Radiological Category Neuroradiology Principal Modality 1 MRI Principal







- Slides: 39
Radiological Category: Neuroradiology Principal Modality (1): MRI Principal Modality (2): CTA, Angiography Case Report # 809 Submitted by: Cantrell, Sarah M. D. Faculty reviewer: Sitton, Clark, M. D. , The University of Texas Medical School at Houston Date accepted: 15 April, 2011

Case History 9 year old with presents after having suffered left sided paresis and rightward eye deviation followed by progressive decline in level of consciousness and seizure that began at 11 am while in school. EMS was called by school RN and patient was brought to MHH ED. Significant past medical history includes history of symptoms associated with increased intracranial pressure evaluated at OSH that was assumed to be hydrocephalus/pseudotumor cerebri of unclear etiology and treated with Diamox.
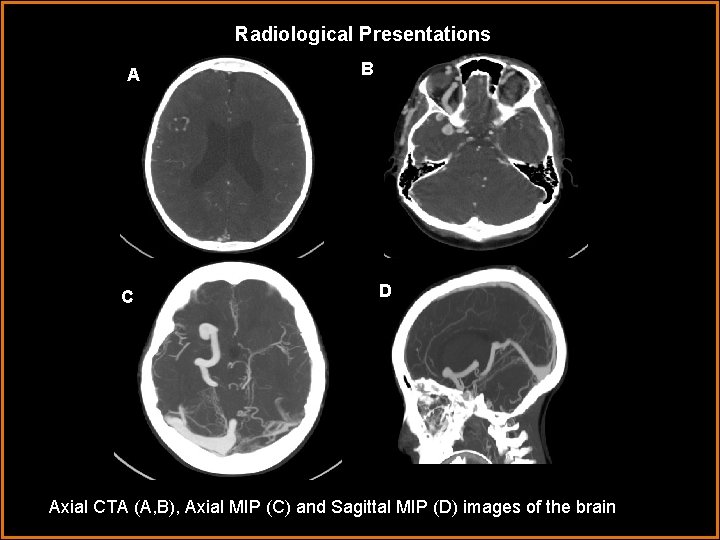
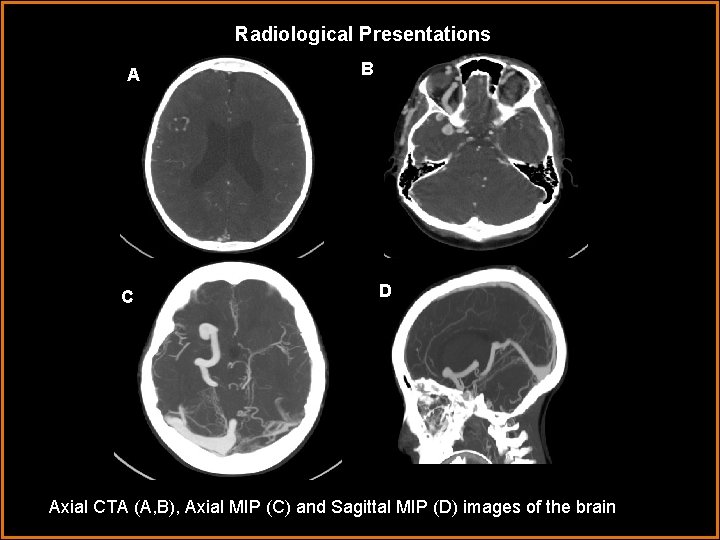
Radiological Presentations A C B D Axial CTA (A, B), Axial MIP (C) and Sagittal MIP (D) images of the brain
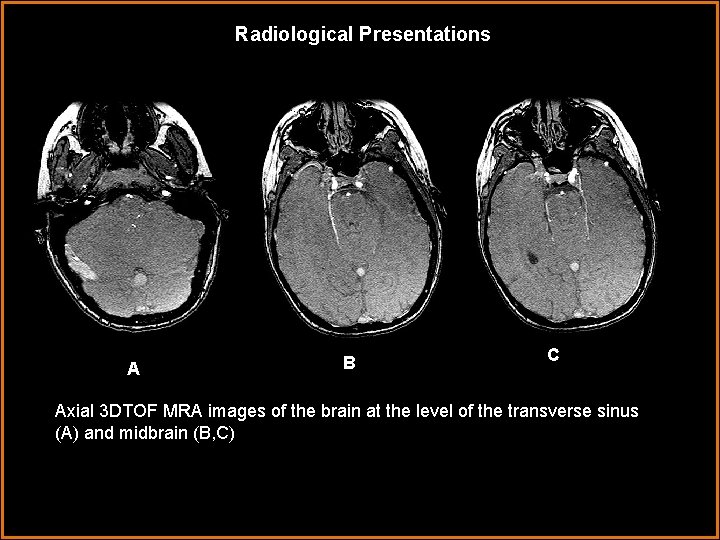
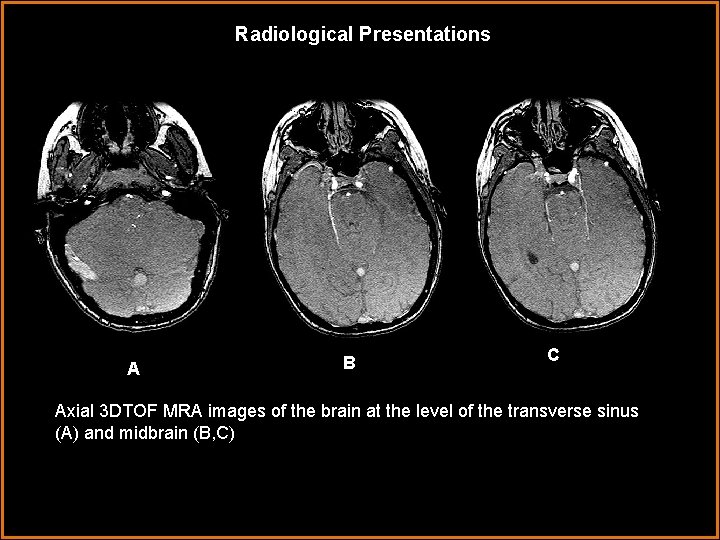
Radiological Presentations AA B C Axial 3 DTOF MRA images of the brain at the level of the transverse sinus (A) and midbrain (B, C)
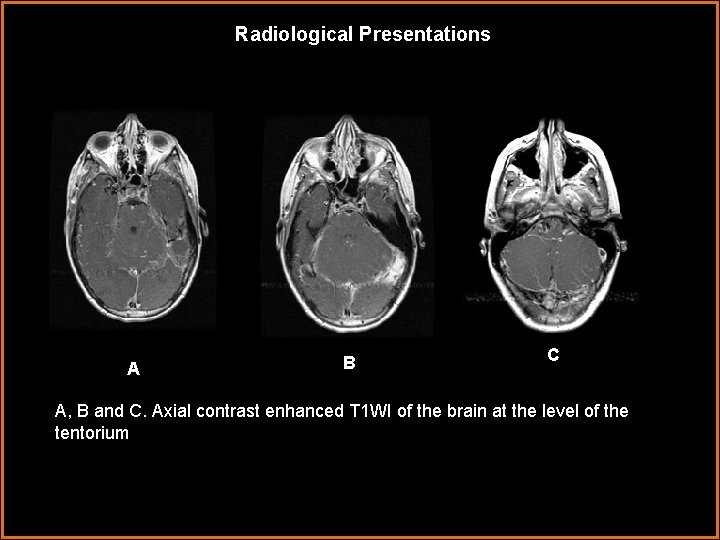
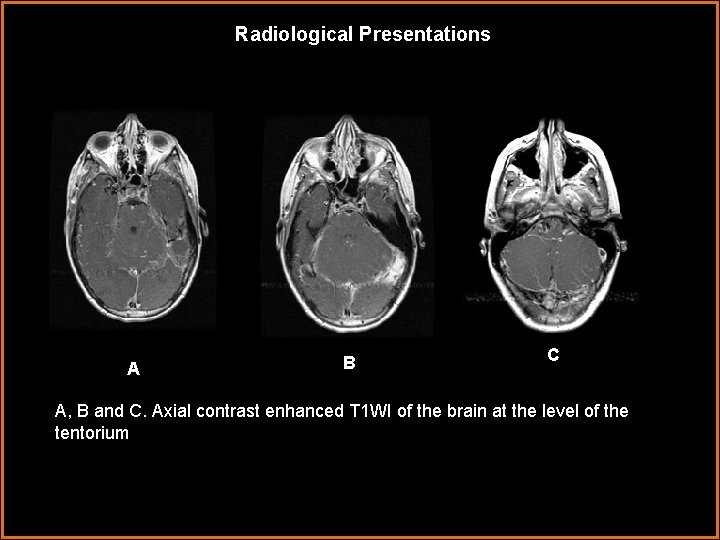
Radiological Presentations AA B C A, B and C. Axial contrast enhanced T 1 WI of the brain at the level of the tentorium
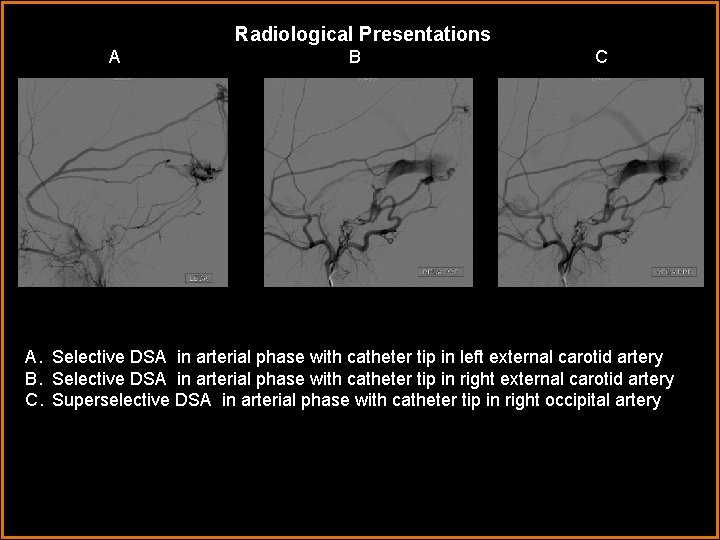
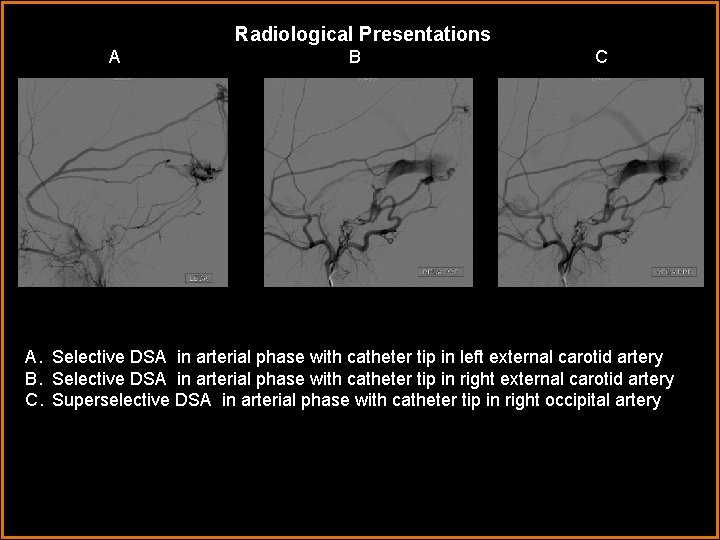
Radiological Presentations A B C A. Selective DSA in arterial phase with catheter tip in left external carotid artery A B. Selective DSA in arterial phase with catheter tip in right external carotid artery C. Superselective DSA in arterial phase with catheter tip in right occipital artery
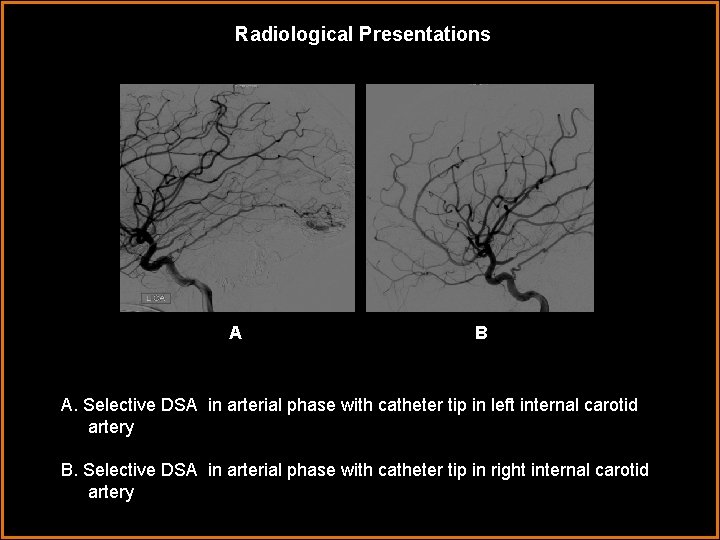
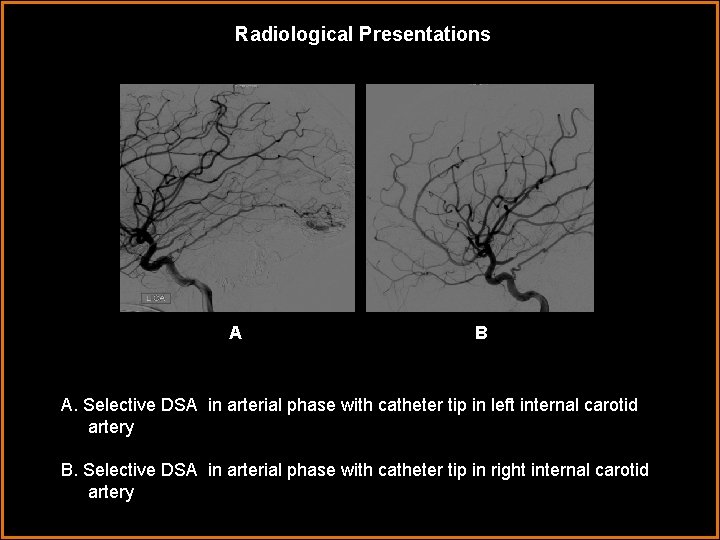
Radiological Presentations AA B A. Selective DSA in arterial phase with catheter tip in left internal carotid artery B. Selective DSA in arterial phase with catheter tip in right internal carotid artery

Radiological Presentations A A B A & B. Selective DSA in late venous filling phase with catheter tip in right external carotid artery
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Dural arteriovenous fistula, acquired • Arteriovenous malformation • Thrombosed dural venous sinus
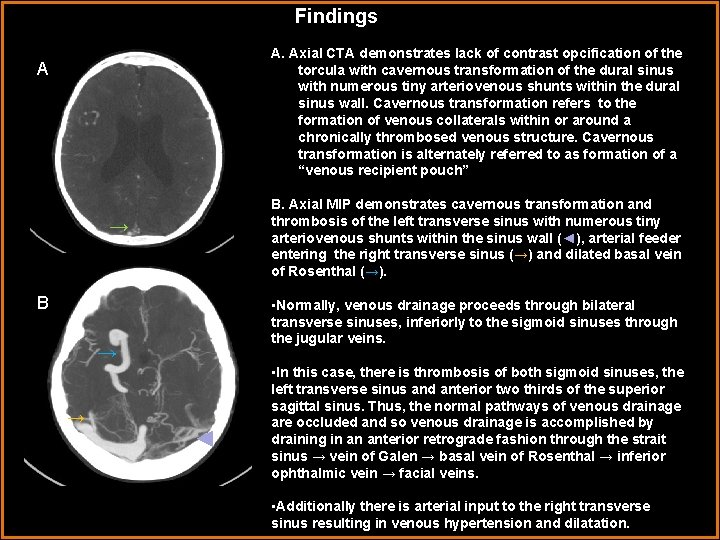
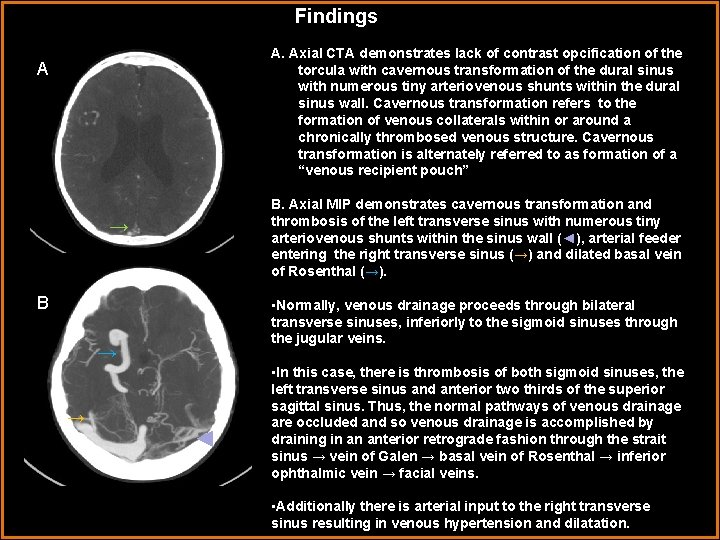
Findings A. Axial CTA demonstrates lack of contrast opcification of the torcula with cavernous transformation of the dural sinus with numerous tiny arteriovenous shunts within the dural sinus wall. Cavernous transformation refers to the formation of venous collaterals within or around a chronically thrombosed venous structure. Cavernous transformation is alternately referred to as formation of a “venous recipient pouch” A B. Axial MIP demonstrates cavernous transformation and thrombosis of the left transverse sinus with numerous tiny arteriovenous shunts within the sinus wall (◄), arterial feeder entering the right transverse sinus (→) and dilated basal vein of Rosenthal (→). → B • Normally, venous drainage proceeds through bilateral transverse sinuses, inferiorly to the sigmoid sinuses through the jugular veins. → → ◄ • In this case, there is thrombosis of both sigmoid sinuses, the left transverse sinus and anterior two thirds of the superior sagittal sinus. Thus, the normal pathways of venous drainage are occluded and so venous drainage is accomplished by draining in an anterior retrograde fashion through the strait sinus → vein of Galen → basal vein of Rosenthal → inferior ophthalmic vein → facial veins. • Additionally there is arterial input to the right transverse sinus resulting in venous hypertension and dilatation.
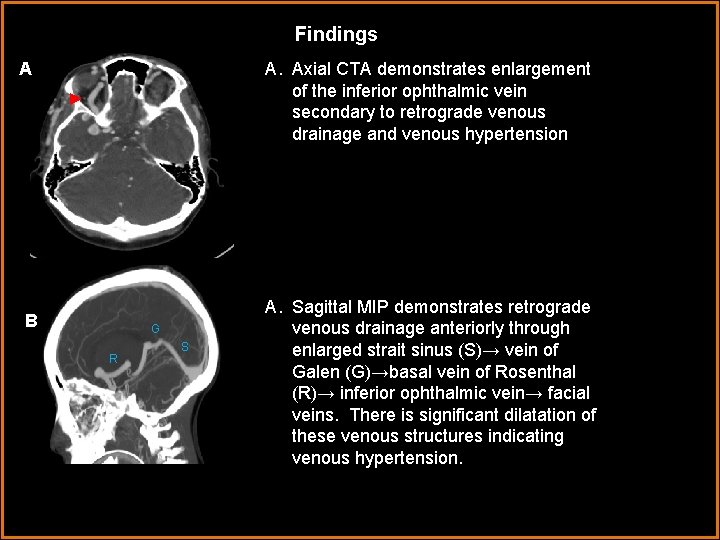
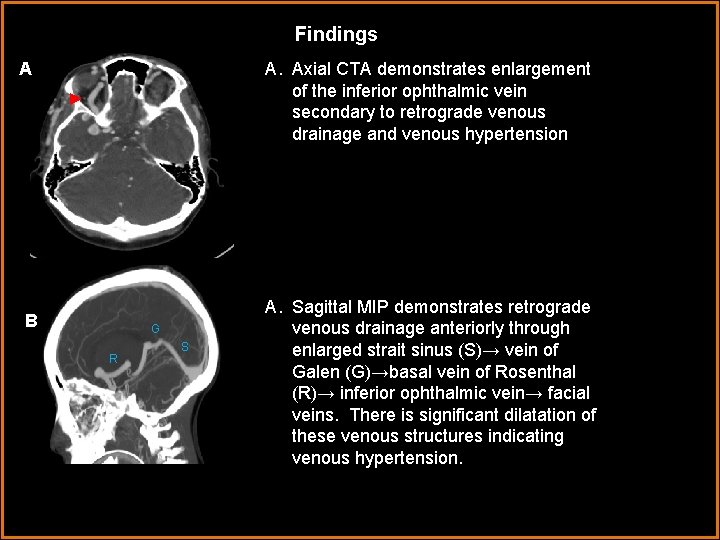
Findings A. Axial CTA demonstrates enlargement of the inferior ophthalmic vein secondary to retrograde venous drainage and venous hypertension A ► B G R S A. Sagittal MIP demonstrates retrograde venous drainage anteriorly through enlarged strait sinus (S)→ vein of Galen (G)→basal vein of Rosenthal (R)→ inferior ophthalmic vein→ facial veins. There is significant dilatation of these venous structures indicating venous hypertension.
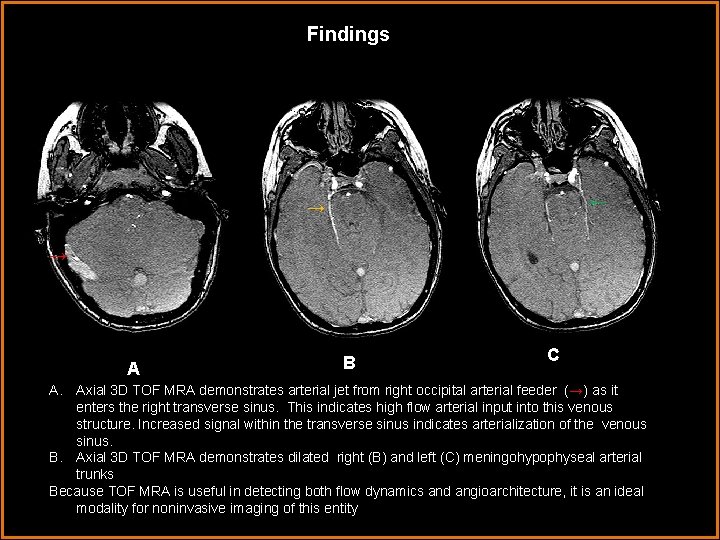
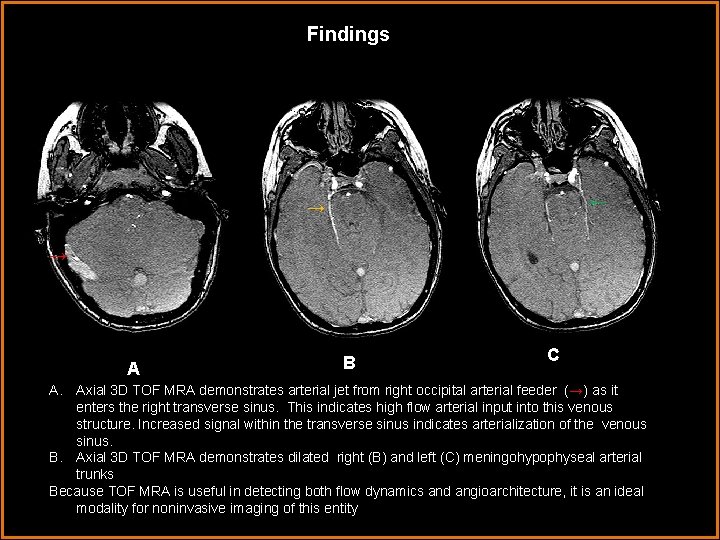
Findings ← → → AA B C A. Axial 3 D TOF MRA demonstrates arterial jet from right occipital arterial feeder (→) as it enters the right transverse sinus. This indicates high flow arterial input into this venous structure. Increased signal within the transverse sinus indicates arterialization of the venous sinus. B. Axial 3 D TOF MRA demonstrates dilated right (B) and left (C) meningohypophyseal arterial trunks Because TOF MRA is useful in detecting both flow dynamics and angioarchitecture, it is an ideal modality for noninvasive imaging of this entity

Findings ↓ AA ↓↓ ↓ ↓ B C A, B and C. Axial contrast enhanced T 1 WI at the level of the tentorium demonstrate dilated enhancing venous collaterals along the surface of the cerebellum. The dilated appearance of these collaterals and edematous appearance of the cerebellum are consistent with significant venous hypertension.
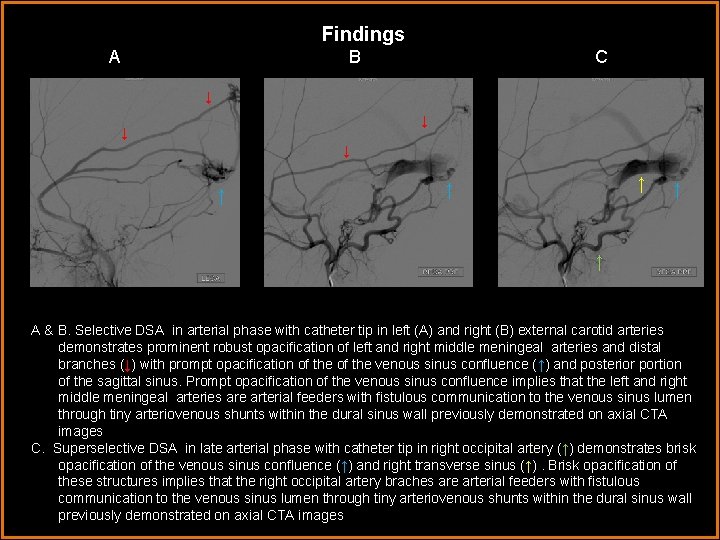
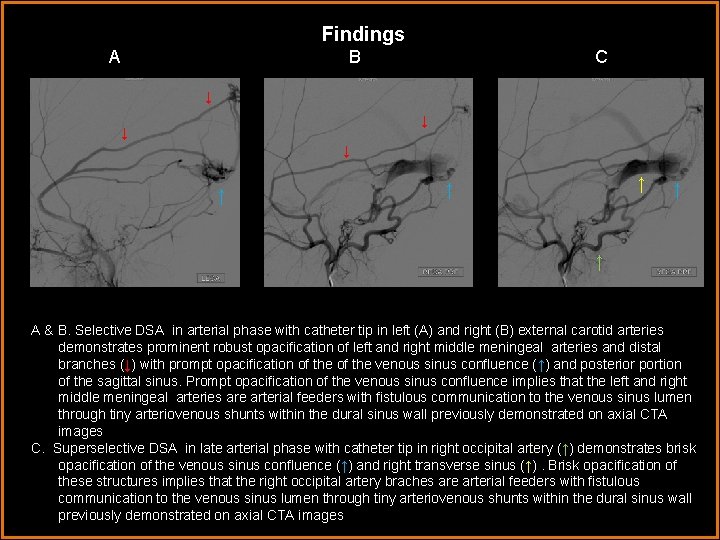
Findings A B C ↓ ↓ ↑ ↑ ↑ A & B. Selective DSA in arterial phase with catheter tip in left (A) and right (B) external carotid arteries demonstrates prominent robust opacification of left and right middle meningeal arteries and distal branches. A (↓) with prompt opacification of the venous sinus confluence (↑) and posterior portion of the sagittal sinus. Prompt opacification of the venous sinus confluence implies that the left and right middle meningeal arteries are arterial feeders with fistulous communication to the venous sinus lumen through tiny arteriovenous shunts within the dural sinus wall previously demonstrated on axial CTA images C. Superselective DSA in late arterial phase with catheter tip in right occipital artery (↑) demonstrates brisk opacification of the venous sinus confluence (↑) and right transverse sinus (↑). Brisk opacification of these structures implies that the right occipital artery braches are arterial feeders with fistulous communication to the venous sinus lumen through tiny arteriovenous shunts within the dural sinus wall previously demonstrated on axial CTA images
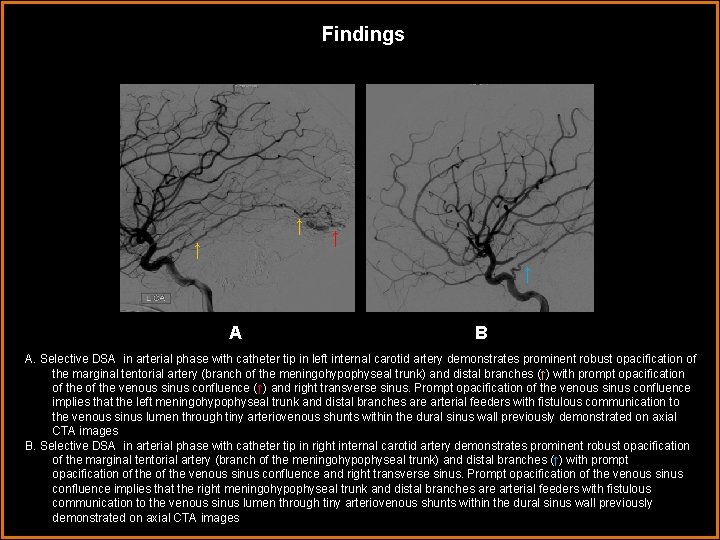
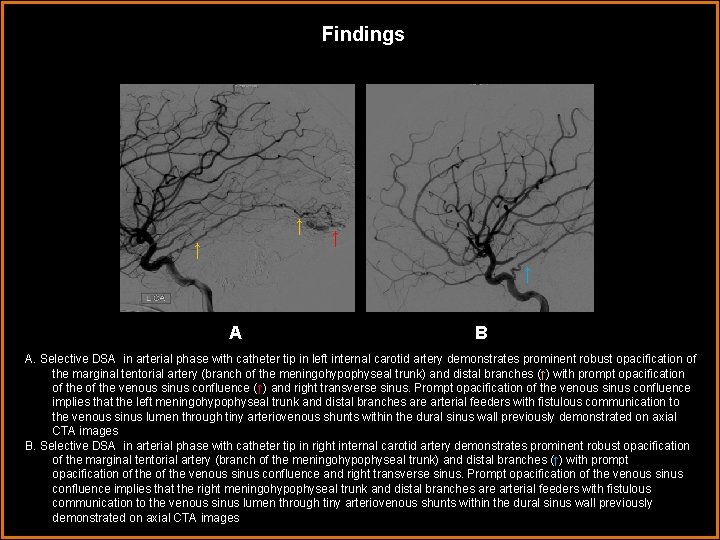
Findings ↑ ↑ AA B A. Selective DSA in arterial phase with catheter tip in left internal carotid artery demonstrates prominent robust opacification of the marginal tentorial artery (branch of the meningohypophyseal trunk) and distal branches (↑) with prompt opacification of the venous sinus confluence (↑) and right transverse sinus. Prompt opacification of the venous sinus confluence implies that the left meningohypophyseal trunk and distal branches are arterial feeders with fistulous communication to the venous sinus lumen through tiny arteriovenous shunts within the dural sinus wall previously demonstrated on axial CTA images B. Selective DSA in arterial phase with catheter tip in right internal carotid artery demonstrates prominent robust opacification of the marginal tentorial artery (branch of the meningohypophyseal trunk) and distal branches (↑) with prompt opacification of the venous sinus confluence and right transverse sinus. Prompt opacification of the venous sinus confluence implies that the right meningohypophyseal trunk and distal branches are arterial feeders with fistulous communication to the venous sinus lumen through tiny arteriovenous shunts within the dural sinus wall previously demonstrated on axial CTA images
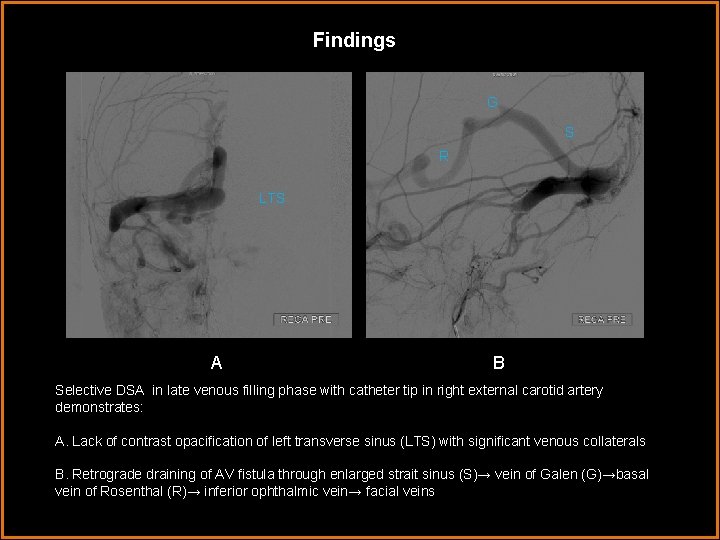
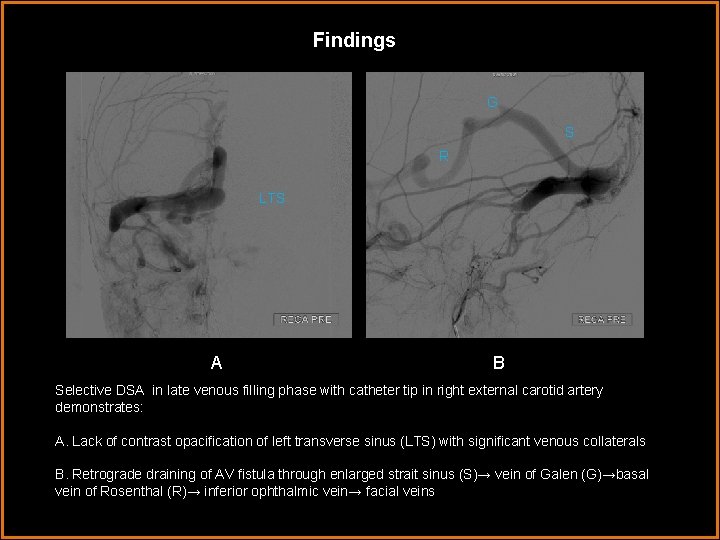
Findings G S R LTS A A B Selective DSA in late venous filling phase with catheter tip in right external carotid artery demonstrates: A. Lack of contrast opacification of left transverse sinus (LTS) with significant venous collaterals B. Retrograde draining of AV fistula through enlarged strait sinus (S)→ vein of Galen (G)→basal vein of Rosenthal (R)→ inferior ophthalmic vein→ facial veins
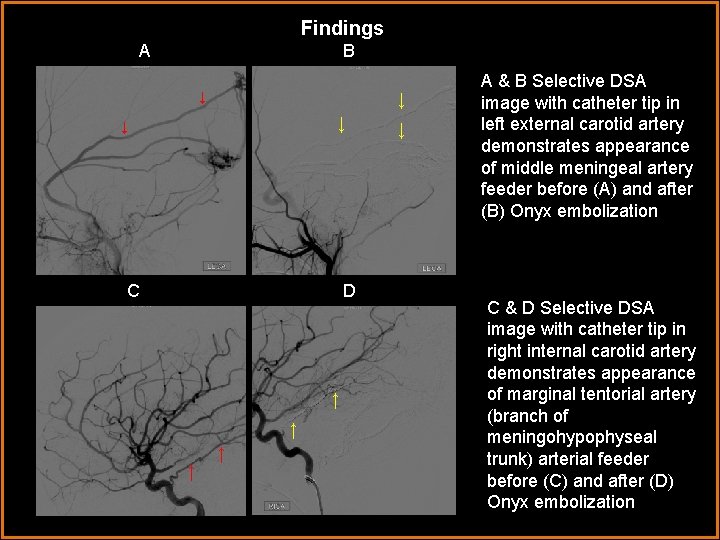
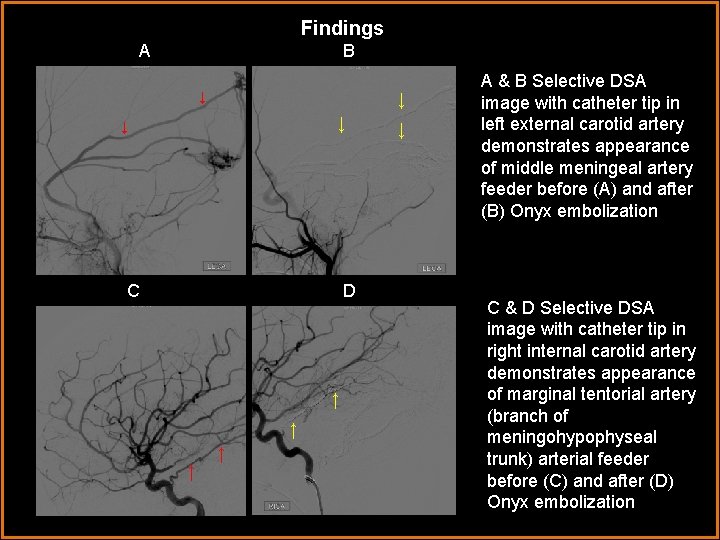
Findings A B ↓ ↓ C D A ↑↑ ↑↑ ↓ A & B Selective DSA image with catheter tip in left external carotid artery demonstrates appearance of middle meningeal artery feeder before (A) and after (B) Onyx embolization C & D Selective DSA image with catheter tip in right internal carotid artery demonstrates appearance of marginal tentorial artery (branch of meningohypophyseal trunk) arterial feeder before (C) and after (D) Onyx embolization

Findings The most salient feature within all images is marked venous hypertension. Imaging findings of intracranial venous hypertension include: • NECT: demonstrates hypodense parenchyma with effacement of sulci in regions of cerebral edema which do not have adequate venous drainage • CECT: demonstrates dilated draining veins and aforementioned features of cerebral edema • MRI: T 1 W 1: demonstrates hypointense edematous brain parenchyma • T 1+C: demonstrates dilated enhancing venous sinuses and cortical veins with decreased signal intensity of surrounding edematous brain parenchyma. • T 2 W 1: demonstrates increased signal intensity within surrounding edematous brain parenchyma indicating retrograde leptomeningeal flow • TOF MRA: increased signal intensity correlates with high flow and thus arterialization of venous structrures, if present, is readily apparent • Angiogram: demonstrates dilated venous sinuses and cortical veins. Stagnate flow, slow flow and retrograde flow within dilated venous structures are apparent on real time conventional angiography
Findings Differential diagnosis for intracranial venous hypertension includes: • Arteriovenous malformation • Dural arteriovenous fistula • Venous sinus thrombosis Following discussion of each of the above individually, a summary detailing how to differentiate among the three will be provided.
Discussion Dural AV fistula • • Definition: network of tiny arteriovenous shunts resulting in direct communication between small dilated arteries within the wall of a chronically thrombosed/stenosed dural venous sinus and the dural venous sinus lumen. Etiology: – Chronic thrombosis of a dural venous sinus results in pathologic activation of neoangiogenesis and direct fistulous communication of the venous sinus lumen with tiny arteries within the sinus wall. This results in the formation of innumerable arteriovenous shunts within the sinus wall. – Communication with arterial “feeders” results in arterializations of the venous sinus, increased pressure within the venous sinus and increased venous back pressure. – In response to increased venous pressure and impaired venous drainage, cortical veins dilate. With significantly elevated pressure, retrograde and stagnate flow results. – Consequences of impaired venous drainage by dilated, high pressure cortical veins include parenchymal hemorrhage, subarachnoid hemorrhage, venous infarction and increased intracranial pressure
Discussion Dural AV fistula • • Location: most commonly the transverse and cavernous sinuses Clinical Presentation: depends on size and location of lesion – Parenchymal hemorrhage, seizure, altered mental status secondary to increased intracranial pressure – Glaucoma, visual loss and proptosis: cavernous sinus dural AV fistula with resultant nontraumatic cavernous carotid fistula and impaired venous drainage from the ophthalmic vein – Tinnitus and bruit heard best over the temporal bone: sigmoid sinus dural AV fistula – Increased intracranial pressure and intacerebral hemorrhage: transverse and superior saggital sinus dural AV fistula
Discussion Dural AV fistula Staging/grading: Cognard classification system: focuses on correlation between intracerebral hemorrhage, venous drainage pattern and degree of venous hypertension I – Antegrade sinus drainage II – Insufficient antegrade sinus drainage IIa – Retrograde sinus drainage only IIb – Retrograde cortical venous reflux (CVR) only (10 -20% hemorrhage rate) III – CVR only without venous ectasia (40% hemorrhage rate) IV – CVR only with venous ectasia (66% hemorrhage rate) V – Spinal venous drainage

Discussion Dural AV Fistula Imaging CT Findings • NECT: most often normal. May see hyperdense clot within venous sinus. • CTA: may show tortuous, dilated feeding arteries with enlarged dural sinuses and cortical draining veins. MRI Findings • T 1 WI: isointense thrombosed dural sinus ± "flow voids“ • T 2 WI: hyperintensity of brain parenchyma adjacent to thrombosed sinus secondary to impaired venous drainage and retrograde flow. Thrombosed sinus may be isointense ± "flow voids“ • FLAIR: Venous congestion of adjacent brain parenchyma and isointense thrombosed sinus • DWI: No restricted diffusion unless ischemia of brain parenchyma is present • T 1 WI C+: may show enlarged draining veins • MRA: TOF MRA useful in depicting both flow dynamics and angioarchitecture. In high flow lesions, may see arterial jet in very high flow vessels. May be negative with slow flow shunts. • MRV: demonstrates occluded sinus and collateral flow.
Discussion Dural AV Fistula Imaging • Angiographic Findings • Demonstrates dural and transosseous feeders and arterial inflow into “recipient pouch” composed of parallel venous channels. • Demonstrates thrombosis of parent sinus with extensive venous collaterals • Delayed filling and flow reversal within dural sinus and draining cortical veins due to venous hypertension
Discussion Dural AV Fistula Treatment • Treatment: goal is to eliminate venous hypertension resulting from dural arteriovenous fistula • 2 options: – transarterial endovascular embolization – Surgery • Surgery is reserved for dural arteriovenous fistulas involving the tentorium and frontobasis, which often require a combination of surgery and endovascular embolization. Anterior fossa dural arteriovenous fistulas involving the ophthalmic arteries require surgical disconnection of the arterial feeders.
Discussion Dural AV Fistula Treatment • Transarterial embolization: – Infusion of intraarterial agents is achieved through insertion of a microcatheter through the femoral artery then selective catheterization of meningeal arterial feeders, most often arising from the external carotid artery. The catheter is advanced to the distal portion of the feeding artery and intraarterial embolic agent is injected into the distal portion of the feeder meningeal artery, through the arteriovenous shunt within the wall of the venous sinus proximal venous pouch. The goal is for the embolic agent to cross the arteriovenous fistula and occlude the proximal venous pouch. – Onyx is a commonly used liquid embolic agent composed of EVOH (ethylene vinyl alcohol) copolymer dissolved in DMSO (dimethyl sulfoxide) and suspended micronized tantalum powder to provide contrast for visualization under fluoroscopy. – Unlike previous agents, onyx does not polymerize but instead precipitates as DMSO diffuses under aqueous conditions, solidifying upon contact with blood, thereby forming a spongy embolus. Initial injection with Onyx forms a cast which is gradually filled with each injection.
Discussion Arteriovenous Malformation Definition: Vascular malformation composed of one or more enlarged feeding arteries, a nidus and an enlarged draining vein with no intervening brain parenchyma. The nidus is composed of a network of tiny arteriovenous shunts. Intranidal aneurysms are found in up to 50%. Increased number or intranidal aneurysms and decreased number and size of draining veins within an unruptured AVM is associated with increased risk of intracranial hemorrhage. Etiology: Congenital anomaly resulting from dysregulated angiogenesis Location: 85% supratentorial, 15% posterior fossa

Discussion Arteriovenous Malformation Associated with Wyburn-Mason syndrome (retinal, cutaneous, mandibular and brain stem vascular malformations), Klippel-Trenaunay-Weber syndrome (hemihypertrophy, angiomatosis of extremity and brain), Sturge Weber spectrum, and hereditary hemorrhagic telangiectasia (mucocutaneous telangiectasias and visceral AVMs) Clinical presentation: most present between 20 -40 years of age with headache, seizure , focal neurologic deficits or nontraumatic intracranial hemorrhage. Steal phenomenon has been observed secondary to ischemia of surrounding brain parenchyma resulting from preferential shunting of blood away from normal brain parenchyma toward the AV malformation. Treatment: embolization, microneurosurgical resection and stereotactic radiosurgery
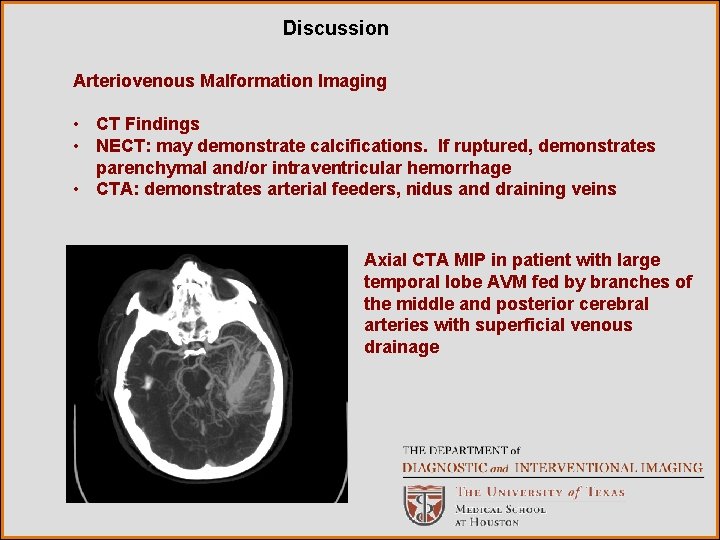
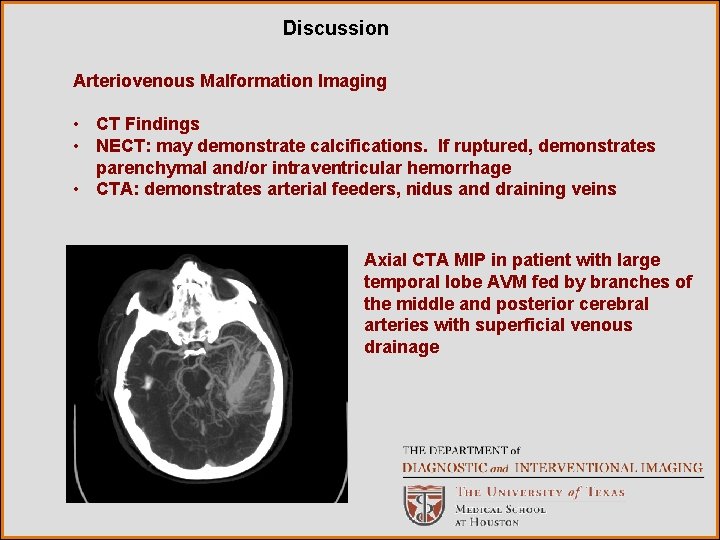
Discussion Arteriovenous Malformation Imaging • CT Findings • NECT: may demonstrate calcifications. If ruptured, demonstrates parenchymal and/or intraventricular hemorrhage • CTA: demonstrates arterial feeders, nidus and draining veins Axial CTA MIP in patient with large temporal lobe AVM fed by branches of the middle and posterior cerebral arteries with superficial venous drainage
Discussion Arteriovenous Malformations Imaging • MR Findings • T 1 WI: demonstrates nidus seen as a “honeycomb” of flow voids associated with a draining vein • T 2 WI: demonstrates nidus seen as a “honeycomb” of flow voids with no intervening brain parenchyma and associated draining vein. Gliotic brain parenchyma having suffered long term ischemia secondary to shunting phenomenon may demonstrate high signal intensity. • FLAIR: demonstrates flow voids within the nidus and may show high signal gliotic brain parenchyma • T 2* GRE: "Blooming" if hemorrhage present • T 1 WI C+: demonstrates enhancement within the nidus and draining veins. • MRA: most helpful in demonstrating flow post treatment; not particularly useful for demonstrating angioarchitecture • Angiographic Findings: best tool for delineating angioarchitecture. Demonstrates enlarged feeding arteries, aneurysms if present, nidus and early draining veins with/without venous stenosis due to high flow venopathy
Discussion Venous sinus thrombosis • Definition: occlusion of a dural venous sinus by thrombus or infectious material. Venous sinus thrombosis may result in propagation to cortical veins with resultant elevation of venous pressures and impaired venous outflow from congested brain parenchyma. Eventually, increased venous pressures and vasogenic edema may lead to hemorrhage and cytotoxic edema. Herniation due to increased intracranial pressure from hemorrhage may occur in severe cases. • Etiology depends on patient demographics – Hypercoagulable state with a variety of predisposing factors including OCPs, pregnancy, collagen vascular disorders, vasculitis, inflammatory (IBD), sickle cell disease, protein S deficiency, prothrombin gene mutation – Trauma – Dehydration, mastoiditis, meningitis and sickle cell disease common causes in the pediatric population • Clinical presentation: headache, nausea, vomiting are most common. May or may not have neurologic deficit. High degree of clinical suspicion should be maintained in the appropriate clinical setting.
Discussion Venous Sinus Thrombosis • Staging and Grading: based on degree of venous ischemia – Type 1: No abnormality – Type 2: Hyperintense on T 2/FLAIR; no enhancement – Type 3: Hyperintense on T 2/FLAIR; enhancement – Type 4: Hemorrhage or venous infarction • Treatment: most often anticoagulation via heparin and coumadin. In severe cases endovascular mechanical thrombectomy with/without local heparin infusion may be attempted.
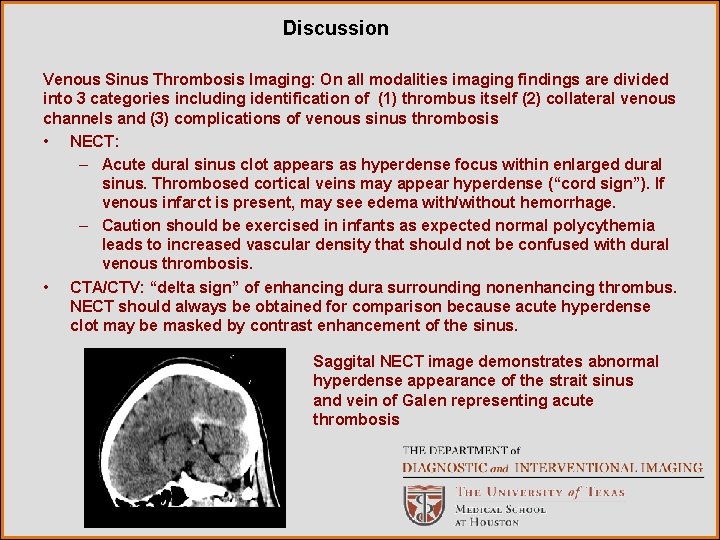
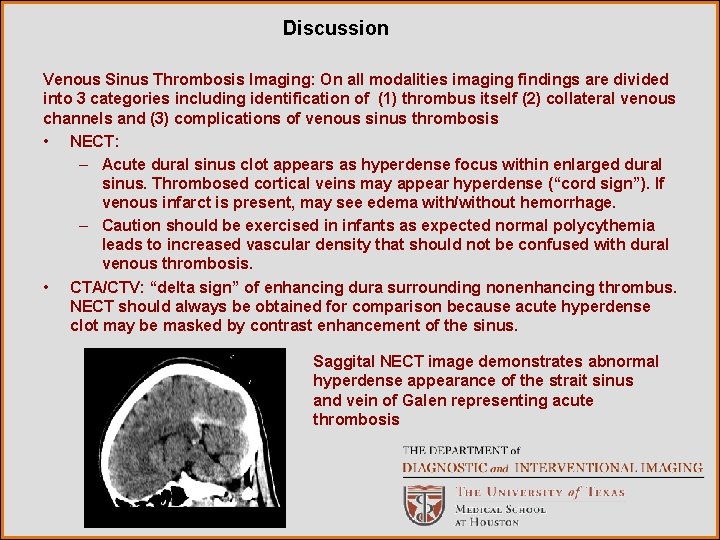
Discussion Venous Sinus Thrombosis Imaging: On all modalities imaging findings are divided into 3 categories including identification of (1) thrombus itself (2) collateral venous channels and (3) complications of venous sinus thrombosis • NECT: – Acute dural sinus clot appears as hyperdense focus within enlarged dural sinus. Thrombosed cortical veins may appear hyperdense (“cord sign”). If venous infarct is present, may see edema with/without hemorrhage. – Caution should be exercised in infants as expected normal polycythemia leads to increased vascular density that should not be confused with dural venous thrombosis. • CTA/CTV: “delta sign” of enhancing dura surrounding nonenhancing thrombus. NECT should always be obtained for comparison because acute hyperdense clot may be masked by contrast enhancement of the sinus. Saggital NECT image demonstrates abnormal hyperdense appearance of the strait sinus and vein of Galen representing acute thrombosis
Discussion Venous Sinus Thrombosis Imaging MR Findings: in general MRI is more useful than CT in detecting complications of venous thrombosis such as hemorrhage and edema • T 1 WI: signal intensity varies with age of the thrombus. Acute thrombus appears isointense. Subacute thrombus appears hyperintense. Chronic sinus thrombosis appears isointense. • T 2 WI: signal intensity varies with age of the thrombus. Acute thrombus appears hypointense (may be mistaken for normal flow void). Subacute thrombus appears hyperintense. Chronic sinus thrombosis appears hyperintense. Eventually, isointense signal develops as the sinus becomes fibrotic. • FLAIR: most useful for detecting venous infarction which appears hyperintense. • T 2* GRE Hypointense thrombus within sinus and cortical veins will demonstrate blooming artifact which improves conspicuity of thrombus • DWI: useful for determining venous infarction (DWI hyperintense with restricted diffusion) verses reversible venous edema (DWI hyperintense with increased diffusion) • T 1 WI C+: demonstrates enhancing dura around thrombus. Potential pitfall can occur with chronic thrombus which can demonstrate enhancement. • MRV: – 2 D TOF MRV: demonstrates absence of flow in occluded sinus, frayed or shaggy appearance of the venous sinus and abnormal collaterals. Potential pitfall of 2 D TOF MRV is that T 1 hyperintense intrasinus clot will mimic flow. This can be resolved by adding enhanced TOF sequence. • Angiographic Findings: occlusion of the involved sinus and collateral venous drainage
Discussion Unique imaging features of dural arteriovenous fistula that eliminate arteriovenous malformation and venous sinus thrombosis as possible diagnoses include: 1. Cavernous transformation of the thrombosed transverse and sagittal sinuses with numerous enhancing arteriovenous shunts within the sinus wall visualized on CTA. 2. Venous collaterals along the surface of the cerebellum visualized on contrast enhanced MRI T 1 WI. 3. Occipital feeder arterial jet with arterialization of the right transverse sinus seen on MRA, indicating direct fistulous communication of an arterial feeder with the dural venous sinus. 4. Arterial feeders arising from the meningeal arteries (middle and posterior meningeal arteries, artery of falx cerebelli, tentorial branches of cavernous ICA, occipital artery, artery of Davidoff and Schechter).
Discussion Why not AVM? In addition to the unique features of dural arteriovenous fistula discussed on the previous slide, this case also demonstrates: 1. Lack of a nidus: unlike arteriovenous malformations which are composed of arterial feeders, a nidus, and dilated draining veins, dural arteriovenous fistulas do not have a nidus. No nidus was demonstrated within this case. 2. Arterial supply arising from the meningeal arteries. Arteriovenous malformations have arterial supply arising from the pial arteries, not the meningeal arteries. Why not venous sinus thrombosis? Cavernous transformation of dural sinuses, venous collaterals, arterialization of the venous sinuses and fistulous communication between arterial and venous structures demonstrated within this case are not features of venous sinus thrombosis.

Diagnosis Dural Arteriovenous fistula
References Baleato González S, Vilanova Busquets JC, García Figueiras R, Villalba Martín C, Seoane Pose C, Martínez de Alegría A, Castiñeira Mourenza J. Imaging Arteriovenous Fistulas. Am. J. Roentgenol. , Nov 2009; 193: 1425 - 1433. Geibprasert S, Pongpech S, Jiarakongmun P, Shroff MM, Armstrong DC, Krings T. Radiologic assessment of brain arteriovenous malformations: what clinicians need to know. Radiographics. 2010 Mar; 30(2): 483 -501. Hirata E, Higashi T, Iwamuro Y, Watanabe Y, Ando M, Arakawa Y, Nakahara I. Angioplasty and stent deployment in acute sinus thrombosis following endovascular treatment of dural arteriovenous fistulae. J Clin Neurosci. 2009 May; 16(5): 725 -7. Epub 2009 Mar 4. Kai Y, Hamada J, Morioka M, Todaka T, Mizuno T, Ushio Y. Pre and post treatment MR imaging and single photon emission CT in patients with dural arteriovenous fistulas and retrograde leptomeningeal venous drainage. J Neuroradiol. 2003 Apr; 24(4): 619 -25. Kiyosue H, Hori Y, Okahara M, Tanoue S, Sagara Y, Matsumoto S, Nagatomi H, Mori H. . Treatment of intracranial dural arteriovenous fistulas: current strategies based on location and hemodynamics, and alternative techniques of transcatheter embolization. Radiographics. 2004 Nov-Dec; 24(6): 163753.
References Klisch J, Schumacher M. Dural arteriovenous fistulae: noninvasive diagnosis with dynamic MR digital subtraction angiography. AJNR Am J Neuroradiol. 2002 Oct; 23(9): 1614; author reply 1614 -5. Lagares A, Millán JM, Ramos A, Alén JA, Gallego JH. Perfusion computed tomography in a dural arteriovenous fistula presenting with focal signs: vascular congestion as a cause of reversible neurologic dysfunction. Neurosurgery. 2010 Jan; 66(1): E 226 -7 Miyamoto N, Naito I, Takatama S, Shimizy T, Iwai T, Schimaguchi H. Clinical and angiographic characteristics of cavernous sinus dural arteriovenous fistulas manifesting as venous infarction and/or intracranial hemorrhage. Neuroradiology. 2009 Jan; 51(1): 53 -60. Epub 2008 Oct 25. Noguchi K, Melhem ER, Kanazawa T, Kubo M, Kuwayama N, Seto H. Intracranial dural arteriovenous fistulas: evaluation with combined 3 D time-of-flight MR angiography and MR digital subtraction angiography. AJR Am J Roentgenol. 2004 Jan; 182(1): 183 -90. Probst EN. Dural arteriovenous fistula, a review. Clinical Neuroradiology 19: 91 -100. Yousem D, Grossman R. The Requisites Neuroradiology, Third Edition. Mosby, Inc Philadelphia 2010.
 Ohsu neuroradiology
Ohsu neuroradiology Pa erate
Pa erate Tennessee division of radiological health
Tennessee division of radiological health Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Radiological dispersal device
Radiological dispersal device Mri principal
Mri principal Epistemic modality
Epistemic modality Capacitive field diathermy
Capacitive field diathermy What is modality in statistics
What is modality in statistics Callendreasonlocaluserinitiated
Callendreasonlocaluserinitiated Sodality vs modality
Sodality vs modality Crow's foot notation
Crow's foot notation Epistemic modality
Epistemic modality Modality erd
Modality erd Modality in software engineering
Modality in software engineering Data modeling fundamentals
Data modeling fundamentals Birad
Birad Pacs modality workstation
Pacs modality workstation Modality
Modality Modality in software engineering
Modality in software engineering Characteristics of sensory neurons
Characteristics of sensory neurons Deontic modality
Deontic modality Modality in software engineering
Modality in software engineering Cardinality and modality
Cardinality and modality Modality
Modality Skill focus: persuasion
Skill focus: persuasion Mri position
Mri position Imelda bonheiden gynaecologie
Imelda bonheiden gynaecologie Pons radiology
Pons radiology Dog mri hancock county
Dog mri hancock county Mri
Mri Haghighat mri center
Haghighat mri center Osteopoikilosis mri
Osteopoikilosis mri Nmv mri
Nmv mri Red nucleus mri
Red nucleus mri How mri works
How mri works Cnr mri
Cnr mri Falks cerebri
Falks cerebri Fgatir ge mri
Fgatir ge mri