Past history No underlying disease No drugs or









- Slides: 62




Past history • No underlying disease • No drugs or food allergy • No smoking and alcohol drinking • No Hx of surgery or previous anesthesia • FC I
Past history • Current medication • Prednisolone(5) 1 x 3 (>2 months) • Pyridostigminine(60) 1 tab PO q 6 hrs (240 mg/day)
Physical examination Vital signs BP 100/62 mm. Hg PR 71 BPM BT 37°C RR 16 breaths /min • BW 44 kg, Height 155 cm (BMI 18. 4 kg/m 2) • GA : A Thai female, good consciousness, well co-operated, not pale, no jaundice
Physical examination • HEENT : No ptosis, not pale, no jaundice, no buffalo hump, no hoarsness , no thyroid gland enlargement • Pulmonary : no dyspnea , no tachypnea , no use of accessory muscle , clear and equal breath sound both lungs • CVS : Pulse full & regular , no heaving, no thrill, normal S 1&S 2, no murmurs
Physical examination • Airway examination : Limit neck of motion : No Thyromental distance > 6 cm Mouth opening > 3 cm Prominent incisor : No Mallampati grade : grade 1
Physical examination • Abdomen : soft, not tender, liver & spleen can not palpable, no abdominal striae • Extremities : no deformity, no pitting edema • Neuro : E 4 M 6 V 5, no facial palsy, full EOM, Pupil 2 mm RTLBE, normal gag reflex, motor grade V/V all, DTR 2+all
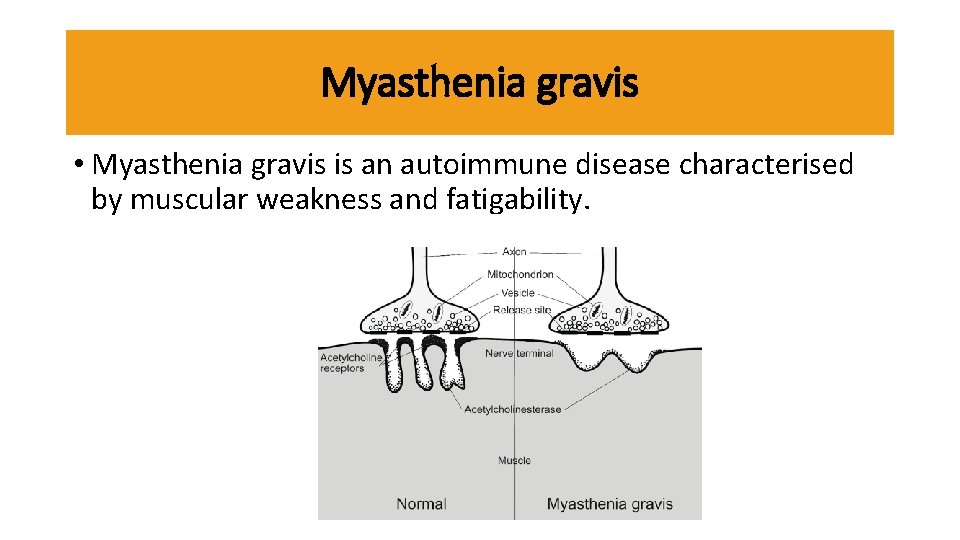
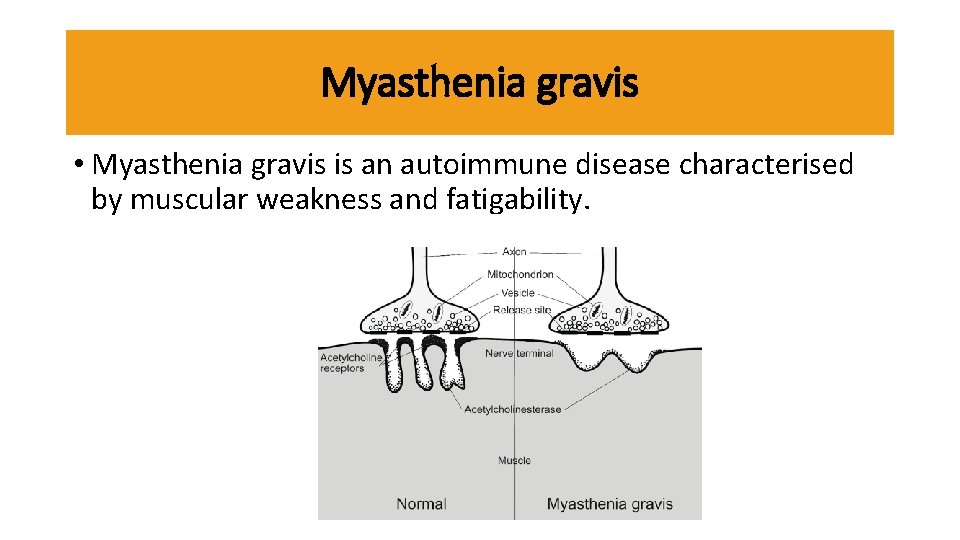
Myasthenia gravis • Myasthenia gravis is an autoimmune disease characterised by muscular weakness and fatigability.
Diagnostic tests • History and clinical exam • Electrophysiologic test • Pharmacologic test • Serologic test
Differential diagnosis
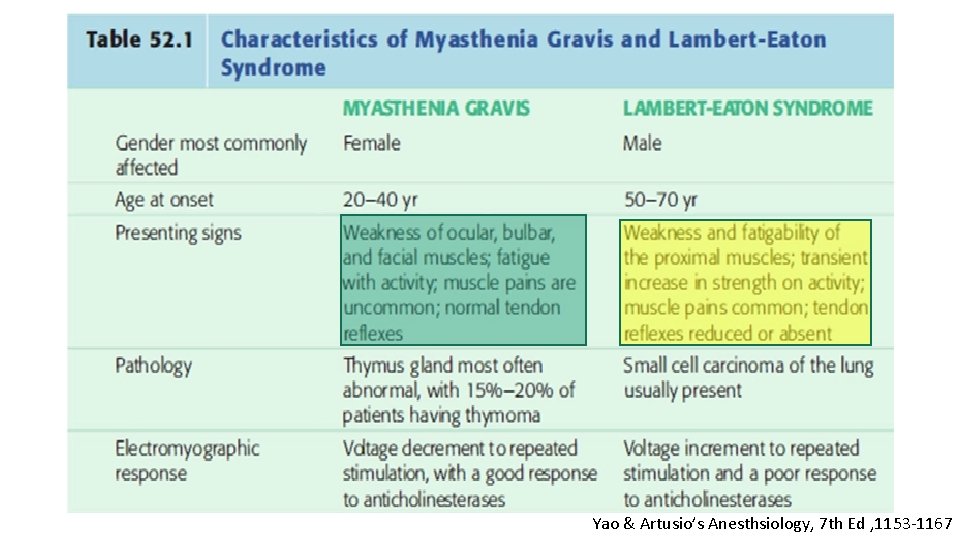
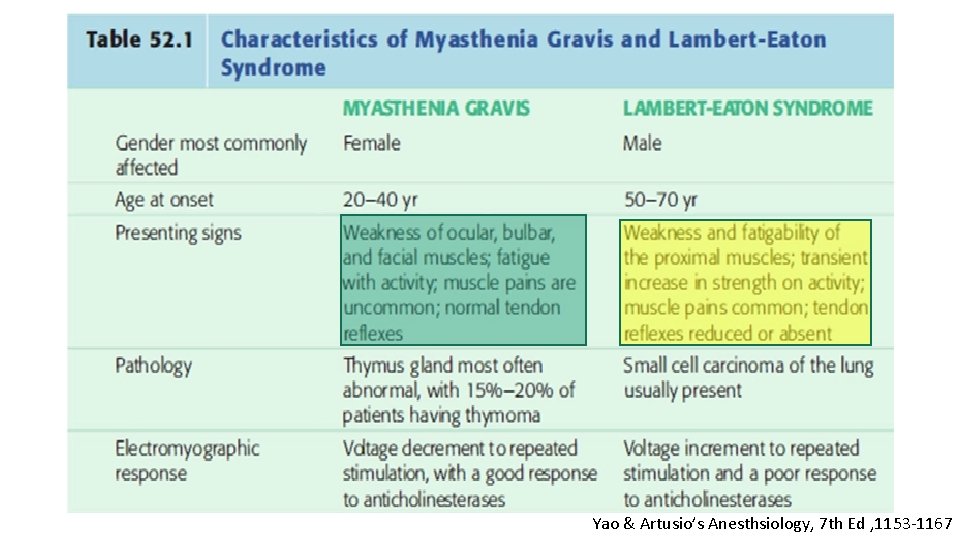
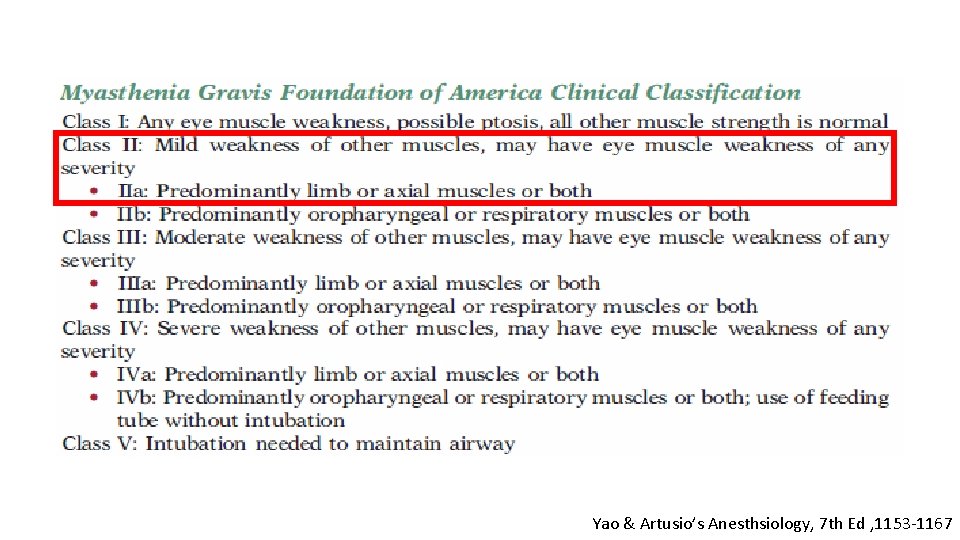
Yao & Artusio’s Anesthsiology, 7 th Ed , 1153 -1167
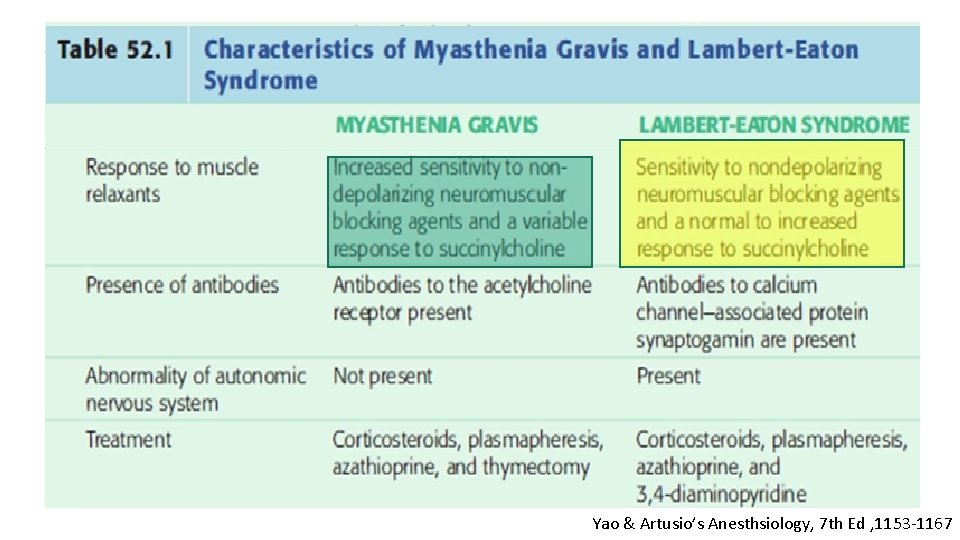
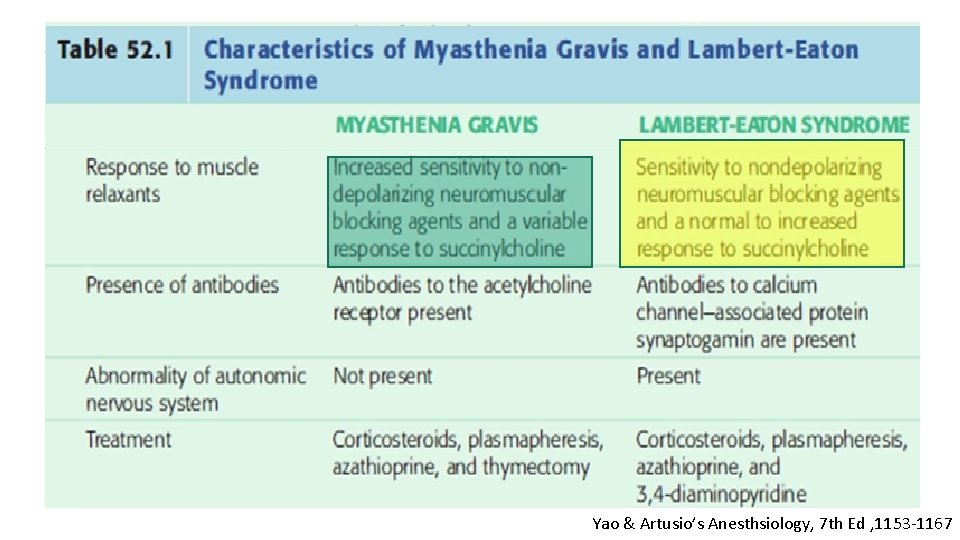
Yao & Artusio’s Anesthsiology, 7 th Ed , 1153 -1167
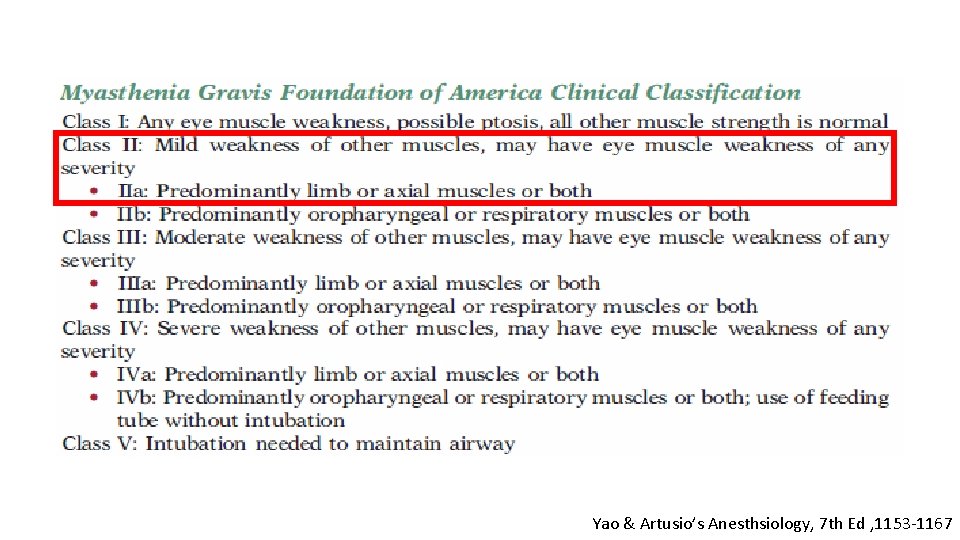
Yao & Artusio’s Anesthsiology, 7 th Ed , 1153 -1167

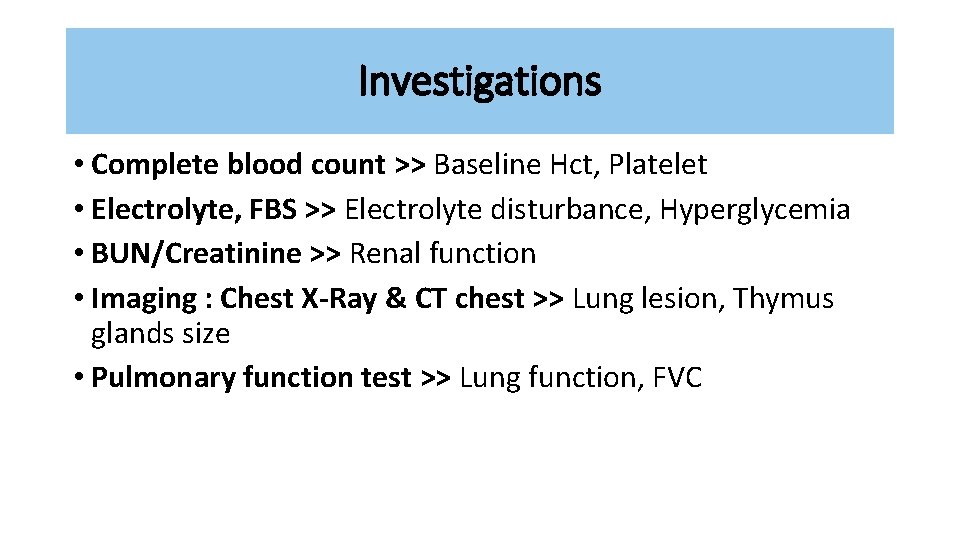
R 1 Investigations
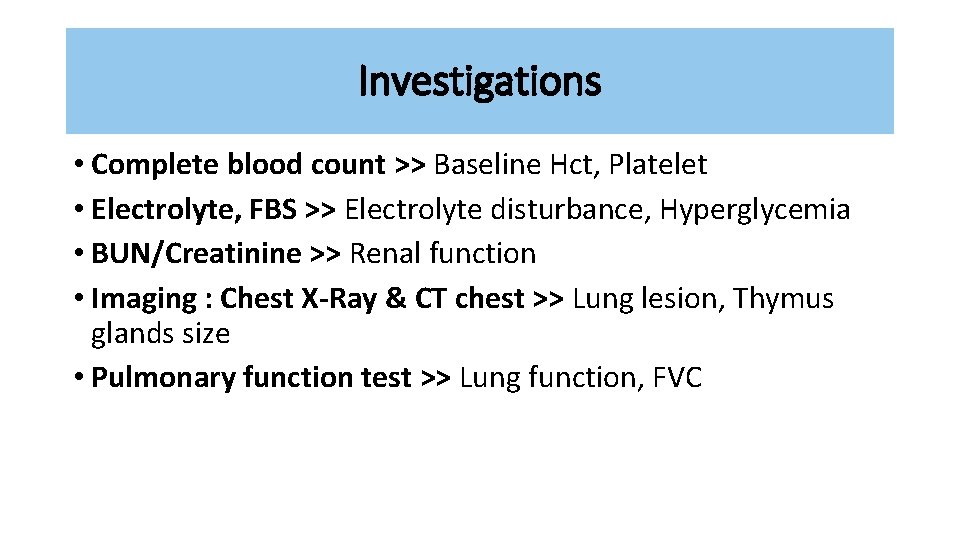
Investigations • Complete blood count >> Baseline Hct, Platelet • Electrolyte, FBS >> Electrolyte disturbance, Hyperglycemia • BUN/Creatinine >> Renal function • Imaging : Chest X-Ray & CT chest >> Lung lesion, Thymus glands size • Pulmonary function test >> Lung function, FVC
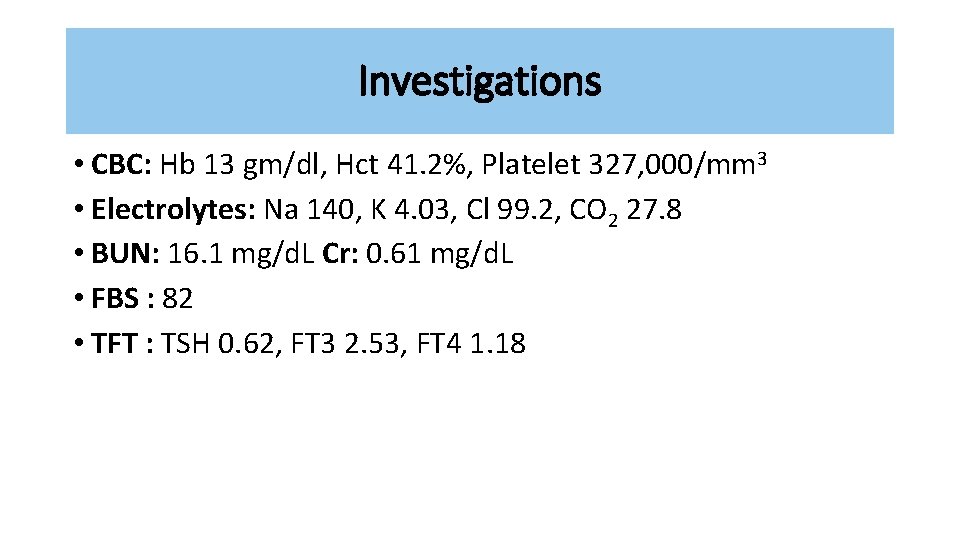
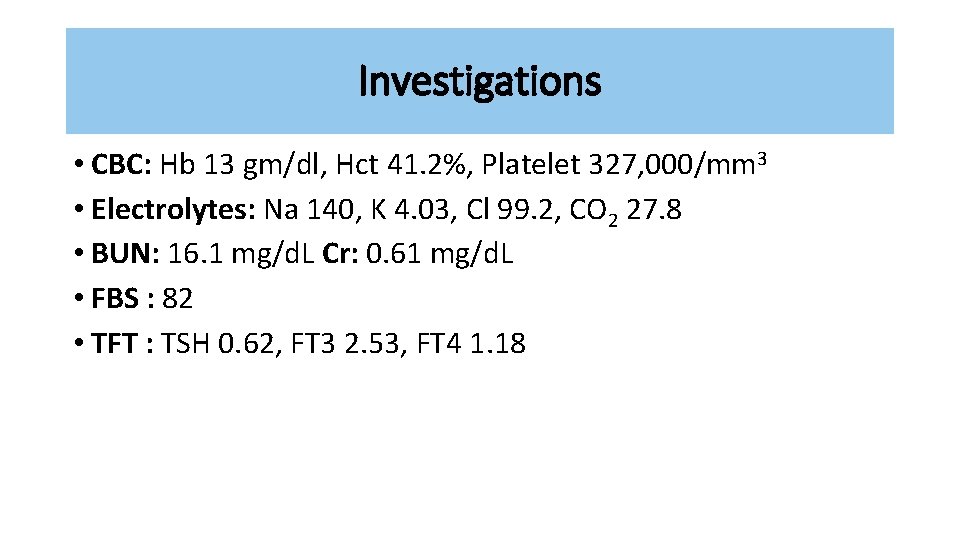
Investigations • CBC: Hb 13 gm/dl, Hct 41. 2%, Platelet 327, 000/mm 3 • Electrolytes: Na 140, K 4. 03, Cl 99. 2, CO 2 27. 8 • BUN: 16. 1 mg/d. L Cr: 0. 61 mg/d. L • FBS : 82 • TFT : TSH 0. 62, FT 3 2. 53, FT 4 1. 18
Investigations • CXR
Investigations • CT-Chest : • Thymus size 1. 2 x 2 cm. Otherwise are unremarkable
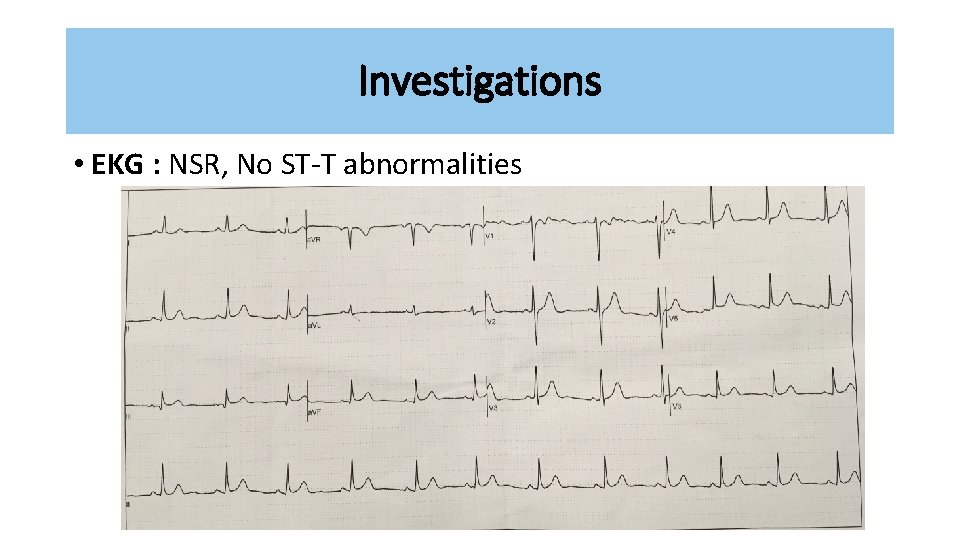
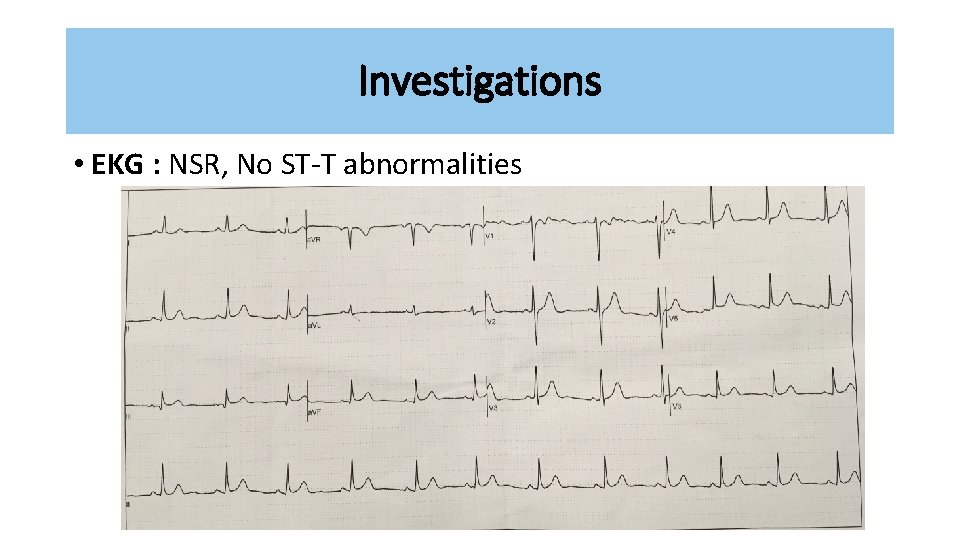
Investigations • EKG : NSR, No ST-T abnormalities
R 2 Problem list
Problem list • Female 20 years-old • Myasthenia gravis Class IIa • Secondary adrenal insufficiency
ASA classification ASA class II FC I
R 2 Preoperative evaluation
Preoperative evaluation Myasthenia gravis • Identify Associated diseases • Review of the severity of the patient’s disease and the treatment regimen
Preoperative evaluation Myasthenia gravis • Associated disease >> Autoimmune diseases • Thyroid abnormalities • Rheumatoid arthritis • SLE No associated • Pernicious anemia diseases
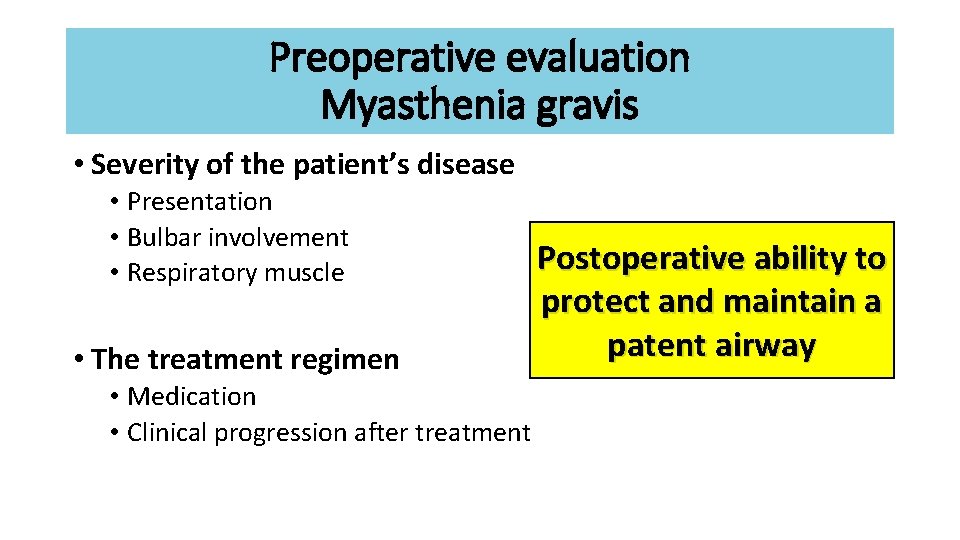
Preoperative evaluation Myasthenia gravis • Severity of the patient’s disease • Presentation • Bulbar involvement • Respiratory muscle • The treatment regimen • Medication • Clinical progression after treatment Postoperative ability to protect and maintain a patent airway
Preoperative evaluation Myasthenia gravis • Medical therapies for MG can be classified into three groups: • Anticholinesterase drugs : Pyridostigmine >> Mg/day • Immunosuppressive drugs : Corticosteroid >> Dose&duration • Short-term immunotherapies (plasmapheresis and immunoglobulin)
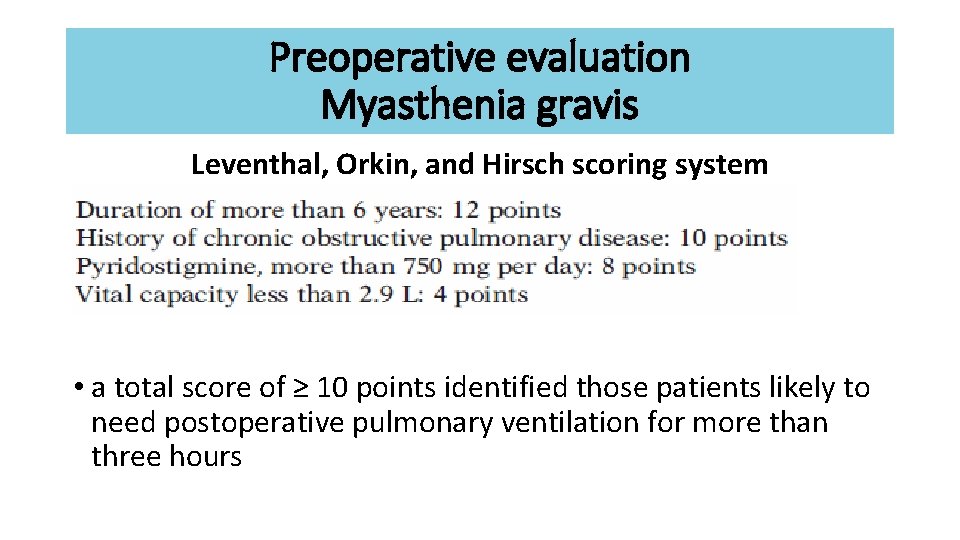
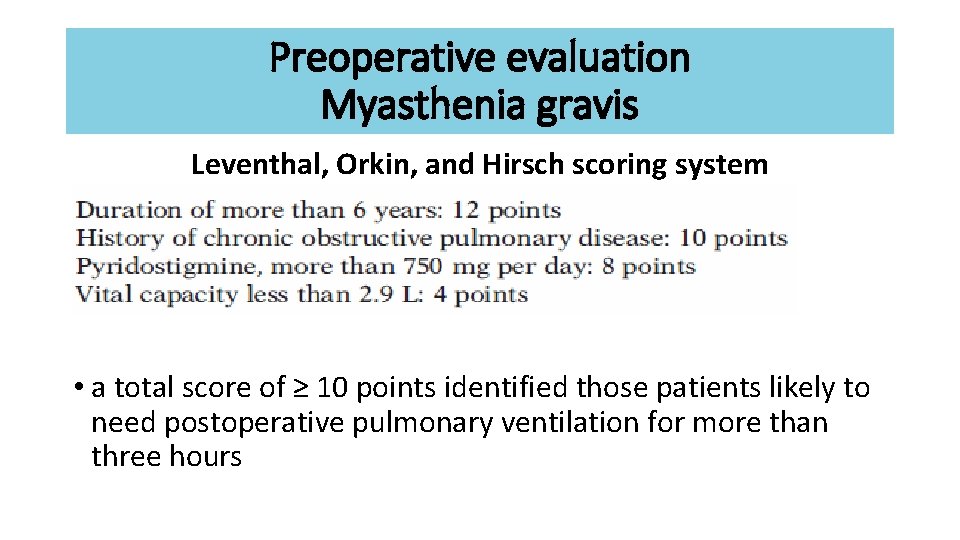
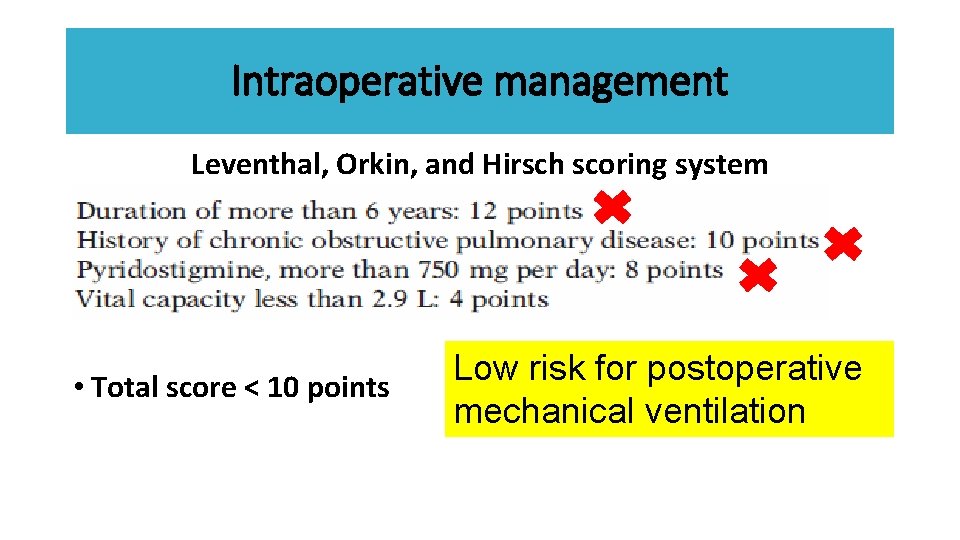
Preoperative evaluation Myasthenia gravis Leventhal, Orkin, and Hirsch scoring system • a total score of ≥ 10 points identified those patients likely to need postoperative pulmonary ventilation for more than three hours
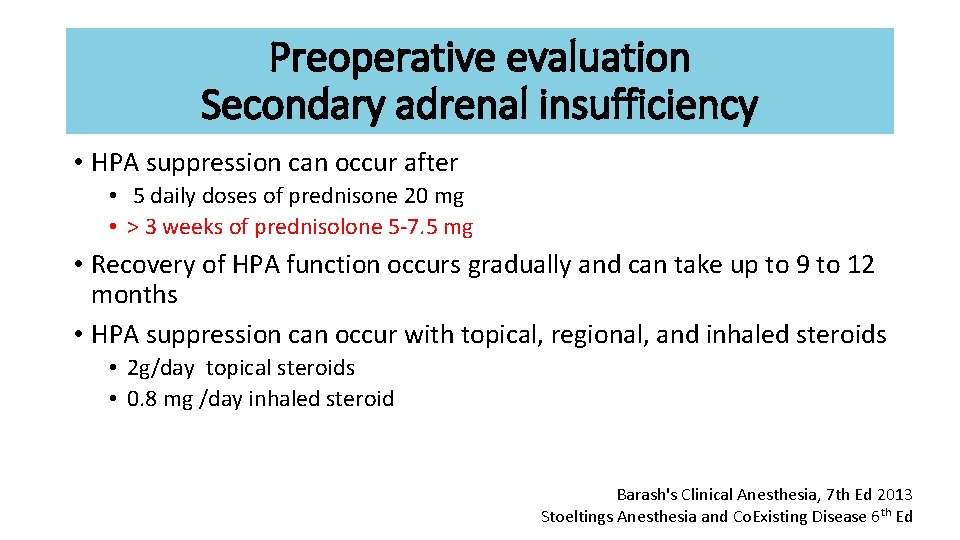
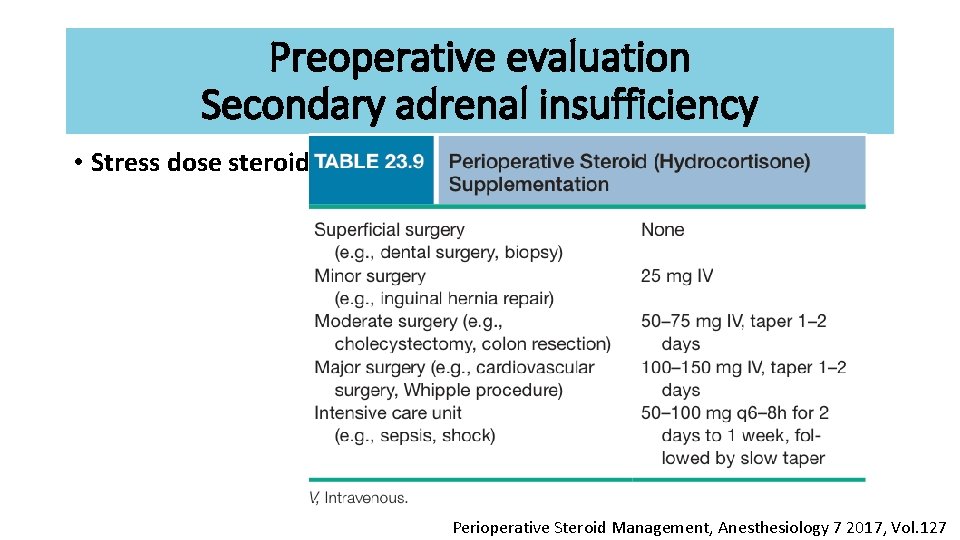
Preoperative evaluation Secondary adrenal insufficiency • HPA suppression can occur after • 5 daily doses of prednisone 20 mg • > 3 weeks of prednisolone 5 -7. 5 mg • Recovery of HPA function occurs gradually and can take up to 9 to 12 months • HPA suppression can occur with topical, regional, and inhaled steroids • 2 g/day topical steroids • 0. 8 mg /day inhaled steroid Barash's Clinical Anesthesia, 7 th Ed 2013 Stoeltings Anesthesia and Co. Existing Disease 6 th Ed
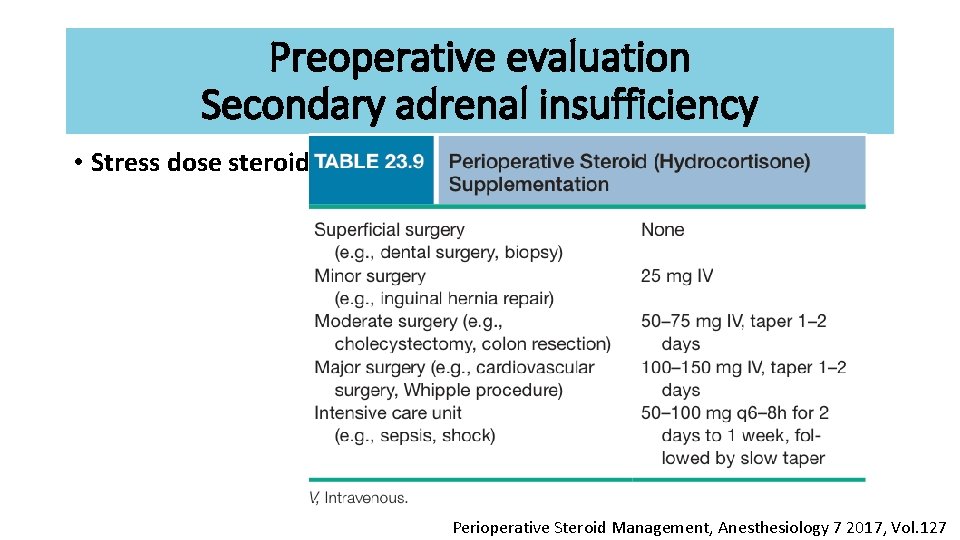
Preoperative evaluation Secondary adrenal insufficiency • Stress dose steroid Perioperative Steroid Management, Anesthesiology 7 2017, Vol. 127
Preparation & premedication • Advice risk of post-op intubation and mechanical ventilation • Breathing exercise & incentive spirometry • Set OR first case of day (ideally)
Preparation & premedication • Pre op anticholinesterase ? ? ? • Avoid drug interaction • Patient weakness before arrival operating room • Anxiolytic, sedative, and opioid • Increase sensitivity to respiratory depression
Preparation & premedication • • • NPO Inform consent 5%DN/2 1000 ml iv drip 80 ml /hr Hydrocortisone 100 mg iv G/M PRC 1 u ATB Warm iv fluid Large bore IV Force air warmer
R 3 Anesthetic consideration
Response to anesthetic drug • Inhaled Anesthetic Agents • More sensitive to neuromuscular depressant • Slightly greater than 1 MAC depresses (EMG) responses • Sevoflurane > concentration-dependent decrease in T 1 & T 4/T 1 • More effect of neuromuscular depressant in Baseline T 4/T 1 < 0. 9 Barash's Clinical Anesthesia, 7 th Ed 2013, 1065 -1068
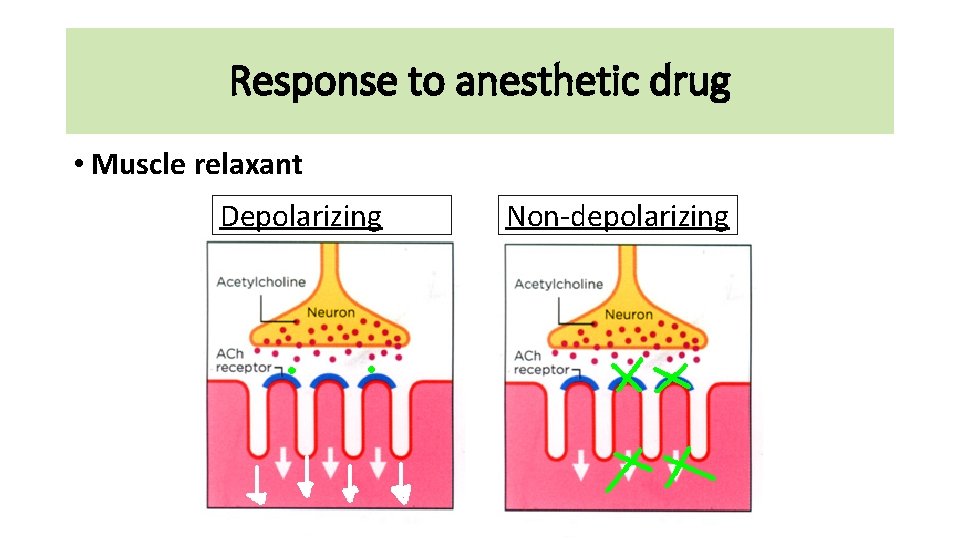
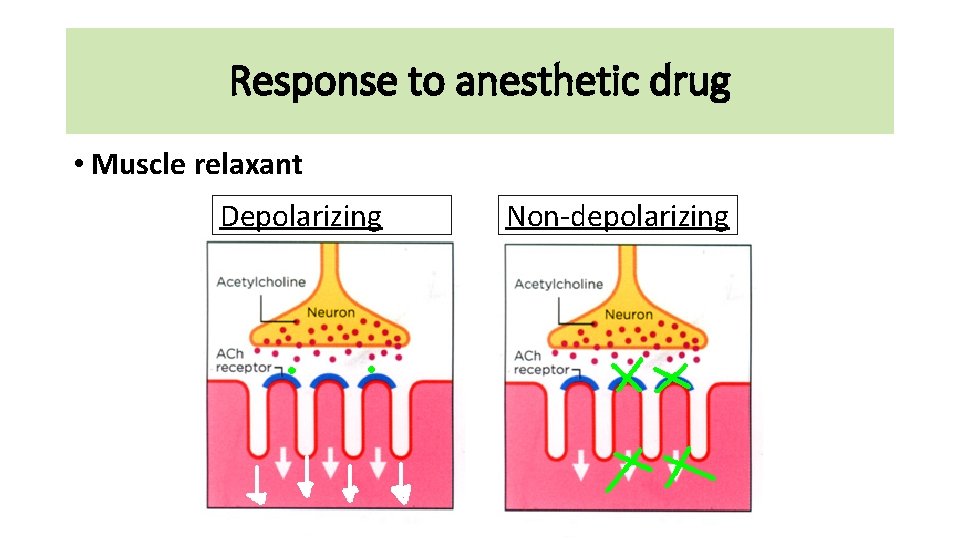
Response to anesthetic drug • Muscle relaxant Depolarizing Non-depolarizing
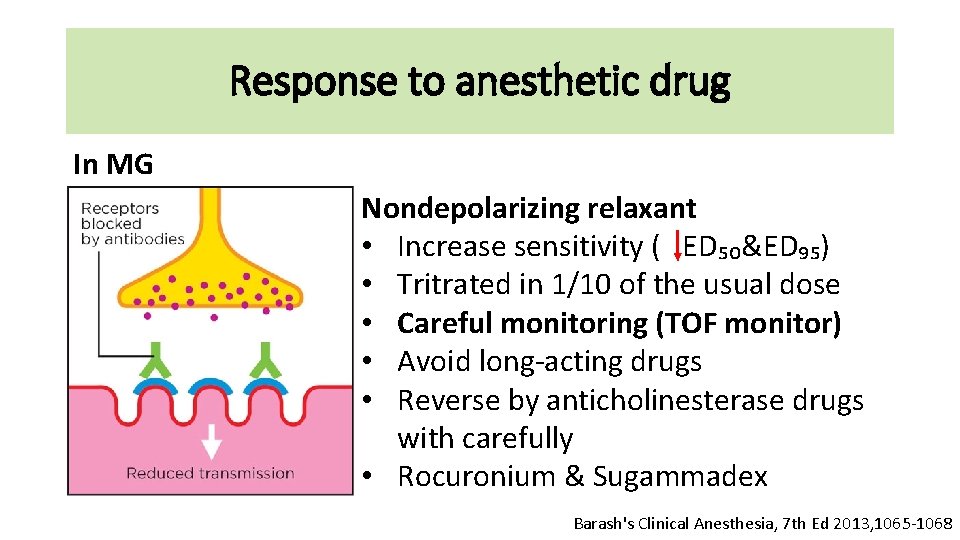
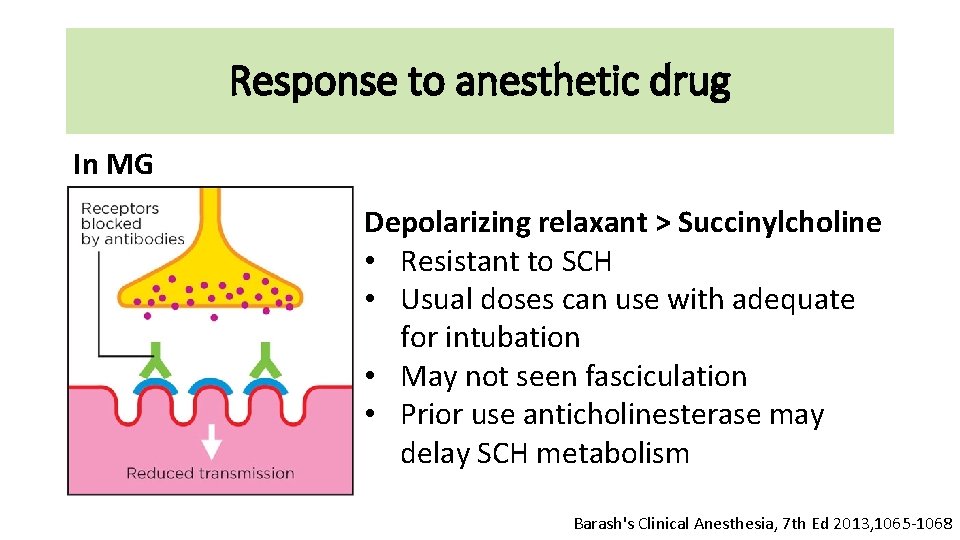
Response to anesthetic drug In MG Nondepolarizing relaxant • Increase sensitivity ( ED₅₀&ED₉₅) • Tritrated in 1/10 of the usual dose • Careful monitoring (TOF monitor) • Avoid long-acting drugs • Reverse by anticholinesterase drugs with carefully • Rocuronium & Sugammadex Barash's Clinical Anesthesia, 7 th Ed 2013, 1065 -1068
Response to anesthetic drug In MG Depolarizing relaxant > Succinylcholine • Resistant to SCH • Usual doses can use with adequate for intubation • May not seen fasciculation • Prior use anticholinesterase may delay SCH metabolism Barash's Clinical Anesthesia, 7 th Ed 2013, 1065 -1068
Response to anesthetic drug • Opioids • At therapeutic range not effect neuromuscular transmission • Central respiratory depression • Short acting opioid c titrate dose • IV anesthetics • barbiturates and propofol are safely use for myasthenic patients • Propofol has theoretic advantages of short duration of action without effect on neuromuscular transmission Barash's Clinical Anesthesia, 7 th Ed 2013, 1065 -1068

Intraoperative management
Choice of anesthesia • GA with ETT with control ventilation • Combine with Thoracic epidural
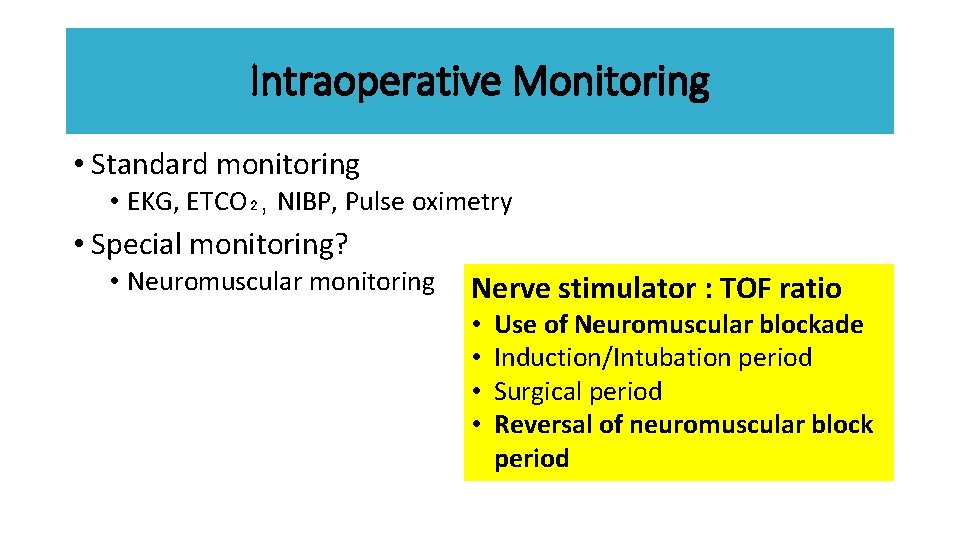
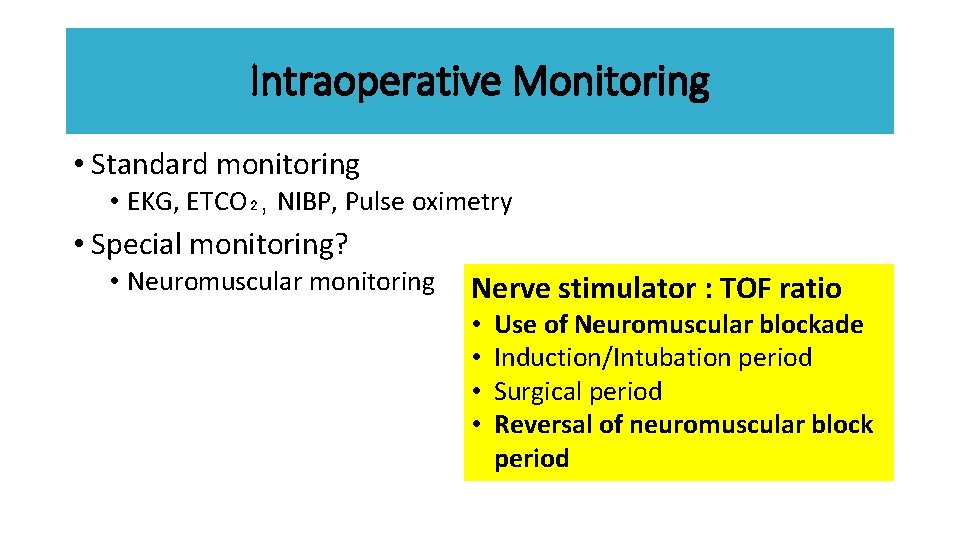
Intraoperative Monitoring • Standard monitoring • EKG, ETCO₂, NIBP, Pulse oximetry • Special monitoring? • Neuromuscular monitoring Nerve stimulator : TOF ratio • • Use of Neuromuscular blockade Induction/Intubation period Surgical period Reversal of neuromuscular block period

Induction & intubation • IV induction vs Inhalation induction • Muscle relaxant • SCH • Non depolarizing neuromuscular blockers • Avoid long acting • Non muscle relaxant technique
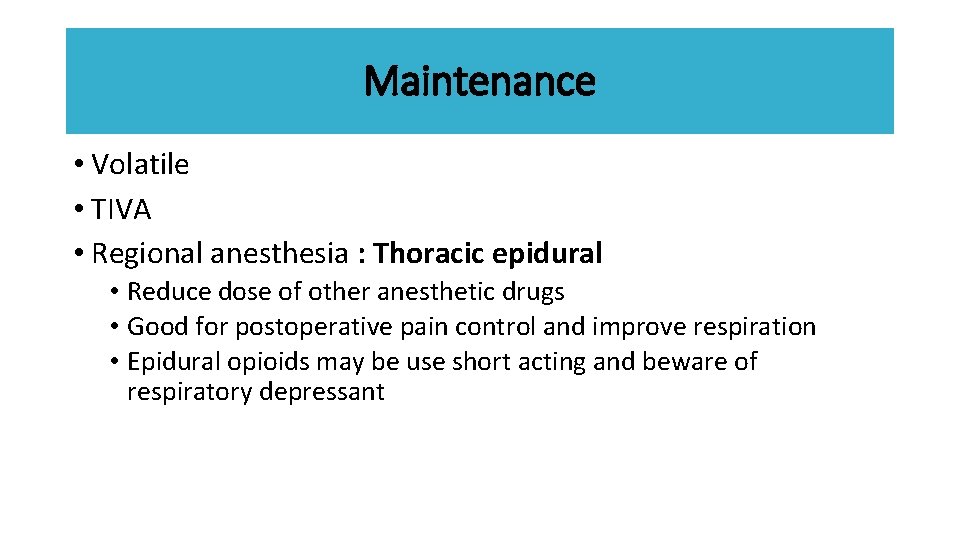
Maintenance • Volatile • TIVA • Regional anesthesia : Thoracic epidural • Reduce dose of other anesthetic drugs • Good for postoperative pain control and improve respiration • Epidural opioids may be use short acting and beware of respiratory depressant
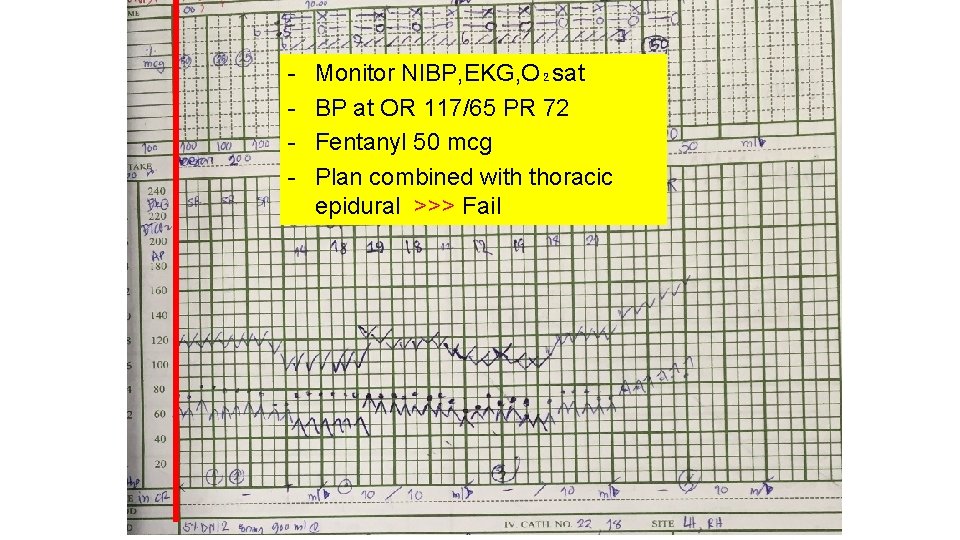
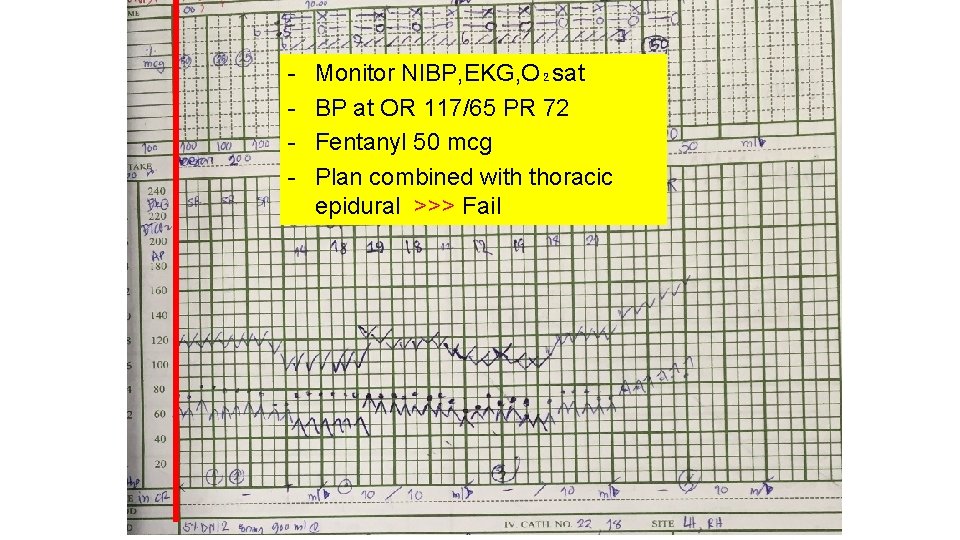
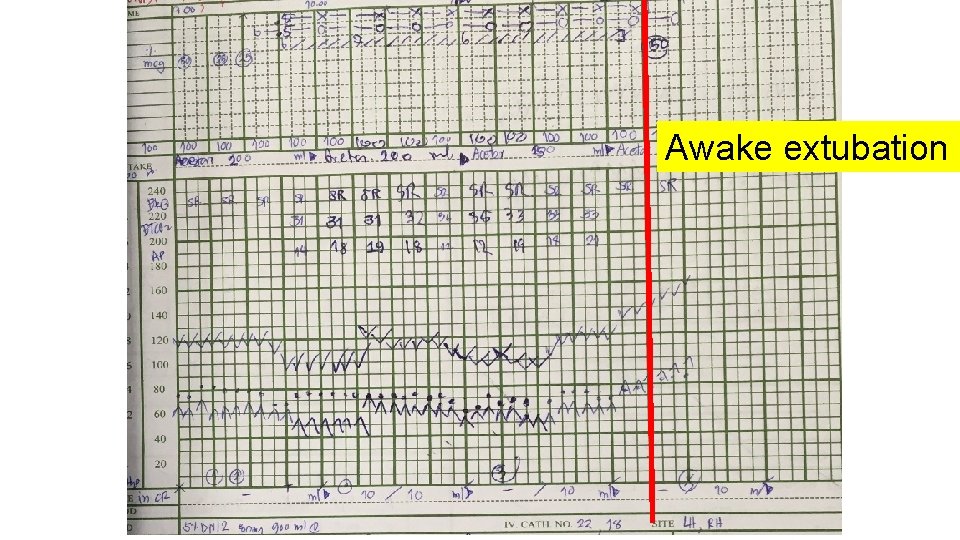
- Monitor NIBP, EKG, O₂sat BP at OR 117/65 PR 72 Fentanyl 50 mcg Plan combined with thoracic epidural >>> Fail
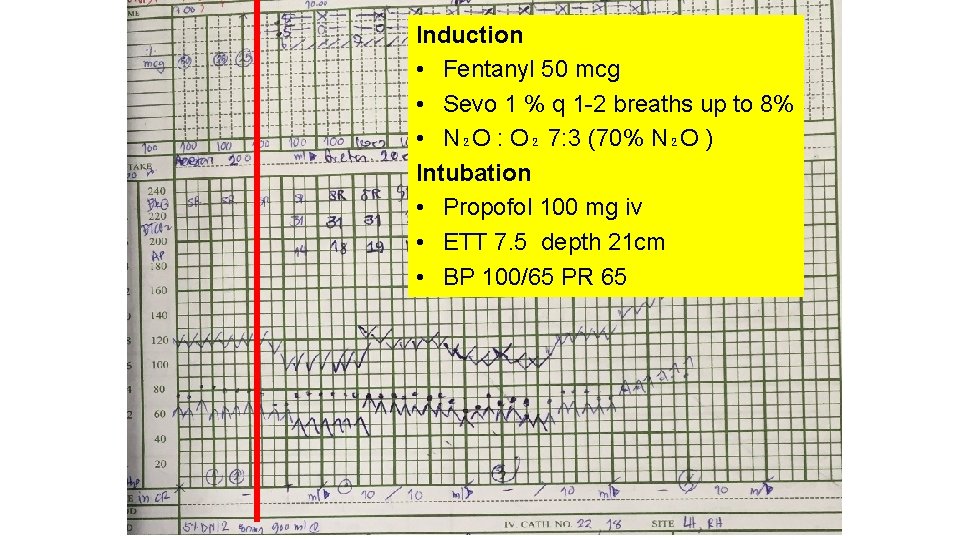
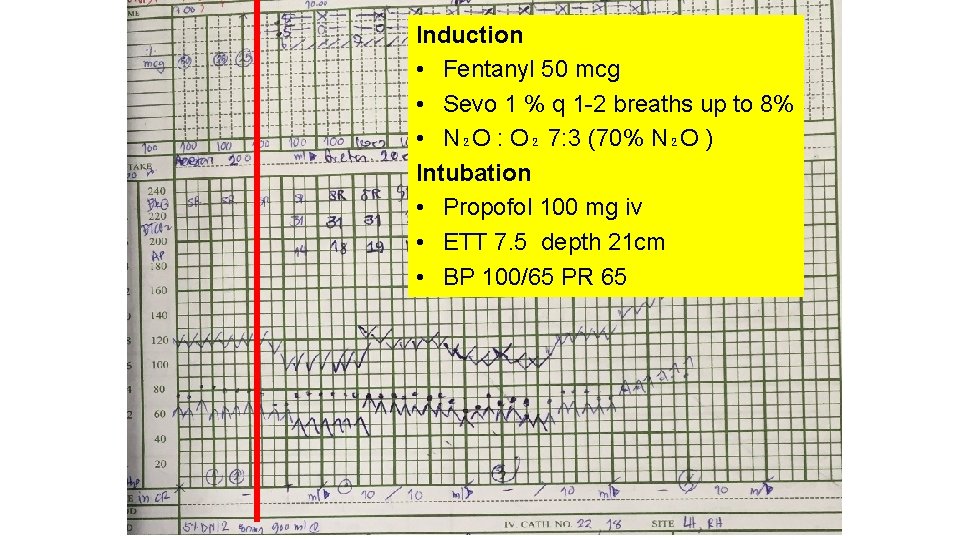
Induction • Fentanyl 50 mcg • Sevo 1 % q 1 -2 breaths up to 8% • N₂O : O₂ 7: 3 (70% N₂O ) Intubation • Propofol 100 mg iv • ETT 7. 5 depth 21 cm • BP 100/65 PR 65
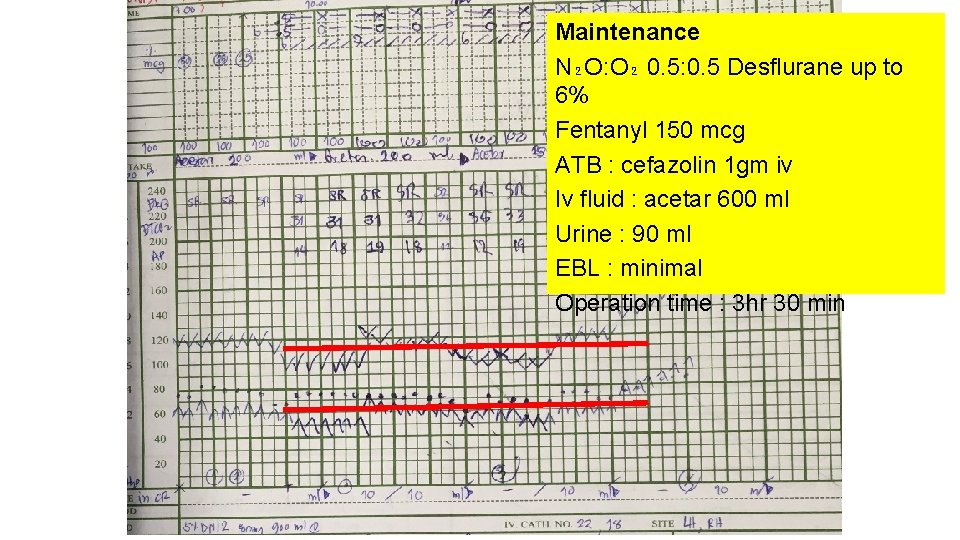
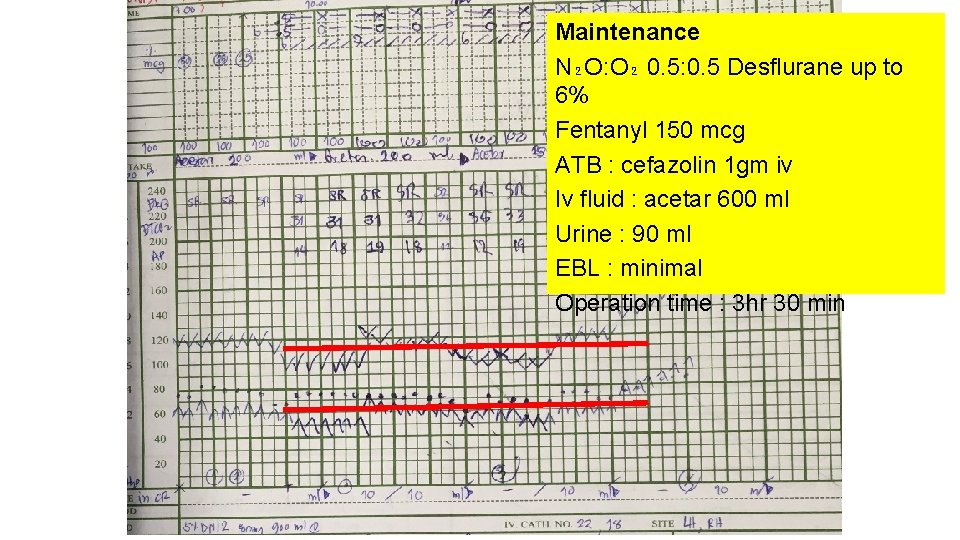
Maintenance N₂O: O₂ 0. 5: 0. 5 Desflurane up to 6% Fentanyl 150 mcg ATB : cefazolin 1 gm iv Iv fluid : acetar 600 ml Urine : 90 ml EBL : minimal Operation time : 3 hr 30 min
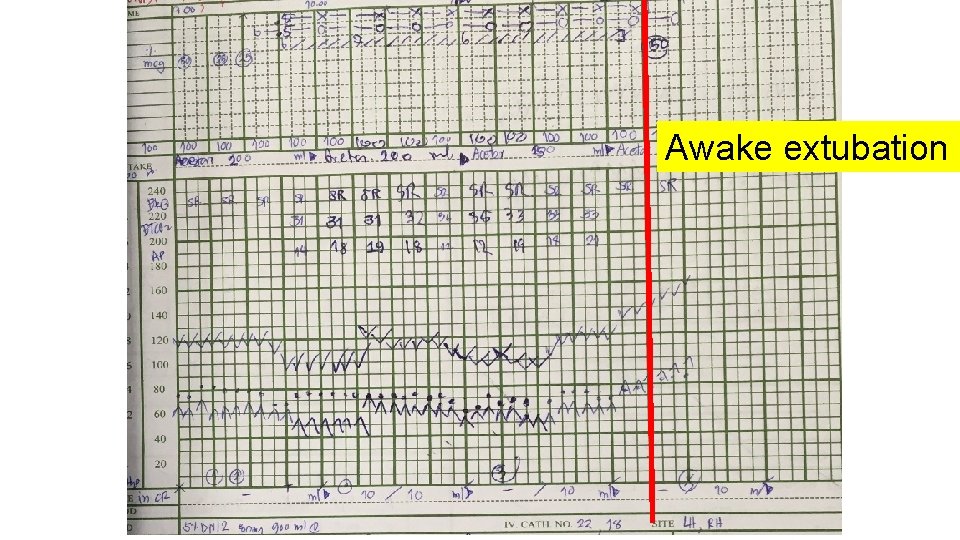
Awake extubation
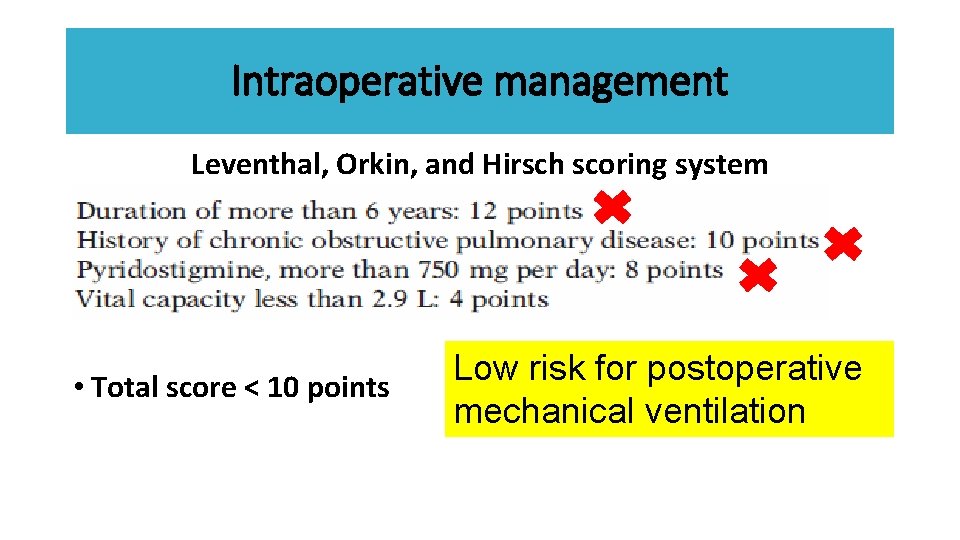
Intraoperative management Leventhal, Orkin, and Hirsch scoring system • Total score < 10 points Low risk for postoperative mechanical ventilation
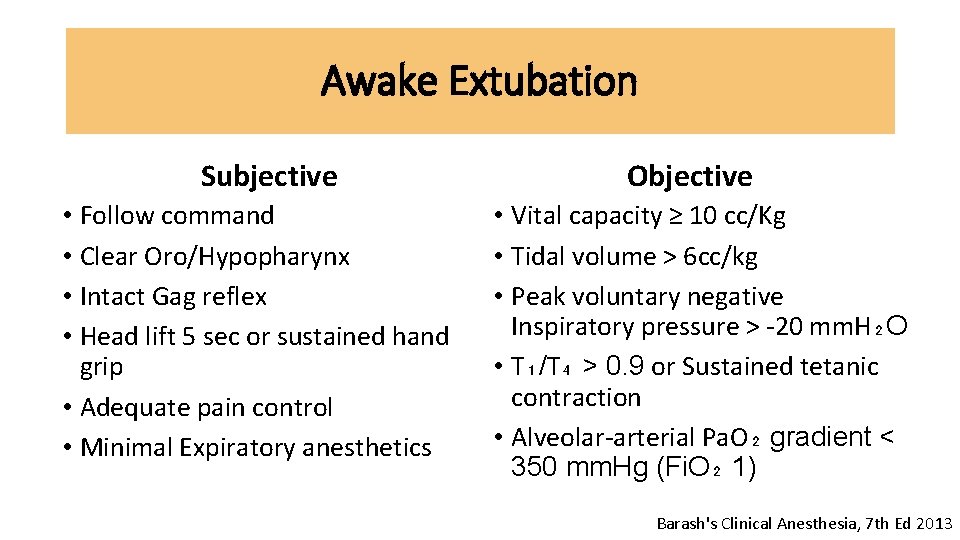
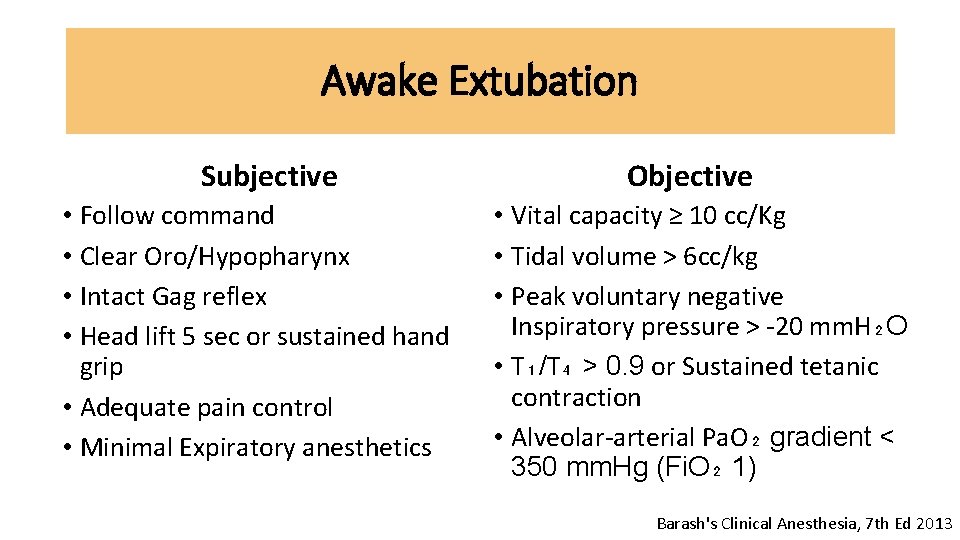
Awake Extubation Subjective • Follow command • Clear Oro/Hypopharynx • Intact Gag reflex • Head lift 5 sec or sustained hand grip • Adequate pain control • Minimal Expiratory anesthetics Objective • Vital capacity ≥ 10 cc/Kg • Tidal volume > 6 cc/kg • Peak voluntary negative Inspiratory pressure > -20 mm. H₂O • T₁/T₄ > 0. 9 or Sustained tetanic contraction • Alveolar-arterial Pa. O₂ gradient < 350 mm. Hg (Fi. O₂ 1) Barash's Clinical Anesthesia, 7 th Ed 2013
Post operative period • Need for postoperative mechanical ventilation • Adequate pain control • Pulmonary toilet
Post operative weakness • Myasthenic crisis • Cholinergic crisis • Residual effects of anesthetic drugs
Cholinergic crisis • Cholinergic crisis results from an excess of cholinesterase inhibitors • flaccid muscle paralysis • Miosis • SLUDGE syndrome (salivation, lacrimation, urinary incontinence, diarrhoea, GI upset and hypermotility, emesis)
Myasthenic crisis • Facial muscles may be slack, and the face may be expressionless • Inability to support the head, which will fall onto the chest while the patient is seated • Gag reflex is often absent, and such patients are at risk for aspiration of oral secretions • bronchospasm with wheezing, bronchorrhea, respiratory failure, diaphoresis, and cyanosis

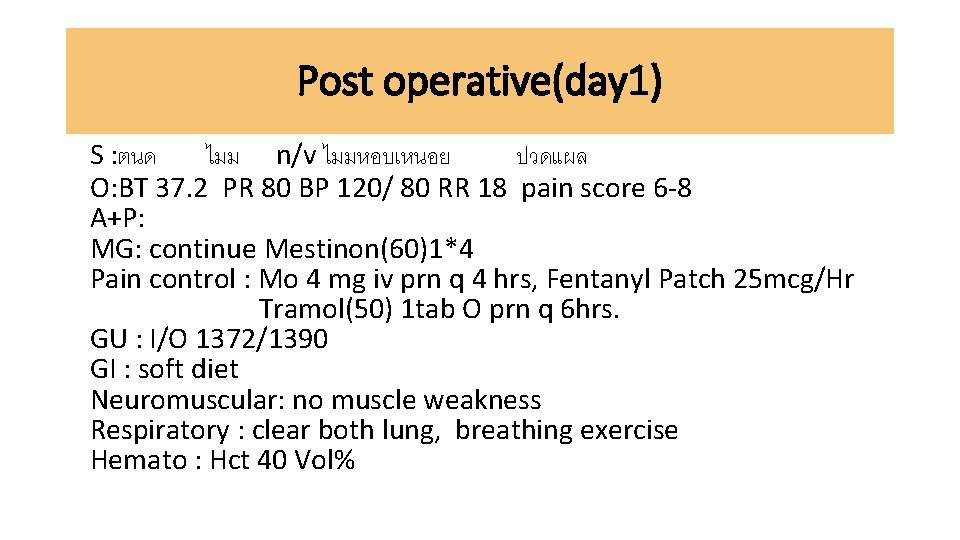
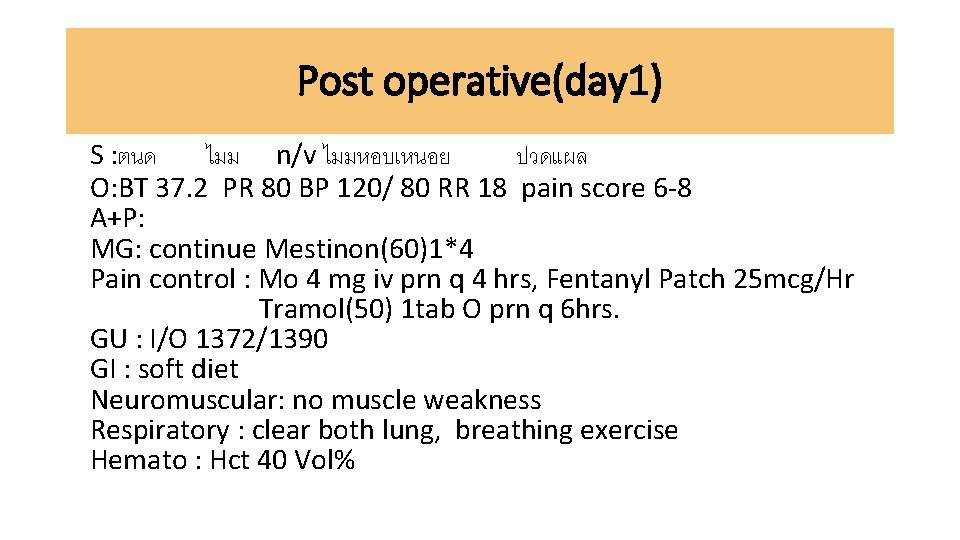
Post operative(day 1) S : ตนด ไมม n/v ไมมหอบเหนอย ปวดแผล O: BT 37. 2 PR 80 BP 120/ 80 RR 18 pain score 6 -8 A+P: MG: continue Mestinon(60)1*4 Pain control : Mo 4 mg iv prn q 4 hrs, Fentanyl Patch 25 mcg/Hr Tramol(50) 1 tab O prn q 6 hrs. GU : I/O 1372/1390 GI : soft diet Neuromuscular: no muscle weakness Respiratory : clear both lung, breathing exercise Hemato : Hct 40 Vol%
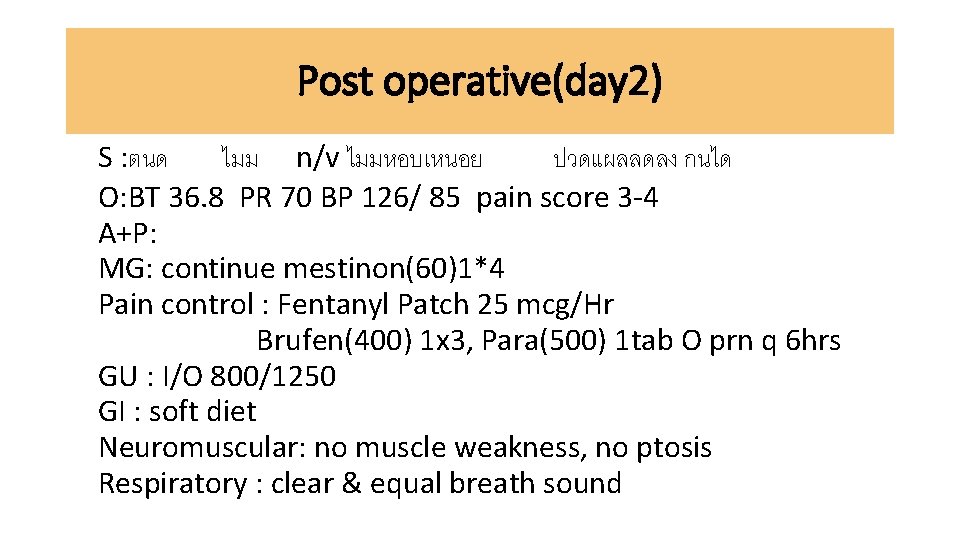
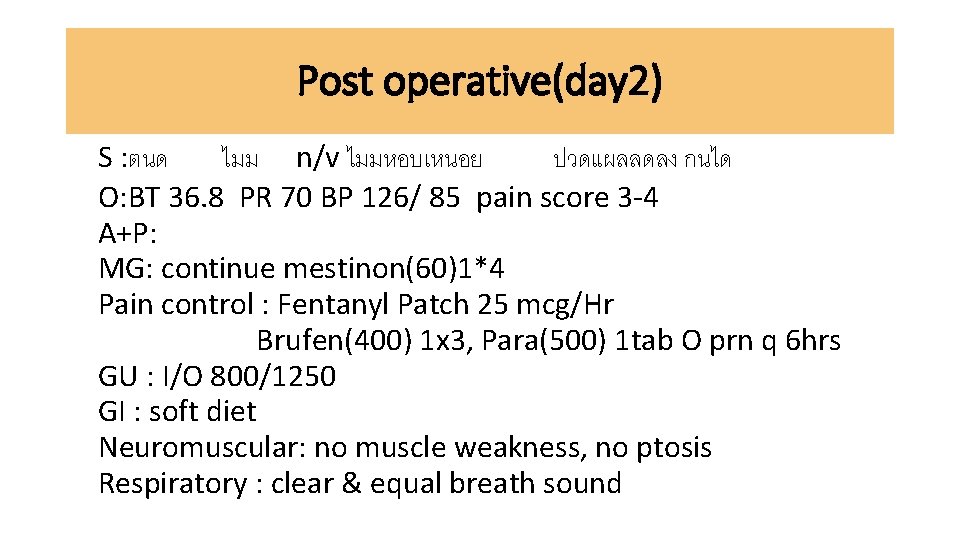
Post operative(day 2) S : ตนด ไมม n/v ไมมหอบเหนอย ปวดแผลลดลง กนได O: BT 36. 8 PR 70 BP 126/ 85 pain score 3 -4 A+P: MG: continue mestinon(60)1*4 Pain control : Fentanyl Patch 25 mcg/Hr Brufen(400) 1 x 3, Para(500) 1 tab O prn q 6 hrs GU : I/O 800/1250 GI : soft diet Neuromuscular: no muscle weakness, no ptosis Respiratory : clear & equal breath sound
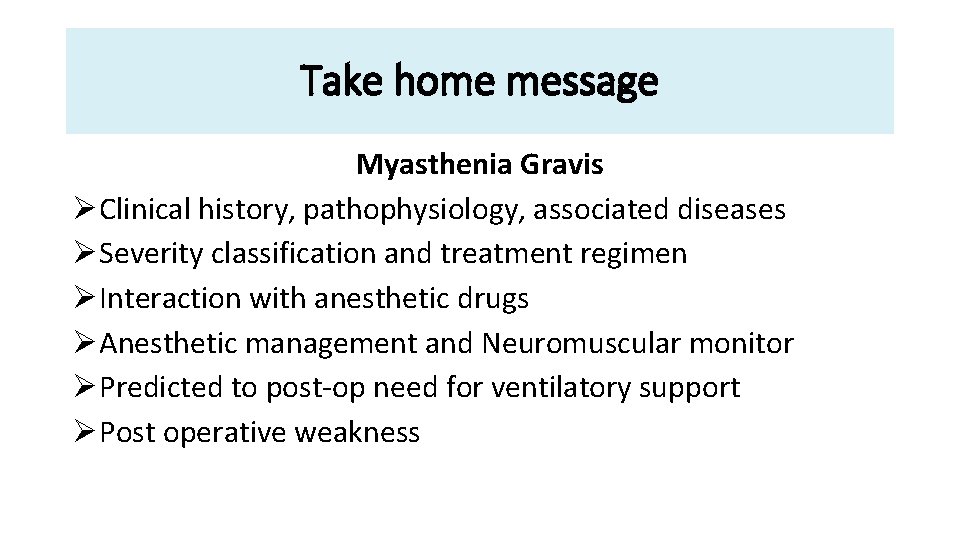
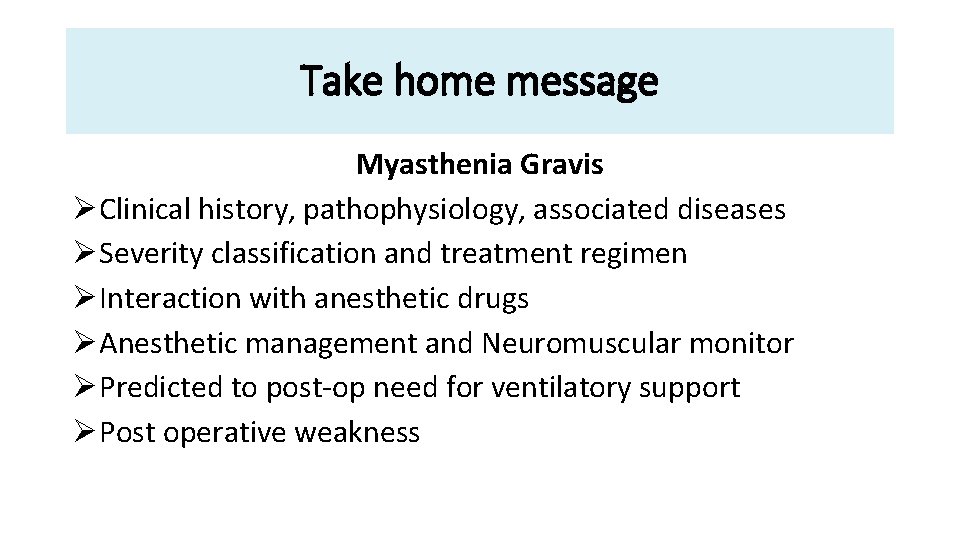
Take home message Myasthenia Gravis ØClinical history, pathophysiology, associated diseases ØSeverity classification and treatment regimen ØInteraction with anesthetic drugs ØAnesthetic management and Neuromuscular monitor ØPredicted to post-op need for ventilatory support ØPost operative weakness

THANK YOU
 Disease modifying antirheumatic drugs
Disease modifying antirheumatic drugs Communicable disease and non communicable disease
Communicable disease and non communicable disease Threshold theory bilingualism
Threshold theory bilingualism Underlying theory in research
Underlying theory in research Impelism
Impelism Ter thin client
Ter thin client Underlying magic pitch deck examples
Underlying magic pitch deck examples Derivatives week
Derivatives week The underlying theme of the conceptual framework is
The underlying theme of the conceptual framework is Underlying causes of ww1
Underlying causes of ww1 Powder keg of europe ww1
Powder keg of europe ww1 Ww1 cause
Ww1 cause Basic mechanisms underlying seizures and epilepsy
Basic mechanisms underlying seizures and epilepsy Underlying technology
Underlying technology Underlying undirected graph
Underlying undirected graph Underlying technology
Underlying technology Bryanna and charles are in a dancing competition
Bryanna and charles are in a dancing competition Underlying assumptions of ai
Underlying assumptions of ai Underlying network
Underlying network Underlying magic pitch deck
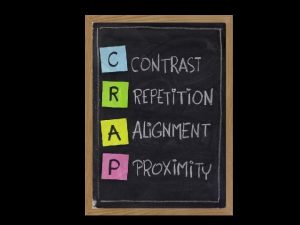
Underlying magic pitch deck Underlying design
Underlying design Underlying magic slide
Underlying magic slide Physics color wheel
Physics color wheel Assumptions of conceptual framework
Assumptions of conceptual framework Underlying magic
Underlying magic Conceptual framework underlying financial accounting
Conceptual framework underlying financial accounting History of performance enhancing drugs
History of performance enhancing drugs Natural history of disease adalah
Natural history of disease adalah Prepathogenesis phase
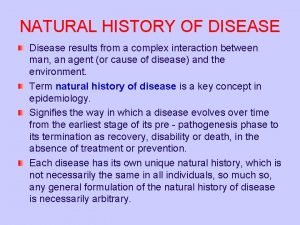
Prepathogenesis phase Natural history of disease
Natural history of disease Natural history of disease is best studied by
Natural history of disease is best studied by Natural history and spectrum of disease
Natural history and spectrum of disease Manifestational criteria
Manifestational criteria Spectrum of disease meaning
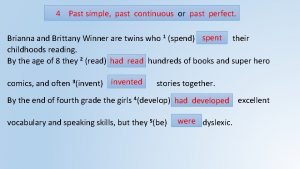
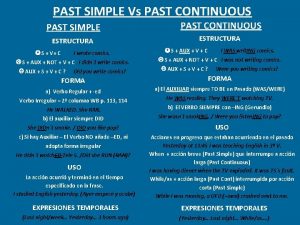
Spectrum of disease meaning Past simple vs past continuous vs past perfect exercises
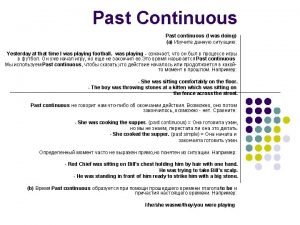
Past simple vs past continuous vs past perfect exercises Past continuous past perfect
Past continuous past perfect Past simple past continuous past perfect timeline
Past simple past continuous past perfect timeline Past continuous past simple past perfect
Past continuous past simple past perfect Llll progressive form
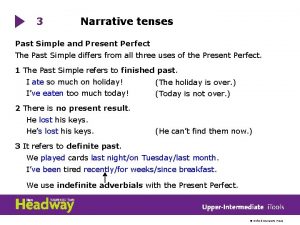
Llll progressive form Narrative tenses past simple
Narrative tenses past simple Past simple continuous
Past simple continuous E past continuous
E past continuous Past narrative tenses
Past narrative tenses Simple past vs present perfect
Simple past vs present perfect Also history physical
Also history physical Past medical history
Past medical history Ib history ib exam questions
Ib history ib exam questions History edexcel igcse past papers
History edexcel igcse past papers Edexcel gcse history crime and punishment exam questions
Edexcel gcse history crime and punishment exam questions Past medical history
Past medical history Past medical history
Past medical history Aqa a level history tudors past papers
Aqa a level history tudors past papers Ccna drugs
Ccna drugs Schedule 1 drugs
Schedule 1 drugs Antithyroid drugs classification
Antithyroid drugs classification Anistreplase
Anistreplase Fibrinolytic agents
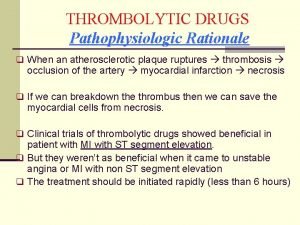
Fibrinolytic agents Thrombolytic drugs
Thrombolytic drugs Thrombolytic drugs mechanism of action
Thrombolytic drugs mechanism of action Fibrinolytic drugs
Fibrinolytic drugs British model involved with drugs
British model involved with drugs Sympathomimetic agents
Sympathomimetic agents Sar of cholinergic drugs
Sar of cholinergic drugs