Primary Care FirstSerious Illness Population Annie Acs NHPCO

- Slides: 24
Primary Care First/Serious Illness Population Annie Acs, NHPCO Director Health Policy & Innovation Lori Bishop, NHPCO Vice President Palliative & Advanced Care Khue Nguyen, Emprise Health Jeremy Powell, Acclivity Health November 15, 2019 1 Leading Person-Centered Care
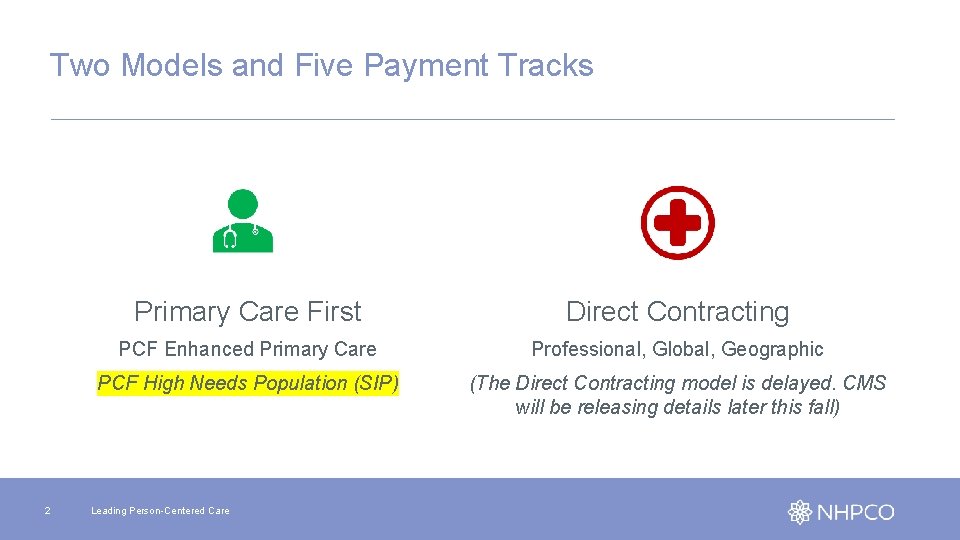
Two Models and Five Payment Tracks 2 Primary Care First Direct Contracting PCF Enhanced Primary Care Professional, Global, Geographic PCF High Needs Population (SIP) (The Direct Contracting model is delayed. CMS will be releasing details later this fall) Leading Person-Centered Care
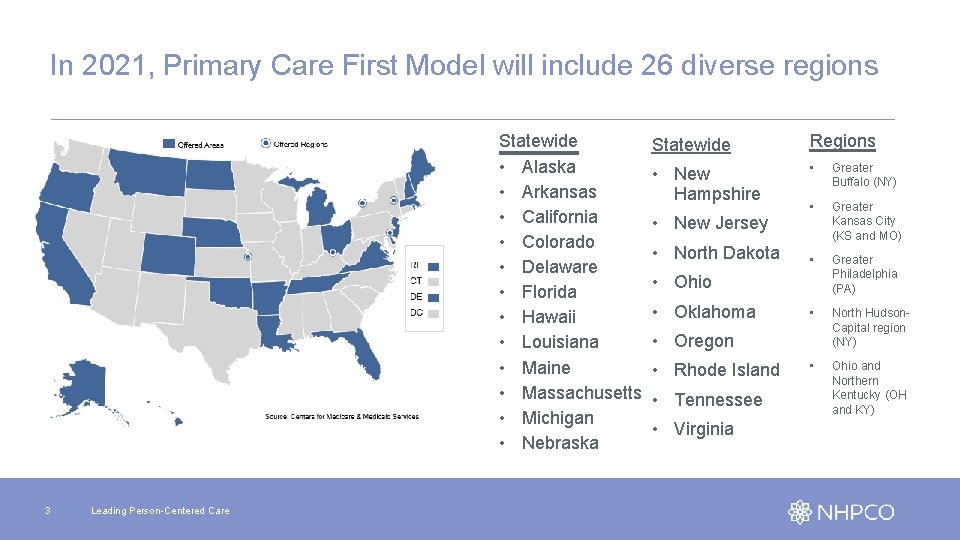
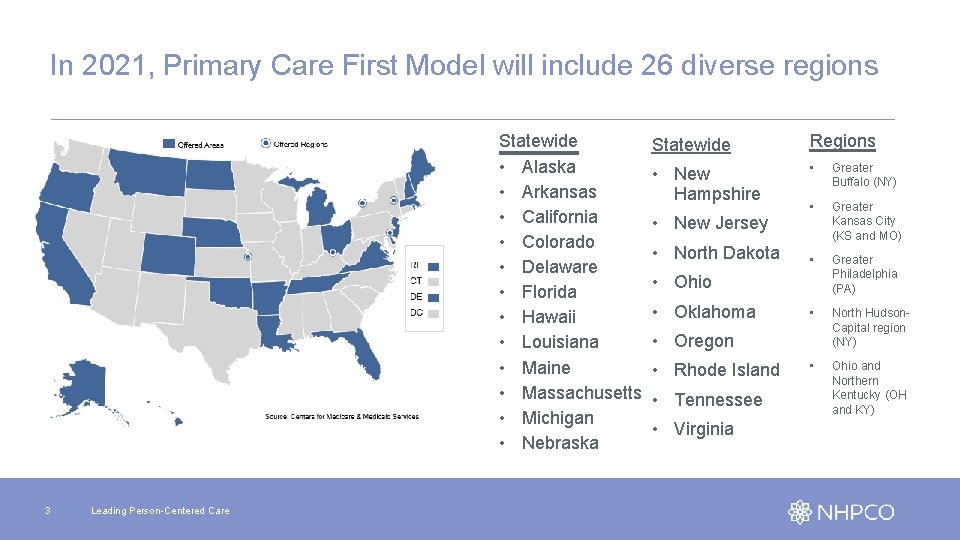
In 2021, Primary Care First Model will include 26 diverse regions Statewide • Alaska • Arkansas • California • Colorado • Delaware • Florida • Hawaii • Louisiana • Maine • Massachusetts • Michigan • Nebraska 3 Leading Person-Centered Care Statewide Regions • New Hampshire • Greater Buffalo (NY) • Greater Kansas City (KS and MO) • Greater Philadelphia (PA) • North Hudson. Capital region (NY) • Ohio and Northern Kentucky (OH and KY) • New Jersey • North Dakota • Ohio • Oklahoma • Oregon • Rhode Island • Tennessee • Virginia
What is the SIP Option? • Primary Care First is geared towards advanced primary care practices that are ready to accept financial risk in exchange for greater flexibility, increased transparency, and performance-based payments that reward participants for outcomes. SIP is one component of the broader Primary Care First model. Practices have three options: • In Primary Care First, CMS will provide payments that are higher than historical Medicare fee-for-service (FFS) payments, in the aggregate, for participating practices that care for complex, chronically ill patients. 2) Practices may choose to participate only in the SIP component of Primary Care First, and not in the PCF-General component, i. e. “SIPonly practices”; 4 Leading Person-Centered Care 1) Practices may choose to participate only in the PCF-General component of Primary Care First, and not in the SIP component, i. e. “PCFGeneral practices”; 3) Practices may choose to participate in both the SIP and PCF-General components of Primary Care First, i. e. “hybrid practices. ”
Participation Options for Hospice and Palliative Care Providers 1. Contract with a PCF hybrid practice participant to take care of their SIP patients 2. Apply to participate as a SIP only practice (one-year delay of 2015 CEHRT requirement) 3. Apply to participate as a hybrid practice (SIP and PCF General) • Your practice must meet the minimum 125 patients AND • 70% of care is as the primary care provider AND • Use 2015 Edition CEHRT 5 Leading Person-Centered Care
Model Details § Participants: § Participating practices will generally include primary care practitioners § Other clinicians that are managing high need, seriously ill populations • Patient Eligibility: § Seriously Ill Population (SIP) patients lacking: • Primary care practitioner or • Care coordination 6 Leading Person-Centered Care • Timing: § Application period: October 24, 2019 through January 22, 2020. § Practice and payer selections: Winter. Spring 2020 § Start Date: January 2021 § Duration: 6 performance years, 2 cohorts • 2021 through 2025 or • 2022 through 2026 (CPC+ only)
Eligibility: Serious Illness Medicare beneficiaries that meet one of the following claims-based criteria will be deemed to satisfy the serious illness requirement: 1) Have significant chronic or other serious illness (defined as an HCC risk score at 3. 0 or greater). 2) Have high hospital utilization in the context of chronic illness, demonstrated by both of the following: • Have an HCC risk score greater than 2. 0 and less than 3. 0; AND • Have two or more unplanned hospital admissions in the previous 12 months. 3) Show signs of frailty, as evidenced by a DME claim submitted to Medicare by a provider or supplier for a hospital bed or transfer equipment. 7 Leading Person-Centered Care
Eligibility: Care Fragmentation • No single practice (defined at the TIN level) provided more than half of their evaluation and management visits; OR • The beneficiary had two or more Emergency Department visits or observation stays in the previous 12 months; OR • Such other claims-based criteria as may be set forth in the Participation Agreement. 8 Leading Person-Centered Care
Engagement of SIP Beneficiaries: CMS Following identification, CMS will reach out to beneficiaries who meet the SIP claims-based criteria in order to solicit their interest in the model: • Once a beneficiary has indicated interest in the model, CMS will immediately (i. e. within 24 -48 hours) provide their contact information to a SIP practice through a secure information transfer method, and, depending on beneficiary and practice preferences, may even help the beneficiary schedule their first appointment. • CMS will also provide the identified practice with an updated list of SIPeligible beneficiaries on a monthly basis for tracking purposes. 9 Leading Person-Centered Care
Engagement of SIP Beneficiaries: Practice • Practices are expected to reach out to beneficiaries as soon as possible, ideally within 24 hours after they receive a beneficiary’s contact information from CMS, though they will have 60 days from when CMS includes a SIP beneficiary on their monthly SIP-eligible beneficiary list to engage that beneficiary. • After the participating practice has submitted a claim for the first face-to-face visit with the SIP beneficiary, the SIP beneficiary will be attributed to the practice and the monthly SIP payments (calculated on a PBPM basis but paid quarterly) will begin. • The practice must have a face-to-face visit with the beneficiary at least once every 60 days, as defined by dates of service on claims billed under the practice’s TIN. 10 Leading Person-Centered Care
SIP Services • Proactive engagement of seriously ill beneficiaries • Facilitate goals of care discussions to understand what matters most to seriously ill beneficiaries • Develop a care plan based on the beneficiary’s goals • Execute the plan through face-to-face and telephonic encounters • Facilitate a warm transition to the beneficiary’s long-term care provider (e. g. primary care practitioner or hospice) 11 Leading Person-Centered Care
SIP: Intensive, Time-Limited Intervention • Once a beneficiary has achieved clinical stabilization, care intensity is expected to decline, and the higher level of payment provided under the SIP component of the model is no longer necessary. • SIP-only and hybrid practices will notify CMS when they have transitioned a SIP beneficiary out of the SIP component, which will end the higher SIP PBPM payments that the practice had been receiving for that beneficiary. 12 Leading Person-Centered Care
Transition Process As part of the transition process, SIP-only and hybrid practices must: • Develop a transition plan; • Communicate the transition plan to the SIP beneficiary and obtain their approval; • Transfer the beneficiary’s detailed care plan to the receiving practitioner (if different than the SIP practitioner); and • Have a conversation with the receiving practitioner about the beneficiary (if different than the SIP practitioner). 13 Leading Person-Centered Care
Transition Process for Beneficiary • Must notify beneficiaries of the transition prior to their final face-to-face visit under the SIP component, ensuring that they understand which practitioner is responsible for their longer term care after the transition, and in instances where that practitioner is different from the SIP practitioner, facilitating a warm transition to ensure that SIP beneficiaries do not revert to fragmented care patterns • e. g. , by helping a beneficiary schedule a first appointment with the practitioner they are being transitioned to and helping the beneficiary arrange transportation to the appointment, if necessary • CMS expects that these practices will help their SIP beneficiaries establish a relationship with another health care provider in the community who will be accountable for coordinating and managing their care post-transition 14 Leading Person-Centered Care
Transitions Process to Primary Care Provider • Must have a care agreement with that provider that governs the transition and expectations of support and care coordination after the transition. • Only transition a beneficiary to another health care provider if that provider can also demonstrate advanced competencies and relevant clinical capabilities for successfully managing complex patients such as • Interdisciplinary care teams; • Comprehensive, person-centered care management, family and caregiver engagement; • 24/7 access to a member of the care team; and • Connections with community resources to address social determinants of health and behavioral health issues. 15 Leading Person-Centered Care
Possible Transition Pathways Attribution (and SIP-level payment) will last for up to 12 months*, or until one of the following circumstances occurs: 1. Beneficiary opts out of the SIP component after the first face-to-face visit (in this scenario, the practice should notify CMS); 2. The practice notifies CMS that the beneficiary has been transitioned out of the SIP component; (NOTE: the practice can still follow under fee-for-service) 3. Beneficiary began receiving hospice care, as evidenced by hospice claims 4. Beneficiary moved out of the practice's service area for SIP beneficiaries; OR 5. Beneficiary died prior to the care transition. *In some cases, it may not be possible to transition patients out of SIP after 12 months. SIP practices under good standing may request case-by-case extension. 16 Leading Person-Centered Care
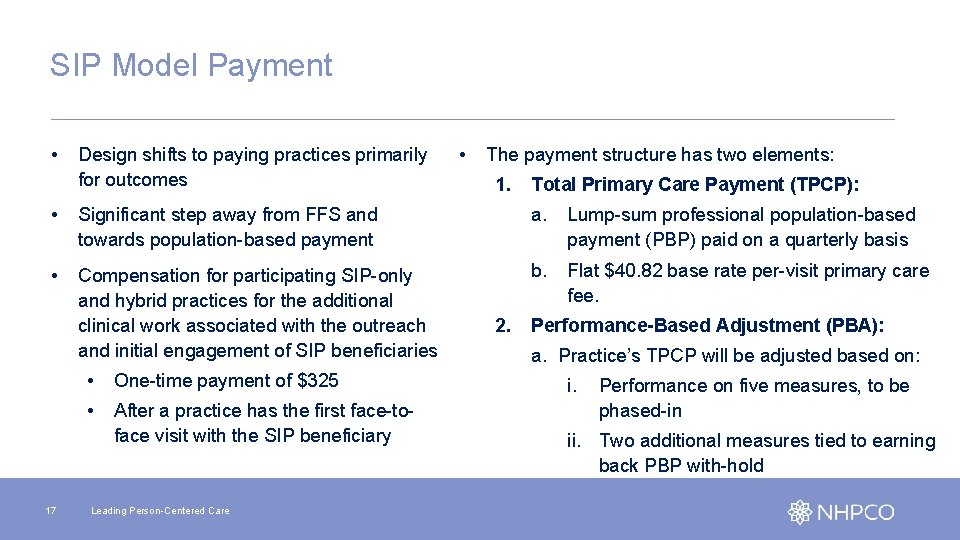
SIP Model Payment • Design shifts to paying practices primarily for outcomes • The payment structure has two elements: 1. Total Primary Care Payment (TPCP): • Significant step away from FFS and towards population-based payment a. Lump-sum professional population-based payment (PBP) paid on a quarterly basis • Compensation for participating SIP-only and hybrid practices for the additional clinical work associated with the outreach and initial engagement of SIP beneficiaries b. Flat $40. 82 base rate per-visit primary care fee. 17 • One-time payment of $325 • After a practice has the first face-toface visit with the SIP beneficiary Leading Person-Centered Care 2. Performance-Based Adjustment (PBA): a. Practice’s TPCP will be adjusted based on: i. Performance on five measures, to be phased-in ii. Two additional measures tied to earning back PBP with-hold
$50 PBPM Withhold Measures • Average SIP Length of Stay: 8 months • Rate of care transition success: At or below CMS TBD benchmark for hospitalizations or emergency department (ED) visits in the three months following their transition out of the SIP component 18 Leading Person-Centered Care
Quality Bonus Measures Performance year one: 1) The advance care plan MIPS CQM measure which requires that a clinician discuss and/or document their beneficiaries’ advance directive to ensure their preferences are considered at the end of life; and 2) Total per capita cost (TPCC), as used in MIPS. Performance year two: CMS will add a CAHPS® measure to the PBA calculation. CMS will also begin developing two quality measures for use in later years of the model: 1) Days at Home (claims-based): measures the number of days a Medicare beneficiary remains outside of an institutional care setting during a standardized time period 2) 24/7 Access to a Practitioner (survey-based): measures beneficiaries’ perception of round-the-clock access (data collected through a binary yes/no question that will be added to the CAHPS® survey currently in use for CPC+ and that will be used for Primary Care First) 19 Leading Person-Centered Care
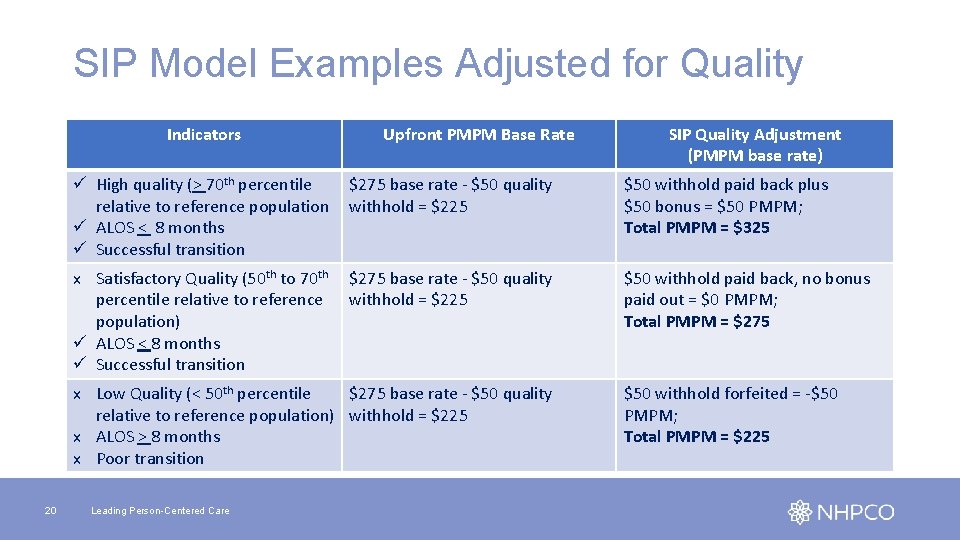
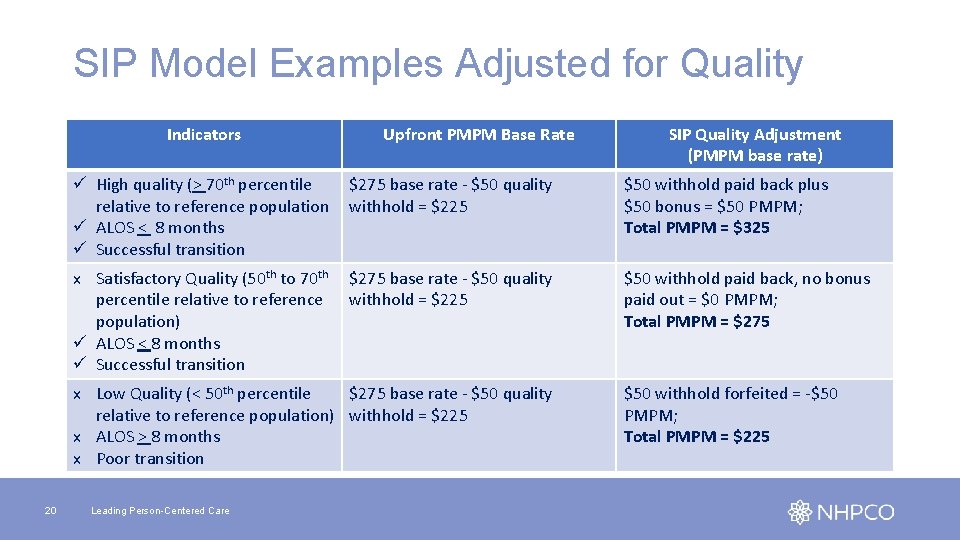
SIP Model Examples Adjusted for Quality Indicators Upfront PMPM Base Rate ü High quality (> 70 th percentile relative to reference population ü ALOS < 8 months ü Successful transition $275 base rate - $50 quality withhold = $225 $50 withhold paid back plus $50 bonus = $50 PMPM; Total PMPM = $325 x Satisfactory Quality (50 th to 70 th percentile relative to reference population) ü ALOS < 8 months ü Successful transition $275 base rate - $50 quality withhold = $225 $50 withhold paid back, no bonus paid out = $0 PMPM; Total PMPM = $275 x Low Quality (< 50 th percentile $275 base rate - $50 quality relative to reference population) withhold = $225 x ALOS > 8 months x Poor transition 20 SIP Quality Adjustment (PMPM base rate) Leading Person-Centered Care $50 withhold forfeited = -$50 PMPM; Total PMPM = $225
Ongoing Support for NHPCO Members • Edge • Help with readiness evaluation, application process and additional program development: access Acclivity Health and Emprise Health (member discount/password protected) • Understanding the opportunity: access our Business webinar series • NHPCO New Care Models Learning Collaborative • Office hours • Learning community at My. NHPCO • Up to date info: Models and Demos (password protected) • National Hospice and Palliative Care Coalition Webinar November 19 • CMS staff will present with Coalition members • Link to register: https: //www. nationalcoalitionhpc. org/apm-webinar/ 21 Leading Person-Centered Care
Poll question Which of these best describes the services your organization offers today: • Hospice only • Some pre-hospice services • Many, mature pre-hospice services 22 Leading Person-Centered Care
Poll questions Are you planning to apply for the PCF SIP model? • Yes • Undecided • No What areas of the model do you need more information about? • Patient eligibility criteria and engagement • Provider eligibility • Services • Quality • Payment 23 Leading Person-Centered Care

Questions? 24 Leading Person-Centered Care
 Nhpco gip tip sheet
Nhpco gip tip sheet Primary secondary and tertiary health care
Primary secondary and tertiary health care Improving chronic illness care model
Improving chronic illness care model Population ecology section 1 population dynamics answer key
Population ecology section 1 population dynamics answer key Section 1 population dynamics
Section 1 population dynamics Population ecology section 1 population dynamics
Population ecology section 1 population dynamics Population ecology section 1 population dynamics answer key
Population ecology section 1 population dynamics answer key Acs to ise migration tool
Acs to ise migration tool Rd acs
Rd acs Fort gordon tasc
Fort gordon tasc Secure access control server
Secure access control server Acs uzbūve
Acs uzbūve Acs beacon
Acs beacon Anderson cook
Anderson cook Acs cts
Acs cts Acs bogdana
Acs bogdana Acs functions
Acs functions Acs programming language
Acs programming language Retorno acs esquema
Retorno acs esquema Acs comp
Acs comp Acs
Acs Acs attitude control system
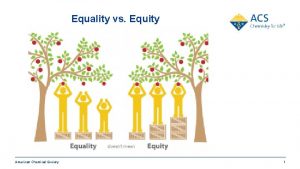
Acs attitude control system Acs green chemistry institute
Acs green chemistry institute Concurso acs recife
Concurso acs recife Acs
Acs