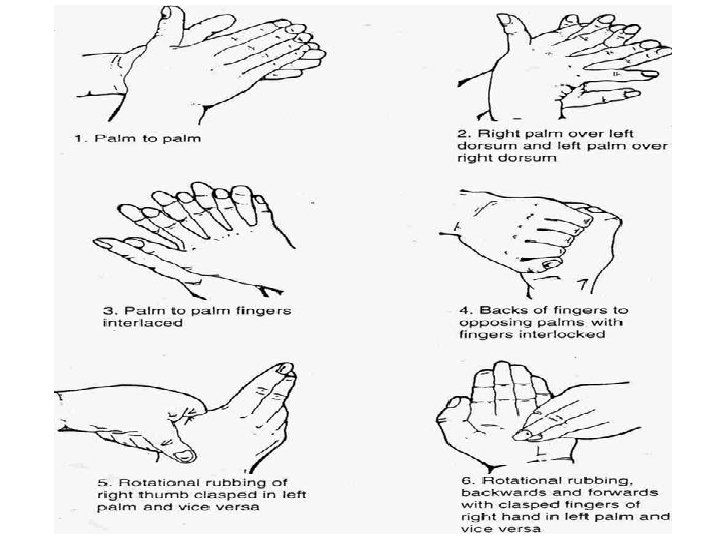
Surgical hand washing • A surgical hand wash is required before any invasive or surgical procedure requiring the use of sterile gloves. • An antimicrobial skin cleanser, – usually containing chlorhexidine or – detergent-based povidone-iodine, is used.
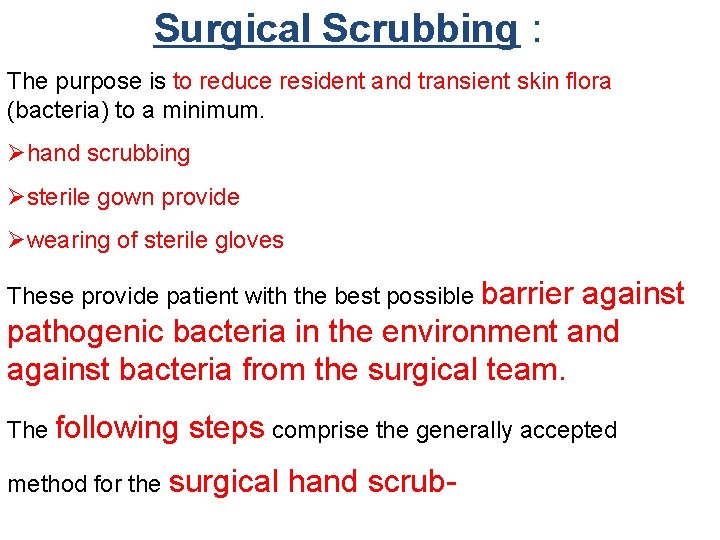
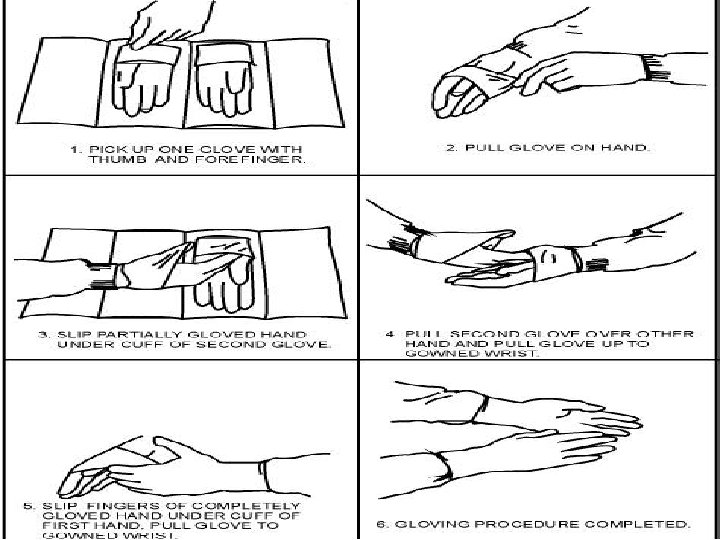
Surgical Scrubbing : The purpose is to reduce resident and transient skin flora (bacteria) to a minimum. Øhand scrubbing Østerile gown provide Øwearing of sterile gloves These provide patient with the best possible barrier against pathogenic bacteria in the environment and against bacteria from the surgical team. The following steps comprise the generally accepted method for the surgical hand scrub-

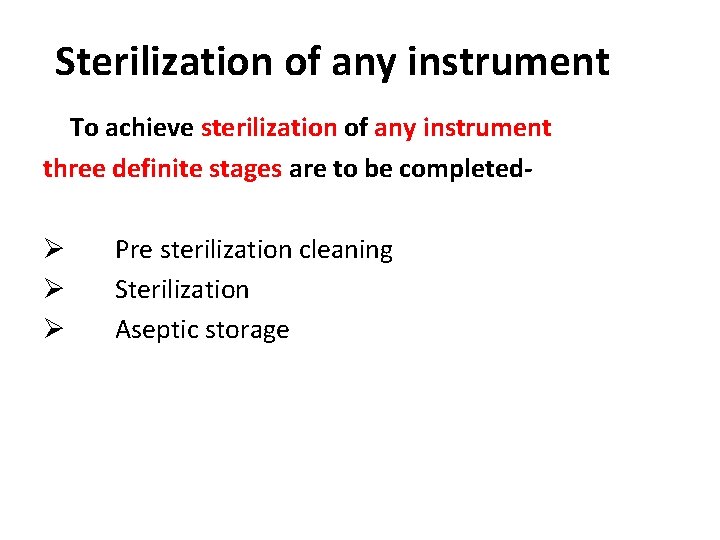
Sterilization of any instrument To achieve sterilization of any instrument three definite stages are to be completed- Ø Ø Ø Pre sterilization cleaning Sterilization Aseptic storage

Presterilization cleaning • • Objective. Removal of the organic matters, blood and saliva which provide protective barrier for microorganisms and prevents its destruction. There are three methods for cleaning 1. 2. 3. -Manual -Ultrasonic -Mechanical washing
MANUAL CLEANING Simplest and the cheapest method, • – – • • time consuming and difficult to achieve. heavy duty gloves and glasses must be worn to protect needle stick injury and to protect eye. Material used for manual cleaning 1. 2. Soaps Detergents

ULTRASONIC CLEANING Principle- conversion of electrical energy into vibratory sound waves which pass through a soap solution containing the instrument. Used mainly for bone files, bone cutter, artery forceps, saw etc.
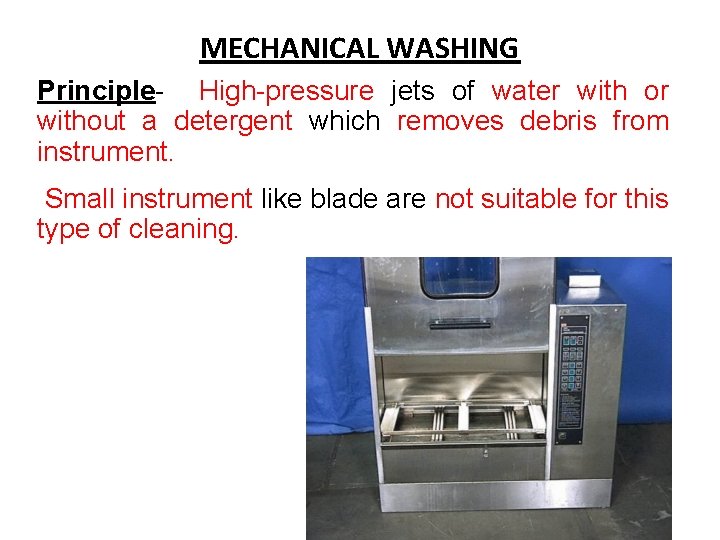
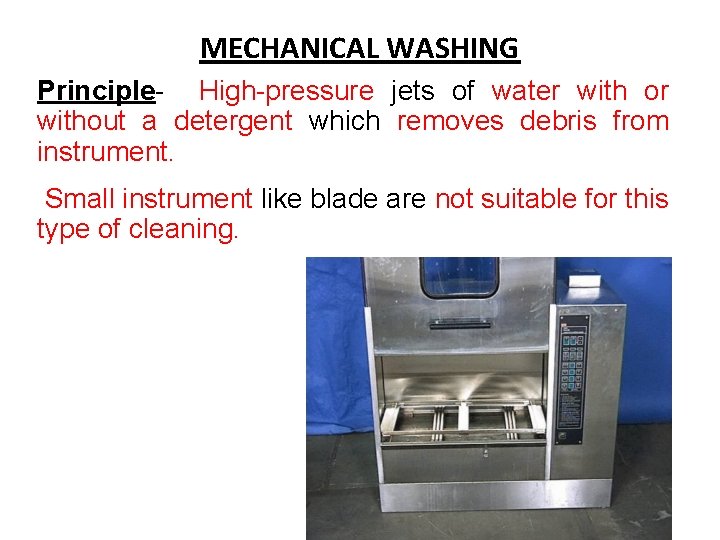
MECHANICAL WASHING Principle- High-pressure jets of water with or without a detergent which removes debris from instrument. Small instrument like blade are not suitable for this type of cleaning.

Sterile Techniques
Sterile Techniques STERILISATION: Ø any process that effectively kills or eliminates transmissible agents (such as fungi, bacteria, viruses, spore forms, etc. ) from a surface, equipment, article of food or medication, or biological culture medium. Ø Sterilization can be achieved through application of heat, chemicals, irradiation, high pressure or filtration.
STERILISATION Types I. CHEMICAL METHODS II. PHYSICAL METHODS A. Heat : 1. Dry heat 2 Moist heat B. Radiations 1. Ultraviolet radiations 2. Ionizing radiations C. Filtration
Chemical sterilization

Chemical sterilization • Sterilization includes both liquid and gas chemicals
Mechanism of action of chemical disinfectants : The mechanism of action of most of the chemicals are nonspecific and complex but most of them effect microorganisms by one of the following mechanisms. 1. Cell membrane injury. 2. Denaturation. 3. Interactions with functional groups of proteins.
1. ALDEHYDE COMPOUNDS a. Formaldehyde: Ø A broad-spectrum antimicrobial agent, used for disinfection, Ø limited sporicidal activity. Ø Hazardous substance, inflammable and irritant to the eye, skin and respiratory tract. b. Glutaraldehyde: Ø It is a high level disinfectant Ø A solution of 2% glutaraldehyde requires Ø 20 minutes for disinfection; Ø 6 to 10 hours of immersion for sterilization.

2. ALCOHOLS Act by denaturing bacterial proteins. Øethanol Ø Solutions of 70% ethanol are more effective than higher concentrations, as the presence
3. IODOPHOR COMPOUNDS Ø iodophor compounds are the most effective antiseptics. ØIodine is complexed with organic surface-active agents, such as, polyvinylpyrrolidone (Betadine, Isodine). ØTheir activity is dependent on the release of iodine from the complex. ØThese compounds are effective against most bacteria, spores, viruses, and fungi. ØThese are the most commonly used surface disinfectants along with hypochlorite.

4. Biguanide : Ø Most commonly used biguanide compound is chlorhexidine. Ø It is a powerful non-irritating antiseptic Ø disrupts bacterial cell membrane. Ø It persists on skin for longer period of time and that is why it is extensively used Ø for surgical scrubbing, Ø neonatal bath, Ø mouth wash and Ø a general skin anti-septic.

Vapors and Gases • formaldehyde, beta-propiolactone and ethylene oxide are not routinely used in laboratory sterilization practices. • These sterilants are used in hospitals and commercial facilities where closed systems controlling temperature, humidity, and concentration are required to achieve sterilization using these agents.
Heat sterilization
Two methods of Heat sterilization 1. Dry Heat sterilization 2. Moist Heat sterilization
Dry Heat sterilization ØDry heat, as the name indicates, Øutilizes hot air that is Øeither free from water vapour, or has very little of it, and Ømoisture plays a minimal or no role in the process of sterilization

Mechanism of killing by dry heat 1. Dry heat kills the organisms by destruction of essential cell constituents 2. Killing of the most resistant spores by dry heat requires a temperature of about 160 °C for 60 minutes 3. Dry heat is employed for glassware; syringes, metal instruments and paper wrapped goods, which are not spoiled by high temperatures. 4. It is also used for anhydrous fats, oils and powders that are impermeable to moisture.
METHODS OF STERILIZATION BY DRY HEAT 1. 2. 3. 4. RED HEAT FLAMING HOT AIR OVEN NON IONIZING RADIATION
1. RED HEAT • Inoculating wires, • points of forceps and spatulas are sterilized by holding them in the flame of Bunsen burner until they are seen to be red-hot.
2. FLAMING • This method is used for sterilizing scalpel, mouth of culture tubes, glass slides etc. It involves passing of an article through Bunsen flame without allowing it to become red-hot.
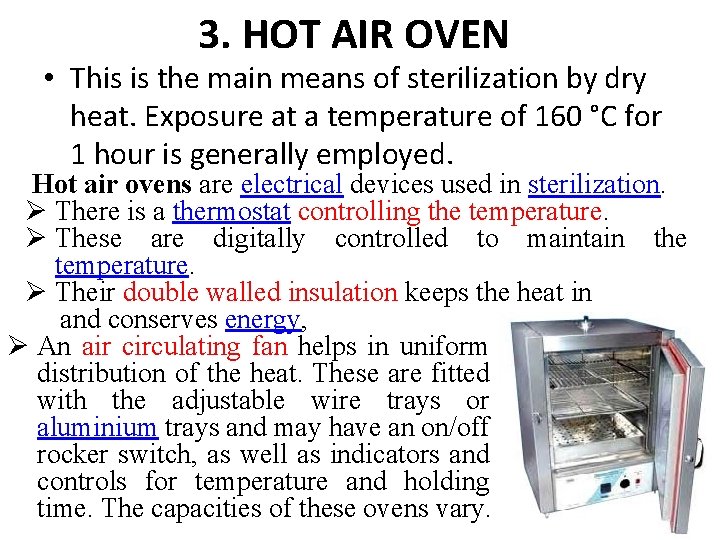
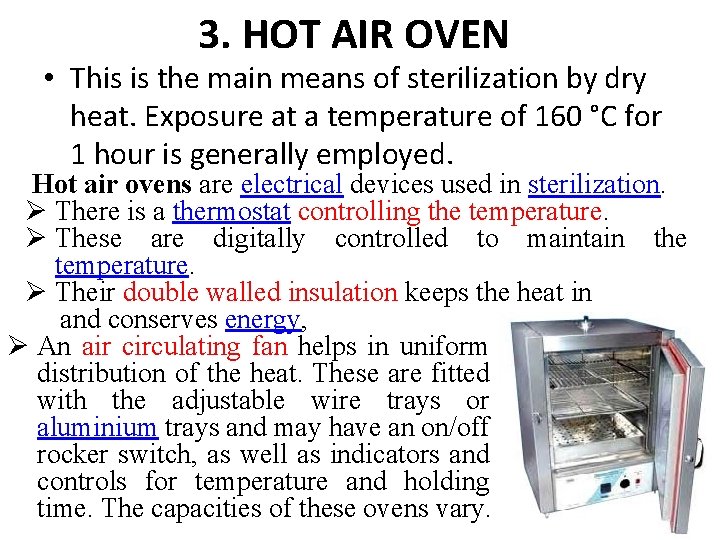
3. HOT AIR OVEN • This is the main means of sterilization by dry heat. Exposure at a temperature of 160 °C for 1 hour is generally employed. Hot air ovens are electrical devices used in sterilization. Ø There is a thermostat controlling the temperature. Ø These are digitally controlled to maintain the temperature. Ø Their double walled insulation keeps the heat in and conserves energy, Ø An air circulating fan helps in uniform distribution of the heat. These are fitted with the adjustable wire trays or aluminium trays and may have an on/off rocker switch, as well as indicators and controls for temperature and holding time. The capacities of these ovens vary.
4. Non ionizing radiation • UV light and infrared • Affect 3 -D structure of proteins and nucleic acid

Moist Heat sterilization
METHODS OF STERILIZATION BY MOIST HEAT Moist heat can be employed at 1. Temperature below 100 °C 2. Temperature of 100 °C 3. Temperature above 100 °C
MOIST HEAT BELOW 100 °C EXAMPLE: Pasteurization of milk In Pasteurization of milk the temperature employed is either Ø 63 °C for 30 minutes or Ø 72 °C for 20 seconds. All nonspore forming pathogens in milk like Salmonellae, M. tuberculosis are killed.
MOIST HEAT ABOVE 100°C Sterilization in an autoclave 1. Autoclaving is the most reliable method. It is the method most widely used for sterilization of culture media and surgical supplies 2. When water is boiled within a closed vessel at an increased pressure, the temperature at which it boils and the steam it forms will rise above 100 °C. This principle is used in the autoclave
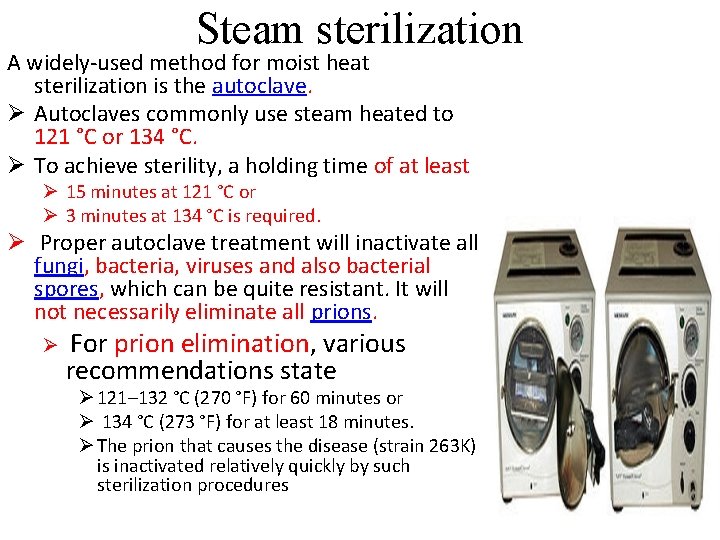
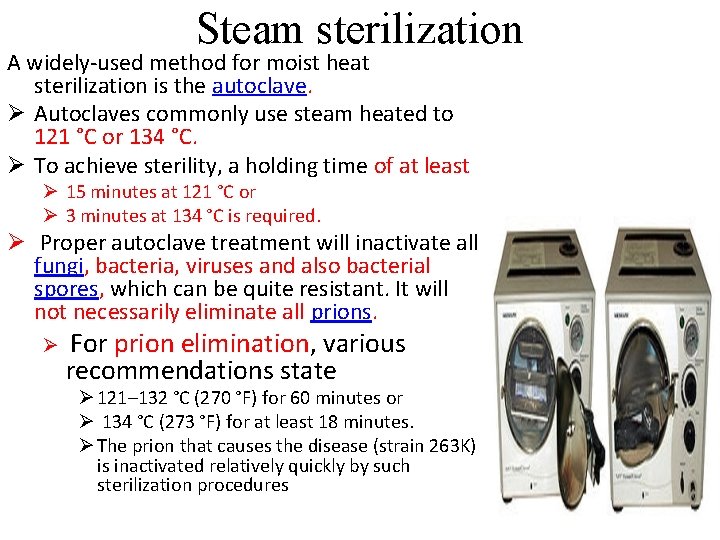
Steam sterilization A widely-used method for moist heat sterilization is the autoclave. Ø Autoclaves commonly use steam heated to 121 °C or 134 °C. Ø To achieve sterility, a holding time of at least Ø 15 minutes at 121 °C or Ø 3 minutes at 134 °C is required. Ø Proper autoclave treatment will inactivate all fungi, bacteria, viruses and also bacterial spores, which can be quite resistant. It will not necessarily eliminate all prions. Ø For prion elimination, various recommendations state Ø 121– 132 °C (270 °F) for 60 minutes or Ø 134 °C (273 °F) for at least 18 minutes. Ø The prion that causes the disease (strain 263 K) is inactivated relatively quickly by such sterilization procedures
Mechanism of killing by moist heat 1. Moist heat kills the organisms by denaturing their enzymes and structural protein. 2. Sterilization by moist heat of the most resistant spores generally requires 121 °C for 15 -30 minutes. 3. Moist heat is used for the sterilization of culture media, and all other materials through which steam can penetrate
FACTORS INFLUENZING STERILIZATION BY HEAT 1. The temperature and time: they are inversely related, shorter time is sufficient at high temperatures. 2. Number of microorganisms and spores: 3. Depends on the species, strains and spore 4. Depends on the nature of material: a high content of organic substances generally tends to protect spores and vegetative organisms against heat. 5. Presence of organic or inorganic disinfectants facilitates killing by heat 6. p. H also plays an important role in the killing of microorganisms
MERITS AND DEMERITS OF HEAT STERILIZATION Advantages of heat sterilization 1. Sterilization is very effective 2. Instruments are standardized to deliver the required effective heat 3. Heat deliver system can be monitored effectively with various controls like pressure gauge, temperature meters etc.
Disadvantages of heat sterilization 1. Steam impermeable materials like fats, oils and powders can not be sterilized by autoclaving. 2. Heat sensitive materials can not be sterilized by heat Examples: 1. Serum can not be sterilized 2. Antibiotics 3. Plastic materials 4. Vaccines 5. Rubbers 3. Presence of organic matters interfere with effective sterilization 4. Dangers of explosion when high pressure is used

STERILIZATION BY FILTRATION
STERILIZATION BY FILTRATION 1. When fluids are passed through bacteria stopping filters, they are made free from bacteria. 2. It is useful for making preparations of soluble products of bacterial growth such as toxins 3. Liquids that would be damaged by heat such as serum and antibiotic solutions can be sterilized by filtration
Aseptic storage The maintenance of sterility during transportation and storage is of utmost importance. • Instruments are kept wrapped until ready for use. • To reduce the risk of contamination, sterile packs must be handled as little as possible. • Sterilized packs should be allowed to cool before storage; otherwise condensation will occur inside the packs. • To prevent contamination from rodents, and cockroaches, the store must be subjected to adequate pest control. • Sterile packs must be stored and issued in correct date order. The packs, preferably, are stored in drums which can be locked.