Spondylolysis repair with impaction grafting and rigid fixation



- Slides: 17
Spondylolysis repair with impaction grafting and rigid fixation: prospective outcome study Matthew D Hepler, MD* Matthew T Walker, MD Eugene Lautenschlager, Ph. D *Vero Orthopaedics and Vero Neurology Departments of Orthopaedic Surgery and Neuroradiology Northwestern Memorial Hospital Chicago, IL mdhepler@hotmail. com
Introduction Spondylolysis is common diagnosis (6%) Chronic lesions l l l alter lumbar biomechanics progress to spondylolysthesis or DDD cause back pain and disability Surgical treatment l l Pars repair high failure rate fusion sacrifices motion no consensus
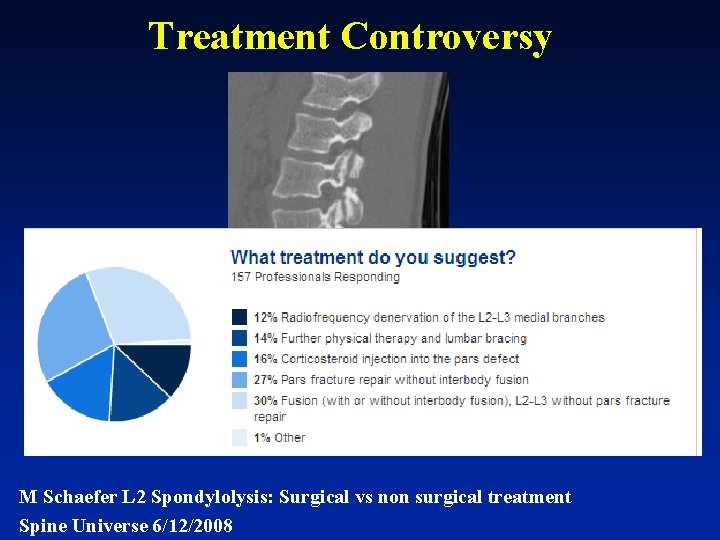
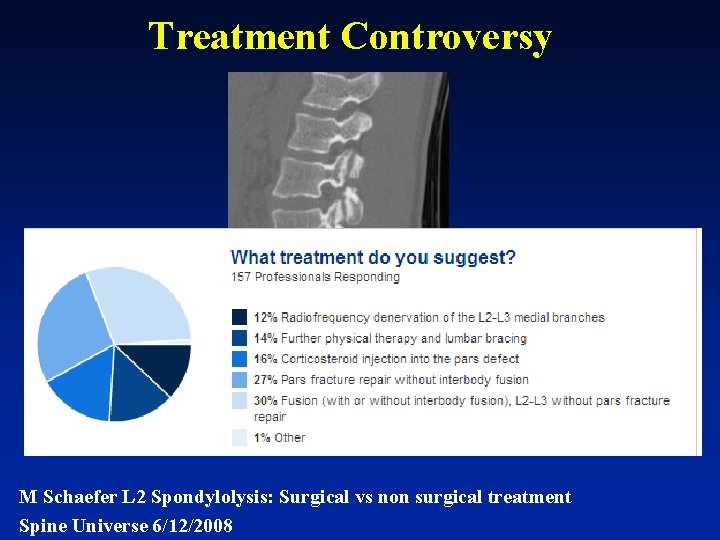
Treatment Controversy M Schaefer L 2 Spondylolysis: Surgical vs non surgical treatment Spine Universe 6/12/2008
Purpose l Prospective evaluation of clinical and radiologic outcomes of spondylolysis treated with fracture debridement, impaction grafting, and rigid fixation.
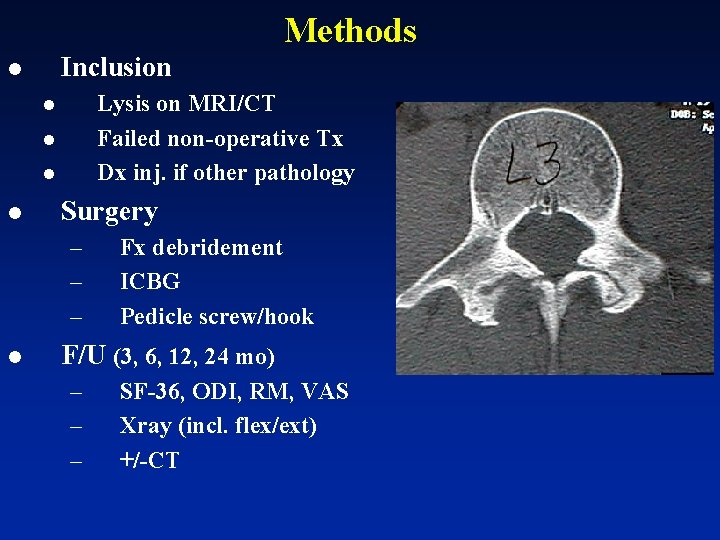
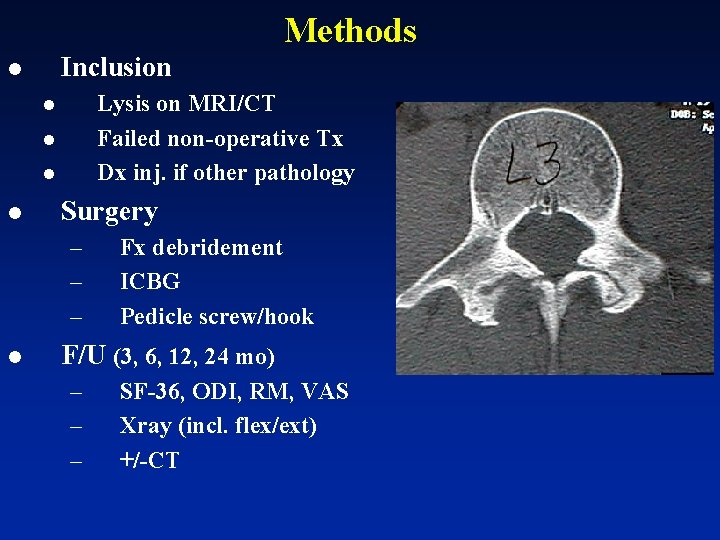
Methods Inclusion l Lysis on MRI/CT Failed non-operative Tx Dx inj. if other pathology l l Surgery – – – l Fx debridement ICBG Pedicle screw/hook F/U (3, 6, 12, 24 mo) – – – SF-36, ODI, RM, VAS Xray (incl. flex/ext) +/-CT
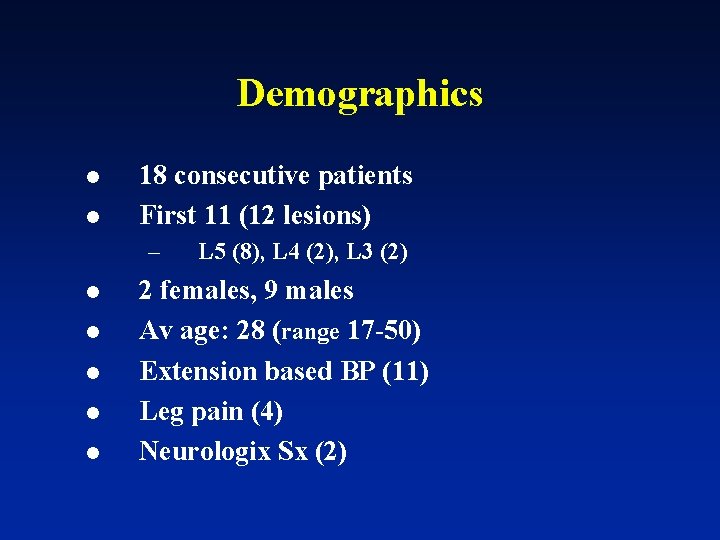
Demographics l l 18 consecutive patients First 11 (12 lesions) – l l l L 5 (8), L 4 (2), L 3 (2) 2 females, 9 males Av age: 28 (range 17 -50) Extension based BP (11) Leg pain (4) Neurologix Sx (2)
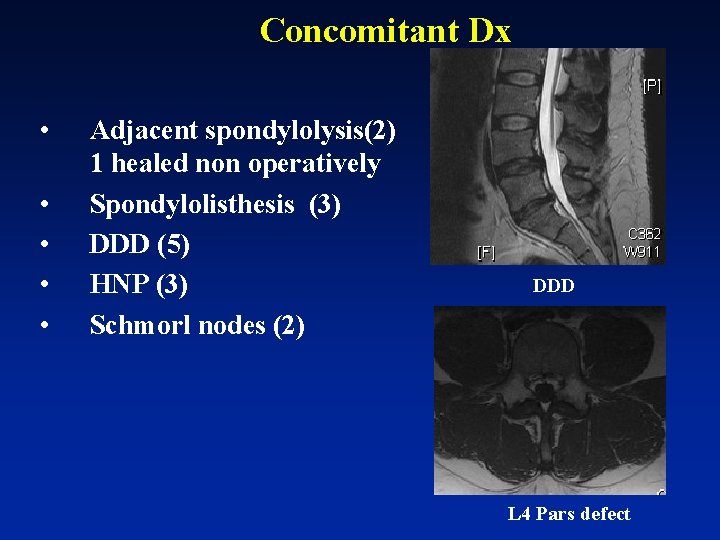
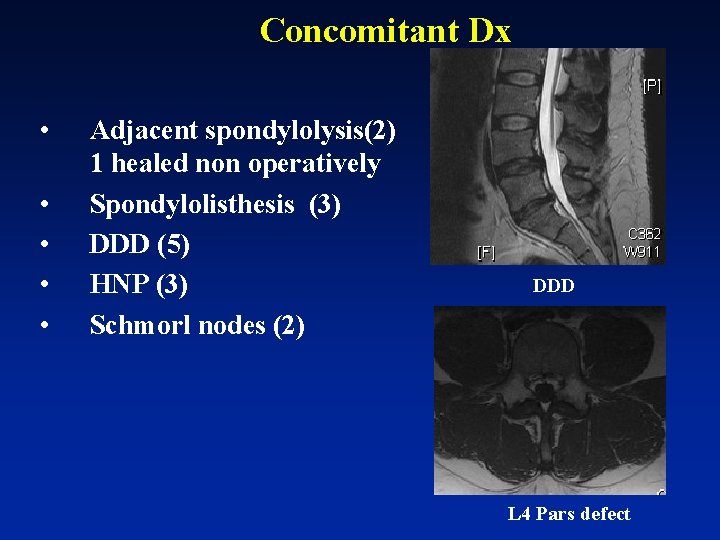
Concomitant Dx • • • Adjacent spondylolysis(2) 1 healed non operatively Spondylolisthesis (3) DDD (5) HNP (3) Schmorl nodes (2) DDD L 4 Pars defect
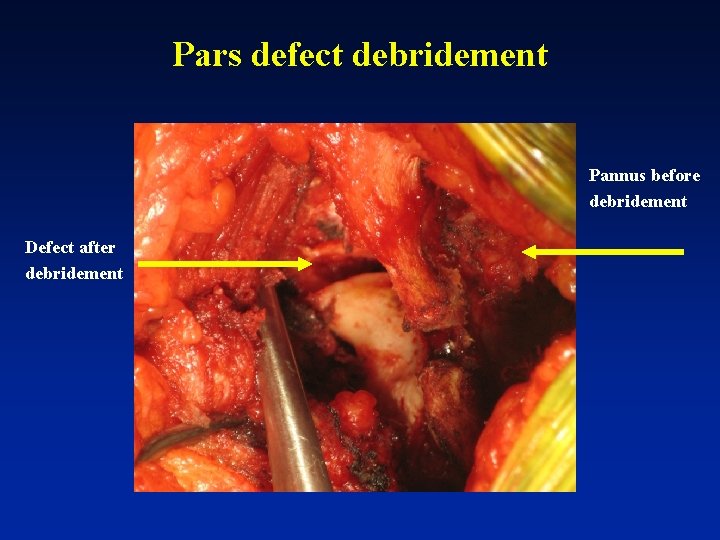
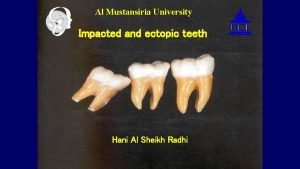
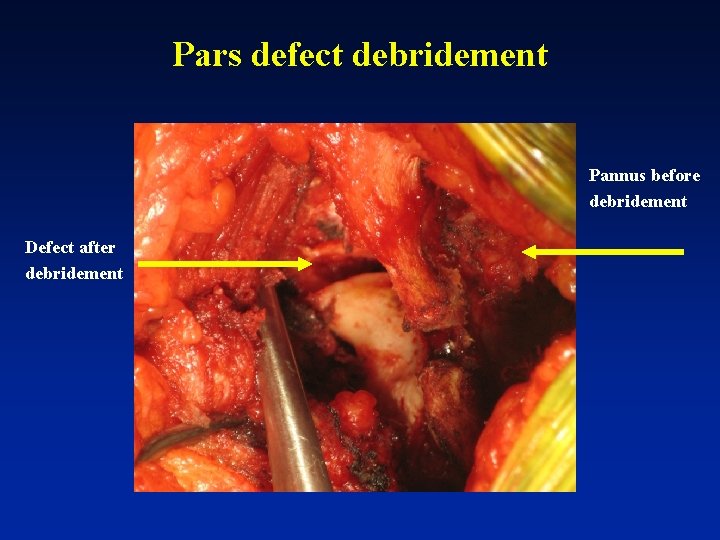
Pars defect debridement Pannus before debridement Defect after debridement
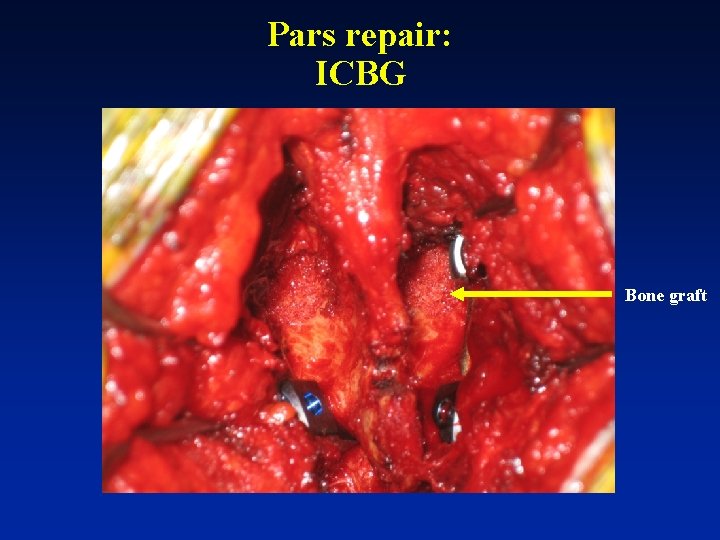
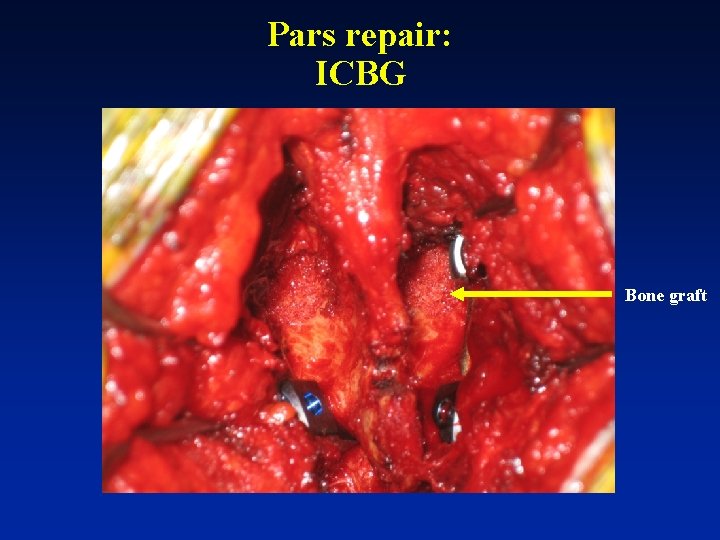
Pars repair: ICBG Bone graft
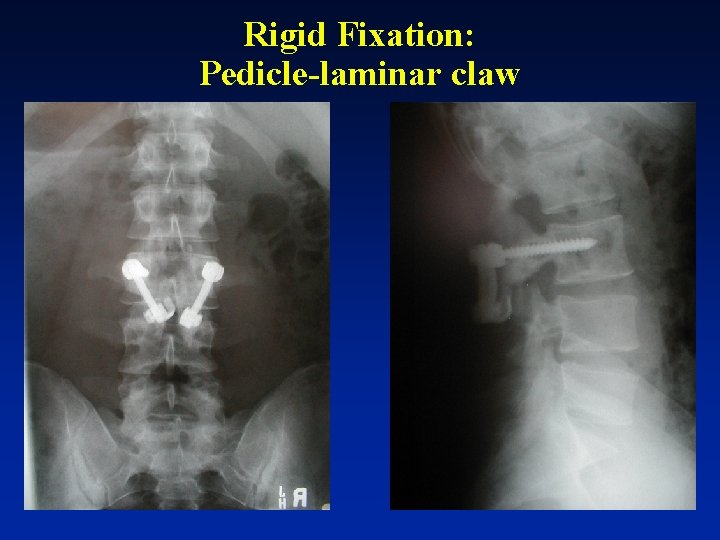
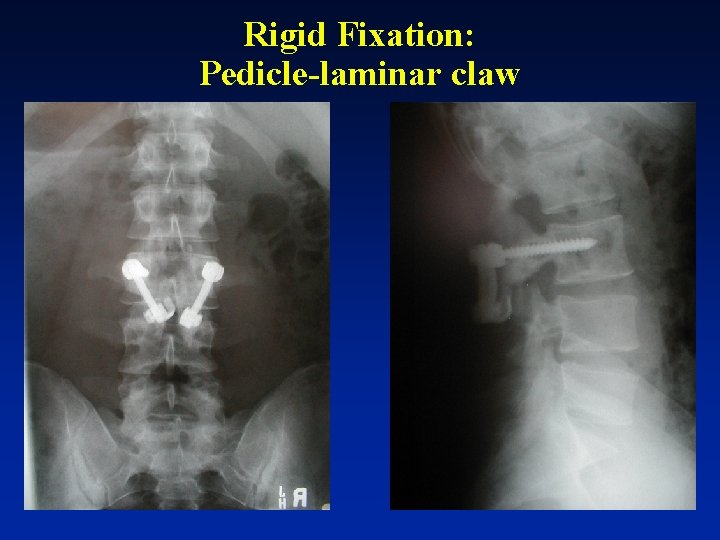
Rigid Fixation: Pedicle-laminar claw
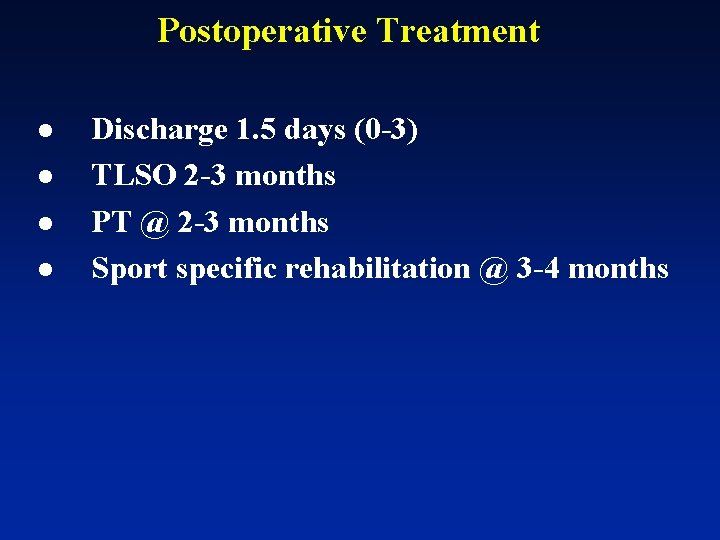
Postoperative Treatment l l Discharge 1. 5 days (0 -3) TLSO 2 -3 months PT @ 2 -3 months Sport specific rehabilitation @ 3 -4 months

Clinical Follow-up l l No infections No revision surgery All patients returned to unrestricted activities @ 6 months 1 fusion for DDD @ 3 yr f/u
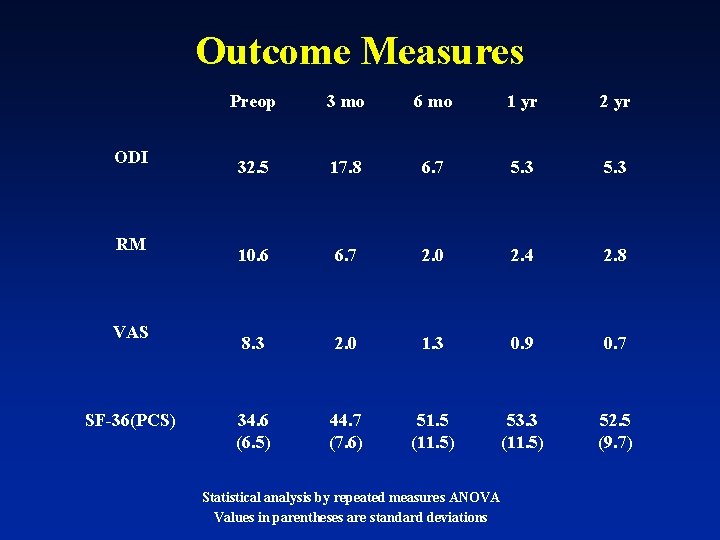
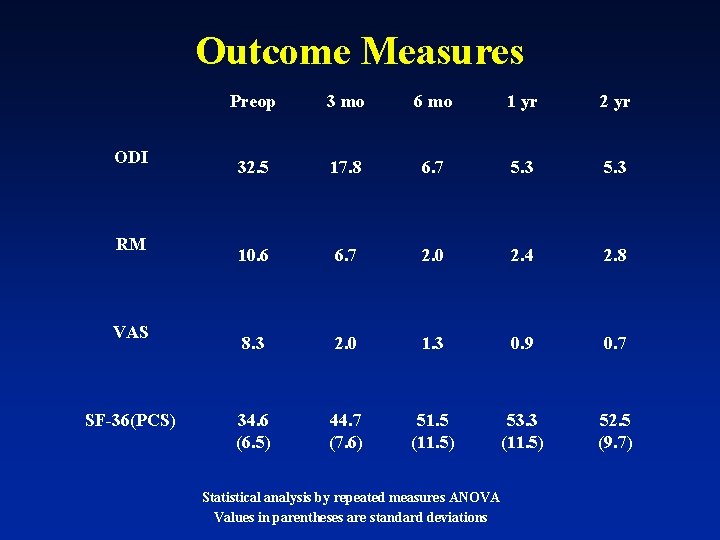
Outcome Measures Preop 3 mo 6 mo 1 yr 2 yr 32. 5 17. 8 6. 7 5. 3 RM 10. 6 6. 7 2. 0 2. 4 2. 8 VAS 8. 3 2. 0 1. 3 0. 9 0. 7 34. 6 (6. 5) 44. 7 (7. 6) 51. 5 (11. 5) 53. 3 (11. 5) 52. 5 (9. 7) ODI SF-36(PCS) Statistical analysis by repeated measures ANOVA Values in parentheses are standard deviations

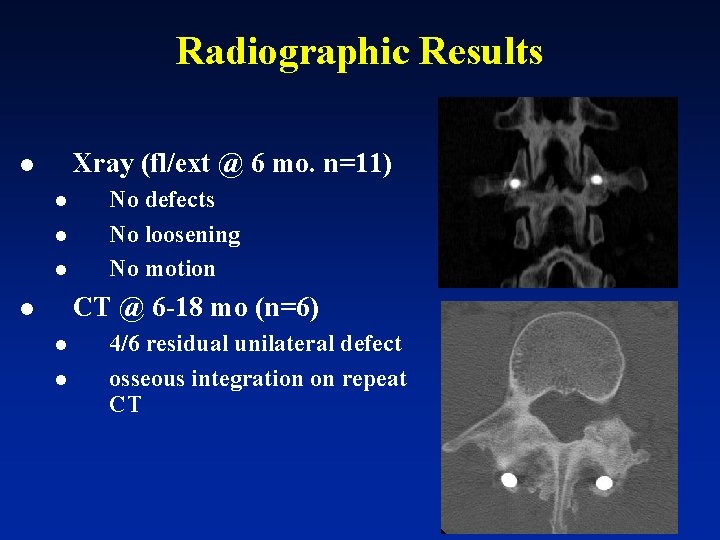
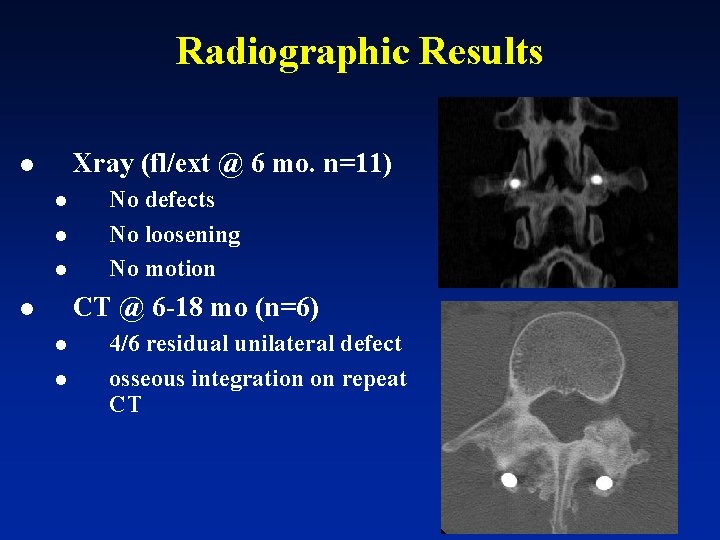
Radiographic Results Xray (fl/ext @ 6 mo. n=11) l l No defects No loosening No motion CT @ 6 -18 mo (n=6) l l l 4/6 residual unilateral defect osseous integration on repeat CT
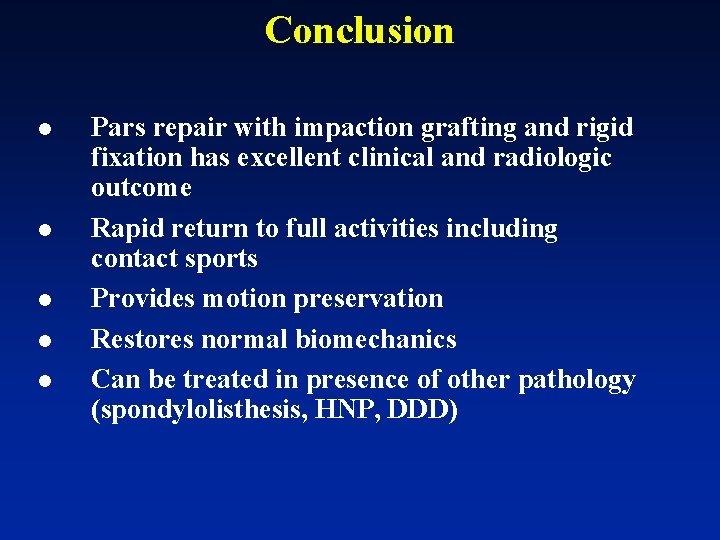
Conclusion l l l Pars repair with impaction grafting and rigid fixation has excellent clinical and radiologic outcome Rapid return to full activities including contact sports Provides motion preservation Restores normal biomechanics Can be treated in presence of other pathology (spondylolisthesis, HNP, DDD)

 Fiksasi eksternal fraktur
Fiksasi eksternal fraktur M
M Vasculáris
Vasculáris Gerinc ct
Gerinc ct Overflow dams
Overflow dams Irrational exponential function
Irrational exponential function Nucleotide excision repair
Nucleotide excision repair Rec a
Rec a Inertial impaction
Inertial impaction Inertial impaction
Inertial impaction Inertial impaction
Inertial impaction Csu impaction matrix
Csu impaction matrix Distoangular impaction
Distoangular impaction Impacted colon pictures
Impacted colon pictures Laxative effect
Laxative effect Impaction mucoide
Impaction mucoide Rigid vs non rigid transformations
Rigid vs non rigid transformations What is grafting
What is grafting