Positive Prevention Gus Cairns UKC UK Coalition of








![HIV+ people do use condoms… l In SUMIT study* [see more below] 83% of HIV+ people do use condoms… l In SUMIT study* [see more below] 83% of](https://slidetodoc.com/presentation_image/2428641cf6da54d8b65da857cb5e2003/image-28.jpg)


![RCTs of disclosure interventions… l [NONE] RCTs of disclosure interventions… l [NONE]](https://slidetodoc.com/presentation_image/2428641cf6da54d8b65da857cb5e2003/image-34.jpg)







- Slides: 59
Positive Prevention Gus Cairns UKC UK Coalition of People Living with HIV and AIDS
What is it? l l Work with/for people living with HIV and AIDS (PLHAs) to prevent the onward transmission of HIV Gets called both ‘primary’ and ‘secondary’ prevention according to tradition
Positive prevention makes sense l On an economic and efficiency level l On a legal level l On a human rights level
Positive prevention makes sense “Preventive interventions with positive individuals are likely to have a greater impact on the epidemic, for an equivalent input of cost, time, resources, than preventative interventions focused on negative individuals. “A change in the risky behaviour of an HIV positive person will, on average, and in almost all affected populations, have a much bigger impact on the spread of the virus than an equivalent change in the behaviour of an HIV negative person. ” King-Spooner S. HIV prevention and the positive population. Int J STD AIDS 10(3): 141 -50. 1999.
Why not part of prevention from the start? “Historically, there has been a reluctance to work on HIV/STI prevention with people with HIV because of perceptions that the concept of prevention for people already infected is inherently contradictory. “There have also been justifiable concerns about victimising an already stigmatised group. In addition, there has been a reluctance to acknowledge that people with HIV have sex, and also to get to grips with the complex ethical issues surrounding people with HIV’s responsibilities towards others. ” International HIV/AIDS Alliance. Positive Prevention: Prevention Strategies for People with HIV/AIDS. Draft Background Paper available at http: //www. aidsalliance. org/sw 9438. asp. July 2003.

What might it involve? (International HIV/AIDS Alliance paper, 2003)
Summary l l l l Voluntary Testing…and counselling? Post-test counselling Condom provision Behavioural skills interventions Help with disclosure Prevention of MTCT Peer and community support Family support and disclosure ARV provision Harm reduction for IDUs Other biomedical interventions (‘New’ prevention technologies) Reducing stigma Legislative reform Empowerment of women Improving the legal and social position of MSM Economic development
Discussed here l l l Normalising universal testing What do PLHAs already do to reduce transmission? Counselling and condom provision Serosorting Other risk-reduction strategies Disclosure What works? Mass-media programmes ARV and STI treatment provision ‘New’ prevention technologies Criminalisation and its impact

Test, test… l CDC in USA calculates that when diagnosed, PLHAs cut risk behaviour by 2/3 l l Universal testing drive: recommended testing all 13 -65 year olds: Washington DC recently extended this to 85 Then what? CDC prevention interventions mention: l l ongoing case management focused risk-reduction counselling medical interventions (leaving these undefined) support for other psychosocial stressors (leaving these also undefined)
Are CDC’s assumptions justified? l l l Meta-analysis of 11 US studies 53% reduction in unprotected sex post -diagnosis 78% reduction in unsafe (i. e. unprotected and serodiscordant) sex after diagnosis
Are CDC’s assumptions justified? l l Typical study: 113 recently HIV-infected gay men. Interviewed 3 months and six weeks after diagnosis. 47% reported decline in sexual partners at second interview, 34% the same, 19. 5% an increase. Overall decline; 34% Unprotected sex did not decline but unprotected sex with negative partners declined 37. 5% and with partners of unknown status 47%. Limitations: small numbers, no long-term followup Gorbach PM et al. Transmission behaviors of recently HIV-infected men who have sex with men. JAIDS 42(1), 80 -85. 2006.

Are CDC’s assumptions justified? l l l l Longitudinal study in HIV- negative female ‘sex workers’, Mombasa, 1993 -2000 Ave follow-up > five years, 3. 8 post-diagnosis N= 1600: 265 seroconversions = 7. 7% p. a. 44% reduction in unsafe sex incidents after seroconversion – maintained through time – but after adjusting for age OR= 0. 69 100% condom use up from 59% to 67% More than one sexual partner in previous week declined from 20% to 9% More than two sexual encounters in previous week declined from 27% to 16% Mc. Clelland RS et al. HIV-1 acquisition and disease progression are associated with decreased high-risk sexual behaviour among Kenyan female sex workers. AIDS 20(15): 1969 -1973. 2006.

How much behaviour change do you need to reduce prevalence? * l l l When R(t) >1, epidemics will increase. R(t) = c. annual incidence/prevalence ratio (IPR(t)) IPR must be < 1/ survival time for prevalence to decline. If mean survival with HIV is 20 years, IRP has to be <0. 05. Denmark study†: Survival time with HIV if diagnosed at 25 = 18 years men, 24 years women IPR in gay men in UK is c. 0. 11 and slowly increasing. ∴ May need 50 -66% further reduction in transmission events to contain epidemic. * White PJ et al. Is HIV out of control in Britain? An example of analysing patterns of HIV spreading using incidence-to-prevalence ratios. AIDS 20(14), 1898 -1901. 2006. † Lohse N et al. Median survival and age-specific mortality of Danish HIV-infected individuals: a comparison with the general population. 16 th International AIDS Conference, Toronto, 2006. Abstract MOPE 0310.
The incidence problem l l l Baltimore African-American gay men: 48% positive* Two-thirds unaware 87% of these had tested: 60% in the previous year HIV incidence age 15 -22 4%, age 23 -29 15% London gay men†: 11% HIV+, of which 1/3 undiagnosed and 1/5 had previous negative test * MMWR, HIV incidence among young MSM – 7 US Cities, 1994 -2000, June 01, 2001 † Dodds JP et al. Increasing risk behaviour and high levels of undiagnosed HIV infection in a community sample of homosexual men. Sex. Transm. Inf. 2004; 80; 236 -240

Test, test…concs. l l CDC estimate: diagnosis ≥ 66% reduction in unsafe sex. May be an overestoimate. ‘Universal’ testing = probably cost- effective where general prevalence <0. 2%. l Opt-out testing at GUM clinics essential. l GP and A&E staff awareness-raising l l Need for ethical safeguards so that voluntary testing remains voluntary Home testing? Reliability questions
Positive prevention and positive-led prevention l l l Easier to reinforce a positive behaviour than change a negative one Information alone is not enough. People need information, motivation and behavioural skills Programmes should be tailored to help people sustain behaviour that supports good sexual health and relationships, and to address barriers to adopting them.
What do PLHAs already do? l Pamina Gorbach: JAIDS 42(1): 80 -85. 2006 (again): deline in sexual risk behaviour in post-diagnosis gay men. l l l Ave. 34% decrease in partner numbers in previous 3 months (7. 9 to 5. 2) Half decreased partner numbers, a third stayed the same, a fifth increased numbers. Condom use increase? No. 59% had UAI at both timepoints: difference was with whom…
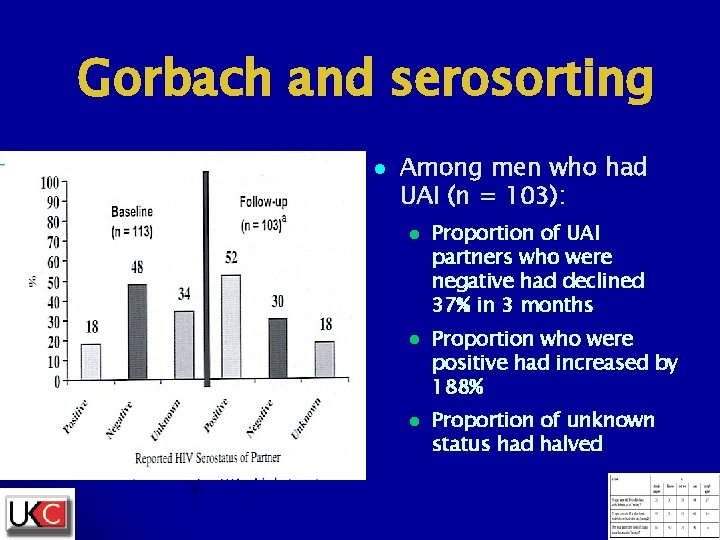
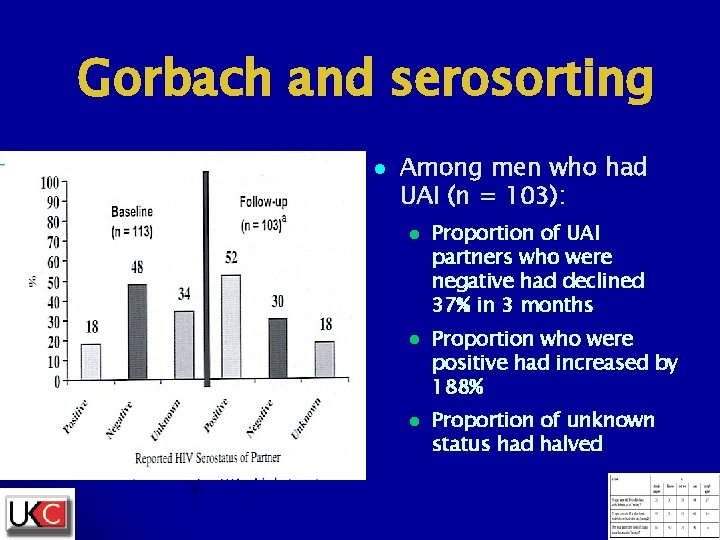
Gorbach and serosorting l Among men who had UAI (n = 103): l l l Proportion of UAI partners who were negative had declined 37% in 3 months Proportion who were positive had increased by 188% Proportion of unknown status had halved
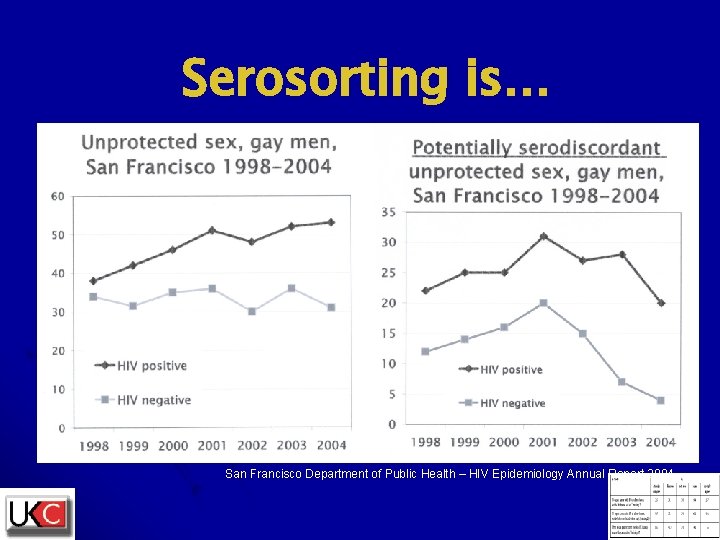
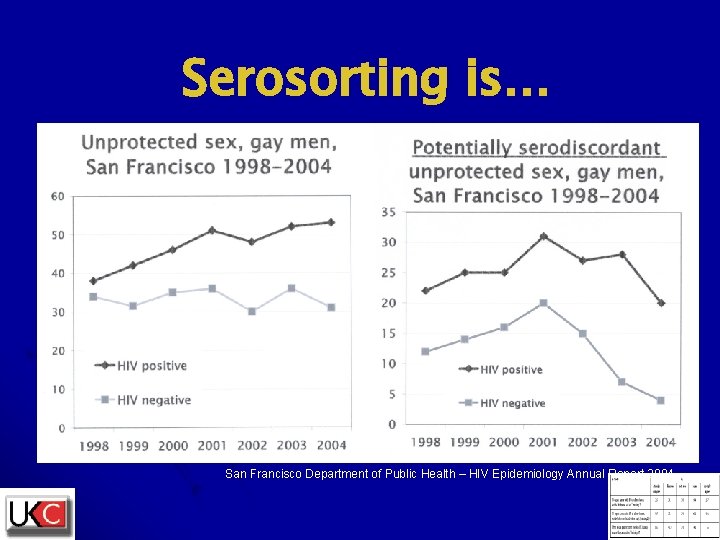
Serosorting is… San Francisco Department of Public Health – HIV Epidemiology Annual Report 2004
And in London… Elford J et al. High-risk sexual behaviour among London gay men: no longer increasing. AIDS 19(18) 2171 -2174. 2005.
…and in London (contd) l Elford 2006 (UK): 1, 687 people attending HIV clinics in NE London. Women and gay men 50% less likely to have unprotected sex if partner negative than if they were positive and heterosexual men 75% less likely.
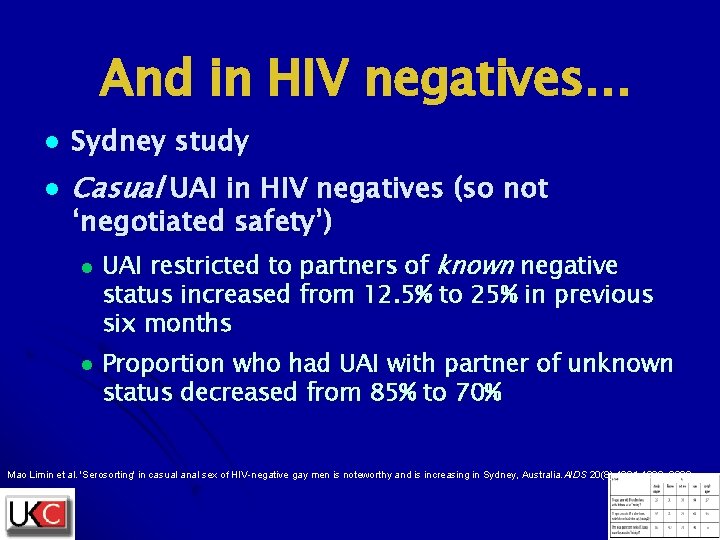
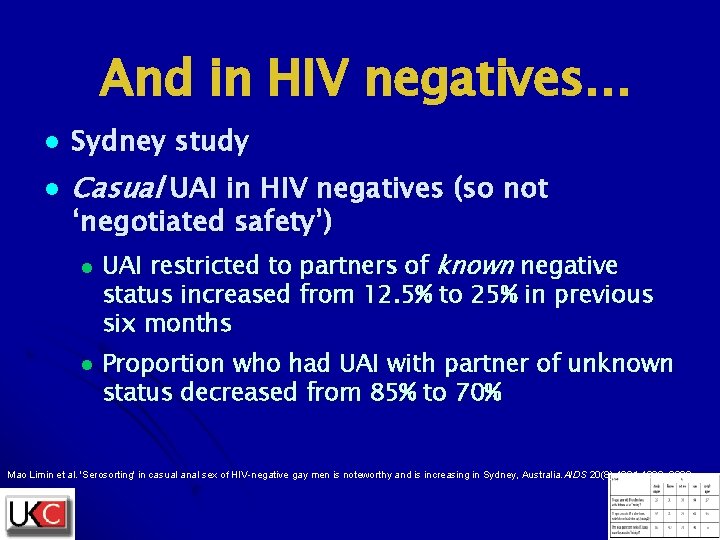
And in HIV negatives… l Sydney study l Casual UAI in HIV negatives (so not ‘negotiated safety’) l l UAI restricted to partners of known negative status increased from 12. 5% to 25% in previous six months Proportion who had UAI with partner of unknown status decreased from 85% to 70% Mao Limin et al. 'Serosorting' in casual anal sex of HIV-negative gay men is noteworthy and is increasing in Sydney, Australia. AIDS 20(8): 1204 -1206. 2006.

Does serosorting work? l Golden M. , CROI 2006 (abstract #163) l New diagnoses among: l ‘Always’ l No special precautions: 4. 1% l Tried to serosort: 2. 6% l Condom l condom users: 1. 5% use 76% effective Serosorting about 40% effective

Does serosorting work? (contd) l San Francisco gay men*, 1998 -2003: l l Rectal gonorrhoea (good marker for URAI) increased 97% during this time Syphilis from 8 cases 1998 to 314 cases 2003 HIV incidence peaked in 1999 at 4% - down or steady since then Increases in UAI but decreases in UAI between partners of unknown status during this time *Truong HM et al. HIV serosorting? Increases in sexually transmitted infections and risk behavior without concurrent increase in HIV incidence among men who have sex with men in San Francisco. Sixteenth International AIDS Conference, Toronto, abstract MOAC 0105, 2006.

Should we promote serosorting? l ‘Knowledge’ of another person’s HIV status may in fact be guesswork* *Hickson F et al. London Counts: HIV prevention needs and interventions among gay and bisexual men in the sixteen London Health Authorities. Sigma Research, 2001. ISBN 0 872956 51 3
Should we promote serosorting? l Serosorting does not prevent other Sexually Transmitted Infections† Herida M et al. Rectal lymphogranuloma venereum surveillance in France 2004 -2005. Eurosurveillance Monthly, vol 11 Issue 9, September 2006.
Should we promote serosorting? l l Serosorting is elective unprotected sex. Ethical problem about promotion. But serosorting requires two conditions to work…. l Knowledge l Disclosure l of status …and we should promote those!
![HIV people do use condoms l In SUMIT study see more below 83 of HIV+ people do use condoms… l In SUMIT study* [see more below] 83% of](https://slidetodoc.com/presentation_image/2428641cf6da54d8b65da857cb5e2003/image-28.jpg)
HIV+ people do use condoms… l In SUMIT study* [see more below] 83% of HIV+ gay men used condoms with HIV- or unknown status partners – but inconsistently *Wolitski RJ et al. Effects of a peer-led behavioral intervention to reduce HIV transmission and promote serostatus disclosure among HIV-seropositive gay and bisexual men. AIDS 19(Suppl 1): S 99109. 2005.
Condoms and counselling in a high-risk group can make a dramatic difference… l l Ghana Pr. EP study, high risk women* One-third as many infections in women on tenofovir as on placebo Not statistically significant (p=0. 24), partly because incidence half of what was anticipated Condom use at last sex was 52% at screening and 94% at follow-up = 87. 5% decrease in unprotected sex Peterson L. et al. Findings from a double-blind, randomized, placebo-controlled trial of tenofovir disoproxil fumarate (TDF) for prevention of HIV infection in women. Sixteenth International AIDS Conference, Toronto. Abstract Th. Lb 0103, 2006.

…and in HIV-positive people l l Rotherham-Borus, 2003* HIV+ youth, 13 -24, 37/36/27 Latino/White/Black Randomised to ‘Act Safe’ 23 -session intervention or control Intervention 82% fewer unprotected sexual acts, 45% fewer sexual partners, 50% fewer HIV-negative sexual partners, 31% less substance use *Rotherham-Borus MJ et al. Efficacy of a preventive intervention for youths living with HIV. Am J Public Health. 2001 March; 91(3): 400– 405.
…and via brief interventions l l l Richardson, 2004* Eligible HIV+ patients at six California HIV clinics randomised to control or 3 -5 minute ‘gain framed’ or ‘loss-framed’ [see below] counselling intervention 38% reduction in unprotected sex in recipients of ‘loss-framed’ counselling who had >1 sex partner *Richardson J et al. Effect of brief safer-sex counseling by medical providers to HIV-1 seropositive patients: a multi-clinic assessment. AIDS 18(8) 1179 -1186. 2004.
Disclose, disclose… l Point A: l l l Only 20% of HIV+ gay men disclose before sex, 40% never do, 40% sometimes Point B: l l l Unpublished GMFA survey, basis of ‘Why won’t he tell? ’ campaign: Bruno Spire, France*: 97% of HIV+ people in a steady relationship eventually disclose and of the other 3%, 2% use condoms We have to help PLHAs get from point A to point B as fast as possible *Spire B et al. Concealment of HIV and unsafe sex with steady partner is extremely infrequent. 3 rd IAS Conference on HIV Pathogenesis and Treatment, Rio. Abstract Mo. Pe. LB 10. 7 P 01. 2005.

Toronto disclosure posters l l Uganda (King): 1, 092 HIV-positive. 69% had disclosed HIV status to partner. Higher rates of disclosure ⇔ higher rates of condom use. South Africa (Simbayi): > 1, 000 HIV+ people: 58% disclosed HIV status to partner: disclosure ⇔ less unprotected sex. France (Spire): 1, 187 HIV+ people: 95% of men and 91% of women had disclosed to partner: non-disclosure ⇔ unprotected sex in gay men but in heterosexuals with poverty Botswana (Percy-de Korte) 90% of 275 ARV recipients disclosed HIV status to family, 71% to partner. 48% had reduced number of sexual partners since diagnosis. But 39% said that receiving ARVs had resulted in either reduced condom use or more partners.
![RCTs of disclosure interventions l NONE RCTs of disclosure interventions… l [NONE]](https://slidetodoc.com/presentation_image/2428641cf6da54d8b65da857cb5e2003/image-34.jpg)
RCTs of disclosure interventions… l [NONE]
Other strategies l ‘Strategic positioning’ = HIV+ on bottom l Insertive free sex 10 x less risky but not risk- l Withdrawal – see next slide l Viral load –see slide after next
Withdrawal l l Campaigns based on assumption that withdrawal before ejaculation is less risky Widely practised but as contraception and STD prevention method anyway

Withdrawal and strategic positioning… l l l Poster at Toronto questions these assumptions* Case-control study of Ontario gay men, 128 HIV+, 255 HIVAdjusted Odds Ratios for seroconversion: l l l Unprotected insertive anal sex (UIAS) with HIV+: 3. 05 Unprotected receptive anal sex (URAS) with HIV+: 3. 02 URAS with exposure to semen: 1. 72 URAS without exposure to semen, i. e. withdrawal: 2. 70 URAS with delayed application of condom: 4. 25 Another study from Australia† found that UIAS without ejaculation was more risky than with ejaculation *Burchell AN et al. Sexual Risk Factors Leading to Recent HIV Infection among Gay and Bisexual Men in Ontario, Canada. Sixteenth International AIDS Conference, Toronto. Abstract no MOPE 0378. † Read T et al. Risk factors for incident HIV infection amongst homosexually active men in Melbourne, Australia: a case-control study. Sixteenth International AIDS Conference, Toronto. Abstract no CDC 0067.
Viral load l l l 78% of 507 gay men in SF* knew term `viral load` and 1/3 had discussed it with a serodiscordant partner to make decisions about sexual practices. 119 men in Sydney† in HIV-serodiscordant regular relationship used VL to help decisions on condom use. 39. 4% had UAI when partner’s HIV last VL test was undetectable, 20. 8% when it was detectable Problem is that 12. 5% of gay men at any one time have detectable HIV VL in semen when it is not detectable in plasma‡ *Goldhammer H et al. Beliefs about viral load, sexual positioning and transmission risk among HIV+ men who have sex with men (MSM): Shaping a secondary prevention intervention. 2005 National HIV Prevention Conference, Atlanta, USA, presentation W 0 -D 1201. †Van de Ven P et al. Undetectable viral load is associated with sexual risk taking in HIV serodiscordant gay couples in Sydney. AIDS 19(2): 179 -184. 2005. ‡Taylor S et al. Seminal Super Shedding of HIV: implications for Sexual Transmission. 10 th CROI, Boston, 2003. Abstract 454.
So what works in behavioural interventions? (Two meta-analyses, 2006) l Nicole Crepaz, AIDS 20: 143– 157. 2006. l l l Measured ‘sexual risk incidents’ after 12 RCT interventions Significant reduction (43%) What worked: l l l Interventions specifically focused on safer sex… Which also included help with disclosure, self-esteem etc Were intensive Were delivered in a clinical setting or at a voluntary organisation providing services At least partly delivered by professional counsellors At least partly delivered on a one-to-one basis
What works II l l Blair Johnson, JAIDS 41(5): 642 -650. 2006. 19 RCT interventions Ave 16% increase in condom use Worked better for: l l Younger ‘Motivational*’ or taught behavioural skills (12% condom use increase) or both (33%) Non-gay; but no programme directed at gay men provided both ingredients proven to be necessary Information alone made no difference but helped other components * Motivational = providing things that improved participants’ overall quality of life such as increased social support or self-confidence.
Quote from Johnson l “Perhaps the most surprising finding of this work is that more than two decades into the epidemic, there have been so few randomlycontrolled trials of interventions that focus in people living with HIV, though there have been literally hundreds of studies conducted with uninfected populations. There is an urgent need for research in this area. ”
Compare prevention for HIVl l Largest meta-analysis is Albarracin (2005). Covered 345 intervention groups and 99 control groups. Only outcome measure = condom use What worked best: l l l ‘Active’ interventions increased condom use by 30%, ‘passive’ ones by 5% Taught behavioural skills Used cognitive work to improve attitudes towards condom use At least partly delivered in clinical settings Arguments that used threat or fear [‘loss framed’] consistently failed to work

Loss-framed and gainframed messages l l From Richardson, 2004 Gain-framed: l l Loss-framed: l l l “We encourage you to make choices that do not put yourself or others at risk. Safer sex protects you from other STDs and other strains of HIV” “We encourage you to make choices that do not put yourself or others at risk. Unsafe sex exposes you to other STDs and strains of HIV” Loss-framed messages do not work with HIV negative people. Gain framed messages do not work with HIV positive people. Why? Control. People respond to messages implying that they are capable of making a change that will have a directly protective effect on their health.
BEWARE: what seems to work may not! l SUMIT study, SF and NY, USA* l l l 811 HIV+ gay men randomised to one discussion session or six 3 -hour workshops. Videos, discussion groups, roleplay, freebies They loved it! Very high scores for enjoyment, learning, life changes, new friends Made no difference to behaviour at all. Unprotected sex marginally but non-significantly improved; disclosure got marginally worse *Wolitski RJ et al. Effects of a peer-led behavioral intervention to reduce HIV transmission and promote serostatus disclosure among HIV-seropositive gay and bisexual men. AIDS 19(Suppl 1): S 99 -109. 2005.
What seems to work may not. Why? l l l l Used community rather than clinical setting: health not emphasised Emphasis on protecting partners rather than own health. Selfinterest works better than guilt. Gain-framed messages (‘you’ll protect others’) rather than lossframed ones (‘you’ll mess up if you don’t’). Evidence* that lossframed messages work better with HIV+ people. Peer group structure can be counterproductive. The cautious end up modelling the risk-takers! Improved confidence can mean improved ability to find sex! Too many choices? Maybe one method (condom use, disclosure, serosorting) should be taught at a time. Worked better in SF than NY. Pre-existing community structure and norms matter. *Richardson J. Prevention in HIV Clinical Settings. 13 th Conference on Retroviruses and Opportunistic Infections, Denver, Abstract 165. 2006.

What works? Conclusion l l l l Based on behavioural theory At least partly conducted by skilled professionals Clinical or service-providing setting One-to-one or group, but not ‘peer group’ ‘Loss framed’, emphasising adverse consequences of unsafe sex to health and relationships Specifically addresses safer-sex skills but also… …Addresses what Johnson calls ‘myriad of other issues relating to HIV’ eg mental health, disclosure, stigma, employability, poverty, isolation etc.

What about the 88%? l According to CDC only 12% of HIV positive people have ever attended an in-person HIV prevention intervention
Do mass interventions work for PLHAs? l l l Not if they portray PLHAs as the danger… Not if they address them in the third person… Where would you put them anyway? Targetaudience publications are read by HIV- and HIV+, who need different messages
Internet interventions (www. hivstopswithme. org, US)
Internet interventions (www. DIPEx. org, UK)

Evaluation of Internet interventions l l 54% were more likely to use condoms with HIVnegative or unknown status partners as a result of viewing www. hivstopswithme. org 43% said they were more likely to disclose HIV status before sex. No RCT trial done of intervention: it’s all about the effect people believe the campaign will have on them DIPEx HIV section will be evaluated in an RCT, using it as an ‘add-on’ to standard post-test counselling in newly diagnosed and in high-risk repeat –STItesters
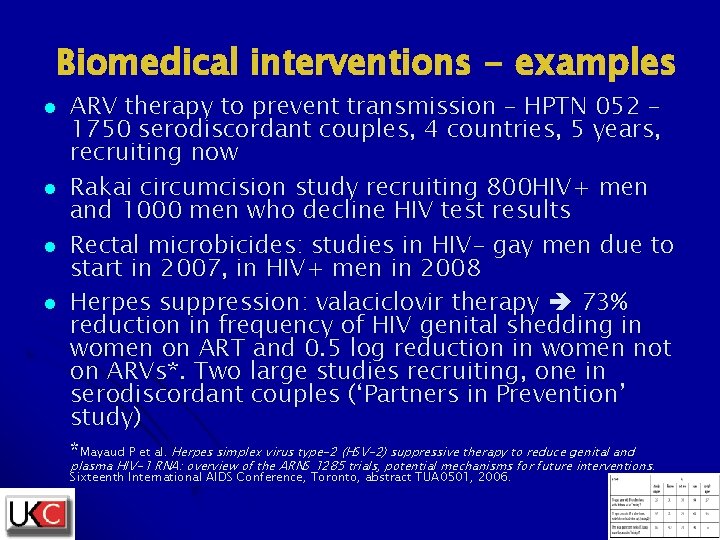
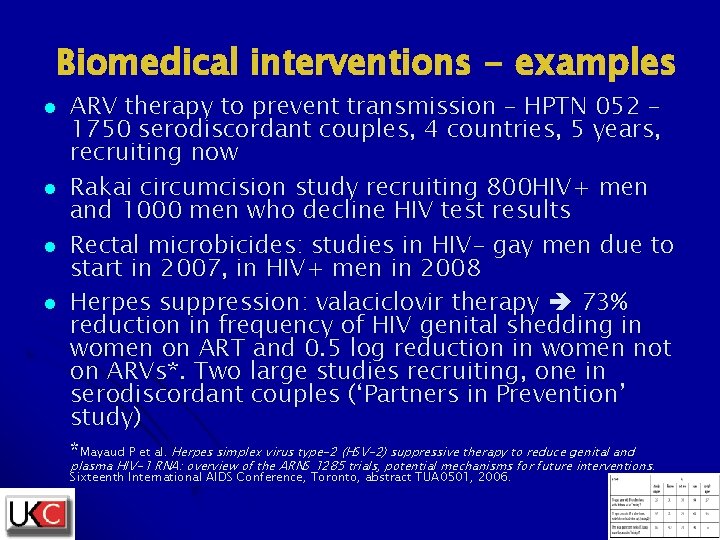
Biomedical interventions - examples l l ARV therapy to prevent transmission – HPTN 052 – 1750 serodiscordant couples, 4 countries, 5 years, recruiting now Rakai circumcision study recruiting 800 HIV+ men and 1000 men who decline HIV test results Rectal microbicides: studies in HIV- gay men due to start in 2007, in HIV+ men in 2008 Herpes suppression: valaciclovir therapy 73% reduction in frequency of HIV genital shedding in women on ART and 0. 5 log reduction in women not on ARVs*. Two large studies recruiting, one in serodiscordant couples (‘Partners in Prevention’ study) *Mayaud P et al. Herpes simplex virus type-2 (HSV-2) suppressive therapy to reduce genital and plasma HIV-1 RNA: overview of the ARNS 1285 trials, potential mechanisms for future interventions. Sixteenth International AIDS Conference, Toronto, abstract TUA 0501, 2006.
Someone who didn’t get enough prevention help
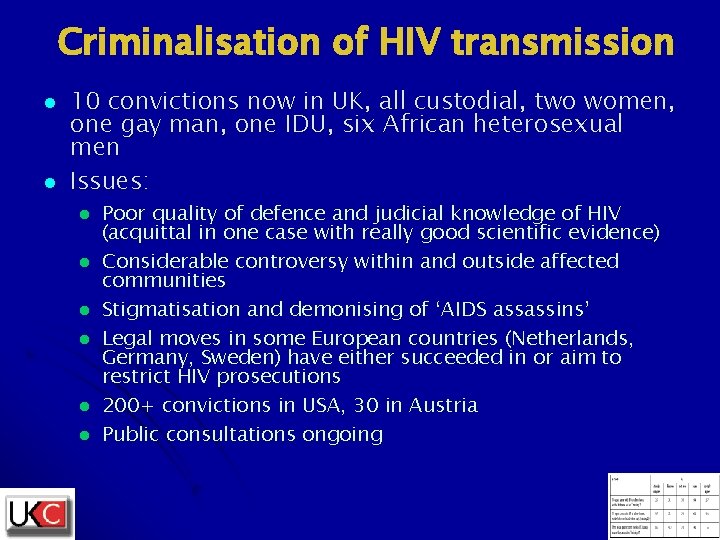
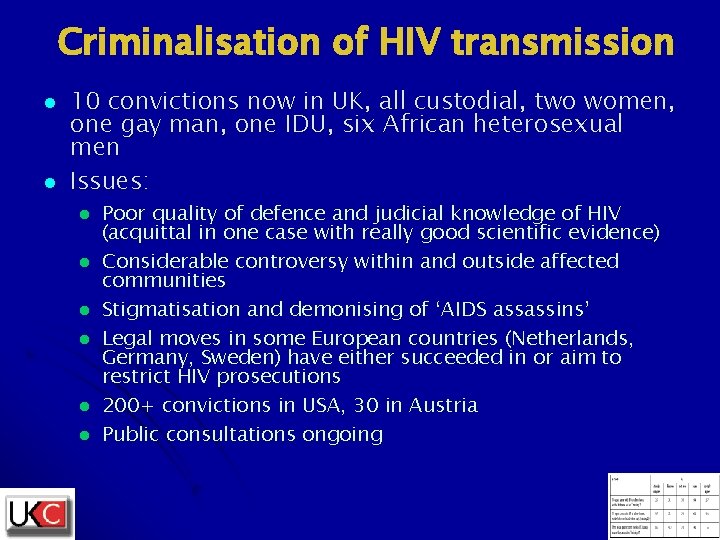
Criminalisation of HIV transmission l l 10 convictions now in UK, all custodial, two women, one gay man, one IDU, six African heterosexual men Issues: l l l Poor quality of defence and judicial knowledge of HIV (acquittal in one case with really good scientific evidence) Considerable controversy within and outside affected communities Stigmatisation and demonising of ‘AIDS assassins’ Legal moves in some European countries (Netherlands, Germany, Sweden) have either succeeded in or aim to restrict HIV prosecutions 200+ convictions in USA, 30 in Austria Public consultations ongoing

Criminalisation has changed the game l If PLHAs are going to continue to get jailed for transmitting HIV then: l l l We have a legal, social and moral responsibility to help PLHAs not transmit HIV Notions of ‘joint responsibility’ are less relevant: we are not jointly responsible for preventing HIV if the law says it’s the HIV+ partner who is And since prevention work directed at PLHAs is more efficient anyway, prevention funding must either increase or be redirected to work with PLHAs

Criminalisation activity l l l Two public consultations in UK, with Department of health and Crown prosecution Service EATG and WHO Technical Consultation on criminalisation, this Monday 16 th Community Satellite on HIV and the law at the 8 th Eighth International Congress on Drug Therapy in HIV Infection, Glasgow
This ought to be true. The law says it isn’t.
Questions l l Should we concentrate HIV prevention resources on PLHAs? What methods would work to increase the uptake of HIV testing? What kind of intervention do you think would work best to help PLHAs reduce risk of onward transmission? Given the limited reach and labour-intensive nature of counselling and support-group work, what ‘broadcast’ methods might work?
Thank you! l l l Keith Alcorn, Edwin J Bernard, Michael Carter, NAM Kim Mulji, Naz Foundation International Prof. Jonathan Elford, City University Yusef Azad, National AIDS Trust Nikos Dedes, EATG Jack Summerside, Stephen Bitti, Bernard Forbes, UKC Jim Pickett, AIDS Foundation Chicago Julie Davids, CHAMP Network Dr Mike Youle, Royal Free Hospital Dr Jane Anderson, Homerton hospital Dr Chris Wood, North Middlesex Hospital Elijah Amooti, ACIA and Thandi Haruperi, Restorego
 Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Ntranslate
Ntranslate Sastav mozga
Sastav mozga Global hiv prevention coalition
Global hiv prevention coalition Ciri-ciri gus dus
Ciri-ciri gus dus Gusano
Gusano Cairns legal aid
Cairns legal aid Ffa fun facts
Ffa fun facts Gus finance
Gus finance James lange vs cannon bard
James lange vs cannon bard Gregory cairns
Gregory cairns Gus lego masters
Gus lego masters Andy goldsworthy cairns
Andy goldsworthy cairns Dr alison vaughan
Dr alison vaughan Gus medina
Gus medina Quigley street night shelter
Quigley street night shelter John cairns 8 out of 10 cats
John cairns 8 out of 10 cats Gus giordano technique
Gus giordano technique How to make conceptual framework
How to make conceptual framework Wilbur soot quotes
Wilbur soot quotes Gus uams login
Gus uams login Gus social fergus
Gus social fergus Gram positive catalase positive
Gram positive catalase positive Negative numbers rules
Negative numbers rules Positive practice positive outcomes
Positive practice positive outcomes Florida coalition against domestic violence
Florida coalition against domestic violence Canadian supply chain food safety coalition
Canadian supply chain food safety coalition Rng coalition members
Rng coalition members Az housing coalition
Az housing coalition Homeless coalition martinsburg wv
Homeless coalition martinsburg wv Global npo
Global npo Safe surgery coalition
Safe surgery coalition Canadian coalition for seniors mental health
Canadian coalition for seniors mental health Michigan audiology coalition
Michigan audiology coalition Minnesota soil health coalition
Minnesota soil health coalition National transitions of care coalition
National transitions of care coalition Florida health care coalition
Florida health care coalition National coalition academy
National coalition academy Coalition definition
Coalition definition Southern nevada regional planning coalition
Southern nevada regional planning coalition Self-driving coalition for safer streets
Self-driving coalition for safer streets Coalition of sensible taxpayers
Coalition of sensible taxpayers Tennessee affordable housing coalition
Tennessee affordable housing coalition Early learning coalition duval
Early learning coalition duval Navajo nation breastfeeding coalition
Navajo nation breastfeeding coalition Freedom coalition for charter schools
Freedom coalition for charter schools Maryland breastfeeding coalition
Maryland breastfeeding coalition Pakistan agriculture coalition
Pakistan agriculture coalition The japanese concept of a company coalition of suppliers is
The japanese concept of a company coalition of suppliers is Coalition evaluation for communities
Coalition evaluation for communities Oregon self advocacy coalition
Oregon self advocacy coalition Community coalition action theory
Community coalition action theory Global business coalition for health
Global business coalition for health Scholarly publishing and academic resources coalition
Scholarly publishing and academic resources coalition I 95 corridor coalition
I 95 corridor coalition Coalition building public health
Coalition building public health Global health technologies coalition
Global health technologies coalition Coalition for physician enhancement
Coalition for physician enhancement Georgia recycling coalition
Georgia recycling coalition Coalition for juvenile justice
Coalition for juvenile justice