RENAL SYSTEM ASSESSMENT PYRAMID POINTS Renal and urinary
- Slides: 40
RENAL SYSTEM ASSESSMENT
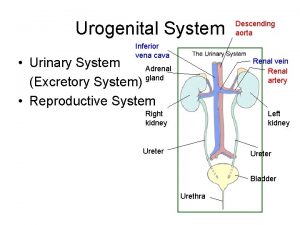
PYRAMID POINTS • • • Renal and urinary tract assessment techniques Risk factors associated with renal disorders Normal renal function test results Procedure for collecting a 24 -hour urine test Preprocedure and postprocedure care for an intravenous pyelogram (IVP) and renal angiogram • Preprocedure care for a client scheduled for a cystoscopy and biopsy • Expected and unexpected findings in the postprocedure period following cystoscopy and biopsy
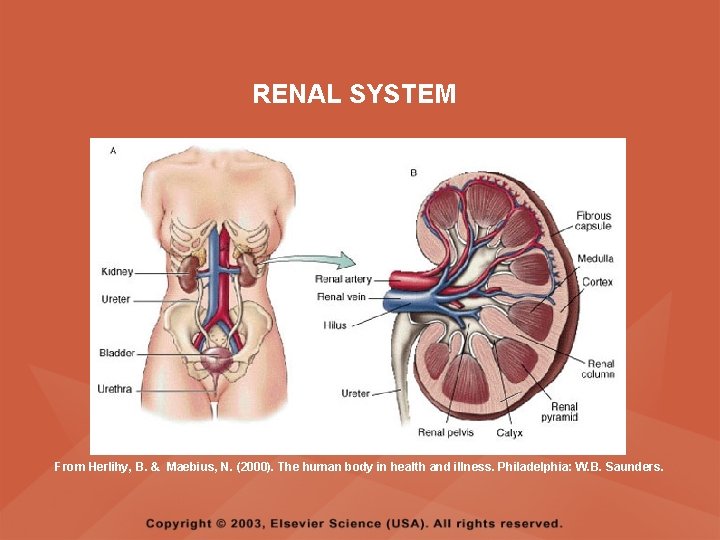
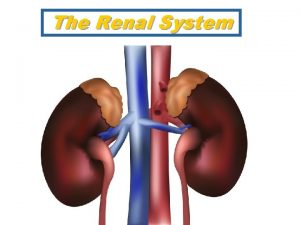
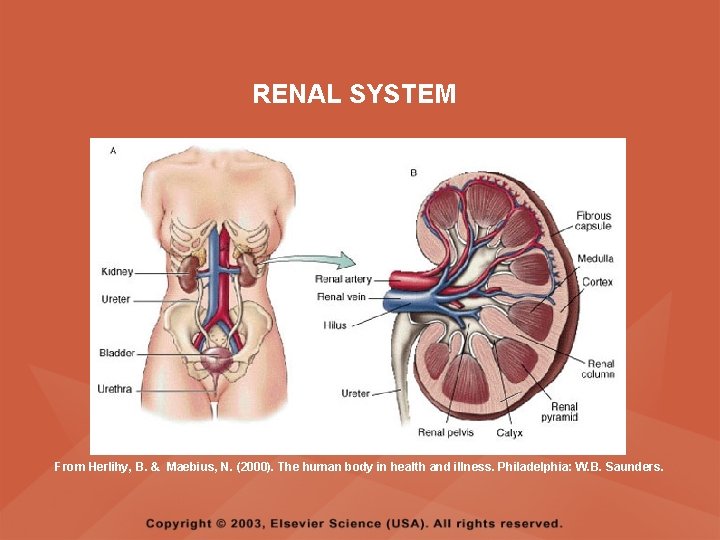
RENAL SYSTEM From Herlihy, B. & Maebius, N. (2000). The human body in health and illness. Philadelphia: W. B. Saunders.
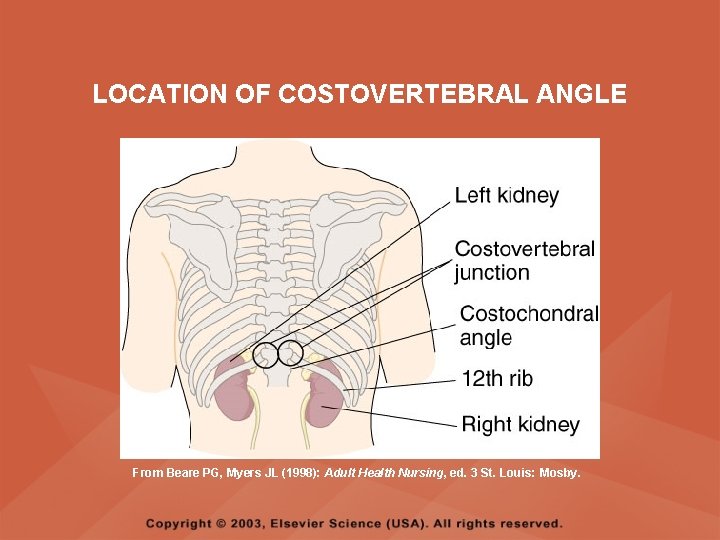
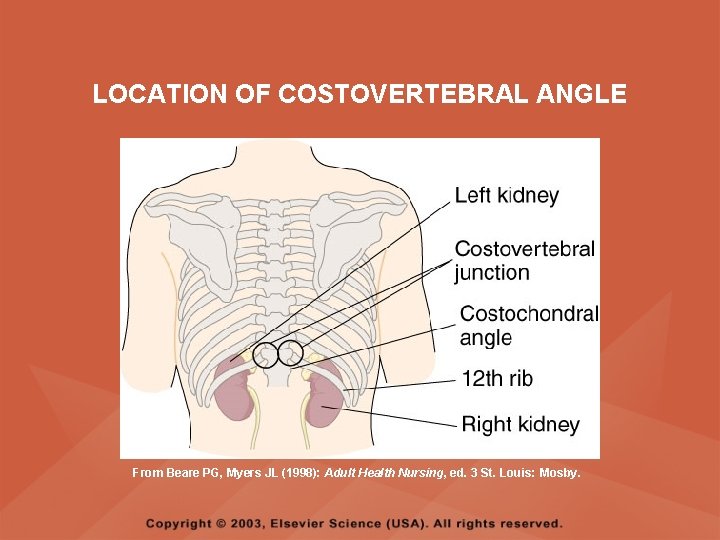
LOCATION OF COSTOVERTEBRAL ANGLE From Beare PG, Myers JL (1998): Adult Health Nursing, ed. 3 St. Louis: Mosby.
RISK FACTORS OF RENAL DISORDERS • • Associated medical conditions Contact sports Family history of renal disease Frequent urinary tract infections High-sodium diet History of hypertension Medication use Trauma and injury
NORMAL RENAL FUNCTION TESTS • • • Blood urea nitrogen (BUN), 8 to 25 mg/dl Serum creatinine, 0. 6 to 1. 3 mg/dl Creatinine clearance, 100 to 120 ml/minute Uric acid serum, 2. 5 to 8. 0 ng/dl Uric acid urine, 250 to 750 mg/24 hours
URINALYSIS • DESCRIPTION – A urine test for evaluation of the renal system and for determining renal disease • IMPLEMENTATION – Wash perineal area and use a clean container – Obtain 10 to 15 ml of the first morning sample – Note that refrigerated samples may alter the specific gravity – If the client is menstruating, indicate this on the laboratory requisition form
SPECIFIC GRAVITY DETERMINATION • DESCRIPTION – A urine test that measures the kidney’s ability to concentrate urine – Normal value is 1. 016 to 1. 022 – An increase in specific gravity (more concentrated urine) occurs with insufficient fluid intake, decreased renal perfusion, or the presence of ADH – A decrease in specific gravity (less concentrated urine) occurs with increased fluid intake, diuretic administration, and diabetes insipidus
SPECIFIC GRAVITY DETERMINATION • IMPLEMENTATION – Can be measured by multiple-test dipstick (most common method), refractometer (an instrument used in the laboratory setting), or by a urinometer (least accurate method) – Factors that interfere with an accurate reading include radiopaque contrast agents, glucose, and proteins – Cold specimens may produce a false high reading
URINE CULTURE AND SENSITIVITY • DESCRIPTION – A urine test that identifies the presence of microorganisms and determines the specific antibiotics that will appropriately treat the existing microorganism
URINE CULTURE AND SENSITIVITY • IMPLEMENTATION – Clean perineal area and urinary meatus with bacteriostatic solution – Collect midstream sample in a sterile container – Send the collected specimen to the laboratory immediately – Note that urine from the client who forced fluids may be too dilute to provide a positive culture – Identify any sources of potential contaminants during the collection of the specimen, such as the hands, skin, clothing, hair, or vaginal or rectal secretions
CREATININE CLEARANCE TEST • DESCRIPTION – A blood and timed urine specimen that evaluates kidney function – Blood is drawn at the start of the test and the morning of the day that the 24 -hour urine specimen collection is complete
CREATININE CLEARANCE TEST • IMPLEMENTATION – Encourage adequate fluids before and during the test – Instruct the client to avoid tea, coffee, and medications during testing – If the client is taking corticosteroids or thyroid medication, check with the physician regarding the administration of these medications during testing – Maintain the specimen on ice or refrigerate, and check with the laboratory regarding the addition of a preservative to the specimen during collection
VANILLYLMANDELIC ACID (VMA) TEST • DESCRIPTION – A 24 -hour urine collection to diagnose pheochromocytoma, a tumor of the adrenal gland – The test identifies an assay of urinary catecholamines in the urine
VANILLYLMANDELIC ACID (VMA) TEST • IMPLEMENTATION – Instruct the client to avoid foods such as caffeine, cocoa, vanilla, cheese, gelatin, licorice, and fruits for at least 2 days prior to beginning the urine collection and during the collection, and to avoid taking medications for 2 to 3 days prior to beginning the test as prescribed – Instruct the client to avoid stress and to maintain adequate food and fluids during the test
VANILLYLMANDELIC ACID (VMA) TEST • IMPLEMENTATION – Save all urine, label the container, add preservative, and place the specimen on ice or refrigerate – Check with the laboratory regarding medication restrictions
URIC ACID TEST • DESCRIPTION – A 24 -hour urine collection to diagnose gout and kidney disease • IMPLEMENTATION – Encourage fluids and a regular diet during testing – Place the specimen on ice or refrigerate, and check with the laboratory regarding the addition of a preservative
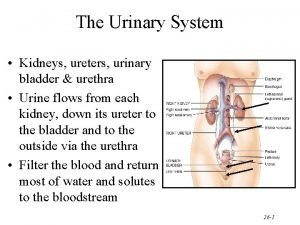
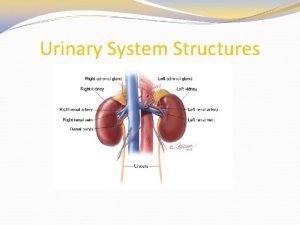
KIDNEYS, URETERS, AND BLADDER RADIOGRAPH • DESCRIPTION – Known as a KUB – An x-ray film that views the urinary system and adjacent structures – Used to detect urinary calculi • IMPLEMENTATION – There is no specific preparation
BLADDER ULTRASONOGRAPHY • DESCRIPTION – A noninvasive method of measuring the volume of urine in the bladder – May be performed for evaluating urinary frequency or inability to urinate • IMPLEMENTATION – There is no specific preparation
INTRAVENOUS PYELOGRAM (IVP) • DESCRIPTION – The injection of a radiopaque dye that outlines the renal system – Performed to identify abnormalities in the system
INTRAVENOUS PYELOGRAM (IVP) • PREPROCEDURE – Obtain a consent form – Assess the client for allergies to iodine, seafood, and radiopaque dyes – Withhold food and fluids after midnight on the night before the test – Inform the client about possible throat irritation, flushing of the face, warmth, or a salty taste that may be experienced during the test
INTRAVENOUS PYELOGRAM (IVP) • POSTPROCEDURE – Monitor vital signs – Instruct the client to drink at least 1 liter of fluid unless contraindicated – Assess the venipuncture site for bleeding – Monitor urinary output
RENAL ANGIOGRAPHY • DESCRIPTION – The injection of a radiopaque dye through a catheter for examination of the renal arterial supply
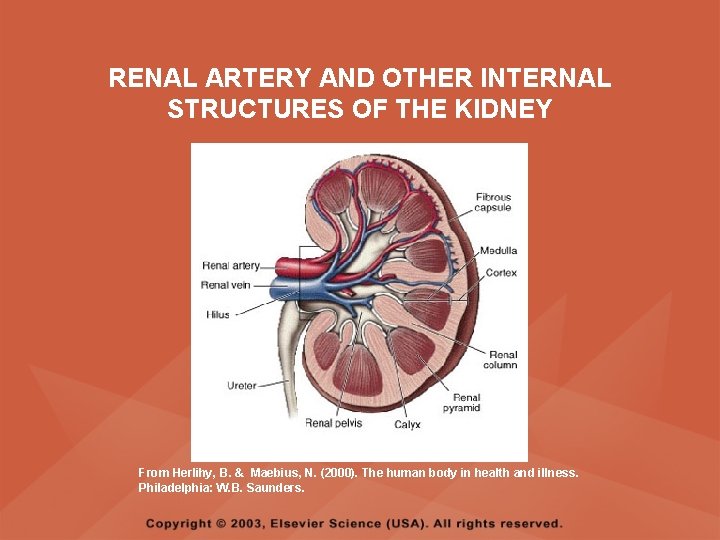
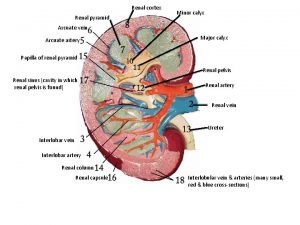
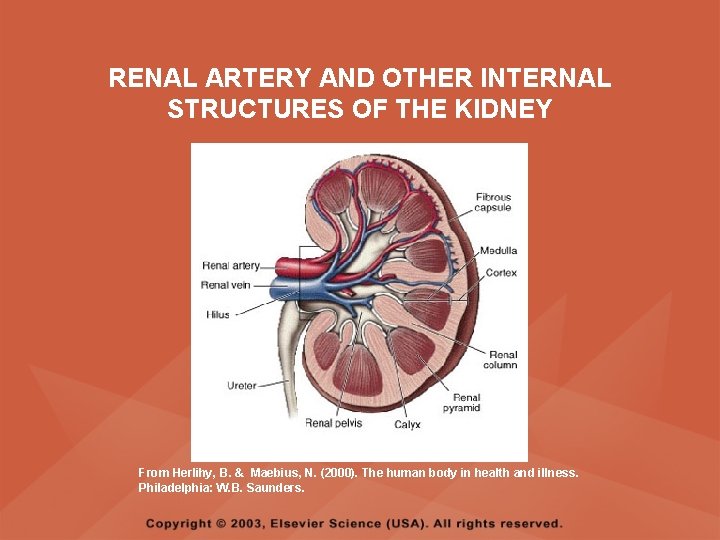
RENAL ARTERY AND OTHER INTERNAL STRUCTURES OF THE KIDNEY From Herlihy, B. & Maebius, N. (2000). The human body in health and illness. Philadelphia: W. B. Saunders.
RENAL ANGIOGRAPHY • PREPROCEDURE – Obtain a consent form – Assess the client for allergies to iodine, seafood, and radiopaque dyes – Inform the client about a possible burning feeling or a feeling of heat along the vessel when the dye is injected – Withhold food and fluids after midnight on the night before the test
RENAL ANGIOGRAPHY • PREPROCEDURE – Instruct the client to void immediately before the procedure – Administer enemas as prescribed – Shave injection sites as prescribed – Assess and mark the peripheral pulses
RENAL ANGIOGRAPHY • POSTPROCEDURE – Assess vital signs and peripheral pulses – Provide bed rest and use of a sandbag at the insertion site for 4 to 8 hours – Assess the color and temperature of the involved extremity – Inspect the catheter insertion site for bleeding or swelling – Force fluids unless contraindicated – Monitor urinary output
RENAL SCAN • DESCRIPTION – An IV injection of a radioisotope for visual imaging of renal blood flow
RENAL SCAN • PREPROCEDURE – Obtain a consent form – Assess for allergies – Assist with administering radioisotope as necessary – Instruct the client that he or she will be required to remain motionless – Instruct the client that imaging may be repeated at various intervals before the test is complete
RENAL SCAN • POSTPROCEDURE – Encourage fluids unless contraindicated – Assess the client for signs of delayed allergic reaction, such as itching and hives – Note that the radioactivity is eliminated in 24 hours – Follow standard precautions when caring for incontinent clients and double-bag client linens per agency policy
CYSTOMETROGRAM (CMG) • DESCRIPTION – A graphic recording of the pressures exerted at varying phases of the bladder • PREPROCEDURE – Inform the client of the voiding requirements during the procedure • POSTPROCEDURE – Monitor the client’s voiding after the procedure
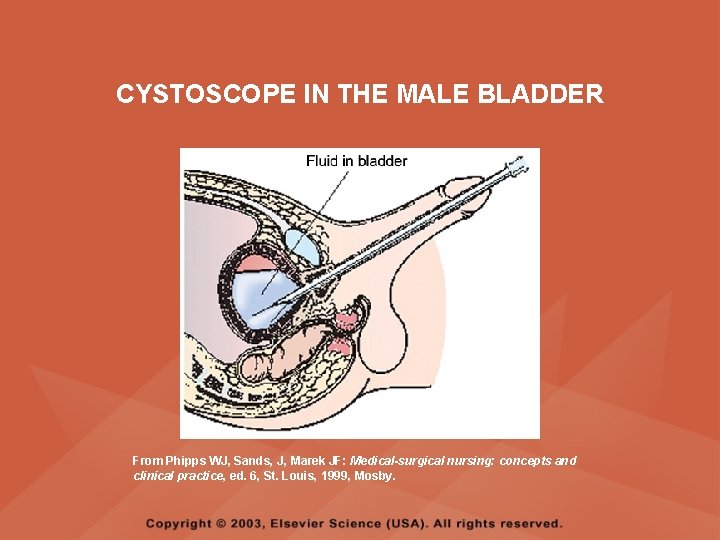
CYSTOSCOPY AND BLADDER BIOPSY • DESCRIPTION – The bladder mucosa is examined for inflammation, calculi, or tumors by means of a cystoscope – Tissue may be obtained for biopsy
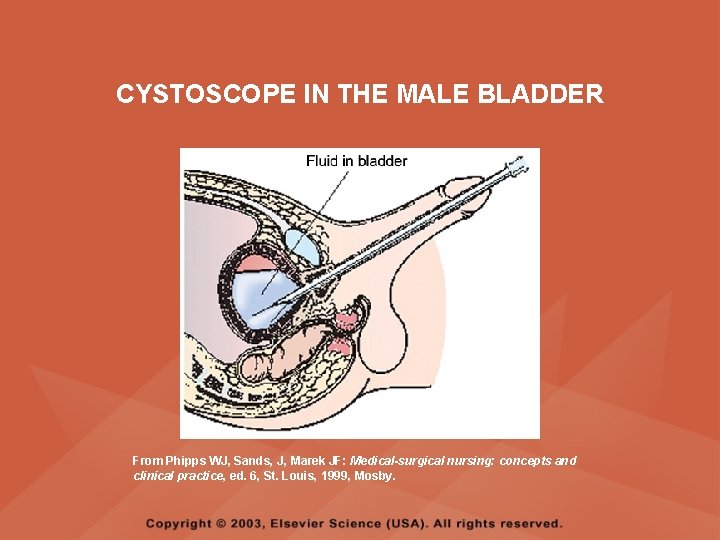
CYSTOSCOPE IN THE MALE BLADDER From Phipps WJ, Sands, J, Marek JF: Medical-surgical nursing: concepts and clinical practice, ed. 6, St. Louis, 1999, Mosby.
CYSTOSCOPY AND BLADDER BIOPSY • PREPROCEDURE – Obtain a consent form – Withhold food and fluids after midnight on the night before the test – Administer enemas and medications as prescribed
CYSTOSCOPY AND BLADDER BIOPSY • POSTPROCEDURE – Monitor vital signs – Monitor for postural hypotension – Force fluids as prescribed – Monitor intake and output – Encourage deep-breathing exercises to relieve bladder spasms – Administer analgesics as prescribed – Administer sitz baths for back and abdominal pain
CYSTOSCOPY AND BLADDER BIOPSY • POSTPROCEDURE – Note that leg cramps are common due to the lithotomy position maintained during the procedure – Assess the urine for color and consistency – Note that pink-tinged or tea-colored urine is common – Monitor for bright red urine or clots and notify the physician if this occurs
RENAL BIOPSY • DESCRIPTION – Insertion of a needle into the kidney to obtain a sample of tissue for examination
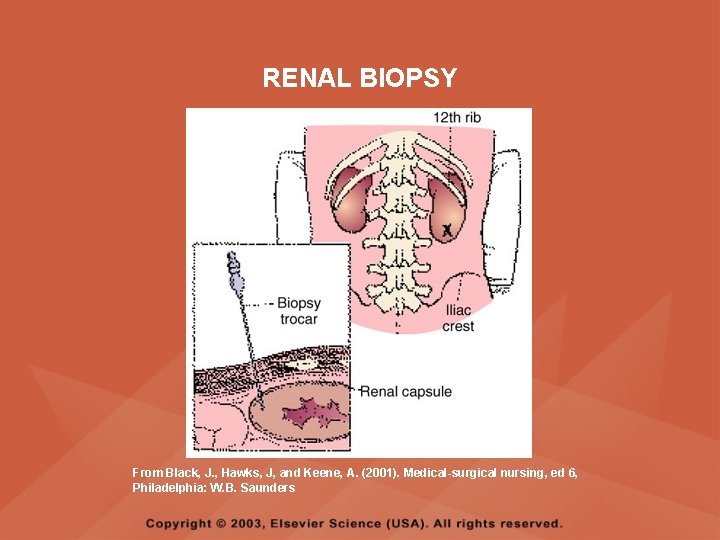
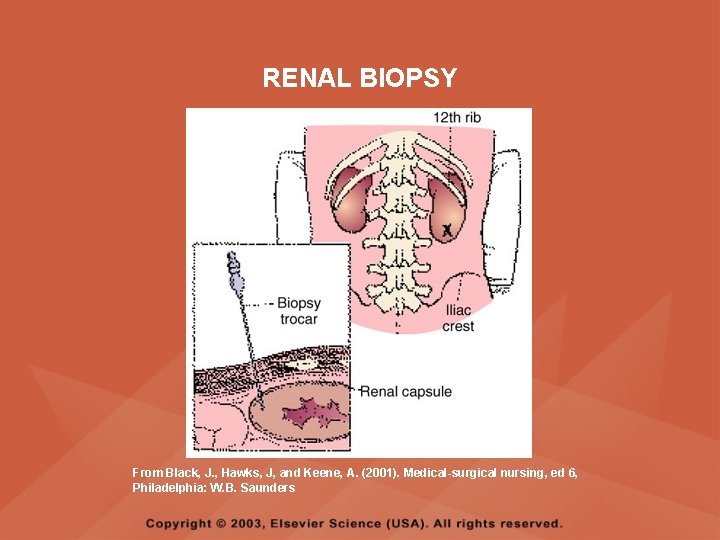
RENAL BIOPSY From Black, J. , Hawks, J, and Keene, A. (2001). Medical-surgical nursing, ed 6, Philadelphia: W. B. Saunders
RENAL BIOPSY • PREPROCEDURE – Assess vital signs – Assess baseline clotting studies – Obtain a consent form – Withhold food and fluids after midnight on the night before the test • DURING THE PROCEDURE – Position the client prone with a pillow under the abdomen and shoulders
RENAL BIOPSY • POSTPROCEDURE – Monitor vital signs – Monitor hemoglobin and hematocrit – Place the client in the supine position and on bed rest for 8 hours as prescribed – Provide pressure to the biopsy site for 30 minutes – Check the biopsy site for bleeding – Force fluids to 1500 to 2000 ml as prescribed – Instruct the client to avoid heavy lifting and strenuous activity for 2 weeks
 Ira pré renal renal e pós renal
Ira pré renal renal e pós renal Sindrome nefrótica
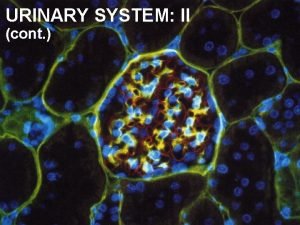
Sindrome nefrótica Renal corpuscle
Renal corpuscle Lymphatic system and urinary system
Lymphatic system and urinary system Renal pyramid
Renal pyramid Calyx minor
Calyx minor Apex of renal pyramid
Apex of renal pyramid Detrusal
Detrusal Bullseye brand positioning
Bullseye brand positioning Point of difference and point of parity
Point of difference and point of parity Physiology of urine formation
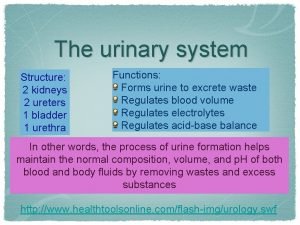
Physiology of urine formation Chapter 15 urinary system
Chapter 15 urinary system Polyrrhagia
Polyrrhagia Interesting facts about the urinary system
Interesting facts about the urinary system Pig reproductive anatomy
Pig reproductive anatomy Chapter 30 the urinary system
Chapter 30 the urinary system Kidney pyramid labeled
Kidney pyramid labeled Chapter 20 urinary/excretory system
Chapter 20 urinary/excretory system Urinary system model
Urinary system model Urinary system fun fact
Urinary system fun fact Alimentary canal
Alimentary canal Urinary system powerpoint
Urinary system powerpoint Proximal convoluted tubule histology
Proximal convoluted tubule histology Function of antidiuretic hormone
Function of antidiuretic hormone Urinary system histology
Urinary system histology Figure 15-4 is a diagram of a nephron
Figure 15-4 is a diagram of a nephron Prone
Prone Defination of urine
Defination of urine Excretory system
Excretory system Endocrine system of rat
Endocrine system of rat Rat urinary system
Rat urinary system Vena cava excretory system
Vena cava excretory system Kidneys location and structure figure 15-2
Kidneys location and structure figure 15-2 Macula densa cells
Macula densa cells Renal tubule
Renal tubule Urinary system
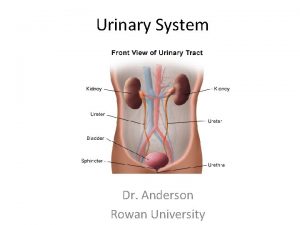
Urinary system Normal constituents of urine
Normal constituents of urine What is this called
What is this called Normal and abnormal constituents of urine
Normal and abnormal constituents of urine Layers of kidney
Layers of kidney Urinary system
Urinary system