Psychosomatic medicine History and Current Trends The term

- Slides: 25
Psychosomatic medicine History and Current Trends
The term psychosomatic is derived from the Greek words psyche (soul) and soma (body). The term literally refers to how the mind affects the body.
Major Conceptual Trends in the History of Psychosomatic Medicine
Psychoanalytic
Sigmund Freud (1900): Somatic involvement occurs in conversion hysteria, which is psychogenic in origin—e. g. , paralysis of an extremity. Conversion hysteria always has a primary psychic cause and meaning; i. e. , it represents the symbolic substitutive expression of an unconscious conflict. It involves organs innervated only by the voluntary neuromuscular or the sensorimotor nervous system. Psychic energy that is dammed up is discharged through physiological outlets.
Sandor Ferenczi (1910): The concept of conversion hysteria is applied to organs innervated by the autonomic nervous system; e. g. , the bleeding of ulcerative colitis may be described as representing a specific psychic fantasy.
George Groddeck (1910): Clearly organic diseases, such as fever and hemorrhage, are held to have primary psychic meanings; i. e. , they are interpreted as conversion symptoms that represent the expression of unconscious fantasies

Psychophysiological
Walter Cannon (1927): Demonstrated the physiological concomitants of some emotions and the important role of the autonomic nervous system in producing those reactions. The concept is based on Pavlovian behavioral experimental designs.
Hans Selye (1945): Under stress a general adaptation syndrome develops. Adrenal cortical hormones are responsible for the physiological reaction.
Sociocultural
Karen Horney (1939), James Halliday (1948): Emphasized the influence of the culture in the development of psychosomatic illness. They thought that culture influences the mother, who, in turn, affects the child in her relationship with the child— e. g. , nursing, child rearing, anxiety transmission.
Systems theory
Adolph Meyer (1958): Formulated the psychobiological approach to patient assessment that emphasizes the integrated assessment of developmental, psychological, social, environmental, and biological aspects of the patient's condition. Basic concept of the biopsychosocial model is implicit in his approach.
Current Trends The practice of psychosomatic medicine has evolved considerably since its early clinical origins and has come to focus on psychiatric illnesses that occur in the setting of physical health care
In large part this evolution has occurred as a result of the increased complexity of medicine, the increased understanding of the relationship of medical illness to psychiatric illness, and the greater appreciation of mind and body as one. A key outcome of this has been the granting of subspecialty status for psychosomatic medicine.
Importance
The extent of the burden caused by co-occurring mental and physical disorders represents a tremendous public health problem.
Psychiatric morbidity is very common in patients with medical conditions, with a prevalence ranging from 20 to 67 percent, depending on the illness.
Psychiatric morbidity has serious effects on medically ill patients and is often a risk factor for their medical conditions.
In addition, depression and other mental disorders significantly impact quality of life and the ability of patients to adhere to treatment regimens (e. g. , in patients with diabetes mellitus).
Failure to identify, evaluate, diagnose, treat, or achieve symptom resolution of psychiatric morbidity in medical care settings results in significantly increased service utilization.
The Clinical Practice of Psychosomatic Medicine The primary objective for psychosomatic medicine is the diagnosis and treatment of psychiatric disorders in patients with complex medical conditions.
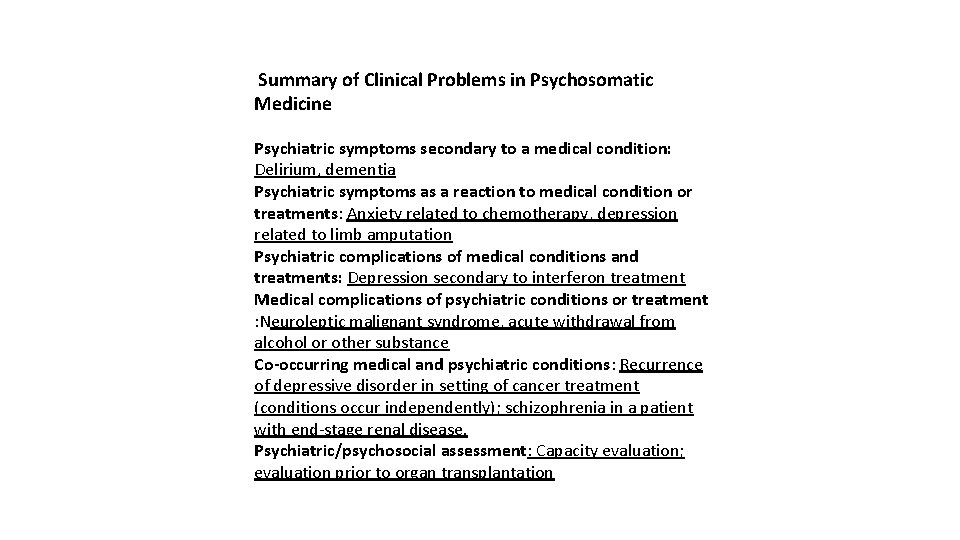
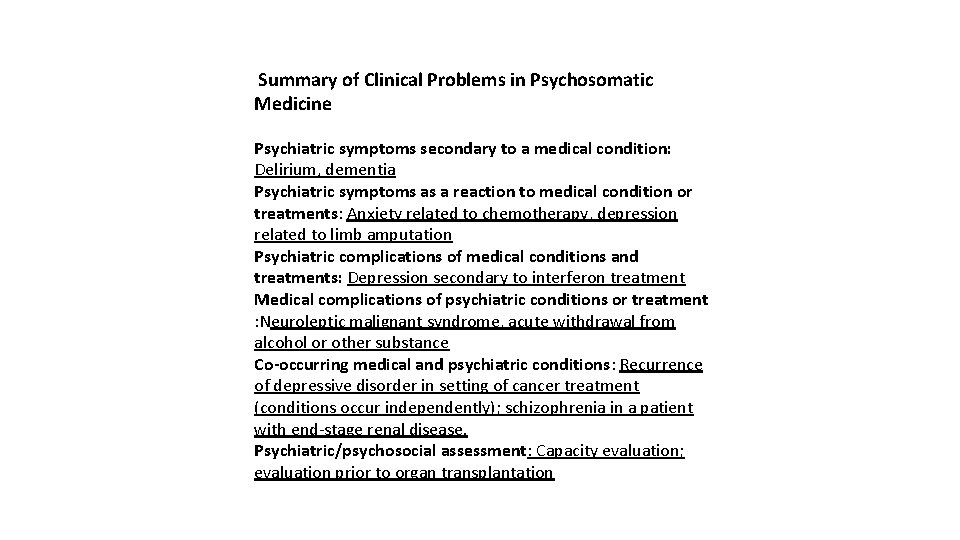
Summary of Clinical Problems in Psychosomatic Medicine Psychiatric symptoms secondary to a medical condition: Delirium, dementia Psychiatric symptoms as a reaction to medical condition or treatments: Anxiety related to chemotherapy, depression related to limb amputation Psychiatric complications of medical conditions and treatments: Depression secondary to interferon treatment Medical complications of psychiatric conditions or treatment : Neuroleptic malignant syndrome, acute withdrawal from alcohol or other substance Co-occurring medical and psychiatric conditions: Recurrence of depressive disorder in setting of cancer treatment (conditions occur independently); schizophrenia in a patient with end-stage renal disease. Psychiatric/psychosocial assessment: Capacity evaluation; evaluation prior to organ transplantation
consultation-liaison psychiatrist
 Psychosomatic
Psychosomatic Discuss the current technologies of media and information
Discuss the current technologies of media and information Trends in molecular medicine
Trends in molecular medicine Trends in project portfolio management
Trends in project portfolio management Emerging trends in strategic management
Emerging trends in strategic management Lystya
Lystya Current trends in music
Current trends in music Current trends in athletic training
Current trends in athletic training Current trends in medical education
Current trends in medical education Current trends in counseling
Current trends in counseling A balanced delta connected load having an impedance 20-j15
A balanced delta connected load having an impedance 20-j15 Difference between phase voltage and line voltage
Difference between phase voltage and line voltage Energy band diagram of pn junction diode
Energy band diagram of pn junction diode Lesson 4 three-phase motors
Lesson 4 three-phase motors Drift current
Drift current Drift current and diffusion current in semiconductor
Drift current and diffusion current in semiconductor Balanced wye wye connection
Balanced wye wye connection Slideplayer
Slideplayer Diffusion current formula
Diffusion current formula Chapter 1 history and trends of health care
Chapter 1 history and trends of health care Chapter 1 history and trends of health care
Chapter 1 history and trends of health care In this figure
In this figure Why is sma welding current referred to as constant current?
Why is sma welding current referred to as constant current? Touch current vs leakage current
Touch current vs leakage current Mesh current method with current source
Mesh current method with current source Five historical periods of pharmacy
Five historical periods of pharmacy