Quality Assurance in Diagnostic Medical Sonography HHHoldorf QUALITY


- Slides: 53

Quality Assurance in Diagnostic Medical Sonography HHHoldorf
QUALITY ASSURANCE 1. 2. 3. 4. Quality Assurance -The “routine” periodic evaluation of the US system to guarantee optimal image quality Requirements Assessment of system components Repairs Preventive maintenance Record keeping Done for medical and legal matters
QUALITY ASSURANCE Goals -proper equipment operation -detect gradual changes -minimize downtime -reduce number of repeat scans
QUALITY ASSURANCE Methods -test under known conditions -constant instrument settings *Results based on Transducer Type Receiver Gain Power Position of transducer Depth *Make sure that when testing equip. that the derived conclusion is system variation and not change in procedure -use phantom with measurable characteristics
QUALITY ASSURANCE Performed by the Sonographer -It is the duty of the sonographer to perform quality assurance -Although the manufacturer’s service engineer may be involved, the ultimate responsibility for QA always rests with the sonographer -Various aspects of all instrumentation should be routinely inspected to ensure consistency of its performance -It is important to validate the reliability of the images produced and the measurements made with each transducer on each US system.
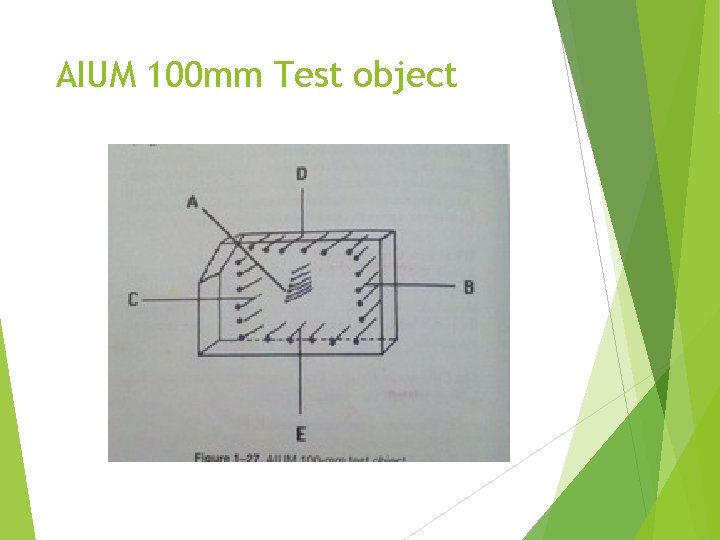
QUALITY ASSURANCE AIUM 100 mm Test Object -fluid filled tank containing strategically located stainless steel pins or plastic strings -speed of sound in the AIUM object is identical to that of soft tissue -Evaluates accuracy and performance characteristics of a system. -BUT, the AIUM test object does not have the attenuation properties of soft tissue, so a grayscale cannot be evaluated (BISTABLE)
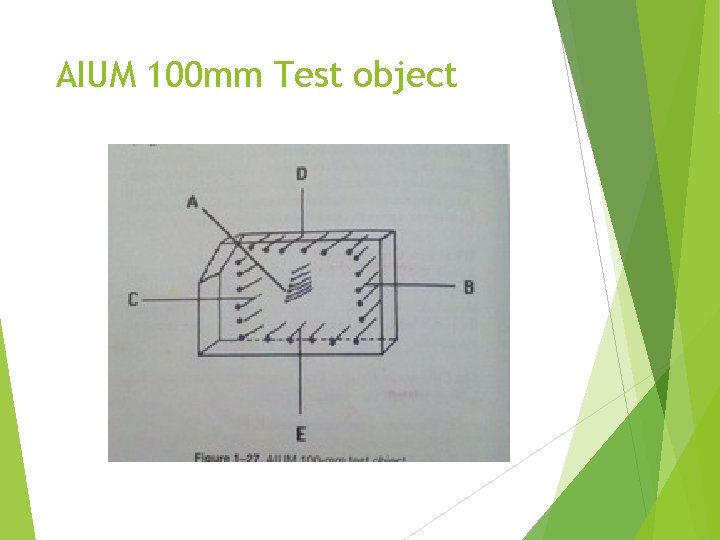
AIUM 100 mm Test object
QUALITY ASSURANCE 1. 2. 3. 4. Placing the transducer on the top, sides and on the oblique side of the object provides a variety of orientations between the sound beam and the pins. Axial resolution= evaluated when the pins in the test object are parallel to the sound beam’s main axis Lateral resolution= evaluated when the pins in the test object are perpendicular to the sound beam Electronic caliper accuracy= evaluated by comparing the distances between reflections on the display with the actual distances in the test object Dead zone= evaluated by scanning the pins located at the top of the test object, very close to the transducer.
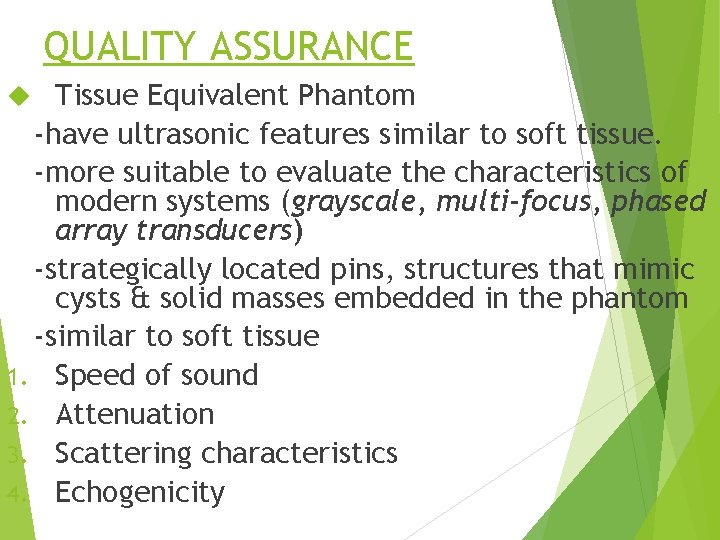
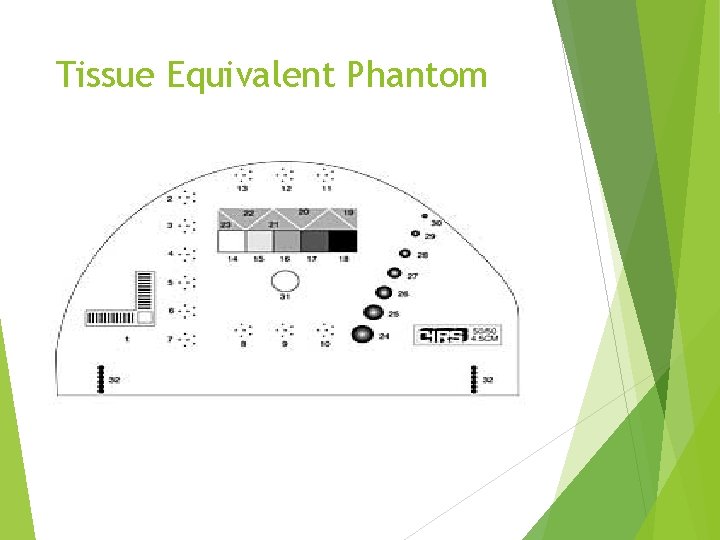
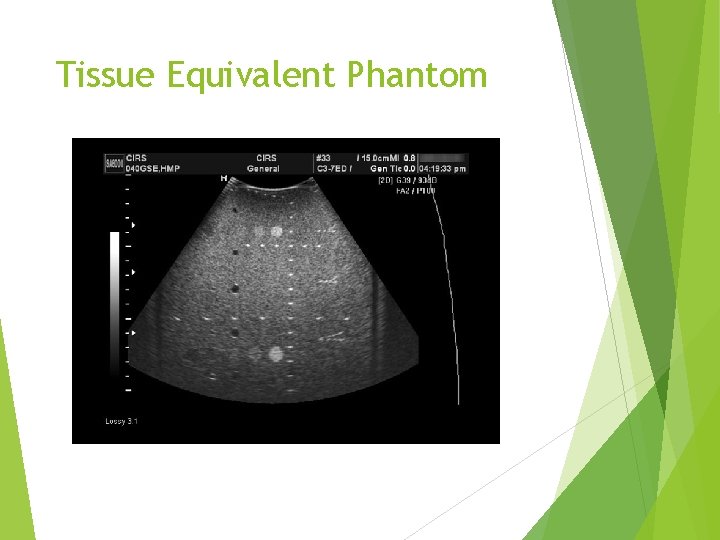
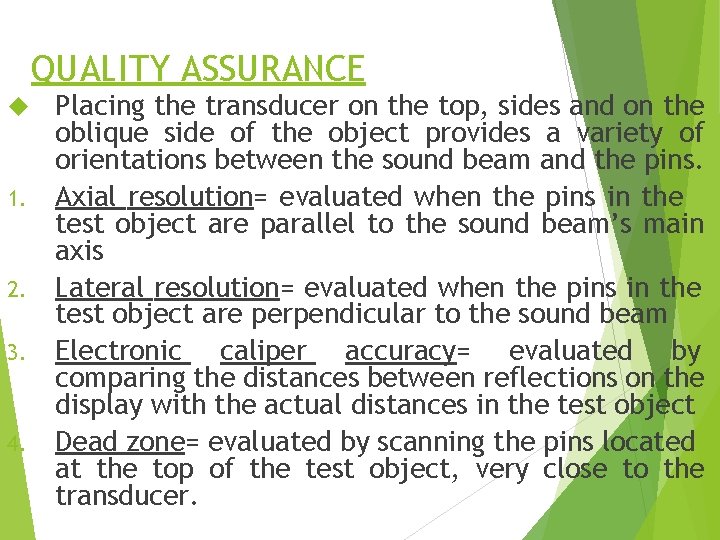
QUALITY ASSURANCE Tissue Equivalent Phantom -have ultrasonic features similar to soft tissue. -more suitable to evaluate the characteristics of modern systems (grayscale, multi-focus, phased array transducers) -strategically located pins, structures that mimic cysts & solid masses embedded in the phantom -similar to soft tissue 1. Speed of sound 2. Attenuation 3. Scattering characteristics 4. Echogenicity
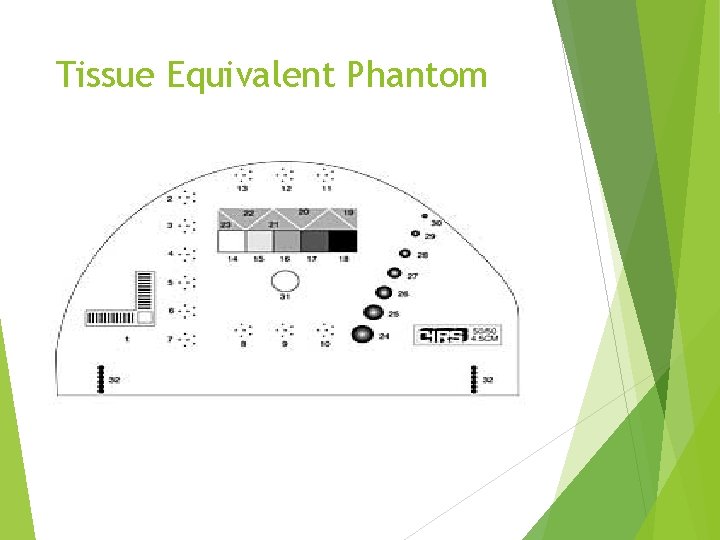
Tissue Equivalent Phantom
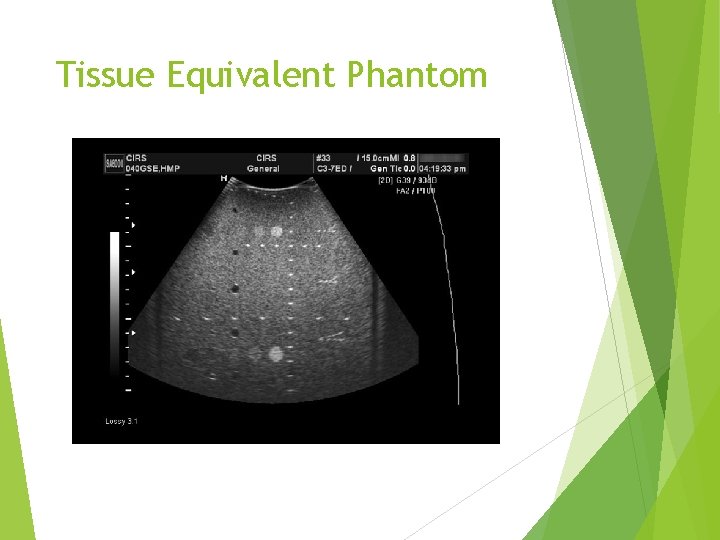
Tissue Equivalent Phantom
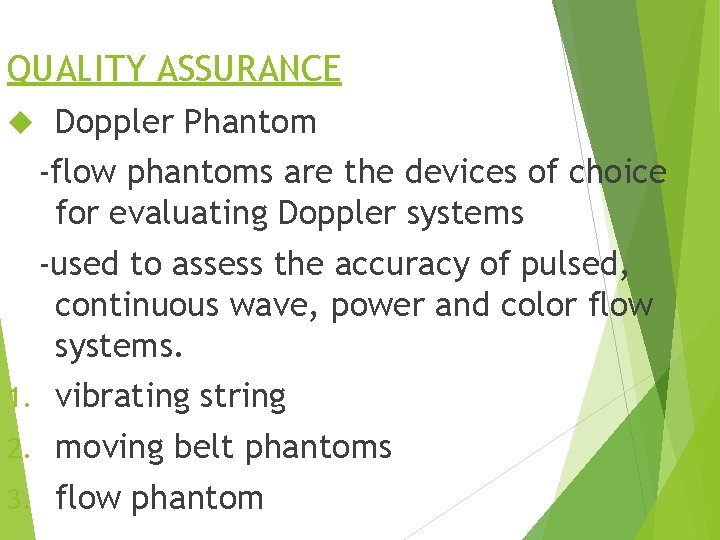
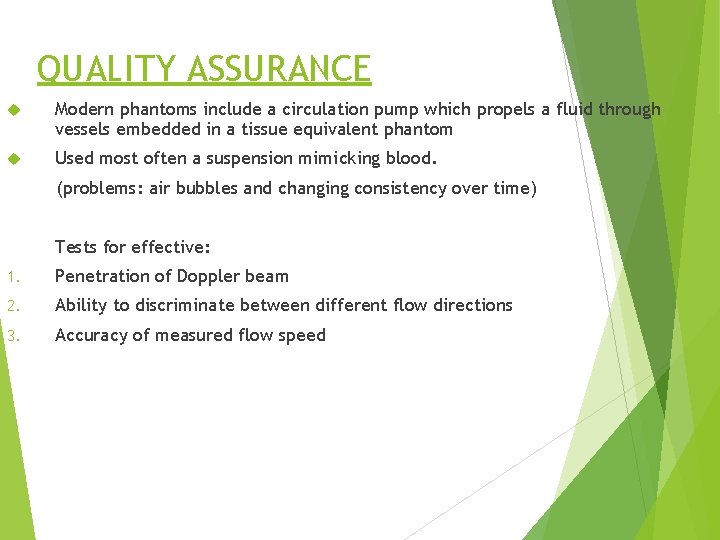
QUALITY ASSURANCE Doppler Phantom -flow phantoms are the devices of choice for evaluating Doppler systems -used to assess the accuracy of pulsed, continuous wave, power and color flow systems. 1. vibrating string 2. moving belt phantoms 3. flow phantom

Doppler Phantom
QUALITY ASSURANCE Modern phantoms include a circulation pump which propels a fluid through vessels embedded in a tissue equivalent phantom Used most often a suspension mimicking blood. (problems: air bubbles and changing consistency over time) Tests for effective: 1. Penetration of Doppler beam 2. Ability to discriminate between different flow directions 3. Accuracy of measured flow speed
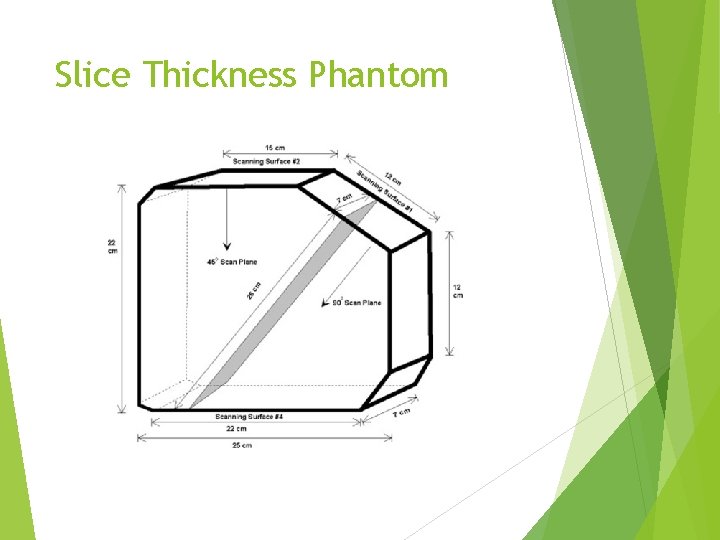
QUALITY ASSURANCE Slice Thickness Phantom -evaluation of slice thickness is also called elevational thickness -imaging plane is thicker than either the beam width or the SPL. -phantom’s medium mimics soft tissue. -thicker slices diminish spatial resolution and reduce the ability to visualize small, low contrast lesions -When the US beam is overly thick, cystic structures may appear filled in “ARTIFACTS”
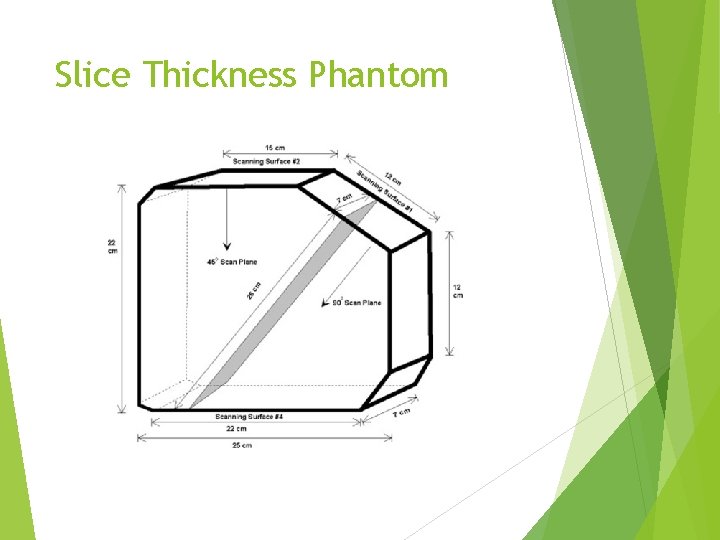
Slice Thickness Phantom
QUALITY ASSURANCE Performance Measures Sensitivity is the ability of a system to display low level echoes with a tissue equivalent phantom. 1. Minimum sensitivity (image deeper) Pick a deep pin, with the TGC set flat, increasing the gain from its minimum value to the point when an echo is displayed on the CRT determines the minimum sensitivity. The same rod in the test object should always be imaged for continuity. Assesses the detection of low level echoes in the far field
QUALITY ASSURANCE 2. Normal sensitivity Settings are those which all the pins, solid masses, and cystic structures in the test phantom are accurately displayed. Output power, TGC, and amplification are adjusted to establish normal sensitivity Found at higher gain than the minimum sensitivity All subsequent quality assurance and performance measurements are made at the normal sensitivity. (because we have to see all the structures to make measurements)
QUALITY ASSURANCE 3. Maximum sensitivity (image shallower) Evaluated with the output power and amplification of the system set to the maximum practical levels With these settings, a tissue equivalent phantom is imaged, and the depth of tissue-like texture is determined. Maximum visualization depth is used to assess sensitivity, and should not differ from one routine evaluation to the next ***Sensitivity is also assessed when the sonographer adjusts the system controls to change echo brightness from barely visible to full brightness
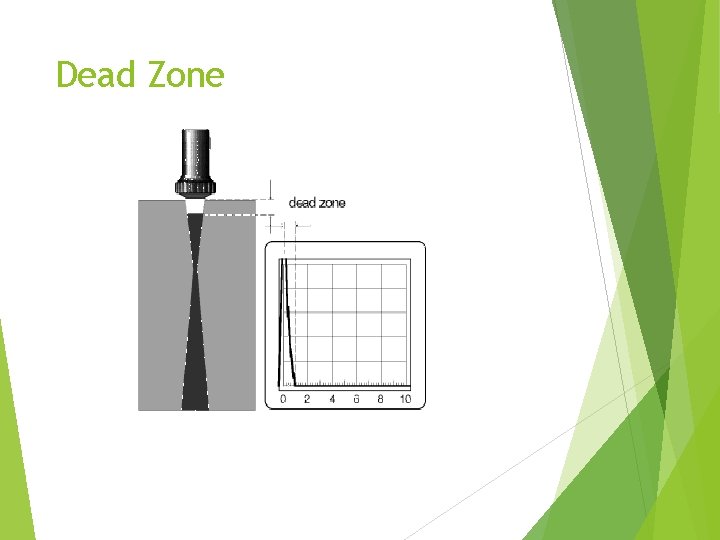
QUALITY ASSURANCE Dead Zone -results from the time that it takes for the system to switch from the transmit to the receive mode -region close to the transducer where images are inaccurate -extends from the transducer to the shallowest depth from which meaningful reflections appear -information within the dead zone is unreliable and may not be used in the diagnostic setting -the dead zone is assessed with the most shallow series of pins in a test object
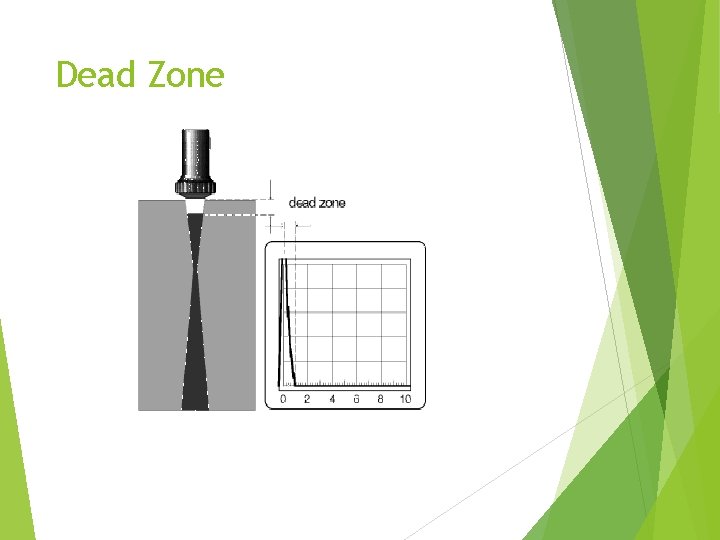
Dead Zone
QUALITY ASSURANCE Dead Zone -an acoustic standoff, or “gel pack” positioned between the transducer and the patient allows accurate imaging of important superficial structures (50 cc bag of IV fluid) -an increasingly deeper dead zone may indicate a cracked crystal, detached backing material, or a longer pulse duration
QUALITY ASSURANCE Registration Accuracy -ability of the system to place reflections in proper positions while imaging from different orientations Range Accuracy (vertical depth calibration) -system’s accuracy in placing reflectors at correct depths located parallel to the sound beam -if differences appear the error may be caused by 1. System malfunction 2. The speed of sound in the phantom is different than 1, 540 m/s
QUALITY ASSURANCE Horizontal calibration -system’s ability to place echoes in their correct position perpendicular to the sound beam Focal zone (surrounds focus) -focus of phased array transducers, must be carefully evaluated -lateral resolution is excellent in the focal zone -systems with dynamic receive focusing should produce narrow reflections over a wide range of depths
QUALITY ASSURANCE Axial Resolution -smallest distance at which two pins parallel to the sound beam are displayed as two distinct echoes. -evaluated by scanning a set of closely spaced pins within the phantom -uses pins parallel to the sound beam Lateral Resolution -minimum distance that two side-by-side rods are displayed as two distinct images -look to see if pins are perpendicular to sound beam
QUALITY ASSURANCE Compensation Operation or Uniformity -Using a tissue equivalent phantom and scanning from the top, the echoes are displayed with TIME GAIN COMPENSATION (TGC) off and then with the TGC on. -With the TGC off, the echoes should be displayed with reduced amplitude as depth increases -With the TGC on, all of the echoes should have the same amplitude, regardless of depth
QUALITY ASSURANCE Mock Cysts and Tumors -Using the tissue equivalent phantom to check dimensions of cysts -Also, note texture and fill-in Display and Grayscale Dynamic Range -Adjusting the system’s output power and amplification should produce changes in the grayscale display. -Important to compare the relationship between the image on the system’s screen with the output of all other display devices, such as remote viewing stations
BIOEFFECTS GOLD STANDARD: a perfect technique that we deem 100% accurate to which our ultrasound results are compared. Since the majority of sound energy produced by the transducer remains in the body, it is important to know output of the ultrasound system.
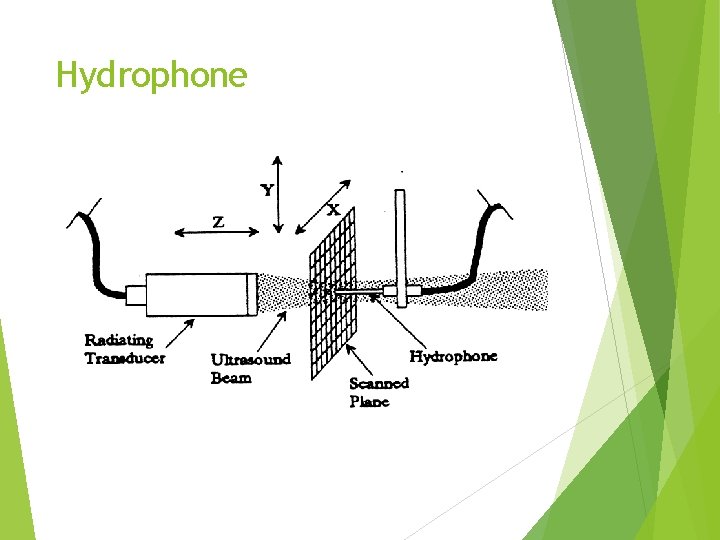
BIOEFFECTS Hydrophone -small needle with a piezoelectric crystal at its end - a wire connects the PZT crystal to an oscilloscope and the needle is placed in the ultrasound beam -displayed are acoustic signals received by the crystal -since the hydrophone is small, the acoustic pressure is measured at specific locations within the sound beam -can quantitate amplitude, period, pulse duration and pulse repetition period
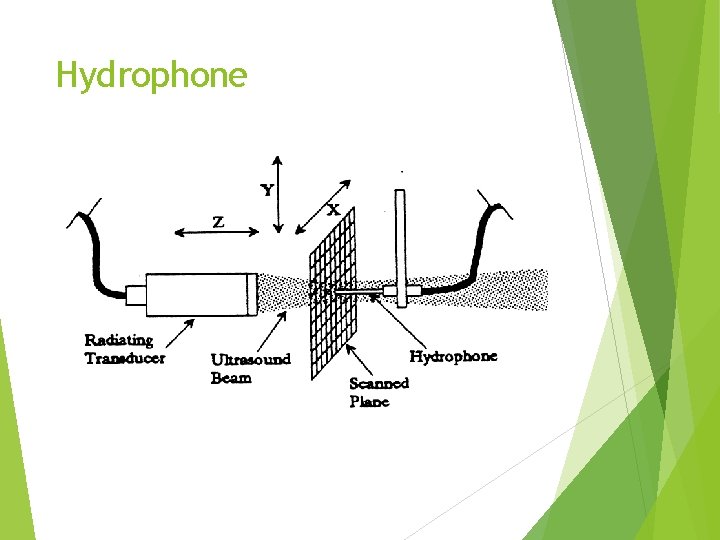
Hydrophone
BIOEFFECTS Radiation Force -transducer’s sound beam creates a very small, but measureable force on any target that it strikes. -if the target is a balance or a float, the measured force relates to the power in the beam -when the sound beam is entirely absorbed or reflected by the target, the target acts as an extremely sensitive miniature postal scale -measures SATA or SPTA intensity
BIOEFFECTS Acoustic-Optics -Based on the interaction of sound and light -A shadowing system, called Schlieren, uses this principle to allow us to view the shape of a sound beam in a medium -Quantitation of the PRP, amplitude, period, and pulse duration
BIOEFFECTS Three devices measure the output of ultrasound transducers by absorption, the conversion of sound energy into heat: 1. Calorimeter -measures the total power of the entire sound beam through the process of absorption -the sound beam is directed into the calorimeter where the sound energy is converted into heat (absorption) -the sound beam’s total power is calculated by measuring the temperature rise and the time of heating
BIOEFFECTS Thermocouple -tiny electronic thermometer -a dab of absorbing material is placed on thermocouple -the thermocouple is inserted into the sound beam and the temperature is measured by absorbing material -the temperature rise is related to the power of the sound beam at the particular location where the device is located
BIOEFFECTS Liquid Crystals -certain crystals change color based on their temperature -tank full of crystals -When a sound beam strikes a crystal, the sound energy is absorbed -The change in temperature causes a change in their color, providing insight into the shape and strength of the sound beam
BIOEFFECTS RISK-BENEFIT RELATIONSHIP 1. Benefits must outweigh the risks of the exam 2. Obstetrics and fetal medicine is a common application of diagnostic sonography. There is no confirmation of harm resulting from its use 3. Extremely high ultrasound intensities damage biologic tissue 4. Low intensity ultrasound has no known Bioeffects 5. Under controlled circumstances, Bioeffects are beneficial
BIOEFFECTS AIUM’S AND FDA’S Bioeffects intensity limit: SPTA (Spatial Peak/Temporal Average) Highest output intensities with pulsed Doppler Lowest output intensities with gray scale imaging 100 m. W/cm 2 unfocused 1, 000 m. W/cm 2 focused
BIOEFFECTS Focused beams are less likely to cause temperature elevation in tissues Unfocused beams are more likely to cause temperature elevation in tissues **this occurs because a narrow beam heats only a small region of tissue and the heat is rapidly transferred to and dissipated by adjacent tissues that were not heated by the US beam.
BIOEFFECTS Dosimetry -Science of identifying and measuring the characteristics of an ultrasound beam that are relevant to its potential for producing biological effects. Bioeffects may be conducted in two broad areas: 1. In Vivo- living 2. In Vitro- nonliving
BIOEFFECTS 1. In Vivo -performed within the living body of a plant or an animal. e. g. Studying the effects of US exposure on the lung tissue of a laboratory rat. ***Difficult to study in vivo because of attenuation*** 2. In Vitro -performed outside the living body in an artificial environment. e. g. A computer model estimating the temperature elevation of tissues during exposure to US.
BIOEFFECTS AIUM Statement on In Vitro Bioeffects 1. In vitro Bioeffects research is important 2. In vitro Bioeffects are real even though they may not apply to the clinical setting 3. In vitro Bioeffects which claim direct clinical significance should be viewed with caution (without in vivo validation)
BIOEFFECTS 1. STUDY TECHNIQUES: Mechanistic Approach - begins as a proposal that a specific mechanism has the potential to produce Bioeffects -based on that proposal, a theoretical analysis is performed to estimate the scope of the Bioeffects at various exposure levels. -searches for a cause and effect relationship
BIOEFFECTS EMPERICAL APPROACH -based on acquisition and review of information from patients or animals exposed to US -studying charts of patients who have been exposed to US -seeks a relationship between the exposure to US and the effects of that exposure -searches for a relationship between an exposure and a response ***strongest conclusions when conclusions to both approaches agree.
BIOEFFECTS 1. MECHANISMS OF BIOEFFECTS Thermal=proposes that Bioeffects result from tissue temperature elevation -as sound travels in the body, energy is converted into heat. -bone is an absorber. There fore temperature elevation at a tissue-bone interface is more likely. -temperature elevation in fetal soft tissue is considered of potentially greater harm than adults. Thus, fetal soft tissues adjacent to bone are of great concern
BIOEFFECTS Body core temperature is regulated at 37 degrees C. Life processes do not function normally at other temperatures. Any exam that causes an elevation in temperature of less than 2 degrees C may be used without reservation Any exam that causes a temperature elevation to greater than 41 degrees C is considered potentially harmful to a fetus.
BIOEFFECTS Thermal index (TI): useful predictor of max. temperature increase under most clinically relevant conditions. 3 forms: 1. TIS=assumes that sound is traveling in soft tissue 2. TIB=assumes that bone is at or near the focus of the sound beam 3. TIC=assumes that the cranial bone is in the sound beam’s near field
BIOEFFECTS 1. 2. 3. 4. Empirical findings: Serious tissue damage occurs from prolonged elevation of body temperature Tissue heating is related to the output characteristics of the transducer and the properties of the tissue A 2 degree to 4 degree in testicular temperature can cause infertility A combination of temp and exposure time determine the likelihood of harmful Bioeffects
BIOEFFECTS 5. No confirmed Bioeffects have been reported for temp elevations of up to 2 degrees above normal for exposures of less than 50 hrs. 6. Max. heating is related to the beam’s SPTA intensity 7. Fetal tissues appear less tolerant of tissue heating than adults. 8. A greater amount of acoustic energy is absorbed by bone than by soft tissue.
BIOEFFECTS Mechanistic findings: 1. Theoretical models appear to correlate with experimental data even though: -the ultrasound beam is quite complex -diagnostic equipment is diverse -tissue characteristics are different ***strong argument***
BIOEFFECTS 2. Cavitation=interaction of sound waves with microscopic, stabilized, gas bubbles in the tissues. -Also known as gaseous nuclei= NOT CONTRAST AGENTS. NATURAL GASEOUS NUCLEI THAT OCCURS NATURALLY IN THE BODY. Excitation takes on the form of shrinking and expanding of the bubble. Potential of near total energy absorption where the nuclei exist may lead to thermal injury MI relates to cavitation
BIOEFFECTS 1. Stable Cavitation -occurs at lower MI levels -the gaseous nuclei tend to oscillate or expand contract. -bubbles that are a few millimeters in diameter might double in size-bubble does not burst -the bubbles intercept and absorb much of the acoustic energy -EFFECTS: the fluids surrounding the cells undergo micro streaming and the cells are exposed to shear stresses
BIOEFFECTS 2. Transient Cavitation (inertial or normal) -at higher MI levels, transient cavitation occurs -bubble bursting -EFFECTS: produces highly localized, violent effects, including: 1. Colossal temperatures 2. Shock waves -The destructive effects of transient cavitation are not considered clinically important since they are highly localizes and affect few cells. -The pressure threshold for transient is only 10% higher than that required for stable cavitation
Conclusion The American College of Radiology (ACR) strongly recommends that the training for “appropriately trained sonographers or service engineers” conducting routine QC be provided by a qualified medical physicist. If unable to acquire training by a qualified medical physicist, training can be achieved through the ultrasound equipment manufacturer or through an appropriate course.
 Washington medical quality assurance commission
Washington medical quality assurance commission Sound travels fastest in
Sound travels fastest in Duplex vs doppler
Duplex vs doppler Main lobar fissure liver
Main lobar fissure liver Ouhsc sonography
Ouhsc sonography Quality assurance vs quality control
Quality assurance vs quality control Quality control vs quality assurance pmp
Quality control vs quality assurance pmp Pmp gold plating
Pmp gold plating Define seminar in nursing management
Define seminar in nursing management Quality improvement vs quality assurance
Quality improvement vs quality assurance Quality assurance vs quality control
Quality assurance vs quality control Medical practitioners assurance framework
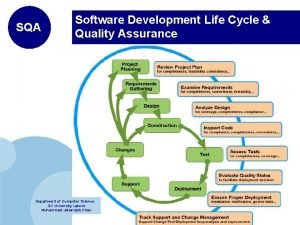
Medical practitioners assurance framework Sdlc quality assurance
Sdlc quality assurance Quality assurance theory
Quality assurance theory In process quality metrics
In process quality metrics Iso 9001 software quality assurance
Iso 9001 software quality assurance Software assurance plan
Software assurance plan Types of internal quality control
Types of internal quality control Software quality challenges
Software quality challenges Quality assurance definition
Quality assurance definition Iuqb
Iuqb Contoh kegiatan quality control di rumah sakit
Contoh kegiatan quality control di rumah sakit Pharmacovigilance quality assurance
Pharmacovigilance quality assurance Data entry quality control
Data entry quality control Lqa language quality assurance
Lqa language quality assurance Principles of quality assurance
Principles of quality assurance International network for quality assurance agencies
International network for quality assurance agencies Maiborn wolff
Maiborn wolff Gcp quality assurance
Gcp quality assurance Foqa
Foqa European quality assurance standards
European quality assurance standards Distribution of records
Distribution of records Software quality assurance notes
Software quality assurance notes Continuous airworthiness maintenance program (camp)
Continuous airworthiness maintenance program (camp) Difference between bpr and tqm
Difference between bpr and tqm Pillars of quality assurance
Pillars of quality assurance Sqa tools and techniques
Sqa tools and techniques Software quality assurance models
Software quality assurance models Statistical quality assurance in software engineering
Statistical quality assurance in software engineering Quality assurance coaching techniques
Quality assurance coaching techniques Youtube.com
Youtube.com Pcb quality assurance
Pcb quality assurance Quality assurance instruments
Quality assurance instruments Qat quality assurance testing
Qat quality assurance testing Emmett mitchell engineering
Emmett mitchell engineering Epa requirements for quality assurance project plans
Epa requirements for quality assurance project plans Farm quality assurance
Farm quality assurance Infrastructure quality assurance
Infrastructure quality assurance Formal technical
Formal technical Quality assurance card
Quality assurance card Hospice quality assurance
Hospice quality assurance Nche quality assurance framework
Nche quality assurance framework Call may be monitored for quality assurance
Call may be monitored for quality assurance Statistical software quality assurance
Statistical software quality assurance