Screen discovered nodules What next 18 th Annual



- Slides: 28
Screen discovered nodules: What next? 18 th Annual Perspectives in Thoracic Oncology Anil Vachani, MD, MS Assistant Professor of Medicine Director, Lung Nodule Program University of Pennsylvania Medical Center
Disclosures • Research Funding – NIH, DOD – Integrated Diagnostics, Allegro Diagnostics, • Scientific Advisory Board – Allegro Diagnostics
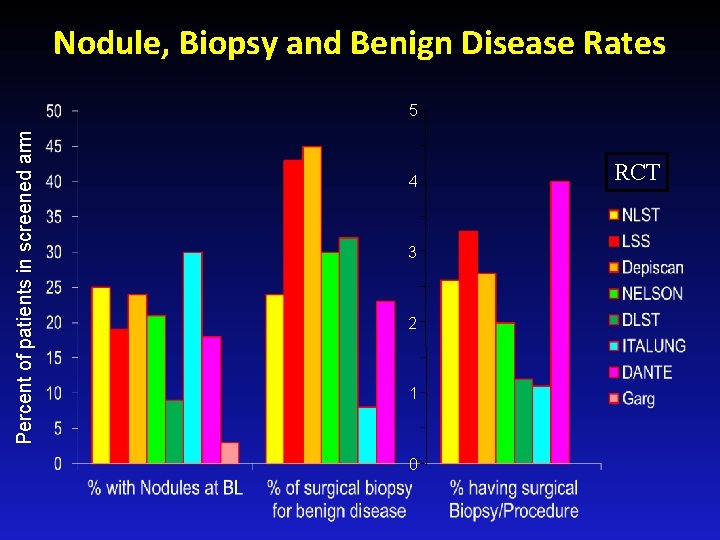
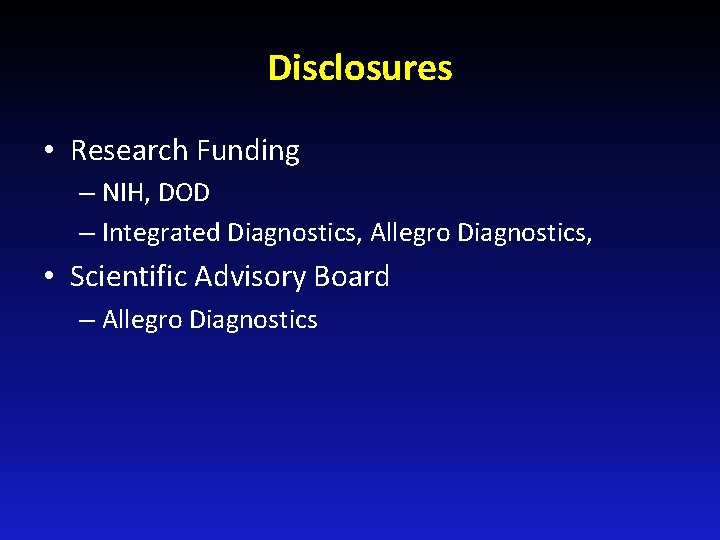
Nodule, Biopsy and Benign Disease Rates Percent of patients in screened arm 5 4 3 2 1 0 RCT
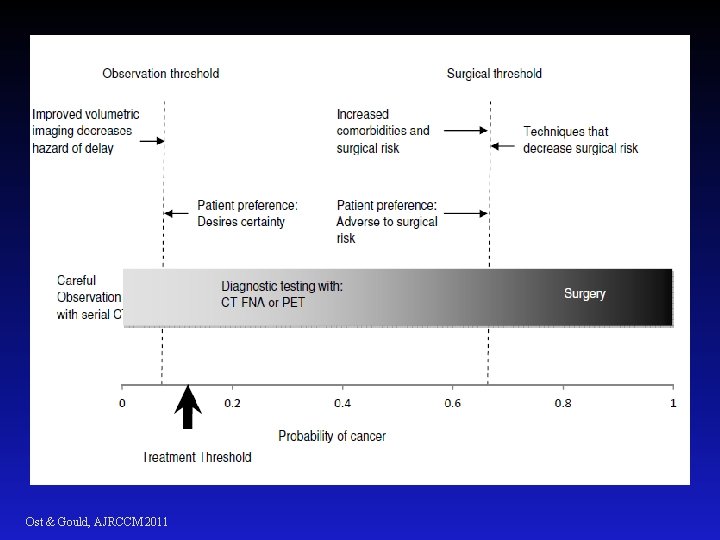
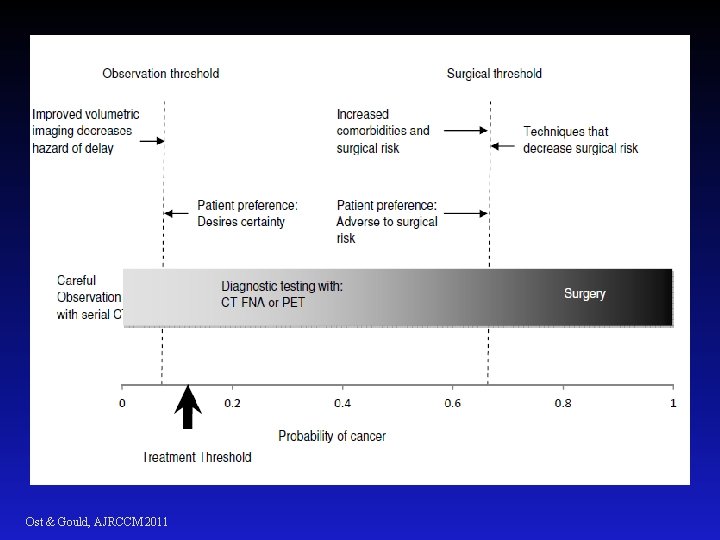
Ost & Gould, AJRCCM 2011
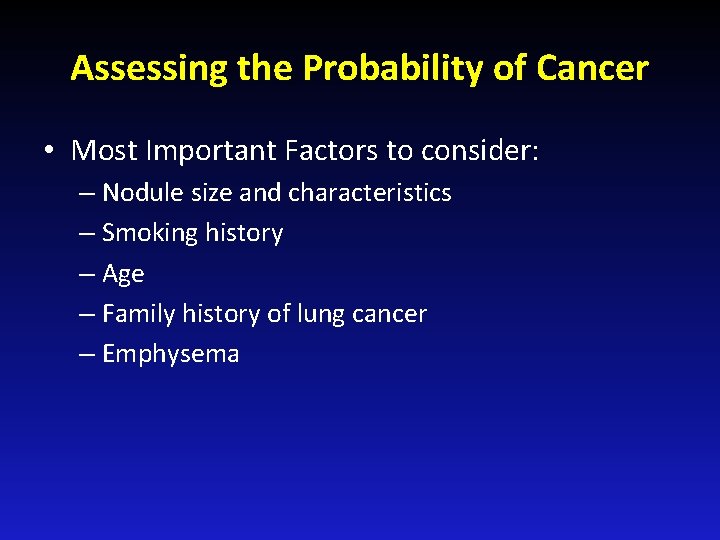
Assessing the Probability of Cancer • Most Important Factors to consider: – Nodule size and characteristics – Smoking history – Age – Family history of lung cancer – Emphysema
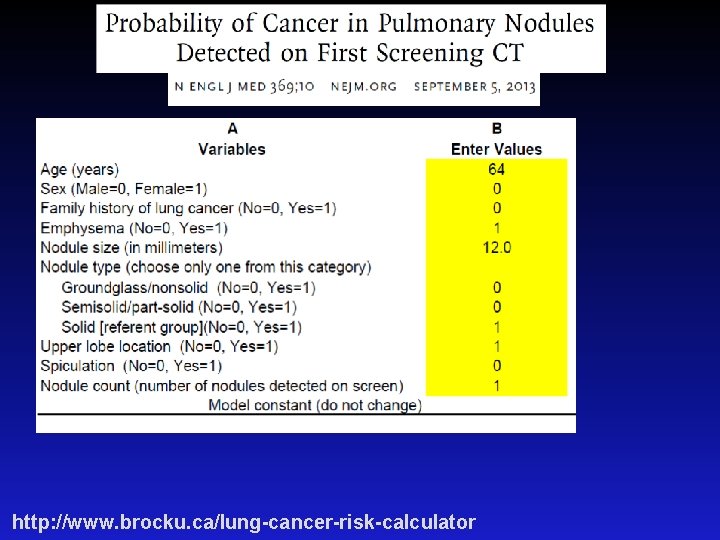
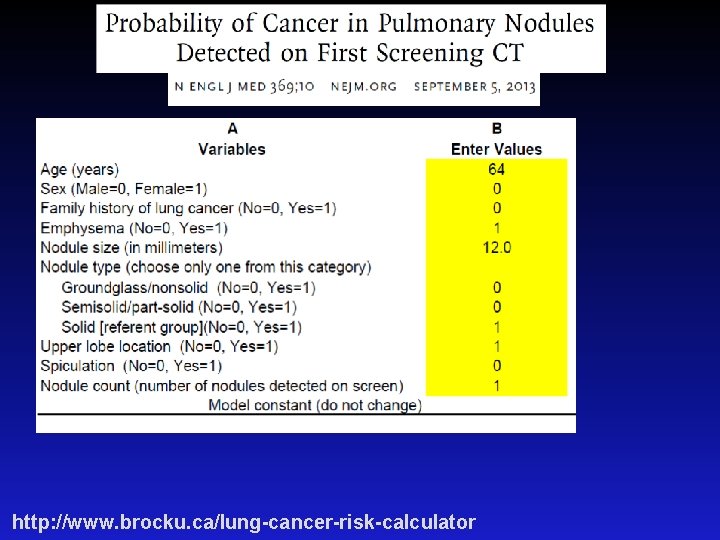
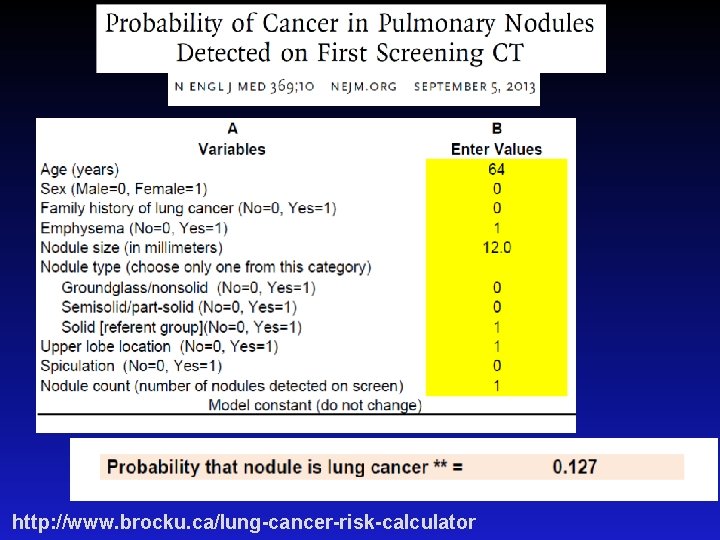
http: //www. brocku. ca/lung-cancer-risk-calculator
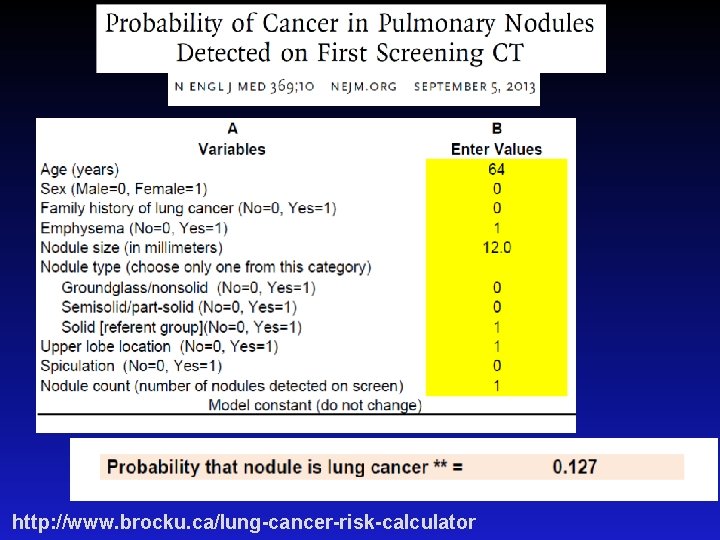
http: //www. brocku. ca/lung-cancer-risk-calculator
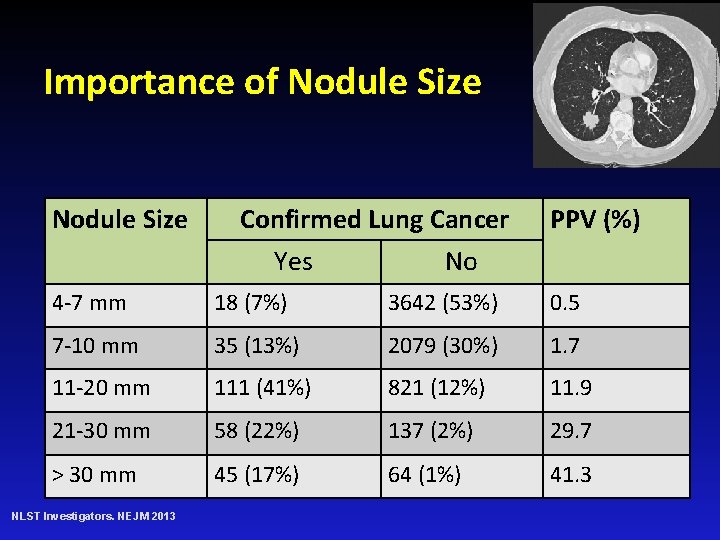
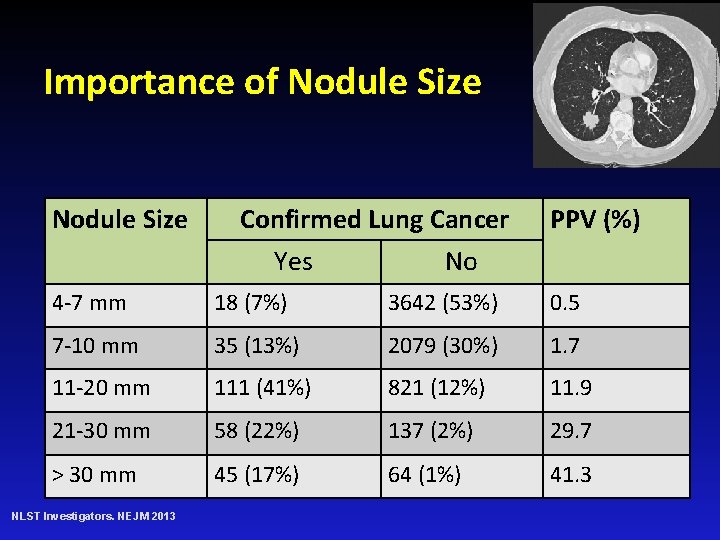
Importance of Nodule Size Confirmed Lung Cancer Yes No PPV (%) 4 -7 mm 18 (7%) 3642 (53%) 0. 5 7 -10 mm 35 (13%) 2079 (30%) 1. 7 11 -20 mm 111 (41%) 821 (12%) 11. 9 21 -30 mm 58 (22%) 137 (2%) 29. 7 > 30 mm 45 (17%) 64 (1%) 41. 3 NLST Investigators. NEJM 2013
Guidelines
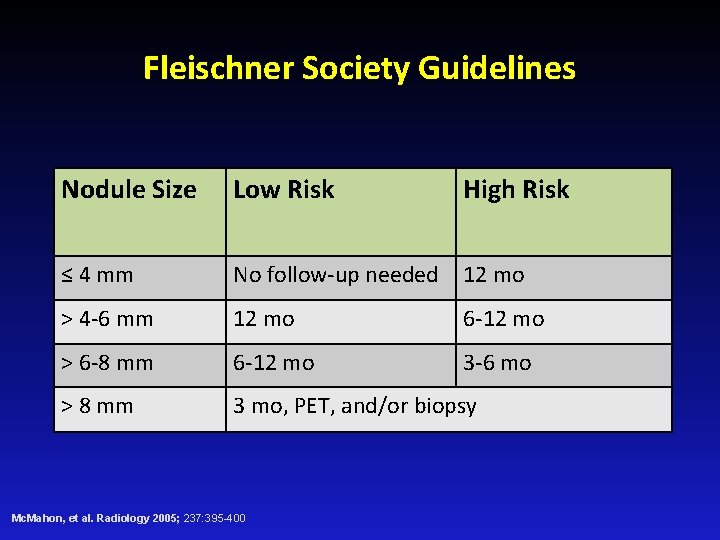
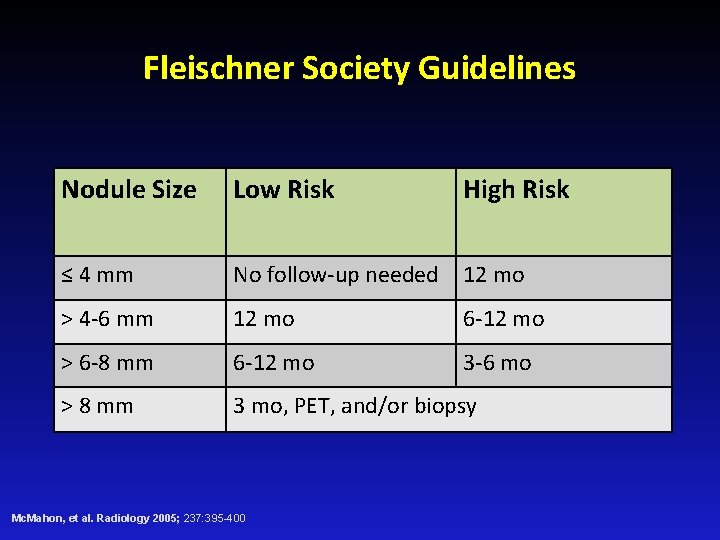
Fleischner Society Guidelines Nodule Size Low Risk High Risk ≤ 4 mm No follow-up needed 12 mo > 4 -6 mm 12 mo 6 -12 mo > 6 -8 mm 6 -12 mo 3 -6 mo > 8 mm 3 mo, PET, and/or biopsy Mc. Mahon, et al. Radiology 2005; 237: 395 -400

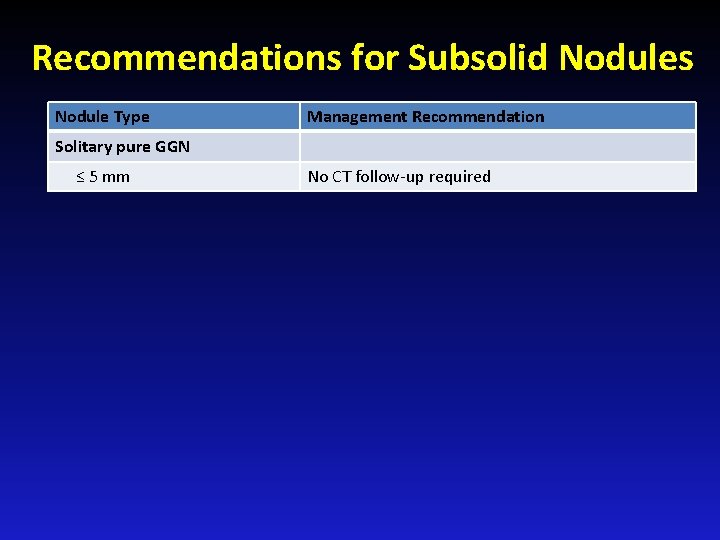
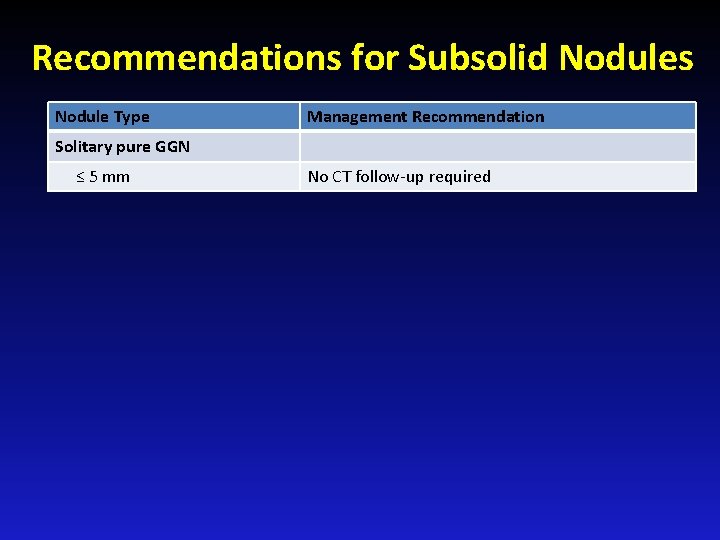
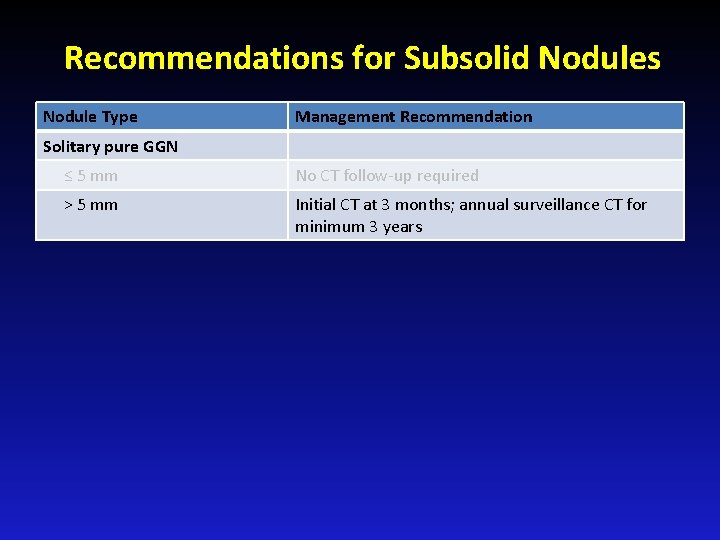
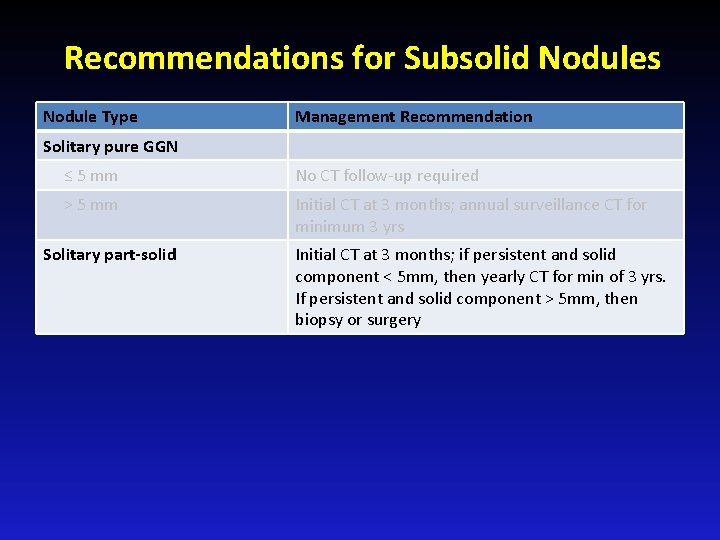
Recommendations for Subsolid Nodules Nodule Type Management Recommendation Solitary pure GGN ≤ 5 mm No CT follow-up required
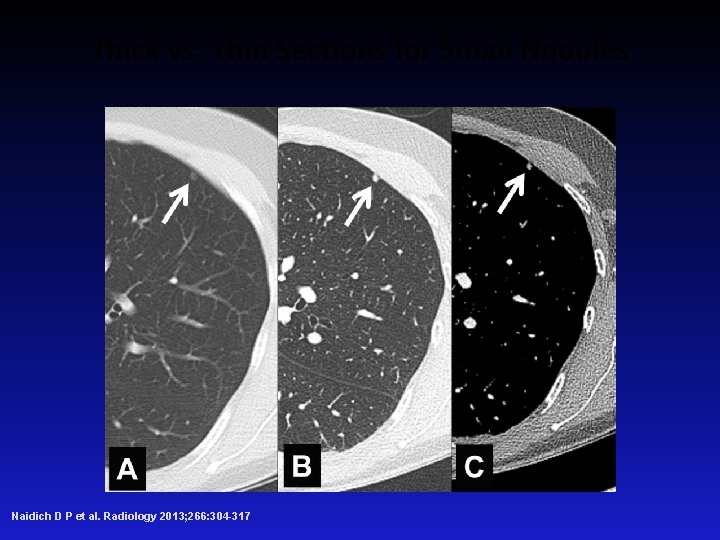
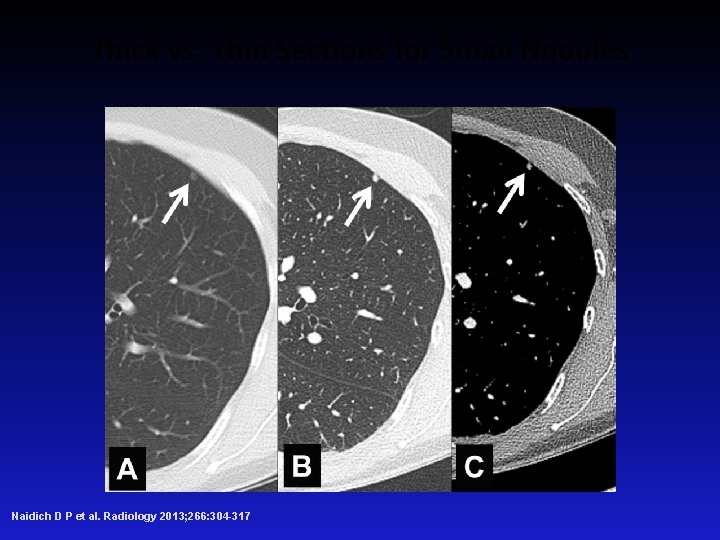
Thick vs. Thin Sections for Small Nodules Naidich D P et al. Radiology 2013; 266: 304 -317
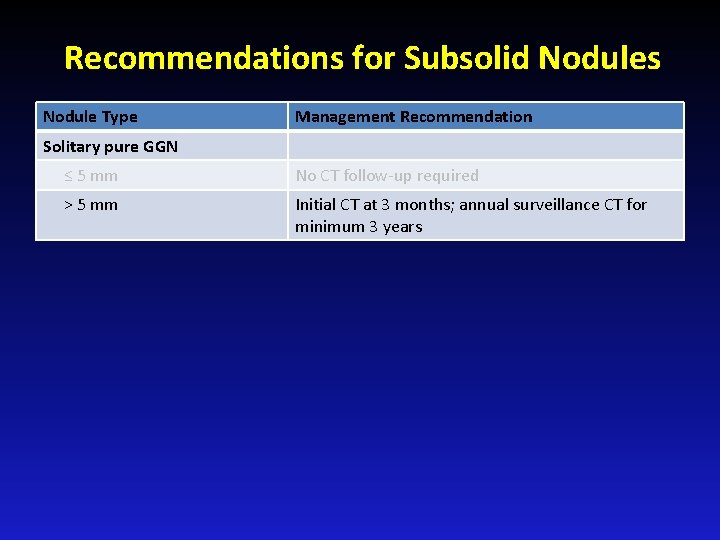
Recommendations for Subsolid Nodules Nodule Type Management Recommendation Solitary pure GGN ≤ 5 mm No CT follow-up required > 5 mm Initial CT at 3 months; annual surveillance CT for minimum 3 years
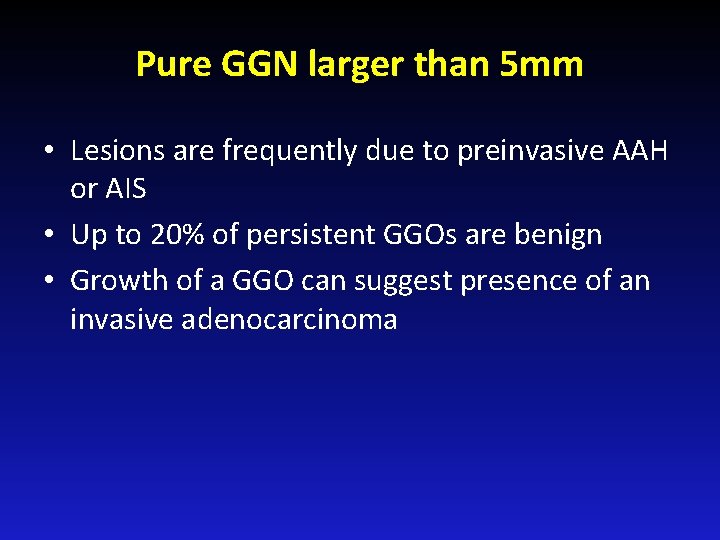
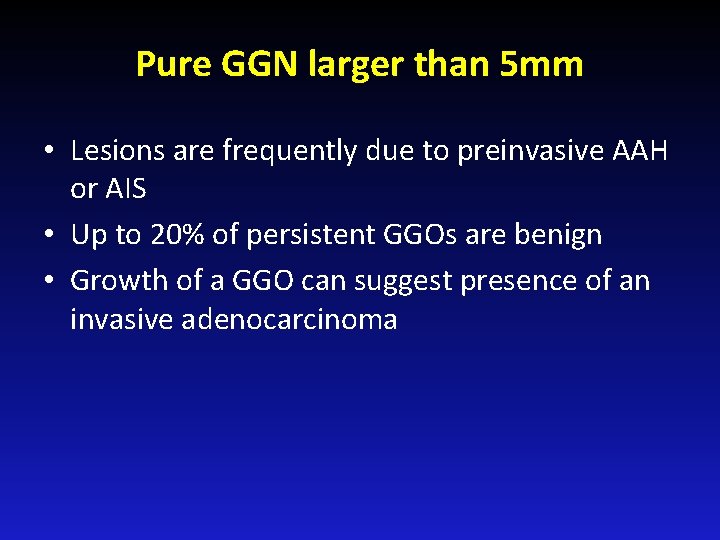
Pure GGN larger than 5 mm • Lesions are frequently due to preinvasive AAH or AIS • Up to 20% of persistent GGOs are benign • Growth of a GGO can suggest presence of an invasive adenocarcinoma
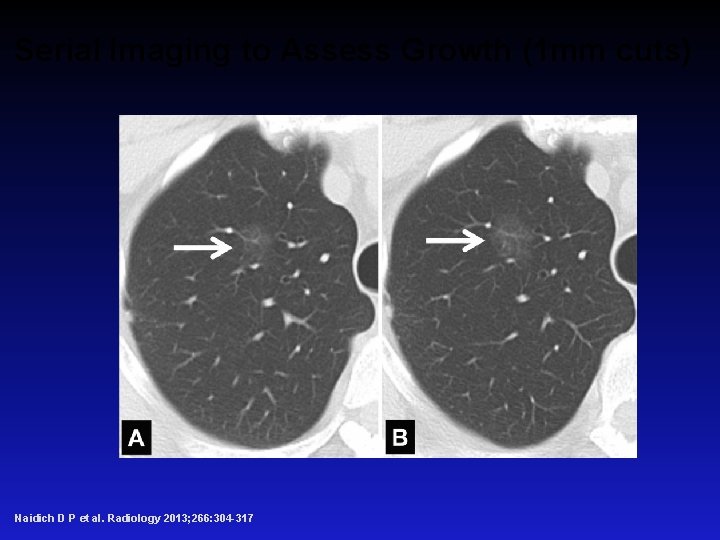
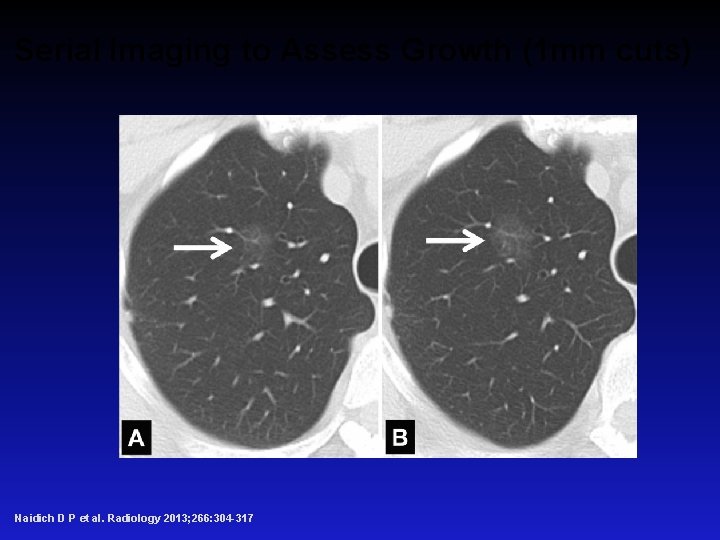
Serial Imaging to Assess Growth (1 mm cuts) Naidich D P et al. Radiology 2013; 266: 304 -317
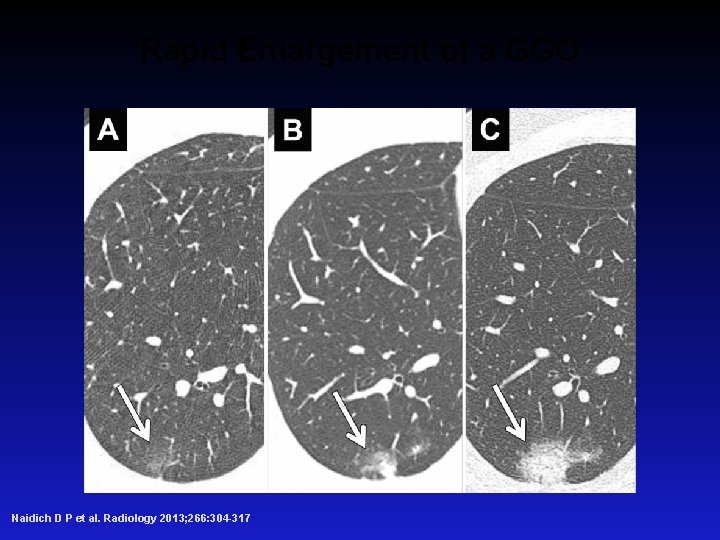
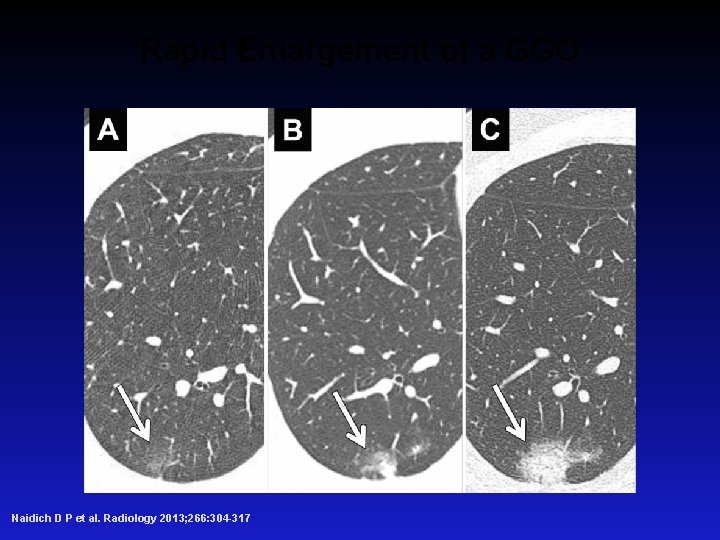
Rapid Enlargement of a GGO Naidich D P et al. Radiology 2013; 266: 304 -317
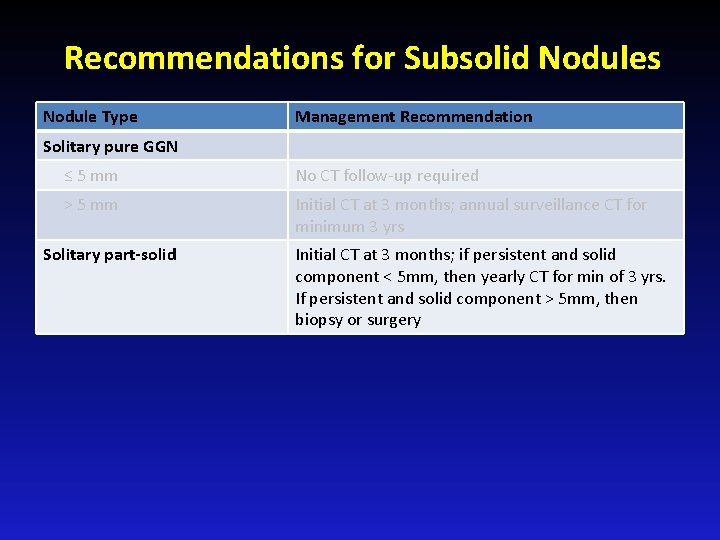
Recommendations for Subsolid Nodules Nodule Type Management Recommendation Solitary pure GGN ≤ 5 mm No CT follow-up required > 5 mm Initial CT at 3 months; annual surveillance CT for minimum 3 yrs Solitary part-solid Initial CT at 3 months; if persistent and solid component < 5 mm, then yearly CT for min of 3 yrs. If persistent and solid component > 5 mm, then biopsy or surgery

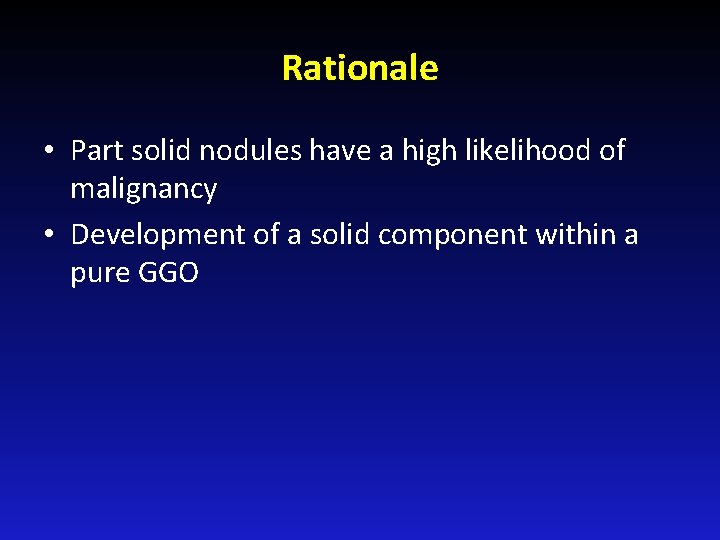
Rationale • Part solid nodules have a high likelihood of malignancy • Development of a solid component within a pure GGO
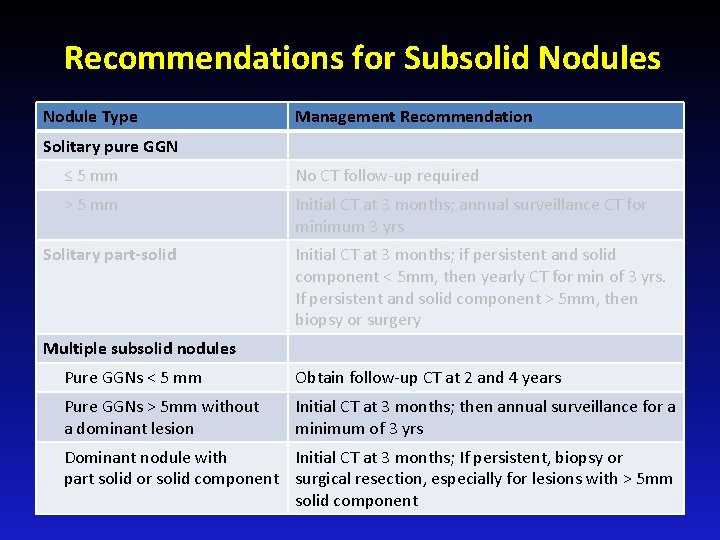
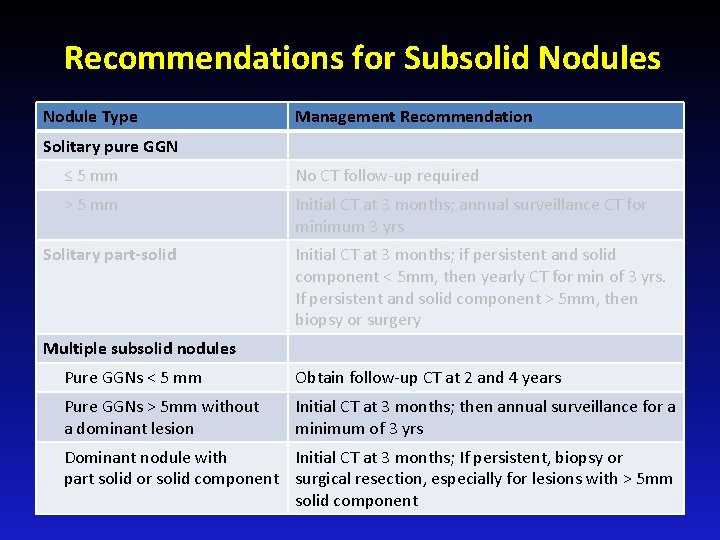
Recommendations for Subsolid Nodules Nodule Type Management Recommendation Solitary pure GGN ≤ 5 mm No CT follow-up required > 5 mm Initial CT at 3 months; annual surveillance CT for minimum 3 yrs Solitary part-solid Initial CT at 3 months; if persistent and solid component < 5 mm, then yearly CT for min of 3 yrs. If persistent and solid component > 5 mm, then biopsy or surgery Multiple subsolid nodules Pure GGNs < 5 mm Obtain follow-up CT at 2 and 4 years Pure GGNs > 5 mm without a dominant lesion Initial CT at 3 months; then annual surveillance for a minimum of 3 yrs Dominant nodule with Initial CT at 3 months; If persistent, biopsy or part solid or solid component surgical resection, especially for lesions with > 5 mm solid component
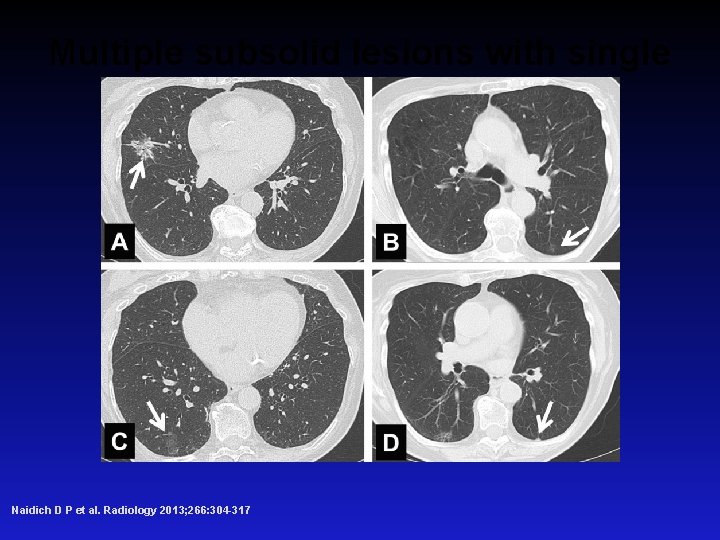
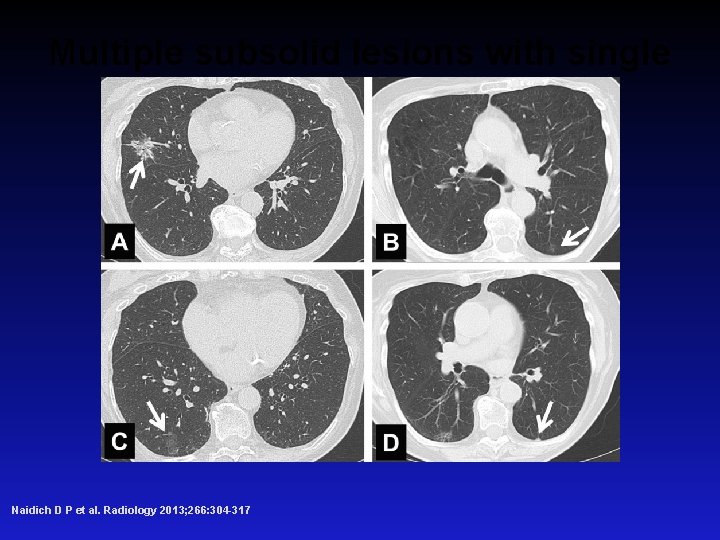
Multiple subsolid lesions with single dominant focus. Naidich D P et al. Radiology 2013; 266: 304 -317
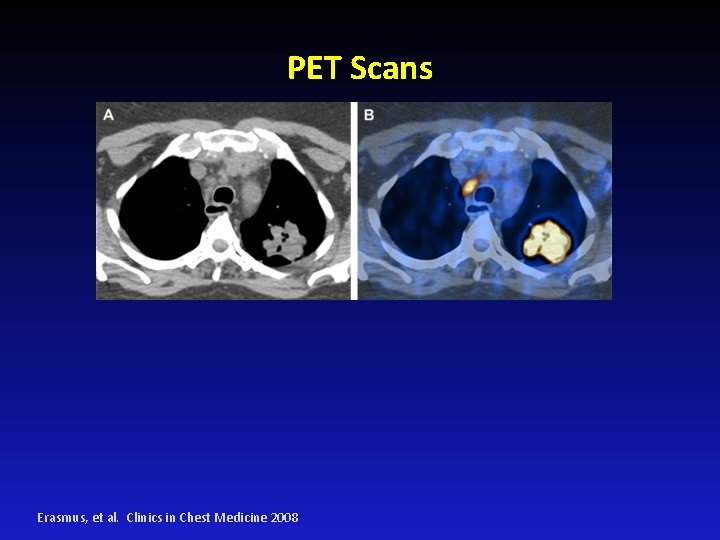
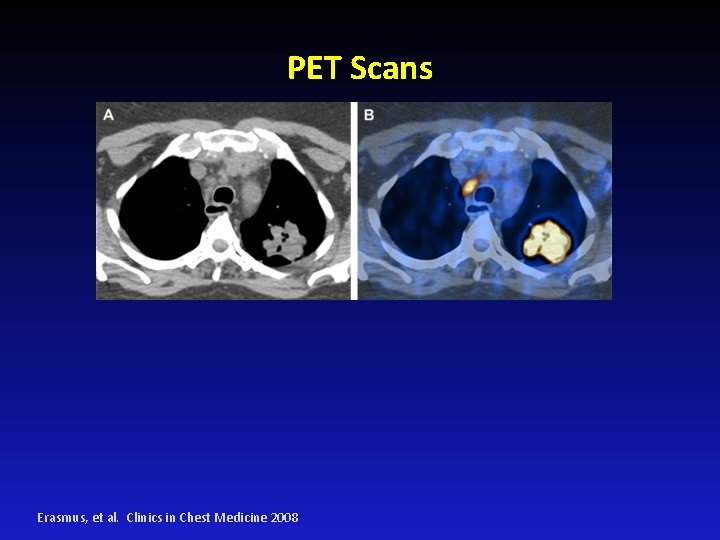
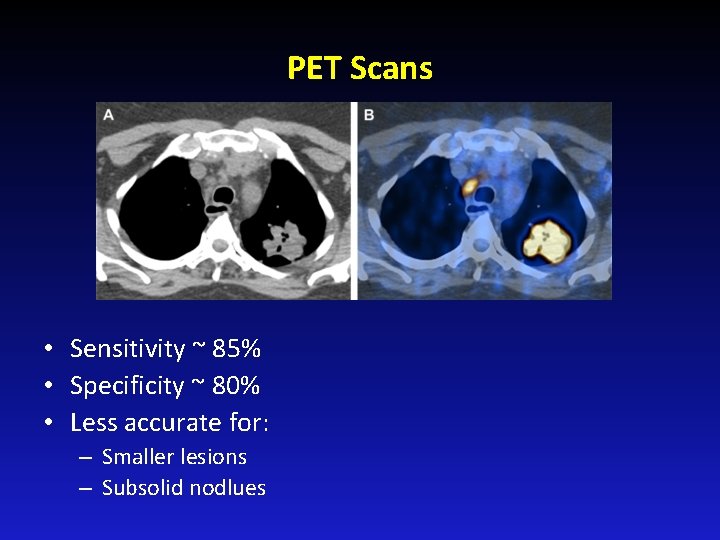
PET Scans Erasmus, et al. Clinics in Chest Medicine 2008
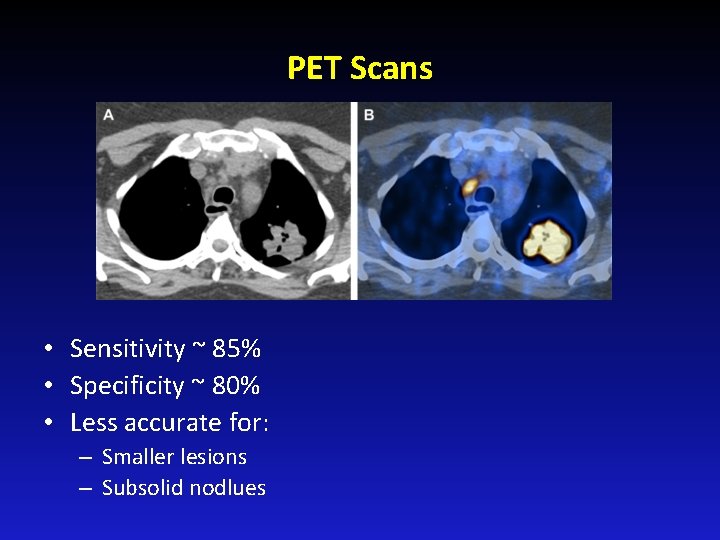
PET Scans • Sensitivity ~ 85% • Specificity ~ 80% • Less accurate for: – Smaller lesions – Subsolid nodlues
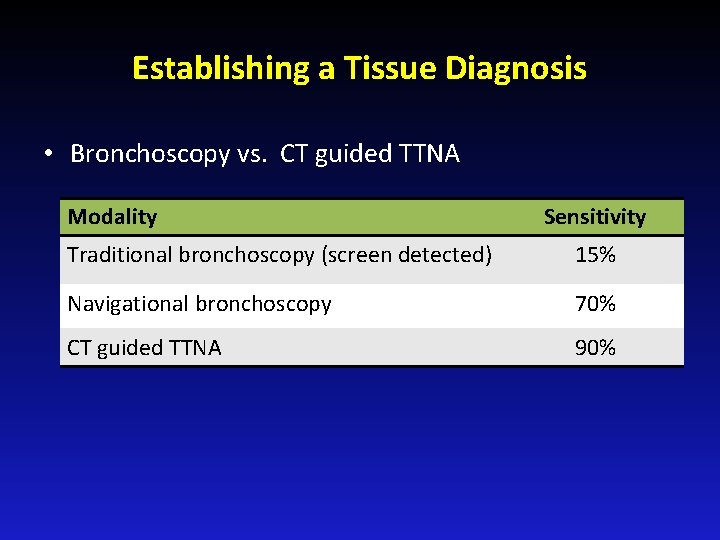
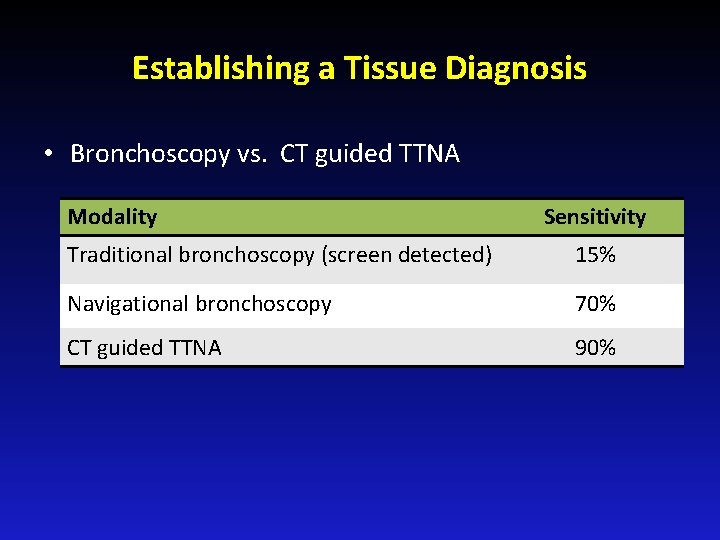
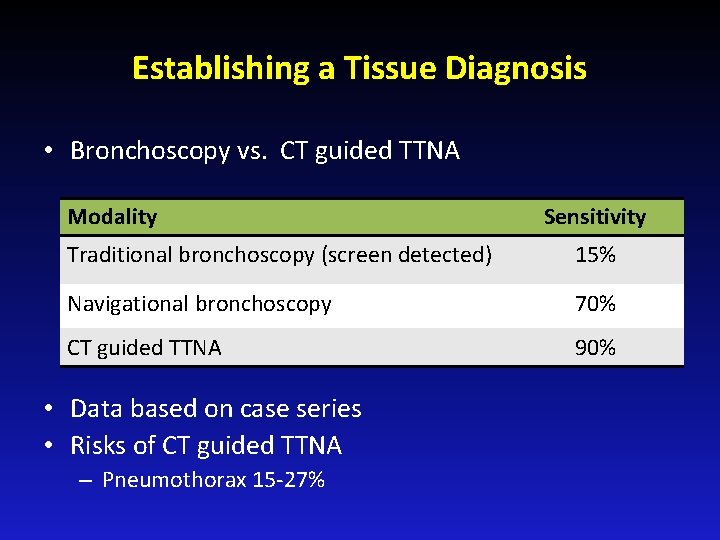
Establishing a Tissue Diagnosis • Bronchoscopy vs. CT guided TTNA Modality Sensitivity Traditional bronchoscopy (screen detected) 15% Navigational bronchoscopy 70% CT guided TTNA 90%
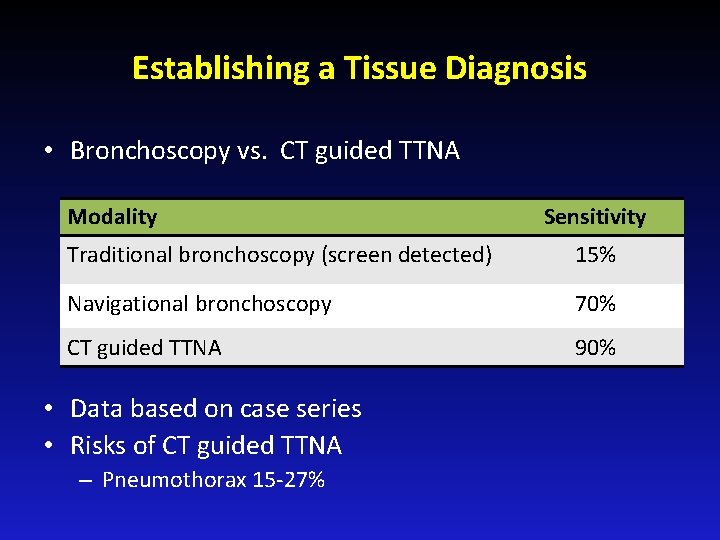
Establishing a Tissue Diagnosis • Bronchoscopy vs. CT guided TTNA Modality Sensitivity Traditional bronchoscopy (screen detected) 15% Navigational bronchoscopy 70% CT guided TTNA 90% • Data based on case series • Risks of CT guided TTNA – Pneumothorax 15 -27%
Conclusions • Lung nodules are increasingly common • Important to elicit patient preferences • Management should include – Estimation of cancer risk • Nodules ≤ 8 mm are infrequently malignant – CT scan surveillance is best option in most cases • If high likelihood of malignancy and low surgical risk, consider surgical evaluation • Emergence of peripheral blood biomarkers

THANK YOU