Palliative Care Recognising Dying and Challenging Conversations Dr




- Slides: 36
Palliative Care Recognising Dying and Challenging Conversations Dr Joanna Davies Consultant Palliative Medicine St George’s
Learning objectives • Consider what we mean by a ‘good death’ and how we enable this • Identify indicators which suggest that a patient is dying • Consider the changing focus of medical care at the end of life • Consider priorities for personalised end of life care • Consider how to approach communication at the end of life

World death rates: 3

What do we mean by ‘a good death’? Remember that this will differ from person to person, but these are some general principles: – Maintaining dignity and privacy – To retain a degree of choice and control – To have an understanding of what to expect – Adequate relief from pain and other symptoms (palliative care in any location) – The opportunity to ensure wishes are respected (advance care planning, or in some cases an ADRT) – To die naturally and not have life prolonged pointlessly Adapted from BMJ, 2000
What are the issues that might be important to someone when they are dying? You might consider: – Treatment decisions – Concerns – Who to involve – Where to be
Dying: how not to do it……? • • In pain or with unrelieved symptoms Scared On your own? In the middle of a busy ward? You weren’t expecting it Your family weren’t expecting it No chance to say things – Sorry! – I forgive you! – Thank you! – I love you! • With no dignity…. .

Why bother? • GRIEF: – Shock, disbelief, denial – Guilt, regret – Sense of Injustice – Loss – Envy – Loneliness – Anger – Relief
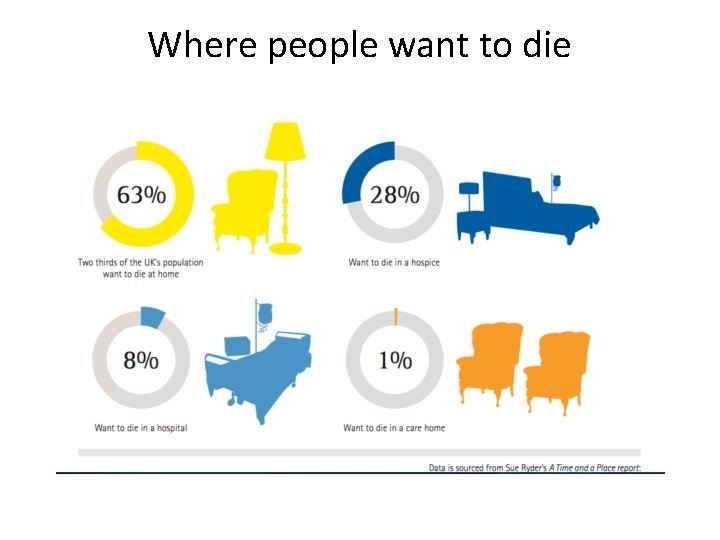
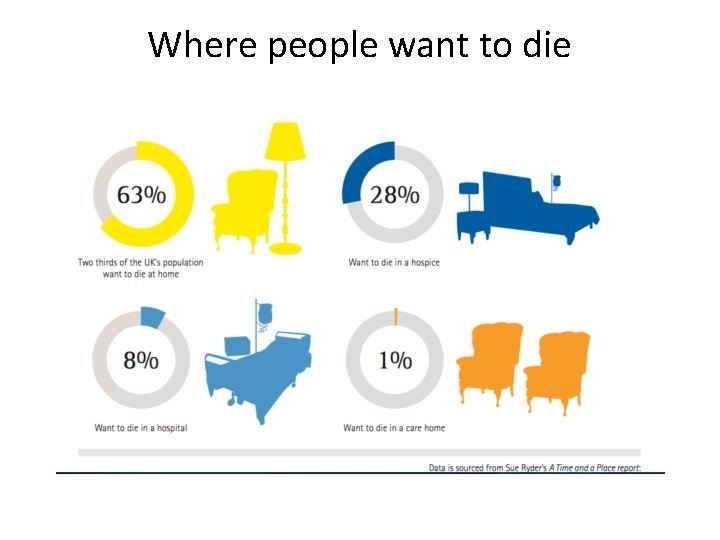
Where people want to die
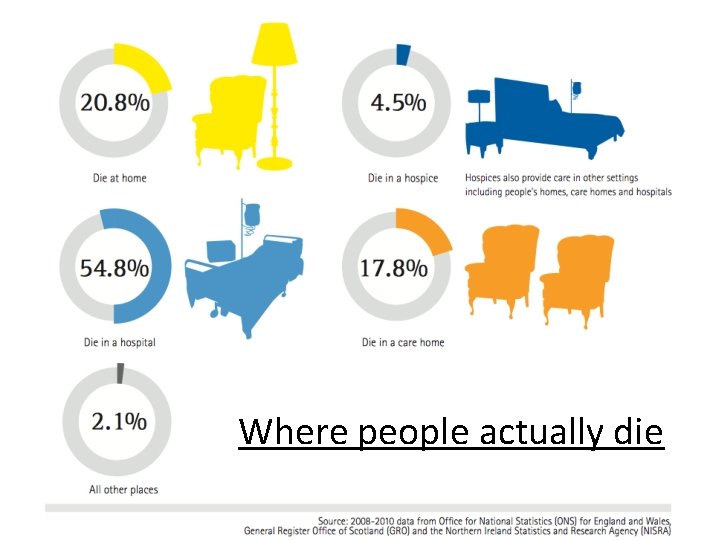
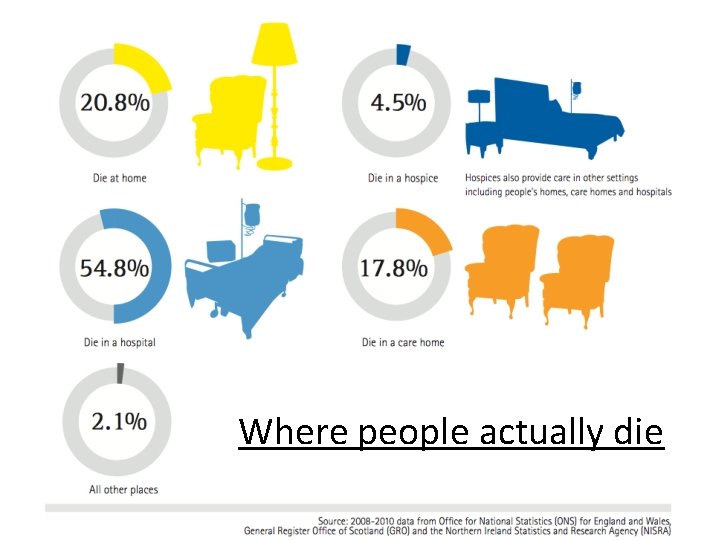
Where people actually die
The Challenge of Diagnosing Dying Ø Ø Ø Professionals can perceive it as “failing” the patient Complex Fear of missing reversible causes One last course of antibiotics and fluidsØ Hard to stop and question ‘should we’ Death denying society in fast paced health system Ø Focus changes from active disease management to intensive symptom control Ø There are occasions when a patient who is thought to be dying lives longer than expected and vice versa. Ø Seek a second opinion or specialist palliative care support
Consistent overestimation of survival • Parks (1972); • Maltoni, et al (1994); • Vigano, et al (2000); • Glare, et al (2003); • Lam (2008).
How do you know when someone is dying? • Not always easy and obvious. • No ‘tests’…yet • Which healthcare workers in a hospice are best able to predict imminent death? (Oxenham & Cornbleet 1998) • Doctors over optimistic (Christakis 2000)
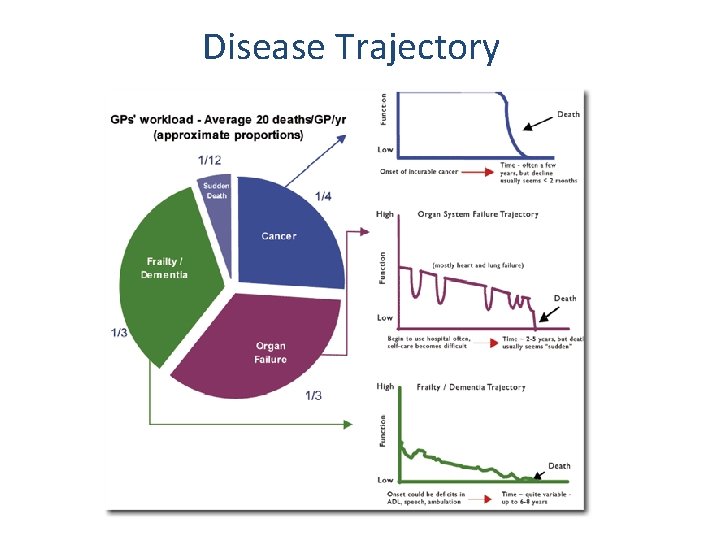
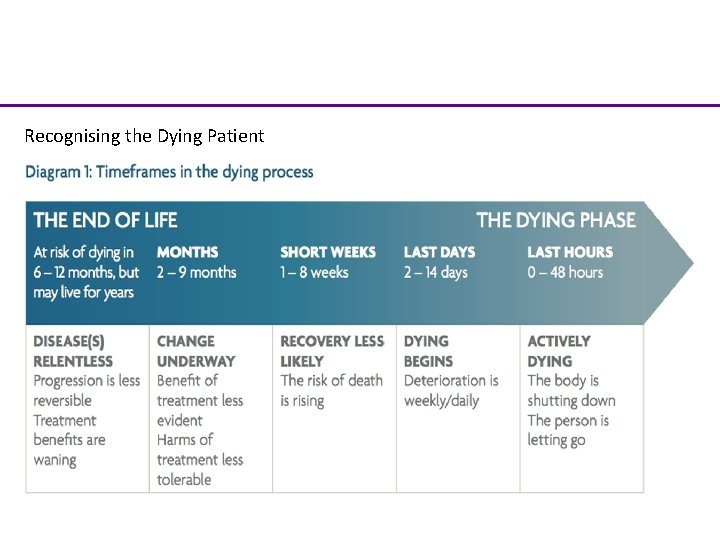
Recognising dying • Difficult to predict exactly when death will occur • Tools to help you: – Consider likely disease trajectory – Disease extent, biochemical markers e. g. albumin – Response to treatment (reversibility) – Rate of change – Patient’s perceptions – The ‘surprise’ question
Surprise Question • Will you be surprised if the patient dies in the next 12 months? • 75% accurate – but wide ranges of sensitivity and specificity White 2017
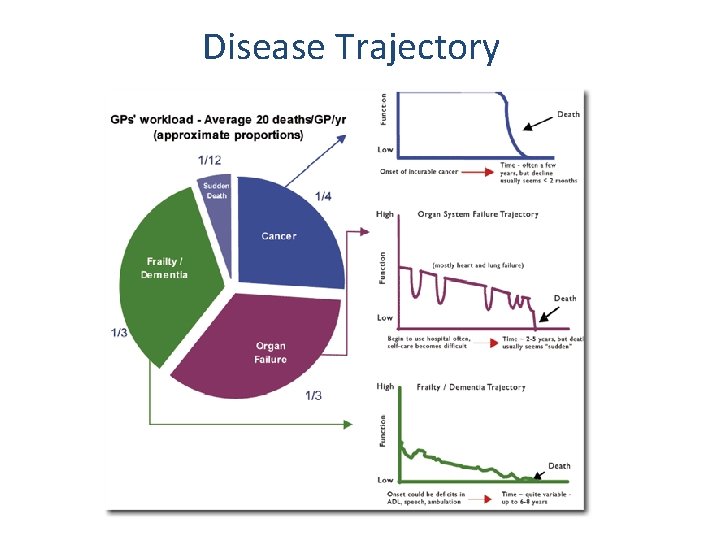
Disease Trajectory
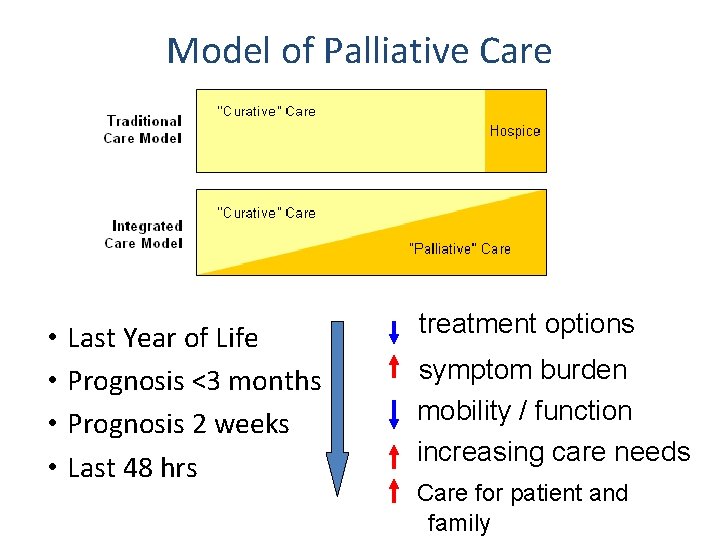
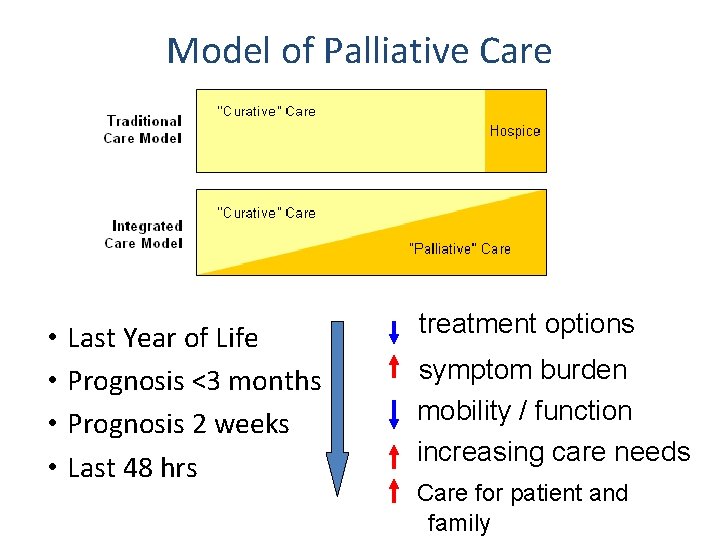
Model of Palliative Care • • Last Year of Life Prognosis <3 months Prognosis 2 weeks Last 48 hrs treatment options symptom burden mobility / function increasing care needs Care for patient and family
Almost half of over 85 year olds will die in the year following hospital admission
30% of adult hospital inpatients are dead in 12 months
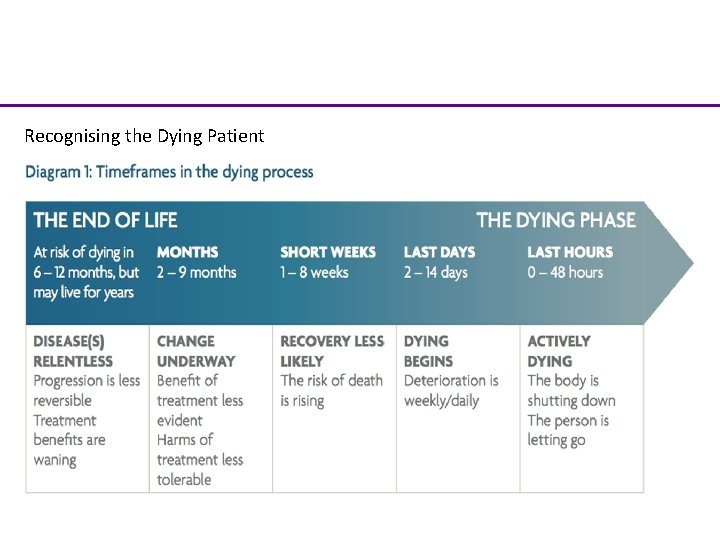
Recognising the Dying Patient Excellence in specialist and community healthcare
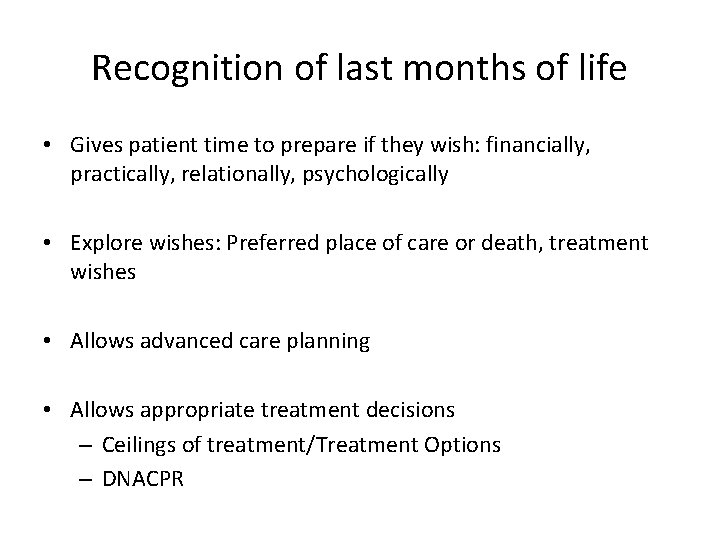
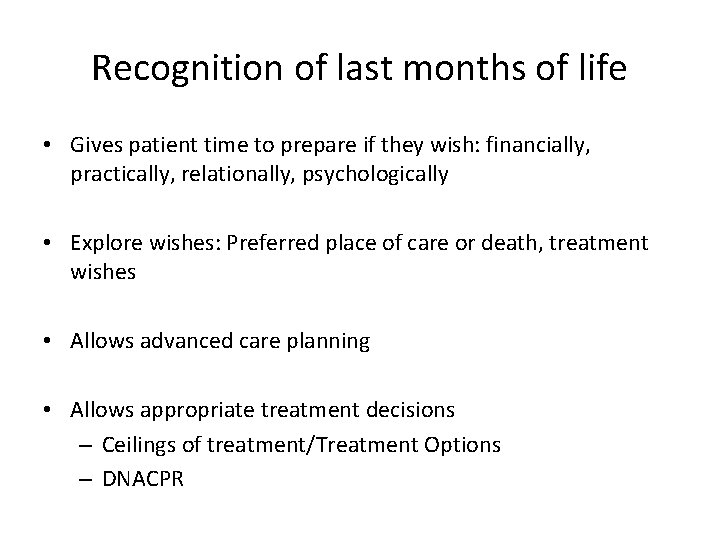
Recognition of last months of life • Gives patient time to prepare if they wish: financially, practically, relationally, psychologically • Explore wishes: Preferred place of care or death, treatment wishes • Allows advanced care planning • Allows appropriate treatment decisions – Ceilings of treatment/Treatment Options – DNACPR
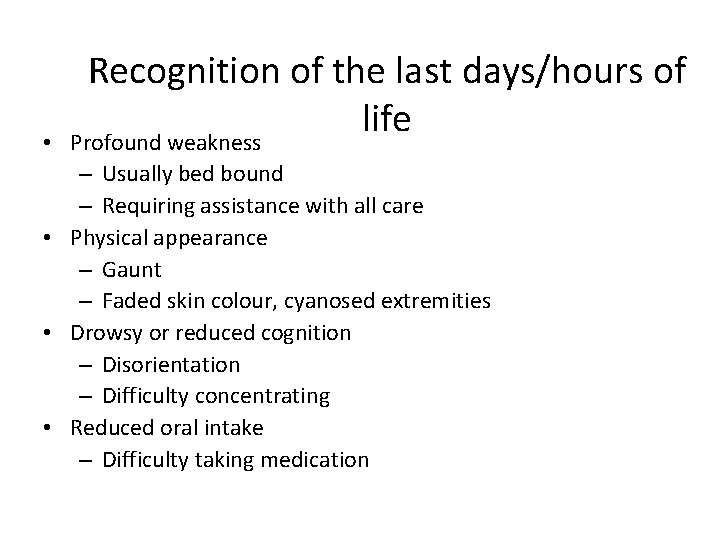
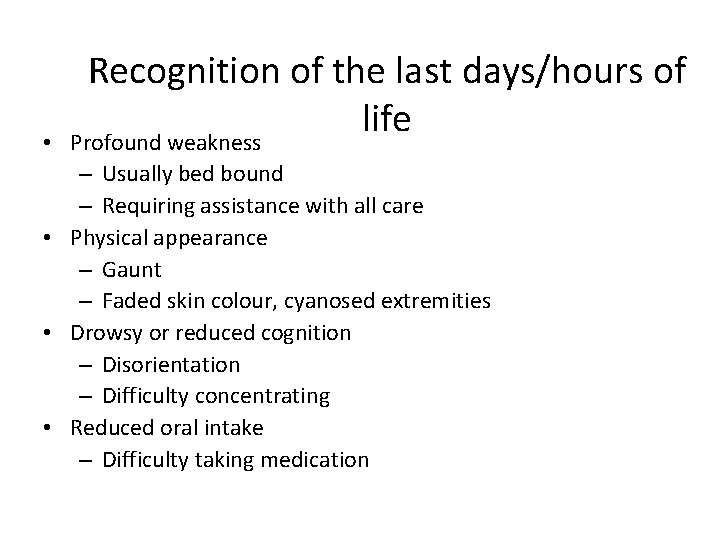
• Recognition of the last days/hours of life Profound weakness – Usually bed bound – Requiring assistance with all care • Physical appearance – Gaunt – Faded skin colour, cyanosed extremities • Drowsy or reduced cognition – Disorientation – Difficulty concentrating • Reduced oral intake – Difficulty taking medication
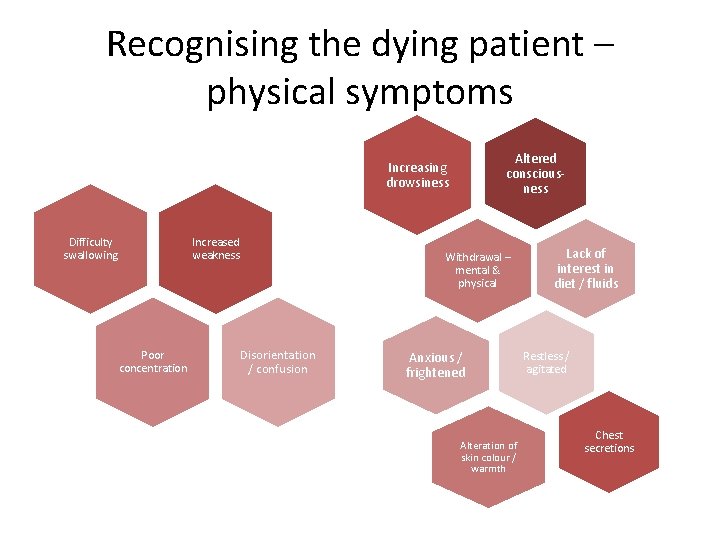
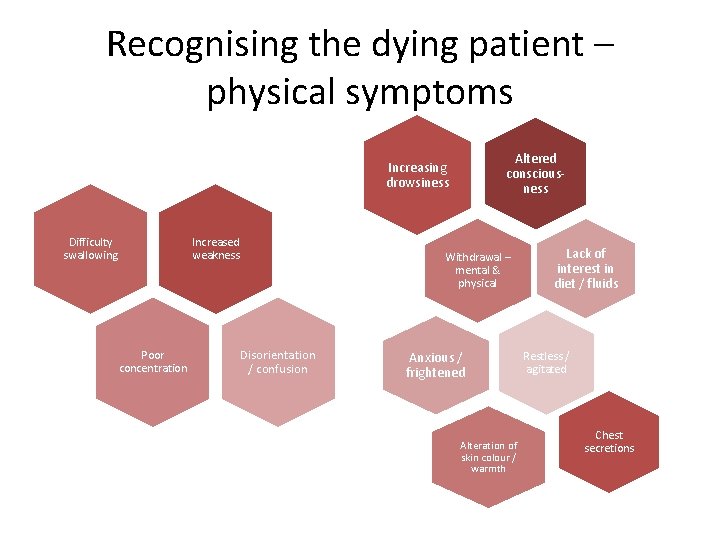
Recognising the dying patient – physical symptoms Altered consciousness Increasing drowsiness Difficulty swallowing Increased weakness Poor concentration Withdrawal – mental & physical Disorientation / confusion Anxious / frightened Alteration of skin colour / warmth Lack of interest in diet / fluids Restless / agitated Chest secretions
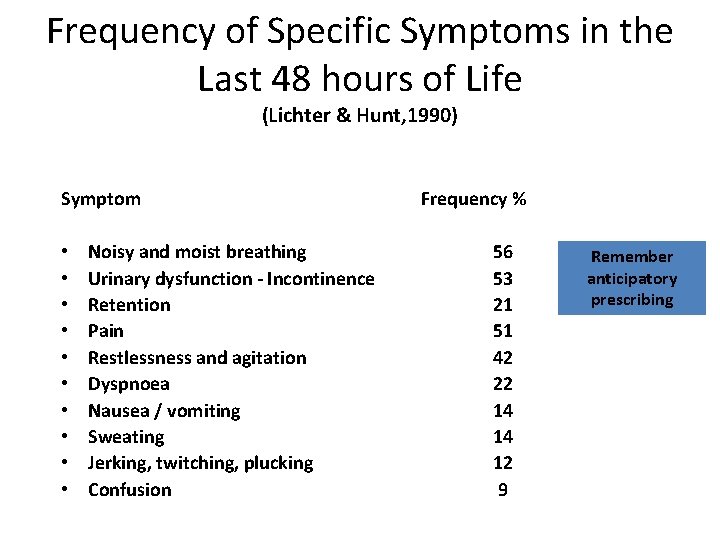
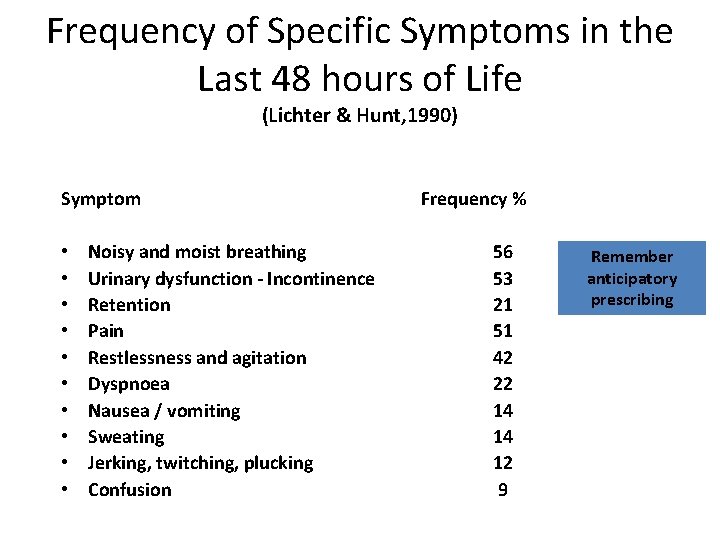
Frequency of Specific Symptoms in the Last 48 hours of Life (Lichter & Hunt, 1990) Symptom • • • Noisy and moist breathing Urinary dysfunction - Incontinence Retention Pain Restlessness and agitation Dyspnoea Nausea / vomiting Sweating Jerking, twitching, plucking Confusion Frequency % 56 53 21 51 42 22 14 14 12 9 Remember anticipatory prescribing
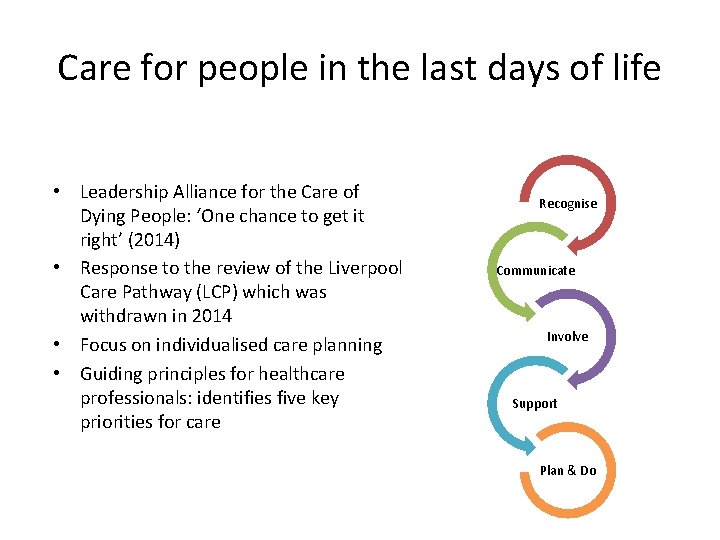
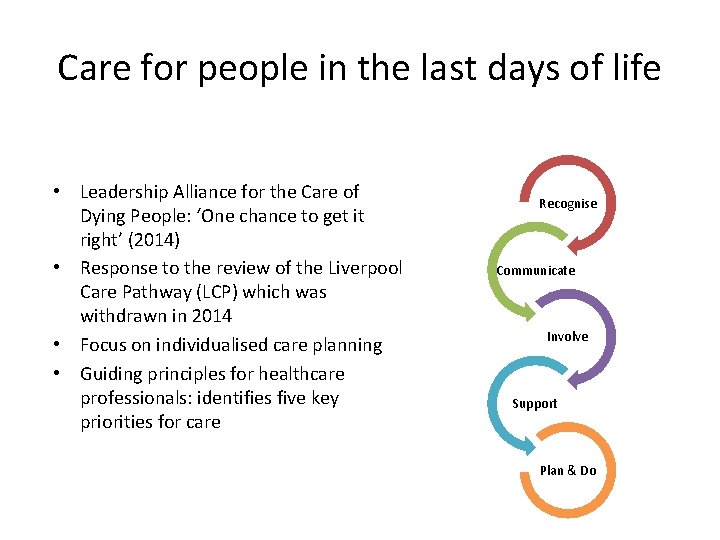
Care for people in the last days of life • Leadership Alliance for the Care of Dying People: ‘One chance to get it right’ (2014) • Response to the review of the Liverpool Care Pathway (LCP) which was withdrawn in 2014 • Focus on individualised care planning • Guiding principles for healthcare professionals: identifies five key priorities for care Recognise Communicate Involve Support Plan & Do
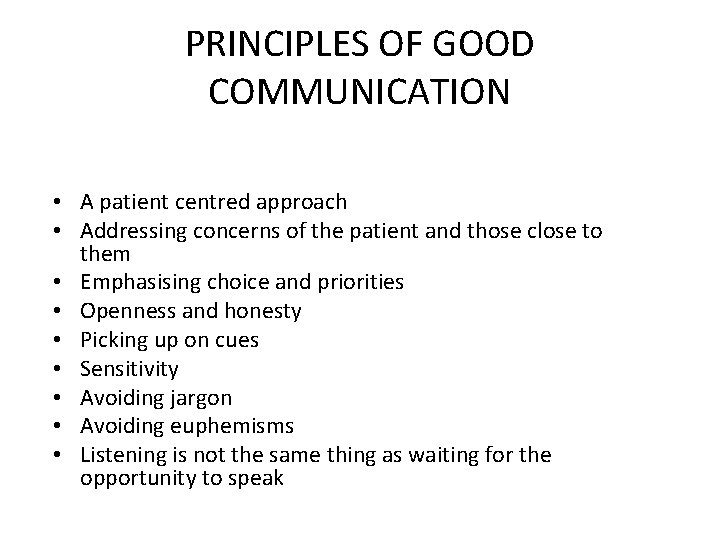
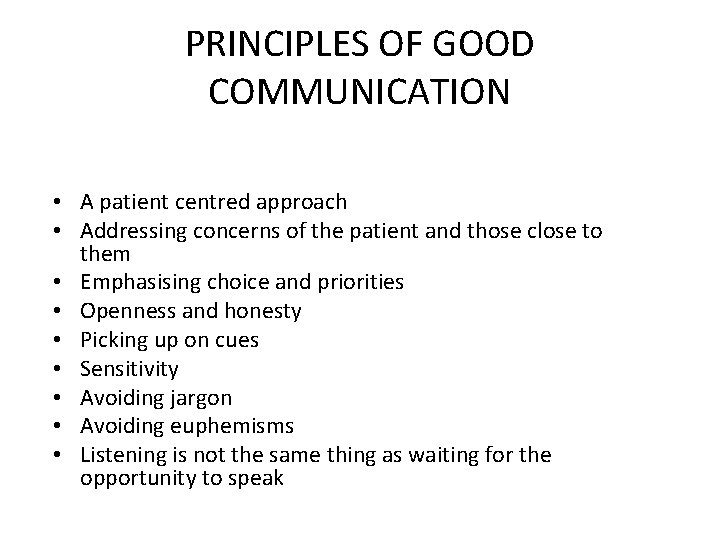
PRINCIPLES OF GOOD COMMUNICATION • A patient centred approach • Addressing concerns of the patient and those close to them • Emphasising choice and priorities • Openness and honesty • Picking up on cues • Sensitivity • Avoiding jargon • Avoiding euphemisms • Listening is not the same thing as waiting for the opportunity to speak
DYING IS NOT A MEDICAL THING. IT’S A HUMAN THING.
Advance Care Planning • • • Identify patients nearing the end of life Talk to them about what they want Plan how this might be achieved Communicate plan to relevant teams Deploy resources to achieve plan Review
ACP-What makes it so difficult? • Highlighted as one of the most difficult areas for healthcare professionals. • Starting a conversation • It may involve talking about ‘death & dying’ and I am not a specialist • Don’t have all the facts about what might happen in the future • ‘I’m only a xxx’ etc
What is ACP in of end of life care? • A process • Initiated in light of advanced, incurable, progressive disease. • A tool for a person to register their wishes/views- recorded oral expressions can be used instead of actual form • According to personal preference an individual may or may not involve family & friends • Enables patient and their families to reflect on what they do and don’t want to happen at the end of life
End of Life Registers • London – ‘Coordinate my Care’ – – Electronic register Londonwide GP/DN/LAS/hospice/SPCT Cerner interoperability Someone may already have started the conversation
https: //www. youtube. com/watch? v=Cru. BRZh 8 quc

Support & Self-care Compassion Fatigue: Defined as a combination of physical, emotional and spiritual depletion associated with caring for patients in significant emotional pain and physical distress Speak to your manager Staff Support Service- confidential service
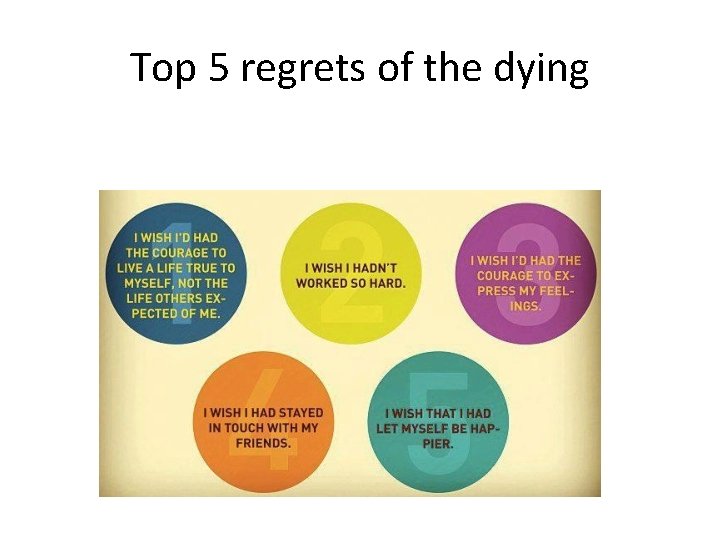
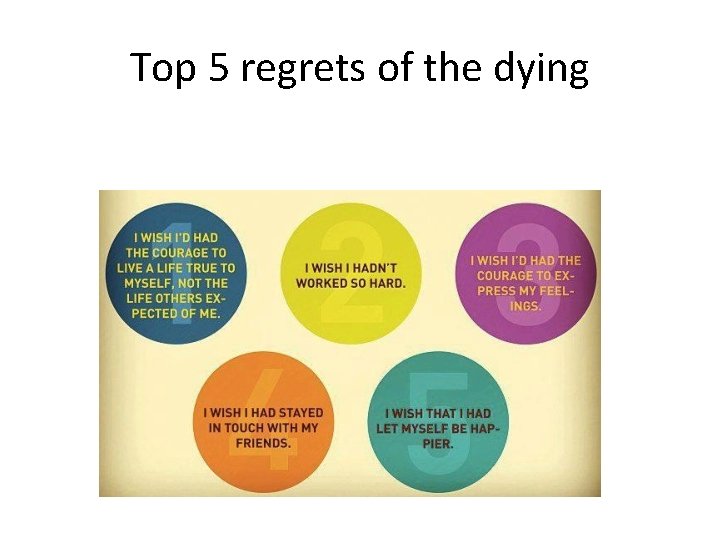
Top 5 regrets of the dying
Questions