Radiological Category Neuroradiology Principal Modality 1 MRI Principal

- Slides: 15
Radiological Category: Neuroradiology Principal Modality (1): MRI Principal Modality (2): None Case Report #0416 Submitted by: Susanna Spence, M. D. Faculty reviewer: Clark Sitton, M. D. Date accepted: 13 April 2007
Case History 51 year old white female with 2 month history of increasingly severe gait disturbance, balance problems and dementia. Glasgow coma scale when she arrived to HH was 10. She moved all extremities, localized to pain. Incomprehensible voice sounds only. PMHx: hypothyroidism, hyperlipidemia During her stay in the hospital, her condition progressively worsened. In less than a month, she was localizing to pain only.
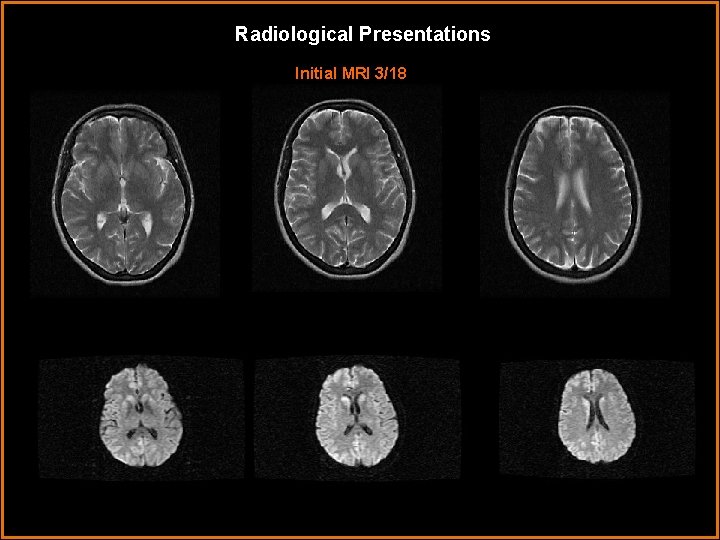
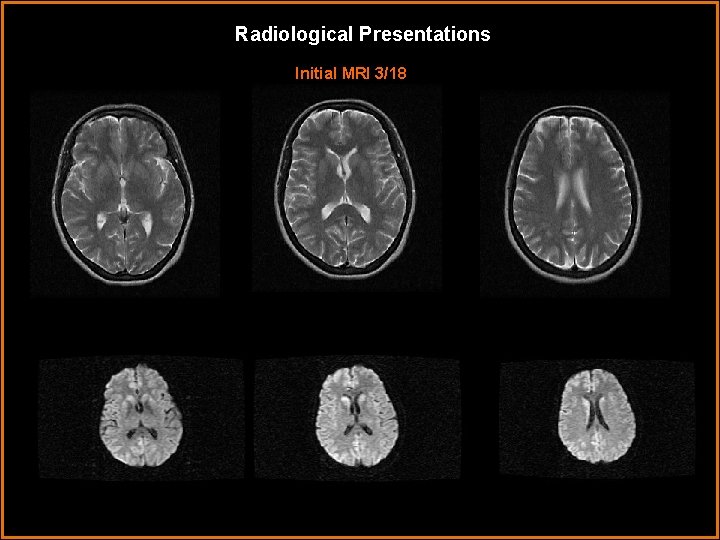
Radiological Presentations Initial MRI 3/18
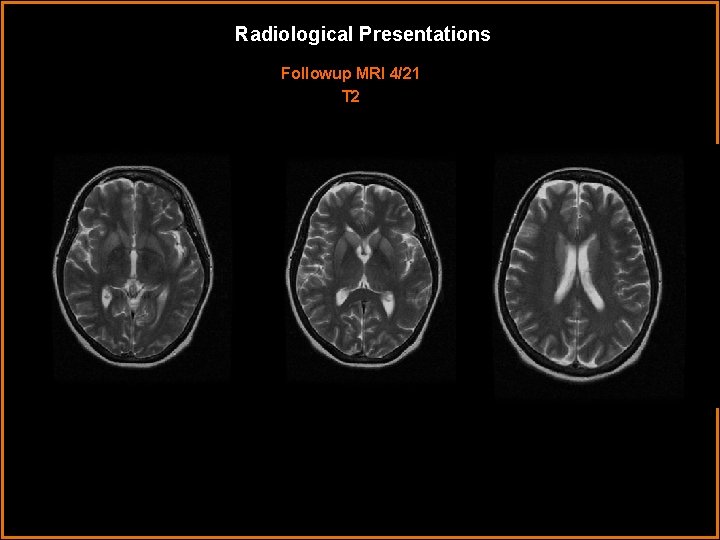
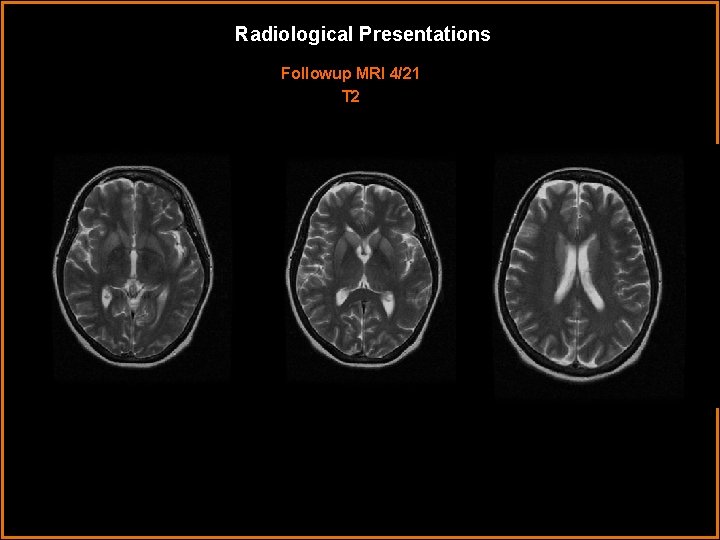
Radiological Presentations Followup MRI 4/21 T 2
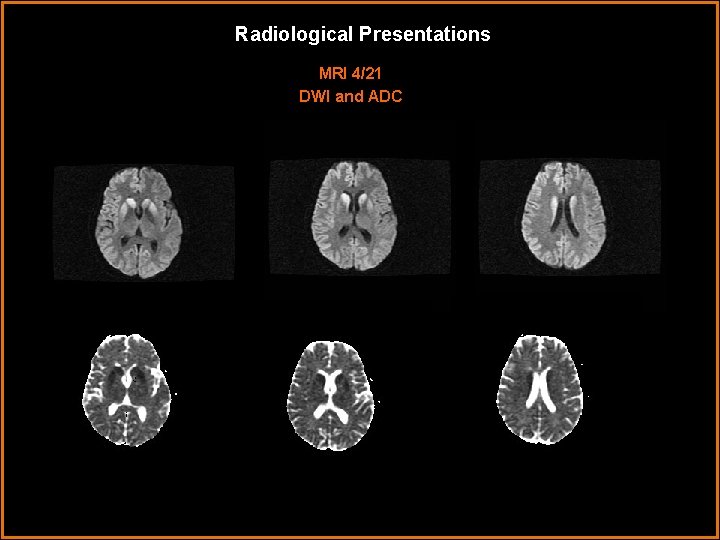
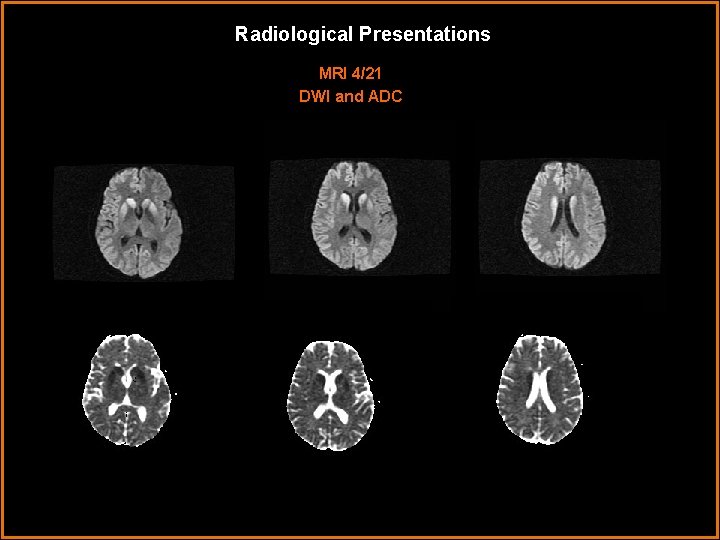
Radiological Presentations MRI 4/21 DWI and ADC
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Carbon monoxide poisoning • Methanol poisoning • Creutzfeld jakob disease • Mitochondrial disease • Lead poisoning • Anoxic injury
Findings and Differentials Findings: The initial MRI on 3/18 shows the beginnings of T 2 hyperintensity in the region of the basal ganglia, particularly notable in the region of the caudate and putamen, which corresponds to diffusion abnormality on the DWI images. The follow up MRI 4/21 shows that those T 2 signal abnormalities are brighter, and that the DWI abnormalities have not only failed to resolve, but have in fact become even more prominent. Differentials: • Infectious (prion diseases) • Toxic (heavy metal, carbon monoxide, lead) • Metabolic • Mitochondrial • Anoxic
Discussion This patient presented with a pattern of relentlessly worsening motor and cognitive symptoms, progressing rapidly over a few months. She had first cousin on her father’s side with Creutzfeld-Jakob disease, and this was considered high in the differential. Serum evaluation of lead, mercury and copper were normal. There was no history of methanol intoxication or carbon monoxide poisoning. This patient was tested for neuron specific enolase in the reference laboratory in Mayo clinic, with the following results: Creutzfeldt-Jakob (CSF): 505 ng/m. L Expected values: <20 NORMAL >35 INDICATIVE OF CJD
Discussion Typical imaging findings of CJD are as follows: In the early stage of the disease, clinical symptoms may be non-specific, and T 2 and FLAIR imaging can be normal. However, cortical and basal ganglia diffusion restriction can be identified on DWI. This may initially be a unilateral process (See patient’s initial MRI on 3/18) • In the intermediate stage, after the onset of myoclonus and EEG changes, definite increased T 2 signal intensity is seen the basal ganglia. Areas that showed partial/unilateral involvement on DWI (such as partial involvement of the putamen) become full and bilateral involvement. The DWI signal abnormalities fail to resolve over time. (see followup MRI 4/21) • These findings tend to progress into the terminal stage of the disease, and findings of cortical atrophy may be prominent. DWI findings FAIL TO RESOLVE. Rarely, the T 2 signal hyperintensity will fade in the terminal stage.
Discussion • Alternative diagnoses: • Mitochondrial encephalomyopathies: symmetric bilateral lesions of the basal ganglia, generally with extensive involvement of the cortex also. – Kearns-Sayre syndrome: a mitochondrial encephalomyopathy with preferential involvement of the globus pallidus and thalami bilaterally. • Lead poisoning: – Acute: symmetric. T 2 -weighted MRI high signal intensity in the periventricular white matter, basal ganglia, insula, posterior thalamus, and pons. – Chronic lead poisoning can lead to symmetrical calcifications in the cerebellum and basal ganglia. • Chronic carbon monoxide poisoning: – symmetric globus pallidus lesions, and focal cortical atrophy, most commonly affecting the parieto-occipital region. • Anoxic injury: – bilateral infarction of the caudate and putamen, along with cortical laminar necrosis. DWI abnormalities would resolve over time. • Metabolic: – hypoglycemic injury can cause bilateral caudate, lenticular, and/or thalamic nuclei infarctions • Methanol poisoning: bilateral necrosis of the putamen
Discussion Creutzfeld-Jakob disease: Prodromal symptoms prior to the first neurologic sign or symptom are common and include insomnia, headache, anorexia, behavioral changes, and depression. Initial neurologic symptoms are variable, and may involve ataxia, visual and memory disturbance. The majority (75 -85%) of sporadic CJD cases will show an EEG pattern which consists of slowing of brain waves and/or the presence of periodic sharp wave complexes; this pattern is non-specific, and may be seen in a variety of encephalopathic states. A CSF protein called the 14 -3 -3 test has recently been used to diagnose CJD, however the sensitivity and specificity have not been well established, and this protein may be elevated in many other forms of rapidly progressive dementia. In many cases, clinical and laboratory data are suggestive of CJD, but the diagnosis is not confirmed until autopsy. There is no known successful treatment that will halt or even slow the progression of CJD, although medications that are currently under investigation are Quinacrine, Pentosan Polysulphate and Flupirtine. The patient in this example was transferred to hospice approximately 6 weeks after admission.

Discussion Creutzfeld-Jakob disease: Pathology slides courtesy of Dr. Clay Goodman, Baylor College of Medicine Pathology Department- with permission Pathology shows neuronal loss and vacuolization within the gray matter, giving the typically “spongiform” appearance of CJD. The altered prion protein takes on an abnormal 3 dimensional structure, that is though to cause other, originally normal prion proteins within the cell, to convert into the same structure. These abnormal proteins are resistant to cellular proteases, and therefore progressively accumulate over time, eventually leading to cell vacuolization and cell death.
Discussion There are several forms of CJD: • 10 -15% are familial, with autosomal dominant inheritance and reduced penetrance of a mutation at the prion gene Pr. P on chromosome 20. Over 20 different mutations have been discovered. Survival and age of onset vary by mutation. • ~85% are sporadic (s. CJD), with no known family history or known infectious source. The prognosis is dismal, with an average 4. 5 month survival from symptom onset. • <1% are due to iatrogenic CJD, from causes such as corneal transplantation, contaminated human growth hormone, and use of cadaveric dura mater, which caused 97 cases of iatrogenic CJD in Japan before 2003. • Much attention has been paid in recent years to variant CJD (v. CJD), associated with consumption of undercooked beef in animals with mad cow disease. 159 probable/definite cases have been reported in the UK since 1990. Pts with v. CJD tend to be younger (average 29) with a slightly longer, 14 month survival period. The other prion related diseases in humans are: • Gerstmann-Sträussler-Scheinker disease: a familial prion disease commonly presents initially with cerebellar ataxia. It’s clinical features are similar to CJD, however it has a slower clinical course, with survival up to 60 months. • Kuru: a condition of the Fore tribe of the Okapa district of the Eastern Highland in Papua New Guinea, where ritual cannibalism of fellow tribesman took place until approximately 1956. These disease is clinically distinctive, in that dementia is not a symptom of the disease. Cerebellar ataxia, weakness and nerve palsies are the major features. • Familial Fatal Insomnia: also a familial disorder, age of onset 40 -60. Begins with mild insomnia, muscle twitching, progressing to complete insomnia, dysautonomia. Characterized pathologically by severe atrophy of the anterior ventral and mediodorsal thalamic nuclei, and spongioform encephalopathy.
References: • 'TSEs' of the Encylcopaedia of Microbiology Volume 4 Academic Press 1992 • Medori et al: Fatal familial insomnia, a prion disease with a mutation at codon 178 of the prion protein gene NEJM 1992: Volume 326: 444 -449 • Ukisu et al: Diffusion-weighted MR Imaging of Early-Stage Creutzfeldt-Jakob Disease: Typical and Atypical Manifestations: Radio. Graphics 2006; 26: S 191 -S 204 Ukisu et al: Serial Diffusion-Weighted MRI of Creutzfeldt-Jakob Disease AJR 2005; 184: 560 -566 • Millar et al: MRI of Five Patients with Mitochondrial Neurogastrointestinal Encephalomyopathy AJR 2004; 182: 1537 -1541 • Uchino et a: MRI of the brain in chronic carbon monoxide poisoning. Neuroradiology. 1994 Jul; 36(5): 399 -401
Diagnosis Creutzfeld-Jakob disease
 Ohsu neuroradiology
Ohsu neuroradiology Erate category 2
Erate category 2 Tennessee division of radiological health
Tennessee division of radiological health Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Radiological dispersal device
Radiological dispersal device Mri principal
Mri principal What is modality in statistics
What is modality in statistics Modality
Modality Modality in software engineering
Modality in software engineering Epistemic modality
Epistemic modality Modality in software engineering
Modality in software engineering Data modeling fundamentals
Data modeling fundamentals Lexical vs auxiliary verbs
Lexical vs auxiliary verbs Skill focus: persuasion
Skill focus: persuasion Pacs modality workstation
Pacs modality workstation