Psychosis in the Older Patient Module 3 Thomas

- Slides: 28
Psychosis in the Older Patient Module 3 Thomas Magnuson, M. D. Assistant Professor Division of Geriatric Psychiatry Department of Psychiatry UNMC Updated 1/25/06
PROCESS A series of modules and questions Step #1: Power point module with voice overlay Step #2: Case-based question and answer Step # 3: Proceed to additional modules or take a break
Overall Objectives Upon completion the learner will be able to: Describe common treatment modalities for psychosis in geriatric patients
Tom; here could we review case you gave in the beginning and “weave” it into treatment?
Treatment If there is a medical cause, treat the cause as well as the symptoms Delirium General medical condition Substance-induced • Intoxication • Withdrawal • Adverse event
Treatment Primary method of treating psychosis is with antipsychotics Treat other psychiatric symptoms appropriately, i. e. depression with an antidepressant Non-pharmacologic interventions In dementia • Psychosocial interventions In schizophrenia • Groups to help with daily life In depression • Psychotherapy
Treatment Antipsychotics Typical versus Atypical agents Adverse effect profile • • • Extra. Pyramidal symptoms (EPS) Anticholinergic Diabetes Hyperlipidemia Cardiac conduction Increased risk of death
Treatment Older typical agents More pure dopamine blockers Divided into high and low potency agents • Both have adverse events associated with their use High potency agents • Haldol (haloperidol), Prolixin (fluphenazine) • More EPS than anticholinergic side effects Low potency agents • Thorazine (chlorpromazine), Mellaril (thioridazine) • More anticholinergic events than EPS
Treatment Newer atypical agents More serotonergic properties • Less EPS • Important for the elderly as they are more prone to drug-induced parkinsonism (DIP) or tardive dyskinesia (TD) • Can lead to falls (fractured hip, subdural hematomas), choking (aspiration pneumonia) More likely used today across all ages
Treatment Concerns with newer agents in the elderly Diabetes Hyperlipidemia Cardiac conduction Association with death in demented patients • Study outcome issues • CVA-related s selection • Pneumonia-related s Monitoring s EPS and sedation

Treatment Atypicals Clozaril (clozapine) • Multiple side effects Risperdal (risperidone) • Dose dependent EPS Zyprexa (olanzepine) • Diabetes, hyperlipidemia Geodon (ziprasidone) • QTc prolongation Seroquel (quetiapine) • Reduces EPS Abilify (aripiprazole) • Little sedation or weight gain
Treatment Atypicals These medications can be used effectively in the elderly, even in demented patients In many cases there are no alternatives for psychosis in this group • Older typical agents can lead to severe morbidity due to adverse events The key is proper selection of patients and continued monitoring of their condition
Treatment Nonpharmacologic Dementia with psychosis • • • Environmental changes Redirection Prevent over or under stimulation Emphasize caregiver, family participation Maintain predictable routines Diffuse restlessness with tasks Feed hunger Exercise Music
Treatment Nonpharmacolgic Dementia with psychosis • • • Evaluate and treat pain Simplify the environment Preform ADL’s and IADL’s as needed Reassess for loneliness, fears, wishes, needs Reevaluate sensory functioning s Eye exams s Audiology exams s Check hearing aid batteries, ear canals
Treatment Nonpharmacologic Schizophrenia • Cognitive behavioral skills training s Helps mediate the effect of psychosis leading to untrue cognitions about life and the environment • Classes on medications, diagnosis s Answer questions, understand their illness and treatment • Functional adaptation group s Problem-solving taught to help patients live in the world s Maintain an apartment, job, relationship
Treatment Depression with psychosis Antidepressants important • Must treat both sets of symptoms May benefit from psychotherapy • Especially supportive therapy Consider ECT • Very effective in the treatment of psychotic depression • Rapid turn around
Objectives Define psychosis Delineate common etiologies for psychosis in the elderly Describe treatment modalities for psychosis in the geriatric patient
The End of the Modules on Psychosis in the Older Patient
Post-test questioned one A 62 -year-old man has schizoaffective disorder that has been stable for 20 years. His early course was characterized by multiple hospitalizations for manic episodes and treatment with electroconvulsive therapy in his 20 s and 30 s. Current medications are lithium carbonate, 1200 mg daily; risperidone, 2 mg three times daily; and benztropine, 0. 5 mg twice daily. This regimen has been stable for several years, and he has taken the same dose of lithium for approximately 20 years. Physical examination reveals grimacing, chewing movements, and eyebrow raising. A fine intention tremor also is noted in both hands. Which of the following is the most likely diagnoses of the abnormal movements? Used with permission from: Murphy JB, et. al. Case Based Geriatrics Review: 500 Questions and Critiques from the Geriatric Review Syllabus. AGS 2002 New York, NY.
Which of the following is the most likely diagnoses of the abnormal movements? A. Tardive dyskinesia involving the orofacial muscles and lithium-induced tremor of the hands B. Tardive dyskinesia involving the hands and acute dystonic movements of the face C. Tardive dyskinesia involving the hands and psychogenic movements of the face D. Progressive supranuclear palsy affecting both the face and hands E. Parkinsonian effects secondary to antipsychotic medication but partially treated with benztropine
Answer: A. Tardive dyskinesia involving the orofacial muscles and lithium-induced tremor of the hands This patient displays classic symptoms of tardive dyskinesia involving the orofacial muscles. These may include facial twitches, grimacing, puffing of the cheeks, chewing, eye blinking, and eyebrow raising. Orofacial involvement is the most common presentation of tardive dyskinesia in older patients taking antipsychotic medications. Abnormal movements of the trunk and extremities also may occur. A fine intention tremor is consistent with lithium use.
Acute dystonic reactions typically develops during initial exposure to or after an increase in antipsychotic medication, usually in a younger person. Dystonic reactions are characterized by acute muscle rigidity, which may involve contortion of the facial or neck muscles, or oculogyric crisis (ie, deviation and upward fixation of the eyes). These symptoms reflect an acute reaction to the medication and do not occur with chronic use at stable doses. Progressive supranuclear palsy (PSP) involves degeneration of the basal ganglia and brainstem. It is considered a Parkinson’s plus syndrome and frequently is diagnosed as Parkinson’s disease initially. PSP is characterized by progressive gait instability, dysphagia, and dysarthria; parkinsonian effects such as muscle rigidity, pill-rolling tremor at rest, shuffling gait, mask-like facies, and excessive salivation are not present. Although these may occur with risperidone, they are more likely to occur with a traditional antipsychotic agent, such as haloperidol or fluphenazine. “Psychogenic” movements—those that are a direct manifestation of a psychiatric syndrome—may be associated with conditions such as hysterical paralysis or other “conversion” reactions in which a source of psychologic stress manifests as bizarre motor symptoms. These usually involve paralysis, paresthesia, or other loss of function. Go to next question
Posttest question 2 A 60 -year-old woman was diagnosed with late-onset schizophrenia at the age of 55 years. Initially she experienced the paranoid delusional belief that her home was being monitored by a government agency. These symptoms responded to mesoridazine for a number of years, but because of her increasing gait instability and concerns about falling, her physician changed her medication to haloperidol 2 weeks ago. Since starting the haloperidol she has felt more agitated, pacing around her home and looking out the windows. She states that she feels restless and uncomfortable. What is the most likely source of this woman’s current problem?
What is the most likely source of this woman’s current problem? A. The extrapyramidal side effect of akathisia B. A relapse of the psychosis with increased paranoia C. An episode of mania secondary to switching medications D. Tardive dyskinesia with prominent limb and truncal involvement E. The anticholinergic side effect of confusion
Answer: A. The extrapyramidal side effect of akathisia The side effect experienced by the patient is that of akathisia, that is, restlessness accompanied by pacing and an uncomfortable sensation of needing to move about. This side effect typically is apparent shortly after starting a high-potency antipsychotic medication such as haloperidol. The presence of akathisia is particularly important to recognize, as often in the face of increasing distress the clinician may choose to increase the dose of antipsychotic medication. This decision likely compounds the problem by increasing the severity of the akathisia and other adverse effects. Whereas akathisia is likely to occur typically within the first 4 weeks after starting or increasing an antipsychotic medication, a relapse of psychosis may take several more weeks to occur and tends to be more insidious. Although this woman has motor restlessness, there is little else to suggest mania.
Although tardive dyskinesia is an important consideration in the older population, it typically does not have an acute presentation and is not associated with subjective distress or agitation. Rather, tardive dyskinesia represents a gradual onset of abnormal movements (often unnoticed by the patient), typically in the orofacial region, such as grimacing, eye blinking, puffing the cheeks, or chewing movements. Anticholinergic side effects are also difficult for the older patient; however, they would occur more commonly with the thioridazine derivative than with haloperidol. These side effects include urinary retention, blurred vision, dry mouth, constipation, and cognitive impairment.
In terms of treatment, akathisia may resolve with a decrease in haloperidol dosage or the addition of a ß-antagonist, benzodiazepine, or anticholinergic agent. Interestingly, akathisia has also rarely been associated with the use of selective serotonin-reuptake inhibitors. end
 Life is older than the trees
Life is older than the trees Syncope in the older patient is
Syncope in the older patient is Module 11 studying the brain
Module 11 studying the brain Patient 2 patient
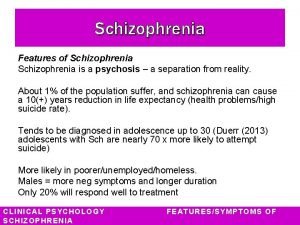
Patient 2 patient Psychosis
Psychosis What is forensic psychiatry
What is forensic psychiatry Infantile autism
Infantile autism First episode psychosis
First episode psychosis Mild psychosis
Mild psychosis How do you get schizophrenia
How do you get schizophrenia Neurosis vs psychosis
Neurosis vs psychosis Jansen orfan
Jansen orfan The dena schlosser case
The dena schlosser case First episode psychosis
First episode psychosis Autoscopic psychosis
Autoscopic psychosis Neurosis vs psychosis
Neurosis vs psychosis Neurosis vs psychosis
Neurosis vs psychosis Peycosis
Peycosis Psychosis and ptsd
Psychosis and ptsd What is postictal confusion
What is postictal confusion Types of psychosis and neurosis
Types of psychosis and neurosis Functional psychosis
Functional psychosis Dopamine hypothesis psychosis
Dopamine hypothesis psychosis Psychosis and neurosis
Psychosis and neurosis Types of psychosis
Types of psychosis Forensic pathologist vs forensic anthropologist
Forensic pathologist vs forensic anthropologist C device module module 1
C device module module 1 Growing older poem
Growing older poem Covids older adults
Covids older adults