Pulmonary eosinophilia Definition Pulmonary eosinophilia is a group

- Slides: 22
Pulmonary eosinophilia
Definition Pulmonary eosinophilia is a group of diseases with eosinophil cells–mediated pulmonary tissue damage and characterized by the association of radiographic (usually pneumonic) abnormalities and peripheral blood eosinophilia.
Classification A/ Extrinsic (cause known) 1. Helminths: e. g. Ascaris, Toxocara, Filaria 2. Drugs: nitrofurantoin, sulfasalazine, imipramine, chlorpropamide. 3. Fungi: e. g. Aspergillus fumigatus causing allergic bronchopulmonary aspergillosis.
B/ Intrinsic (cause unknown) 1. Cryptogenic eosinophilic pneumonia 2. Eosinophilic granulomatosis with polyangiitis (formerly Churg–Strauss syndrome) 3. Hypereosinophilic syndrome 4. Polyarteritis nodosa
Acute eosinophilic pneumonia: a febrile illness of less than 5 days duration with diffuse alveolar damage causing pulmonary infiltrates & hypoxic respiratory failure. Diagnosis is confirmed by bronchoalveolar lavage with > 25% of infiltrate is eosinophil and the treatment is mainly with corticosteroids.
Chronic eosinophilic pneumonia: a insidious onset of fever, malaise, SOB & dry cough, more common in middleaged females. • Radiologically characterized by bilateral & peripheral pulmonary shadowing (photographic negative of pulmonary oedema) with peripheral eosinophilia & high ESR & Ig. E. • Treatment is with steroids.
Tropical pulmonary eosinophilia: secondary to a mosquito borne filarial infection with Wuchereria bancrofti or Brugia malayi. • Treatment is with diethylcarbamazine (6 mg/kg/day for 3 weeks).
Pulmonary vasculitis Granulomatosis with polyangiitis (Wegener’s granulomatosis): • an idiopathic disease manifested by a combination of glomerulonephritis, necrotizing granulomatous vasculitis of the upper and lower respiratory tracts, and varying degrees of small-vessel vasculitis. Symptoms: cough, haemoptysis, chest pain, nasal discharge, crusting, otitis media, fever, weight loss & anaemia. CXR: multiple nodules & cavitation ( mimicking pulmonary tumours or abscess in the lung). Lung biopsy: necrotising granulomas and necrotising vasculitis. Complications: tracheal subglottic stenosis and saddle nose deformity.
Eosinophilic granulomatosis with polyangiitis (formerly Churg-Strauss syndrome) • an idiopathic multisystem vasculitis of small and medium-sized arteries that occurs in patients with asthma. It can be part of a spectrum that includes polyarteritis nodosa. • The skin and lungs are most often involved, but other organs, including the paranasal sinuses, the heart, gastrointestinal tract, liver, and peripheral nerves, may also be affected. • Peripheral eosinophilia greater than 1. 5 × 109/L or greater than 10% of peripheral WBCs is the rule. • CXR-transient opacities, multiple nodules. • The diagnosis requires demonstration of histologic features, including fibrinoid necrotizing epithelioid and eosinophilic granulomas.

• Treatment of pulmonary vasculitis is glucocorticoids & chemotherapy.
Goodpasture’s disease: • A syndrome of pulmonary haemorrhage & glomerulonephritis with Ig. G antibodies attached to glomerular or alveolar basement membrane. The incidence is higher in smoker males. • Pulmonary manifestations are proceeding renal involvement with hypoxia and/or haemoptysis associated with pulmonary infiltrates on CXR.
Connective tissue diseases & pulmonary involvement Rheumatoid diseases: • Lung involvement appears within 5 years of rheumatoid disease onset but it can be earlier manifestation in 10 -20% of patients. • Pulmonary manifestations are pulmonary fibrosis, non-specific interstitial pneumonia, rheumatoid nodules ( multiple, subpleural), Caplan’s syndrome ( rheumatoid nodules & pneumoconiosis), bronchitis & bronchiectasis, crico-arytenoid arthritis, stridor, pleural effusion, pneumothorax. • Treatment-related side effects (methotrexate-pulmonary fibrosis, anti-TNFreactivation of TB).
Systemic lupus erythematosus: • Pleuro-pulmonary involvement is very common & can be a presenting feature of SLE. • Pleural manifestations- very common (up to two thirds of patients) with repeated episodes of pleurisy &/or effusion with possible pericardial involvement. • Acute alveolitis-life threatening diffuse alveolar haemorrhage requires rapid supportive treatment, immunosuppression & glucocorticoids. • Others- pulmonary fibrosis, shrinking lung (SOB with elevated diaphragm due to diaphragmatic myopathy) & pulmonary thromboembolic disease (SLE & Antiphospholipid syndrome).
Systemic sclerosis: • Pulmonary fibrosis- 90% of patients mainly the diffuse form. • Pulmonary hypertension- more common with limited SS (CREST syndrome). • Recurrent aspiration pneumonia- secondary to oesophageal disease. • Hidebound chest- restricted chest wall movement due to extensive skin Involvement.
Occupational lung diseases
Pneumoconiosis Coal worker’s pneumoconiosis: Cause: prolonged inhalation of coal dust causing pulmonary fibrosis through aggregation of alveolar macrophages.
• Classification: • A/ Simple CWP: asymptomatic. • CXR with small radiographic nodules & lung function test is unaffected. • Ceasing exposure prevents progression. • B/ Progressive massive fibrosis: symptomatic ( productive cough (melanoptysis) & SOB) & may end with respiratory failure. • CXR shows masses & cavitation (DDx: TB, lung cancer & polyangiitis & granulomatosis). • Disease is progressive even with ceasing exposure.
Lung diseases due to organic dusts: Hypersensitivity pneumonitis (extrinsic allergic alveolitis) Causes: inhalation of organic dust leading to type III or IV diffuse immune complex reaction with in the alveolar & bronchial walls. Clinical features: more in farmers (farmer’s lung) or pigeon fanciers (bird fancier’s lung) with symptoms related to the extent of exposure to the triggering organic dusts. • Symptoms either acute as influenza-like syndrome or chronic with progressive pulmonary fibrosis.
Investigations: CXR- ill-defined patchy shadowing. HRCT- ground-glass shadowing & consolidations mainly in upper & middle lobes. In chronic cases, CT shows lung volume loss, linear opacities & structural damage. Pulmonary function test- restrictive defect, reduced lung volume & gas transfer. Type I respiratory failure in advanced cases. Serology- searching for positive precipitin antigen.
Clinical predictors: • • • Exposure to a known offending antigen Positive precipitating antibodies to offending antigen Recurrent episodes of symptoms Inspiratory crackles on examination Symptoms occurring 4– 8 hours after exposure Weight loss
Management: 1. 2. 3. 4. Avoid exposure to possible triggers. Wearing masks. Glucocorticoids. O 2 therapy. Complications: Pulmonary fibrosis, respiratory failure, pulmonary hypertension & right side heart failure.
Thank you
 Eosinophilia treatment
Eosinophilia treatment Rvsp calculation
Rvsp calculation Pulmonary hypertension definition
Pulmonary hypertension definition Copd exacerbation nursing management
Copd exacerbation nursing management Two factor theory psychology
Two factor theory psychology Y = a(b)^x
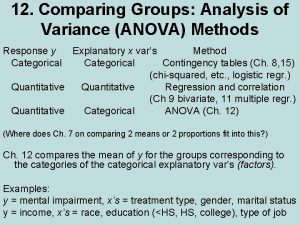
Y = a(b)^x Anova within group and between group
Anova within group and between group Types of social groups in sociology
Types of social groups in sociology Group 1 vs group 2 specialties
Group 1 vs group 2 specialties Group 2 nitrates thermal stability
Group 2 nitrates thermal stability Amino group and carboxyl group
Amino group and carboxyl group Amino group and carboxyl group
Amino group and carboxyl group In group out group
In group out group Group yourselves
Group yourselves Sumner's classification of social groups
Sumner's classification of social groups Joining together group theory and group skills
Joining together group theory and group skills Total anomalous venous return
Total anomalous venous return Content of thoracic cavity
Content of thoracic cavity Arteries
Arteries Neurogenic shock
Neurogenic shock Crista terminalis
Crista terminalis Priyanka breathing
Priyanka breathing Pulmonary surfactant function
Pulmonary surfactant function