Risk Adjustment Hierarchical Condition Categories HCC Coding Payment
- Slides: 19
Risk Adjustment Hierarchical Condition Categories (HCC Coding) Payment Model General Education Guide 1
What is CMS’s Hierarchical Condition Categories? • Medicare Risk Adjustment payment model introduced by the Centers for Medicare and Medicaid (CMS) in 2004. • The goal is to pay Medicare Advantage (MA) and Prescription Drug Plans (PDPs) accurately and fairly by adjusting payment for Enrollees based on their demographics and their health status. • This Risk Adjustment payment model measures the disease burden that includes 70 HCC categories, which are correlated to diagnosis codes. • Accurate diagnosis code documentation (ICD-10 CM) and reporting now determines reimbursement. – 8, 700 ICD-10 codes map to 1 of 70 HCCs (mostly chronic but some are acute). Previously in ICD-9 it was 3, 600 codes. 2
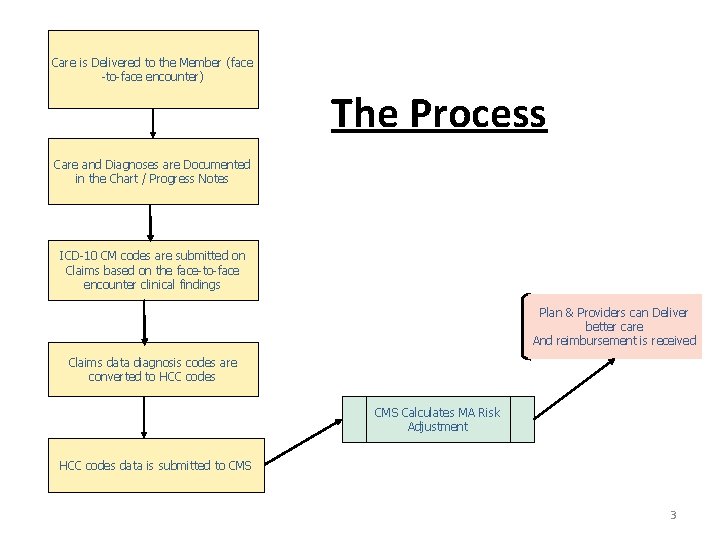
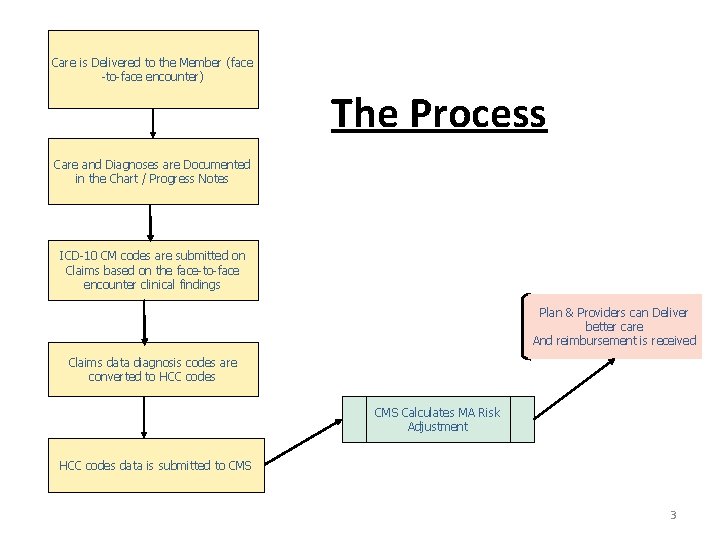
Care is Delivered to the Member (face -to-face encounter) The Process Care and Diagnoses are Documented in the Chart / Progress Notes ICD-10 CM codes are submitted on Claims based on the face-to-face encounter clinical findings Plan & Providers can Deliver better care And reimbursement is received Claims data diagnosis codes are converted to HCC codes CMS Calculates MA Risk Adjustment HCC codes data is submitted to CMS 3
Payment Methodology Payments are based upon acuity of diagnosis. • Sicker patients will require more health care resources. • Diagnoses must be reestablished each year to ensure that next year’s payments will cover costs. For example, an amputation must be reported at least once per year to ensure that services related to this condition will be covered. • Documentation must support the diagnoses that are reported AND A PLAN FOR EACH DIAGNOSIS. Often times physicians get familiar with patients over time and neglect documentation of chronic stable conditions. 4
Questions to consider regarding physician documentation The medical record can be compared to a story book of the patient • Does the documentation paint the complete picture of the patient’s condition? 5
Document, Document • Is your documentation sufficient to fund the care for your sicker patients? Goal = Properly Reflect the Member’s Health Status • Fully assess ALL Chronic Conditions …. …at least annually • Thoroughly Document in the Chart (Progress Notes) ALL conditions evaluated for each visit • Code to the Highest Level of Certainty (fully utilize the ICD-10 Diagnosis Coding System) 6
HCC Payment Methodology and ICD-10 Coding Physicians will need to be more specific in their documentation than they may have been in the past. There is a greater number of codes in ICD-10 versus ICD-9. • Physicians will need to pay more attention to their medical documentation, to make sure that it contains the necessary details so that staff members can choose the right codes for each patient. • Besides the increased specificity of a diagnostic code, doctors also face other documentation challenges, including identification of: ü Conditions that contributes to the complexity of a disease ü The severity of a contributing comorbidity ü The current stage of a disease (such as chronic kidney disease, dementia, or asthma) ü The type of diabetes and its severity ü A complete history of any present illnesses and follow-up visits 7
Coding Changes with ICD-10 Diabetes documentation must include: ü Type of diabetes ü Body system affected ü Complication or manifestation ü If a patient with type 2 diabetes is using insulin, a secondary code for long term insulin use is required Neoplasms documentation must include: ü Type: Malignant (Primary, Secondary, Ca in situ) Benign Uncertain Unspecified behavior ü Location(s) (site specific) ü If malignant, any secondary sites should also be determined ü Laterality, in some cases Asthma documentation must include: ü Severity of disease: ü Mild intermittent ü Mild persistent ü Moderate persistent 8
Coding Changes with ICD-10 Diabetes • There are over 200 ICD-10 codes for diabetes. Medical record documentation must be more specific regarding the disease in order to choose the most appropriate code. Providers MUST create a link between diabetes and its complications. There also some new categories of DM complications in ICD-10: DM with skin complications, DM with oral complications, and DM with arthropathy. • Providers will be required to draw a causal link between the type of diabetes and the complications. Under ICD-10, more than ever, clear and concise documentation will be critical to ensure correct coding and to receive appropriate reimbursement for your risk population. 9
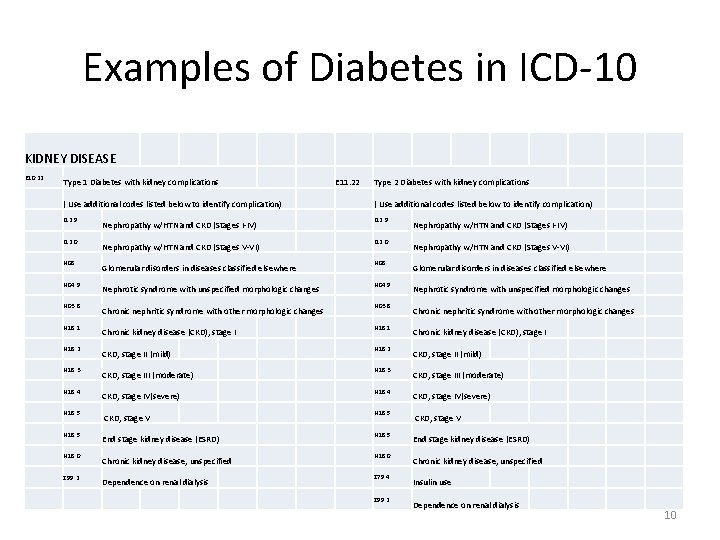
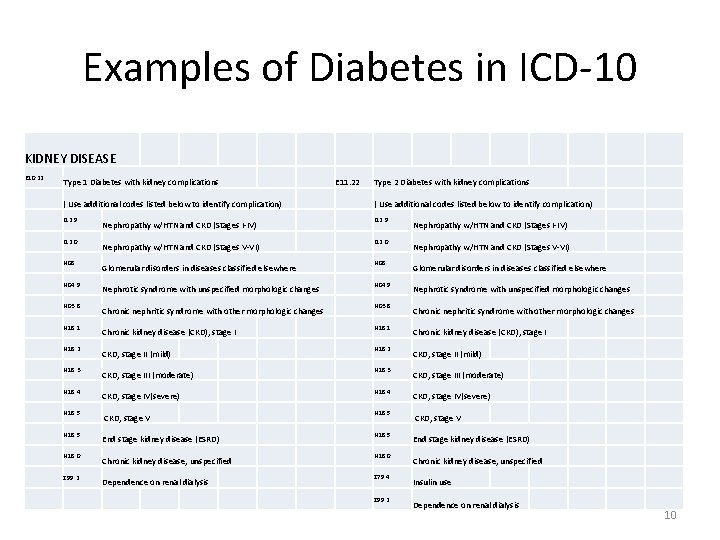
Examples of Diabetes in ICD-10 KIDNEY DISEASE E 10. 22 Type 1 Diabetes with kidney complications E 11. 22 Type 2 Diabetes with kidney complications ( Use additional codes listed below to identify complication) I 12. 9 I 12. 0 N 08 N 04. 9 N 03. 8 N 18. 1 N 18. 2 N 18. 3 N 18. 4 N 18. 5 N 18. 0 Z 99. 2 Nephropathy w/HTN and CKD (Stages I-IV) Nephropathy w/HTN and CKD (Stages V-VI) Glomerular disorders in diseases classified elsewhere Nephrotic syndrome with unspecified morphologic changes Chronic nephritic syndrome with other morphologic changes Chronic kidney disease (CKD), stage I CKD, stage II (mild) CKD, stage III (moderate) CKD, stage IV(severe) CKD, stage V End stage kidney disease (ESRD) Chronic kidney disease, unspecified Dependence on renal dialysis I 12. 0 N 08 N 04. 9 N 03. 8 N 18. 1 N 18. 2 N 18. 3 N 18. 4 N 18. 5 N 18. 0 Z 79. 4 Z 99. 2 Nephropathy w/HTN and CKD (Stages I-IV) Nephropathy w/HTN and CKD (Stages V-VI) Glomerular disorders in diseases classified elsewhere Nephrotic syndrome with unspecified morphologic changes Chronic nephritic syndrome with other morphologic changes Chronic kidney disease (CKD), stage I CKD, stage II (mild) CKD, stage III (moderate) CKD, stage IV(severe) CKD, stage V End stage kidney disease (ESRD) Chronic kidney disease, unspecified Insulin use Dependence on renal dialysis 10
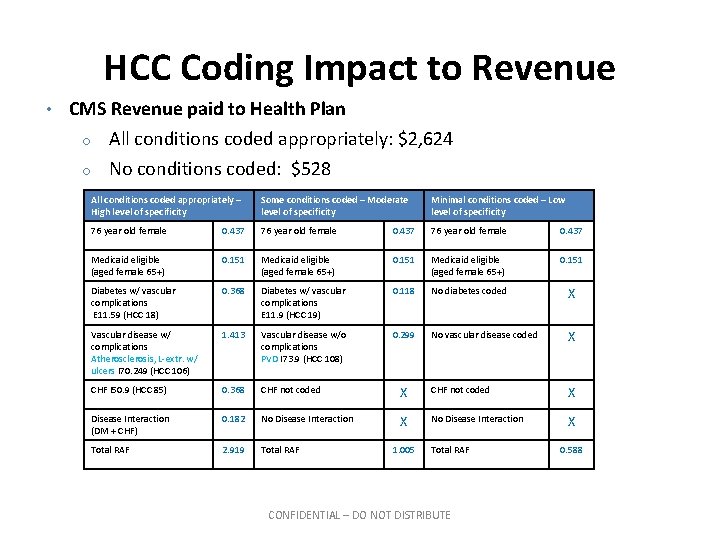
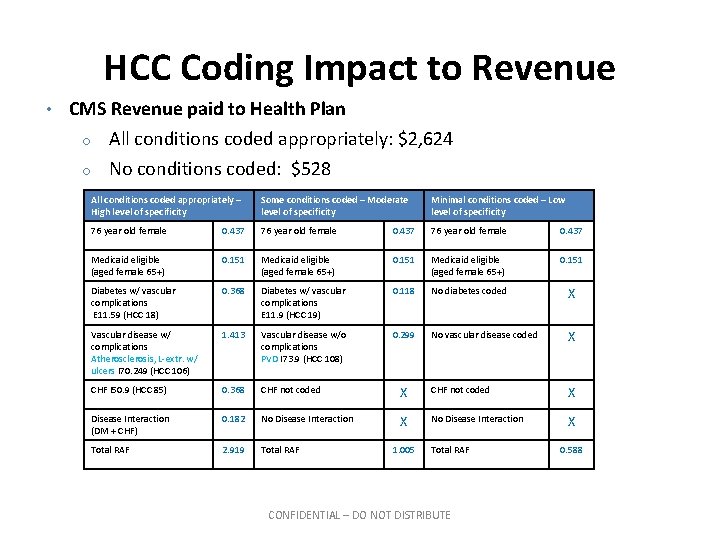
HCC Coding Impact to Revenue • CMS Revenue paid to Health Plan o o All conditions coded appropriately: $2, 624 No conditions coded: $528 All conditions coded appropriately – High level of specificity Some conditions coded – Moderate level of specificity Minimal conditions coded – Low level of specificity 76 year old female 0. 437 Medicaid eligible (aged female 65+) 0. 151 Diabetes w/ vascular complications E 11. 59 (HCC 18) 0. 368 Diabetes w/ vascular complications E 11. 9 (HCC 19) 0. 118 No diabetes coded X Vascular disease w/ complications Atherosclerosis, L-extr. w/ ulcers I 70. 249 (HCC 106) 1. 413 Vascular disease w/o complications PVD I 73. 9 (HCC 108) 0. 299 No vascular disease coded X CHF I 50. 9 (HCC 85) 0. 368 CHF not coded X Disease Interaction (DM + CHF) 0. 182 No Disease Interaction X Total RAF 2. 919 Total RAF 1. 005 Total RAF CONFIDENTIAL – DO NOT DISTRIBUTE 0. 588
Chart Documentation Each patient encounter should include: • Reason for the encounter with relevant history • Examination findings • Diagnostic test results • Assessments • Clinical impressions • Plan of care 12
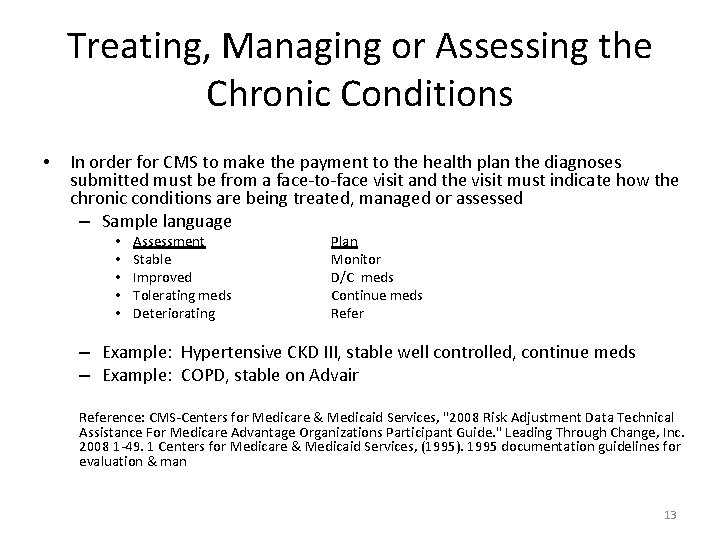
Treating, Managing or Assessing the Chronic Conditions • In order for CMS to make the payment to the health plan the diagnoses submitted must be from a face-to-face visit and the visit must indicate how the chronic conditions are being treated, managed or assessed – Sample language • • • Assessment Stable Improved Tolerating meds Deteriorating Plan Monitor D/C meds Continue meds Refer – Example: Hypertensive CKD III, stable well controlled, continue meds – Example: COPD, stable on Advair Reference: CMS-Centers for Medicare & Medicaid Services, "2008 Risk Adjustment Data Technical Assistance For Medicare Advantage Organizations Participant Guide. " Leading Through Change, Inc. 2008 1 -49. 1 Centers for Medicare & Medicaid Services, (1995). 1995 documentation guidelines for evaluation & man 13
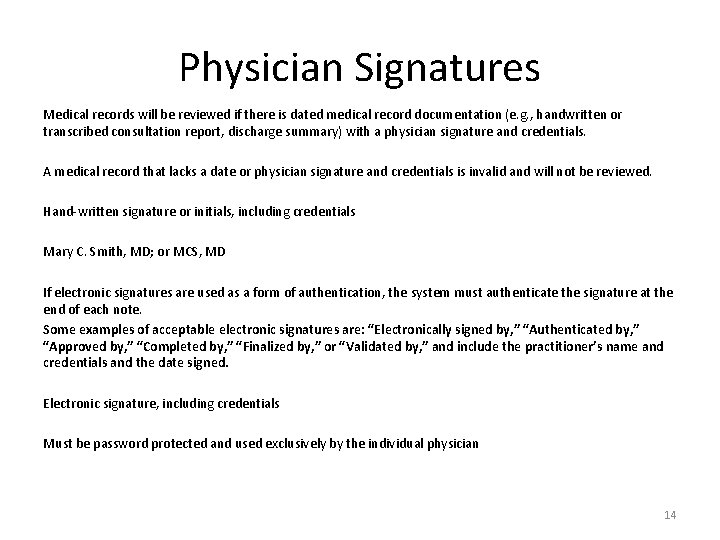
Physician Signatures Medical records will be reviewed if there is dated medical record documentation (e. g. , handwritten or transcribed consultation report, discharge summary) with a physician signature and credentials. A medical record that lacks a date or physician signature and credentials is invalid and will not be reviewed. Hand-written signature or initials, including credentials Mary C. Smith, MD; or MCS, MD If electronic signatures are used as a form of authentication, the system must authenticate the signature at the end of each note. Some examples of acceptable electronic signatures are: “Electronically signed by, ” “Authenticated by, ” “Approved by, ” “Completed by, ” “Finalized by, ” or “Validated by, ” and include the practitioner’s name and credentials and the date signed. Electronic signature, including credentials Must be password protected and used exclusively by the individual physician 14
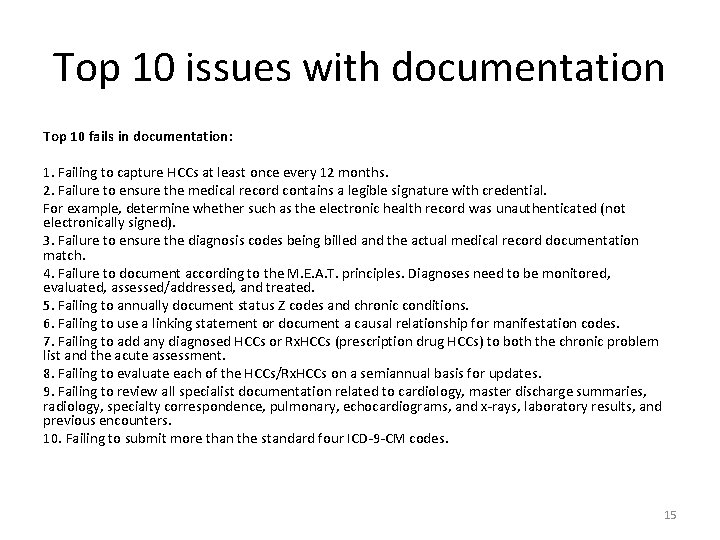
Top 10 issues with documentation Top 10 fails in documentation: 1. Failing to capture HCCs at least once every 12 months. 2. Failure to ensure the medical record contains a legible signature with credential. For example, determine whether such as the electronic health record was unauthenticated (not electronically signed). 3. Failure to ensure the diagnosis codes being billed and the actual medical record documentation match. 4. Failure to document according to the M. E. A. T. principles. Diagnoses need to be monitored, evaluated, assessed/addressed, and treated. 5. Failing to annually document status Z codes and chronic conditions. 6. Failing to use a linking statement or document a causal relationship for manifestation codes. 7. Failing to add any diagnosed HCCs or Rx. HCCs (prescription drug HCCs) to both the chronic problem list and the acute assessment. 8. Failing to evaluate each of the HCCs/Rx. HCCs on a semiannual basis for updates. 9. Failing to review all specialist documentation related to cardiology, master discharge summaries, radiology, specialty correspondence, pulmonary, echocardiograms, and x-rays, laboratory results, and previous encounters. 10. Failing to submit more than the standard four ICD-9 -CM codes. 15
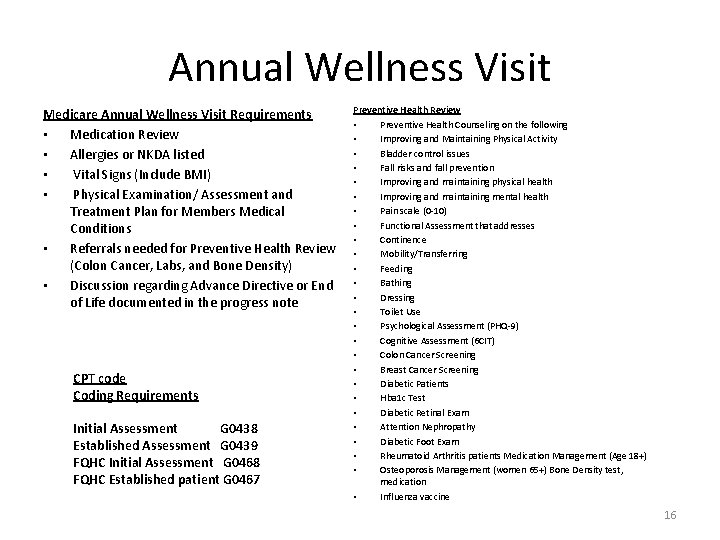
Annual Wellness Visit Medicare Annual Wellness Visit Requirements • Medication Review • Allergies or NKDA listed • Vital Signs (Include BMI) • Physical Examination/ Assessment and Treatment Plan for Members Medical Conditions • Referrals needed for Preventive Health Review (Colon Cancer, Labs, and Bone Density) • Discussion regarding Advance Directive or End of Life documented in the progress note CPT code Coding Requirements Initial Assessment G 0438 Established Assessment G 0439 FQHC Initial Assessment G 0468 FQHC Established patient G 0467 Preventive Health Review • Preventive Health Counseling on the following • Improving and Maintaining Physical Activity • Bladder control issues • Fall risks and fall prevention • Improving and maintaining physical health • Improving and maintaining mental health • Pain scale (0 -10) • Functional Assessment that addresses • Continence • Mobility/Transferring • Feeding • Bathing • Dressing • Toilet Use • Psychological Assessment (PHQ-9) • Cognitive Assessment (6 CIT) • Colon Cancer Screening • Breast Cancer Screening • Diabetic Patients • Hba 1 c Test • Diabetic Retinal Exam • Attention Nephropathy • Diabetic Foot Exam • Rheumatoid Arthritis patients Medication Management (Age 18+) • Osteoporosis Management (women 65+) Bone Density test, medication • Influenza vaccine 16
Annual Wellness Visit Forms 17
Audits • CMS audits medical records to validate documentation. • Validation Audits – Superbills are not considered sufficient documentation … they are a reporting format only. – Documentation must show the diagnosis was assigned within the data collection period. – Data discrepancies that are found as a result of audit may cause a risk adjusted payment to be changed. 18
Contact Information • Please remember, “Documentation is only good if the next physician who treats the patient can pick up your record and know exactly what happened” Please call or email us at anytime for questions or for assistance • • • Jessica Rivas (818) 702 -0100 ext. 430 jrivas@medpointmanagement. com Linda Deaktor (818) 702 -0100 ext. 236 lldeaktor@medpointmanagement. com Kimberley Litzsey (818) 702 -0100 ext. 303 klitzsey@medpointmanagement. com We welcome your feedback and appreciate your cooperation. 19