Physio info for primary care nurses Pip Herd








- Slides: 34
Physio info for primary care nurses Pip Herd Renee Ashby 29/03/2017
Objectives 1. General Physio post op care for common ortho surgeries. So you know what patients should be doing and so we can reinforce the same messages. 2. Overview of early management of common musculoskeletal injuries. Ankle, knee, shoulder, wrist, back and neck pain. 3. Any appropriate splints/braces. 4. Crutches. Who/ when/why/how? ? 5. Accessing equipment. Brief overview of what we offer and how to refer. Community/falls in-service to follow at a later date with regards to this.
Post op physio care Rotator cuff surgery • Sling 24/7 as per ortho instructions (6 -8 wks depending on surgeon). • No Active ROM shoulder or elbow (especially if tenodesis). • Need to start PT 6 -8 weeks for a structured ROM and then strengthening programme. • PT can be private or public • No resisted work until 10 -12 weeks. • ACC patients often attend a SAW programme 10 weeks plus (if off work).
Post op care Total Knee Replacement • • • Really important we are all saying the same thing with this group. Wound check by nurse about 10 days. Need to encourage EARLY ROM please. They have exercises from the ward to push on with. They are WBAT from day 0. They should aim for full extension and 90 flexion early (1 -2 weeks). Early full extension is a good predictor of a good outcome. Please check they have adequate pain relief when you see them. If pain is limiting ROM encourage them to continue/re start analgesia. Encourage ICE/ elevation between exercises if swollen/sore. 2 crutches for 4 -6 weeks. If go to 1 have crutch in the opposite hand.
TKR cont. • • All TKR receive a PT appointment with us about 2 weeks post surgery and attend a gym class twice weekly and pool if required. No driving until after 6 week ortho check. Off work for at least 6 weeks and then gradual return depending on job. Start stationary bike once able to get on and off. • Cycling is an excellent aerobic workout. Calisthenics, swimming, low-resistance rowing, stationary skiing machines, walking, hiking, and low-resistance weight lifting all are excellent ways to maintain fitness without overstressing the implant. Suitable activities also include bowling, croquet, golf, doubles tennis, table tennis, ballroom dancing and square dancing. • In general, patients who have undergone total knee replacement should avoid high-impact activities that cause high stress loads on the implant and therefore may increase the risk of early failure.
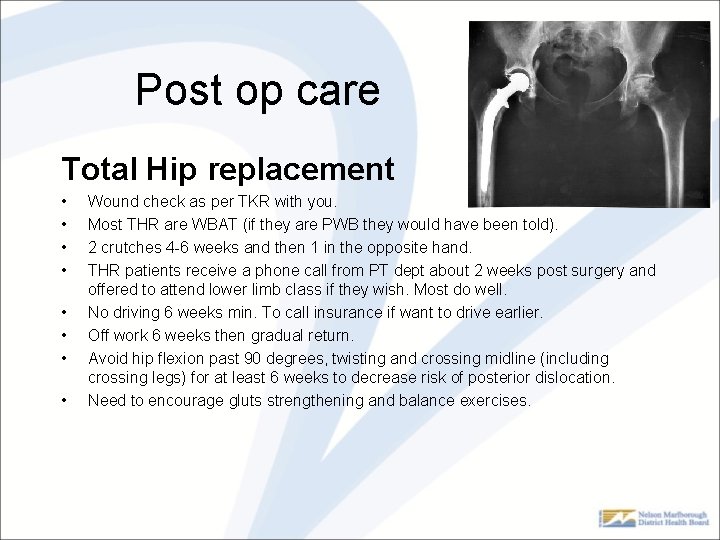
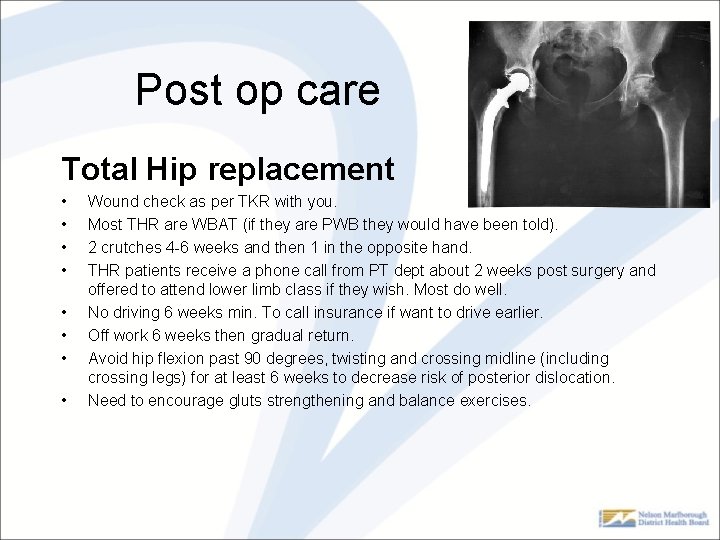
Post op care Total Hip replacement • • Wound check as per TKR with you. Most THR are WBAT (if they are PWB they would have been told). 2 crutches 4 -6 weeks and then 1 in the opposite hand. THR patients receive a phone call from PT dept about 2 weeks post surgery and offered to attend lower limb class if they wish. Most do well. No driving 6 weeks min. To call insurance if want to drive earlier. Off work 6 weeks then gradual return. Avoid hip flexion past 90 degrees, twisting and crossing midline (including crossing legs) for at least 6 weeks to decrease risk of posterior dislocation. Need to encourage gluts strengthening and balance exercises.

THR don'ts!!!
Any Questions? ?
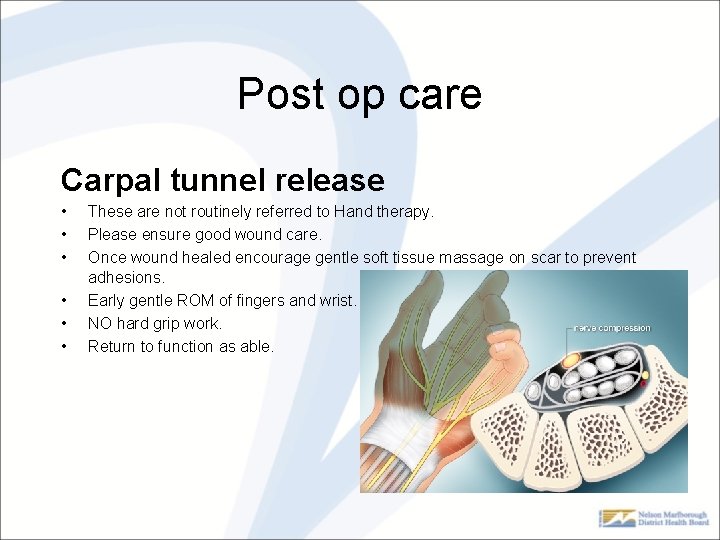
Post op care Carpal tunnel release • • • These are not routinely referred to Hand therapy. Please ensure good wound care. Once wound healed encourage gentle soft tissue massage on scar to prevent adhesions. Early gentle ROM of fingers and wrist. NO hard grip work. Return to function as able.

Post op care Lower leg ORIF/fractures/TA ruptures • • • These all vary slightly depending on injury/ management and surgeon preference. Most of these do not require physio input until after their 6 week ortho appointment. Ortho generally refer them then. If the surgeon wants earlier rehab they will refer to us or give the patient the referral so they can access private physio.

Early management -Ankle Sprain
ACC website guidelines. • • • http: //www. acc. co. nz/publications It is generally accepted that Grades I and II ankle sprains are best managed with rest, ice, compression (tubigrip) and elevation followed by early mobilisation. Protected weight bearing (crutches) + NSAID. Early ROM (up/down and circles) Early return to work and gentle activities. When should you request an x-ray? ? ?
Ottawa Ankle rules • Ankle X-ray is only required if there is any pain in the malleolar zone and any one of the following: 1. Bone tenderness along the distal 6 cm of the posterior edge of the tibia or tip of the medial malleolus, OR 2. Bone tenderness along the distal 6 cm of the posterior edge of the fibula or tip of the lateral malleolus, OR 3. An inability to bear weight both immediately and in the ED for four steps. • Additionally, the Ottawa ankle rules indicate whether a foot X-ray series is required. It states that it is indicated if there is any pain in the midfoot zone and any one of the following: 1. Bone tenderness at the base of the fifth metatarsal (for foot injuries), OR 2. Bone tenderness at the navicular bone (for foot injuries), OR 3. An inability to bear weight both immediately and in ED for four steps.

Ottawa Ankle rules • Certain groups are excluded, in particular – pregnant women – those with diminished ability to follow the test (for example due to head injury or intoxication) • Several studies strongly support the use of the Ottawa Ankle Rules in children over 6 (98. 5% sensitivity) – however, their usefulness in younger children has not yet been thoroughly examined.
Acute Knee Management • • Rule out fracture etc. . . (see “rules” next slide). RICE + crutches Refer to ortho if thought ACL etc. . . Private practice physio probably most appropriate place to refer to (if ruled out need for ortho). • Knee bracing – only be as per a consultants recommendation. • Aim is rule out anything nasty, early ROM, strength and mobilisation.
Ottawa knee rules • • They state that an x-ray is required only in patients who have an acute knee injury with one or more of the following: Age 55 years or older Tenderness at head of fibula Isolated tenderness of patella Inability to flex the knee greater than 90° Inability to bear weight both immediately and in the emergency department (4 steps) The Ottawa knee rules were derived to aid in the efficient use of radiography in acute knee injuries and have since been prospectively validated on multiple occasions in different populations and in both children and adults. [2] Some studies found sensitivities for the Ottawa knee rules of 98 -100% for clinically significant knee fractures, meaning if the patient is negative for all criteria, the patient is likely not to have a knee fracture. However, specificities for the Ottawa knee rules are typically poor, meaning a medical provider cannot say without proper testing what injury the patient may have. The Pittsburgh knee rules have been found to be more specific in diagnosis. [3]
Pittsburg knee rules • • • Blunt trauma or a fall as mechanism of injury AND either of the following: – Age younger than 12 years or older than 50 years. – Inability to walk four weight-bearing steps in the emergency department. If the patient satisfies the above criteria, they should receive an X-ray to assess for a possible fracture. The sensitivity of using the Pittsburgh knee rules is 99% with a specificity of 60%. That means the use of the above rules has a false negative result of 1% and a false positive result of 40%. [1] From a medical point of view, the false positive result is less important as if the patient is positive, they should receive an X-ray to assess for a possible fracture, which has a much higher specificity. However, from a practical point of view, false positives that lead to negative X-ray tests were the very thing that the knee rules are trying to address. Nonetheless, the Pittsburgh knee rules offer fewer false positives than do the Ottawa knee rules, though the Ottawa knee rules are more commonly used. [2] The Ottowa knee rules count even a limping step as a step. Pittsburgh counts only a complete heel/toe plant as a step. This key difference likely accounts for the difference in specificity. The use of the Pittsburgh knee rules reduces the use of knee radiographs by 52%. [3]
X-rays continue • Ottawa rules for x-ray. Options for x-ray are ED at Wairau or Marlborough Medical imaging during working hours. ED is aware access to acute imaging publically is limited and this is currently work in progress to improve this pathway. • Marlborough Medical Imaging (same door as Churchill at back of hospital) accepts referrals for acute x-rays (Mon-Fri 9 am-5 pm). No appointment required. Need a referral either electronically, fax or paper version (someone to send results to). Cost is $25 for ACC claim. $78 Ankle, $86 knee, $90 shoulder for non ACC. Phone: 03 5789109

Acute Back pain
Acute Neck pain

Acute Shoulder pain
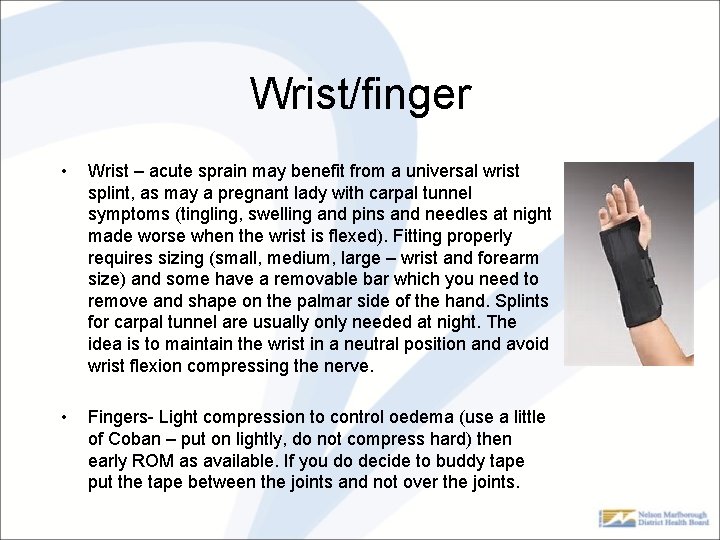
Wrist/finger • Wrist – acute sprain may benefit from a universal wrist splint, as may a pregnant lady with carpal tunnel symptoms (tingling, swelling and pins and needles at night made worse when the wrist is flexed). Fitting properly requires sizing (small, medium, large – wrist and forearm size) and some have a removable bar which you need to remove and shape on the palmar side of the hand. Splints for carpal tunnel are usually only needed at night. The idea is to maintain the wrist in a neutral position and avoid wrist flexion compressing the nerve. • Fingers- Light compression to control oedema (use a little of Coban – put on lightly, do not compress hard) then early ROM as available. If you do decide to buddy tape put the tape between the joints and not over the joints.
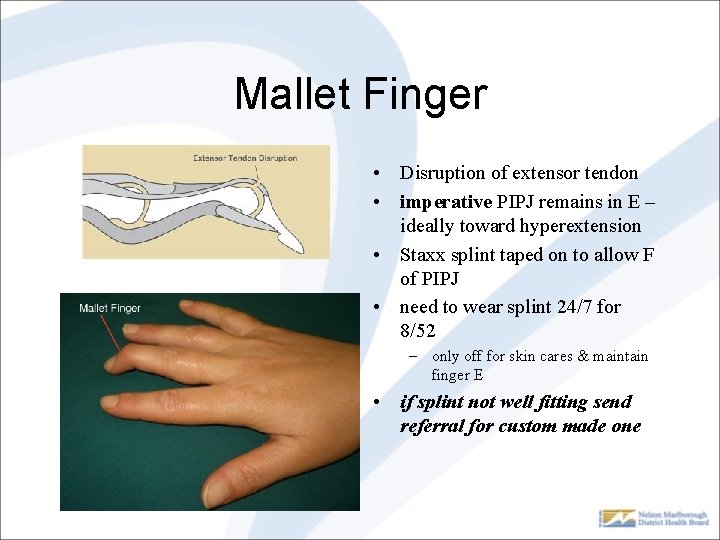
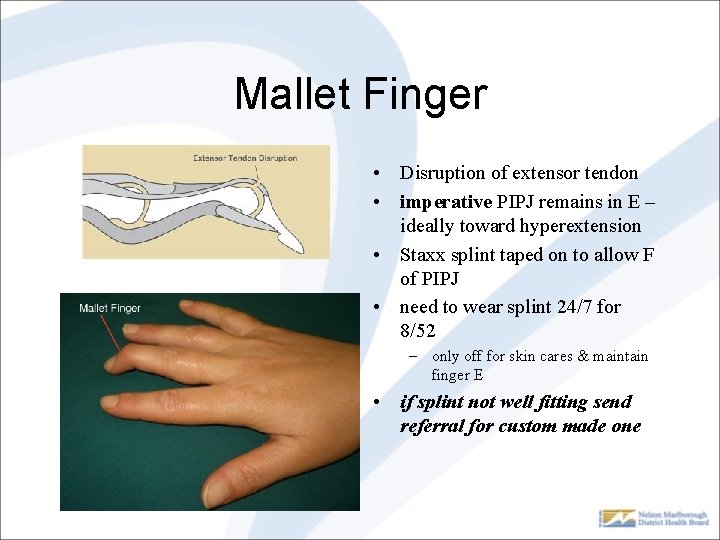
Mallet Finger • Disruption of extensor tendon • imperative PIPJ remains in E – ideally toward hyperextension • Staxx splint taped on to allow F of PIPJ • need to wear splint 24/7 for 8/52 – only off for skin cares & maintain finger E • if splint not well fitting send referral for custom made one
Crutches • PHO have provided crutches for each GP clinic to issue. • After Hours clinic has some. • If bariatric, paediatric or can not manage crutches due to age or co-existing condition please refer to Wairau Physio department with a detailed written referral – will not be clinically assessed – just issued and taught how to use crutches.

Crutches Standing up • Push up off the bed/chair with hands • Fit the crutches only once standing Sitting down • Take your arms out of the crutches and hold them in one hand • Use the other hand to feel back for the chair/bed Walking • Both crutches forward first • Affected Leg • Unaffected Leg Safety Tips • Ensure there is adequate tread on the rubber tips of the crutches • Wear non-slip footwear or bare feet • Take extra care walking on wet surfaces. • If walking with only one crutch, use it in the opposite hand to the affected leg.
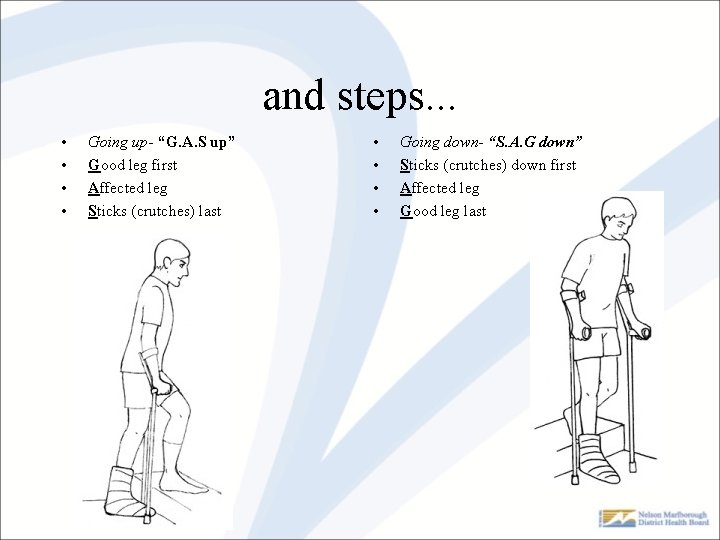
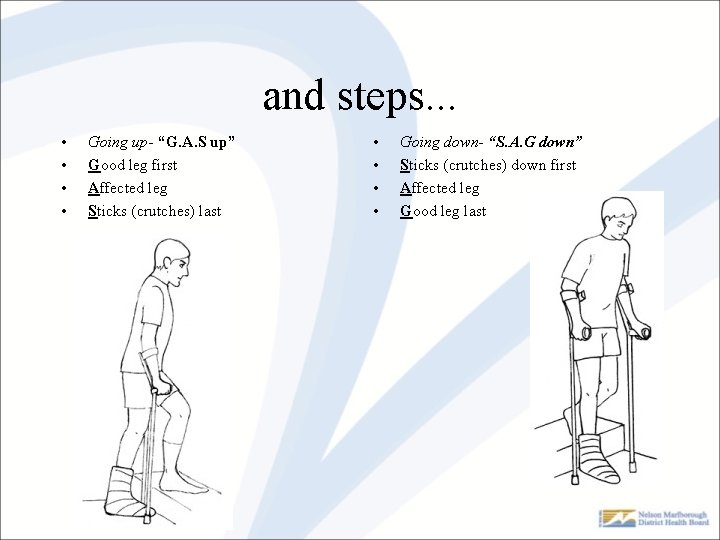
and steps. . . • • Going up- “G. A. S up” Good leg first Affected leg Sticks (crutches) last • • Going down- “S. A. G down” Sticks (crutches) down first Affected leg Good leg last
Equipment • Detailed referral required with condition and current problem. • Crutches - referral as above • Walking frames – requires a mobility assessment • Wheelchairs are not loaned short term by us – only provide for short term loan on discharge from IP where reliant on for indoor mobility • Wheel chair hire is currently – Access mobility, Wairau Pharmacy, and Avanti Plus – Red cross currently reviewing loan policy due to increased maintenance requirements – ACC
Referrals • How do you refer clients? – your normal form written or electronic – same as any hospital referral • Please include as much info as possible – we are regularly getting referrals with insufficient info to triage accurately • Request of orthotic devices need to go to orthotics – cervical soft collars, lumbosacral supports, slings, hernia supports – we can only access these as part of our treatment

Accessing appointments • Health Shuttle – needs 24 hour notice. 0800333781 • ACC – taxis. Clients can claim retrospectively or get taxi chit. Client best discuss with case manager. • Community visits from PT. Often appropriate to visit client in own home environment. If you think this please include reason etc. . . So we can triage accordingly.
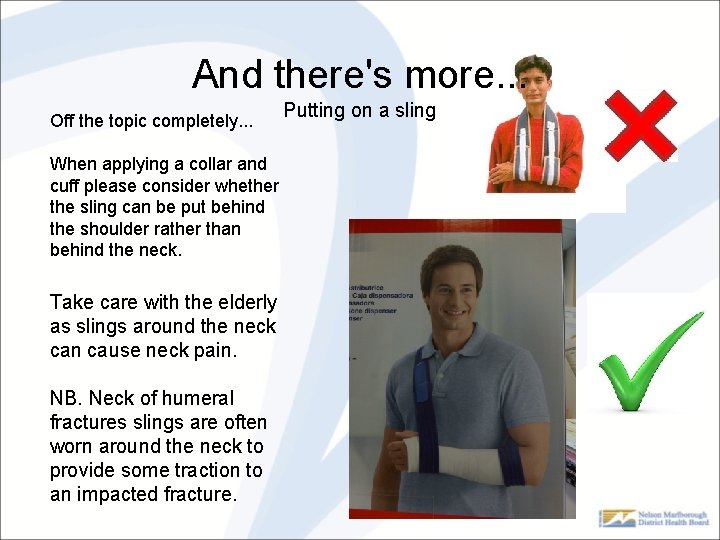
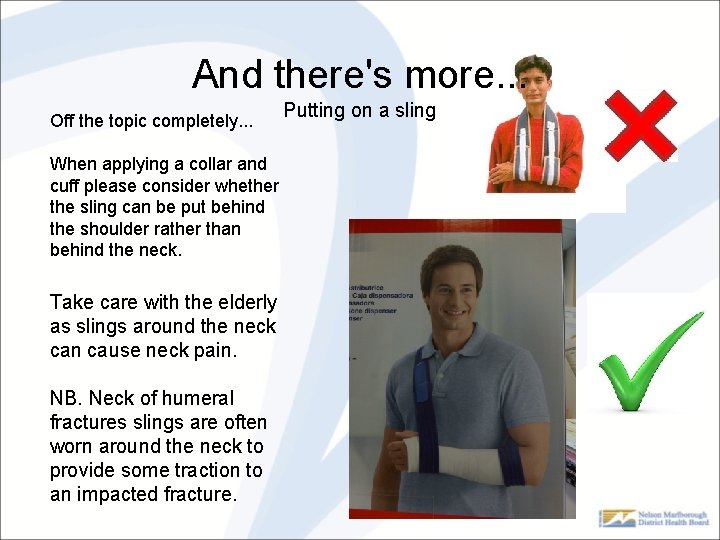
And there's more. . . Off the topic completely. . . Putting on a sling When applying a collar and cuff please consider whether the sling can be put behind the shoulder rather than behind the neck. Take care with the elderly as slings around the neck can cause neck pain. NB. Neck of humeral fractures slings are often worn around the neck to provide some traction to an impacted fracture.