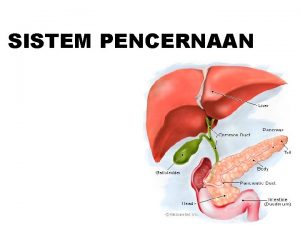
Patofisiologi Gizi Gangguan Sistem Pencernaan penyakit gastrointestinal gangguan

![Jaundice (icterus) n n a. b. c. The normal [bilirubin] in blood plasma is Jaundice (icterus) n n a. b. c. The normal [bilirubin] in blood plasma is](https://slidetodoc.com/presentation_image_h2/871eebd5885d27e468430b4db27a1e41/image-18.jpg)
- Slides: 23
Patofisiologi Gizi Gangguan Sistem Pencernaan • penyakit gastrointestinal • gangguan akibat diare • penyakit hati
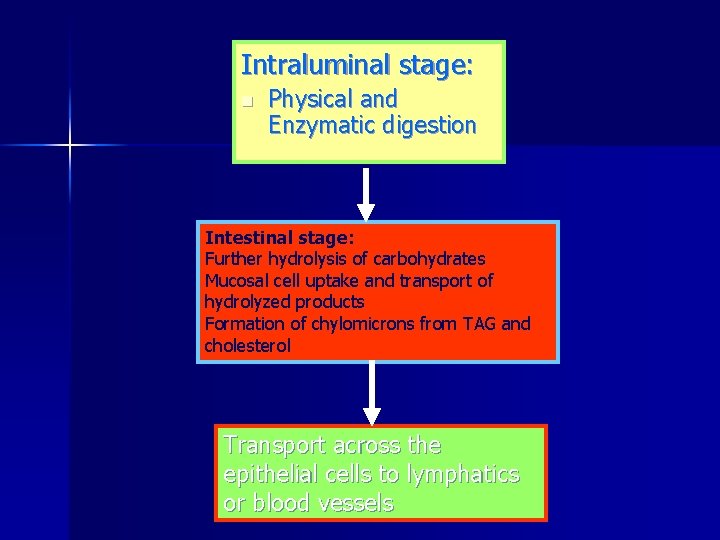
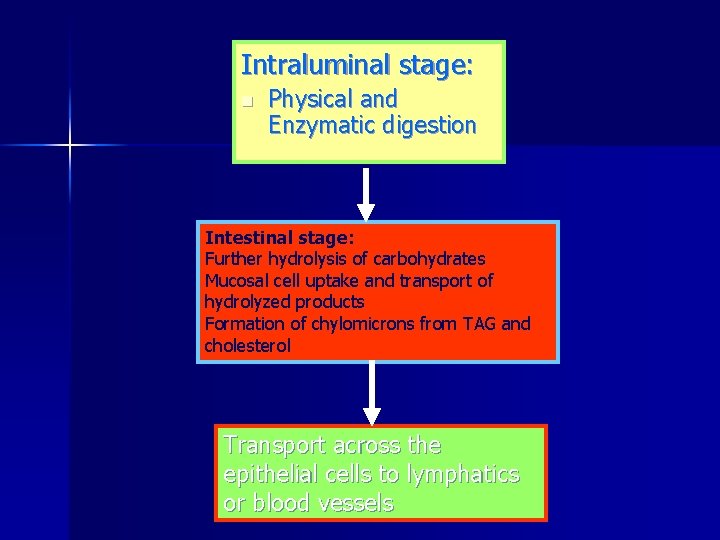
Intraluminal stage: n Physical and Enzymatic digestion Intestinal stage: Further hydrolysis of carbohydrates Mucosal cell uptake and transport of hydrolyzed products Formation of chylomicrons from TAG and cholesterol Transport across the epithelial cells to lymphatics or blood vessels
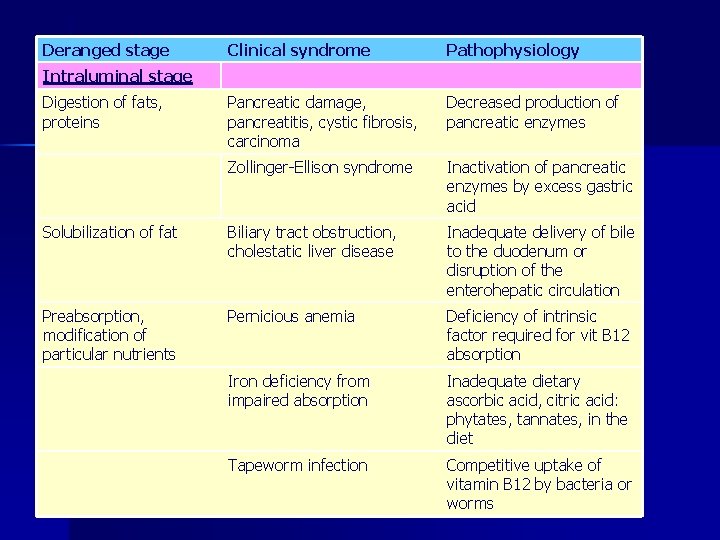
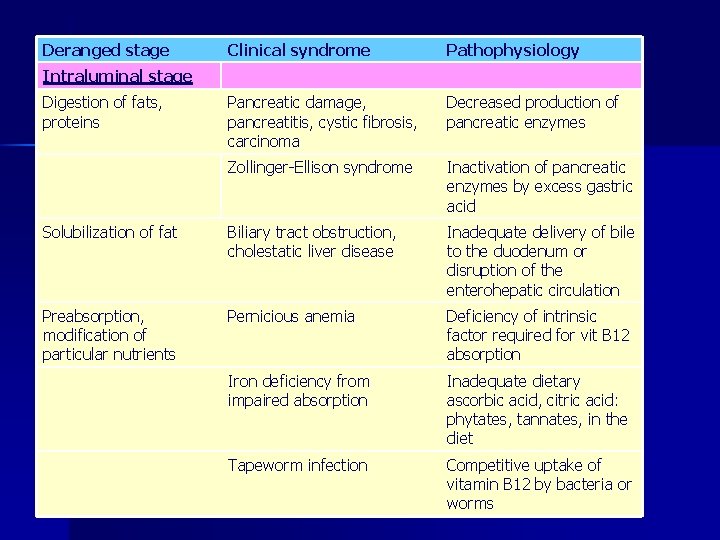
Deranged stage Clinical syndrome Pathophysiology Pancreatic damage, pancreatitis, cystic fibrosis, carcinoma Decreased production of pancreatic enzymes Zollinger Ellison syndrome Inactivation of pancreatic enzymes by excess gastric acid Solubilization of fat Biliary tract obstruction, cholestatic liver disease Inadequate delivery of bile to the duodenum or disruption of the enterohepatic circulation Preabsorption, modification of particular nutrients Pernicious anemia Deficiency of intrinsic factor required for vit B 12 absorption Iron deficiency from impaired absorption Inadequate dietary ascorbic acid, citric acid: phytates, tannates, in the diet Tapeworm infection Competitive uptake of vitamin B 12 by bacteria or worms Intraluminal stage Digestion of fats, proteins
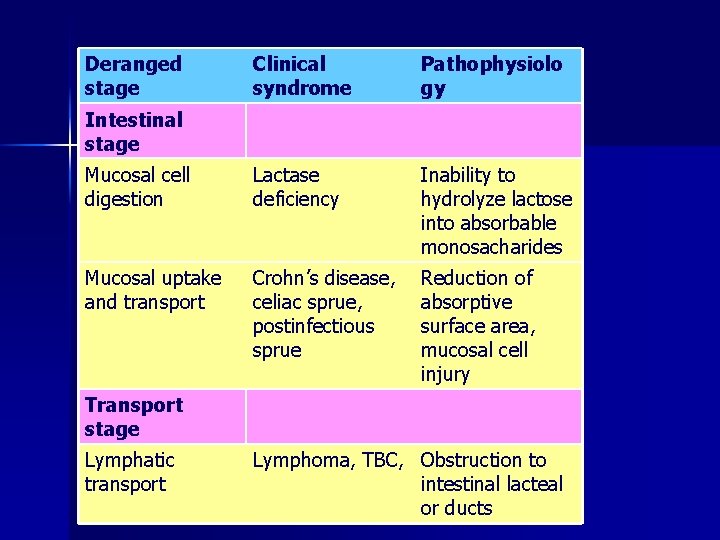
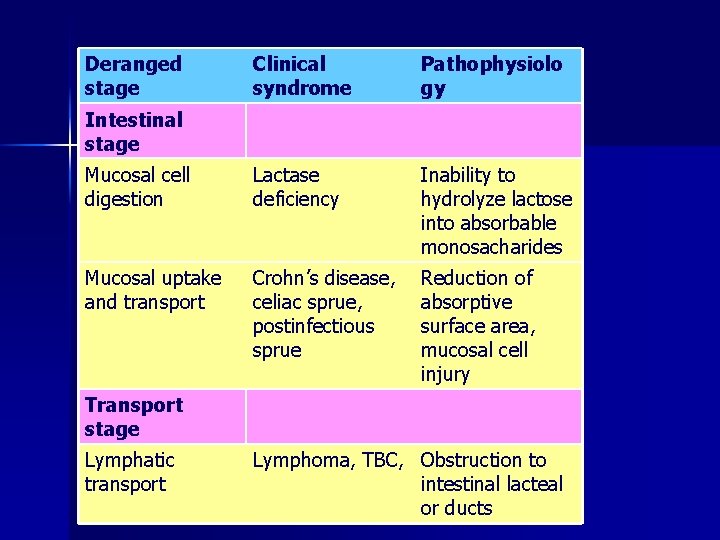
Deranged stage Clinical syndrome Pathophysiolo gy Mucosal cell digestion Lactase deficiency Inability to hydrolyze lactose into absorbable monosacharides Mucosal uptake and transport Crohn’s disease, celiac sprue, postinfectious sprue Reduction of absorptive surface area, mucosal cell injury Intestinal stage Transport stage Lymphatic transport Lymphoma, TBC, Obstruction to intestinal lacteal or ducts
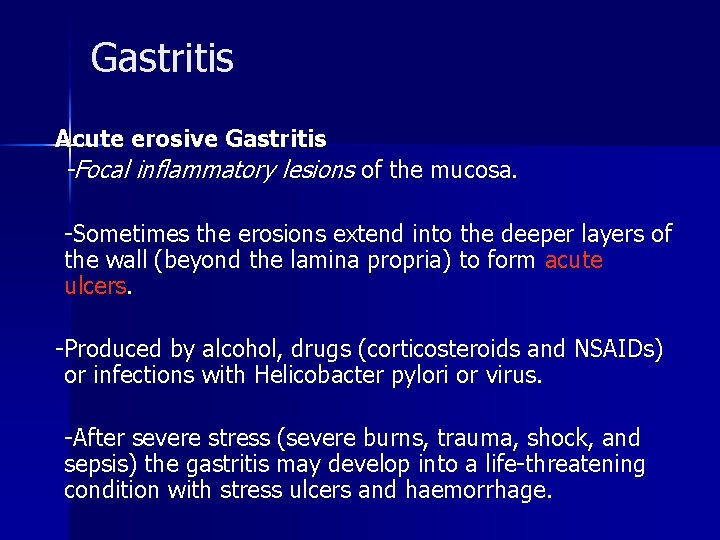
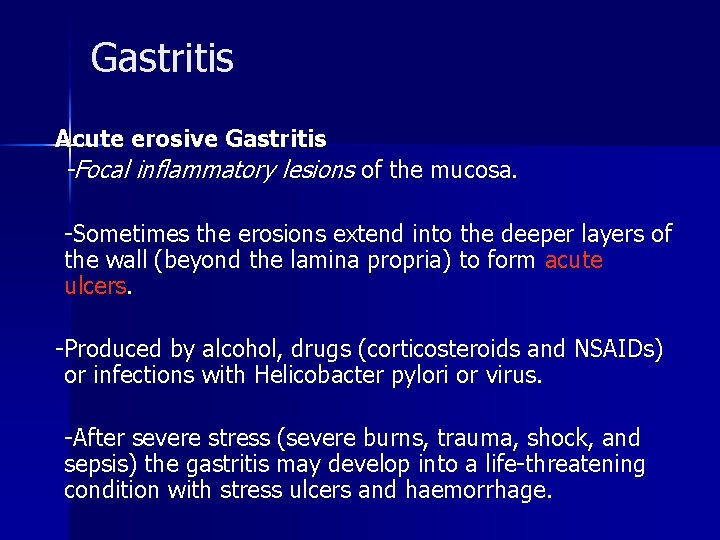
Gastritis Acute erosive Gastritis -Focal inflammatory lesions of the mucosa. Sometimes the erosions extend into the deeper layers of the wall (beyond the lamina propria) to form acute ulcers. Produced by alcohol, drugs (corticosteroids and NSAIDs) or infections with Helicobacter pylori or virus. After severe stress (severe burns, trauma, shock, and sepsis) the gastritis may develop into a life threatening condition with stress ulcers and haemorrhage.
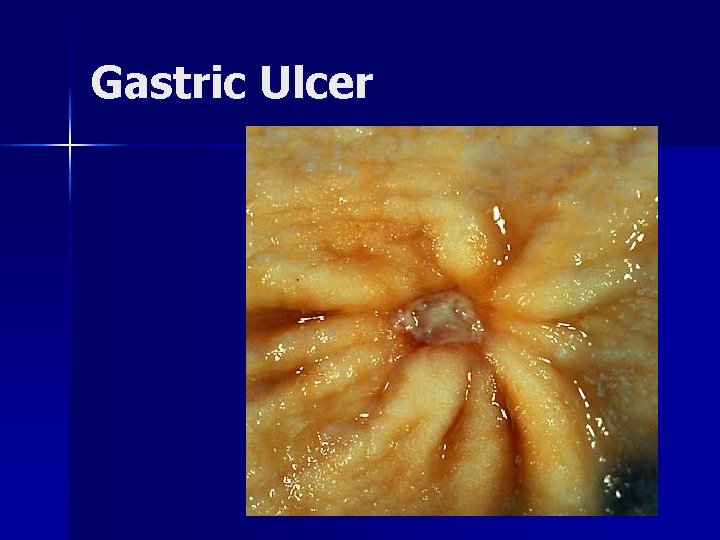
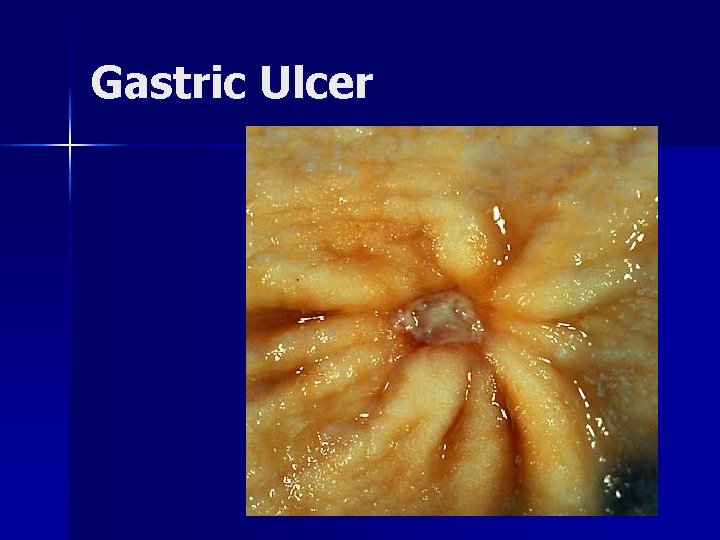
Gastric Ulcer
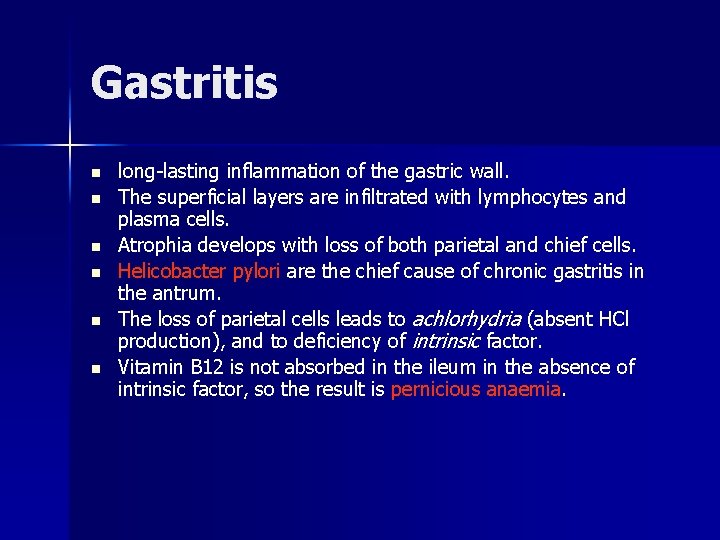
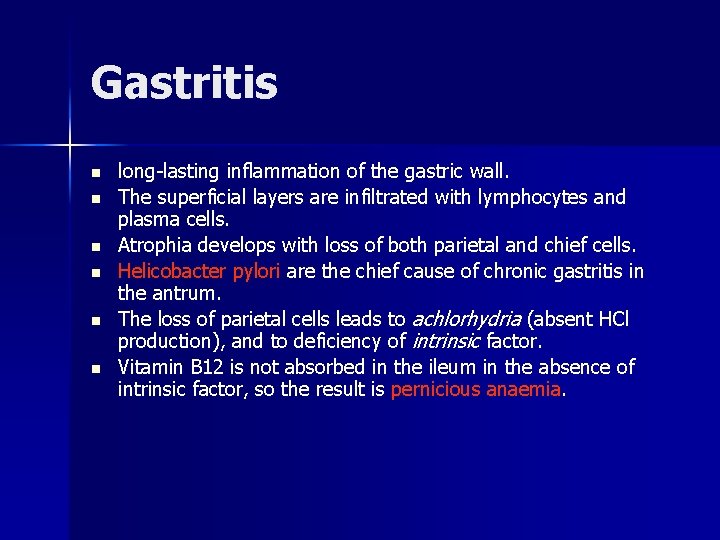
Gastritis n n n long lasting inflammation of the gastric wall. The superficial layers are infiltrated with lymphocytes and plasma cells. Atrophia develops with loss of both parietal and chief cells. Helicobacter pylori are the chief cause of chronic gastritis in the antrum. The loss of parietal cells leads to achlorhydria (absent HCl production), and to deficiency of intrinsic factor. Vitamin B 12 is not absorbed in the ileum in the absence of intrinsic factor, so the result is pernicious anaemia.
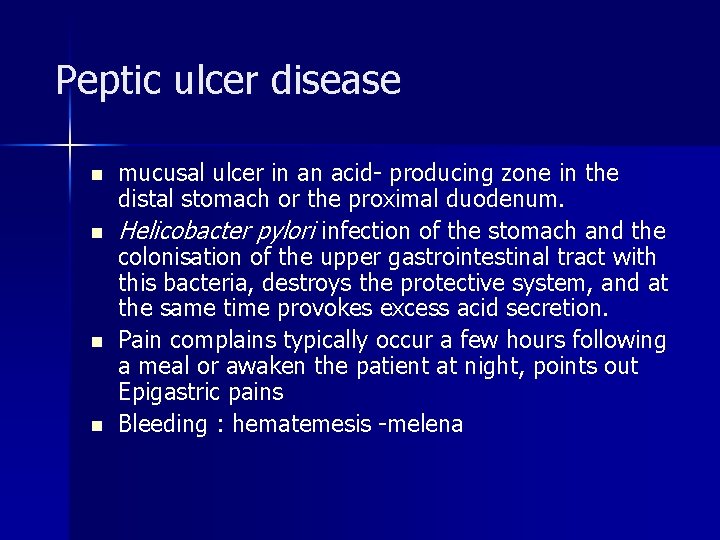
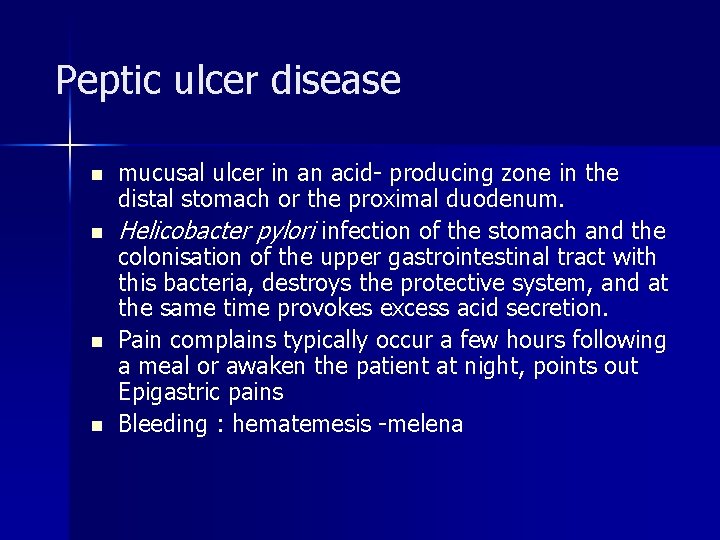
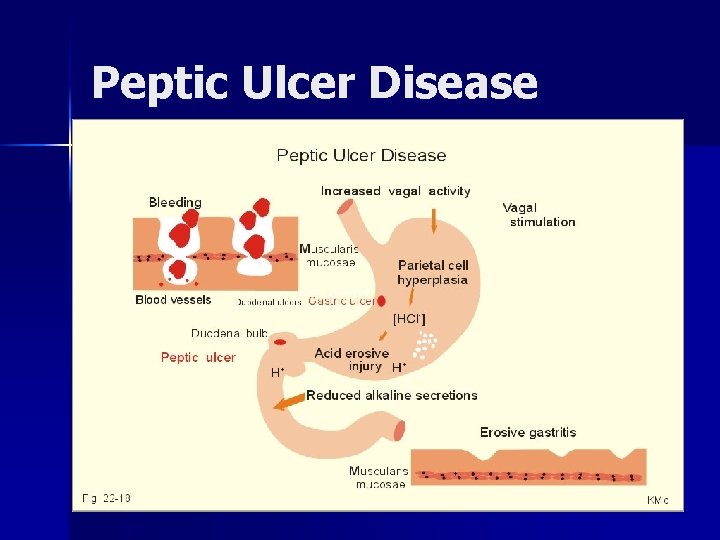
Peptic ulcer disease n n mucusal ulcer in an acid producing zone in the distal stomach or the proximal duodenum. Helicobacter pylori infection of the stomach and the colonisation of the upper gastrointestinal tract with this bacteria, destroys the protective system, and at the same time provokes excess acid secretion. Pain complains typically occur a few hours following a meal or awaken the patient at night, points out Epigastric pains Bleeding : hematemesis melena
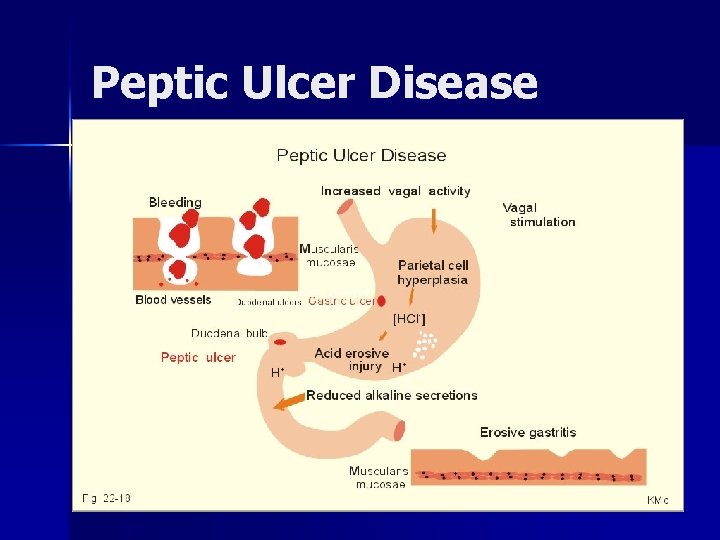
Peptic Ulcer Disease
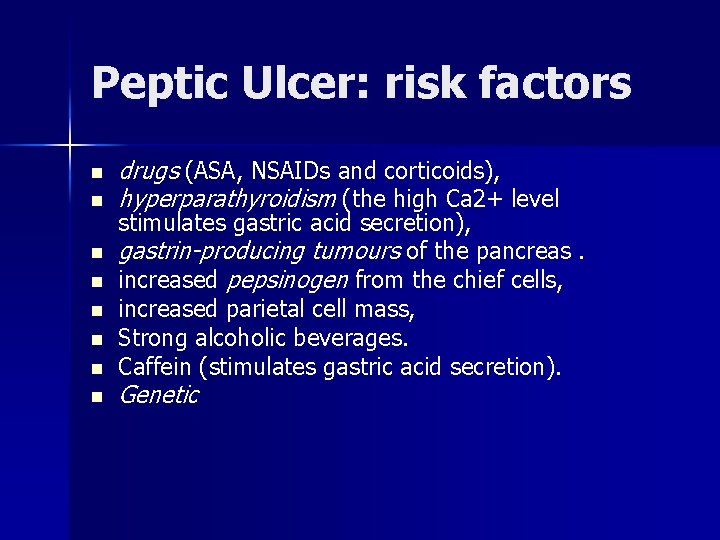
Peptic Ulcer: risk factors n n n n drugs (ASA, NSAIDs and corticoids), hyperparathyroidism (the high Ca 2+ level stimulates gastric acid secretion), gastrin-producing tumours of the pancreas. increased pepsinogen from the chief cells, increased parietal cell mass, Strong alcoholic beverages. Caffein (stimulates gastric acid secretion). Genetic
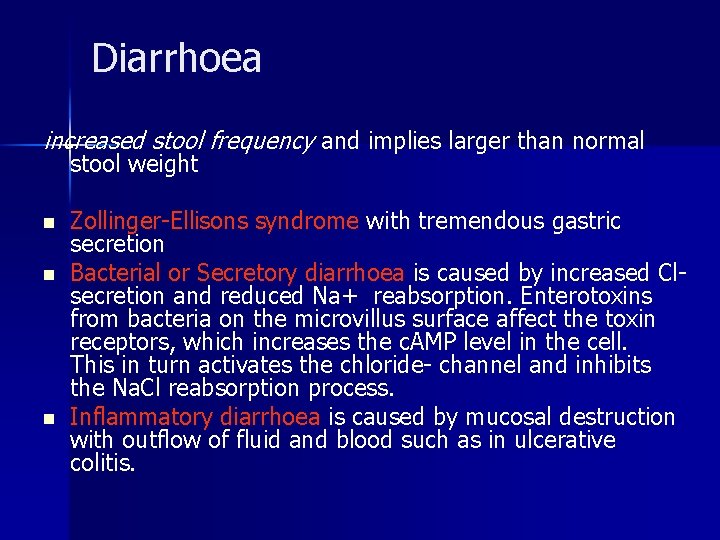
Diarrhoea increased stool frequency and implies larger than normal stool weight n n n Zollinger Ellisons syndrome with tremendous gastric secretion Bacterial or Secretory diarrhoea is caused by increased Cl secretion and reduced Na+ reabsorption. Enterotoxins from bacteria on the microvillus surface affect the toxin receptors, which increases the c. AMP level in the cell. This in turn activates the chloride channel and inhibits the Na. Cl reabsorption process. Inflammatory diarrhoea is caused by mucosal destruction with outflow of fluid and blood such as in ulcerative colitis.
Diarrhoea n n Osmotic diarrhoea caused by active substances in the gut lumen. These substances are normal nutrients in case of malabsorption, or non absorbable substances taken for some reason or other. Diarrhoea following ileal resection. Bile acids are normally reabsorbed in the terminal ileum. Following ileal resection the bile acids enter the colon. Bile acids are toxic to the colonic mucosa and stimulate colonic secretion of large volumes,

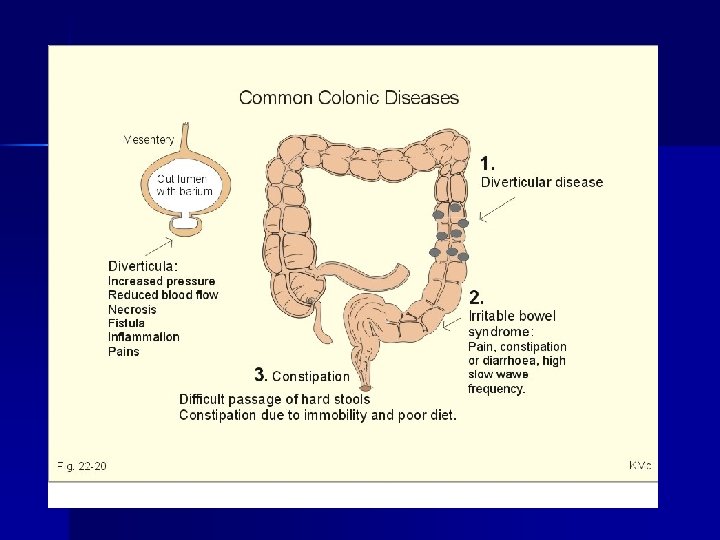
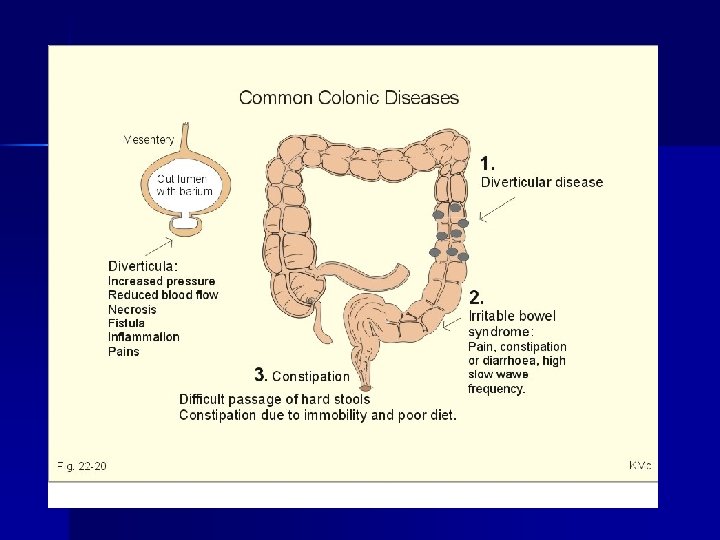
slow colonic motility: Colon irritable n abdominal pain (diffuse or localised to the left iliac fossa), which is relieved by defecation or flatulence. n There are often frequent small volume stools, but the patient feels that the emptying is incomplete. The abdomen is distended. This is a condition with painful spasms causing constipation alternating with mucous diarrhoea. n The condition is related to stress and sedentary life style, and is relieved by daily exercise.
Diverticulosis n n Diverticulosis or diverticular disease is a condition with herniation of the mucosa through the muscular layers of the colon, caused by increased intraluminal pressure. if they are inflamed the condition is called diverticulitis. Persons with disturbed stoolhabits are likely to develop increased intraluminal pressure during defaecation, and they may develop hernias at weak spots in the gut wall. The incidence is high in inactive persons and low in vegetarians or in persons with a high dietary fibre content. Mild clinical cases can be treated with light daily
Constipation n n frequently caused by a low fibre intake in sedentary persons. They often exhibit irregular defaecation habits, and irrational use of laxatives. Such habits suppress the natural reflexes. The condition is improved by a high fibre diet or by daily walking. Suppositories may be necessary, but long term use of laxatives is contraindicated.
![Jaundice icterus n n a b c The normal bilirubin in blood plasma is Jaundice (icterus) n n a. b. c. The normal [bilirubin] in blood plasma is](https://slidetodoc.com/presentation_image_h2/871eebd5885d27e468430b4db27a1e41/image-18.jpg)
Jaundice (icterus) n n a. b. c. The normal [bilirubin] in blood plasma is up to 17 mg /l or 29 mmol/ l The threshold for visible jaundice (icterus) is a [bilirubin] in blood plasma above 18 mg /l or 30 m. M in most people. Three types of icterus can be distinguished: Prehepatic or haemolytic icterus Intrahepatic icterusis Posthepatic icterus
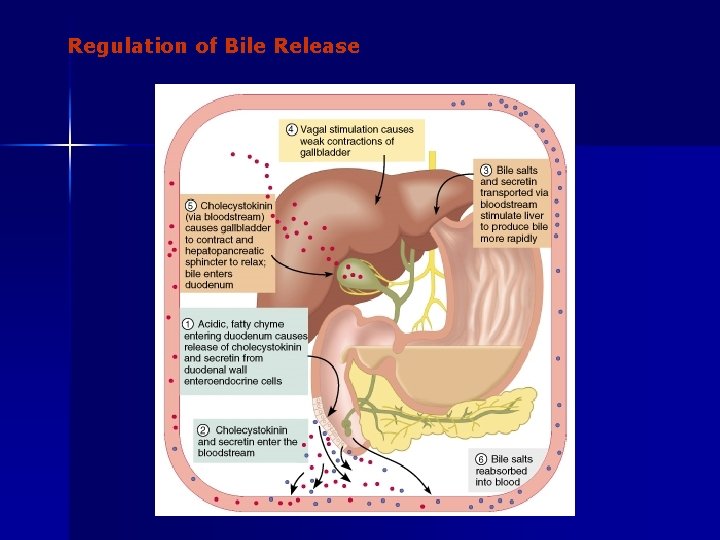
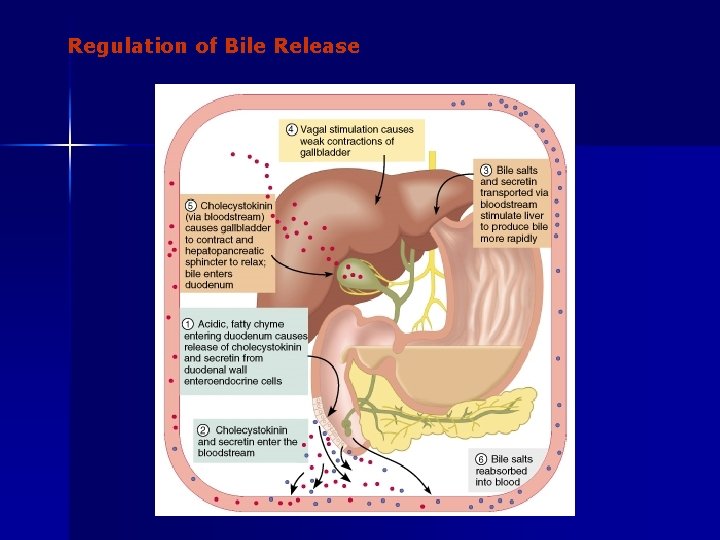
Regulation of Bile Release
Prehepatic or haemolytic icterus • Haemolytic anaemia causes haemolytic jaundice. • Increased destruction of red cells (haemolysis) increases the bilirubin production to the extent that the hepatocytes cannot conjugate the bilirubin as rapidly as it is formed (the key hole enzyme is glucuronyl transferase). • The neurotoxic free bilirubin in blood plasma rises much above normal, and large quantities of urobilinogen is excreted in the urine.
Intrahepatic icterusis n n n Caused by poor hepatocyte function. Damages of the hepatocytes by infections, tumours, or toxic agents impair the uptake, transport and conjugation of bilirubin. Absence of glucuronyl transferase or inhibition of the enzyme by steroids block conjugation of bilirubin.
Posthepatic icterus n n n caused by cholestasis due to gallstones or pancreatic tumours. Gallstones or tumour masses obstruct the bile ducts, which is causing extrahepatic cholestasis with impaired excretion of conjugated bilirubin to the intestine. conjugated bilirubin reflux to the blood. Most of the bilirubin in plasma is therefore conjugated and some of it strongly bound to plasma albumin.
Selamat belajar
 Parotitis adalah gangguan sistem pencernaan yang disebabkan
Parotitis adalah gangguan sistem pencernaan yang disebabkan Patofisiologi penyakit jantung bawaan
Patofisiologi penyakit jantung bawaan Kode icd 10 gangguan pencernaan
Kode icd 10 gangguan pencernaan Patogenesis penyakit defisiensi gizi
Patogenesis penyakit defisiensi gizi Verner morrison sendromu
Verner morrison sendromu Patofisiologi sistem integumen
Patofisiologi sistem integumen Patofisiologi sistem kardiovaskuler
Patofisiologi sistem kardiovaskuler Patofisiologi sistem perkemihan
Patofisiologi sistem perkemihan Pathway sistem pencernaan
Pathway sistem pencernaan Sistem pencernaan echinoidea
Sistem pencernaan echinoidea Hermaroid
Hermaroid Kelenjar pankreas
Kelenjar pankreas Reproduksi aseksual subfilum urochordata dengan cara
Reproduksi aseksual subfilum urochordata dengan cara Apa itu pelecypoda
Apa itu pelecypoda Salah satu organ penyusun sistem gerak yaitu tulang
Salah satu organ penyusun sistem gerak yaitu tulang Sistem pencernaan buaya
Sistem pencernaan buaya Sistem pencernaan arachnida
Sistem pencernaan arachnida Sistem pencernaan amfibi
Sistem pencernaan amfibi Sistem pencernaan
Sistem pencernaan Pencernaan hewan
Pencernaan hewan Sistem organ pencernaan pada manusia disusun oleh
Sistem organ pencernaan pada manusia disusun oleh Sistem pencernaan monogastrik
Sistem pencernaan monogastrik Anatomi dan fisiologi sistem pencernaan
Anatomi dan fisiologi sistem pencernaan Sistem pencernaan
Sistem pencernaan