Radiological Category Neuroradiology Principal Modality 1 MRI Principal

- Slides: 11
Radiological Category: Neuroradiology Principal Modality (1): MRI Principal Modality (2): Case Report 0960 Submitted by: Navid Zaer, M. D. Faculty reviewer: Leo Hochhauser, M. D. Date accepted:
Case History 31 y/o male status post MVC with left forearm fractures requiring extensive orthopedic surgery. Persistent left triceps and deltoid pain as well as weakness in the left hand.
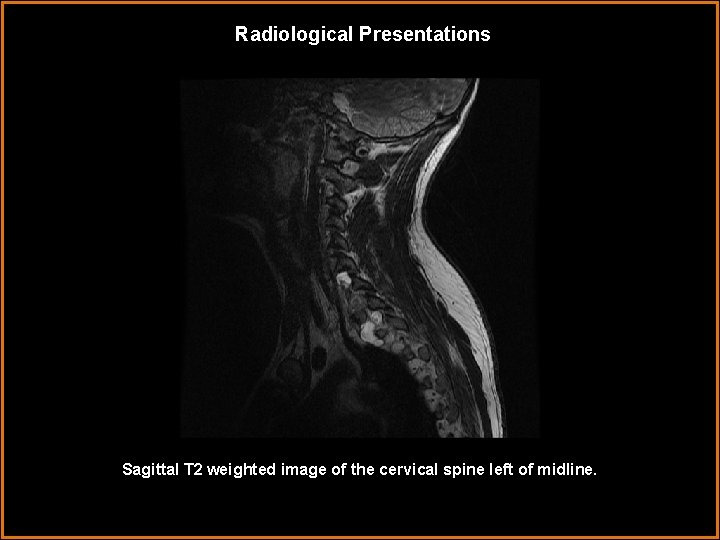
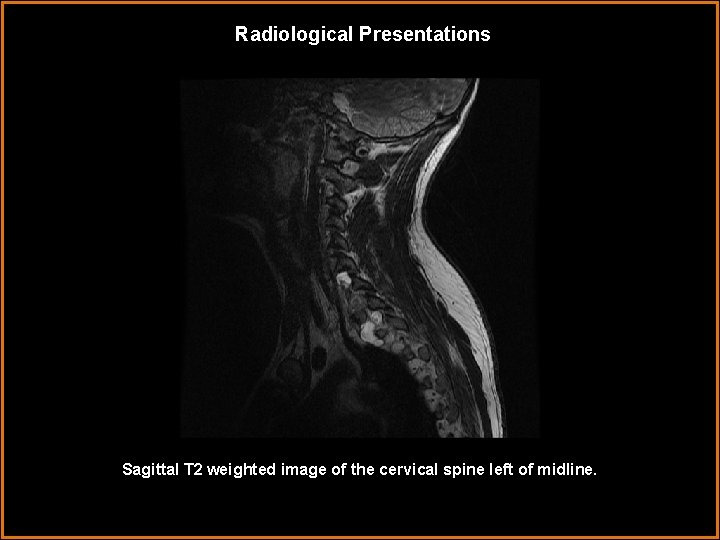
Radiological Presentations Sagittal T 2 weighted image of the cervical spine left of midline.
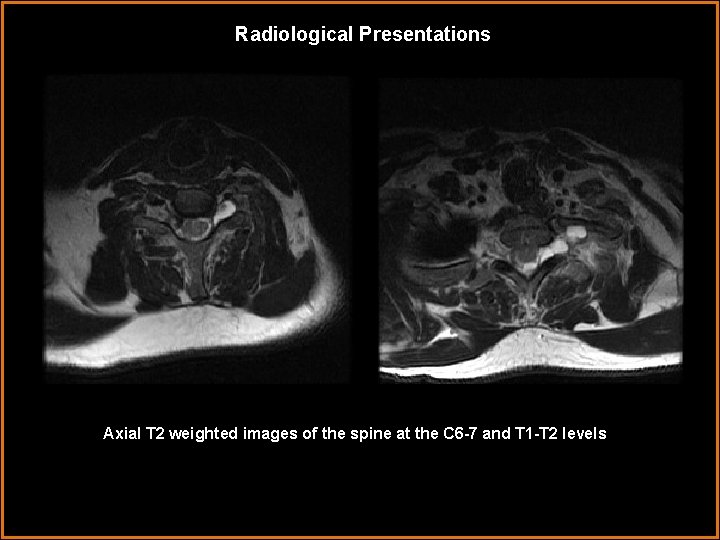
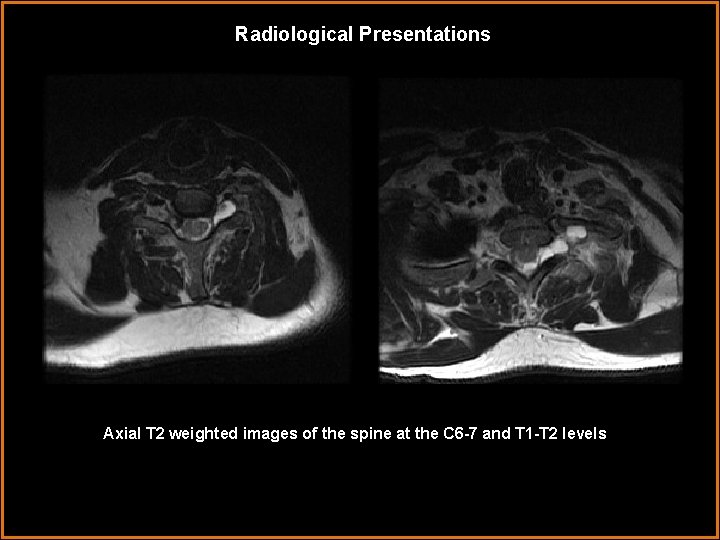
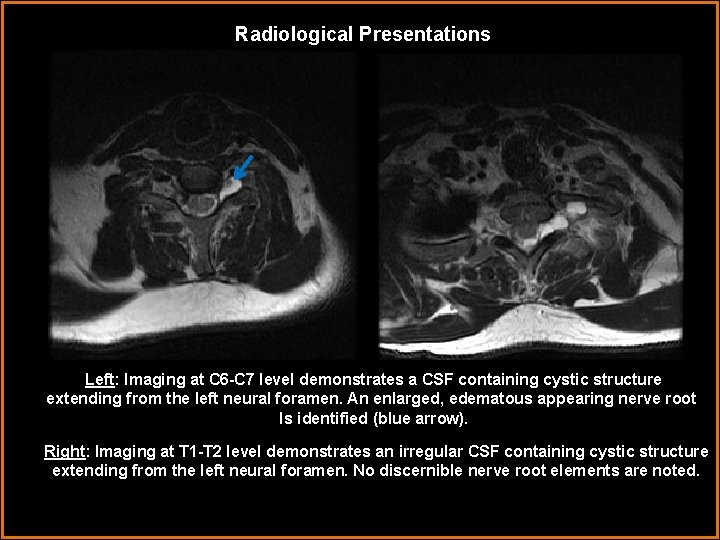
Radiological Presentations Axial T 2 weighted images of the spine at the C 6 -7 and T 1 -T 2 levels
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Multiple perineural cysts • Nerve root avulsion/stretch injuries • Neurofibromas • Lateral meningoceles
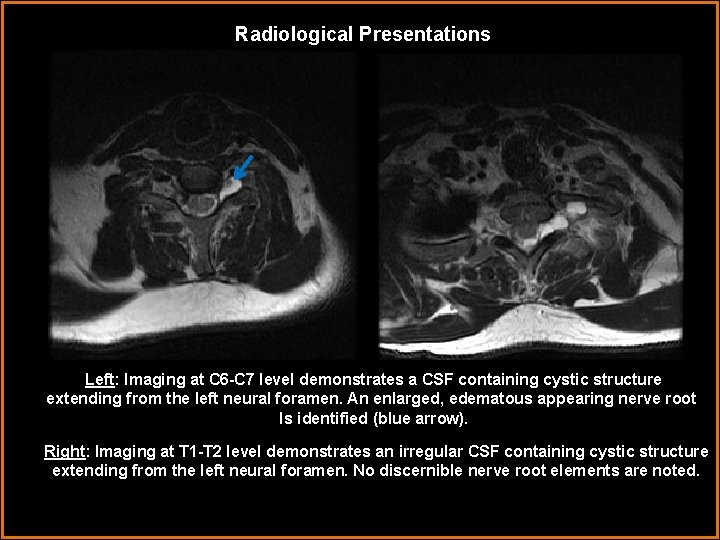
Radiological Presentations Left: Imaging at C 6 -C 7 level demonstrates a CSF containing cystic structure extending from the left neural foramen. An enlarged, edematous appearing nerve root Is identified (blue arrow). Right: Imaging at T 1 -T 2 level demonstrates an irregular CSF containing cystic structure extending from the left neural foramen. No discernible nerve root elements are noted.
Findings and Differentials Findings: Irregular appearing CSF intensity cystic structures extend from the left neural foramina at C 6 -7 and T 1 -2. At C 6 -7, the nerve root appears anteriorly displaced and enlarged within the cystic lesion. No readily identifiable nerve root elements are seen at T 1 -2. The contralateral neural foramina at both levels appear normal. There is no evidence of spinal canal stenosis or cord signal abnormality. Differentials: • Nerve root avulsion/stretch injuries • Multiple perineural cysts • Neurofibromas • Lateral meningoceles
Discussion A history of high velocity trauma is the key to understanding the findings. The patient’s neurologic findings in the left upper extremity were highly suggestive of an underlying brachial plexus injury. Axial T 2 images of the cervical spine depict multi-level left sided pseudomeningoceles – tears in the meningeal sheath resulting in CSF containing outpouchings. At T 1 -2, the neural elements appear markedly irregular and discontinuous compatible with a proximal avulsion injury. The pseudomeningocele is large and extends inferiorly to the T 3 level (not shown). The C 6 -7 pseudomeningocele is smaller and demonstrates a displaced and edematous segment of the nerve root. It is difficult to determine whethere is an avulsion vs. stretch injury at this level. A nerve root stretch injury involves enlargement or attenuation of stretched but contiguous neural elements. Unlike avulsion injuries whose deficits are irreversible, these have the potential of regaining a degree of function over time. Management is typically conservative although surgical repair can be performed in certain post-ganglionic injuries. The patient underwent physical therapy as neurosurgery was not an option.
Diagnosis Differential considerations in the non-traumatic setting include: Multiple perineural (Tarlov) cysts – These are typically thin walled cystic structures whose contents follow CSF intensity. They are common, incidental, and usually asymptomatic. They may cause adjacent bony remodeling and widening of the involved neural foramen. Cysts are most frequently seen in the lumbar spine and sacral region. Sometimes they are multiple and bilateral. The spinal root traverses through the cyst unlike this case where the neural elements are disrupted. Nerve sheath tumors – Neurofibromas are neoplasms containing Schwann cells, fibroblasts, and peripheral nerve fibers. 90% are sporadic and can be solitary, diffuse or plexiform. Plexiform neurofibromas are pathognomonic for NF-1. They are typically cervical and lumbosacral in location and can be bilateral and multilevel in distribution. These lesions are typically long and bulky causing multinodular nerve enlargement. They also demonstrate variable degrees of enhancement unlike the pathology seen here. Lateral meningoceles – CSF signal meningeal protrusion through a neural foramen into adjacent tissues. Found in the thoracic > lumbar spine with 10% being bilateral. If present, one should investigate for presence of NF-1 or Marfan’s syndrome. Unlike nerve sheath tumors, these do not enhance.
Diagnosis Unilateral nerve root injuries at C 6 -7 to T 1 -2 secondary to high velocity trauma.

References 1. Castillo M. Imaging the anatomy of the brachial plexus: review and self-assessment module. Am J Roentgenol 2005; 185: S 196– 204. 2. Yoshikawa T, Hayashi N, Yamamoto S, et al. Brachial plexus injury: clinical manifestations, conventional imaging findings, and the latest imaging techniques. Radiographics 2006; 26: S 133– 43
 Ohsu neuroradiology
Ohsu neuroradiology E-rate category 1 vs category 2
E-rate category 1 vs category 2 Radiological dispersal device
Radiological dispersal device Tennessee division of radiological health
Tennessee division of radiological health Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Mri principal
Mri principal Crow's foot notation
Crow's foot notation Cardinality and modality
Cardinality and modality Epistemic modality
Epistemic modality Modality in software engineering
Modality in software engineering What is modality in statistics
What is modality in statistics