Radiological Category Neuroradiology Principal Modality 1 MRI Principal





- Slides: 22

Radiological Category: Neuroradiology Principal Modality (1): MRI Principal Modality (2): None Case Report # 0943 Submitted by: Miles Foltermann, MD Faculty reviewer: Scott Serlin, MD Date accepted: January 13, 2013
Case History CC: “Weakness. ” HPI: The patient is a 7 -year-old Hispanic girl who presents with generalized weakness. According to her father, she was in good health until approximately 2 months before presentation, when she started becoming lethargic and sleeping more than usual. The patient was able to move all extremities at that time and continued normal physical activities. Approximately 2 weeks prior to presentation, she experienced weakness so severe, she was unable to walk and had great difficulty using her upper extremities. According to her father, the symptoms appeared to be “ascending. ” The patient received treatment at that time (specifics withheld) and was transferred to a rehabilitation facility. At the facility, her weakness progressed, and she developed back pain and a bilateral hand tremor that was worse at rest. These symptoms prompted her to present to the hospital again for a higher level of care. • The patient has idiopathic hypertension. No other relevant history.
Case History Focused Physical Examination: Temp 97. 8, HR 80, BP 137/89, RR 21, s. PO 2 100% on room air. Neuro: Awake, alert, oriented x 3, appropriate speech. Strength in lower extremities 1/5 bilaterally, strength in upper extremities 4/5 bilaterally. Keeps knees extended, pain with flexion. Keeps ankles extended, pain with flexion. Unable to wiggle toes. Unable to lift head off bed, but able to move neck in all directions. Sensation intact. Unable to elicit refluxes in upper and lower extremities. No clonus. Tremor of the hands.
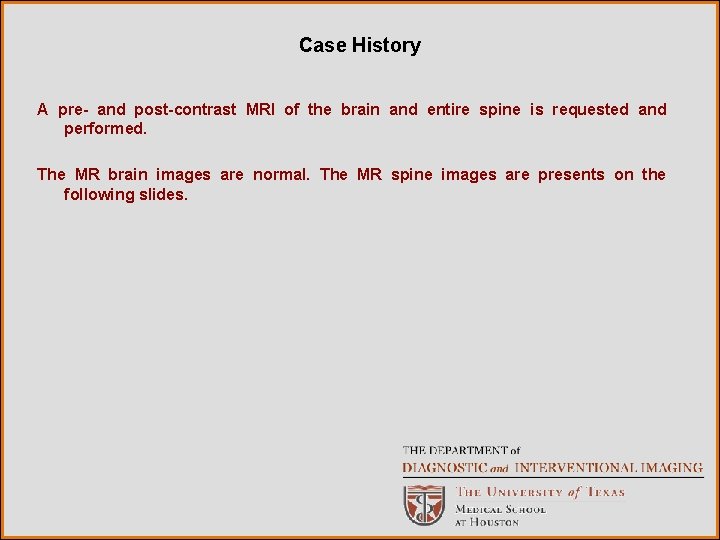
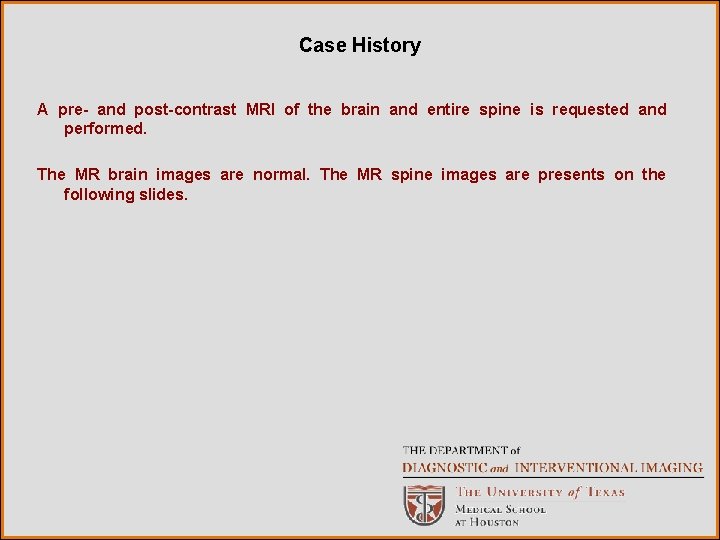
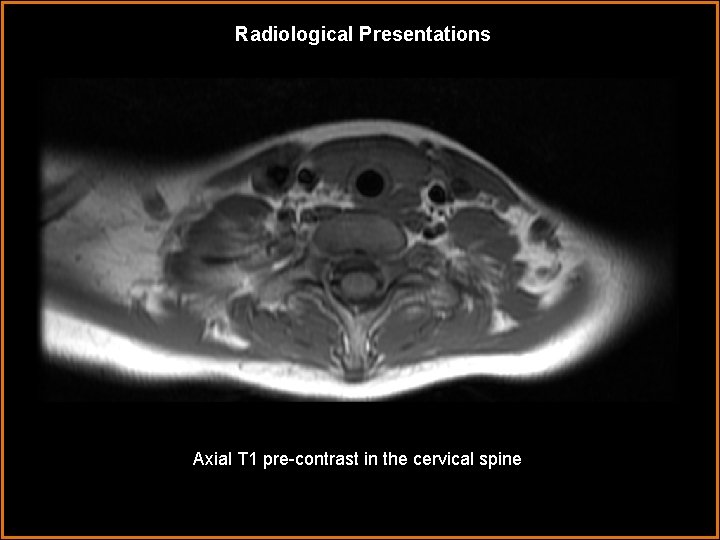
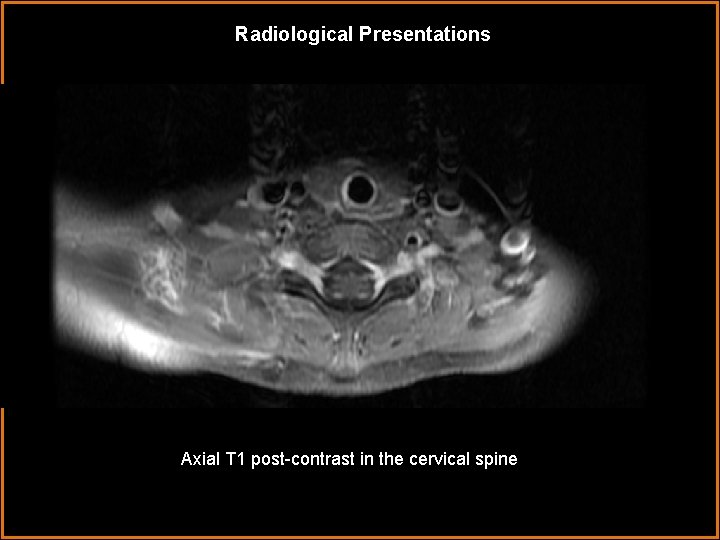
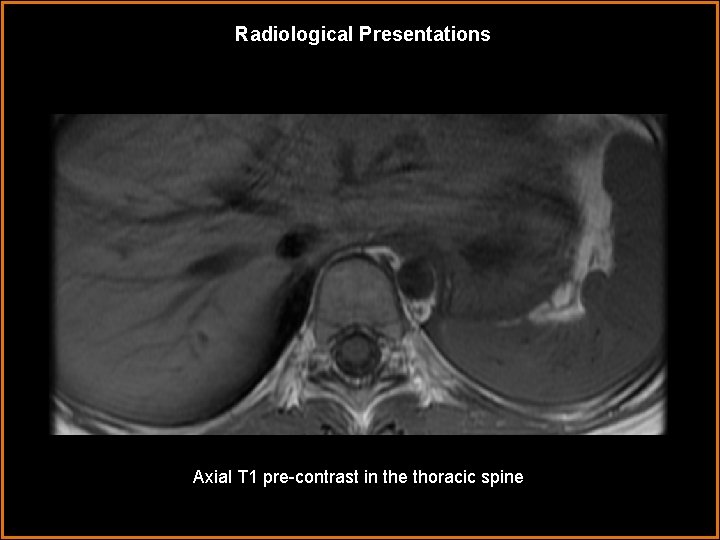
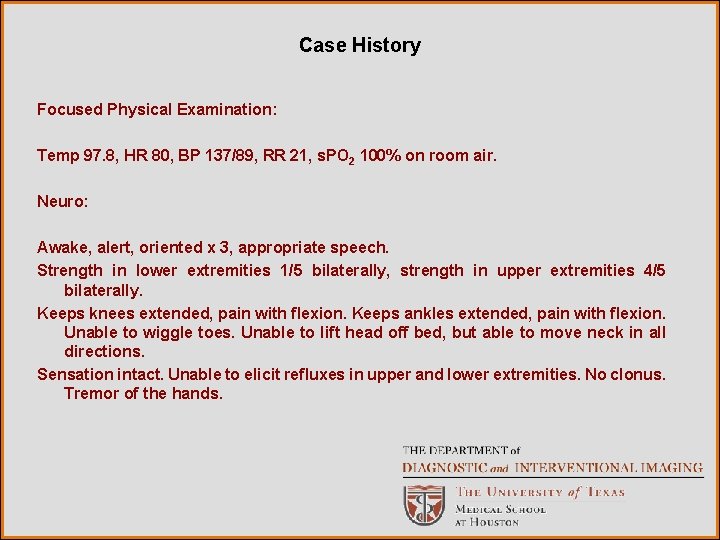
Case History A pre- and post-contrast MRI of the brain and entire spine is requested and performed. The MR brain images are normal. The MR spine images are presents on the following slides.
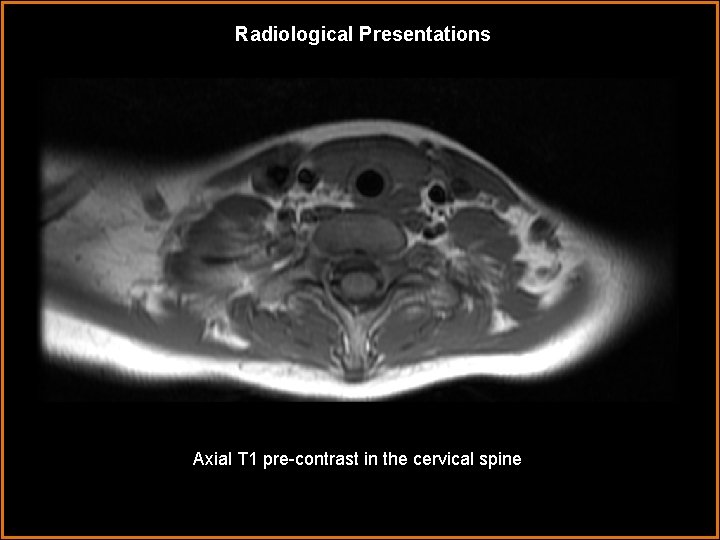
Radiological Presentations Axial T 1 pre-contrast in the cervical spine
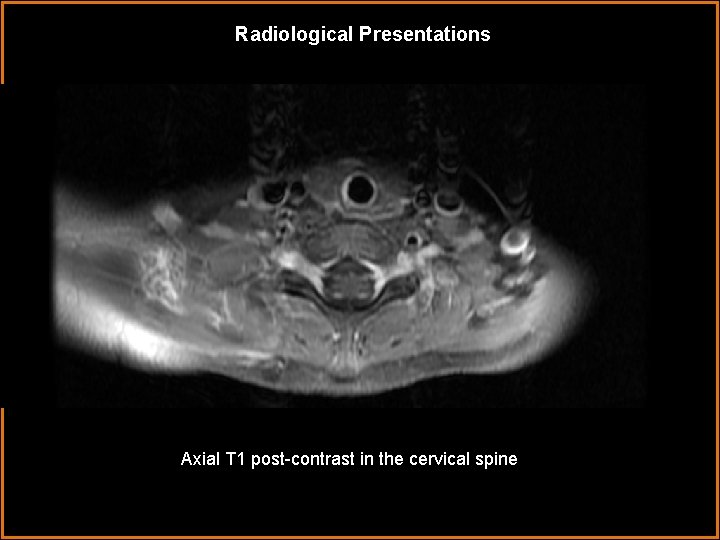
Radiological Presentations Axial T 1 post-contrast in the cervical spine
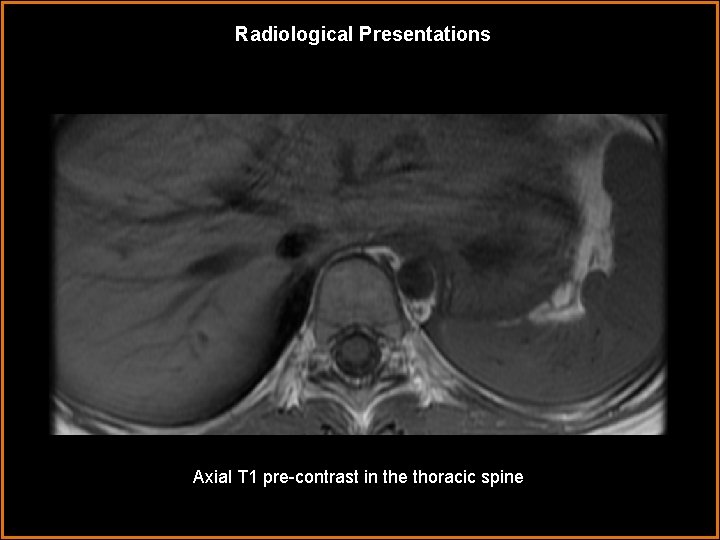
Radiological Presentations Axial T 1 pre-contrast in the thoracic spine
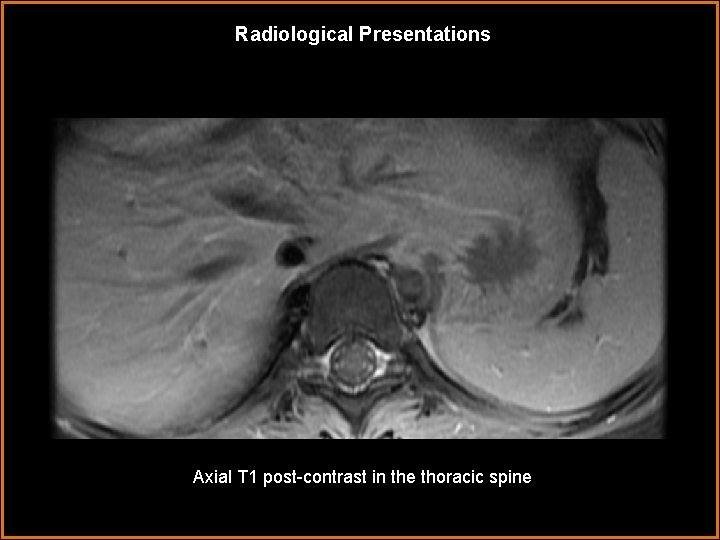
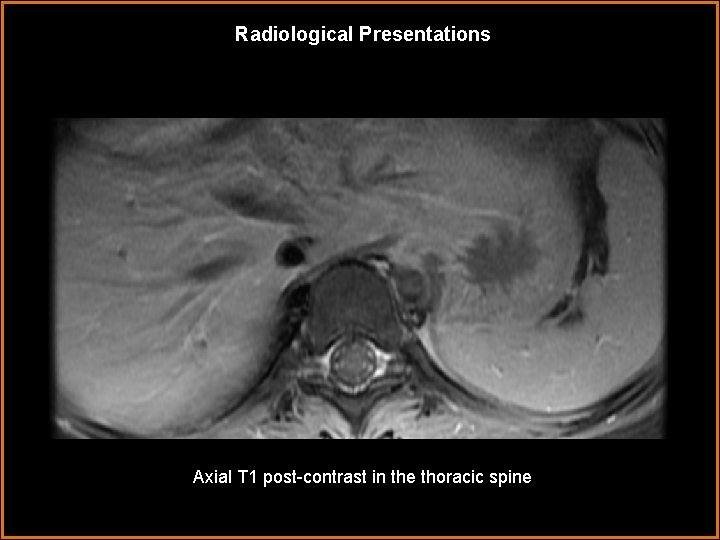
Radiological Presentations Axial T 1 post-contrast in the thoracic spine
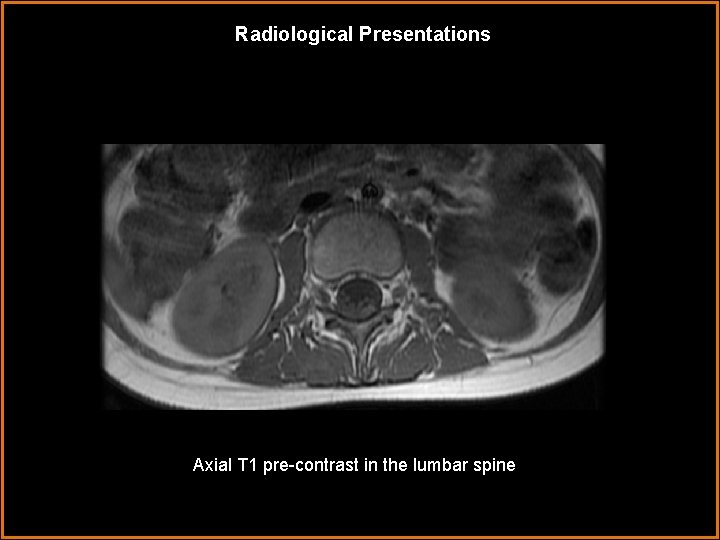
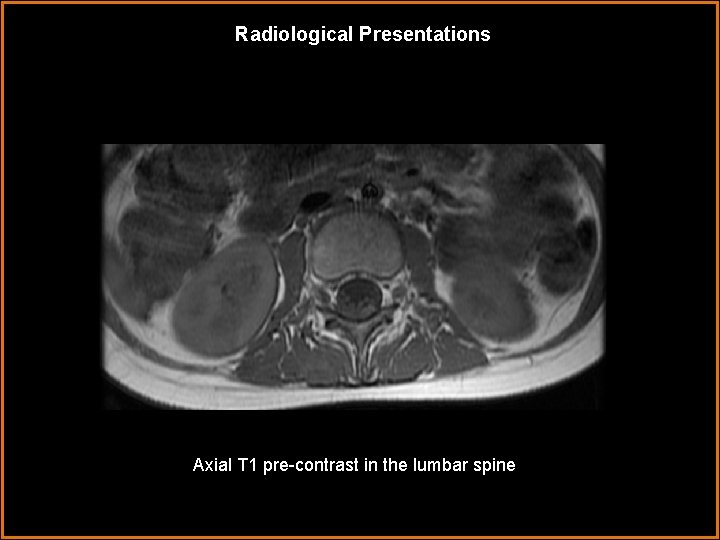
Radiological Presentations Axial T 1 pre-contrast in the lumbar spine =

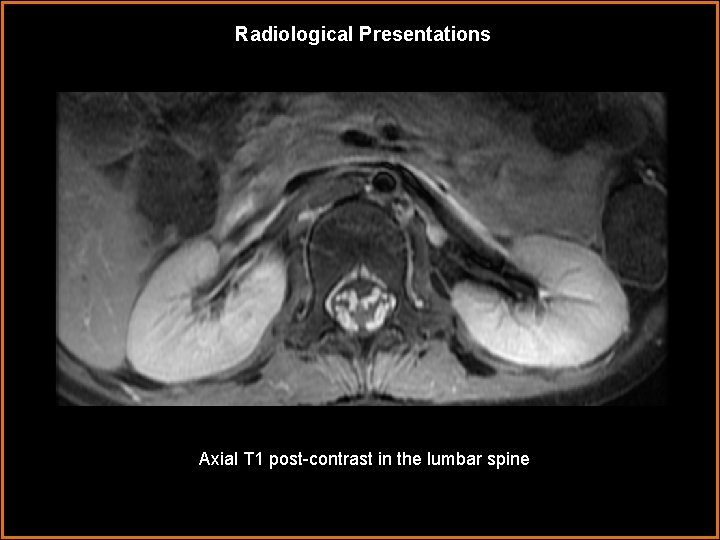
Radiological Presentations Axial T 1 post-contrast in the lumbar spine

Radiological Presentations Axial T 1 pre-contrast in the lumbar spine
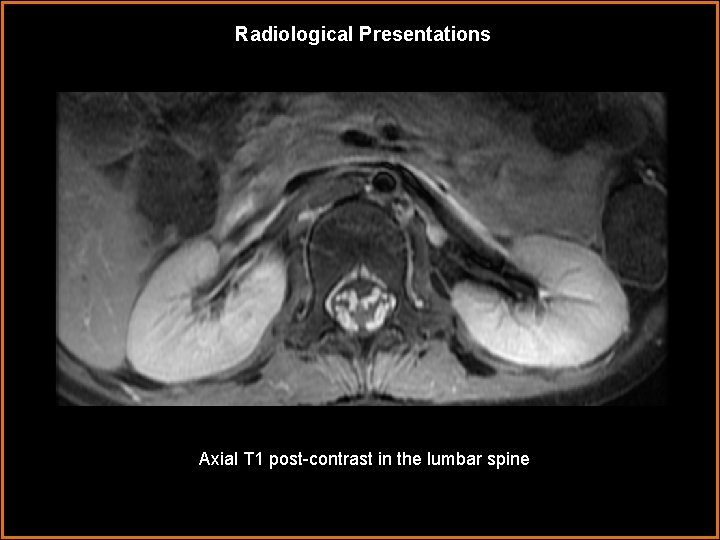
Radiological Presentations Axial T 1 post-contrast in the lumbar spine
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Guillain-Barré syndrome • Miller-Fisher syndrome • Leptomeningeal carcinomatosis • Spinal meningitis
Findings and Differentials Findings: The dorsal and ventral nerve roots are enhancing throughout the cervical, thoracic, and lumbar spine. There is avid contrast enhancement and thickening of the cauda equina nerve roots, both in their intrathecal and extraforaminal segments. The spinal cord is not enhancing. Incidental note Differentials: is made • Guillain-Barré syndrome • Miller-Fisher syndrome • Leptomeningeal carcinomatosis • Spinal meningitis of left lower lobe atelectasis.
Case History A lumbar puncture reveals the following CSF properties: Ig. G: 100 mg/d. L (normal 2 -4 mg/d. L) Albumin: 221 mg/d. L (normal 14 -25 mg/d. L) Total protein: 434 mg/d. L (normal 15 -45 mg/d. L) Glucose: 56 mg/d. L (normal 45 -80 mg/d. L) RBC: 10/mm 3 (normal: none) CSF culture: no growth
Discussion Guillain-Barré syndrome (GBS) is an acute autoimmune post-infectious or postvaccination inflammatory demyelination of peripheral nerves, nerve roots, and cranial nerves. There is an antecedent “trigger” event in 70 percent of cases of GBS. The most common trigger is a viral illness. Campylobacter jejuni has also been implicated as a precipitating agent; one third of GBS patients have positive titers for antibodies against nerve gangliosides, which cross-react with C. jejuni liposaccharides. Histopathologically, the condition is characterized by focal demyelination and perivascular and endoneural lymyphocyte/monocyte infiltration. Patients classically present with peripheral paresthesias followed by ascending paralysis. In more severe cases, cranial nerve and diaphragmatic function may be compromised.
Discussion GBS most commonly occurs in children and young adults. Natural history entails improvement of motor and sensory symptoms over a period of several months to greater than one year. Up to 10 percent of patients incur permanent neurological sequelae. Treatment/management is plasmapheresis or IV immunoglobulin. Respiratory support may also be necessary in severe cases.
Discussion Miller-Fisher syndrome is a rare variant seen in approximately 5 percent of GBS patients. Whereas GBS classically manifests as ascending paralysis, Miller-Fisher syndrome presents in a descending fashion. The extraocular muscles are usually the first muscles to be affected, and the trunk muscles are affected to a greater degree than are the extremity muscles. While Miller-Fisher syndrome can have an MR appearance very similar to GBS, clinical history will distinguish the two entities. The patient in this case had classic GBS symptoms.

Discussion Leptomeningeal carcinomatosis is capable of causing diffuse meningeal enhancement similar to GBS. However, the absence of a known primary tumor and the normal appearance of the brain, make this diagnosis less likely in the current case. In spinal meningitis, there may be avid nerve root enhancement. The appearance of the CSF may help differentiate this diagnosis from GBS. On post-contrast T 1 images, the CSF may appear hyperintense due to high protein content in meningitis. However, lumbar puncture is still warranted for definitive diagnosis. The patient in the above case had CSF laboratory findings typical for GBS. Furthermore, no culture growth was noted.

Discussion The patient required brief intubation for respiratory muscle weakness. She received multiple rounds of IV immunoglobulin. Following respiratory stabilization, she was extubated. The patient was transferred to a rehabilitation facility and scheduled for neurology followup.
Diagnosis Guillain-Barré syndrome.
References 1. Berciano J. MR imaging in Guillain-Barré syndrome. Radiology. 211(1): 290 -1, 1999. 2. Byun WM et al. Guillain-Barré syndrome: MR imaging findings of the spine in eight patients. Radiology. 208: 137 -41, 1998. 3. Fulbright RK et al. Cranial nerve enhancement in the Guillain-Barré syndrome. AJNR Am J Neuroradiol. 16(4): 923 -5, 1995. 4. Georgy BA et al. MR of the spine in Guillain-Barré syndrome. AJNR Am J Neuroradiol. 15(2): 300 -1, 1994.
 Ohsu neuroradiology
Ohsu neuroradiology Aerohive erate
Aerohive erate Radiological dispersal device
Radiological dispersal device Tennessee division of radiological health
Tennessee division of radiological health Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Mri principal
Mri principal Lexical vs auxiliary verbs
Lexical vs auxiliary verbs High modality examples
High modality examples Epistemic modality
Epistemic modality Swd modality
Swd modality Modality microsoft services
Modality microsoft services Modality stats
Modality stats Sodality vs modality
Sodality vs modality Crow's foot notation
Crow's foot notation Epistemic modality
Epistemic modality Cardinality and modality
Cardinality and modality Entity class in software engineering
Entity class in software engineering Data modeling fundamentals
Data modeling fundamentals Diagnostics imaging
Diagnostics imaging Pacs modality workstation
Pacs modality workstation Modality
Modality Modality in software engineering
Modality in software engineering