Randomized Comparison of Percutaneous Coronary Intervention with SirolimusEluting

- Slides: 18
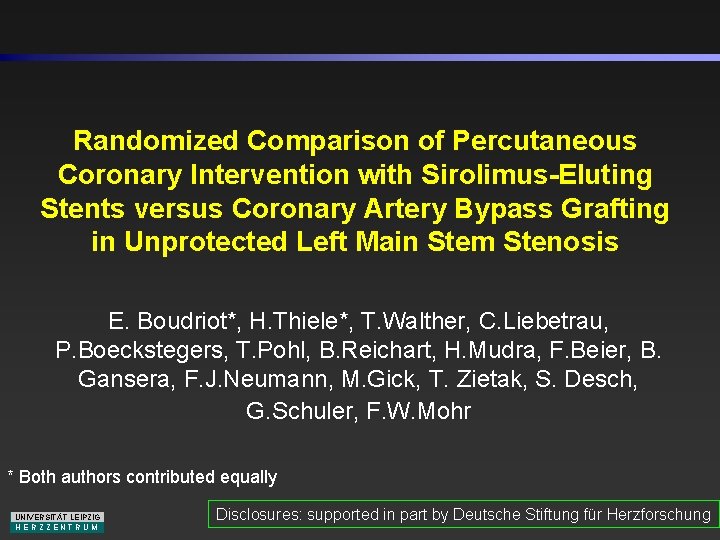
Randomized Comparison of Percutaneous Coronary Intervention with Sirolimus-Eluting Stents versus Coronary Artery Bypass Grafting in Unprotected Left Main Stem Stenosis E. Boudriot*, H. Thiele*, T. Walther, C. Liebetrau, P. Boeckstegers, T. Pohl, B. Reichart, H. Mudra, F. Beier, B. Gansera, F. J. Neumann, M. Gick, T. Zietak, S. Desch, G. Schuler, F. W. Mohr * Both authors contributed equally UNIVERSITÄT LEIPZIG HERZZENTRUM Disclosures: supported in part by Deutsche Stiftung für Herzforschung
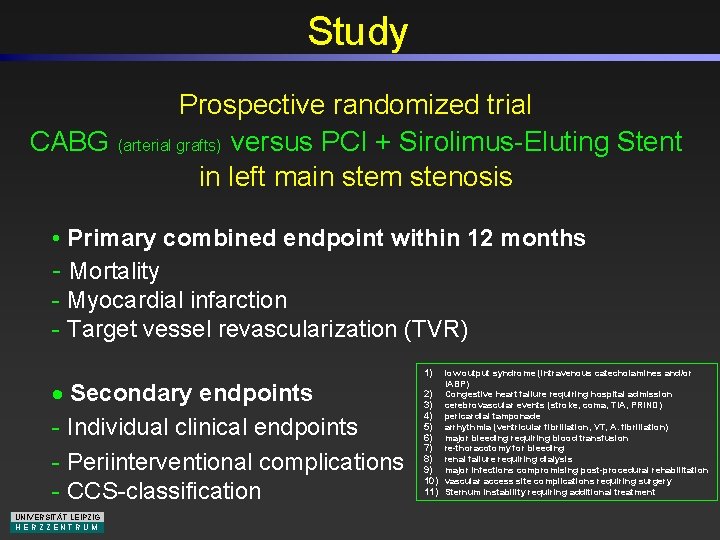
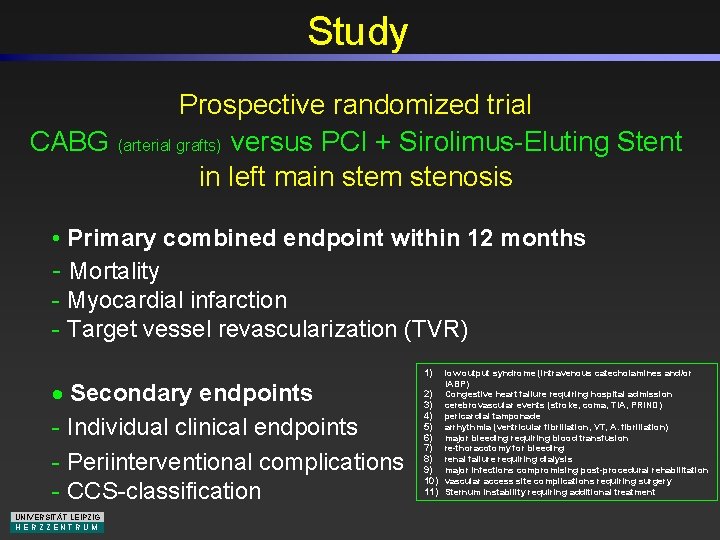
Study Prospective randomized trial CABG (arterial grafts) versus PCI + Sirolimus-Eluting Stent in left main stem stenosis • Primary combined endpoint within 12 months - Mortality - Myocardial infarction - Target vessel revascularization (TVR) · Secondary endpoints - Individual clinical endpoints - Periinterventional complications - CCS-classification UNIVERSITÄT LEIPZIG HERZZENTRUM 1) low output syndrome (intravenous catecholamines and/or IABP) 2) Congestive heart failure requiring hospital admission 3) cerebrovascular events (stroke, coma, TIA, PRIND) 4) pericardial tamponade 5) arrhythmia (ventricular fibrillation, VT, A. fibrillation) 6) major bleeding requiring blood transfusion 7) re-thoracotomy for bleeding 8) renal failure requiring dialysis 9) major infections compromising post-procedural rehabilitation 10) vascular access site complications requiring surgery 11) Sternum instability requiring additional treatment
Study Centers Universität München - Großhadern Klinikum Neuperlach München Herzzentrum Bad Krozingen Herzzentrum Leipzig UNIVERSITÄT LEIPZIG HERZZENTRUM
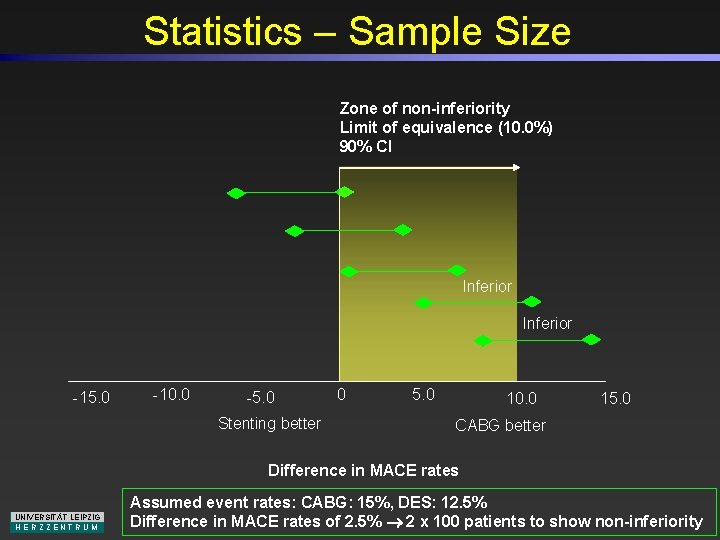
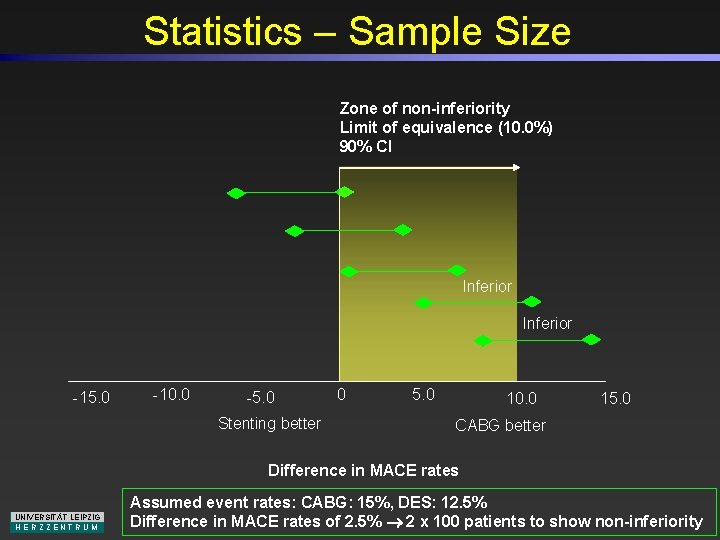
Statistics – Sample Size Zone of non-inferiority Limit of equivalence (10. 0%) 90% CI Inferior -15. 0 -10. 0 -5. 0 Stenting better 0 5. 0 10. 0 15. 0 CABG better Difference in MACE rates UNIVERSITÄT LEIPZIG HERZZENTRUM Assumed event rates: CABG: 15%, DES: 12. 5% Difference in MACE rates of 2. 5% 2 x 100 patients to show non-inferiority

Study Flow Chart 430 Patients with Unprotected Left Main Disease 229 Non-Eligible 201 Eligible 100 Assigned to PCI 101 Assigned to CABG 3 Converted to CABG 5 No Angiographic Follow-up 0 Lost to Follow-up 100 Included in Primary Analysis 100 Included in Secondary Analysis UNIVERSITÄT LEIPZIG HERZZENTRUM 20 No Angiographic Follow-up 1 Lost to Follow-up 100 Included in Primary Analysis 100 Included in Secondary Analysis 22 Infarction < 48 Hours 11 Cardiogenic Shock 8 Chronic Total Occlusion 65 Lesion Length > 30 mm 6 Non-CABG Suitable 14 Prior Cardiac Surgery 36 Age > 80 Years 21 Malignancy 27 Combined Cardiac Surgery 19 Dominant Left Circumflex 179 CABG 40 PCI 10 Conservative
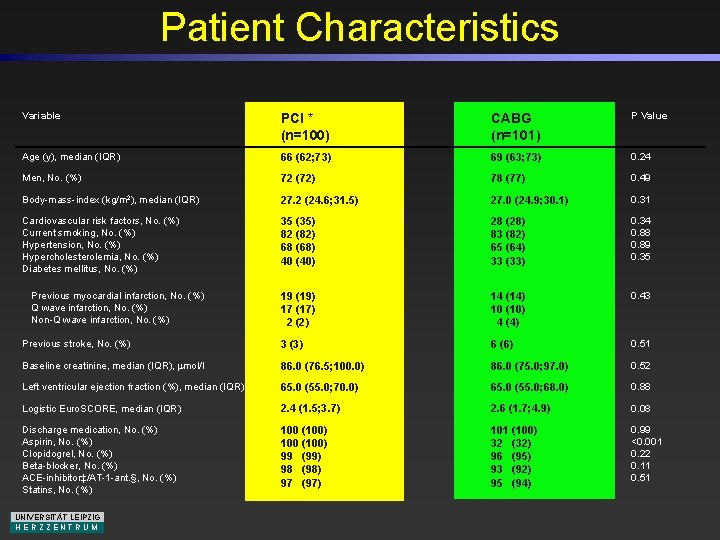
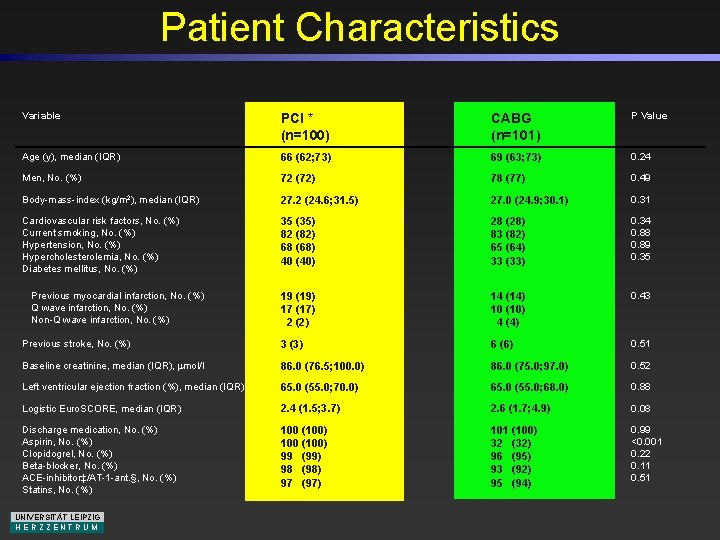
Patient Characteristics Variable PCI * (n=100) CABG (n=101) P Value Age (y), median (IQR) 66 (62; 73) 69 (63; 73) 0. 24 Men, No. (%) 72 (72) 78 (77) 0. 49 Body-mass-index (kg/m 2), median (IQR) 27. 2 (24. 6; 31. 5) 27. 0 (24. 9; 30. 1) 0. 31 Cardiovascular risk factors, No. (%) Current smoking, No. (%) Hypertension, No. (%) Hypercholesterolemia, No. (%) Diabetes mellitus, No. (%) 35 (35) 82 (82) 68 (68) 40 (40) 28 (28) 83 (82) 65 (64) 33 (33) 0. 34 0. 88 0. 89 0. 35 19 (19) 17 (17) 2 (2) 14 (14) 10 (10) 4 (4) 0. 43 Previous stroke, No. (%) 3 (3) 6 (6) 0. 51 Baseline creatinine, median (IQR), mol/l 86. 0 (76. 5; 100. 0) 86. 0 (75. 0; 97. 0) 0. 52 Left ventricular ejection fraction (%), median (IQR) 65. 0 (55. 0; 70. 0) 65. 0 (55. 0; 68. 0) 0. 88 Logistic Euro. SCORE, median (IQR) 2. 4 (1. 5; 3. 7) 2. 6 (1. 7; 4. 9) 0. 08 Discharge medication, No. (%) Aspirin, No. (%) Clopidogrel, No. (%) Beta-blocker, No. (%) ACE-inhibitor‡/AT-1 -ant. §, No. (%) Statins, No. (%) 100 (100) 99 (99) 98 (98) 97 (97) 101 (100) 32 (32) 96 (95) 93 (92) 95 (94) 0. 99 <0. 001 0. 22 0. 11 0. 51 Previous myocardial infarction, No. (%) Q wave infarction, No. (%) Non-Q wave infarction, No. (%) UNIVERSITÄT LEIPZIG HERZZENTRUM
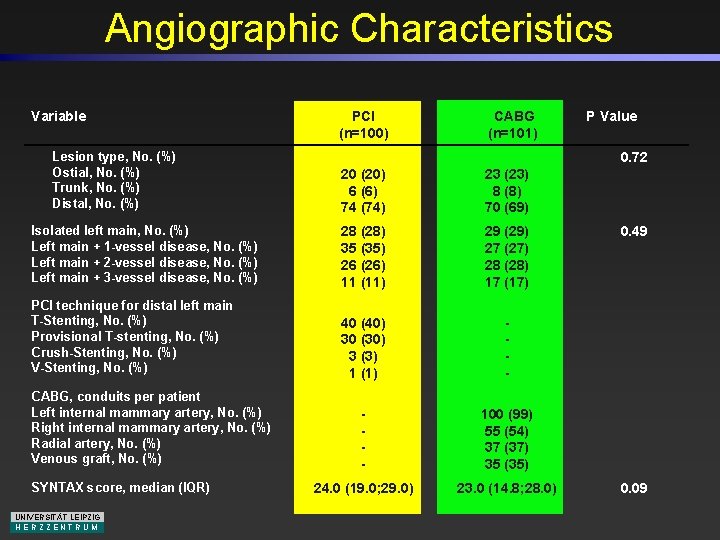
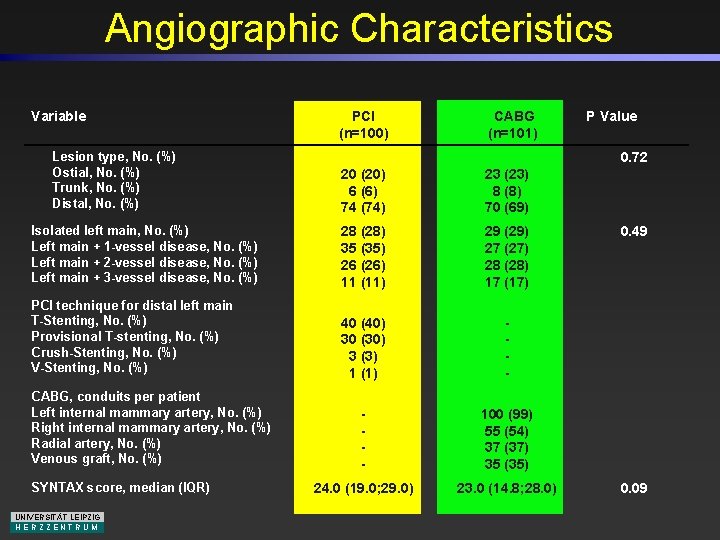
Angiographic Characteristics Variable Lesion type, No. (%) Ostial, No. (%) Trunk, No. (%) Distal, No. (%) PCI (n=100) CABG (n=101) 0. 72 20 (20) 6 (6) 74 (74) 23 (23) 8 (8) 70 (69) Isolated left main, No. (%) Left main + 1 -vessel disease, No. (%) Left main + 2 -vessel disease, No. (%) Left main + 3 -vessel disease, No. (%) 28 (28) 35 (35) 26 (26) 11 (11) 29 (29) 27 (27) 28 (28) 17 (17) PCI technique for distal left main T-Stenting, No. (%) Provisional T-stenting, No. (%) Crush-Stenting, No. (%) V-Stenting, No. (%) 40 (40) 30 (30) 3 (3) 1 (1) - - 100 (99) 55 (54) 37 (37) 35 (35) 24. 0 (19. 0; 29. 0) 23. 0 (14. 8; 28. 0) CABG, conduits per patient Left internal mammary artery, No. (%) Right internal mammary artery, No. (%) Radial artery, No. (%) Venous graft, No. (%) SYNTAX score, median (IQR) UNIVERSITÄT LEIPZIG HERZZENTRUM P Value 0. 49 0. 09
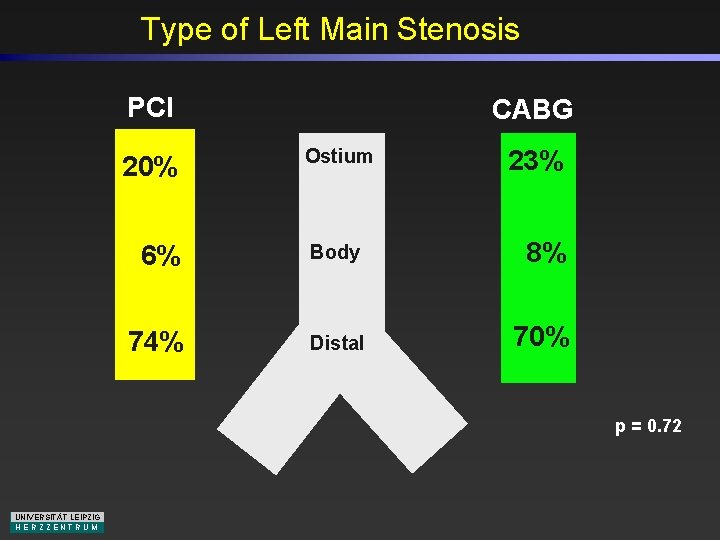
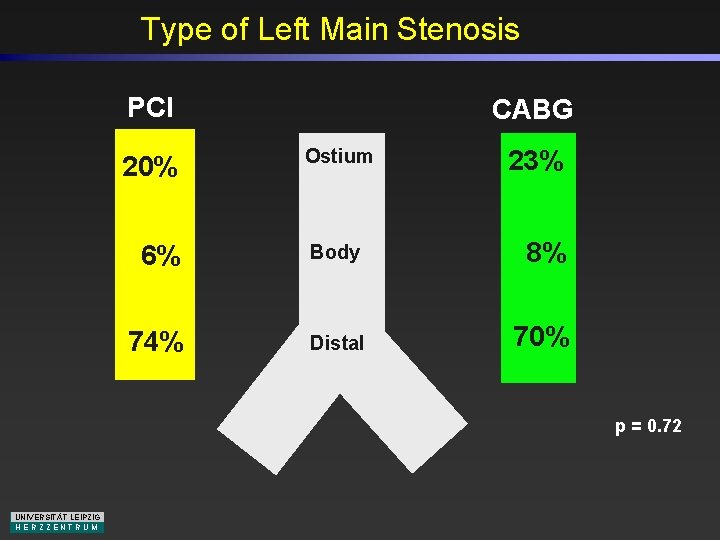
Type of Left Main Stenosis PCI 20% CABG Ostium 23% 6% Body 8% 74% Distal 70% p = 0. 72 UNIVERSITÄT LEIPZIG HERZZENTRUM
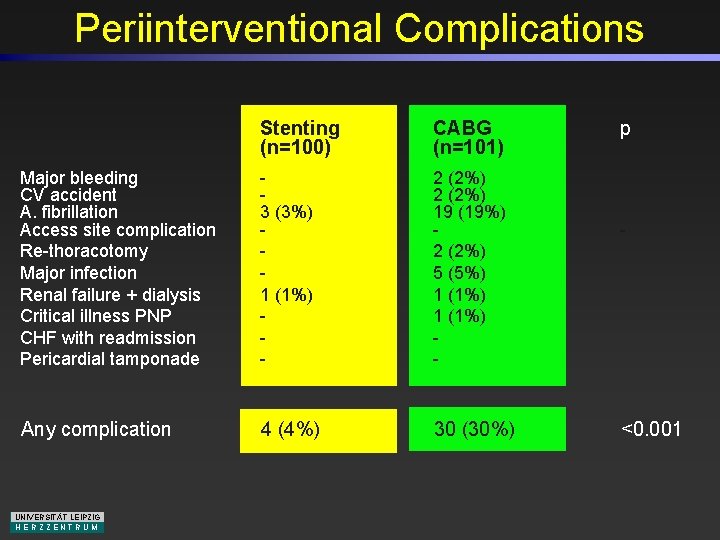
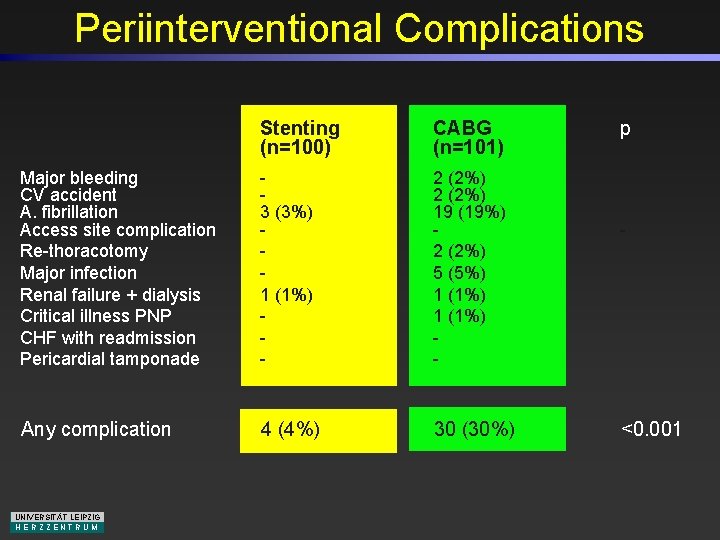
Periinterventional Complications Stenting (n=100) CABG (n=101) Major bleeding CV accident A. fibrillation Access site complication Re-thoracotomy Major infection Renal failure + dialysis Critical illness PNP CHF with readmission Pericardial tamponade 3 (3%) 1 (1%) - 2 (2%) 19 (19%) 2 (2%) 5 (5%) 1 (1%) - Any complication 4 (4%) 30 (30%) UNIVERSITÄT LEIPZIG HERZZENTRUM p - <0. 001
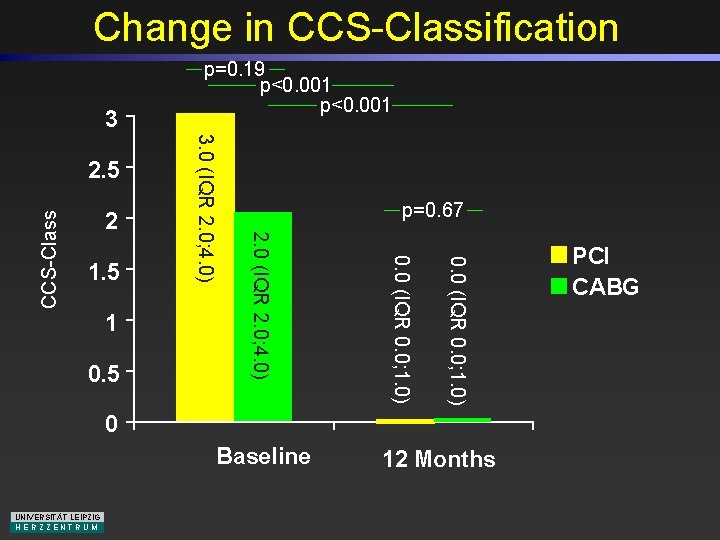
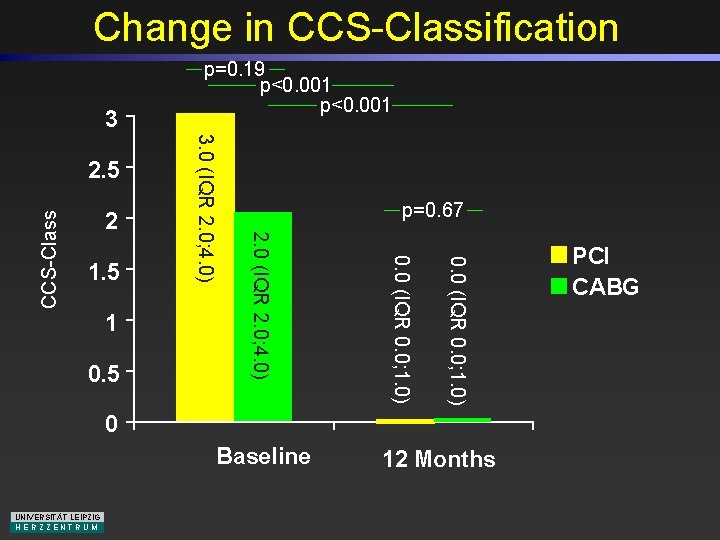
Change in CCS-Classification 3 CCS-Class 0. 5 0. 0 (IQR 0. 0; 1. 0) 1. 5 p=0. 67 2. 0 (IQR 2. 0; 4. 0) 2 3. 0 (IQR 2. 0; 4. 0) 2. 5 p=0. 19 p<0. 001 0 Baseline UNIVERSITÄT LEIPZIG HERZZENTRUM 12 Months PCI CABG
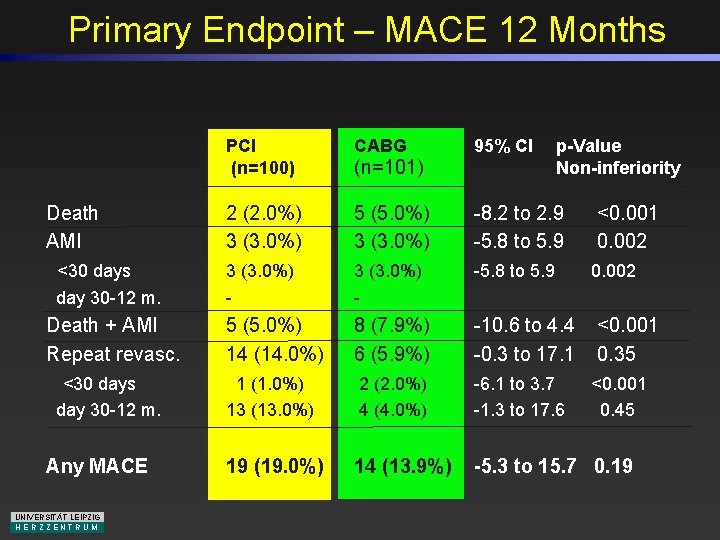
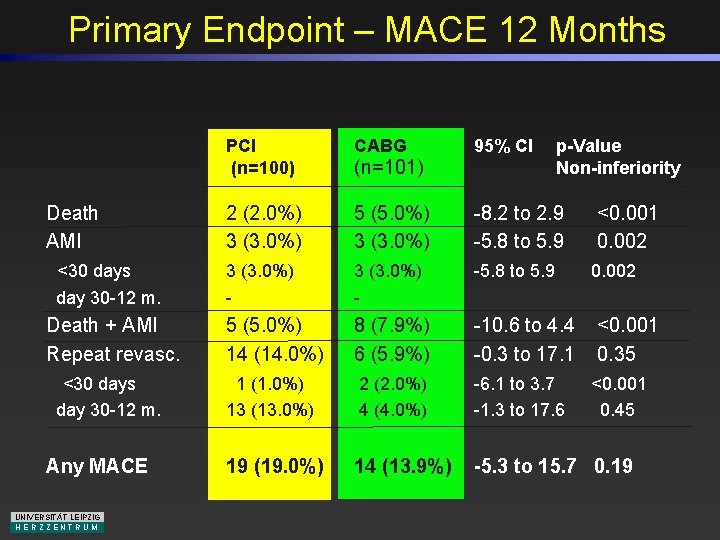
Primary Endpoint – MACE 12 Months PCI (n=100) CABG 2 (2. 0%) 3 (3. 0%) 5 (5. 0%) 3 (3. 0%) -8. 2 to 2. 9 -5. 8 to 5. 9 3 (3. 0%) - -5. 8 to 5. 9 Death + AMI Repeat revasc. 5 (5. 0%) 14 (14. 0%) 8 (7. 9%) 6 (5. 9%) -10. 6 to 4. 4 -0. 3 to 17. 1 <30 days day 30 -12 m. 1 (1. 0%) 13 (13. 0%) 2 (2. 0%) 4 (4. 0%) -6. 1 to 3. 7 -1. 3 to 17. 6 19 (19. 0%) 14 (13. 9%) -5. 3 to 15. 7 0. 19 Death AMI <30 days day 30 -12 m. Any MACE UNIVERSITÄT LEIPZIG HERZZENTRUM 95% CI (n=101) p-Value Non-inferiority <0. 001 0. 002 <0. 001 0. 35 <0. 001 0. 45
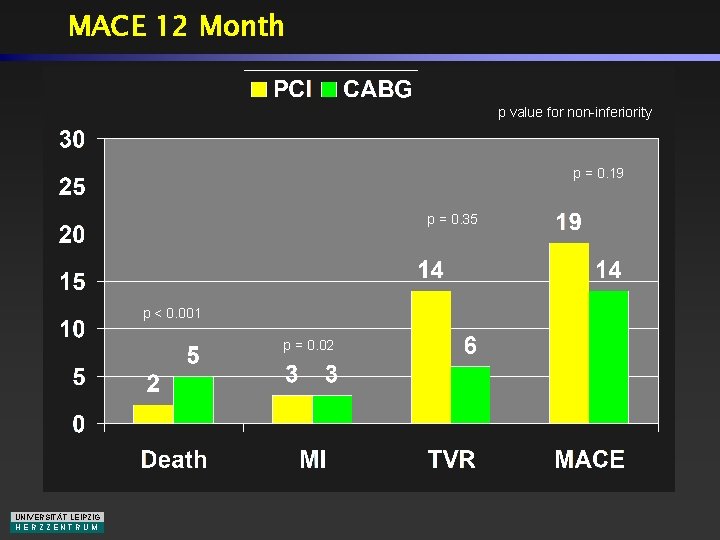
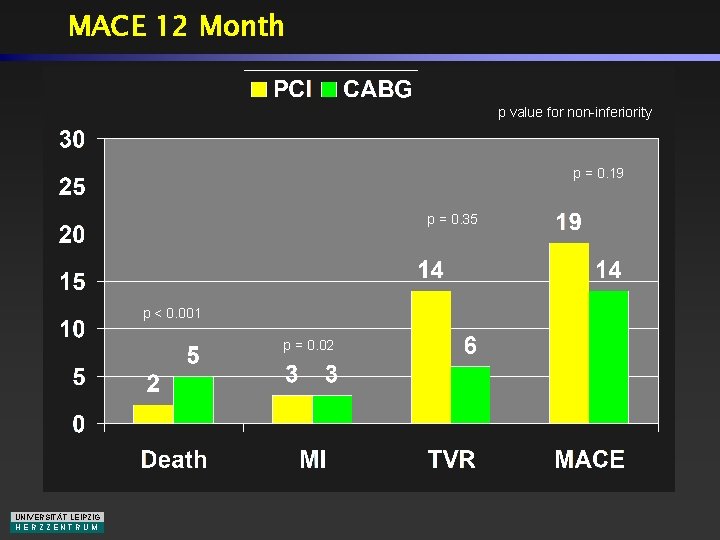
MACE 12 Month p value for non-inferiority p = 0. 19 p = 0. 35 p < 0. 001 p = 0. 02 UNIVERSITÄT LEIPZIG HERZZENTRUM
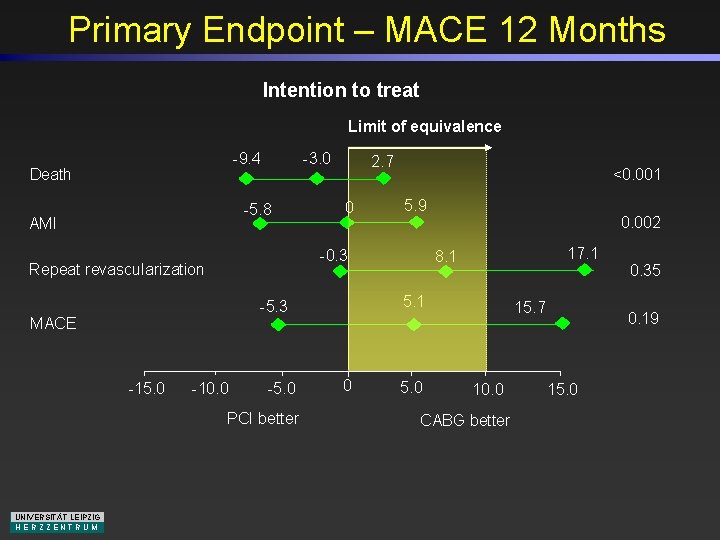
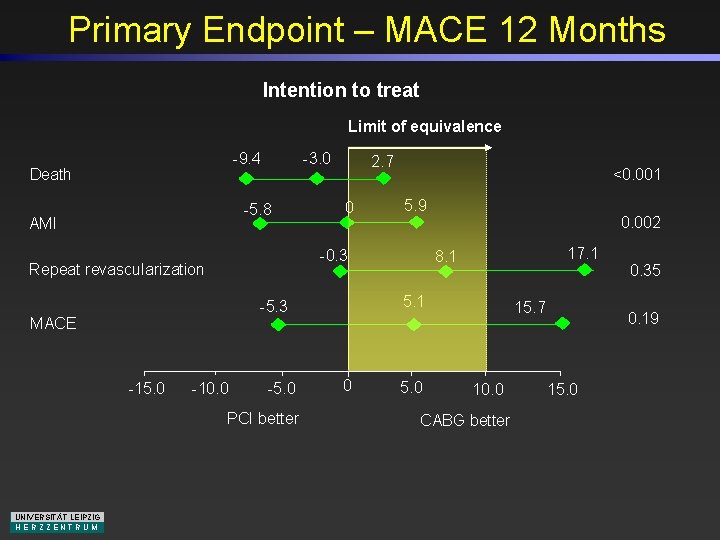
Primary Endpoint – MACE 12 Months Intention to treat Limit of equivalence -9. 4 Death -3. 0 -5. 8 AMI 0 5. 9 MACE -10. 0 -5. 0 PCI better 0. 002 17. 1 8. 1 5. 1 -5. 3 -15. 0 <0. 001 -0. 3 Repeat revascularization UNIVERSITÄT LEIPZIG HERZZENTRUM 2. 7 0 5. 0 15. 7 10. 0 CABG better 0. 35 0. 19 15. 0
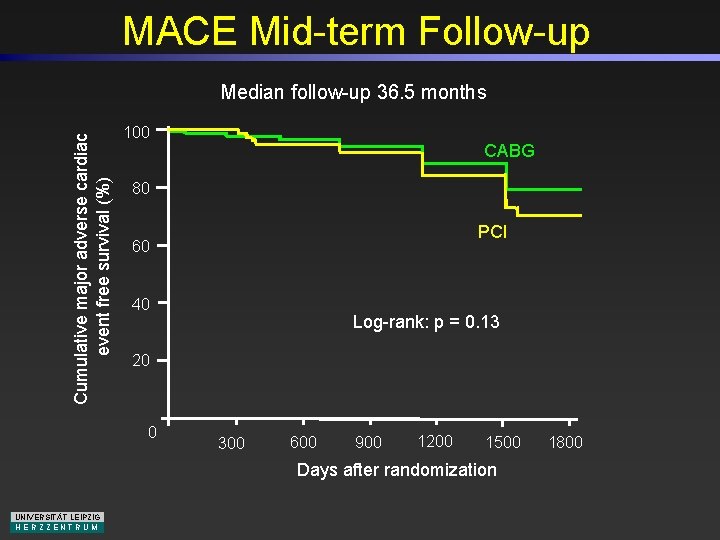
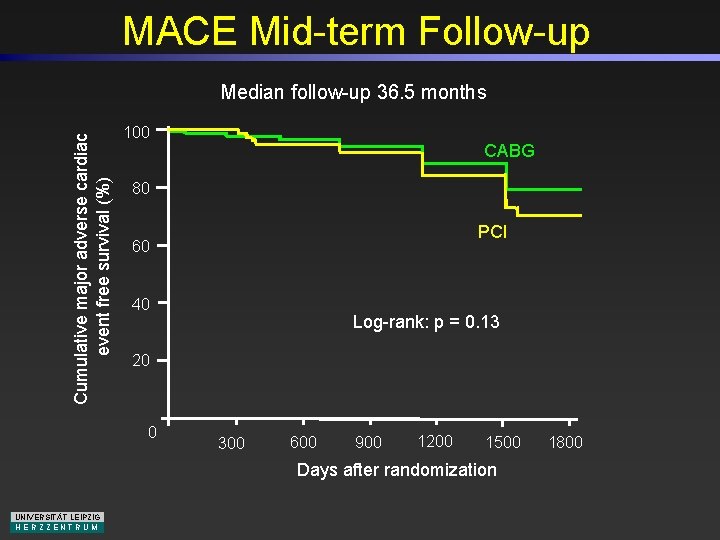
MACE Mid-term Follow-up Cumulative major adverse cardiac event free survival (%) Median follow-up 36. 5 months 100 CABG 80 PCI 60 40 Log-rank: p = 0. 13 20 0 300 600 900 1200 1500 Days after randomization UNIVERSITÄT LEIPZIG HERZZENTRUM 1800
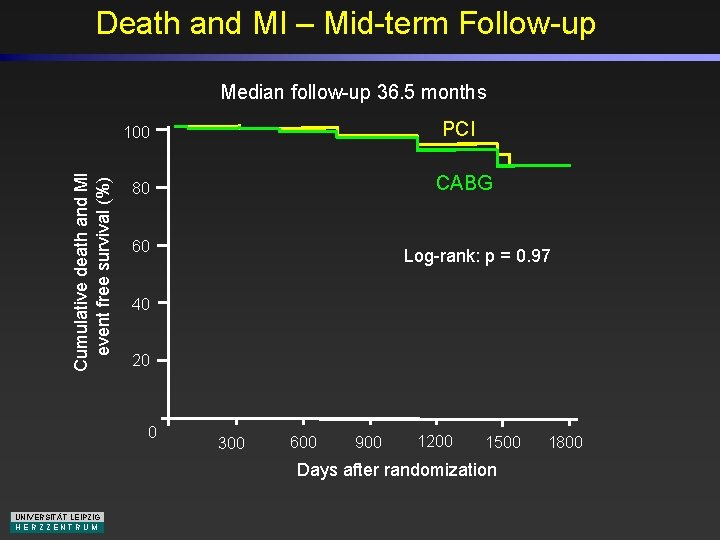
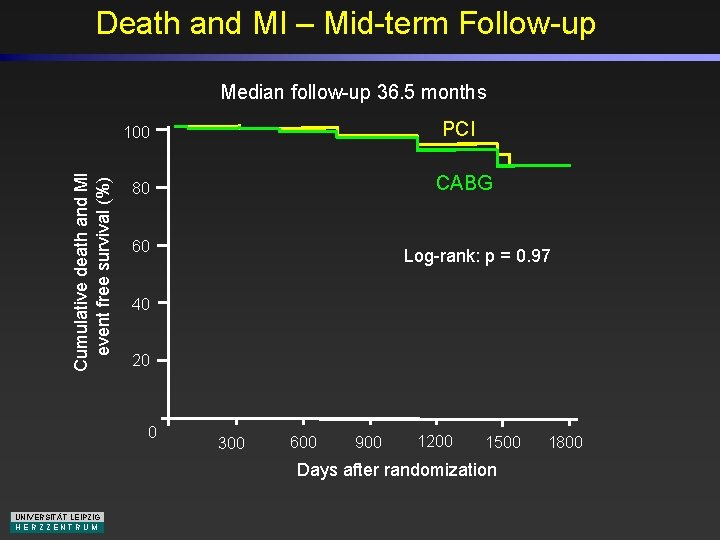
Death and MI – Mid-term Follow-up Median follow-up 36. 5 months PCI Cumulative death and MI event free survival (%) 100 CABG 80 60 Log-rank: p = 0. 97 40 20 0 300 600 900 1200 1500 Days after randomization UNIVERSITÄT LEIPZIG HERZZENTRUM 1800
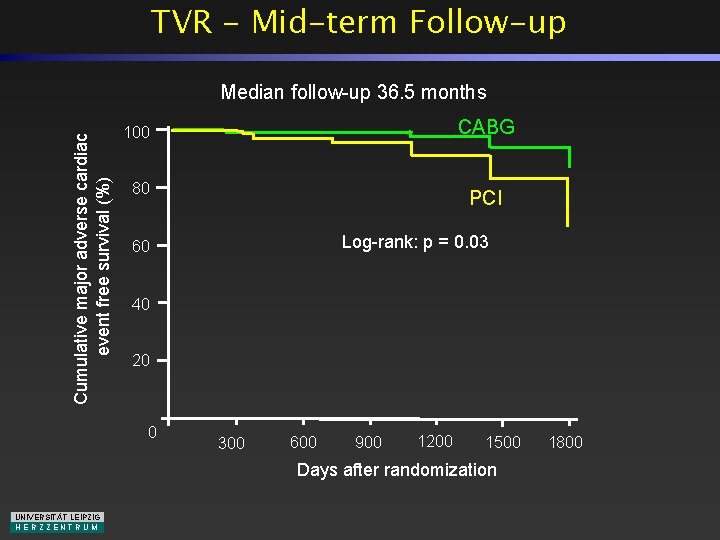
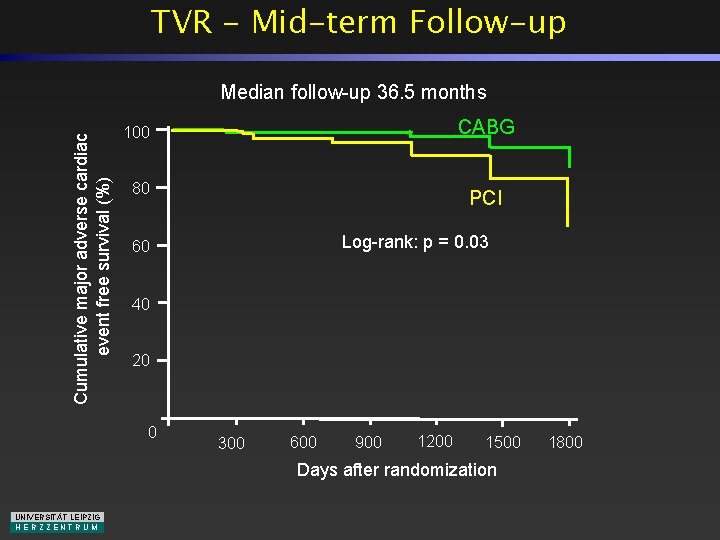
TVR - Mid-term Follow-up Cumulative major adverse cardiac event free survival (%) Median follow-up 36. 5 months CABG 100 80 PCI Log-rank: p = 0. 03 60 40 20 0 300 600 900 1200 1500 Days after randomization UNIVERSITÄT LEIPZIG HERZZENTRUM 1800
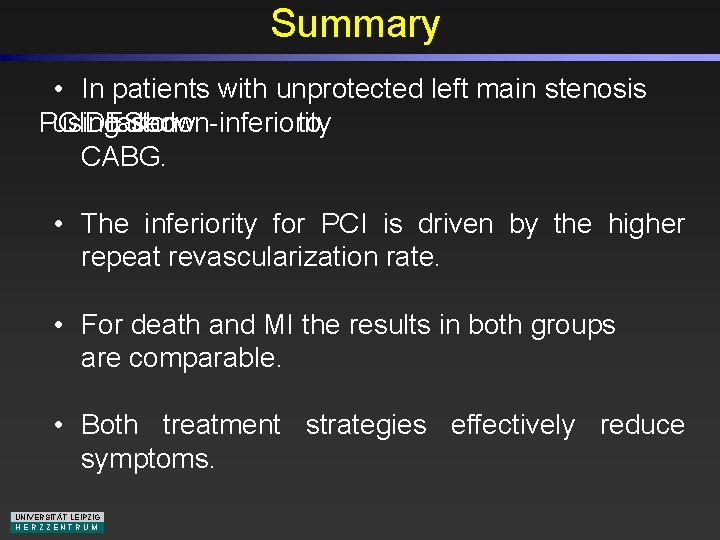
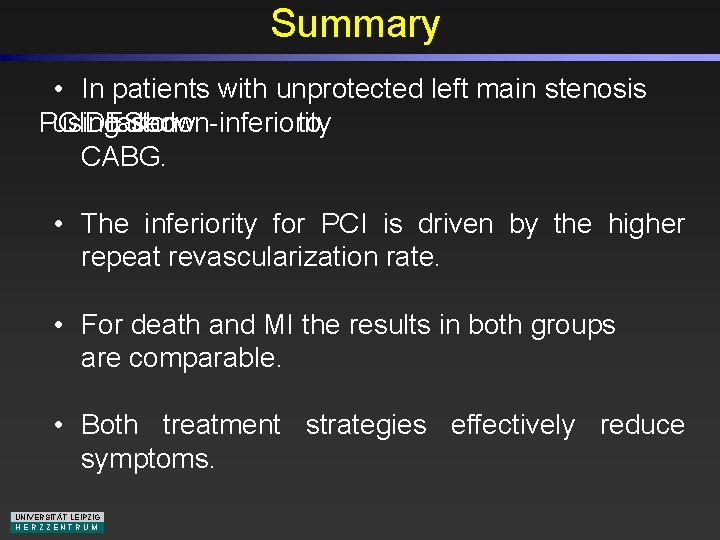
Summary • In patients with unprotected left main stenosis PCI using DES failed show tonon-inferiority to CABG. • The inferiority for PCI is driven by the higher repeat revascularization rate. • For death and MI the results in both groups are comparable. • Both treatment strategies effectively reduce symptoms. UNIVERSITÄT LEIPZIG HERZZENTRUM
Conclusions In highly-experienced centers the decision making process on how to treat unprotected left main disease should therefore be based on an interdisciplinary approach taking into account the - individual success, - periprocedural risk - bypass graft occlusion risk - potential restenosis rate based on the morphology of the underlying lesion and patient comorbidities. UNIVERSITÄT LEIPZIG HERZZENTRUM
 Percutaneous image-guided lumbar decompression
Percutaneous image-guided lumbar decompression Common bile duct diameter
Common bile duct diameter Intrapericardial colon
Intrapericardial colon Ellis curve
Ellis curve Percutaneous transhepatic cholangiography
Percutaneous transhepatic cholangiography Percutaneous umbilical blood sampling
Percutaneous umbilical blood sampling Pico patient intervention comparison outcome
Pico patient intervention comparison outcome Pico patient intervention comparison outcome
Pico patient intervention comparison outcome Limit comparison test and direct comparison test
Limit comparison test and direct comparison test Cardiac plexus
Cardiac plexus Dr eter
Dr eter Coronary heart disease
Coronary heart disease Coronary ligament
Coronary ligament Mesa coronary calcium score
Mesa coronary calcium score Aortic sinus
Aortic sinus Ligamentum arteriosum
Ligamentum arteriosum Coronary personality
Coronary personality Coronary circulation of heart
Coronary circulation of heart Pk papyrus covered coronary stent system
Pk papyrus covered coronary stent system