Renal manifestations of ADPKD R 1 Introduction ADPKD
- Slides: 18
Renal manifestations of ADPKD 신장내과 R 1 최경진
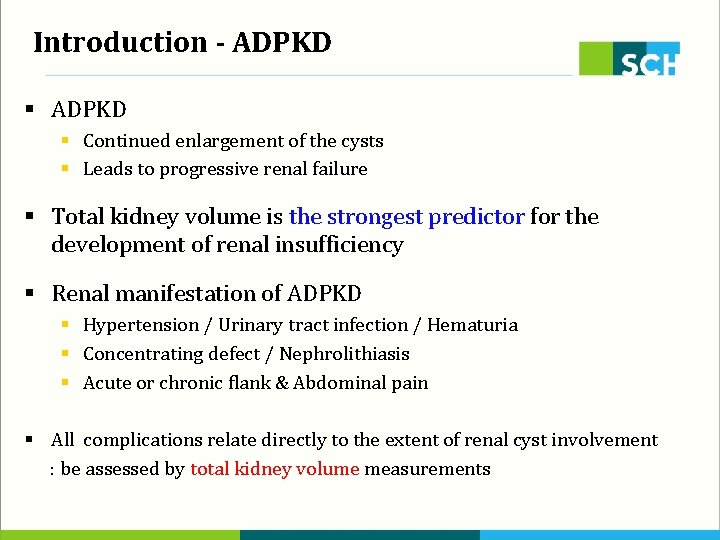
Introduction - ADPKD § Continued enlargement of the cysts § Leads to progressive renal failure § Total kidney volume is the strongest predictor for the development of renal insufficiency § Renal manifestation of ADPKD § Hypertension / Urinary tract infection / Hematuria § Concentrating defect / Nephrolithiasis § Acute or chronic flank & Abdominal pain § All complications relate directly to the extent of renal cyst involvement : be assessed by total kidney volume measurements
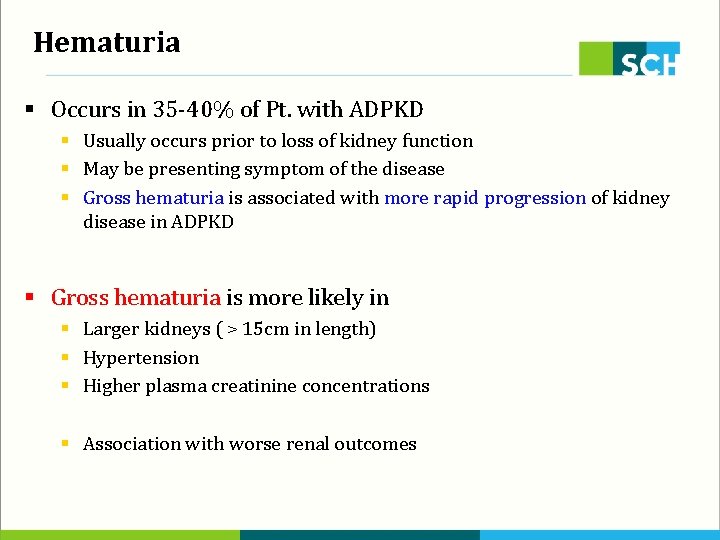
Hematuria § Occurs in 35 -40% of Pt. with ADPKD § Usually occurs prior to loss of kidney function § May be presenting symptom of the disease § Gross hematuria is associated with more rapid progression of kidney disease in ADPKD § Gross hematuria is more likely in § Larger kidneys ( > 15 cm in length) § Hypertension § Higher plasma creatinine concentrations § Association with worse renal outcomes
Hematuria § Rupture of a cyst into the collecting system § Be responsible for the development of hematuria § Although hemorrhage into a cyst is common, typical presentation is pain d/t many cysts don’t communicate with the collecting system § Hematuria resolves within 2 -7 days with conservative therapy : Bed rest, Hydration, Analgesics not NSAID § Unusual & severe bleeding § Percutaneous arterial embolization § Nephrectomy
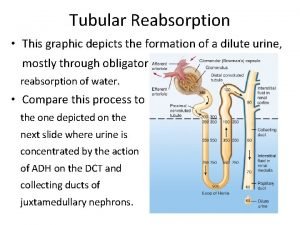
Concentrating defect § Complain of thirst, polyuria, nocturia & urinary frequency § a Decrease in urinary concentrating ability is one of the earliest manifestations of ADPKD § Worsens with increasing age & declining kidney function § Severity of anatomical deformities induced by the cysts § Underlying cause is not known § Disruption of tubular architecture § Defect in principal cell function § Early tubulointerstitial disease
Concentrating defect § Elevation of Vasopression level > Central cause is excluded § occurs early in the course of the disease § in order to preserve water balance § Urine diluting capacity appears to be intact in ADPKD § Increased vasopressin concentration may play a role in disease progression § Strategies to inhibit vasopressin action are potential therapeutic modalities in ADPKD § Vasopressin Rc antagonists § reduce vasopressin levels with increased free water intake
Nephrolithiasis § Occurs in -25% of Pt. with ADPKD § Composition of uric acid > ½ of stones in ADPKD § Risk factor for nephrolithiasis § Increased renal volume : controversial § In one study, renal volume determined by CT was greater in 35 pts with ADPKD and nephrolithiasis, compared with those who had ADPKD but no nephrolithiasis § In the CRISP study of 241 individuals, no association between nephrolithiasis and kidney volume could be established § Low urinary volume / Low urinary citrate § Hyperuricosuria / Hypercalciuria
Nephrolithiasis § Diagnosis of stone § by USG is more difficult than in idiopathic stone formers, § the large cysts obscuring the view of the collecting system § calcifications that may be present in the cyst walls § Most stones can be detected by Intravenous pyelography § By CT scanning is more sensitive for small or radiolucent stones § Treatment of obstructing stones § More difficult than idiopathic stone disease § Cystoscopy : be complicated by an infected cyst § Percutaneous nephrostomy or ESWL is hard d/t large cysts § small stones( < 2 cm in diameter) is successful § Percutaneous nephrolithotomy in a limited patients
Flank & Abdominal pain § Common problem § Can be due to renal or extrarenal etiologies § Acute kidney pain § § Infections (cystic or parenchymal) Nephrolithiasis Cyst hemorrhage Cysts in the liver § Chronic kidney pain § more common in advanced disease who have enlarged kidneys § Dull, persistent § Stretching of the capsule or traction on the renal pedicle
Renal cell carcinoma (RCC) § an infrequent complication of ADPKD § not occur with increased frequency than general population § Differentiating characteristics of RCC in ADPKD § § Patients frequently present with fever Bilateral at presentation Multicentric Sarcomatoid type
Renal cell carcinoma (RCC) § Diagnosis of RCC is difficult in ADPKD § Hematuria / a Flank mass / Bleeding into cysts / a Complex cyst on USG, CT or MRI > common in ADPKD with out malignancy § Some clinical clues may be helpful § systemic signs & symptoms( fever, anorexia, fatigue, Wt. loss) § rapid growth of a complex cyst § Percutaneous aspiration & cytologic examination
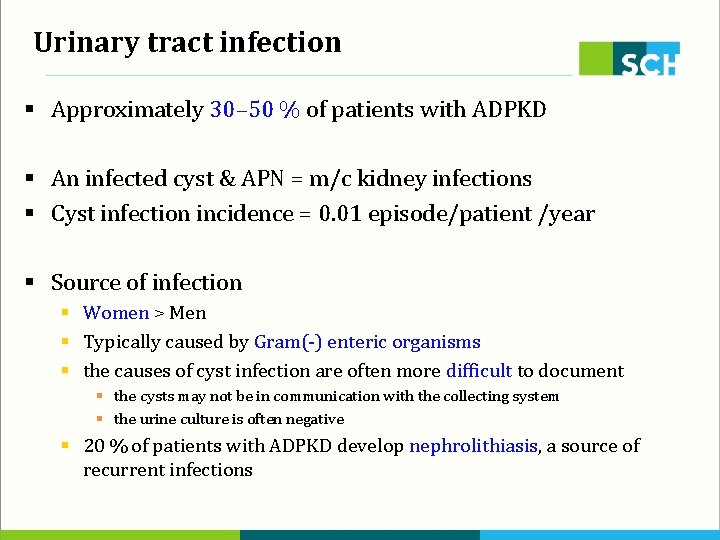
Urinary tract infection § Approximately 30– 50 % of patients with ADPKD § An infected cyst & APN = m/c kidney infections § Cyst infection incidence = 0. 01 episode/patient /year § Source of infection § Women > Men § Typically caused by Gram(-) enteric organisms § the causes of cyst infection are often more difficult to document § the cysts may not be in communication with the collecting system § the urine culture is often negative § 20 % of patients with ADPKD develop nephrolithiasis, a source of recurrent infections
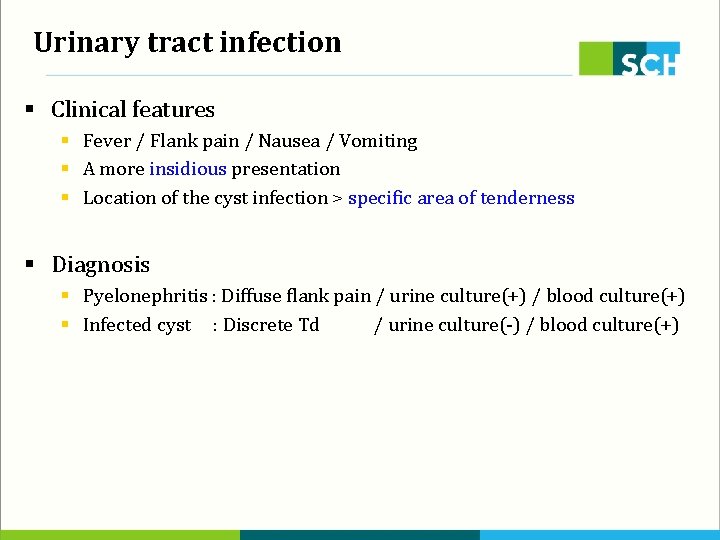
Urinary tract infection § Clinical features § Fever / Flank pain / Nausea / Vomiting § A more insidious presentation § Location of the cyst infection > specific area of tenderness § Diagnosis § Pyelonephritis : Diffuse flank pain / urine culture(+) / blood culture(+) § Infected cyst : Discrete Td / urine culture(-) / blood culture(+)
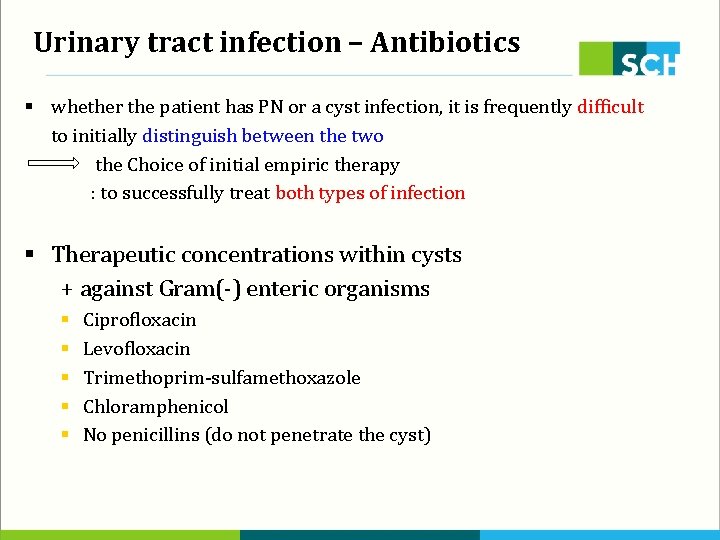
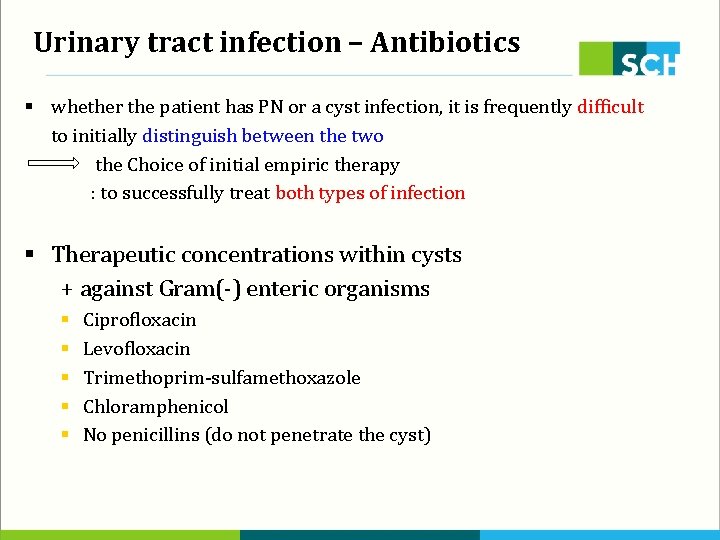
Urinary tract infection – Antibiotics § whether the patient has PN or a cyst infection, it is frequently difficult to initially distinguish between the two the Choice of initial empiric therapy : to successfully treat both types of infection § Therapeutic concentrations within cysts + against Gram(-) enteric organisms § § § Ciprofloxacin Levofloxacin Trimethoprim-sulfamethoxazole Chloramphenicol No penicillins (do not penetrate the cyst)
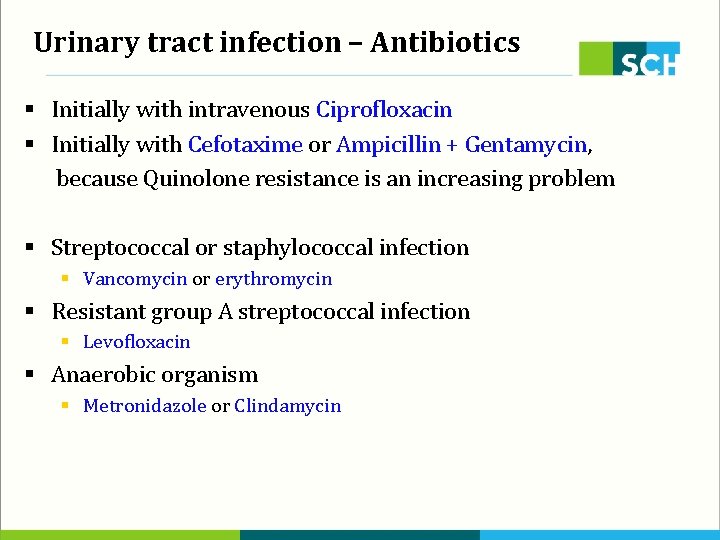
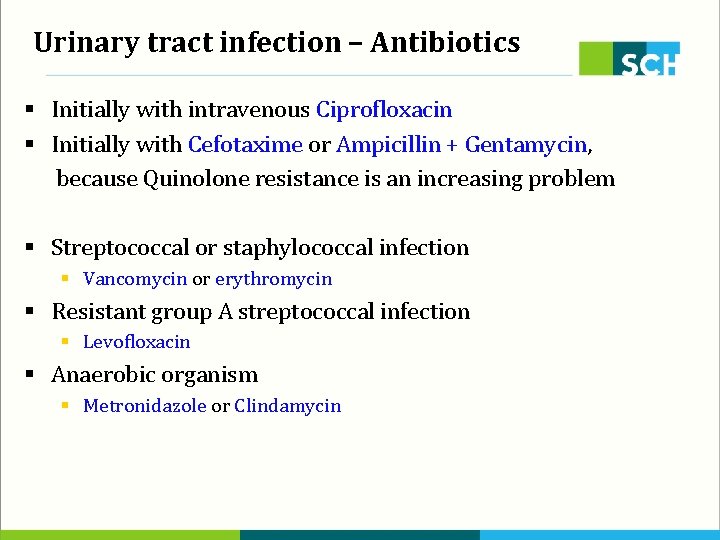
Urinary tract infection – Antibiotics § Initially with intravenous Ciprofloxacin § Initially with Cefotaxime or Ampicillin + Gentamycin, because Quinolone resistance is an increasing problem § Streptococcal or staphylococcal infection § Vancomycin or erythromycin § Resistant group A streptococcal infection § Levofloxacin § Anaerobic organism § Metronidazole or Clindamycin
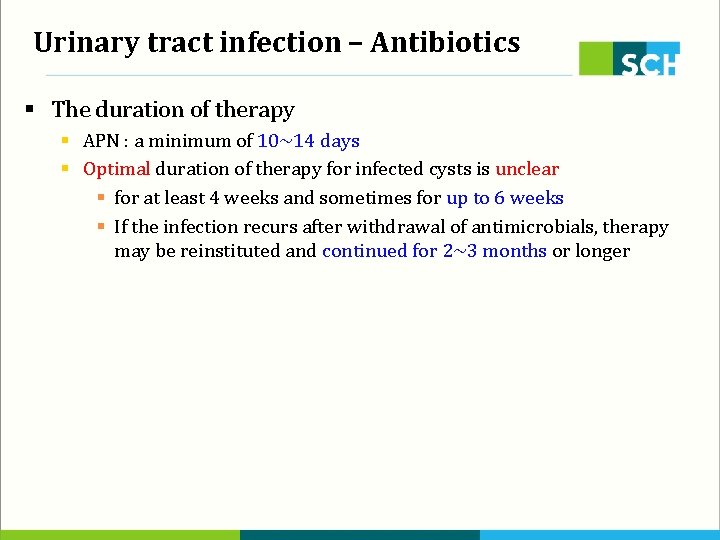
Urinary tract infection – Antibiotics § The duration of therapy § APN : a minimum of 10~14 days § Optimal duration of therapy for infected cysts is unclear § for at least 4 weeks and sometimes for up to 6 weeks § If the infection recurs after withdrawal of antimicrobials, therapy may be reinstituted and continued for 2~3 months or longer
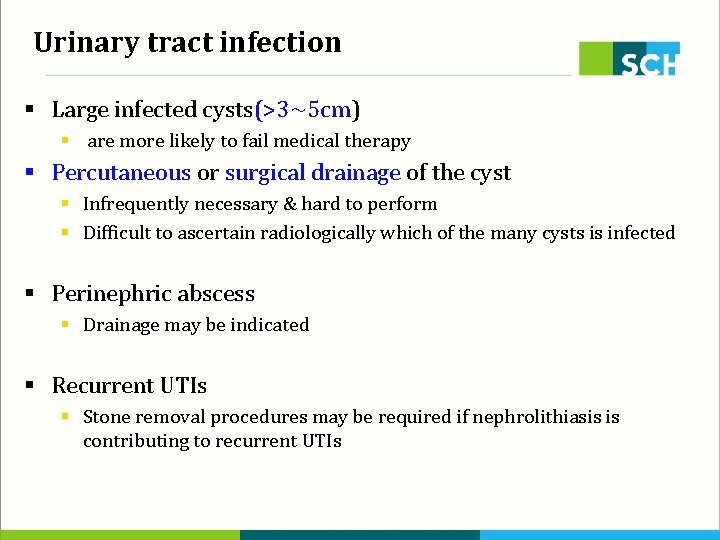
Urinary tract infection § Large infected cysts(>3~5 cm) § are more likely to fail medical therapy § Percutaneous or surgical drainage of the cyst § Infrequently necessary & hard to perform § Difficult to ascertain radiologically which of the many cysts is infected § Perinephric abscess § Drainage may be indicated § Recurrent UTIs § Stone removal procedures may be required if nephrolithiasis is contributing to recurrent UTIs
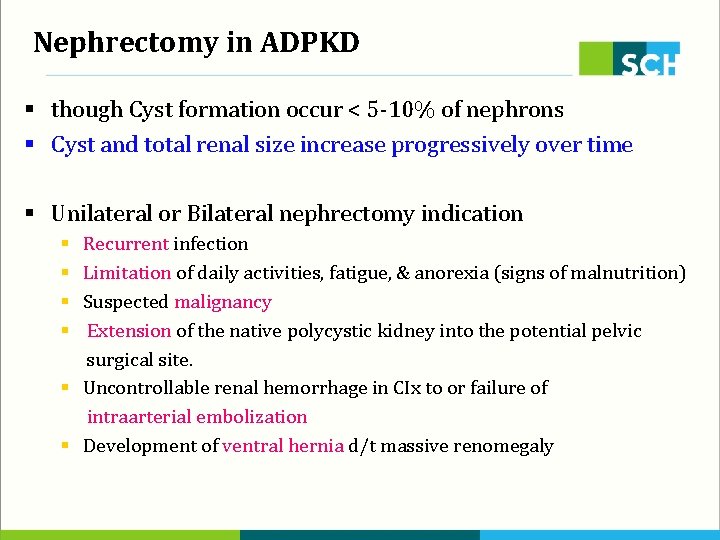
Nephrectomy in ADPKD § though Cyst formation occur < 5 -10% of nephrons § Cyst and total renal size increase progressively over time § Unilateral or Bilateral nephrectomy indication Recurrent infection Limitation of daily activities, fatigue, & anorexia (signs of malnutrition) Suspected malignancy Extension of the native polycystic kidney into the potential pelvic surgical site. § Uncontrollable renal hemorrhage in CIx to or failure of intraarterial embolization § Development of ventral hernia d/t massive renomegaly § §
 Ira pré renal renal e pós renal
Ira pré renal renal e pós renal Sindrome nefrótica
Sindrome nefrótica Mcdk
Mcdk Adpkd
Adpkd Renal corpuscle
Renal corpuscle Manifestations of hypercalcemia
Manifestations of hypercalcemia Rheumatoid arthritis extra-articular manifestations
Rheumatoid arthritis extra-articular manifestations Spirit of jealousy manifestations
Spirit of jealousy manifestations Carbimazole dose
Carbimazole dose Nail pitting
Nail pitting Chapitre 3 l'énergie et ses manifestations
Chapitre 3 l'énergie et ses manifestations Aorta zone
Aorta zone Anna neary
Anna neary Panchajani
Panchajani Glomerular filtration rate
Glomerular filtration rate Hyaline cast urine
Hyaline cast urine Signo de puño percusion renal
Signo de puño percusion renal Naphthylamine
Naphthylamine Where is water reabsorbed in the nephron
Where is water reabsorbed in the nephron