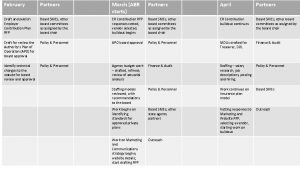
Partners in Advocacy ACS Fellows and The ACS















- Slides: 35
Partners in Advocacy ACS Fellows and The ACS Washington Office 2013 Wisconsin State Chapter Meeting

I don't make jokes. I just watch the government and report the facts. -- Will Rogers
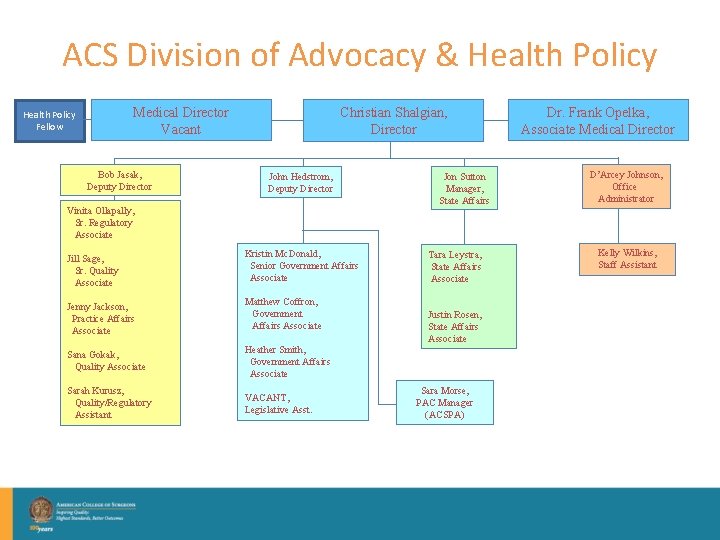
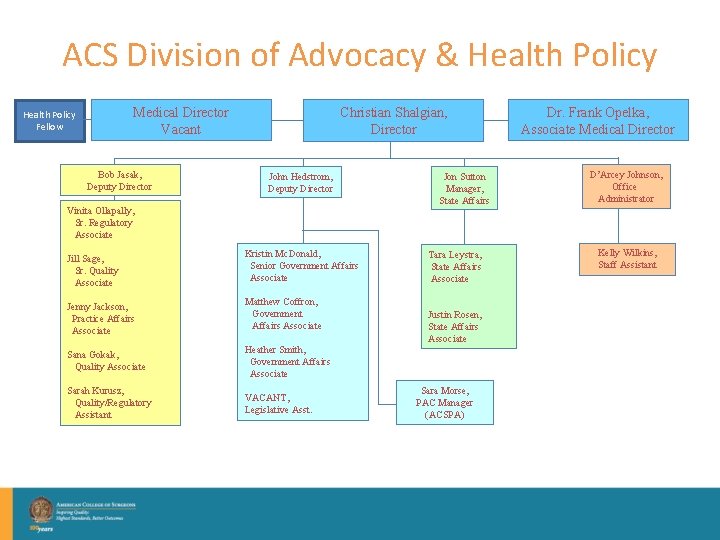
ACS Division of Advocacy & Health Policy Medical Director Vacant Health Policy Fellow Bob Jasak, Deputy Director Christian Shalgian, Director John Hedstrom, Deputy Director Vinita Ollapally, Sr. Regulatory Associate Jill Sage, Sr. Quality Associate Kristin Mc. Donald, Senior Government Affairs Associate Jenny Jackson, Practice Affairs Associate Matthew Coffron, Government Affairs Associate Sana Gokak, Quality Associate Heather Smith, Government Affairs Associate Sarah Kurusz, Quality/Regulatory Assistant VACANT, Legislative Asst. Jon Sutton Manager, State Affairs Tara Leystra, State Affairs Associate Justin Rosen, State Affairs Associate Sara Morse, PAC Manager (ACSPA) Dr. Frank Opelka, Associate Medical Director D’Arcey Johnson, Office Administrator Kelly Wilkins, Staff Assistant



YEAR FORMULA UPDATE ACTUAL UPDATE LEGISLATION 2002 -4. 8% 2003 -4. 4 1. 4% Consolidated Appropriations Resolution 2004 -4. 5% 1. 5% Medicare Modernization Act (P. L. 108 -173) 2005 -3. 3% 1. 5% Medicare Modernization Act (P. L. 108 -173) 2006 -4. 4% 0. 2% Deficit Reduction Act of 2005 (P. L. 109 -171) 2007 -5% 0% Tax Relief and Health Care Act of 2006 (P. L. 109 -432) 2008 January to June -10. 1% 0. 5% Medicare, Medicaid, SCHIP Extension Act of 2007 (P. L. 110 -173) 2008 July to December -10. 6% 0% Medicare Improvements for Patients and Providers Act of 2008 (110 -275) 0% 1. 1% Medicare Improvements for Patients and Providers Act of 2008 (110 -275) 2010 January to February -21. 3% 0% Department of Defense Appropriations Act (P. L. 111 -118) 2010 March -21. 3% 0% Temporary Extensions Act (P. L. 111 -144) 2010 April to May -21. 3% 0% Continuing Extensions Act (P. L. 111 -157) 2010 June to November -21. 3% 2. 2% Preservation of Access to Care for Medicare Beneficiaries and Pension Relief Act (P. L. 111192) 2010 December -23. 6% 2. 2% The Physician Payment and Therapy Relief Act of 2010 (P. L. 111 -286) 2011 -23. 6% 0% Medicare and Medicaid Extenders Act of 2010 (P. L. 111 -309) 2012 January to February -27. 4% 0% Temporary Payroll Tax Cut Continuation Act of 2011 (P. L. 112 -78) 2012 March to December -27. 4% 0% Middle Class Tax Relief and Job Creation Act of 2011 (P. L. 112 -96) 2013 -27% 0% -2% sequester 2014 -24. 4% 2009
SEQUESTER! Great for Scrabble, horrible for budgeting

History of Physician Payment 1989 • Medicare Volume Performance Standard (MVPS) established by OBRA 1966 -1992 • Reasonable Charge Payments 1989 • Medicare Physician Fee Schedule established by Omnibus Budget Reconciliation Act (OBRA) • Effective in 1992 2006 2015 • Physician • Electronic Quality Reporting Initiative 1997 • Sustainable Growth Rate established by Balanced Budget Act Health Records 2012 2015 • Electronic • Physician Prescribing Value-Based Modifier

How Physicians Are Paid Today PQRI Electronic Prescribing Shared Savings Value-Based Modifier Patient Care Performance Demonstrations Electronic Health Records Primary Care Bonus Health Professions Shortage Area General Surgery Bonus

How Most Physicians Feel
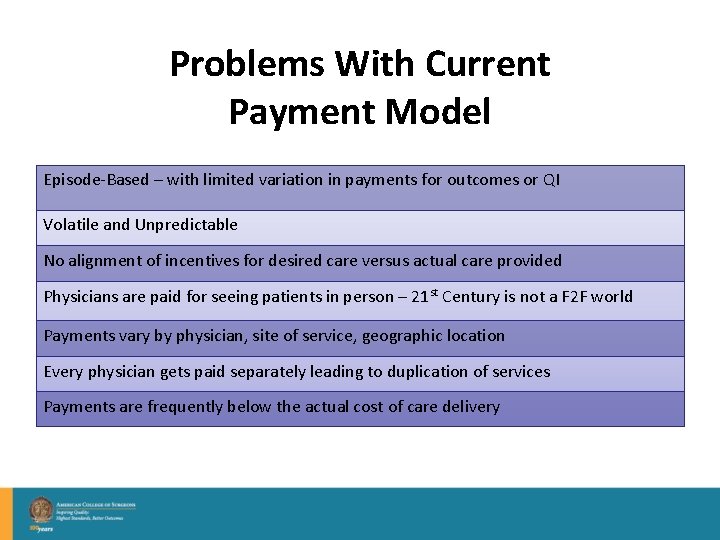
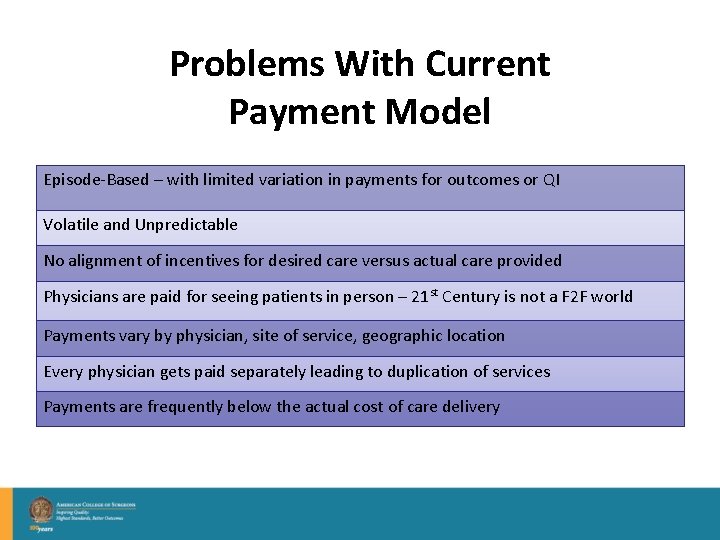
Problems With Current Payment Model Episode-Based – with limited variation in payments for outcomes or QI Volatile and Unpredictable No alignment of incentives for desired care versus actual care provided Physicians are paid for seeing patients in person – 21 st Century is not a F 2 F world Payments vary by physician, site of service, geographic location Every physician gets paid separately leading to duplication of services Payments are frequently below the actual cost of care delivery
We stand today at a crossroads. One path leads to despair and utter hopelessness. The other leads to total extinction. Let us hope we have the wisdom to make the right choice. Woody Allen
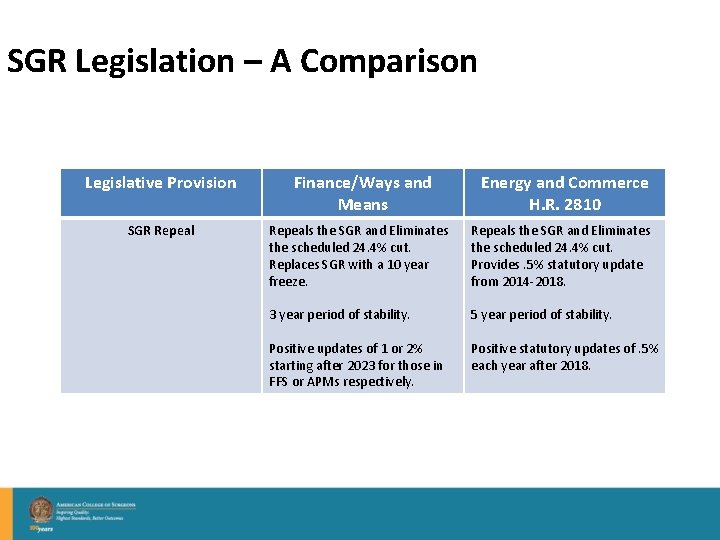
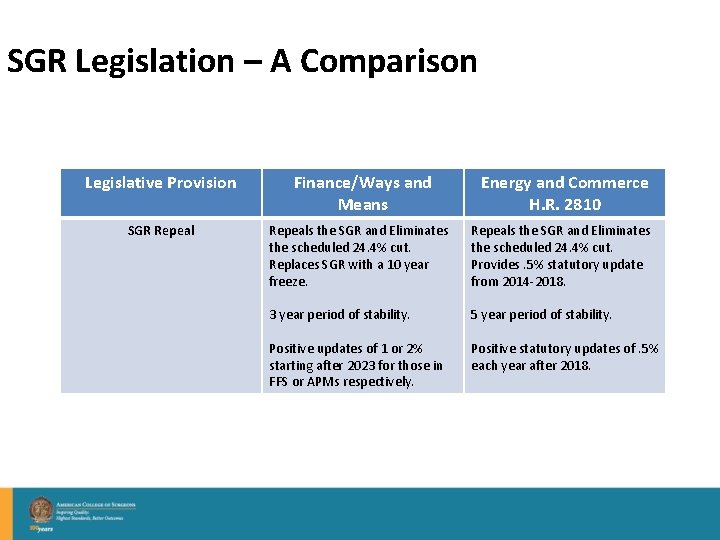
SGR Legislation – A Comparison Legislative Provision Finance/Ways and Means Energy and Commerce H. R. 2810 SGR Repeals the SGR and Eliminates the scheduled 24. 4% cut. Replaces SGR with a 10 year freeze. Repeals the SGR and Eliminates the scheduled 24. 4% cut. Provides. 5% statutory update from 2014 -2018. 3 year period of stability. Positive updates of 1 or 2% starting after 2023 for those in FFS or APMs respectively. 5 year period of stability. Positive statutory updates of. 5% each year after 2018.
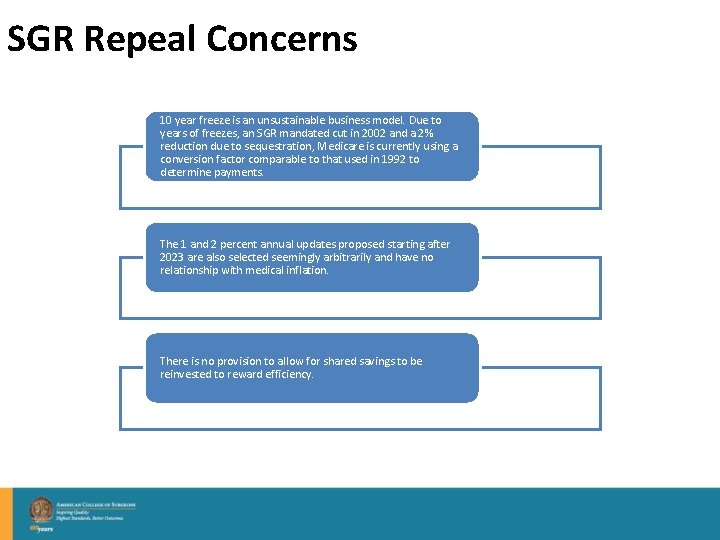
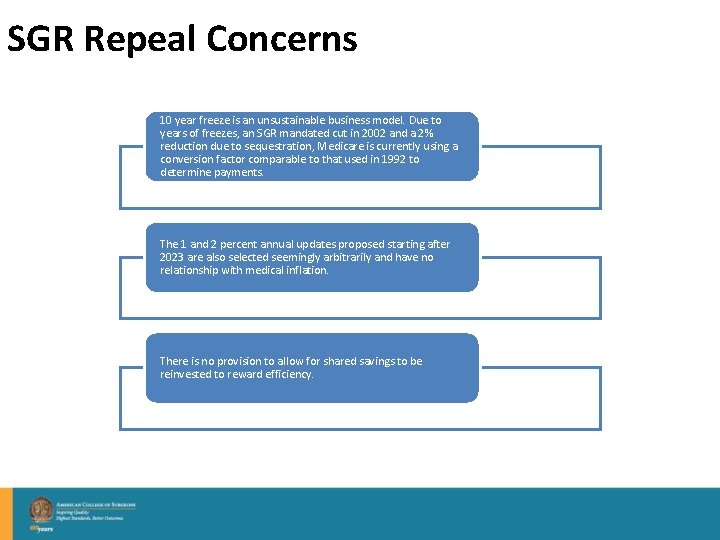
SGR Repeal Concerns 10 year freeze is an unsustainable business model. Due to years of freezes, an SGR mandated cut in 2002 and a 2% reduction due to sequestration, Medicare is currently using a conversion factor comparable to that used in 1992 to determine payments. The 1 and 2 percent annual updates proposed starting after 2023 are also selected seemingly arbitrarily and have no relationship with medical inflation. There is no provision to allow for shared savings to be reinvested to reward efficiency.

SGR Legislation – A Comparison Legislative Provision Value Based Program (Fee for Service) Finance/Ways and Means Energy and Commerce H. R. 2810 Value Based Performance Payment Program – Physicians Continuing in Fee For Service will Take on Risk that is comparable to the amount at risk under current law through PQRS, EHRMU and VBM: 8% in 2017; 9% in 2018; 10% in 2019; Can Increase at Secretary’s Discretion beginning in 2020. While at risk, can also earn performance-based incentive payments through a compulsory budget-neutral program. Professionals who treat few Medicare patients and those who are in the APM are excluded from the VBP program. Performance would be assessed based on a composite score that encompasses all of the applicable categories. Payments for those with higher scores would be offset by those providers with poor performance. Can assess on the group-level at the associated hospital or facility. Assistance to small practices would be provided. Feedback on performance would be available on a timely basis. After period of stability and beginning in 2019, a Quality Update Incentive Program (QUIP) facilitates fee schedule updates for self-selected provider "peer cohorts" based on performance quality measures and participation in "clinical improvement activities". Or physicians can choose to be paid for some or all of their Medicare services under an Alternative Payment Model (APM). Under QUIP, physicians and others contribute to the development of quality measures and clinical practice improvement activitie. Performance based on risk-adjusted relative rankings and quality improvement.
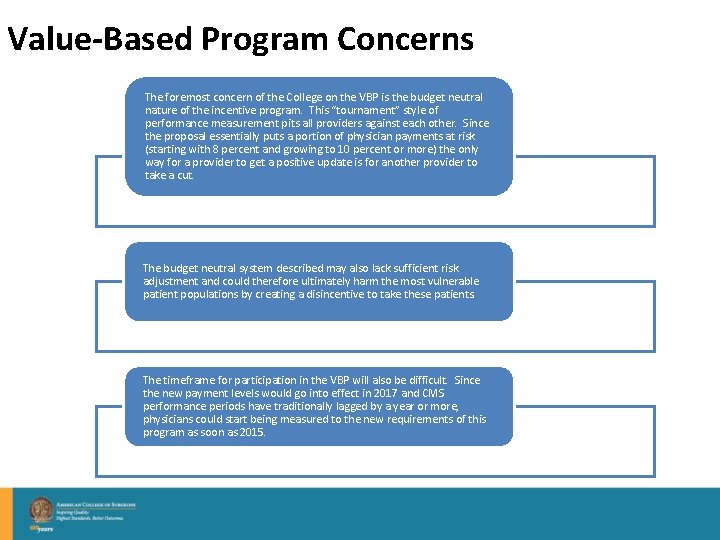
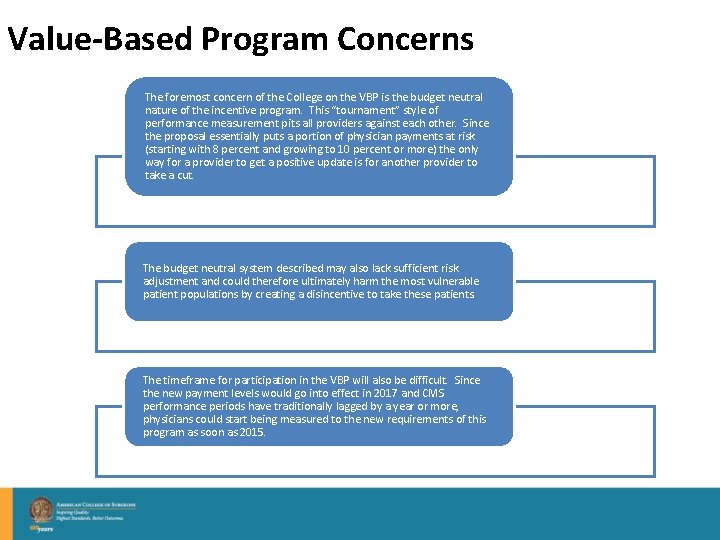
Value-Based Program Concerns The foremost concern of the College on the VBP is the budget neutral nature of the incentive program. This “tournament” style of performance measurement pits all providers against each other. Since the proposal essentially puts a portion of physician payments at risk (starting with 8 percent and growing to 10 percent or more) the only way for a provider to get a positive update is for another provider to take a cut. The budget neutral system described may also lack sufficient risk adjustment and could therefore ultimately harm the most vulnerable patient populations by creating a disincentive to take these patients. The timeframe for participation in the VBP will also be difficult. Since the new payment levels would go into effect in 2017 and CMS performance periods have traditionally lagged by a year or more, physicians could start being measured to the new requirements of this program as soon as 2015.
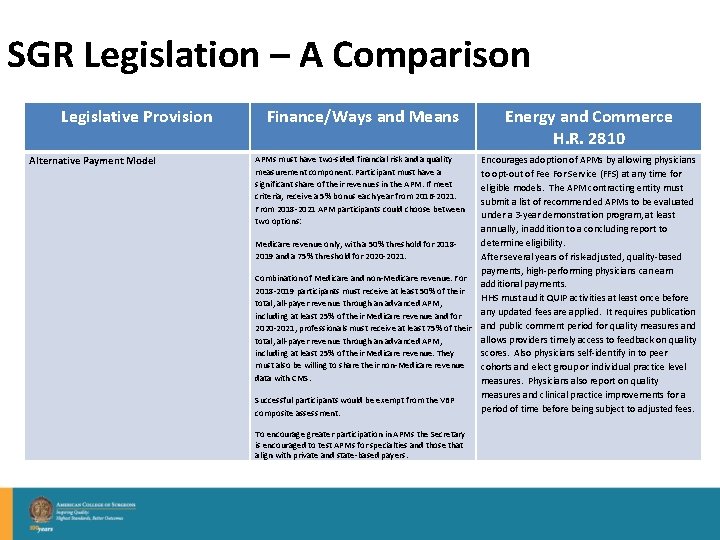
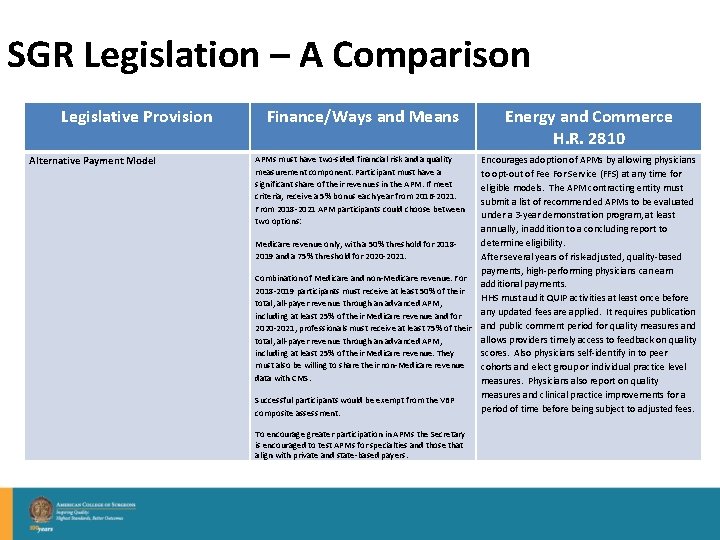
SGR Legislation – A Comparison Legislative Provision Alternative Payment Model Finance/Ways and Means APMs must have two-sided financial risk and a quality measurement component. Participant must have a significant share of their revenues in the APM. If meet criteria, receive a 5% bonus each year from 2016 -2021. From 2018 -2021 APM participants could choose between two options: Energy and Commerce H. R. 2810 Encourages adoption of APMs by allowing physicians to opt-out of Fee For Service (FFS) at any time for eligible models. The APM contracting entity must submit a list of recommended APMs to be evaluated under a 3 -year demonstration program, at least annually, in addition to a concluding report to determine eligibility. Medicare revenue only, with a 50% threshold for 20182019 and a 75% threshold for 2020 -2021. After several years of risk-adjusted, quality-based payments, high-performing physicians can earn Combination of Medicare and non-Medicare revenue. For additional payments. 2018 -2019 participants must receive at least 50% of their HHS must audit QUIP activities at least once before total, all-payer revenue through an advanced APM, any updated fees are applied. It requires publication including at least 25% of their Medicare revenue and for 2020 -2021, professionals must receive at least 75% of their and public comment period for quality measures and allows providers timely access to feedback on quality total, all-payer revenue through an advanced APM, including at least 25% of their Medicare revenue. They scores. Also physicians self-identify in to peer must also be willing to share their non-Medicare revenue cohorts and elect group or individual practice level data with CMS. measures. Physicians also report on quality measures and clinical practice improvements for a Successful participants would be exempt from the VBP period of time before being subject to adjusted fees. composite assessment. To encourage greater participation in APMs the Secretary is encouraged to test APMs for specialties and those that align with private and state-based payers.

Alternative Payment Model Concerns The proposal identifies ACOs, Medical Homes and bundled payments as APMs. Outside of a limited bundled payment (which requires hospital involvement), surgeons are unable to create an APM without an outside entity, while a primary care physician can unilaterally create a “medical home, ” thereby avoiding the VBP program and penalties. In addition, basing APM participation on percentage of revenue – perhaps percentage of patients is better – would make it more difficult to qualify. The overall targets are also extremely ambitious and would be virtually impossible in most parts of the country. Surgeons may not know their revenue breakdown throughout the year – what happens if a surgeon believes they are in an APM, thus exempt from VBP (and its penalties), but misses the revenue calculation? Do they automatically revert into the VBP without having prepared for that fact? Do they just give up their 5% bonus?

SGR Legislation – A Comparison Legislative Provision Valuation of Services Finance/Ways and Means Energy and Commerce H. R. 2810 Sets a target for identifying and revaluing codes. GAO would study the RUC processes. In 2016, 2017, and 2018 the target for identifying misvalued services is 1% of estimated expenditures. The amount would be redistributed in a budget-neutral manner within the physician fee schedule. If the target is not met, fee schedule payments would be reduced by the amount of misvalued services identified for that year. “Jury Duty” valuation: The Secretary is allowed to solicit information from a scope of professionals to determine accurate valuation. Professionals may be compensated for this information and those unwilling for submit information will receive a 10% penalty payment reduction. Practices will not be solicited 2 years in a row. If the downward value for any unit is greater than or equal to 20%, it would be phased in over a two-year period. The bill would also adjust relative value units for certain physicians' services. Allows for up to a 1% net reduction in total payments in each of 2016, 2017 and 2018. (essentially eliminates budget neutrality to allow for an up to 3% cumulative reduction to total physician payments) Creates a new reporting cohort to be named no later than January 1, 2015 to report on service volume and time. The group shall include physicians across settings representing a range of specialties and patient populations. Provides $1 million per year starting in 2014 for payments to physicians reporting data.
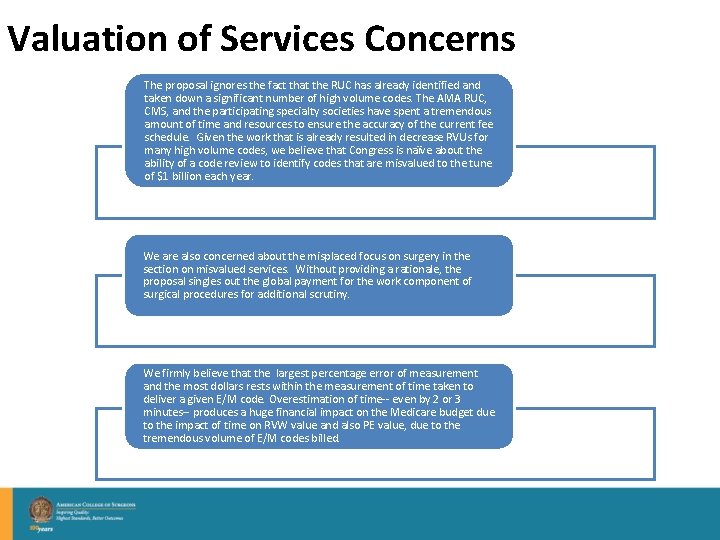
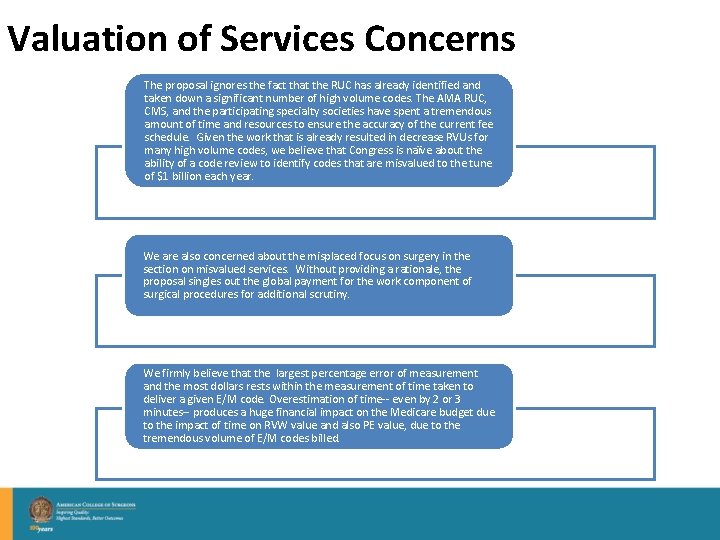
Valuation of Services Concerns The proposal ignores the fact that the RUC has already identified and taken down a significant number of high volume codes. The AMA RUC, CMS, and the participating specialty societies have spent a tremendous amount of time and resources to ensure the accuracy of the current fee schedule. Given the work that is already resulted in decrease RVUs for many high volume codes, we believe that Congress is naïve about the ability of a code review to identify codes that are misvalued to the tune of $1 billion each year. We are also concerned about the misplaced focus on surgery in the section on misvalued services. Without providing a rationale, the proposal singles out the global payment for the work component of surgical procedures for additional scrutiny. We firmly believe that the largest percentage error of measurement and the most dollars rests within the measurement of time taken to deliver a given E/M code. Overestimation of time-- even by 2 or 3 minutes-- produces a huge financial impact on the Medicare budget due to the impact of time on RVW value and also PE value, due to the tremendous volume of E/M codes billed.

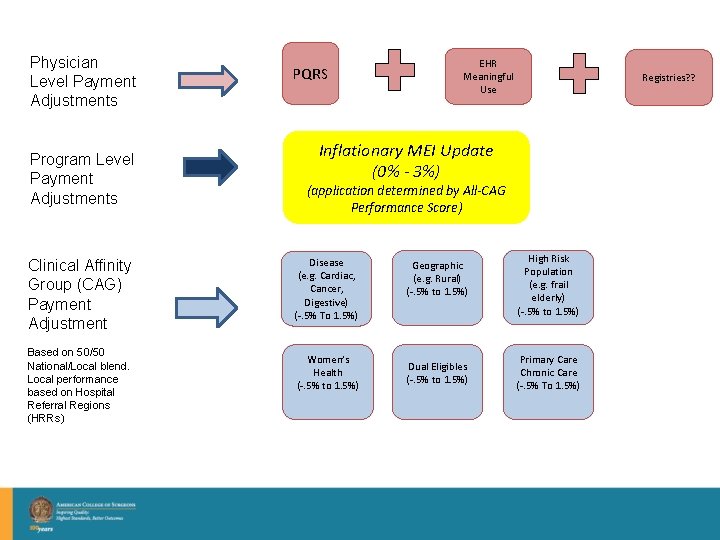
ACS Proposed Solution The Value Based Update (VBU) • • • The fusion of ACS’s 100 years of quality experience and physician payment system Improved, high quality care, shared savings, and resultant cost reduction The Clinical Affinity Group (CAG) • Breaking down physician silos of care • A group of physicians and providers who care for a specific condition, disease or patient population. • CAGs are the core of this proposal, and might include categories such as cancer care, surgery, cardiac care, frail elderly/end of life, digestive diseases, women’s health, rural and primary care/chronic care. • designed to account for regional variations in the provision of care • patient-oriented, outcomes-based, risk-adjusted quality measures designed to foster continuous improvement and help lower costs.
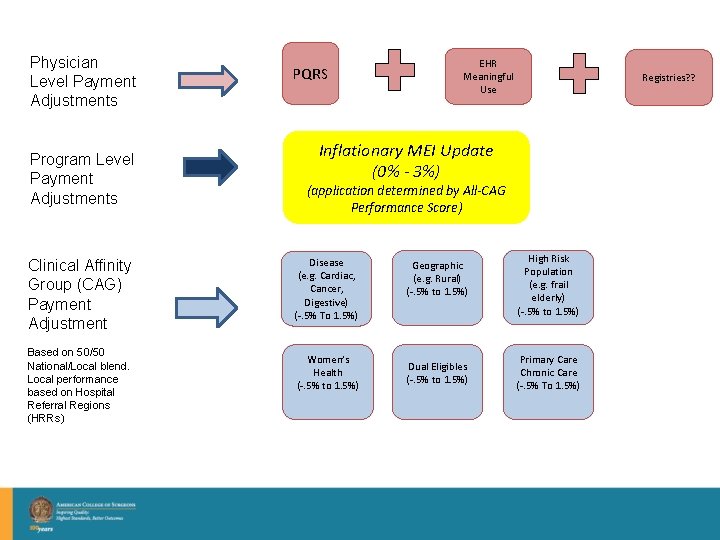
Physician Level Payment Adjustments Program Level Payment Adjustments Clinical Affinity Group (CAG) Payment Adjustment Based on 50/50 National/Local blend. Local performance based on Hospital Referral Regions (HRRs) PQRS EHR Meaningful Use Registries? ? Inflationary MEI Update (0% - 3%) (application determined by All-CAG Performance Score) Disease (e. g. Cardiac, Cancer, Digestive) (-. 5% To 1. 5%) Women’s Health (-. 5% to 1. 5%) Geographic (e. g. Rural) (-. 5% to 1. 5%) Dual Eligibles (-. 5% to 1. 5%) High Risk Population (e. g. frail elderly) (-. 5% to 1. 5%) Primary Care Chronic Care (-. 5% To 1. 5%)

The VBU Further Development • Contracted with group from Brigham & Women’s Hospital and Brandeis University to further evaluate, develop CAG models, and score the VBU concept • • CAG Target Domains • • • Prevention, Quality, Safety, Patient experience, Resource Use/Cost Not all need to be accounted for in a CAG Example - Cardiovascular CAG • • Focus Groups with wide range of individual physicians Diabetes Control, PCI/CABG Outcomes, Adverse drug events, H-CAHPS/S-CAHPS, ECHO appropriateness Example – Prevention/Chronic Care CAG • Cancer Screening/Immunization, CHF Post-discharge care coordination, Drug reconciliation measures, C&G-CAHPS, Care coordination
The VBU Complicated Issues • Accounting for all specialties and primary care • Value-Based Modifier – Should it fit? Where does it fit? • Voluntary Participation? – Designed so that penalties for non-VBU compliant physicians bear greater risk • HOWEVER, an initial report found that between 2014 -2018: – Physician payments (incentive-based) increased $6. 4 billion – Indirect reduction to Parts A and B totaled $15. 77 billion – Net reduction of $9. 355 billion in Parts A and B

ACSPA-Surgeons. Voice Cutting Edge Advocacy An on-going, organized program of recruiting, educating, and motivating members to use their political power to advocate and influence.

Program Components Ø Health Policy Advisory Council –Grassroots Committee l Region Chiefs and State Councilors Ø Surgeons. Voice Online Platform Ø Surgeons. Voice DOCS Program (District Office Contacts by Surgeons) Ø Surgeons. Voice Practice Tours Ø Surgeons. Voice at Advocacy Summit Ø Surgeons. Voice Recognition Program
Surgeons. Voice: Cutting Edge Advocacy Ø Purpose: United surgical voice influencing health policy Ø Goals: Educate, Advocate, Motivate Ø Participants: Leadership, Fellows, Residents • Committees and Councils of the ACS Ø Benefits: Broad-based, diversified, lifelong advocates
Health Policy Advisory Councilors • One Councilor from each chapter • Responsible for fostering an extensive grassroots advocacy network throughout their chapter • Advocacy experts who promote grassroots and political advocacy among their peers • Communicate feedback from surgeons on the ground on legislative and regulatory policy and implementation, back to the Division of Advocacy and Health Policy.
DOCS Program District Office Contacts by Surgeons • Routinely meet with Representative and Senators in state district offices during House and Senate recesses (“in-district work periods”) • Advocate on issues critical to surgery • Foster lasting relationships between participating surgeons and members of Congress • Become knowledgeable and trusted resources on healthcare policy for elected officials

Platform and Program Tools www. surgeonsvoice. org
Advocacy Toolkit One Stop Shopping
Additional Resources Take Action: Contact your Elected Officials • Share Your Story • Key Contact Survey • Interactive Map • Events Calendar • And More… •
Recap: How Can You Get Involved? Ø Visit and use www. Surgeons. Pac. org Ø Visit and use www. Surgeons. Voice. org Ø Become an Advocacy Councilor Ø Join the DOCS Program Ø Save the date: ACS Advocacy Summit– March 30 -April 1, 2014 Ø Respond to Grassroots Action Alerts Ø Host a fundraiser, facility tour, or PAC check delivery for your Congressmen. Ø Get your colleagues involved!!
Thank You all deserve a drink
We in America do not have government by the maj We have government by the majority who participa - Thomas Jefferson Thank you John E. Hedstrom, JD jhedstrom@facs. org 202 -672 -1503
 Partners in advocacy
Partners in advocacy Udel summer fellows
Udel summer fellows Unc hematology oncology fellows
Unc hematology oncology fellows Secretary of defense executive fellows program
Secretary of defense executive fellows program Wharton leadership ventures
Wharton leadership ventures Terry betts
Terry betts Mickey leland international hunger fellows program
Mickey leland international hunger fellows program Uri coastal fellows
Uri coastal fellows Quantitative research objectives examples
Quantitative research objectives examples Advocacy goals and objectives examples
Advocacy goals and objectives examples Advocacy communication and social mobilization
Advocacy communication and social mobilization Advocacy process 8 steps
Advocacy process 8 steps Packaging and delivery of information in advocacy
Packaging and delivery of information in advocacy Lsu jonathan sanders
Lsu jonathan sanders Kanbar center
Kanbar center What is the importance of advocacy in a community
What is the importance of advocacy in a community Self-determination worksheets pdf
Self-determination worksheets pdf Advocacy about self confidence
Advocacy about self confidence Positive advocacy
Positive advocacy Iowa child advocacy match
Iowa child advocacy match Advocacy inquiry model
Advocacy inquiry model Lobby vs advocacy
Lobby vs advocacy Ecumenical advocacy alliance
Ecumenical advocacy alliance Subordinate advocacy
Subordinate advocacy Bug advocacy
Bug advocacy What is advocacy
What is advocacy Advocacy about unemployment
Advocacy about unemployment Sucesos de las islas filipinas annotated by jose rizal
Sucesos de las islas filipinas annotated by jose rizal Advocacy advertising
Advocacy advertising Courageous advocacy powerpoint
Courageous advocacy powerpoint Components of advocacy
Components of advocacy Jennifer masi
Jennifer masi Child advocacy definition
Child advocacy definition Advocacy pronounciation
Advocacy pronounciation Tearfund roots resources
Tearfund roots resources What is advocacy cycle
What is advocacy cycle