Radiological Category Neuroradiology Principal Modality 1 MRI Principal



- Slides: 30
Radiological Category: Neuroradiology Principal Modality (1): MRI Principal Modality (2): CT Case Report # 0948 Submitted by: Patrick Marcin, M. D. Faculty reviewer: Eliana Bonfante, M. D Date accepted: 01 January 2012
Case History 50 -year-old male in prison with history of hepatitis C found unconscious and nonresponsive. By witnesses at the scene, patient was “jerking” on the floor. No other prior past medical history available.

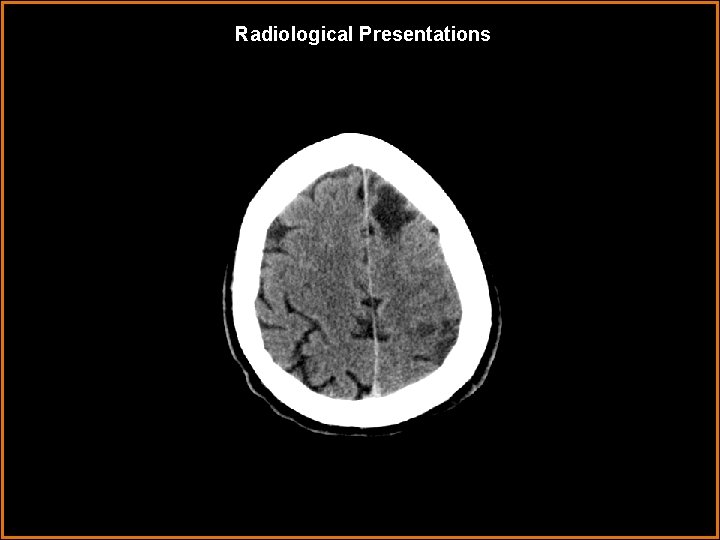
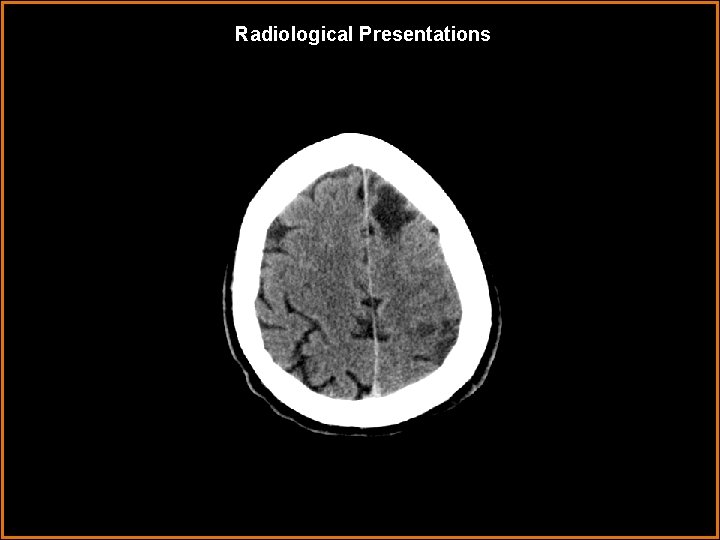
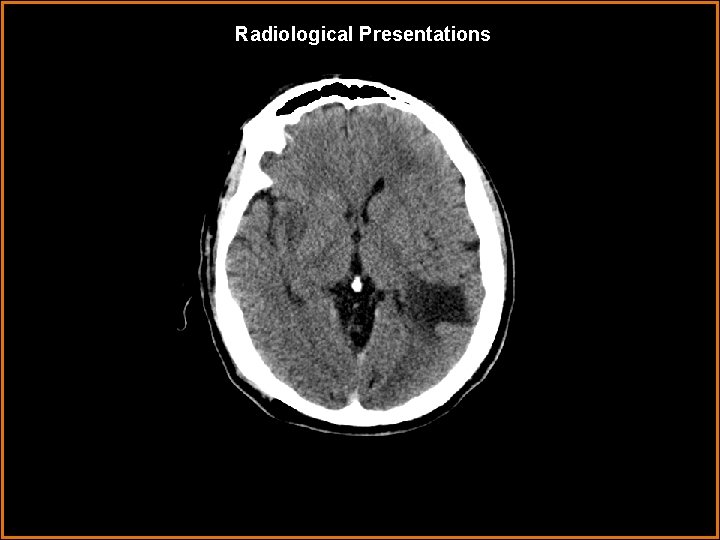
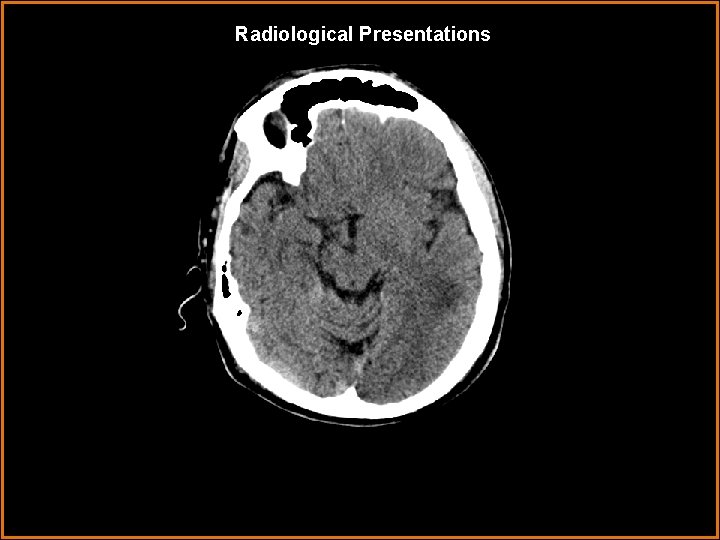
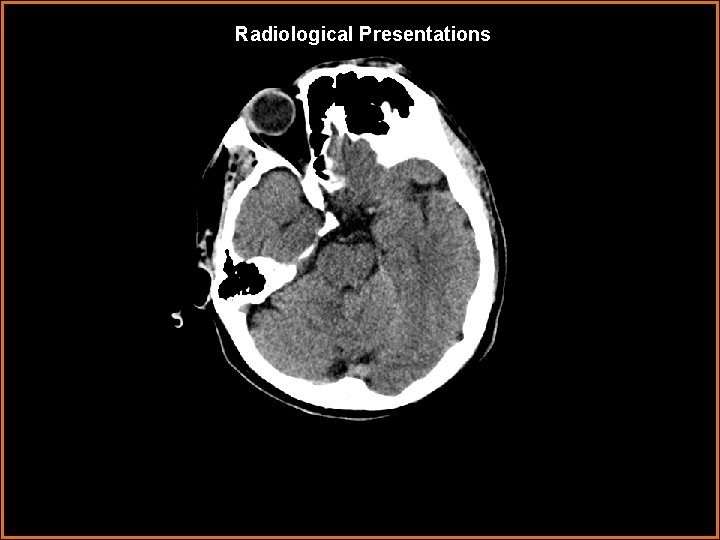
Radiological Presentations
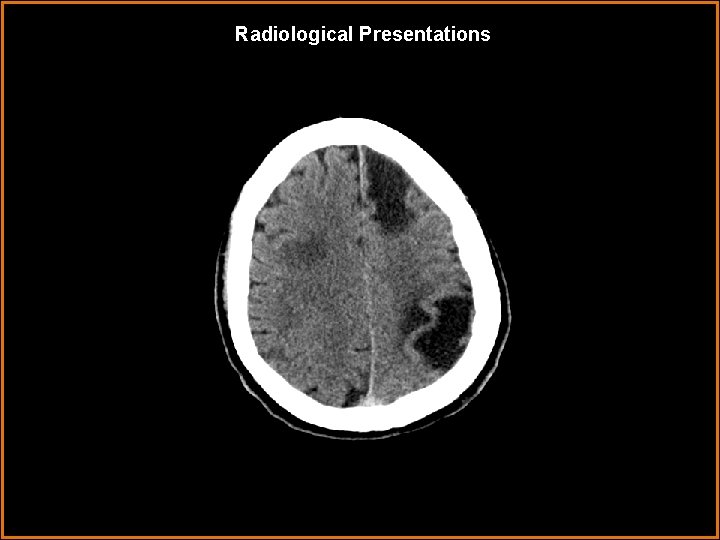
Radiological Presentations
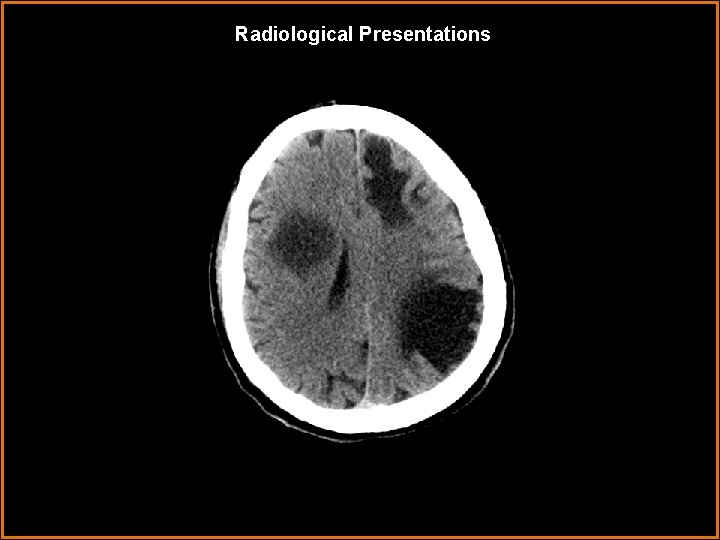
Radiological Presentations
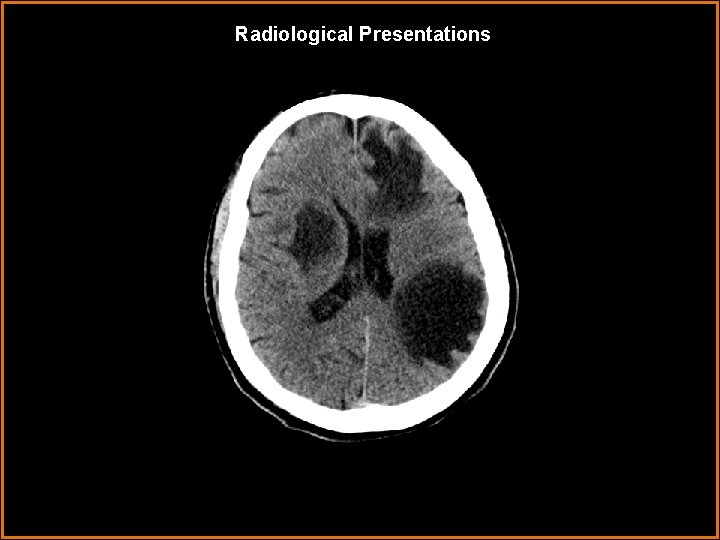
Radiological Presentations
Radiological Presentations
Radiological Presentations
Radiological Presentations
Radiological Presentations
Radiological Presentations
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Metastases • Multiple cerebral abscesses • Multifocal glioblastoma multiforme • Toxoplasmosis • Tumefactive demyelinating lesions • Progressive multifocal leukoencephalopathy
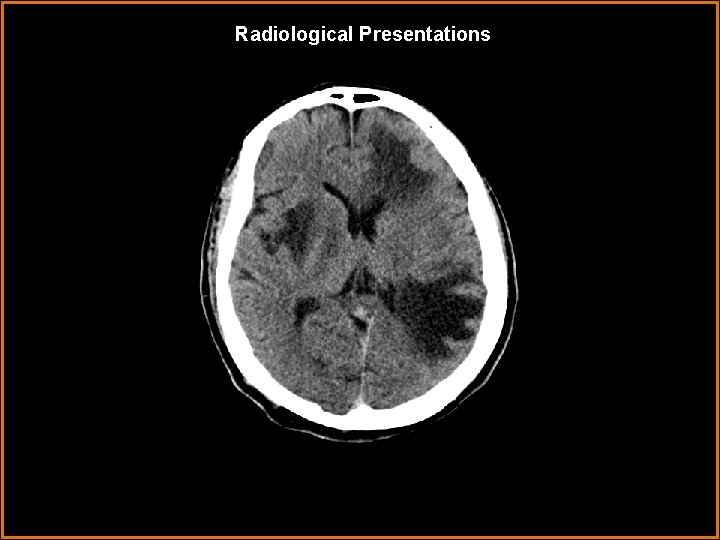
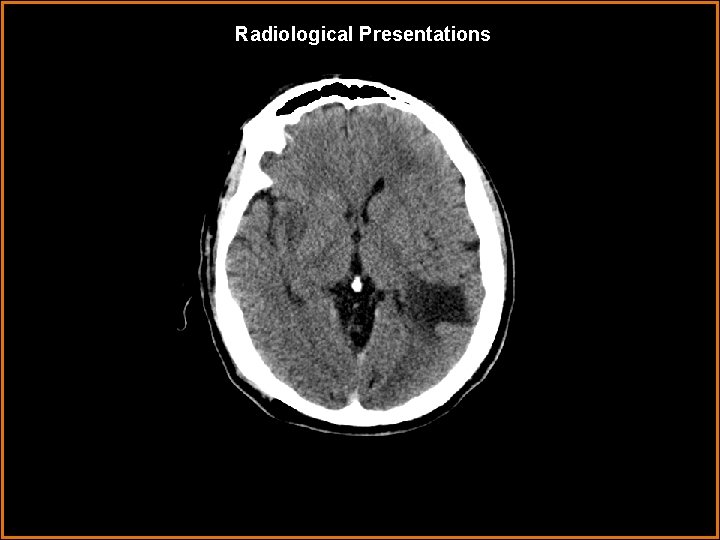
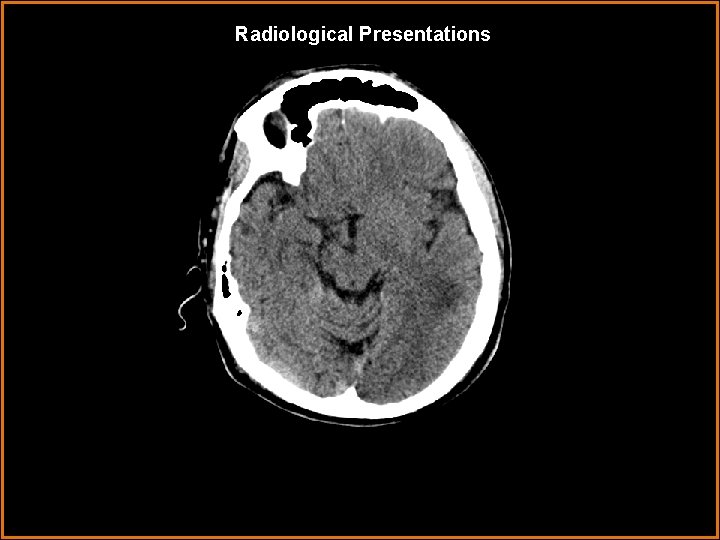
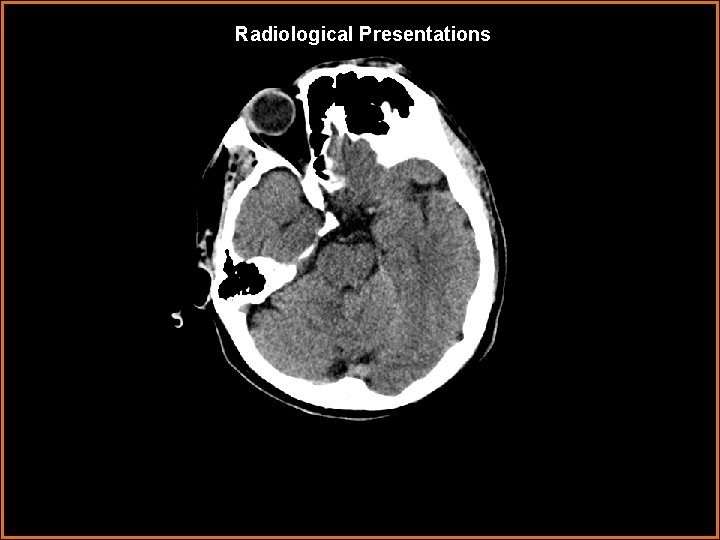
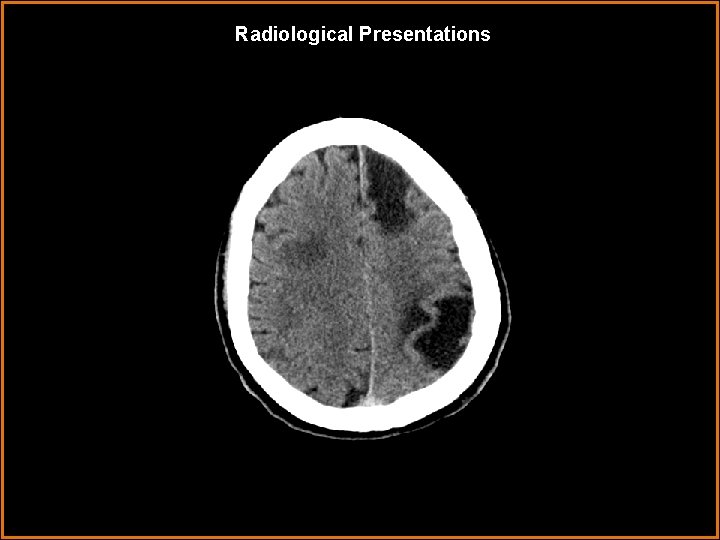
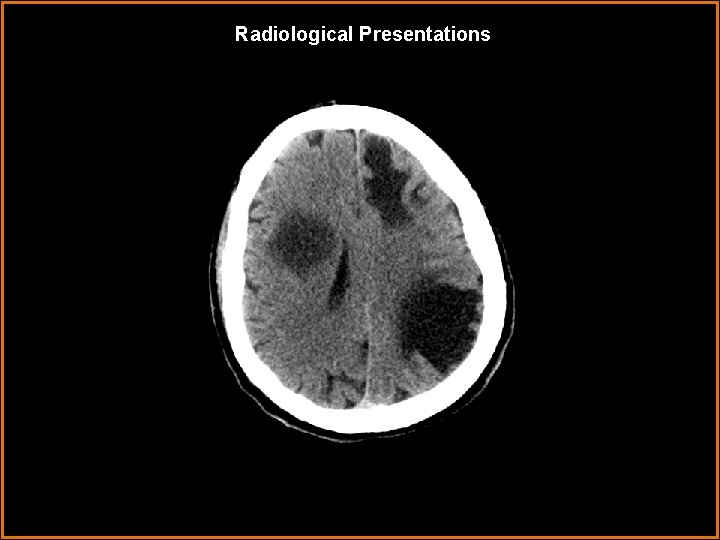
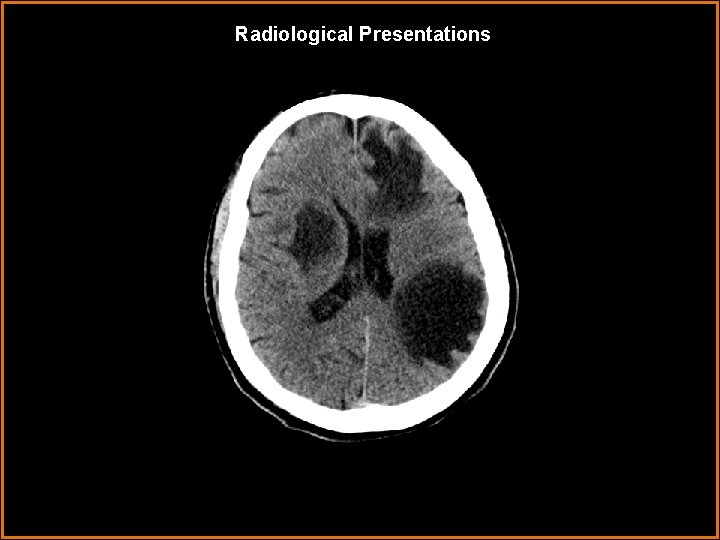
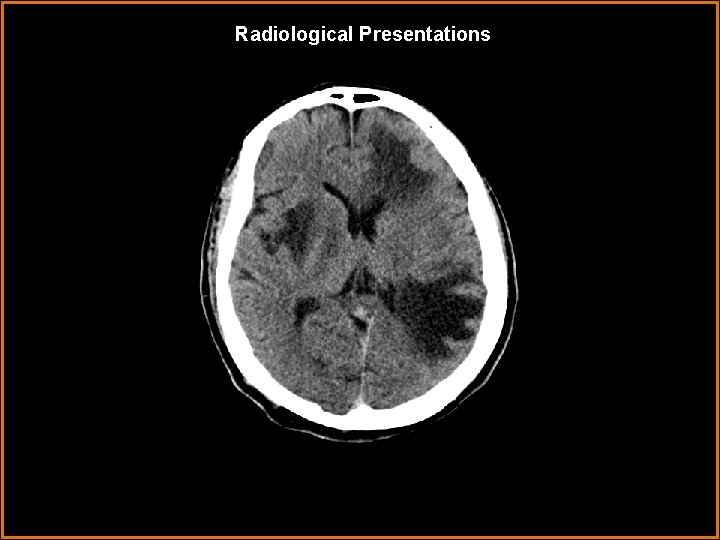
Findings and Differentials Findings: CT: Multiple mass-like areas of low attenuations in the supratentorium within the left anterior frontal lobe, left posterior frontal lobe, and right insular/ periventricular white matter. No hemorrhage or calcifications. Differentials: • Metastases • Multiple cerebral abscesses • Multifocal glioblastoma multiforme • Toxoplasmosis • Tumefactive demyelinating lesions • Progressive multifocal leukoencephalopathy
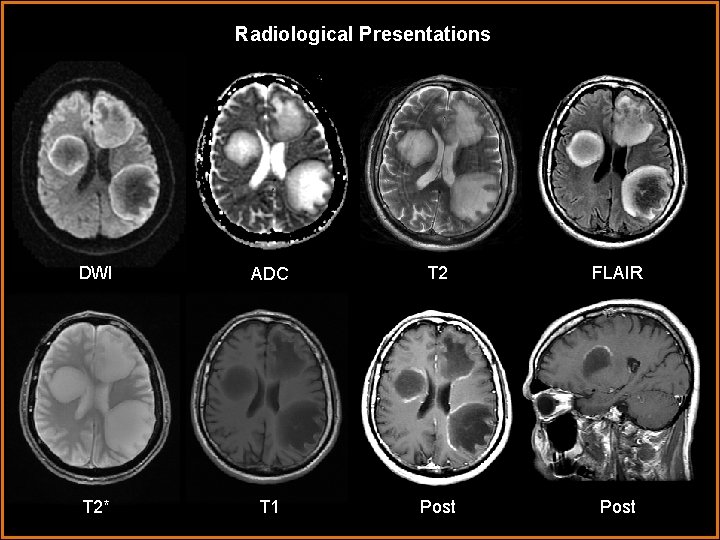
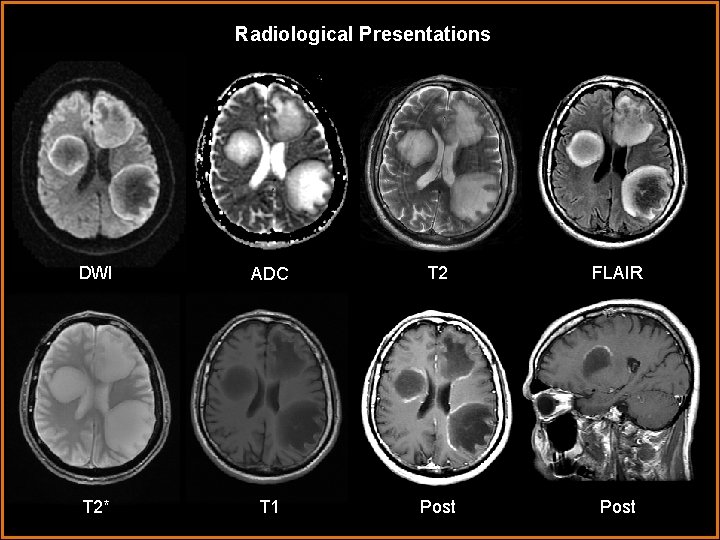
Radiological Presentations DWI ADC T 2 FLAIR T 2* T 1 Post
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Metastases • Multiple cerebral abscesses • Multifocal glioblastoma multiforme • Toxoplasmosis • Tumefactive demyelinating lesions • Progressive multifocal leukoencephalopathy
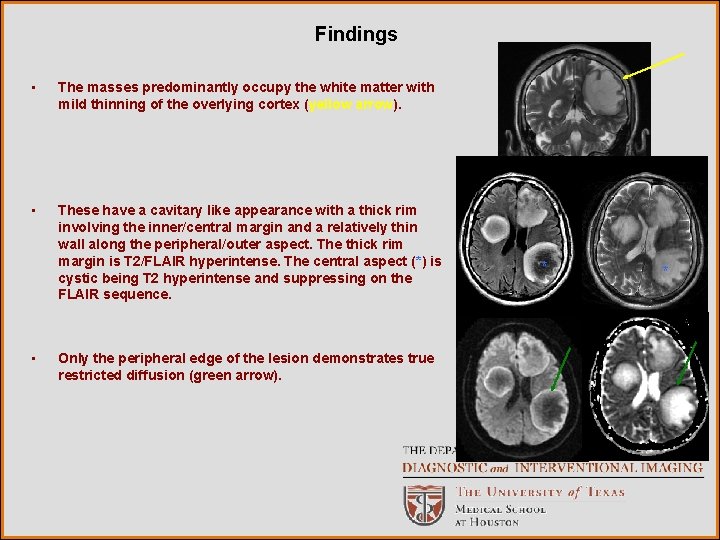
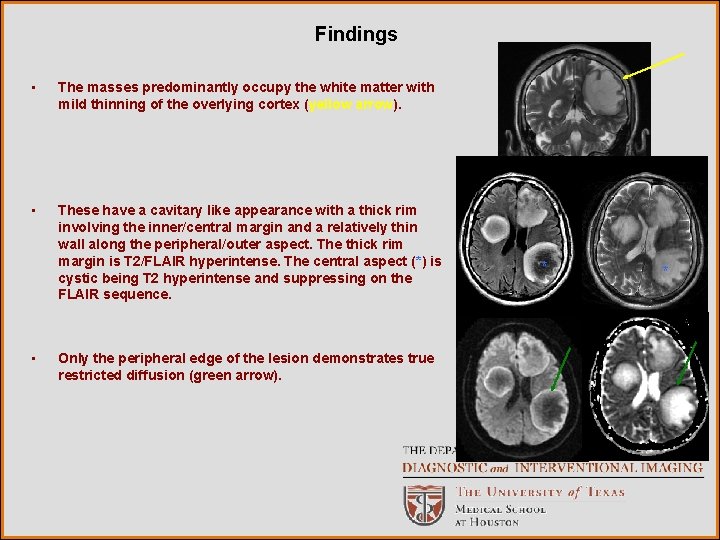
Findings • The masses predominantly occupy the white matter with mild thinning of the overlying cortex (yellow arrow). • These have a cavitary like appearance with a thick rim involving the inner/central margin and a relatively thin wall along the peripheral/outer aspect. The thick rim margin is T 2/FLAIR hyperintense. The central aspect (*) is cystic being T 2 hyperintense and suppressing on the FLAIR sequence. • Only the peripheral edge of the lesion demonstrates true restricted diffusion (green arrow). * *
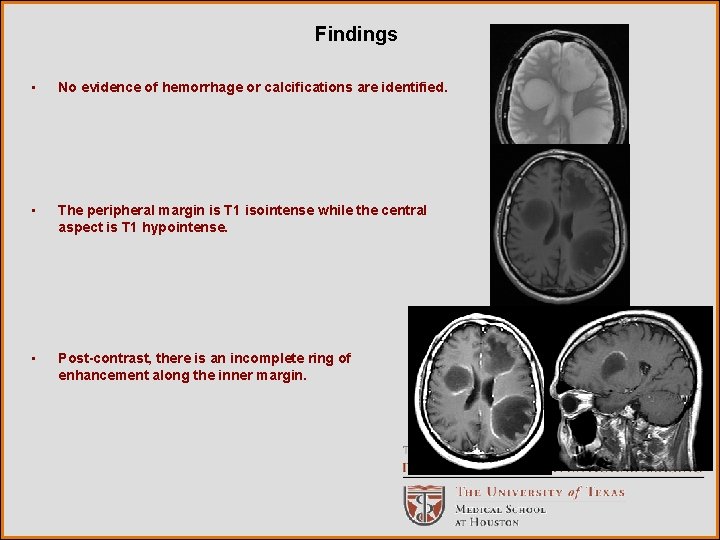
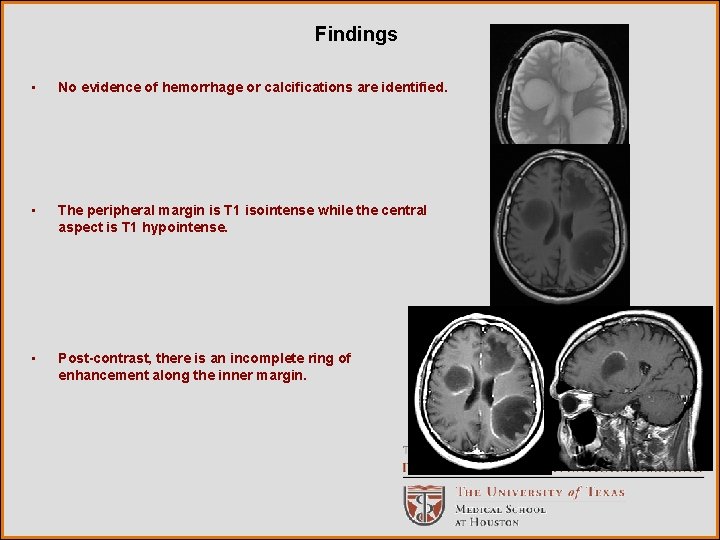
Findings • No evidence of hemorrhage or calcifications are identified. • The peripheral margin is T 1 isointense while the central aspect is T 1 hypointense. • Post-contrast, there is an incomplete ring of enhancement along the inner margin.
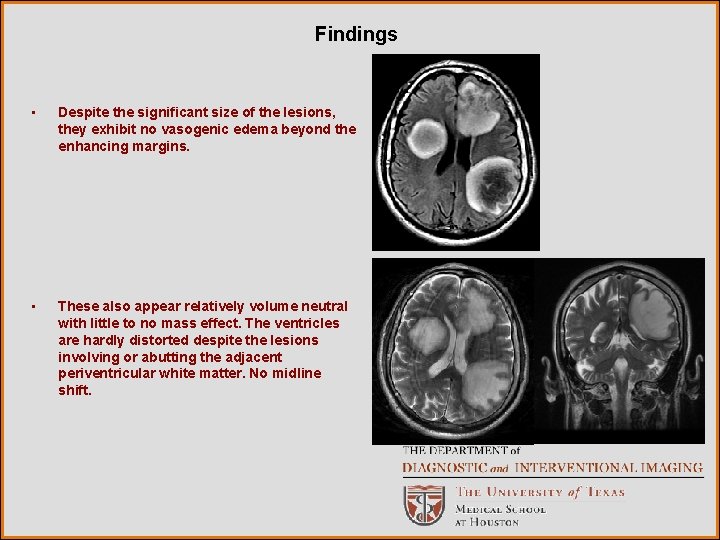
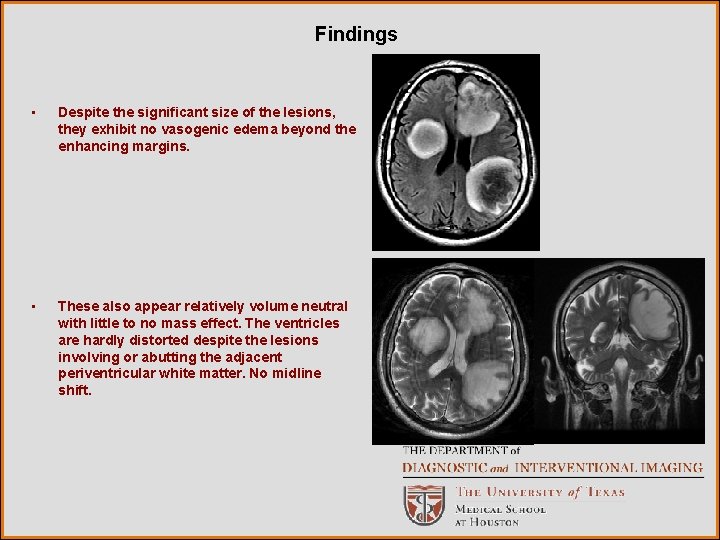
Findings • Despite the significant size of the lesions, they exhibit no vasogenic edema beyond the enhancing margins. • These also appear relatively volume neutral with little to no mass effect. The ventricles are hardly distorted despite the lesions involving or abutting the adjacent periventricular white matter. No midline shift.
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Metastases • Multiple cerebral abscesses • Multifocal glioblastoma multiforme • Toxoplasmosis • Tumefactive demyelinating lesions • Progressive multifocal leukoencephalopathy
Discussion • When these were first encountered, the 3 discrete lesions were felt to most likely represent 3 metastatic lesions, with the hypoattenuating margin representing the edge of the vasogenic edema. • MRI with contrast was requested for further characterization. • The MR characteristics of metastases include; Ø Ø Round enhancing lesion(s) at gray-white interface (arterial border zones) Most mets are circumscribed/discrete >>infiltrating, spherical >> linear 50% are solitary, 20% have 2 metastases, 30% have 3 or more. Almost all metastases enhance due to disruption of the blood-brain-barrier (BBB). Enhancement pattern is variable upon tumor type. Ø Result in disproportionately large amount of surrounding vasogenic edema and mass effect. Ø Variable intrinsic signal intensity. Ø Majority will not restrict diffusion, except in cases of tumors with high cellularity. • While these 3 lesions did share some of the common characteristics of metastases, the fact that they did not have any significant or visible vasogenic edema, metastases were felt to be less likely.
Discussion • The second differential initially entertained based upon the CT was multiple cerebral abscesses, potentially from septic emboli. • The MR characteristics of cerebral abscesses include; Ø Ring enhancing lesion with T 2 hypointense rim. Ø Diffusion restriction. Increased DWI signal intensity in cerebritis and abscess. ADC map with markedly decreased signal centrally within abscess. Ø Typically supratentorial in frontal and parietal lobes. Ø Overall imaging appearance varies with stage of abscess 1. Early cerebritis: Patchy parenchymal enhancement. 2. Late cerebritis: Intense, irregular rim enhancement. 3. Early capsule: Well defined, thin-walled, enhancing capsule. 4. Late capsule: Cavity collapses, capsule thickens. • The 3 lesions demonstrated an “incomplete ring” of enhancement rather than true ring enhancement. There was no T 2 hypointense rim. Finally, the restricted diffusion involved only the enhancing margin, not the central cavitary aspect. • Therefore, these were felt not to be abscesses.
Discussion • Due to the multiplicity of lesions, the differential also entertained the idea of a multifocal primary brain tumor. • At the patients age (50 years), the most common primary brain neoplasm is glioblastoma multiforme (GBM). GBMs are rapidly enlarging malignant astrocystic tumors (WHO grade IV) with hallmarks being necrosis and microvascular proliferation. • The MR characteristics of glioblastoma multiforme include; Ø Thick, irregularly enhancing rind of neoplastic tissue surrounding necrotic core. Ø Heterogeneous, T 2 hyperintense mass with adjacent tumor infiltration/vasogenic edema. Viable tumor extends far beyond signal changes. Ø Necrosis, cysts, hemorrhage, fluid/debris levels, flow voids (neovascularity) may be seen. Ø Most commonly supratentorial white matter lesions, commonly cross white tracts to involve contralateral hemisphere (corpus callosum “butterfly glioma” or post/ant commissures. Ø No restricted diffusion typical. Ø Rarely can be multifocal • The 3 lesions lacked the defining characteristics of a thick irregular rim of enhancement and extensive amount of surrounding T 2 signal changes representative of edema/infiltrative tumor. • Multifocal GBM was felt to be unlikely.
Discussion • The patient was known to have Hepatitis C, however, his HIV status was unknown. • If the patient was immunocomprimised, opportunistic infections such as toxoplasmosis would be a possibility based upon the CT. This is caused by the parasite Toxoplasma gondii and is the most common opportunistic CNS infection in AIDS patients. • The MR characteristics of toxoplasmosis include; Ø T 2 hypointense rim with peripheral hyperintense edema. Ø Peripheral nodular enhancement “target sign” Ø Usually lack central restricted diffusion which can help differentiate from pyogenic abscess and CNS lymphoma. Ø Thallium-201 SPECT and FDG-PET have higher specificity, but lower sensitivity to MR. • Again, the 3 lesions demonstrated no peripheral edema and had a thin smooth “incomplete ring” of enhancement. These MR features were not supportive of toxoplasmosis.
Discussion • A white matter disorder that can arise in the immunosuppressed is progressive multifocal leukoencephalopathy (PML) • This is caused by the JC polyomavirus which infects oligodendrocytes causing demyelination in immunocomprimised patients. • The MR characteristics of PML include; Ø Multifocal T 2 hyperintense demyelination plaques extending from the subcortical white matter to the deep white matter. Ø Characteristic involvement of the subcortical U-fibers. Ø Generally no enhancement or mass effect. Ø Typically bilateral, but asymmetric. Ø Late stage: confluent WM lesions with cavitary changes. • While many of these described characteristics were identified within the 3 lesions, the presence of an incomplete ring of enhancement was more suggestive of an alternative diagnosis. However, because of the large size of the lesions and lack of mass effect, an atypical presentation of PML was included in the final differential. • Later on, his HIV status was found to be negative.
Discussion • Other demyelinating disorders were also included in the differential. • When demyelinating plaques become >2 cm, they are given the term tumefactive demyelinating lesions (TDL), with their imaging characteristics mimicking neoplasms. • With rare exception, the tumefactive demyelinating lesions do not originate as a postinfectious or post-vaccination response. Although the exact pathogenesis is not clearly understood, most patients respond favorably to corticosteroid therapy and do not progress to multiple sclerosis. • In a review of 31 cases, Kepes proposed that tumefactive demyelinating lesions represent an intermediate lesion between those typically seen with multiple sclerosis and acute disseminated encephalomyelitis.
Discussion • The MR characteristics of TDL include; Ø Circumscribed lesions with little or no mass effect or vasogenic edema. Ø Typically involve the supratentorial compartment and are centered in the white matter although they may extend to involve the cortical gray matter. Ø Approximately half will have pathologic enhancement, commonly in the form of incomplete or open ring. The incomplete portion of the ring is on the gray matter side of the lesion. (More typical active multiple sclerosis plaques exhibit this incomplete ring or arc-like pattern of enhancement only 9% of the time. ) The enhancing portion of the ring is believed to be the leading edge of demyelination and thus favors the white matter side. Ø The central nonenhancing core represents a more chronic phase of the inflammatory process. Ø Lack diffusion restriction centrally.

Discussion • Based on the imaging characteristics exhibited by the lesions, the final radiologic diagnosis was that these were tumefactive demyelinating lesions. • The clinicians performed a lumbar puncture however the histochemical analysis of the CSF yielded no oligoclonal-bands. In the study of Lucchinetti and colleagues, 62 of the patients had CSF studies prior to brain biopsy. In 33%, oligoclonal bands were present, and 35% had an elevated Ig. G synthesis rate. Therefore the lack of oligoclonal bands is less helpful when it is absent compared to typical MS. • Ultimately, because diagnosis was still in question, an open biopsy was performed. Pathology revealed; u. White matter infiltration by macrophages, severe reactive astrocytosis and mononuclear inflammatory infiltrate around some blood vessels. u. ABC immunoperoxidase stain for neurofilament protein showed preservation of axons. u. LFB stain for myelin showed weakening of staining for myelin. u. The lesion spares gray matter. u. No evidence of metastatic carcinoma or glioma.
Diagnosis Multiple tumefactive demyelinating lesions
Follow Up The patients clinical status slowly began improving after initiation of high dose corticosteroids. The patient became awake and alert but remained aphasic. The patient was transitioned to PO steroids and discharged, with follow up in the county MS clinic.

References Camacho DL. Differentiation of Toxoplasmosis and Lymphoma in AIDS Patients by Using Apparent Diffusion Coefficients. AJNR. 2003 24: 633 -637 Given CA. The MRI Appearance of Tumefactive Demyelinating Lesions. AJR. January 2004 vol. 182 no. 1 195 -199 Lucchinetti CF. Clinical and radiographic spectrum of pathologically confirmed tumefactive multiple sclerosis. Brain. 2008 July; 131(7): 1759– 1775. Stat. Dx
 Ohsu neuroradiology
Ohsu neuroradiology Erate category 1
Erate category 1 Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Radiological dispersal device
Radiological dispersal device Tennessee division of radiological health
Tennessee division of radiological health Mri principal
Mri principal Modality in software engineering
Modality in software engineering Deontic and epistemic modality exercises
Deontic and epistemic modality exercises Modality in software engineering
Modality in software engineering Cardinality and modality in database
Cardinality and modality in database Lexical vs auxiliary verbs
Lexical vs auxiliary verbs High modality examples
High modality examples Pacs modality workstation
Pacs modality workstation Induction field diathermy
Induction field diathermy Callendreasonlocaluserinitiated
Callendreasonlocaluserinitiated Exteroceptors
Exteroceptors Modality
Modality Sodality vs modality
Sodality vs modality Crow's foot notation
Crow's foot notation Cardinality and modality
Cardinality and modality Cardinality and modality
Cardinality and modality Modality in software engineering
Modality in software engineering Epistemic modality
Epistemic modality Birads categories
Birads categories Modality stats
Modality stats Past tense in xhosa
Past tense in xhosa How mri works
How mri works Mri question
Mri question Mri safety training
Mri safety training Atriclip mri safety
Atriclip mri safety