Direct Contracting Models Annie Acs NHPCO Director Health
- Slides: 22
Direct Contracting Models Annie Acs, NHPCO Director Health Policy & Innovation Lori Bishop, NHPCO Vice President Palliative & Advanced Care Khue Nguyen, Emprise Health Jeremy Powell, Acclivity Health December 9, 2019 1 Leading Person-Centered Care
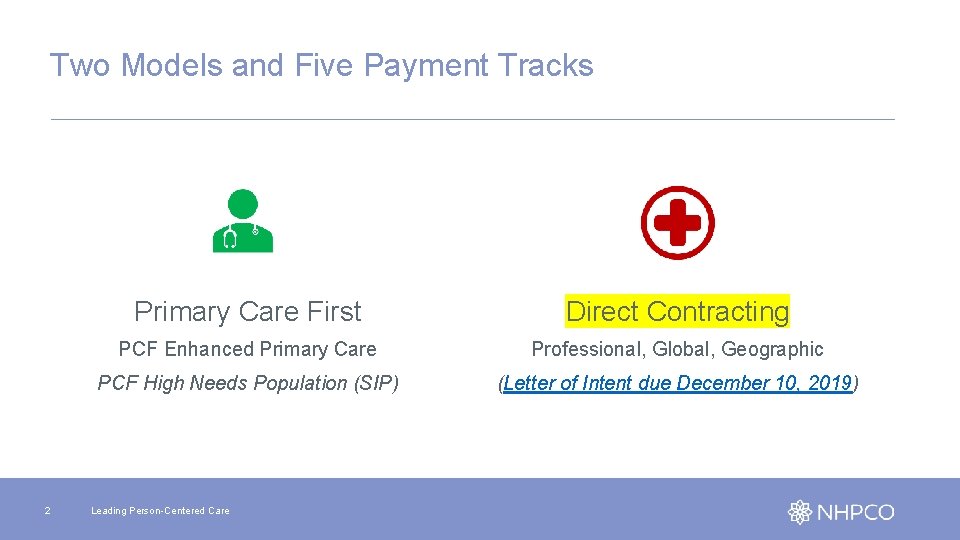
Two Models and Five Payment Tracks 2 Primary Care First Direct Contracting PCF Enhanced Primary Care Professional, Global, Geographic PCF High Needs Population (SIP) (Letter of Intent due December 10, 2019) Leading Person-Centered Care
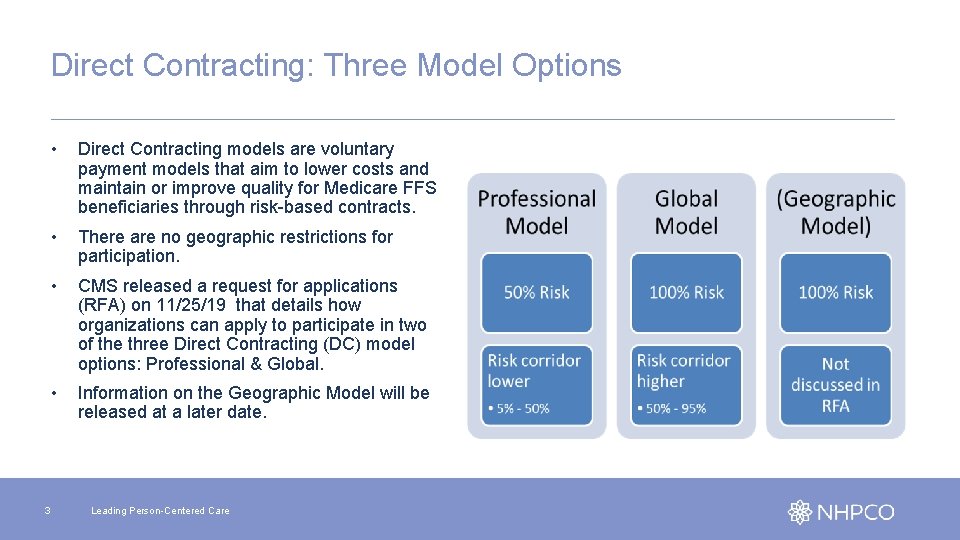
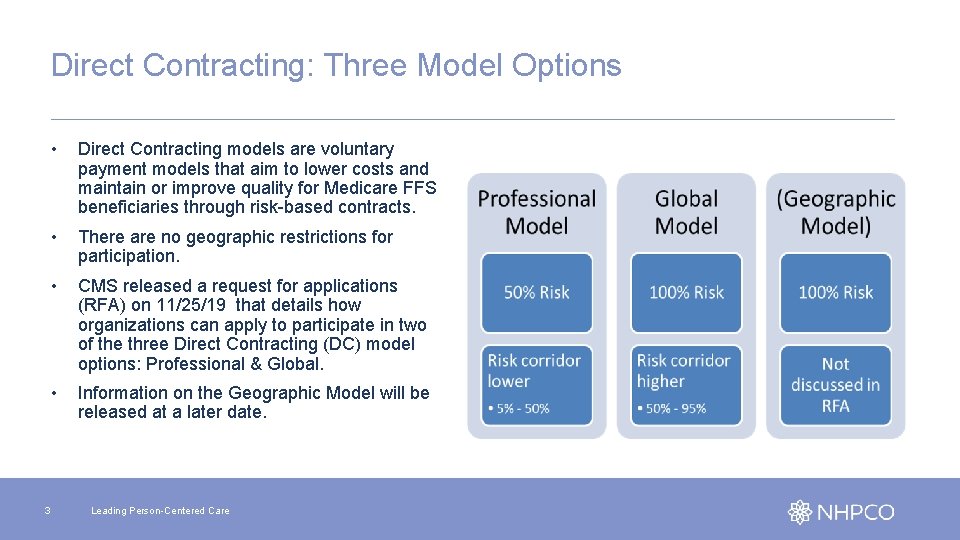
Direct Contracting: Three Model Options 3 • Direct Contracting models are voluntary payment models that aim to lower costs and maintain or improve quality for Medicare FFS beneficiaries through risk-based contracts. • There are no geographic restrictions for participation. • CMS released a request for applications (RFA) on 11/25/19 that details how organizations can apply to participate in two of the three Direct Contracting (DC) model options: Professional & Global. • Information on the Geographic Model will be released at a later date. Leading Person-Centered Care
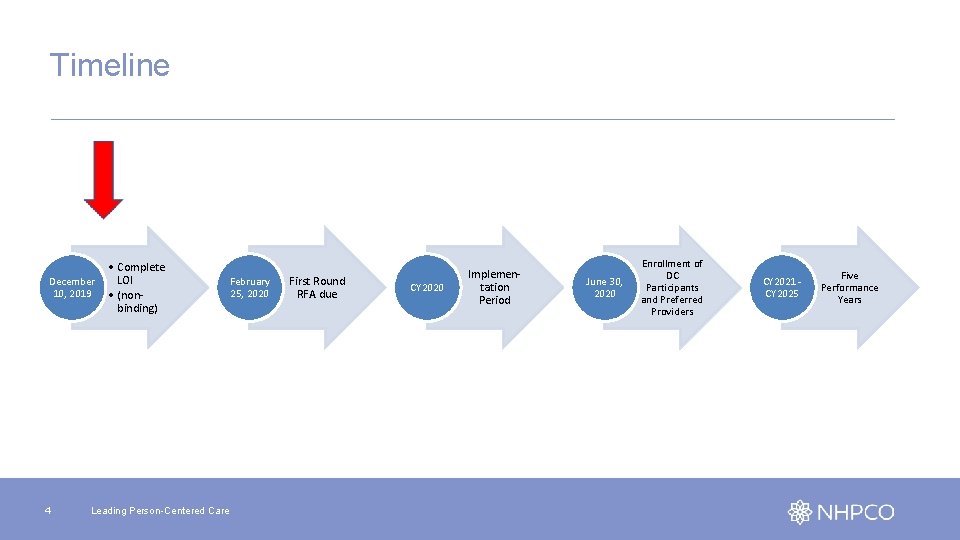
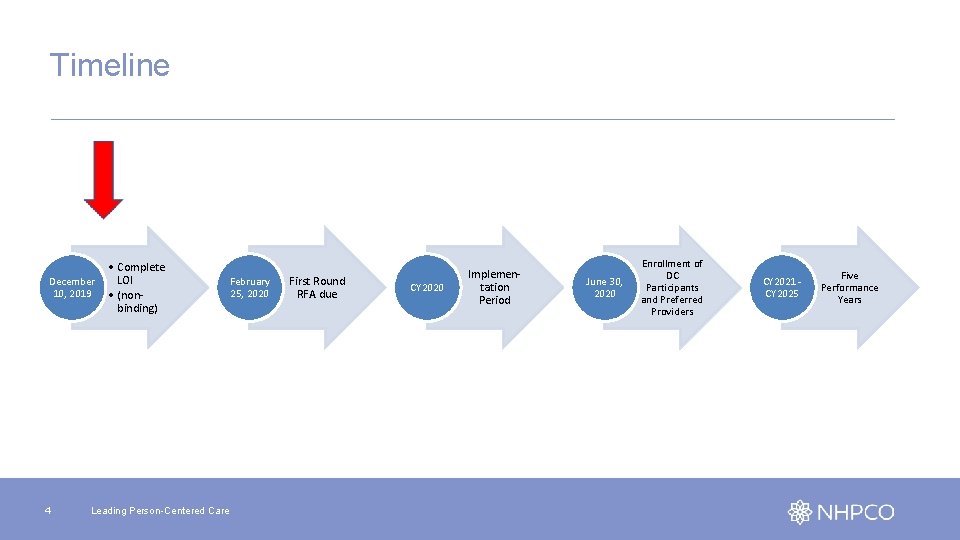
Timeline December 10, 2019 4 • Complete LOI • (nonbinding) Leading Person-Centered Care February 25, 2020 First Round RFA due CY 2020 Implementation Period June 30, 2020 Enrollment of DC Participants and Preferred Providers CY 2021 CY 2025 Five Performance Years
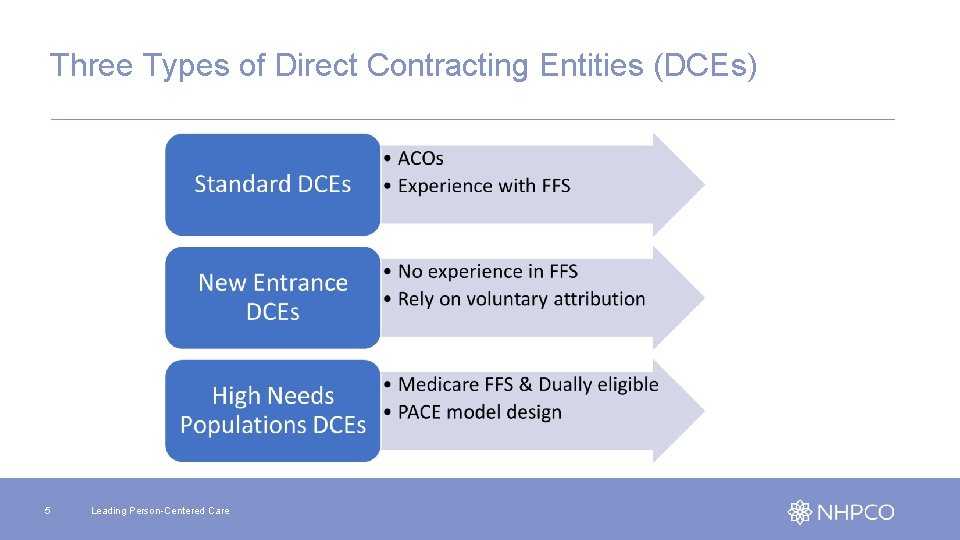
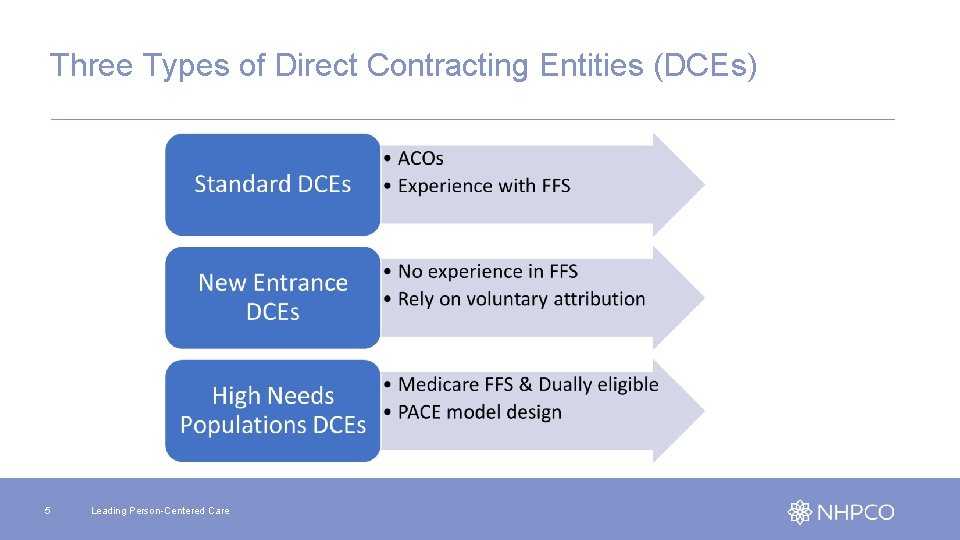
Three Types of Direct Contracting Entities (DCEs) 5 Leading Person-Centered Care
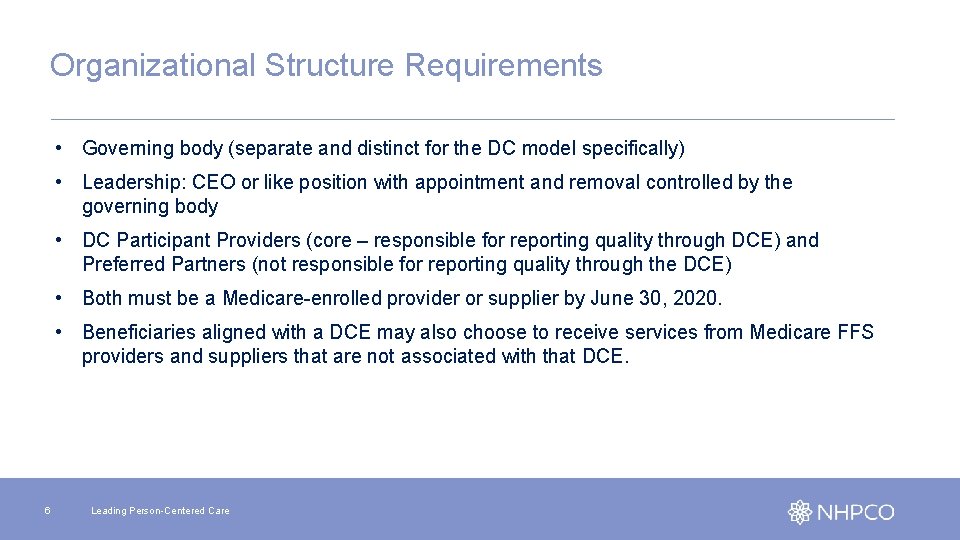
Organizational Structure Requirements • Governing body (separate and distinct for the DC model specifically) • Leadership: CEO or like position with appointment and removal controlled by the governing body • DC Participant Providers (core – responsible for reporting quality through DCE) and Preferred Partners (not responsible for reporting quality through the DCE) • Both must be a Medicare-enrolled provider or supplier by June 30, 2020. • Beneficiaries aligned with a DCE may also choose to receive services from Medicare FFS providers and suppliers that are not associated with that DCE. 6 Leading Person-Centered Care
Participant Providers • Identified by a combination of their TIN and NPI. • However, splitting the TIN will be permitted, which will allow DC Participant Providers with separate NPIs who bill through the same TIN to join separate models. 7 Leading Person-Centered Care
Preferred Partners 1. Preferred Provider for one or more other DCEs participating in Direct Contracting; 2. DC Participant Provider in another DCE participating in Direct Contracting; 3. ACO participant, ACO provider or supplier and/or ACO professional in an ACO in the Shared Savings Program (note: CMS intends to waive the non-duplication requirements under section 1899(b)(4)(A) of the Act and 42 C. F. R. § 425. 114(a) as they apply to Preferred Providers as necessary solely for purposes of testing Direct Contracting); and/or 4. a role similar in function to a DC Participant Provider in another Medicare initiative that involves shared savings. 8 Leading Person-Centered Care
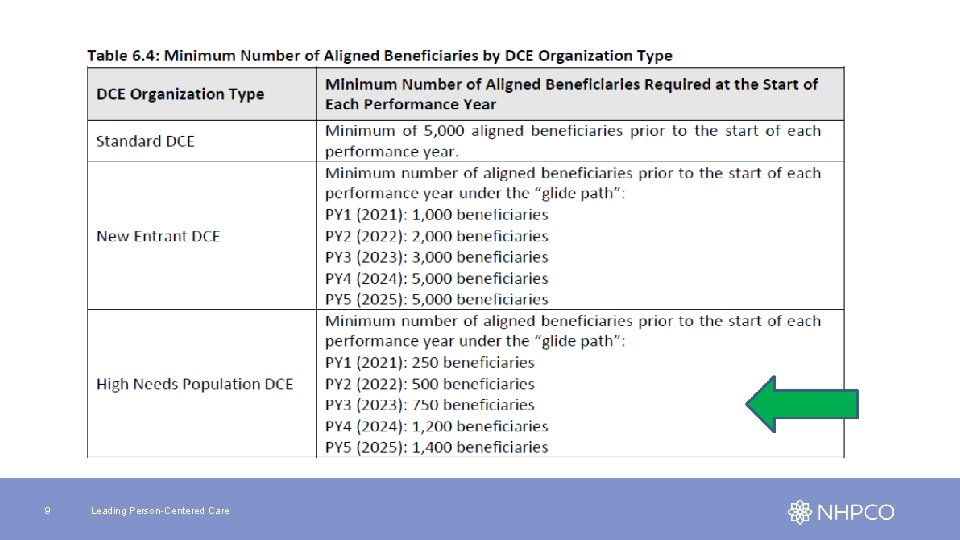
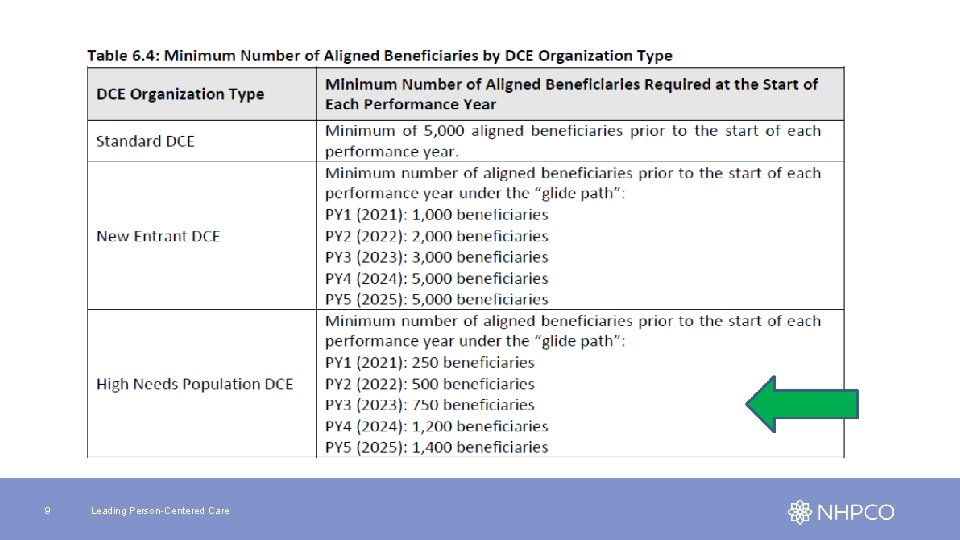
9 Leading Person-Centered Care
High Needs Population (HNP) DCE • Includes Medicare FFS beneficiaries at risk for becoming dually eligible and complex, high needs dually eligible beneficiaries • Replicate PACE model (but not limited to individuals who are age 55 or older) • Enable individuals to continue living in non-institutional, community settings as long as medically and socially feasible • Emphasize preventative care, meet regularly to update the care plan in response to changes in beneficiaries’ functional and health status and provide regular clinical monitoring (reduces hospitalizations due to ambulatory sensitive conditions AND • Manage beneficiaries’ care across settings, which helps facilitate smooth transitions between settings and reduce hospitalizations 10 Leading Person-Centered Care
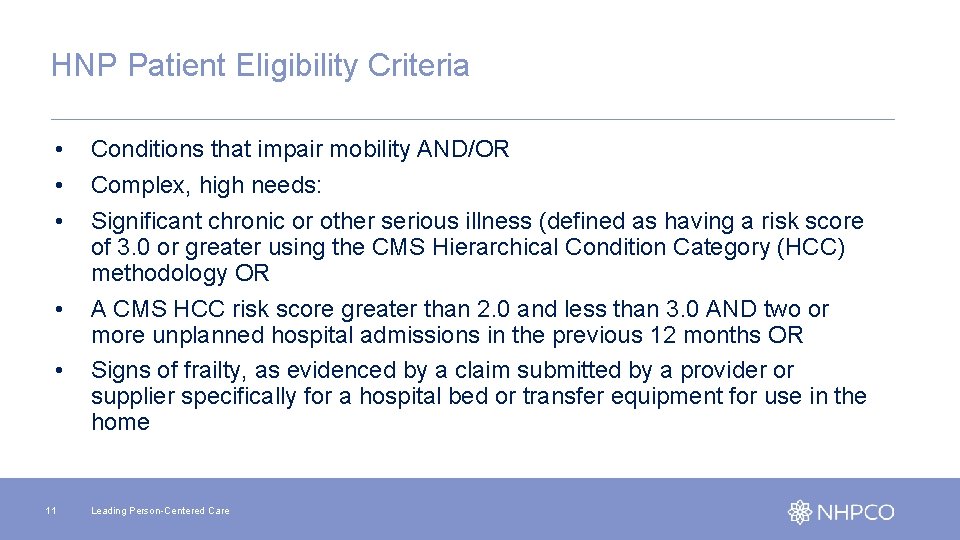
HNP Patient Eligibility Criteria • • • 11 Conditions that impair mobility AND/OR Complex, high needs: Significant chronic or other serious illness (defined as having a risk score of 3. 0 or greater using the CMS Hierarchical Condition Category (HCC) methodology OR A CMS HCC risk score greater than 2. 0 and less than 3. 0 AND two or more unplanned hospital admissions in the previous 12 months OR Signs of frailty, as evidenced by a claim submitted by a provider or supplier specifically for a hospital bed or transfer equipment for use in the home Leading Person-Centered Care
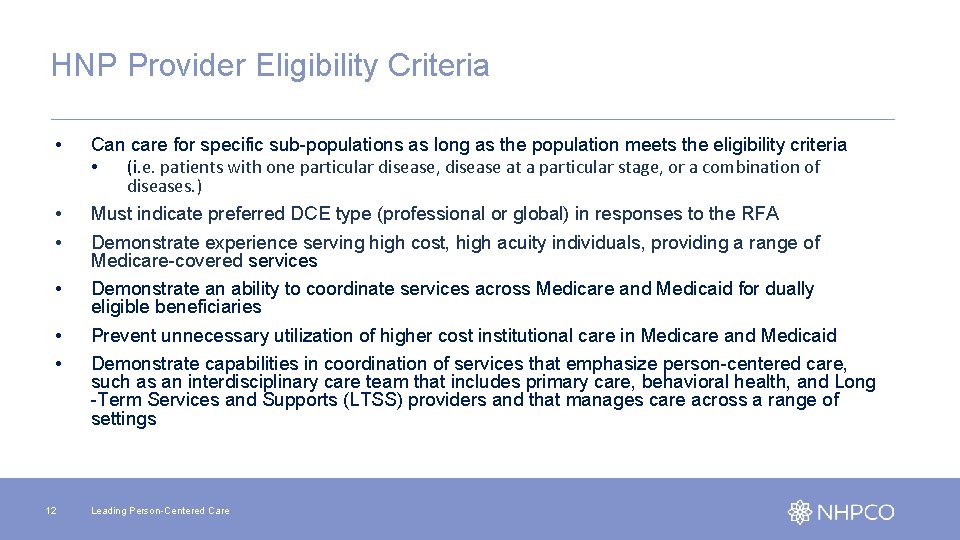
HNP Provider Eligibility Criteria • Can care for specific sub-populations as long as the population meets the eligibility criteria • (i. e. patients with one particular disease, disease at a particular stage, or a combination of diseases. ) • • Must indicate preferred DCE type (professional or global) in responses to the RFA Demonstrate experience serving high cost, high acuity individuals, providing a range of Medicare-covered services Demonstrate an ability to coordinate services across Medicare and Medicaid for dually eligible beneficiaries Prevent unnecessary utilization of higher cost institutional care in Medicare and Medicaid Demonstrate capabilities in coordination of services that emphasize person-centered care, such as an interdisciplinary care team that includes primary care, behavioral health, and Long -Term Services and Supports (LTSS) providers and that manages care across a range of settings • • • 12 Leading Person-Centered Care
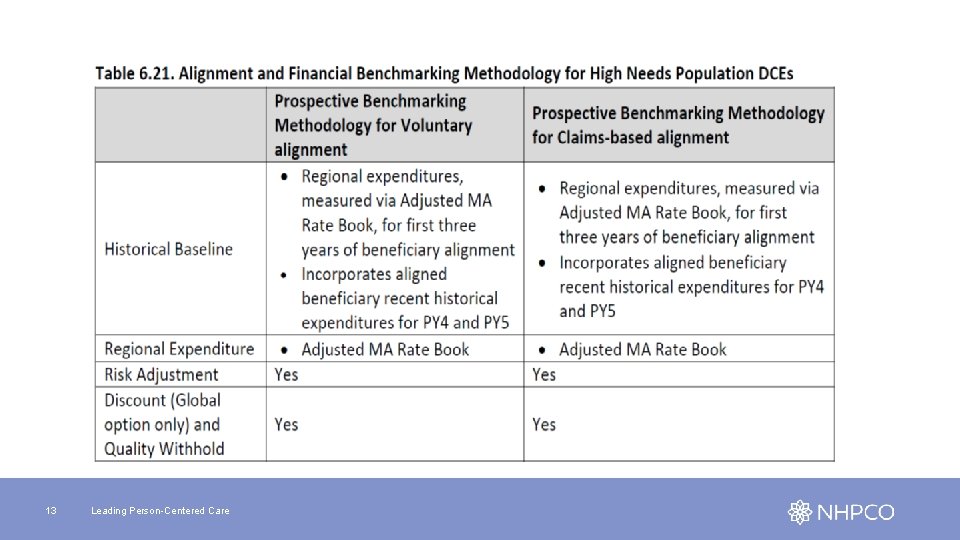
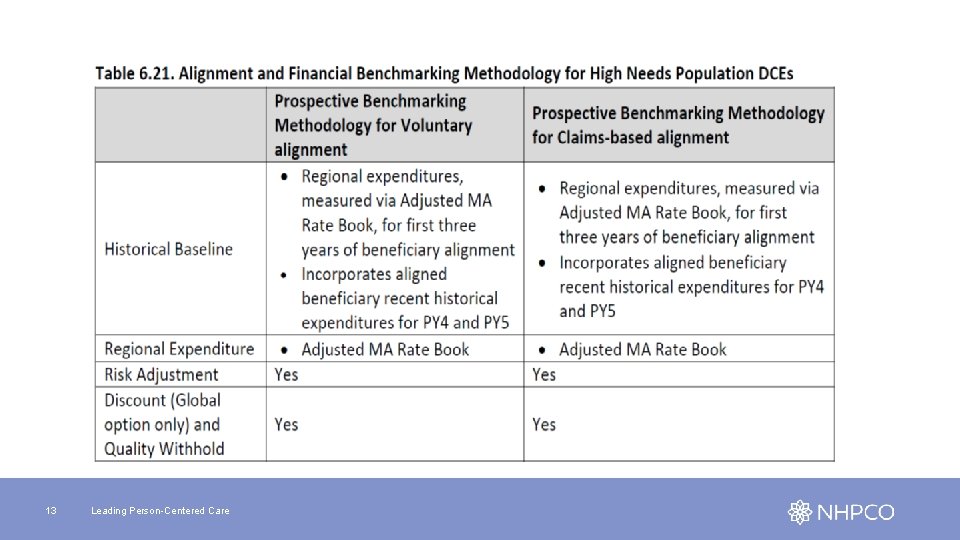
13 Leading Person-Centered Care
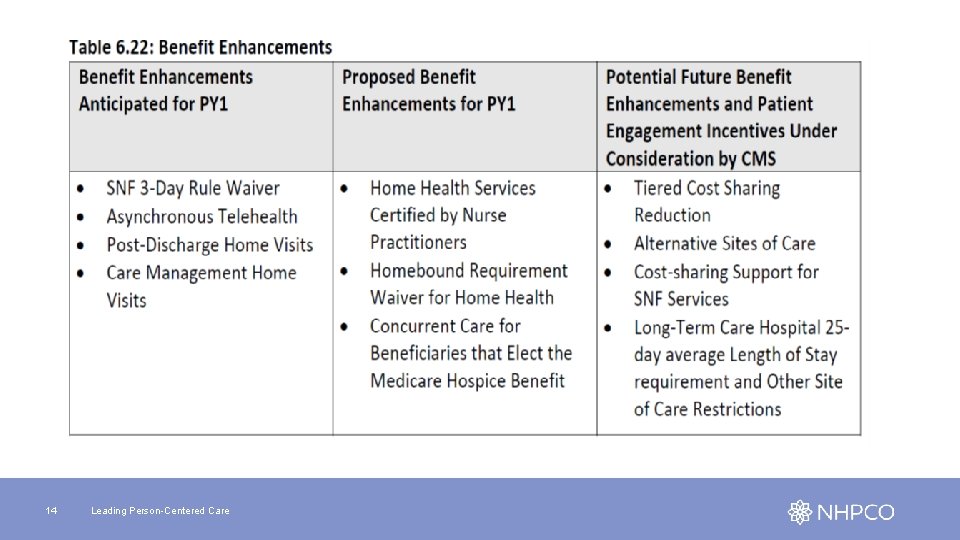
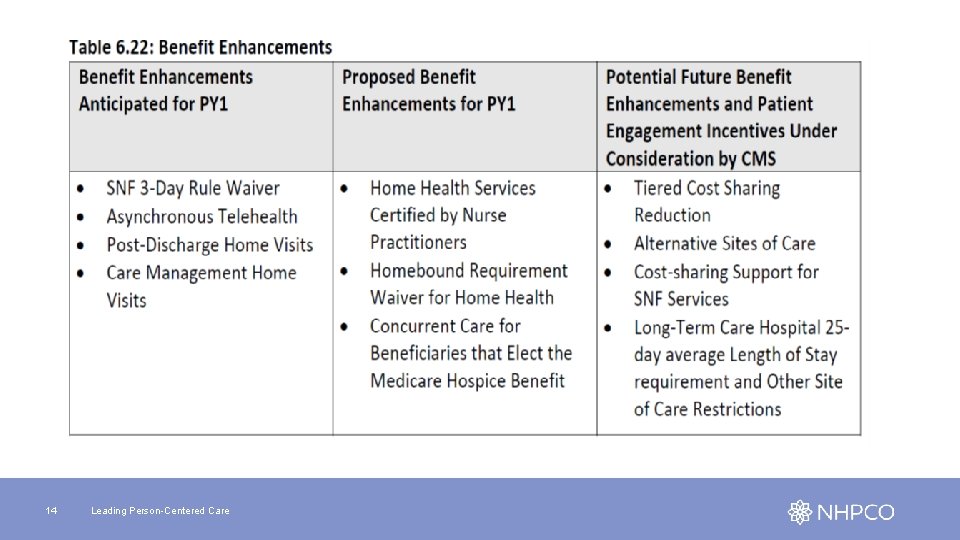
14 Leading Person-Centered Care
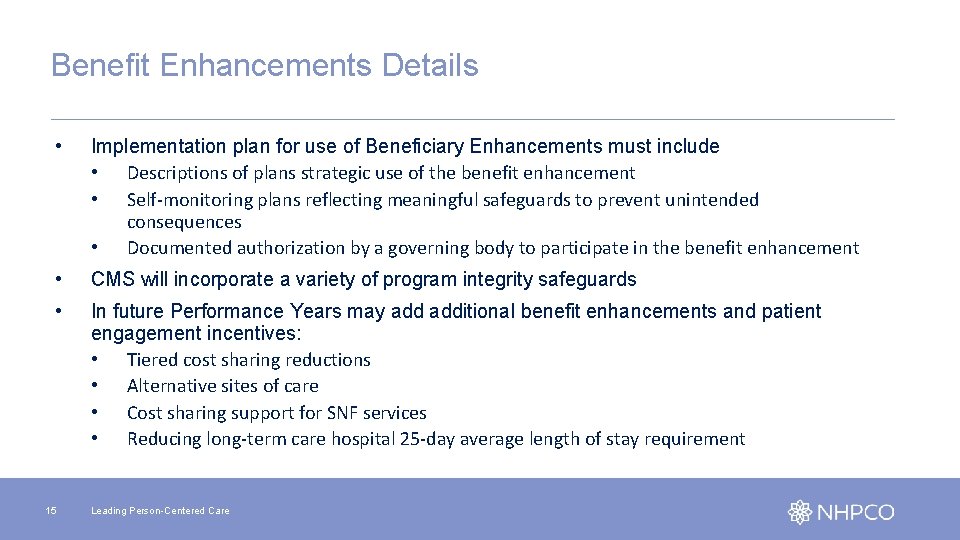
Benefit Enhancements Details • Implementation plan for use of Beneficiary Enhancements must include • Descriptions of plans strategic use of the benefit enhancement • Self-monitoring plans reflecting meaningful safeguards to prevent unintended consequences • Documented authorization by a governing body to participate in the benefit enhancement • CMS will incorporate a variety of program integrity safeguards • In future Performance Years may additional benefit enhancements and patient engagement incentives: • Tiered cost sharing reductions • Alternative sites of care • Cost sharing support for SNF services • Reducing long-term care hospital 25 -day average length of stay requirement 15 Leading Person-Centered Care
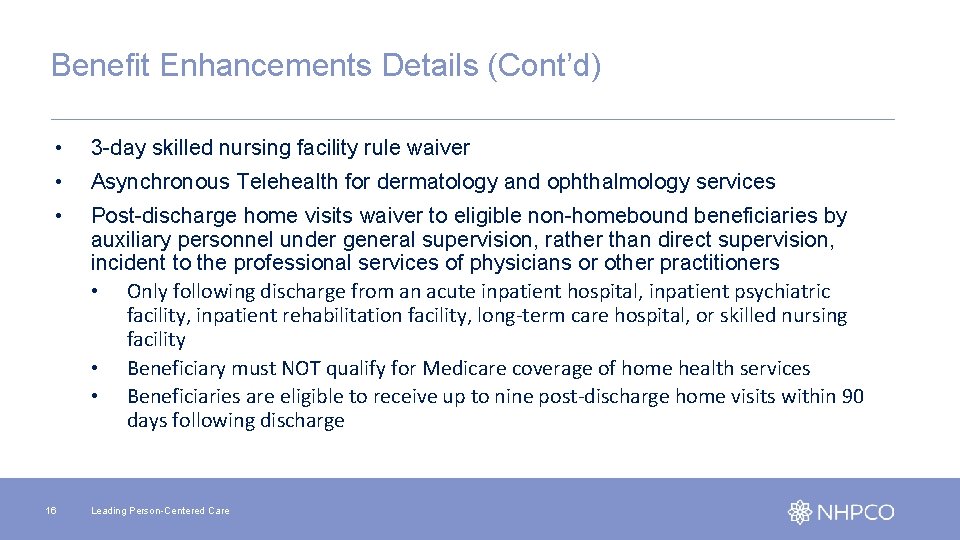
Benefit Enhancements Details (Cont’d) • 3 -day skilled nursing facility rule waiver • Asynchronous Telehealth for dermatology and ophthalmology services • Post-discharge home visits waiver to eligible non-homebound beneficiaries by auxiliary personnel under general supervision, rather than direct supervision, incident to the professional services of physicians or other practitioners • Only following discharge from an acute inpatient hospital, inpatient psychiatric facility, inpatient rehabilitation facility, long-term care hospital, or skilled nursing facility • Beneficiary must NOT qualify for Medicare coverage of home health services • Beneficiaries are eligible to receive up to nine post-discharge home visits within 90 days following discharge 16 Leading Person-Centered Care
Benefit Enhancements Details (Cont’d) • Care Management Home Visits waiver of requirement for direct supervision to allow payment for certain home visits that are furnished to eligible beneficiaries proactively and in advance of potential hospitalization • Services typically covered under Medicare Part B as “incident to” the services of a physician or other practitioner by auxiliary personnel under general supervision, rather than direct supervision • Supplement rather than substitute for visits by the primary care practitioner • May receive up to 12 care management home visits within a calendar year • Home Health Services Certified by Nurse Practitioners • Home Health Homebound Requirement 17 Leading Person-Centered Care
Benefit Enhancements Details (Cont’d) • Concurrent Care for Beneficiaries that Elect the Medicare Hospice Benefit (Global only) • Cannot partner with any hospice that has existing condition level deficiencies that have not been remediated • All hospice programs the DCE partners with must readily offer beneficiaries access to the four levels of hospice care consistent with clinical need (See pages 61 and 62 of the Request for Applications) 18 Leading Person-Centered Care
Quality and Performance • Claims-based and CAHPS for ACOs surveys • DCEs will be required to report quality measures beginning PY 1 (CY 2021) but will not be pay-for-performance initially • May opt to implement a Patient Activation Measure (PAM) survey. CMMI will cover the costs of licensing, data collection, and analysis • CMS may conduct data validation audits • Continuous Improvement/Sustained Exceptional Performance Criteria (CI/SEP) begins PY 2 (CY 2022) to earn back withhold and possibly earn a bonus payment from the High Performers Pool (HPP) 19 Leading Person-Centered Care
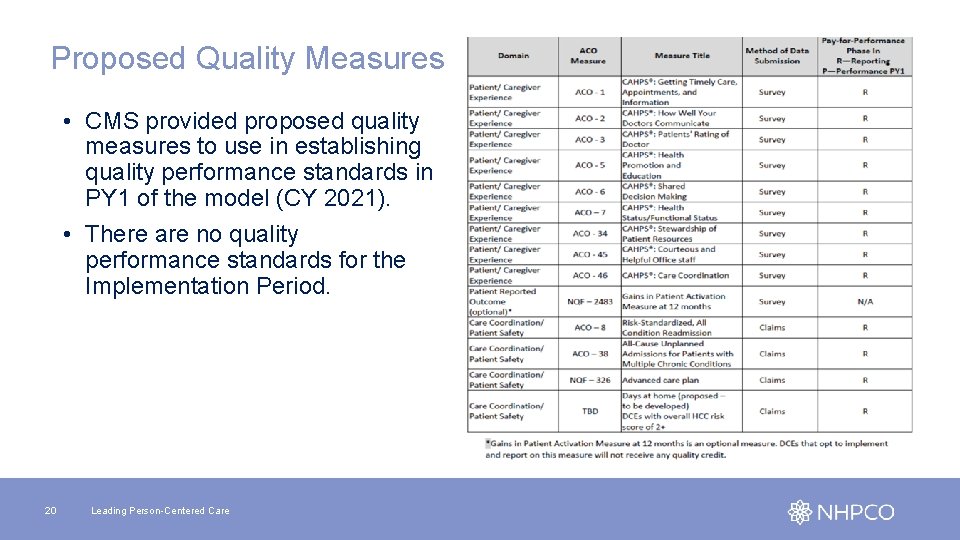
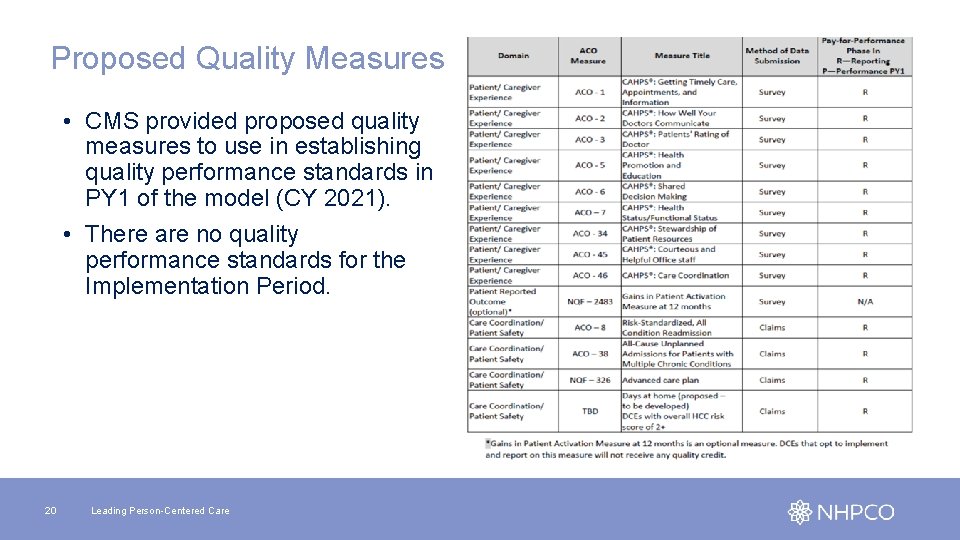
Proposed Quality Measures • CMS provided proposed quality measures to use in establishing quality performance standards in PY 1 of the model (CY 2021). • There are no quality performance standards for the Implementation Period. 20 Leading Person-Centered Care
What Should a Hospice Do? üDetermine your level of participation üIf you are considering participation as a High Needs Population DCE – complete LOI by December 10, 2019 (Tomorrow!) üIdentify DCE activity in your geography üSeek contract as Participant Provider or Preferred Partner 21 Leading Person-Centered Care
Questions? Helpful Links: • CMS Direct Contracting Website (RFA, FAQs, etc. ) • NHPCO Edge Partners • My. NHPCO Palliative Care Community For all other inquiries, please reach out to innovation@nhpco. org 22 Leading Person-Centered Care
 Nhpco gip tip sheet
Nhpco gip tip sheet What is the difference between models and semi modals
What is the difference between models and semi modals Cisco ise upgrade readiness tool
Cisco ise upgrade readiness tool Rd acs
Rd acs Newcomers orientation
Newcomers orientation Secure access acs
Secure access acs Acs uzbūve
Acs uzbūve Preventive services acs
Preventive services acs Atlas timi 51
Atlas timi 51 G staff army
G staff army Bogdan's eso
Bogdan's eso Viktor fedun
Viktor fedun Mphil acs
Mphil acs Retorno acs esquema
Retorno acs esquema Msc acs
Msc acs Acs
Acs Acs attitude control system
Acs attitude control system Acs green chemistry institute
Acs green chemistry institute Concurso acs recife
Concurso acs recife Acs
Acs Acs dobfar welfare
Acs dobfar welfare Dot
Dot Atlas timi 51
Atlas timi 51