Eosinophilia in Tropics Eosinophils They are granulocytic leucocytes

- Slides: 8
Eosinophilia in Tropics
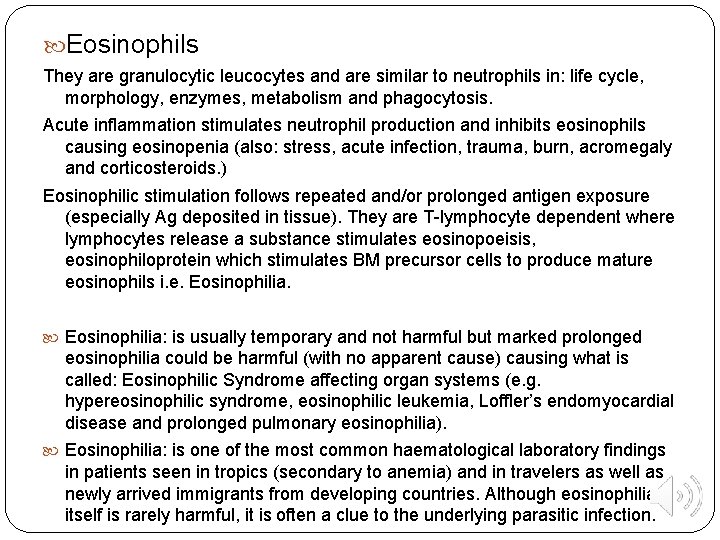
Eosinophils They are granulocytic leucocytes and are similar to neutrophils in: life cycle, morphology, enzymes, metabolism and phagocytosis. Acute inflammation stimulates neutrophil production and inhibits eosinophils causing eosinopenia (also: stress, acute infection, trauma, burn, acromegaly and corticosteroids. ) Eosinophilic stimulation follows repeated and/or prolonged antigen exposure (especially Ag deposited in tissue). They are T-lymphocyte dependent where lymphocytes release a substance stimulates eosinopoeisis, eosinophiloprotein which stimulates BM precursor cells to produce mature eosinophils i. e. Eosinophilia: is usually temporary and not harmful but marked prolonged eosinophilia could be harmful (with no apparent cause) causing what is called: Eosinophilic Syndrome affecting organ systems (e. g. hypereosinophilic syndrome, eosinophilic leukemia, Loffler’s endomyocardial disease and prolonged pulmonary eosinophilia). Eosinophilia: is one of the most common haematological laboratory findings in patients seen in tropics (secondary to anemia) and in travelers as well as newly arrived immigrants from developing countries. Although eosinophilia itself is rarely harmful, it is often a clue to the underlying parasitic infection.
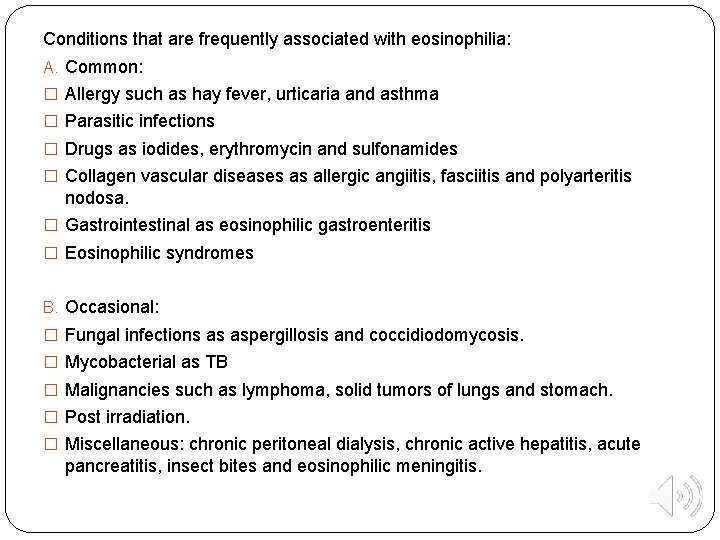
Conditions that are frequently associated with eosinophilia: A. Common: � Allergy such as hay fever, urticaria and asthma � Parasitic infections � Drugs as iodides, erythromycin and sulfonamides � Collagen vascular diseases as allergic angiitis, fasciitis and polyarteritis nodosa. � Gastrointestinal as eosinophilic gastroenteritis � Eosinophilic syndromes B. Occasional: � Fungal infections as aspergillosis and coccidiodomycosis. � Mycobacterial as TB � Malignancies such as lymphoma, solid tumors of lungs and stomach. � Post irradiation. � Miscellaneous: chronic peritoneal dialysis, chronic active hepatitis, acute pancreatitis, insect bites and eosinophilic meningitis.
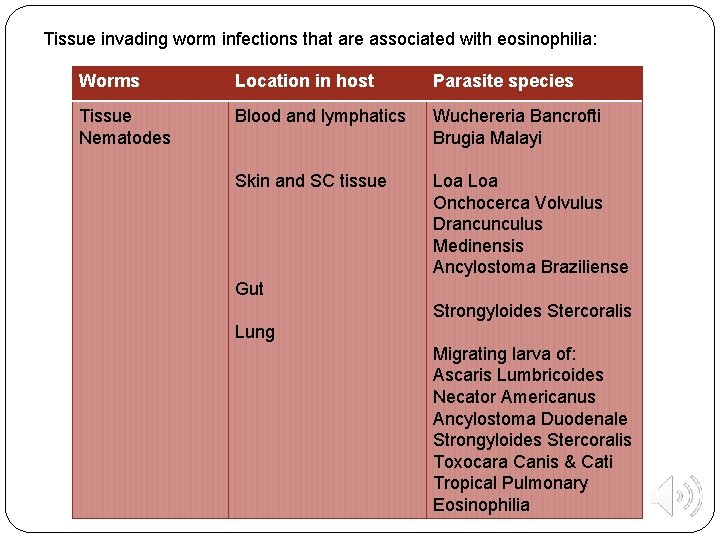
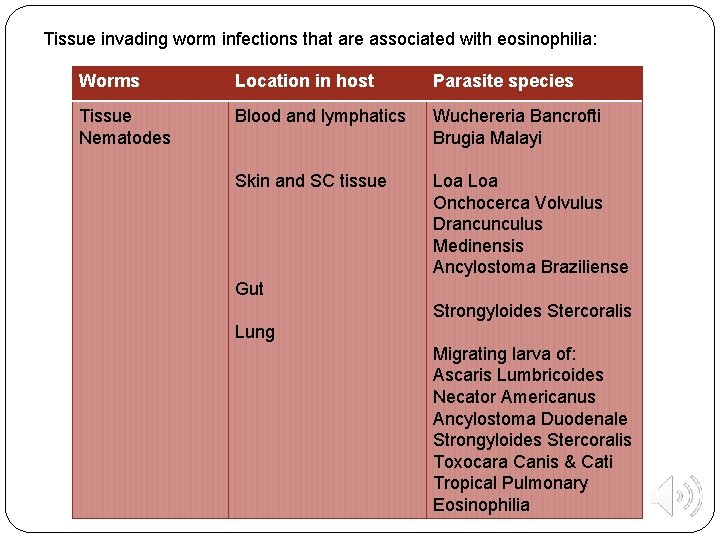
Tissue invading worm infections that are associated with eosinophilia: Worms Location in host Parasite species Tissue Nematodes Blood and lymphatics Wuchereria Bancrofti Brugia Malayi Skin and SC tissue Loa Onchocerca Volvulus Drancunculus Medinensis Ancylostoma Braziliense Gut Strongyloides Stercoralis Lung Migrating larva of: Ascaris Lumbricoides Necator Americanus Ancylostoma Duodenale Strongyloides Stercoralis Toxocara Canis & Cati Tropical Pulmonary Eosinophilia
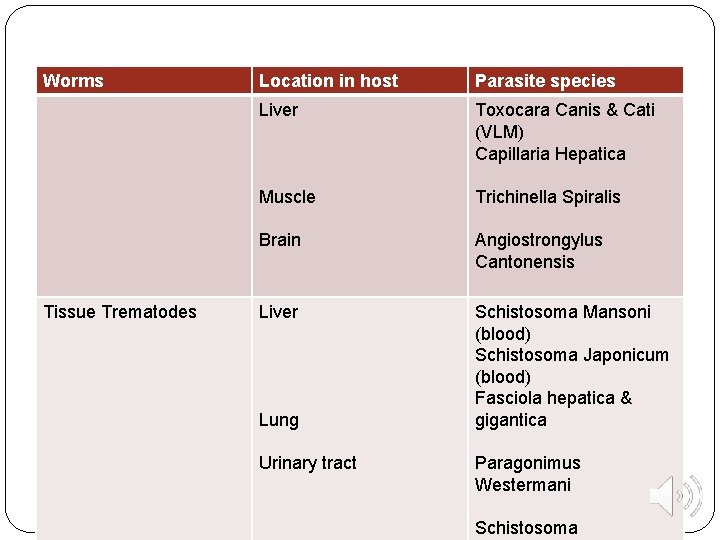
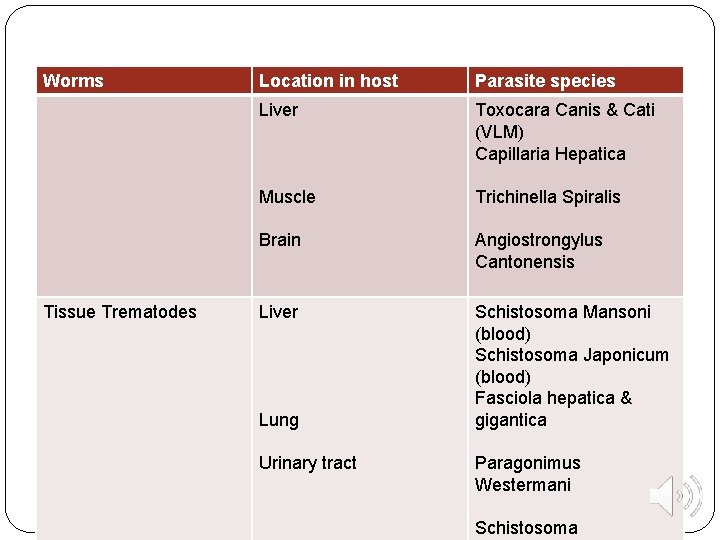
Worms Tissue Trematodes Location in host Parasite species Liver Toxocara Canis & Cati (VLM) Capillaria Hepatica Muscle Trichinella Spiralis Brain Angiostrongylus Cantonensis Liver Schistosoma Mansoni (blood) Schistosoma Japonicum (blood) Fasciola hepatica & gigantica Lung Urinary tract Paragonimus Westermani Schistosoma
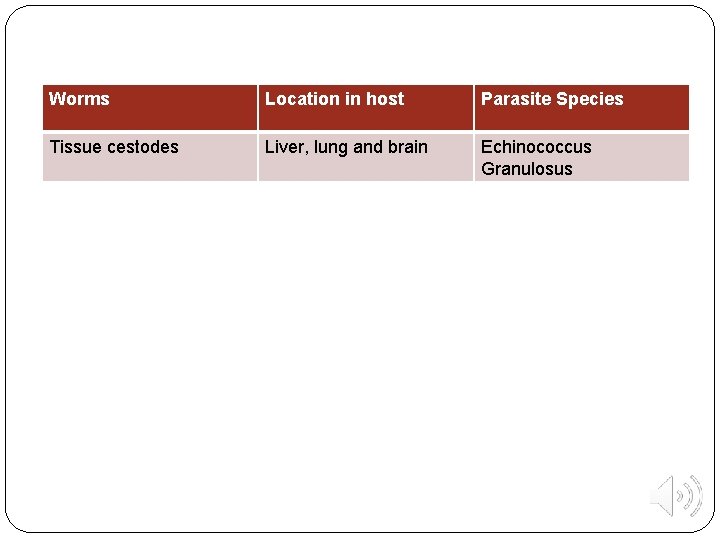
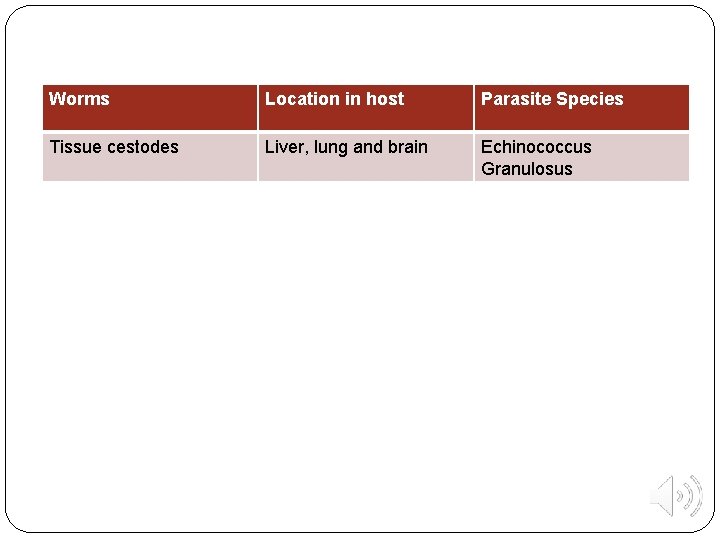
Worms Location in host Parasite Species Tissue cestodes Liver, lung and brain Echinococcus Granulosus

Diagnostic approach to a case of eosinophilia: 1. Is there absolute eosinophilia (>400 -500 cells/mm³) and/or a relative one (Low < 1000, moderate 1000 -3000, high > 3000 cells/mm³) ? 2. Is eosinophilia related to the presenting S&S? (e. g. in travelers). 3. Is eosinophilia possibly related to parasite infections? 4. What are the most appropriate diagnostic steps for the possible cause (especially allergy and parasites)? - History: Allergy, drugs, diet, endemic areas, travel, exposure to infection. - Physical examination: liver, spleen, L. N. , skin affection, etc - Investigations: A- Step 1: baseline CBC, differential leucocyte count, stool & urine analysis. B- Step 2: if history and physical examination suggest specific parasitic infection, do culture for this possible parasite, serology (e. g. strongyloid), day and night blood examination (filariasis). C- Step 3: skin snips (onchocerciasis), liver biopsy (schistosomiasis, fascioliasis) chest x-ray (paragonimiasis) and rectal snip (schistosomiasis). 5. If no diagnosis: further investigations are repeated 3 -6 months later.
THANK YOU