Reduction techniques and implant design moderated interactive session











- Slides: 26
Reduction techniques and implant design moderated interactive session AOTrauma Advances Course
Learning outcomes • Define indications for direct and indirect reduction • Summarize role of implants in achieving desired stability and reduction • Describe the concept of minimally invasive osteosynthesis (MIO)
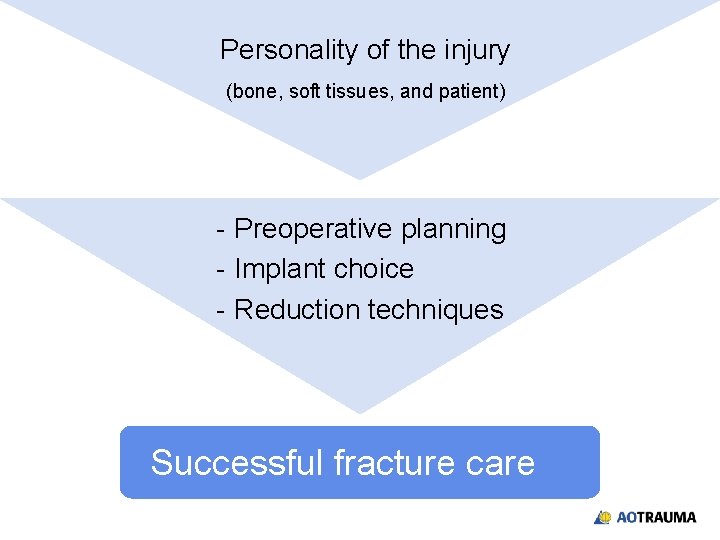
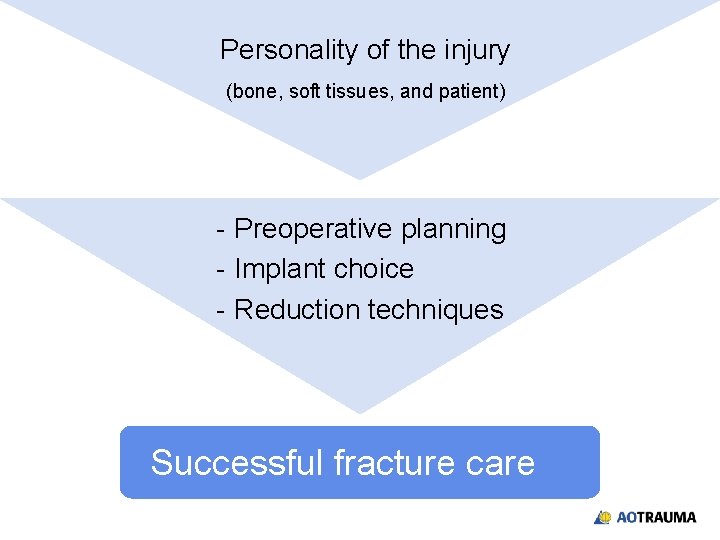
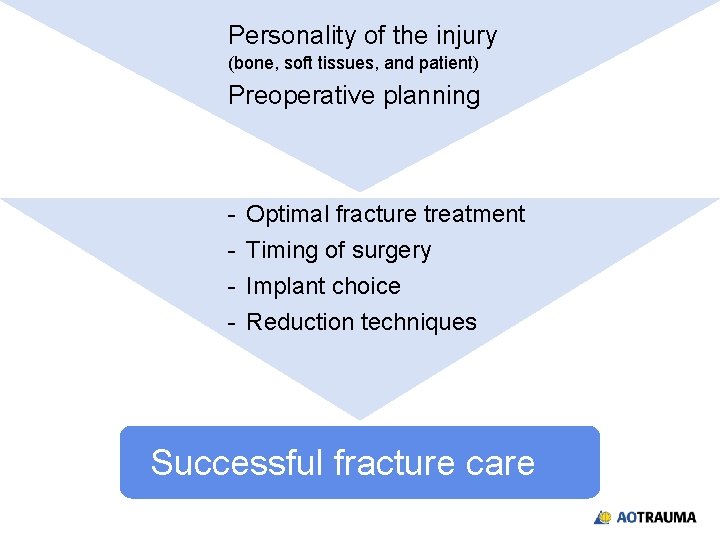
Personality of the injury (bone, soft tissues, and patient) - Preoperative planning - Implant choice - Reduction techniques Successful fracture care
Do you have access to minimally invasive technology? 1. Yes—it is in my hospital 2. No—not available 3. With special planning—it can be brought in
Do you have experience using minimally invasive technology? 1. Lots of experience—many anatomic sites 2. Limited experience—few anatomic sites 3. Tried it once or twice 4. None
Do you know the indications for locked plating? 1. I do not know any good indications for locked plating 2. I am confused about indications for locked plating 3. I generally understand the indications for locked plating, but I still have unanswered questions 4. I have a clear understanding of all indications for locked plating
Key points from lectures Direct and indirect reduction – Balance the benefits of soft-tissue preservation with the problems of ensuring a good reduction Evolution of plate design and function – The importance of locked internal fixators in the treatment of osteoporotic and metaphyseal fractures, the relationship between internal fixators and MIPO.
Key points from lectures Clinical indications for locked plating – Use of locked compression plates in special clinical circumstances and the keys for success and failure. Preoperative planning – Techniques and importance of preoperative planning.

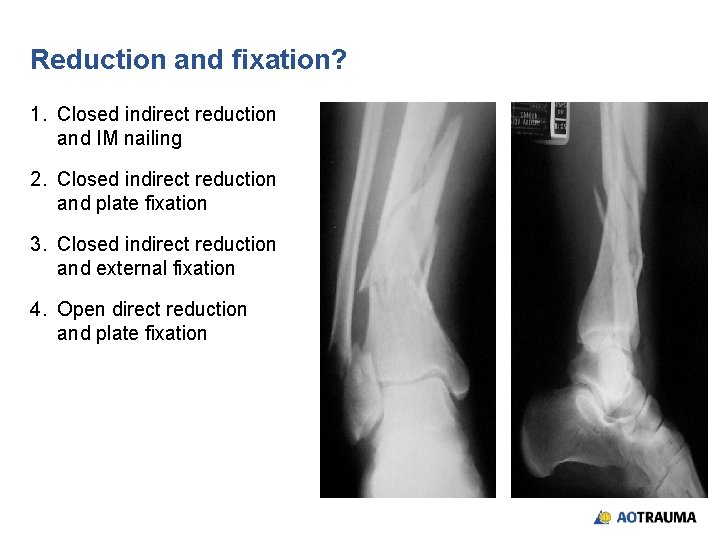
28 -year-old female, parachute accident
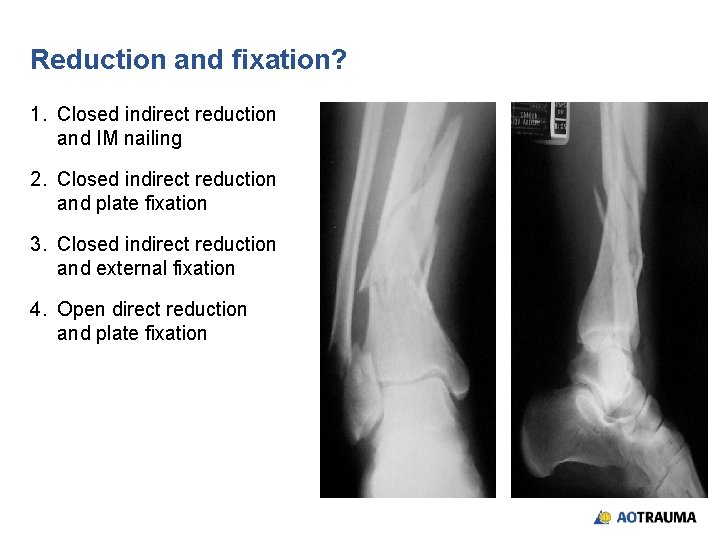
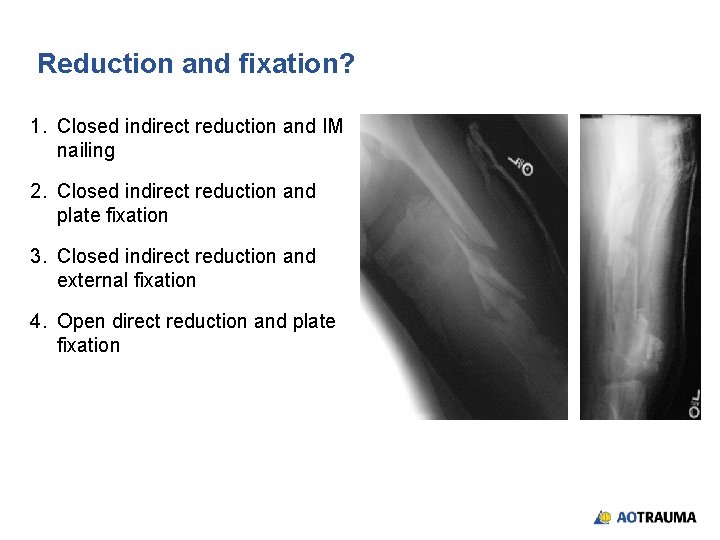
Reduction and fixation? 1. Closed indirect reduction and IM nailing 2. Closed indirect reduction and plate fixation 3. Closed indirect reduction and external fixation 4. Open direct reduction and plate fixation




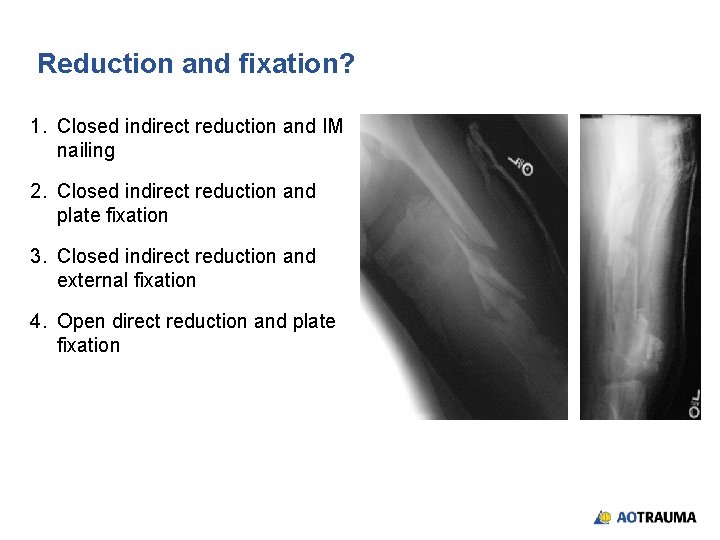
32 -year-old male, motor vehicle accident, open grade II
Reduction and fixation? 1. Closed indirect reduction and IM nailing 2. Closed indirect reduction and plate fixation 3. Closed indirect reduction and external fixation 4. Open direct reduction and plate fixation


Wound healed—what now? 1. Continue with external fixation 2. Closed reduction and retrograde nail 3. Closed reduction and locked plate 4. Open reduction and plating

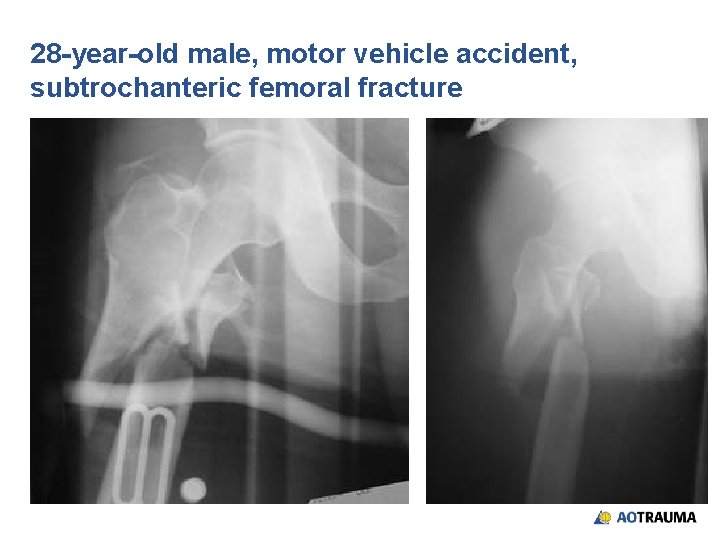
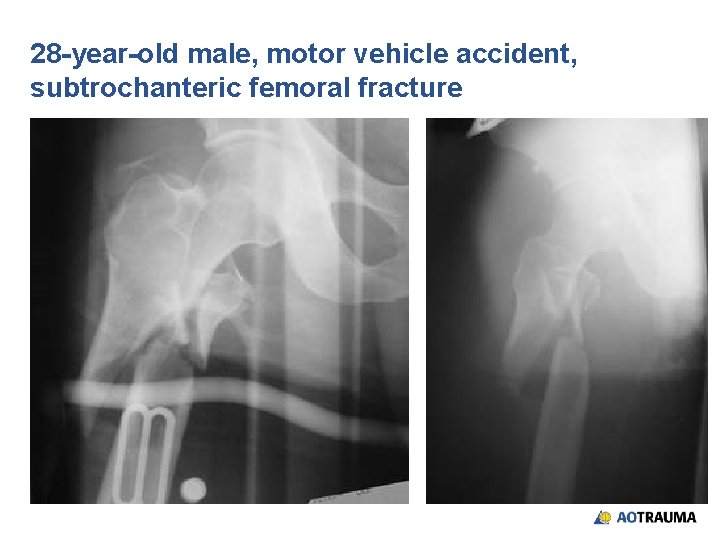
28 -year-old male, motor vehicle accident, subtrochanteric femoral fracture
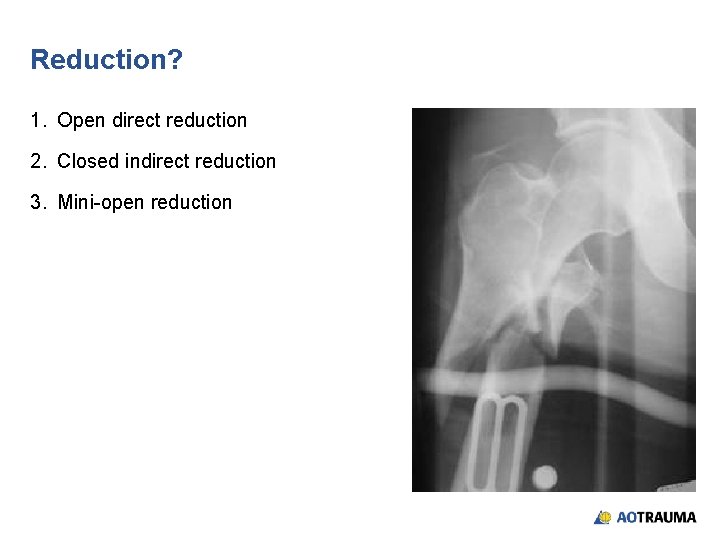
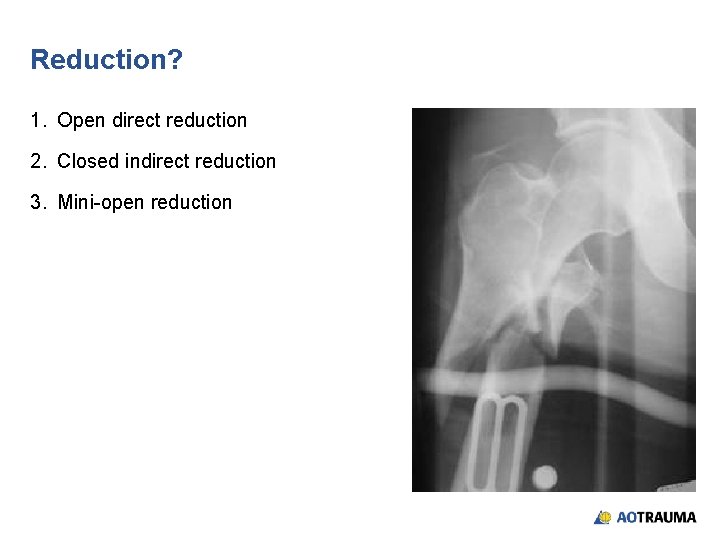
Reduction? 1. Open direct reduction 2. Closed indirect reduction 3. Mini-open reduction
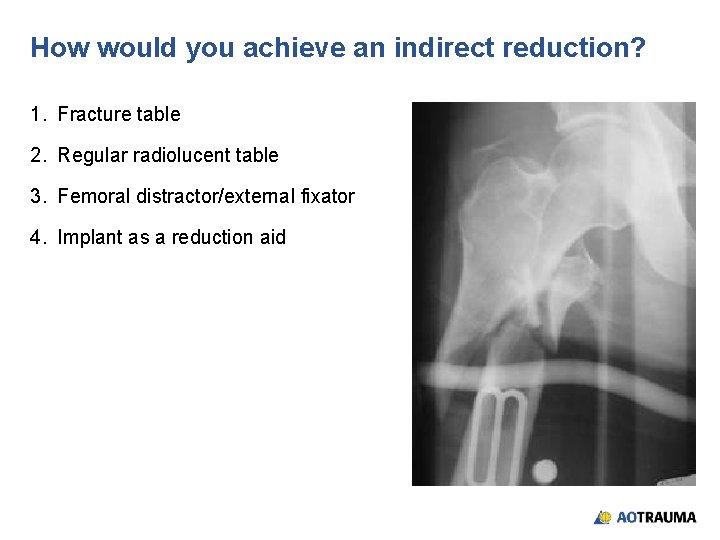
How would you achieve an indirect reduction? 1. Fracture table 2. Regular radiolucent table 3. Femoral distractor/external fixator 4. Implant as a reduction aid



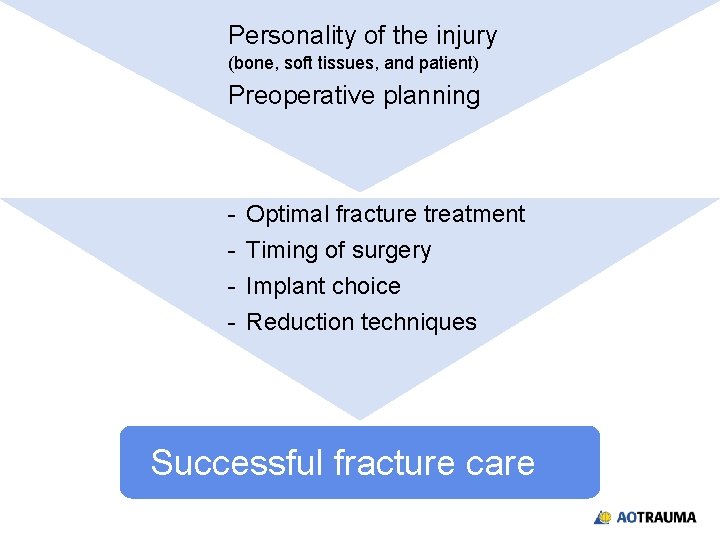
Personality of the injury (bone, soft tissues, and patient) Preoperative planning - Optimal fracture treatment Timing of surgery Implant choice Reduction techniques Successful fracture care
Summary • Direct and indirect reduction have roles in fracture care • Basic principles of plate fixation still apply • Locking head screws have specific indications: – Osteoporotic bone – Failure of fixation or around prostheses – Periarticular fixation (short end segment) • Biological fixation can be achieved with any implant • MIO is an applied concept to minimize dissection, preserve blood supply, and improve biology