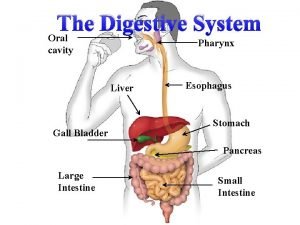
Pancreas gland Pancreases pancreas is a glandular organ






- Slides: 37

Pancreas gland
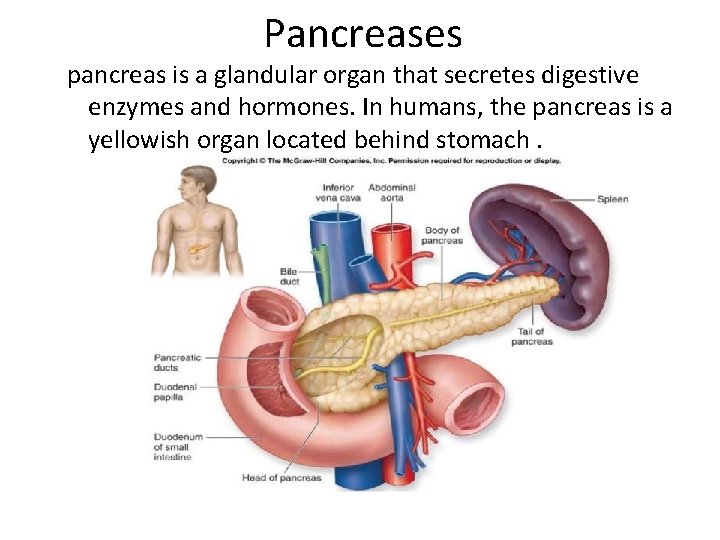
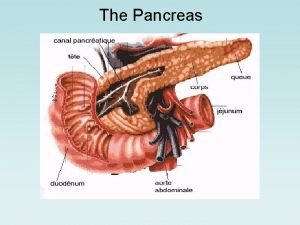
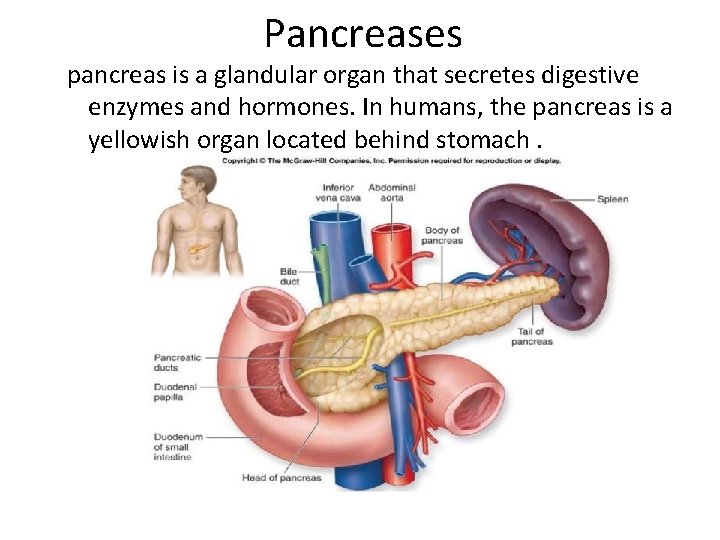
Pancreases pancreas is a glandular organ that secretes digestive enzymes and hormones. In humans, the pancreas is a yellowish organ located behind stomach.
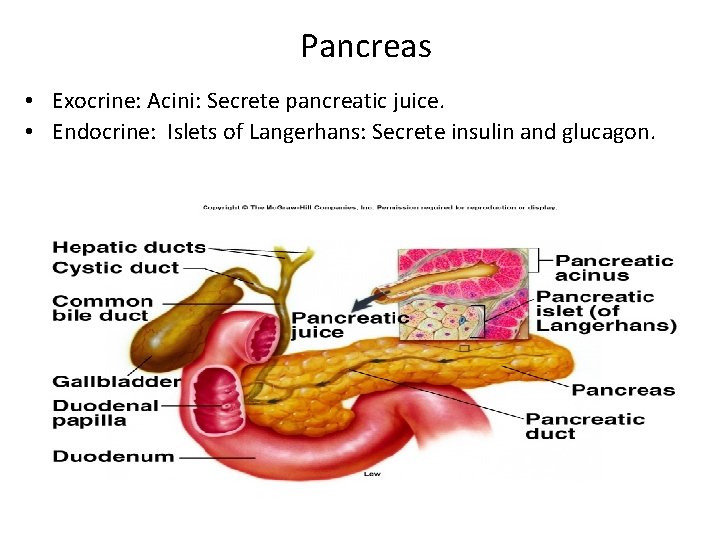
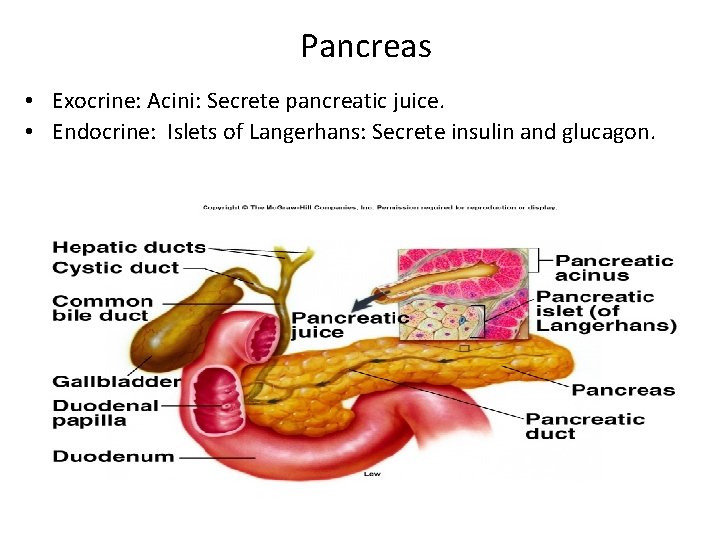
Pancreas • Exocrine: Acini: Secrete pancreatic juice. • Endocrine: Islets of Langerhans: Secrete insulin and glucagon.
The Endocrine Pancreas • • • Approximately 5 percent of the total pancreatic mass is comprised of endocrine cells. These endocrine cells are clustered in groups within the pancreas which look like little islands of cells when examined under a microscope. This appearance led to these groups of pancreatic endocrine cells being called "Pancreatic Islets“ or “islets of langerhans”. Within pancreatic islets are cells which make specific pancreatic endocrine hormones, of which there are only a few (the most famous of course being insulin). These cells within the islets are called "Pancreatic Islet Cells".
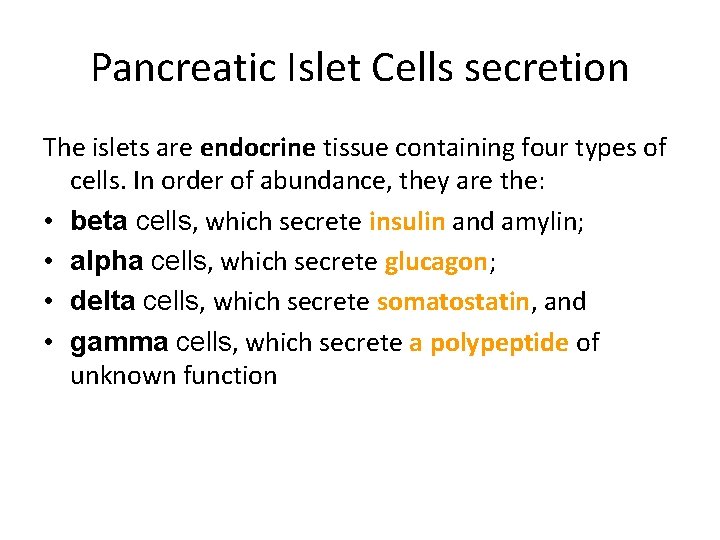
Pancreatic Islet Cells secretion The islets are endocrine tissue containing four types of cells. In order of abundance, they are the: • beta cells, which secrete insulin and amylin; • alpha cells, which secrete glucagon; • delta cells, which secrete somatostatin, and • gamma cells, which secrete a polypeptide of unknown function
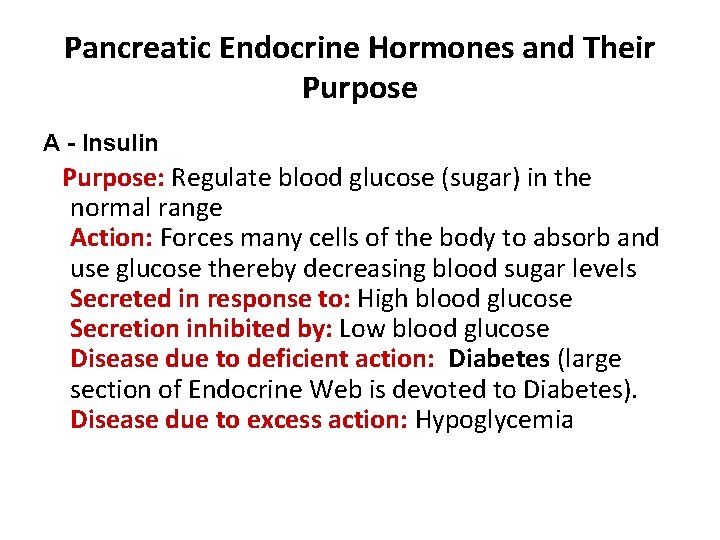
Pancreatic Endocrine Hormones and Their Purpose A - Insulin Purpose: Regulate blood glucose (sugar) in the normal range Action: Forces many cells of the body to absorb and use glucose thereby decreasing blood sugar levels Secreted in response to: High blood glucose Secretion inhibited by: Low blood glucose Disease due to deficient action: Diabetes (large section of Endocrine Web is devoted to Diabetes). Disease due to excess action: Hypoglycemia
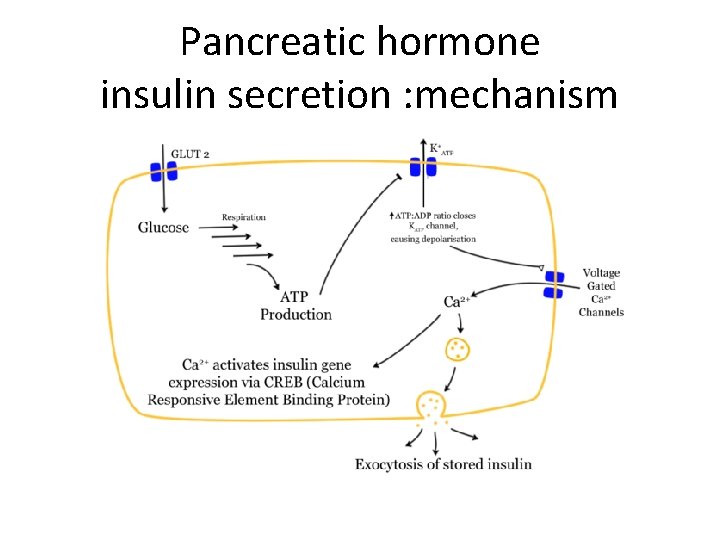
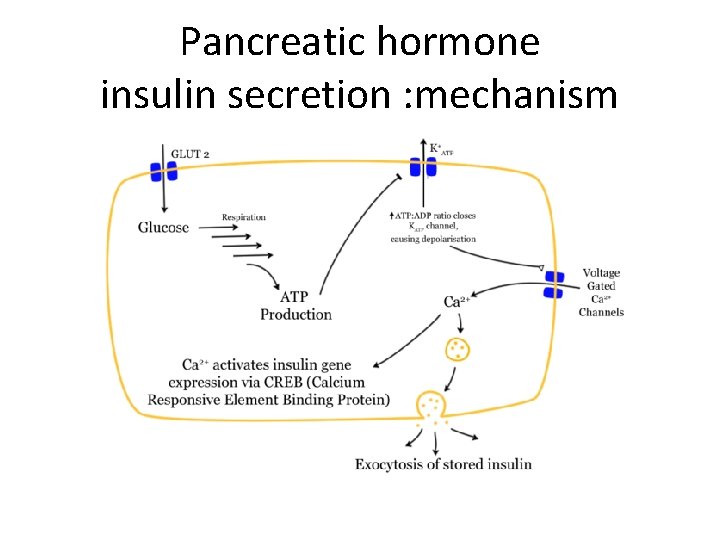
Pancreatic hormone insulin secretion : mechanism
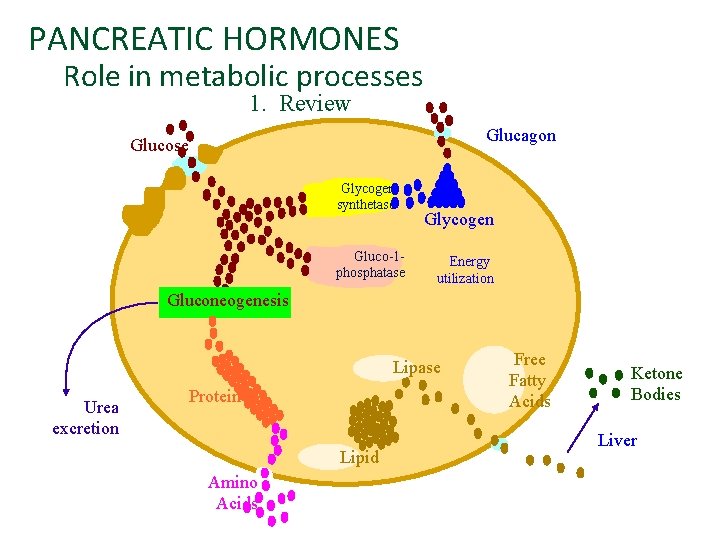
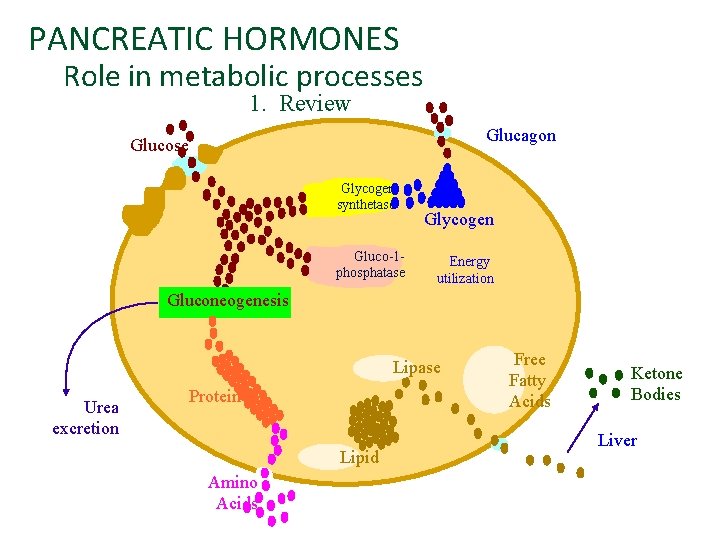
PANCREATIC HORMONES Role in metabolic processes 1. Review Glucagon Glucose Glycogen synthetase R Gluco-1 phosphatase Glycogen Energy utilization Gluconeogenesis Lipase Urea excretion Protein Lipid Amino Acids Free Fatty Acids Ketone Bodies Liver
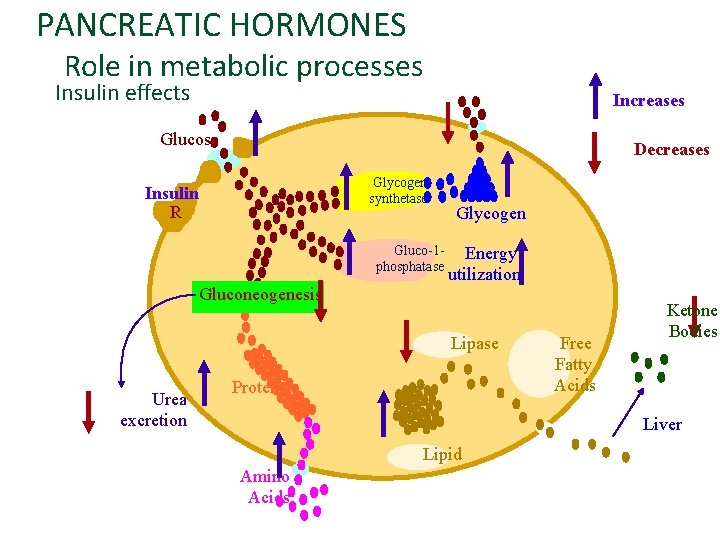
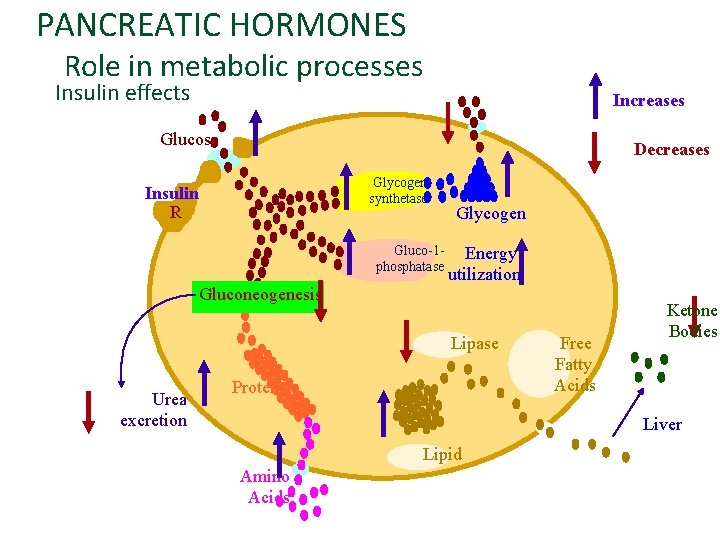
PANCREATIC HORMONES Role in metabolic processes Insulin effects Increases Glucose Decreases Glycogen synthetase Insulin R Gluco-1 phosphatase Glycogen Energy utilization Gluconeogenesis Lipase Urea excretion Protein Free Fatty Acids Ketone Bodies Liver Lipid Amino Acids
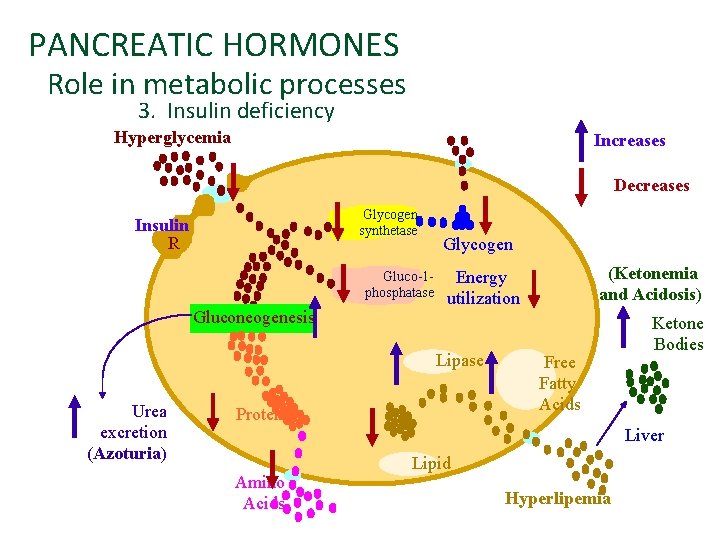
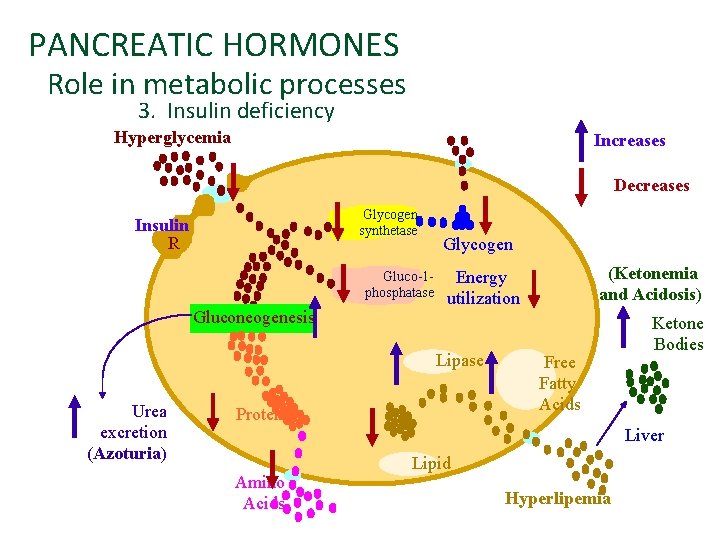
PANCREATIC HORMONES Role in metabolic processes 3. Insulin deficiency Hyperglycemia Increases Decreases Glycogen synthetase Insulin R Gluco-1 phosphatase Gluconeogenesis Glycogen Lipase Urea excretion (Azoturia) (Ketonemia and Acidosis) Energy utilization Protein Free Fatty Acids Ketone Bodies Liver Amino Acids Lipid Hyperlipemia

Pancreatic Endocrine Hormones and Their Purpose B - Glucagon Purpose: Assist insulin in regulating blood glucose (sugar) in the normal range (actions are opposite of insulin) Action: Forces many cells of the body to release (or produce) glucose (increasing blood sugar) Secreted in response to: Low blood glucose Secretion inhibited by: High blood glucose Disease due to deficient action: Some times nothing, sometimes hypoglycemia Disease due to excess action: Hyperglycemia
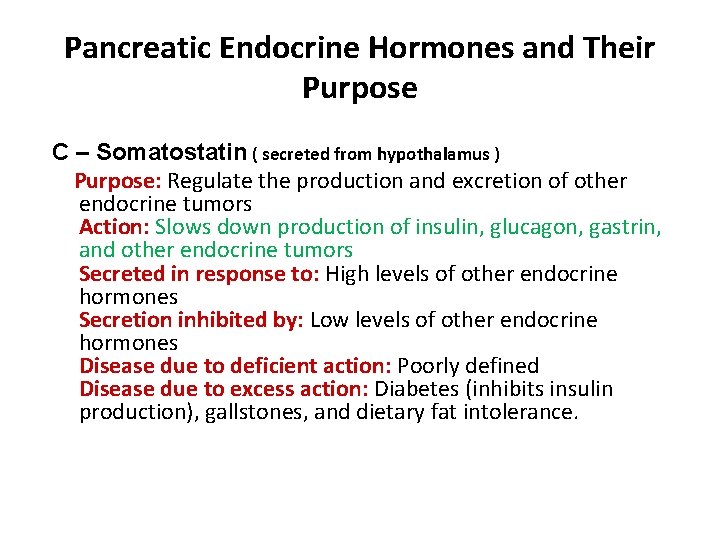
Pancreatic Endocrine Hormones and Their Purpose C – Somatostatin ( secreted from hypothalamus ) Purpose: Regulate the production and excretion of other endocrine tumors Action: Slows down production of insulin, glucagon, gastrin, and other endocrine tumors Secreted in response to: High levels of other endocrine hormones Secretion inhibited by: Low levels of other endocrine hormones Disease due to deficient action: Poorly defined Disease due to excess action: Diabetes (inhibits insulin production), gallstones, and dietary fat intolerance.
Pancreatic Endocrine Hormones and Their Purpose E - Vasoactive Intestinal Peptide (VIP) Purpose: Help control water secretion and absorption from the intestines Action: Causes intestinal sells to secrete water and salts into the intestines (inhibit absorption) Disease due to excess action: Severe watery diarrhea and salt (potassium) imbalances
Pancreatic secretions • The pancreas acts as an exocrine gland by producing pancreatic juice which empties into the small intestine via a duct. It plays an important role • in digestion of lipids proteins and carbohydrates. • in neutralizing the p. H to become suitable for the action of the pancreatic digestive enzymes.

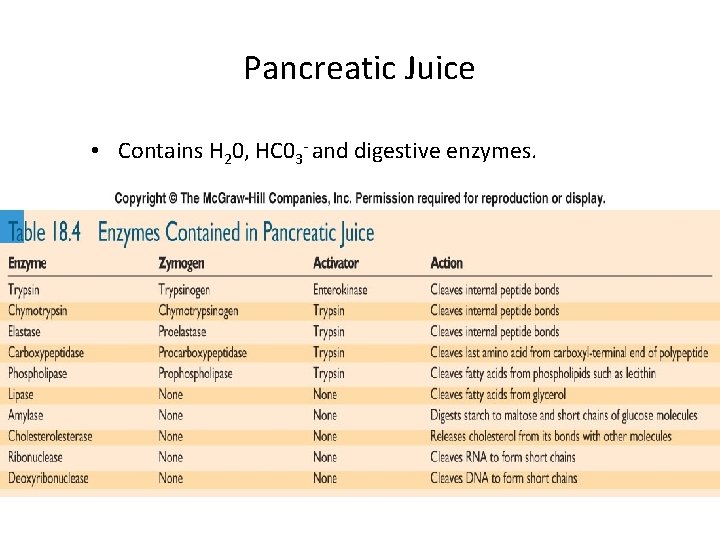
Pancreatic secretions is an alkaline liquid secreted by the pancreas, which contains a variety of enzymes. Composition of pancreatic secretion: 1 - The first component is a solution of bicarbonate, Na+ , K+ and water emitted by the epithelial cells that line the pancreatic ducts. This alkaline solution is designed to help neutralize stomach acid so that digestive enzymes can work more effectively. 2 - The second component is the enzymatic component ; which include: v Trypsinogen v. Chymotrypsinogen v. Procarboxypeptidase v. Pancreatic amylase v. Pancreatic lipases v. Deoxyribonucleases and ribonucleases
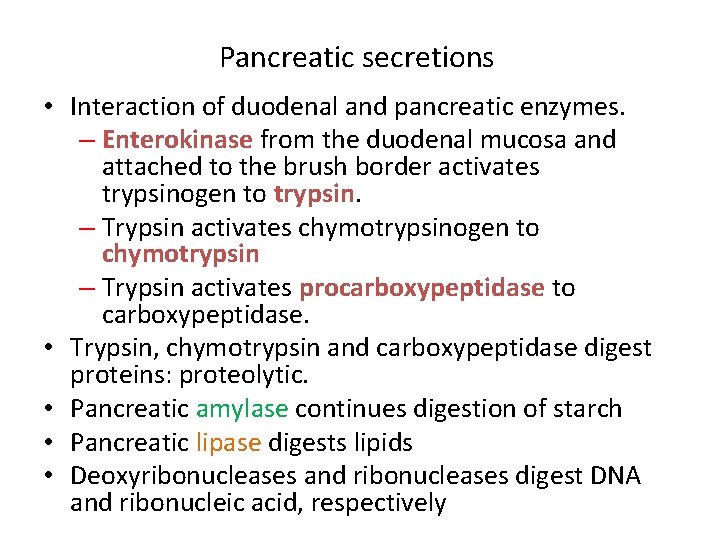
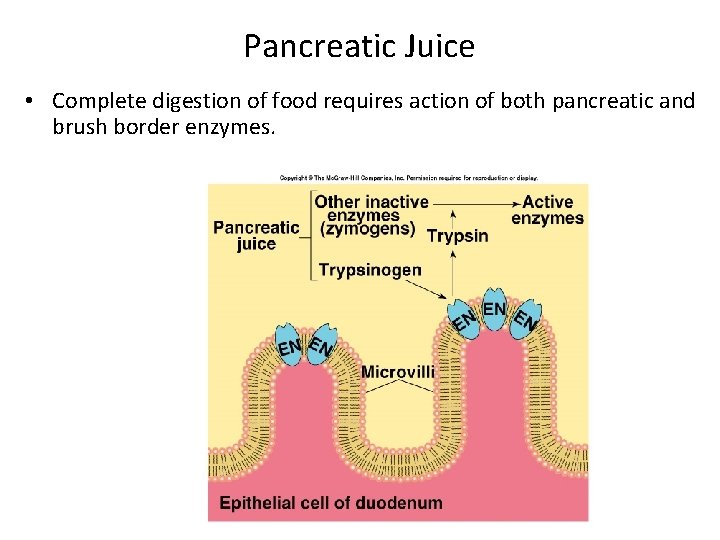
Pancreatic secretions • Interaction of duodenal and pancreatic enzymes. – Enterokinase from the duodenal mucosa and attached to the brush border activates trypsinogen to trypsin. – Trypsin activates chymotrypsinogen to chymotrypsin – Trypsin activates procarboxypeptidase to carboxypeptidase. • Trypsin, chymotrypsin and carboxypeptidase digest proteins: proteolytic. • Pancreatic amylase continues digestion of starch • Pancreatic lipase digests lipids • Deoxyribonucleases and ribonucleases digest DNA and ribonucleic acid, respectively
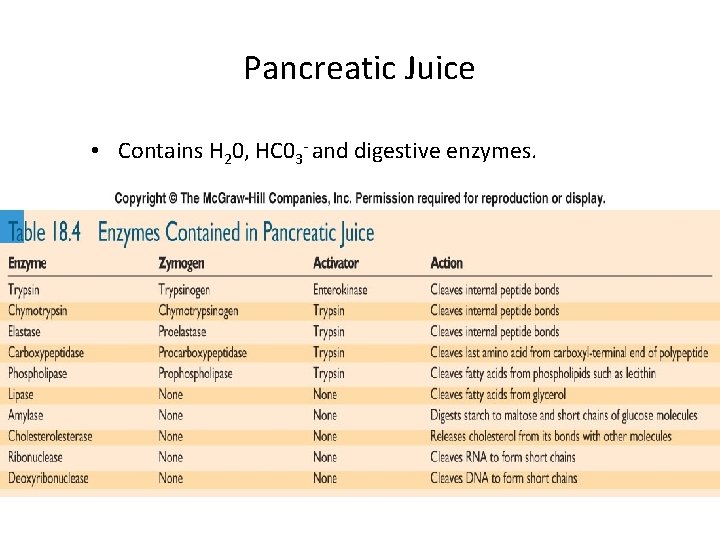
Pancreatic Juice • Contains H 20, HC 03 - and digestive enzymes.
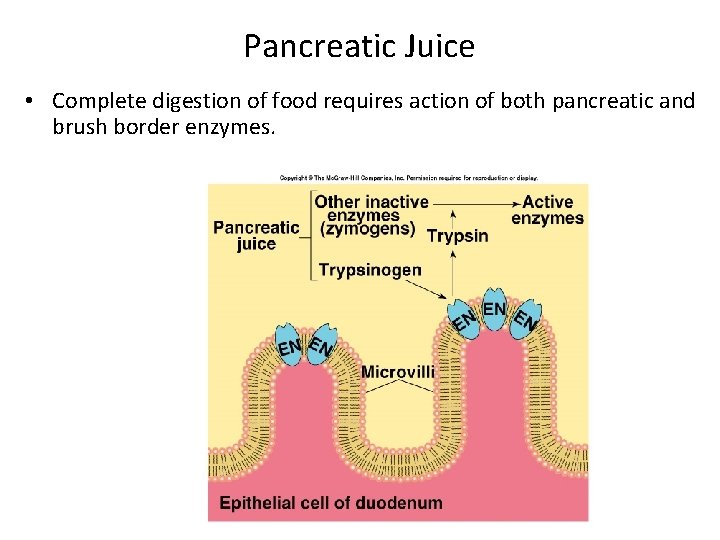
Pancreatic Juice • Complete digestion of food requires action of both pancreatic and brush border enzymes. Fig. 18. 29
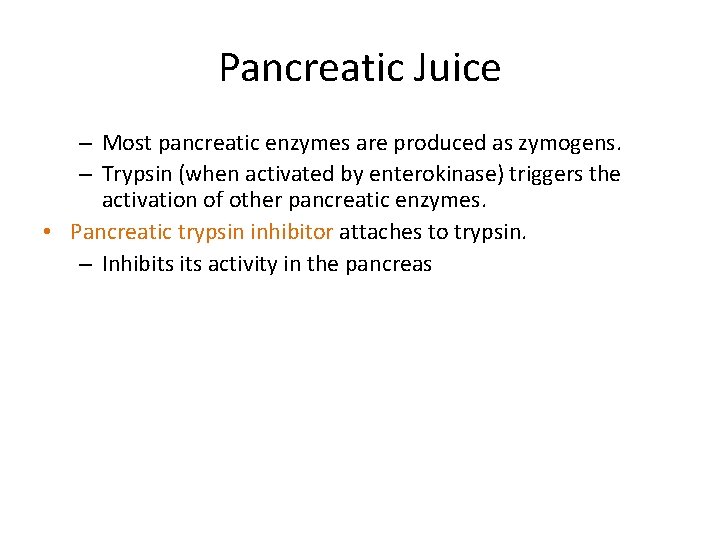
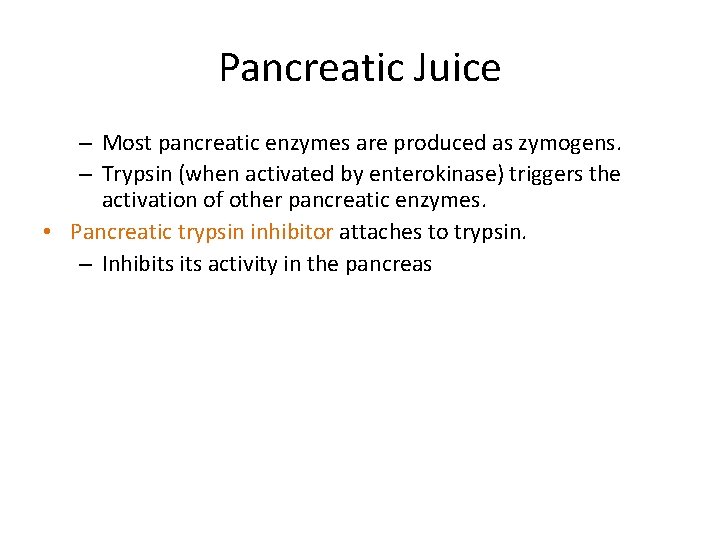
Pancreatic Juice – Most pancreatic enzymes are produced as zymogens. – Trypsin (when activated by enterokinase) triggers the activation of other pancreatic enzymes. • Pancreatic trypsin inhibitor attaches to trypsin. – Inhibits activity in the pancreas
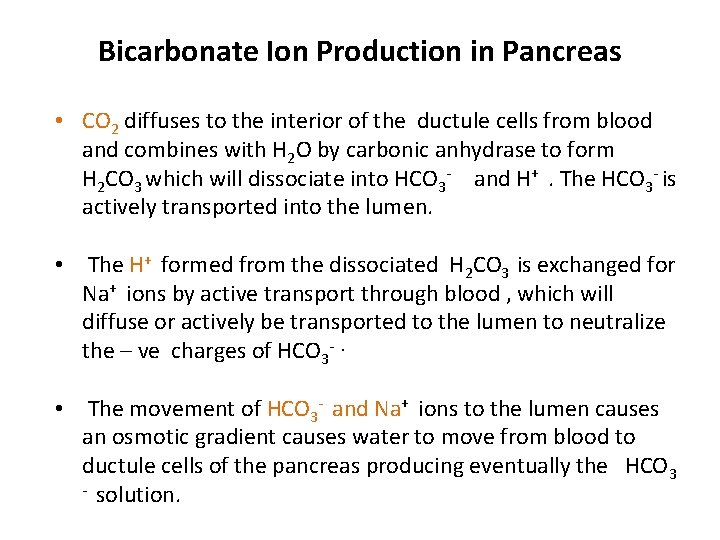
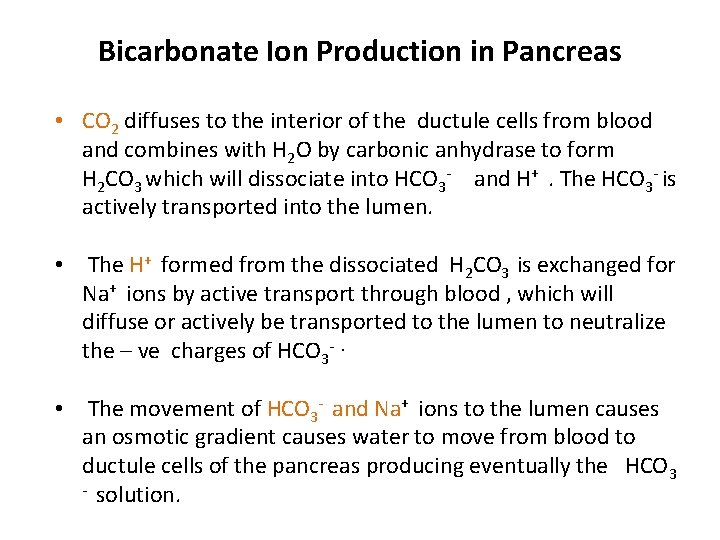
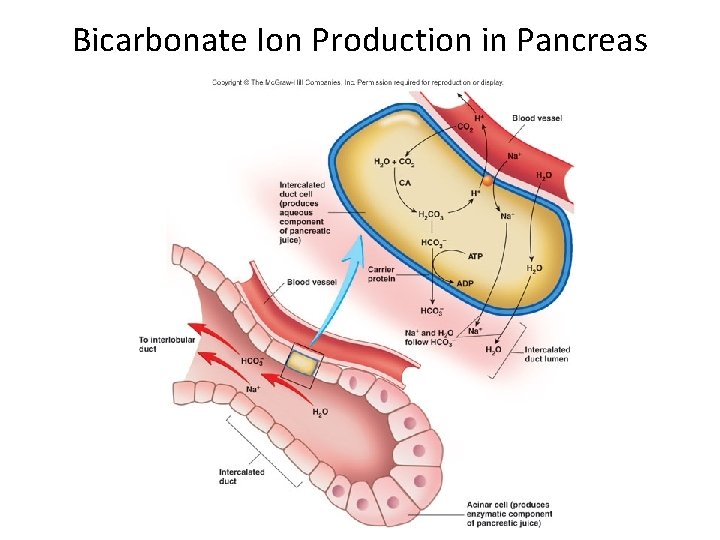
Bicarbonate Ion Production in Pancreas • CO 2 diffuses to the interior of the ductule cells from blood and combines with H 2 O by carbonic anhydrase to form H 2 CO 3 which will dissociate into HCO 3 - and H+. The HCO 3 - is actively transported into the lumen. • The H+ formed from the dissociated H 2 CO 3 is exchanged for Na+ ions by active transport through blood , which will diffuse or actively be transported to the lumen to neutralize the – ve charges of HCO 3 -. • The movement of HCO 3 - and Na+ ions to the lumen causes an osmotic gradient causes water to move from blood to ductule cells of the pancreas producing eventually the HCO 3 - solution.
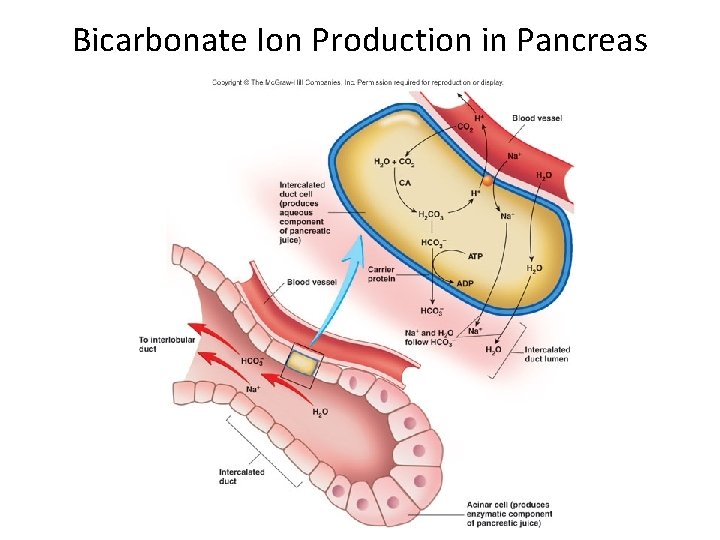
Bicarbonate Ion Production in Pancreas
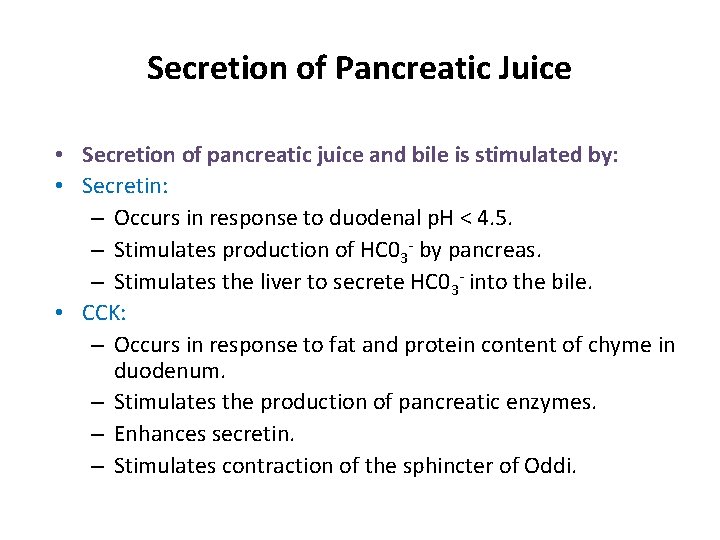
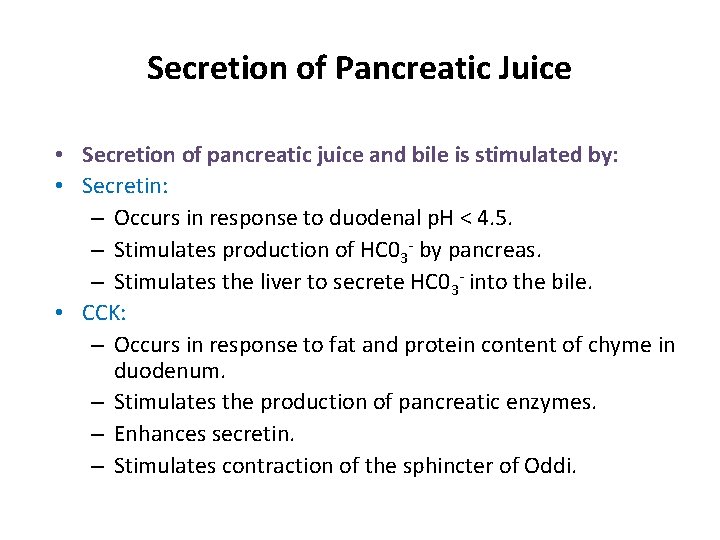
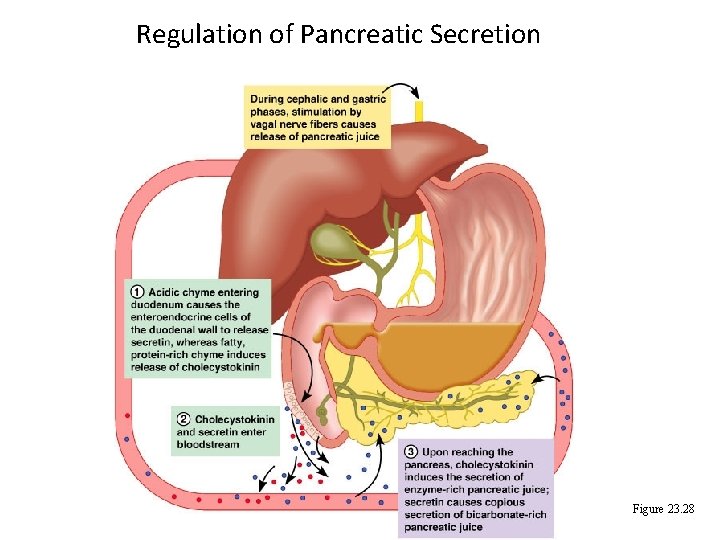
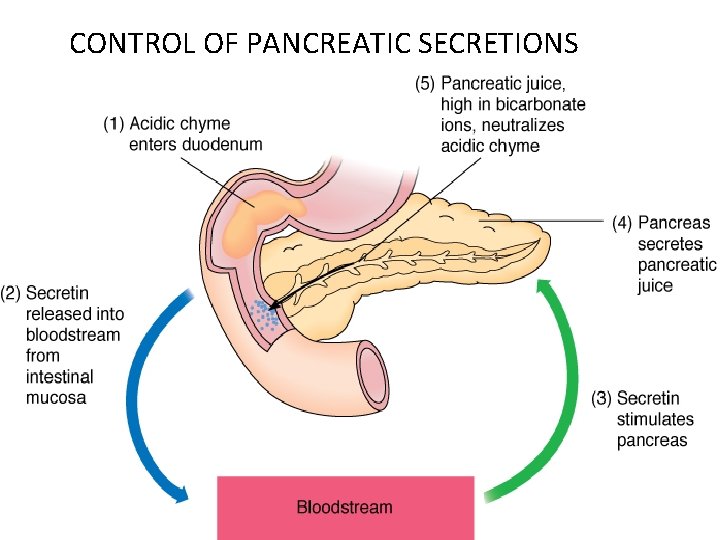
Secretion of Pancreatic Juice • Secretion of pancreatic juice and bile is stimulated by: • Secretin: – Occurs in response to duodenal p. H < 4. 5. – Stimulates production of HC 03 - by pancreas. – Stimulates the liver to secrete HC 03 - into the bile. • CCK: – Occurs in response to fat and protein content of chyme in duodenum. – Stimulates the production of pancreatic enzymes. – Enhances secretin. – Stimulates contraction of the sphincter of Oddi.
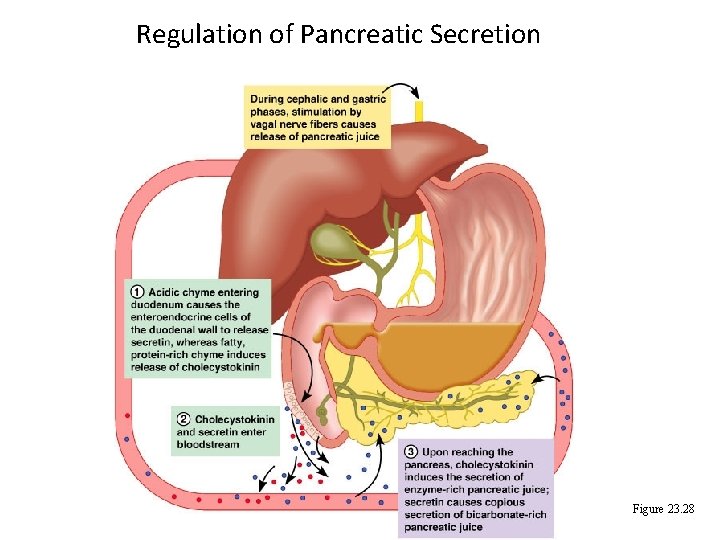
Regulation of Pancreatic Secretion Figure 23. 28
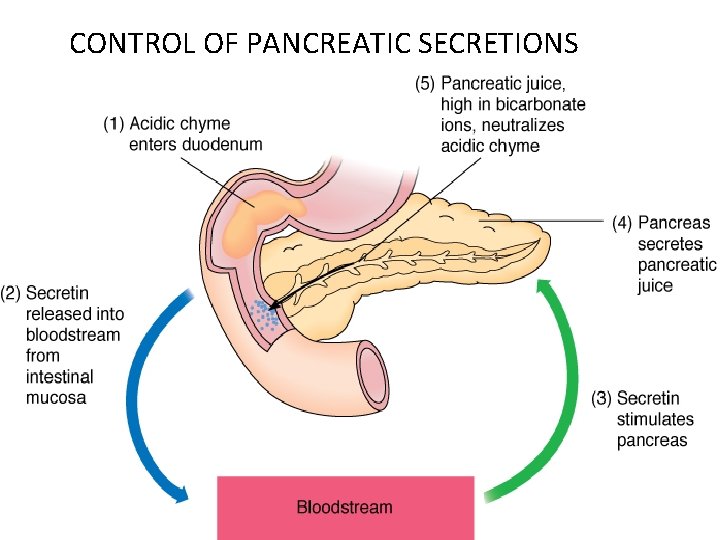
CONTROL OF PANCREATIC SECRETIONS 24

Diabetes Mellitus • Diabetes mellitus is an endocrine disorder characterized by many signs and symptoms.
Diabetes Mellitus Diabetes mellitus is a disorder quite distinct from the similarly-named diabetes insipidus. They both result in the production of large amounts of urine (diabetes), but in one the urine is sweet while in the other (caused by ADH deficiency) it is not. Before the days of laboratory tests, a simple taste test ("mellitus" or "insipidus") enabled the doctor to make the correct diagnosis

Diabetes Mellitus • There are three categories of diabetes mellitus: 1 - Insulin-Dependent Diabetes Mellitus (IDDM) [also called "Type 1" diabetes] and 2 - Non Insulin-Dependent Diabetes Mellitus (NIDDM)["Type 2"] 3 - Inherited Forms of Diabetes Mellitus
Insulin-Dependent Diabetes Mellitus (IDDM) • IDDM (also called Type 1 diabetes) • is characterized by little (hypo) or no circulating insulin; • most commonly appears in childhood. • It results from destruction of the beta cells of the islets.
• IDDM is controlled by carefully-regulated injections of insulin. For many years, insulin extracted from the glands of cows and pigs was used. However, pig insulin differs from human insulin by one amino acid; beef insulin by three. • Although both work in humans to lower blood sugar, they are seen by the immune system as "foreign" and induce an antibody response in the patient that blunts their effect and requires higher doses
Non Insulin-Dependent Diabetes Mellitus (NIDDM) • Many people develop diabetes mellitus without an accompanying drop in insulin levels (at least at first). • In many cases, the problem appears to be a failure to express a sufficient number of glucose transporters in the plasma membrane of their skeletal muscles.
Skeletal muscle is the major "sink" for removing excess glucose from the blood (and converting it into glycogen). In NIDDM, the patient's ability to remove glucose from the blood and convert it into glycogen may be only 20% of normal. This is called insulin resistance.
NIDDM (also called Type 2 diabetes mellitus) usually strikes in adults and, particularly often, in overweight people. However, over the last few years in the U. S. , the incidence of NIDDM in children has grown to the point where they now account for 20% of all newly-diagnosed cases (and, like their adult counterparts, are usually overweight).
Inherited Forms of Diabetes Mellitus • Some cases of diabetes result from mutant genes inherited from one or both parents. Examples: • mutations in one or both copies of the gene encoding the insulin receptor. These patients usually have extra-high levels of circulating insulin but defective receptors. The mutant receptors • a mutant version of the gene encoding glucokinase, the enzyme that phosphorylates glucose in the first step of glycolysis
Pancreatitis • An estimated 50, 000 to 80, 000 cases of acute pancreatitis occur in the United States each year. • This disease occurs when the pancreas suddenly becomes inflamed and then gets better. • Some patients have more than one attack but recover fully after each one. • Most cases of acute pancreatitis are caused either by alcohol abuse or by gallstones. • Other causes may be use of prescribed drugs, trauma or surgery to the abdomen, or abnormalities of the pancreas or intestine.
What Are the Symptoms of Acute Pancreatitis • Acute pancreatitis usually begins with pain in the upper abdomen that may last for a few days. • The pain is often severe. It may be constant pain, just in the abdomen, or it may reach to the back and other areas. • The pain may be sudden and intense, or it may begin as a mild pain that is aggravated by eating and slowly grows worse. The abdomen may be swollen and very tender. • Other symptoms may include nausea, vomiting, fever, and an increased pulse rate. • The person often feels and looks very sick.

Chronic Pancreatitis • The term "chronic pancreatitis" defines the histologic, functional, and clinical results of longstanding or irreversible pancreatic injury. • There a number of things that increase a persons risk of deveolping chronic pancreatits including alcohol consumption, smoking, genetic factors and other conditions or tramatic events that injure the pancreas.
 Pancreas organ function
Pancreas organ function Enterokinase enzyme function
Enterokinase enzyme function Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual Pineal gland pituitary gland
Pineal gland pituitary gland Watch?v=ic7l-zwoiq8
Watch?v=ic7l-zwoiq8 Organ and organ system
Organ and organ system Cell tissue organ organ system organism
Cell tissue organ organ system organism Foto rontgen efusi pleura
Foto rontgen efusi pleura Tissue are grouped together to form various
Tissue are grouped together to form various Organ penyusun sistem koordinasi
Organ penyusun sistem koordinasi Organ penyusun sistem gerak dan fungsinya
Organ penyusun sistem gerak dan fungsinya Site:slidetodoc.com
Site:slidetodoc.com Secrecion
Secrecion Simple branched alveolar gland
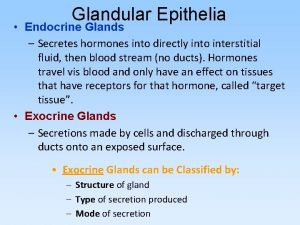
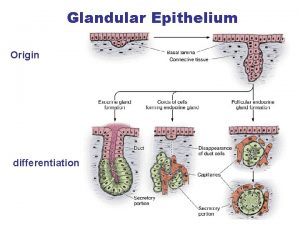
Simple branched alveolar gland Glandular epithelia
Glandular epithelia Citocrinas
Citocrinas Canal epididimar
Canal epididimar Que es el sistema glandular
Que es el sistema glandular Epithelial tissue
Epithelial tissue Cartilage hyalin
Cartilage hyalin Epitelio glandular holocrino
Epitelio glandular holocrino Sistema digestivos de las aves
Sistema digestivos de las aves Holocrine
Holocrine Insufficient glandular tissue pictures
Insufficient glandular tissue pictures Simple squamous
Simple squamous Glandular meats
Glandular meats Larynx function in digestive system
Larynx function in digestive system Sistema exocrino
Sistema exocrino Islets of langerhans location in pancreas
Islets of langerhans location in pancreas Lobulus portalis
Lobulus portalis Histology
Histology Glandula pancreas
Glandula pancreas Como es el proceso de la digestión
Como es el proceso de la digestión Esôfago
Esôfago Tmpi de rama secundaria
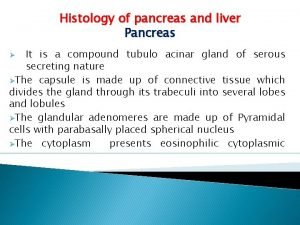
Tmpi de rama secundaria Histology of liver and pancreas
Histology of liver and pancreas Pancreas
Pancreas Baylor
Baylor