Radiological Category Neuroradiology Principal Modality 1 MRI Principal


- Slides: 11
Radiological Category: Neuroradiology Principal Modality (1): MRI Principal Modality (2): CT Case Report #0386 Submitted by: Shalini Mukhi, M. D. Faculty reviewer: Matt Debnam, M. D. Date accepted: 26 February 2007
Case History 66 year old female with history of bladder cancer who presents with delirium following surgery. No other significant past medical history.

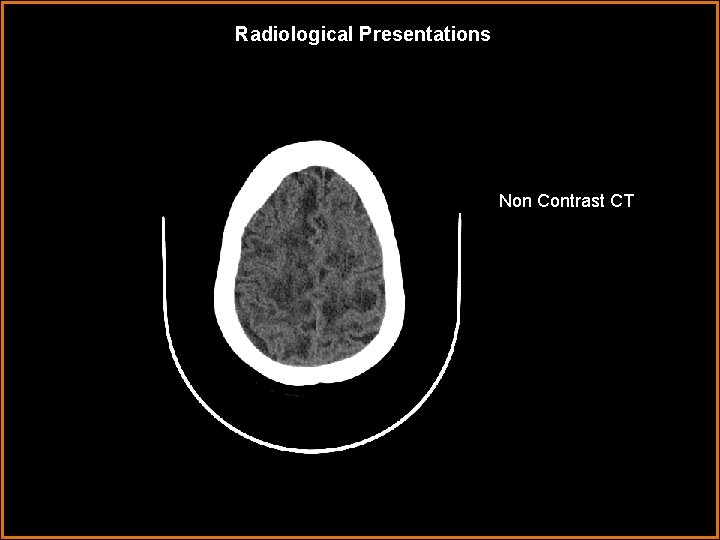
Radiological Presentations Non contrast CT
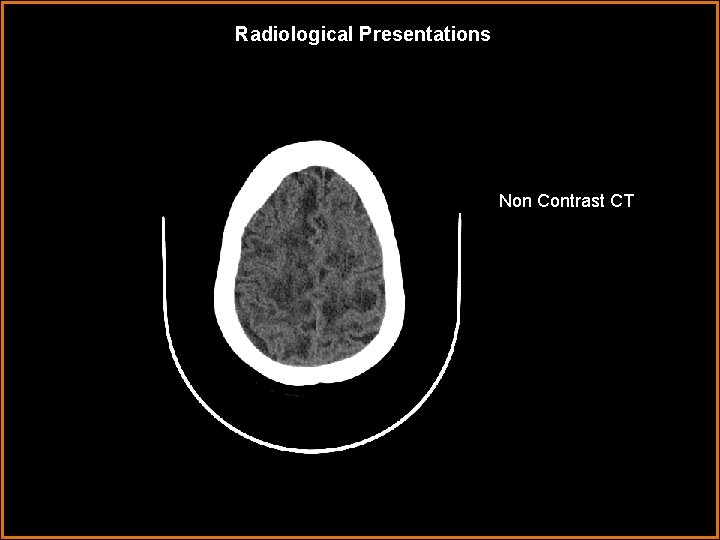
Radiological Presentations Non contrast CT Non Contrast CT
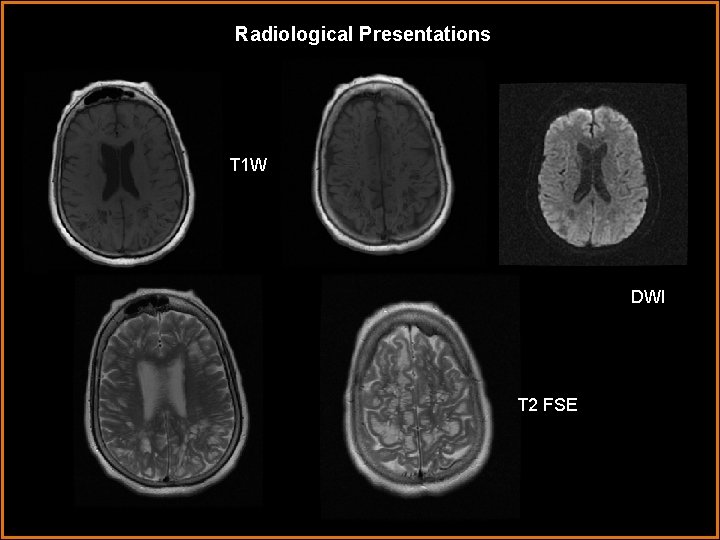
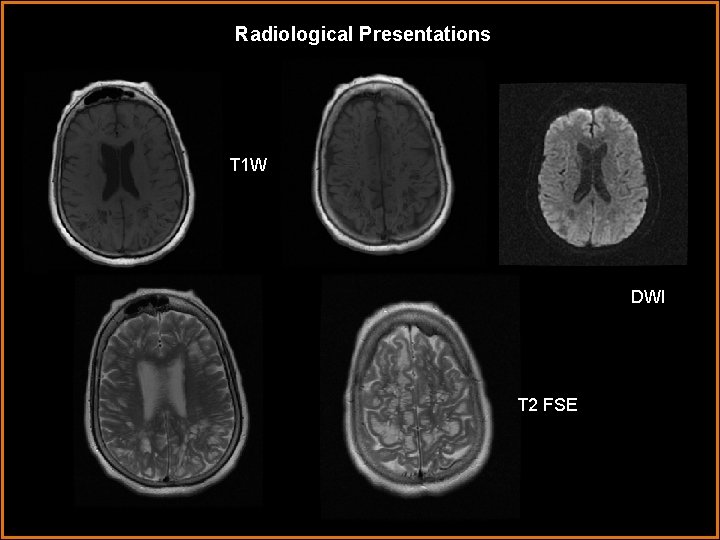
Radiological Presentations T 1 W DWI T 2 FSE
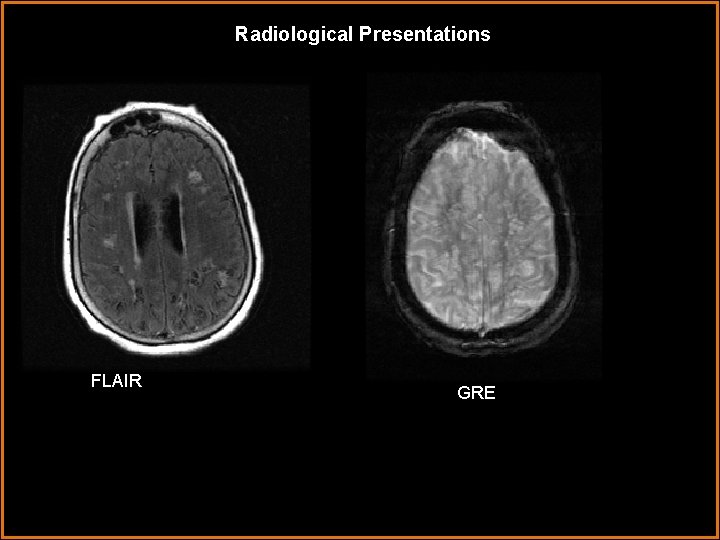
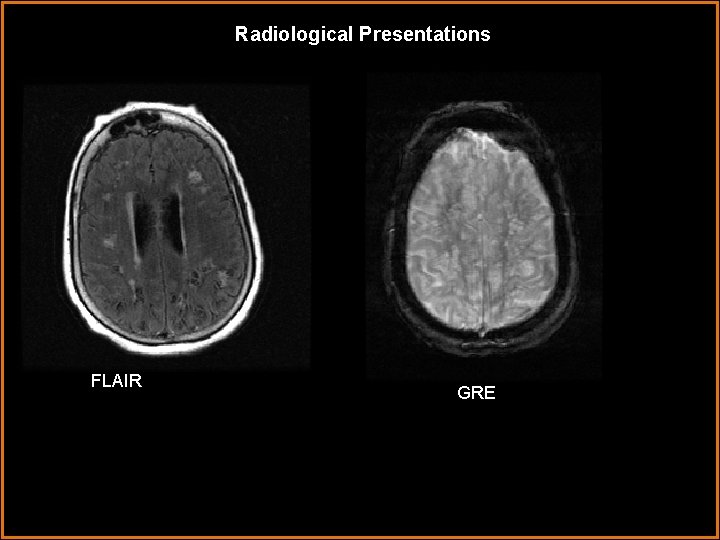
Radiological Presentations FLAIR GRE
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Posterior reversible encephalopathy syndrome • Demyelinating disease • Giant Tumefactive Virchow Robbins Spaces • Mucopolysaccharidoses
Findings and Differentials Findings: CT reveals scattered areas of hypodensity throughout the hemispheric white matter sparing the gray matter. Watershed area posteriorly involves the gray matter. Basal ganglia are spared. MRI reveals multiple, varying in size, cystic appearing lesions involving the periventricular spaces and white matter. These lesions follow CSF signal on all sequences and do not enhance. There is no restricted diffusion or blooming. On FLAIR, focal hyperintensities are seen around some of the lesions. No definite mass effect is seen. Differentials: • Mucopolysaccharidoses • Giant Tumefactive Virchow Robbins Spaces • Demyelinating Disease • Cystic Neoplasm
Discussion Perivascular spaces (PVSs) also known as Virchow Robbins spaces are pial-lined interstitial fluid filled structures that accompany penetrating arteries. When enlarged they may cause mass effect and can be mistaken for a pathologic process. They most often appear as clusters of variable sized cysts that are isointense relative to CSF and do not enhance. They are most common in the mesencephalothalamic region and may cause hydrocephalus. Although the may have striking mass effect, giant PVSs should not be mistaken for neoplasm or other diseases. Patients usually present with nonspecific findings that are not attributable to the giant PVSs. Giant PVSs that occur in the white matter may have surrounding signal intensity abnormality on T 2 weighted or FLAIR images. One theory is that this associated signal intensity alteration may represent advanced chronic ischemic change related to mass effect of the PVSs. In younger patients signal abnormality is more diffuse and is thought to be due to gliosis or spongiosis. As imaging of enlarged PVSs is characteristic, a differential diagnosis can be eliminated. Mucopolysaccharidoses are usually manifested on MR as diffuse cribiform or cystic appearing areas of abnormal signal intensity of white matter. A history significant for mucopolysaccharidoses is usually known.

Diagnosis Giant Tumefactive Virchow Robbins Spaces
References Salzman K, Osborn A, House P, Jinkins J, Ditchfield A, Cooper J, Weller R. Giant Tumefactive Perivascular Spaces. American Journal of Neuroradiology. 2005. (26) 298 -305. Osborn A. , et al. Enlarged Perivascular Spaces. Diagnostic Imaging: Brain. 2004. I (7) 22 -26
 Ohsu neuroradiology
Ohsu neuroradiology Erate pa
Erate pa Tennessee division of radiological health
Tennessee division of radiological health Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Radiological dispersal device
Radiological dispersal device Mri principal
Mri principal What is modality in statistics
What is modality in statistics Modality
Modality Modality in software engineering
Modality in software engineering Deontic and epistemic modality exercises
Deontic and epistemic modality exercises Modality in software engineering
Modality in software engineering