SEIZURES Dr Zolfaghari Assistant Professor of Emergency Medicine







- Slides: 44

SEIZURES Dr. Zolfaghari Assistant Professor of Emergency Medicine Dr. Farahmand Rad Assistant Professor of Emergency Medicine
DEFINITIONS � Seizure: episode of abnormal neurologic function caused by inappropriate electrical discharge of brain neurons. � Epilepsy: clinical condition in which an individual is subject to recurrent seizures.
GENERALIZED SEIZURES Caused by a nearly simultaneous activation of the entire cerebral cortex
PARTIAL SEIZURES Due to electrical discharges in a localized structural lesion of the brain. Affects whatever physical or mental activity that area controls.
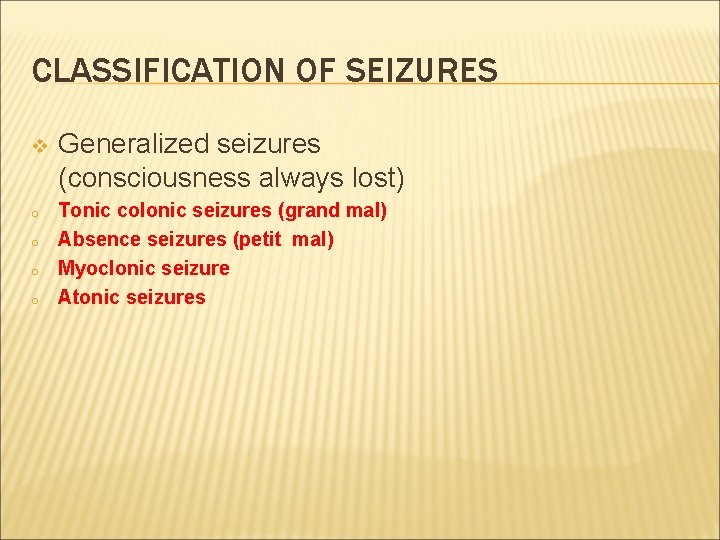
CLASSIFICATION OF SEIZURES v o o Generalized seizures (consciousness always lost) Tonic colonic seizures (grand mal) Absence seizures (petit mal) Myoclonic seizure Atonic seizures
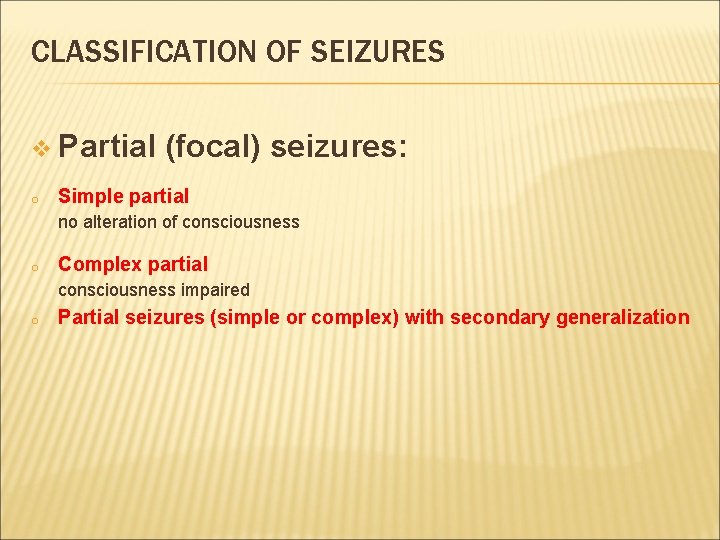
CLASSIFICATION OF SEIZURES v Partial o (focal) seizures: Simple partial no alteration of consciousness o Complex partial consciousness impaired o Partial seizures (simple or complex) with secondary generalization
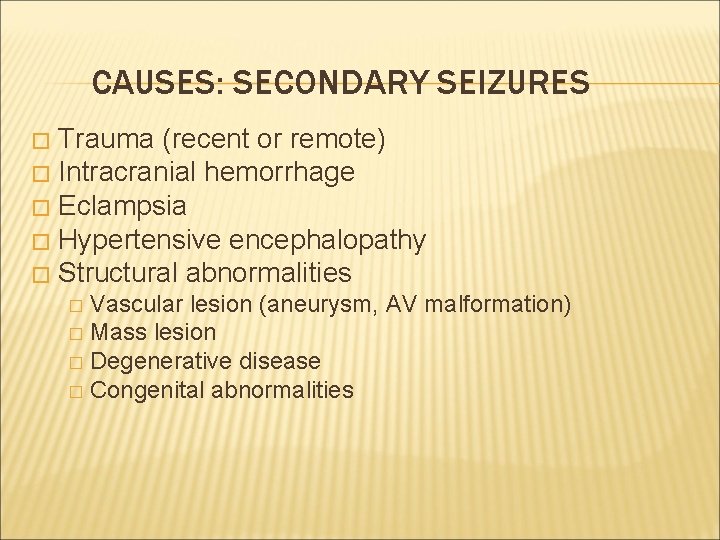
CAUSES: SECONDARY SEIZURES Trauma (recent or remote) � Intracranial hemorrhage � Eclampsia � Hypertensive encephalopathy � Structural abnormalities � Vascular lesion (aneurysm, AV malformation) � Mass lesion � Degenerative disease � Congenital abnormalities �
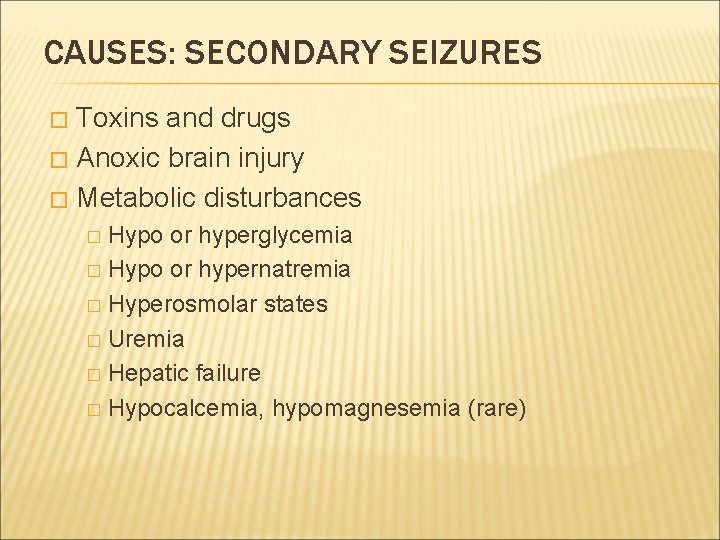
CAUSES: SECONDARY SEIZURES Toxins and drugs � Anoxic brain injury � Metabolic disturbances � Hypo or hyperglycemia � Hypo or hypernatremia � Hyperosmolar states � Uremia � Hepatic failure � Hypocalcemia, hypomagnesemia (rare) �

FEATURES: GENERALIZED SEIZURES � Abrupt loss of consciousness and loss of postural tone � May then become rigid � With extension of the trunk and extremities � Apnea � Cyanosis � Urinary incontinence
FEATURES: TONIC CLONIC SEIZURES � As the tonic (rigid) phase subsides, clonic (symmetric rhythmic) jerking of the trunk and extremities develop � Episode lasts from 60 -90 seconds � Consciousness returns gradually � Postictal confusion may persist for several hours
STATUS EPILEPTICUS � Continuous seizure activity lasting for at least 5 min � Two or more seizures without intervening return to baseline � Non-convulsive status epilepticus is associated with minimal or imperceptible convulsive activity and is confirmed by EEG
HISTORY � Careful history � Important historical information: �Include rapidity of onset, �Presence of a preceding aura �Progression of motor activity (local or generalized) �Incontinence.

HISTORY � Duration of the episode and whethere was postictal confusion � Contributing factors: � Sleep deprivation � Alcohol withdrawal � Infection � Use or cessation of other drugs
HISTORY: FIRST TIME SEIZURES � History of head trauma � Headache � Pregnancy or recent delivery � History of metabolic derangements or hypoxia � Systemic ingestion or withdrawal and alcohol use.
PHYSICAL EXAM: � Injuries resulting from the seizure � � such as fractures, sprains, posterior shoulder dislocation, tongue lacerations, and aspiration. Localized neurological deficits � Todd’s paralysis
DIFFERENTIAL DIAGNOSIS � Syncope � Hyperventilation syndrome � Complex migraine � Movement disorders � Narcolepsy � Pseudo-seizures
TREATMENT: 1) Airway: � Oxygen � Pulse oximetry � Endotracheal intubation � for � If prolonged seizure RSI is performed, a short acting paralytic agent should be used so that ongoing seizure activity can be observed
TREATMENT: 2) Breathing: � Suction � Airway adjuncts 3) Circulation: IV access � IV glucose if confirmed hypoglycemia
STATUS EPILEPTICUS Continuous seizure activity lasting for at least 5 min, or two or more seizures without intervening return to baseline � Continuous seizure activity for >5 min should be treated (most seizures last 1 -2 min) � Impending SE if >3 tonic - colonic seizures within 24 hrs generalized or partial �
STATUS EPILEPTICUS � The longer the seizure continues � The more difficult it is to stop � The more likely permanent CNS injury will occur
TREATMENT � Protect airway (NPA, OPA, ETT). If RSI is required, use short acting paralytics. � Obtain IV access � Blood glucose � Cardiac monitoring



FEBRILE SEIZURES � Antiepileptic drug therapy are only used in pts with: � Underlying neuro deficit (ie CP) � Complex febrile seizure � Repeated seizure in the same febrile illness � Onset under 6 mos of age or more than 3 febrile seizures in 6 mos.
FEBRILE SEIZURES: � Aged 6 month to 5 years � Identify and treat cause � Acetaminophen, ibuprofen and tepid water baths. � Family history increases risk.
ECLAMPSIA � Pregnant women beyond 20 weeks’ gestation or up to 8 weeks postpartum. � Seizures � Hypertension � Edema � Proteinuria
ECLAMPSIA: � Treatment: administration of magnesium sulfate 4 g IV � Followed by 1 -2 mg/ hr, in addition to antiepileptic meds
EPILEPSY � Breakthrough seizures vs. noncompliance with medications � Precipitating factors � Infection � Drug � Treat use or stabilize any injuries secondary to convulsions
EPILEPSY: MANAGEMENT � ABC’s � Monitor VS and check blood glucose � Treat any injuries � Transport to appropriate hospital � IV and monitoring
NO LONGER SEIZING: Recovery position � IV � Blood glucose � Medication history �
IS SEIZING STILL Airway assessment (PA, suction) � Protect patient from self injury � Pulse-ox, monitor, IV access, blood glucose � Hypoglycemia is the most common metabolic but can also be a result of prolonged seizure � Medications �
DELERIUM TREMENS (DT’S) �Advanced stage of alcohol withdrawal �Altered mental status �Generalized seizures � 6 -48 hours after the last drink. �Status epilepticus
DELERIUM TREMENS (DT’S) Tremors Irritability Insomnia Nausea/vomiting Hallucinations (auditory, visual, or olfactory) Confusion Delusions Severe agitation
TREATMENT: � Airway � Suction � high risk for aspiration � oxygen � IV access � Immediate glucose testing or D 50 administration � thiamine administration (100 mg IV) � benzodiazepines in actively seizing pts.
TREATMENT OF DT’S: � Do not use neuroleptics � Administer adequate sedation � To blunt agitation to and prevent the exacerbation of hyperthermia, acidosis, and rhabdomyolysis.
DELIRIUM TREMENS: � Potentially fatal form of ethanol withdrawal. � Symptoms may begin a few hours after the cessation of ethanol, but may not peak until 48 -72 hours. � Early recognition and therapy are necessary to prevent significant morbidity and death.
CASE 1: � 14 month old healthy female with cough and nasal congestion x 2 days, with tactile temperature and 30 second episode of “shaking”? � PE? � Dx? � Treatment?
CASE 2 � 19 year old healthy female breast feeding a newborn has a tonic-clonic seizure � PE? � Dx? � treatment?
CASE 3: � 50 year old male with tonic-clonic seizure lasting 2 minutes. Pt is on tegretol. � PE? � Dx? � Treatment?
CASE 4: � 34 yo male with hx of alcoholism found s/p seizure. � Pt is confused and combative. � Vomiting.
CASE 5: � 22 yo female with 2 episodes of “shaking” in last 6 hours with active seizing for 15 minutes. � PE? � Dx? � Treatment?

Questions? ?
 Hamid zolfaghari
Hamid zolfaghari Cuhk assistant professor salary
Cuhk assistant professor salary Promotion from assistant to associate professor
Promotion from assistant to associate professor Zomisamide
Zomisamide Seizures and tremors
Seizures and tremors What is a seizure
What is a seizure Subclinical seizures eeg
Subclinical seizures eeg Non epileptic seizure
Non epileptic seizure Seizure
Seizure Shaking vs seizure
Shaking vs seizure Basic mechanisms underlying seizures and epilepsy
Basic mechanisms underlying seizures and epilepsy Nursing diagnosis of meningitis slideshare
Nursing diagnosis of meningitis slideshare Pediatric seizures
Pediatric seizures Nikki mehta
Nikki mehta Psychomotor seizures
Psychomotor seizures Seizures
Seizures Lorna myers pnes
Lorna myers pnes Simple partial seizures vs complex
Simple partial seizures vs complex Psychomotor seizures
Psychomotor seizures Dutch north sea emergency medicine conference
Dutch north sea emergency medicine conference Unm im residency
Unm im residency Cmc vellore emergency medicine
Cmc vellore emergency medicine University of arizona emergency medicine
University of arizona emergency medicine Emergency medicine case presentation
Emergency medicine case presentation Leishmanioma
Leishmanioma Danfoss link home assistant
Danfoss link home assistant At the clothes shop dialogue
At the clothes shop dialogue 5 rights of delegation nursing examples
5 rights of delegation nursing examples Patient safety assistant
Patient safety assistant Attribute assistant arcmap
Attribute assistant arcmap The signmaker's assistant main idea
The signmaker's assistant main idea Hacheur assistant
Hacheur assistant Varicocele grading radiology assistant
Varicocele grading radiology assistant Vms4200
Vms4200 University of new england physician assistant program
University of new england physician assistant program Bakersfield adult school
Bakersfield adult school Isentropic efficiency of pump
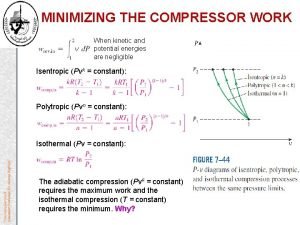
Isentropic efficiency of pump Physician assistant kindergeneeskunde
Physician assistant kindergeneeskunde Student loginusernamepassword
Student loginusernamepassword As a laboratory assistant you measure chemicals
As a laboratory assistant you measure chemicals Arbitre assistant robot
Arbitre assistant robot Mon assistant visuel sncf
Mon assistant visuel sncf Assistant manager career path
Assistant manager career path Good afternoon dear students
Good afternoon dear students Assistant principal portfolio
Assistant principal portfolio