Odessa national medical university Department of Anesthesiology Intensive












- Slides: 52
Odessa national medical university Department of Anesthesiology, Intensive Care and Emergency medicine Intensive therapy of acute respiratory insufficiency (failure)
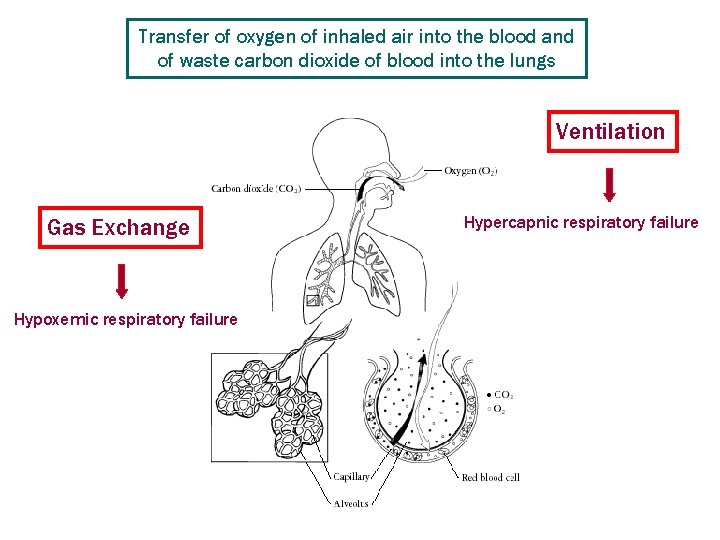
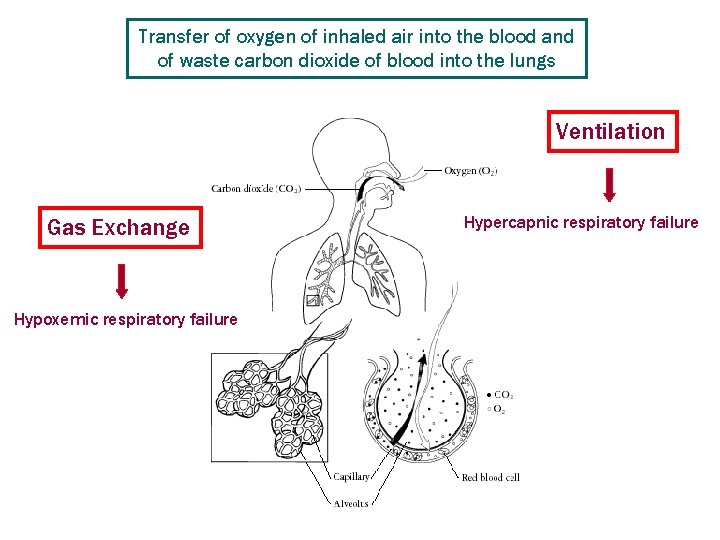
Transfer of oxygen of inhaled air into the blood and of waste carbon dioxide of blood into the lungs Ventilation Gas Exchange Hypoxemic respiratory failure Hypercapnic respiratory failure
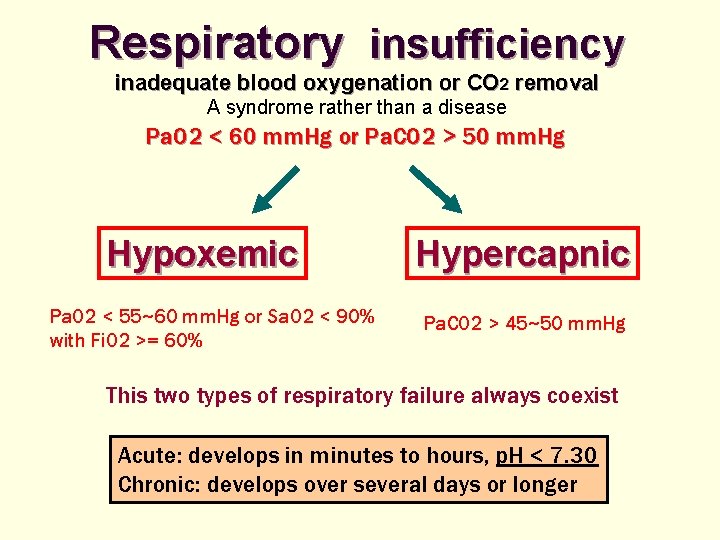
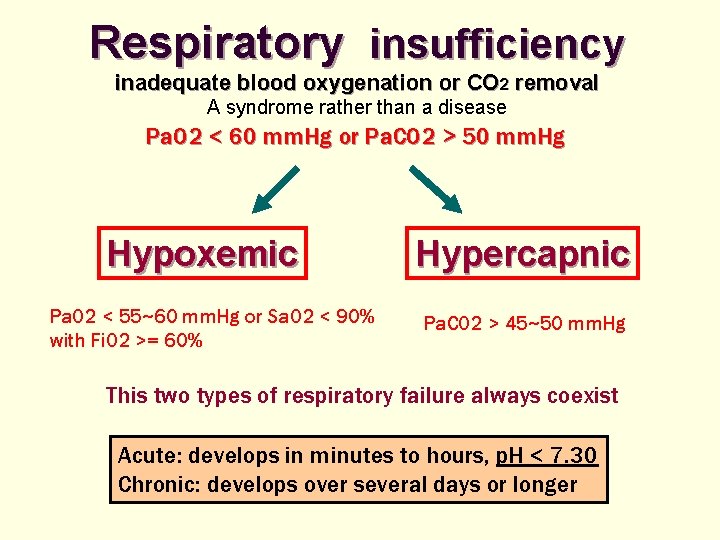
Respiratory insufficiency inadequate blood oxygenation or CO 2 removal A syndrome rather than a disease Pa. O 2 < 60 mm. Hg or Pa. CO 2 > 50 mm. Hg Hypoxemic Pa. O 2 < 55~60 mm. Hg or Sa. O 2 < 90% with Fi. O 2 >= 60% Hypercapnic Pa. CO 2 > 45~50 mm. Hg This two types of respiratory failure always coexist Acute: develops in minutes to hours, p. H < 7. 30 Chronic: develops over several days or longer
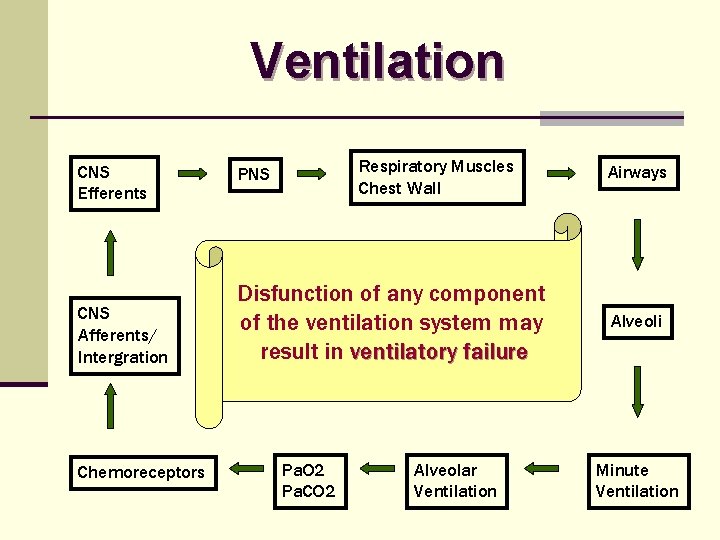
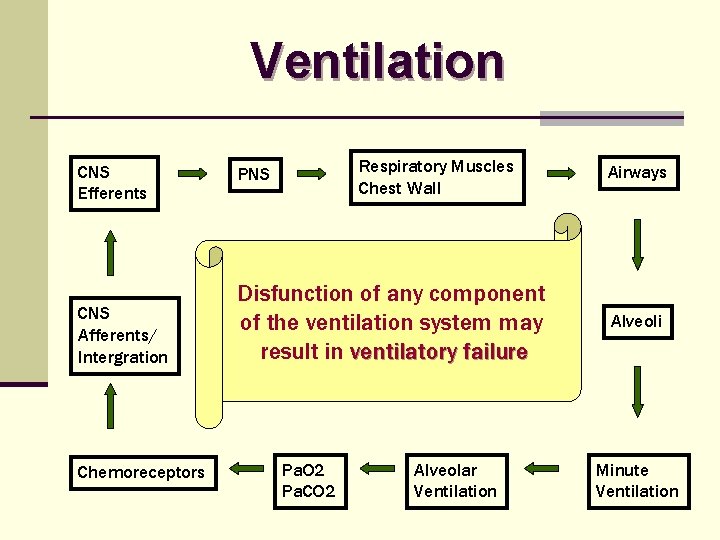
Ventilation CNS Efferents CNS Afferents/ Intergration Chemoreceptors Respiratory Muscles Chest Wall PNS Disfunction of any component of the ventilation system may result in ventilatory failure Pa. O 2 Pa. CO 2 Alveolar Ventilation Airways Alveoli Minute Ventilation
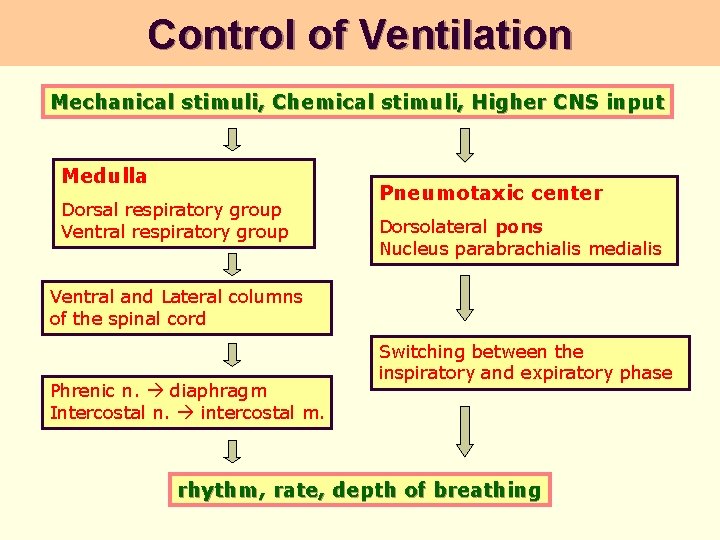
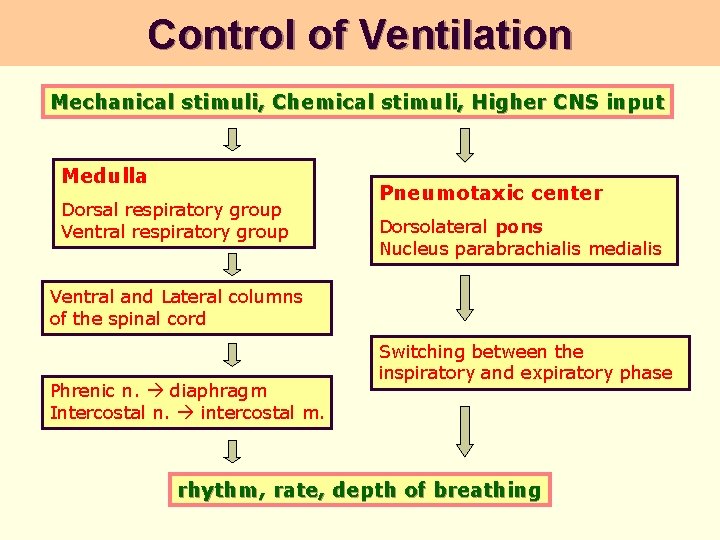
Control of Ventilation Mechanical stimuli, Chemical stimuli, Higher CNS input Medulla Dorsal respiratory group Ventral respiratory group Pneumotaxic center Dorsolateral pons Nucleus parabrachialis medialis Ventral and Lateral columns of the spinal cord Phrenic n. diaphragm Intercostal n. intercostal m. Switching between the inspiratory and expiratory phase rhythm, rate, depth of breathing
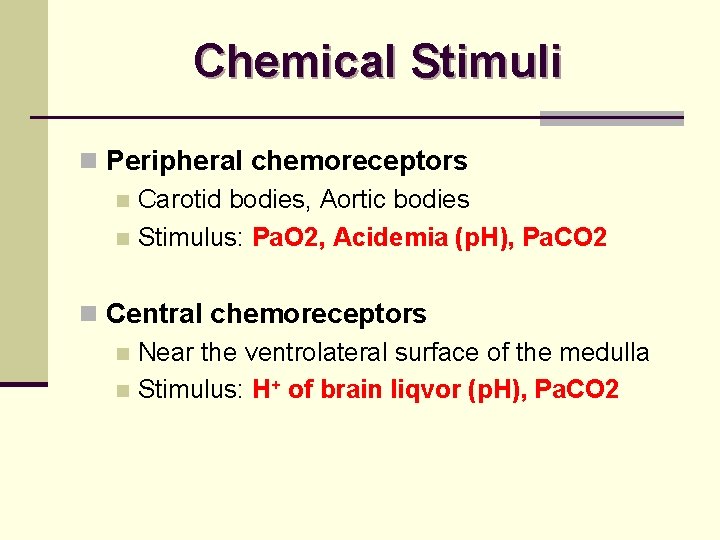
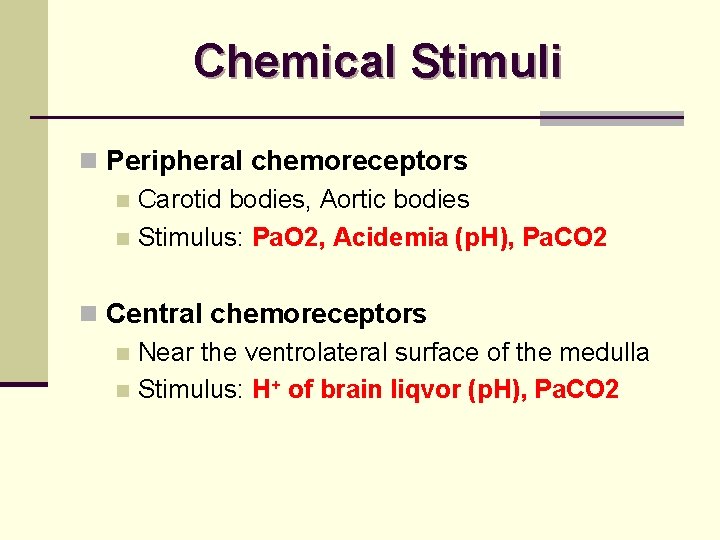
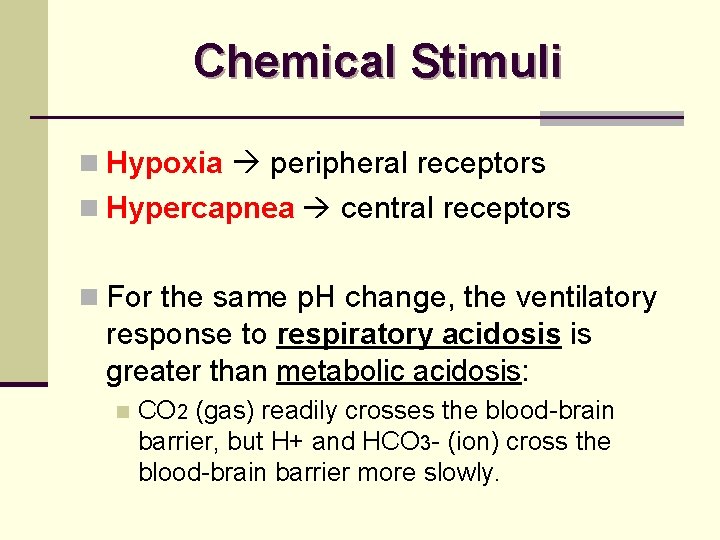
Chemical Stimuli n Peripheral chemoreceptors n Carotid bodies, Aortic bodies n Stimulus: Pa. O 2, Acidemia (p. H), Pa. CO 2 n Central chemoreceptors n Near the ventrolateral surface of the medulla n Stimulus: H+ of brain liqvor (p. H), Pa. CO 2
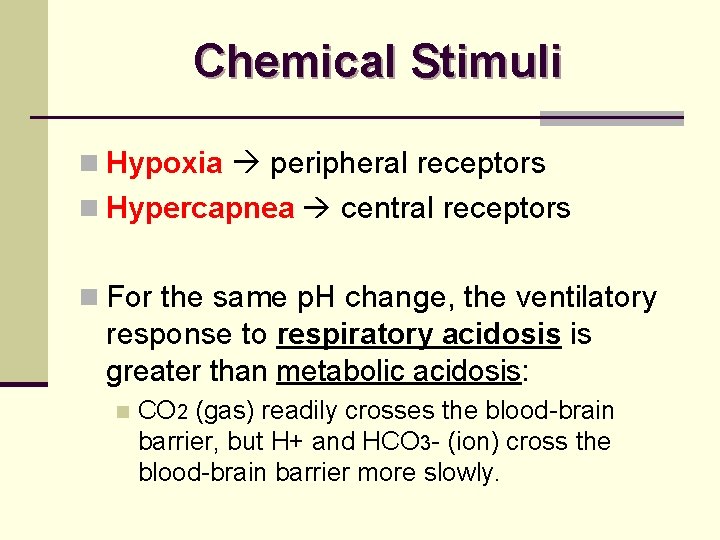
Chemical Stimuli n Hypoxia peripheral receptors n Hypercapnea central receptors n For the same p. H change, the ventilatory response to respiratory acidosis is greater than metabolic acidosis: n CO 2 (gas) readily crosses the blood-brain barrier, but H+ and HCO 3 - (ion) cross the blood-brain barrier more slowly.
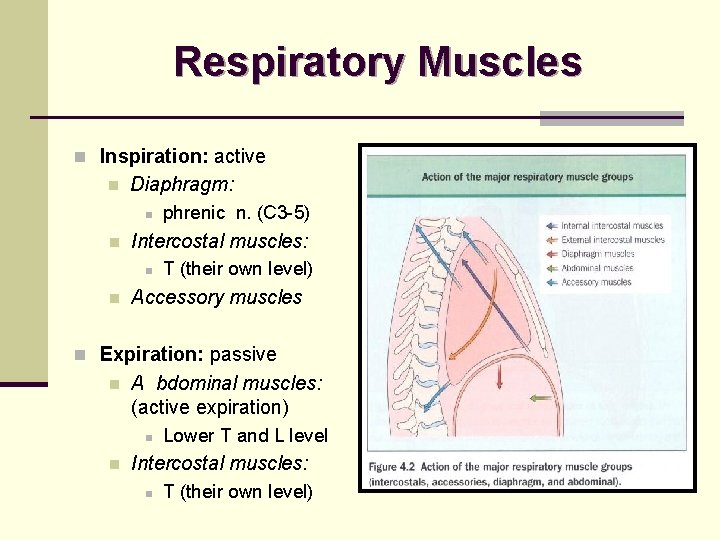
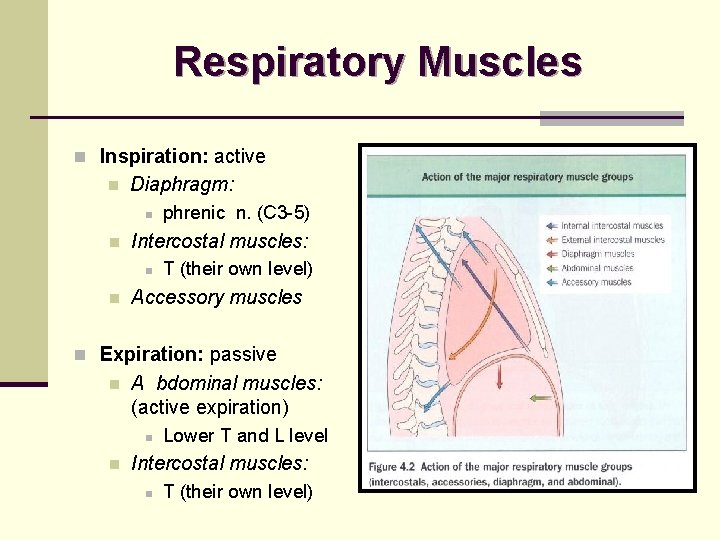
Respiratory Muscles n Inspiration: active n Diaphragm: n n Intercostal muscles: n n phrenic n. (C 3 -5) T (their own level) Accessory muscles n Expiration: passive n A bdominal muscles: (active expiration) n n Lower T and L level Intercostal muscles: n T (their own level)
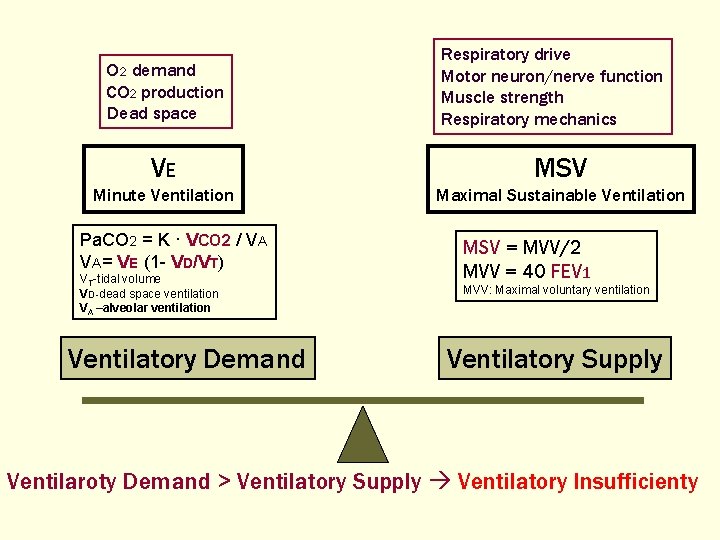
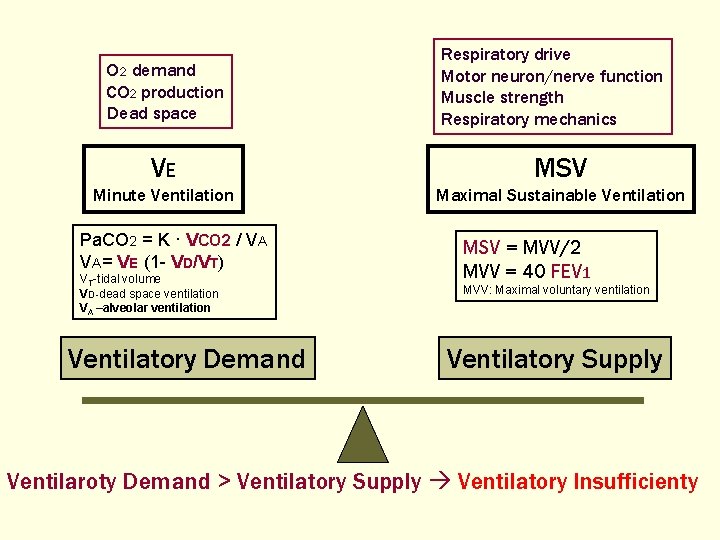
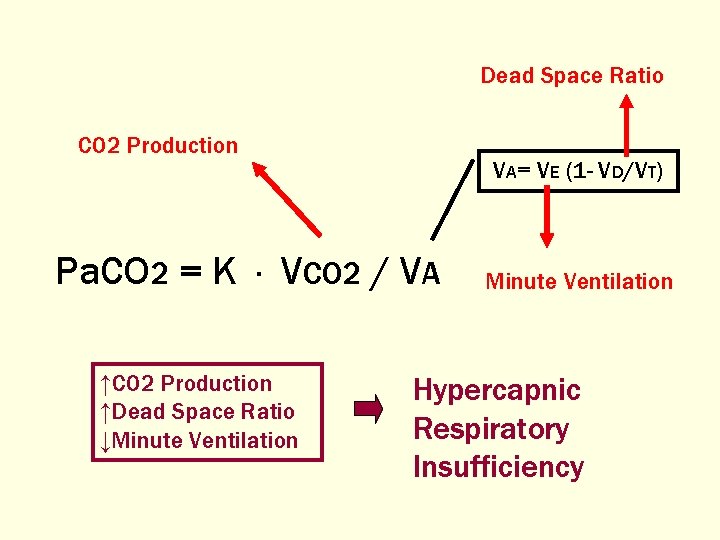
O 2 demand CO 2 production Dead space Respiratory drive Motor neuron/nerve function Muscle strength Respiratory mechanics VE MSV Minute Ventilation Maximal Sustainable Ventilation Pa. CO 2 = K · VCO 2 / VA VA= VE (1 - VD/VT) VT-tidal volume VD-dead space ventilation VA –alveolar ventilation Ventilatory Demand MSV = MVV/2 MVV = 40 FEV 1 MVV: Maximal voluntary ventilation Ventilatory Supply Ventilaroty Demand > Ventilatory Supply Ventilatory Insufficienty
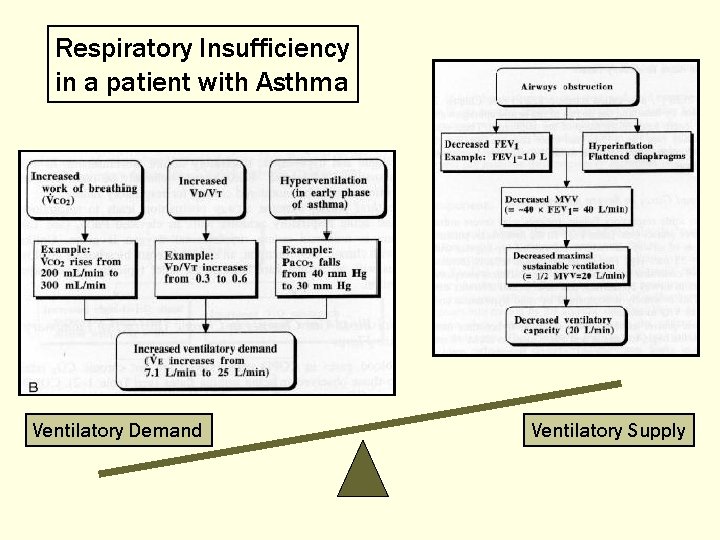
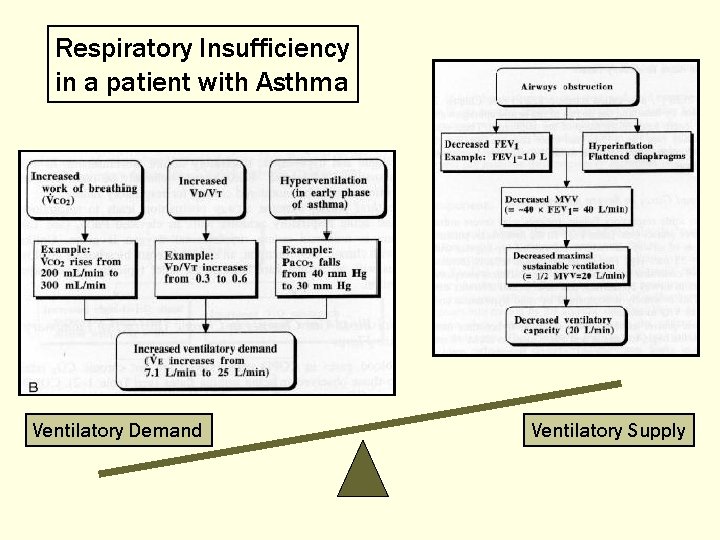
Respiratory Insufficiency in a patient with Asthma Ventilatory Demand Ventilatory Supply
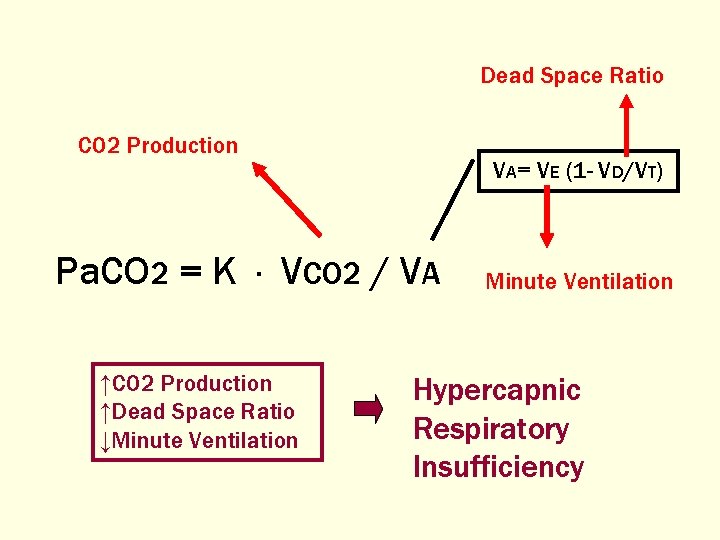
Dead Space Ratio CO 2 Production VA= VE (1 - VD/VT) Pa. CO 2 = K · VCO 2 / VA ↑CO 2 Production ↑Dead Space Ratio ↓Minute Ventilation Hypercapnic Respiratory Insufficiency
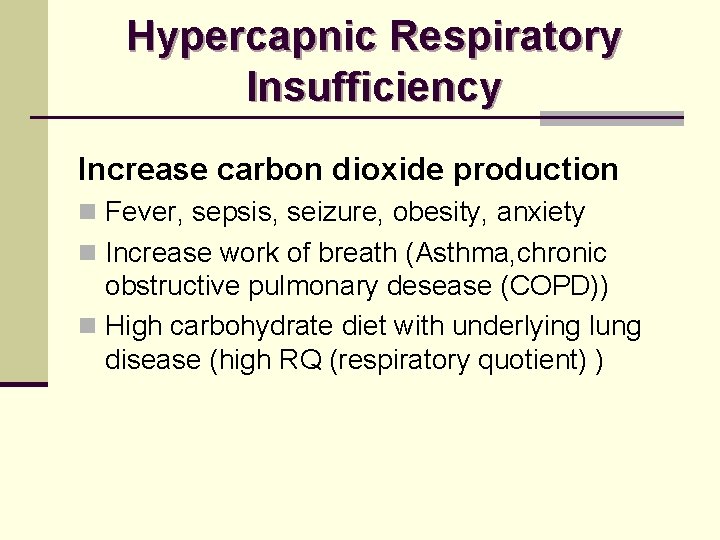
Hypercapnic Respiratory Insufficiency Increase carbon dioxide production n Fever, sepsis, seizure, obesity, anxiety n Increase work of breath (Asthma, chronic obstructive pulmonary desease (COPD)) n High carbohydrate diet with underlying lung disease (high RQ (respiratory quotient) )
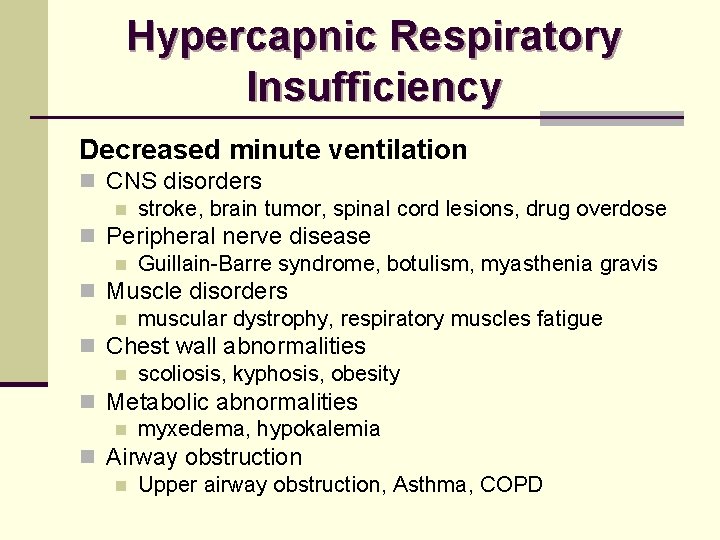
Hypercapnic Respiratory Insufficiency Decreased minute ventilation n CNS disorders n stroke, brain tumor, spinal cord lesions, drug overdose n Peripheral nerve disease n Guillain-Barre syndrome, botulism, myasthenia gravis n Muscle disorders n muscular dystrophy, respiratory muscles fatigue n Chest wall abnormalities n scoliosis, kyphosis, obesity n Metabolic abnormalities n myxedema, hypokalemia n Airway obstruction n Upper airway obstruction, Asthma, COPD
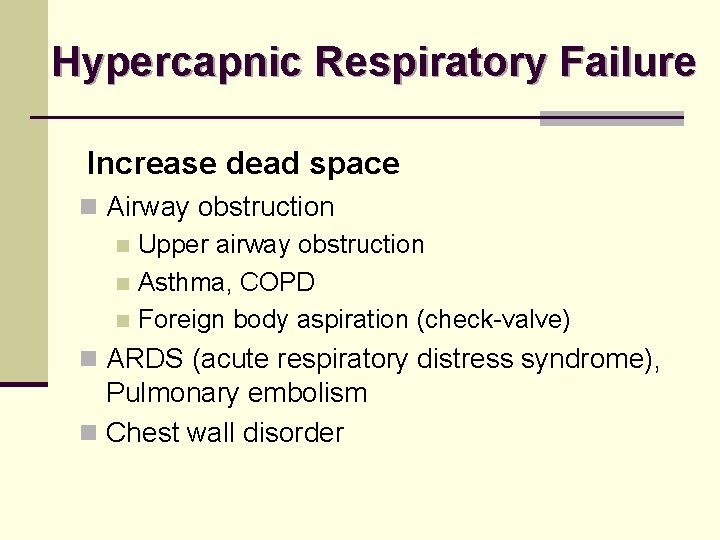
Hypercapnic Respiratory Failure Increase dead space n Airway obstruction n Upper airway obstruction n Asthma, COPD n Foreign body aspiration (check-valve) n ARDS (acute respiratory distress syndrome), Pulmonary embolism n Chest wall disorder
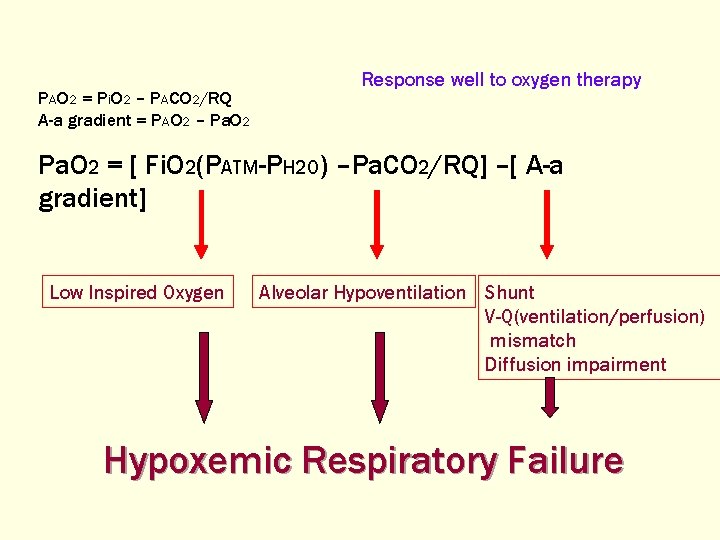
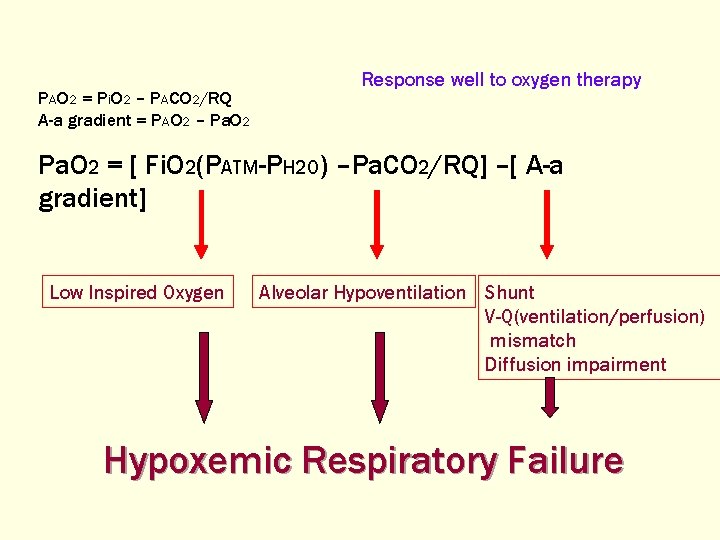
PAO 2 = Pi. O 2 – PACO 2/RQ A-a gradient = PAO 2 – Pa. O 2 Response well to oxygen therapy Pa. O 2 = [ Fi. O 2(PATM-PH 2 O) –Pa. CO 2/RQ] –[ A-a gradient] Low Inspired Oxygen Alveolar Hypoventilation Shunt V-Q(ventilation/perfusion) mismatch Diffusion impairment Hypoxemic Respiratory Failure
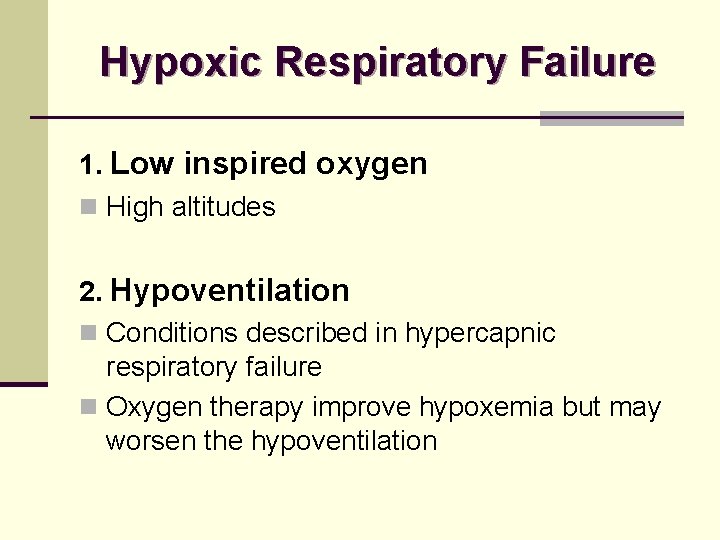
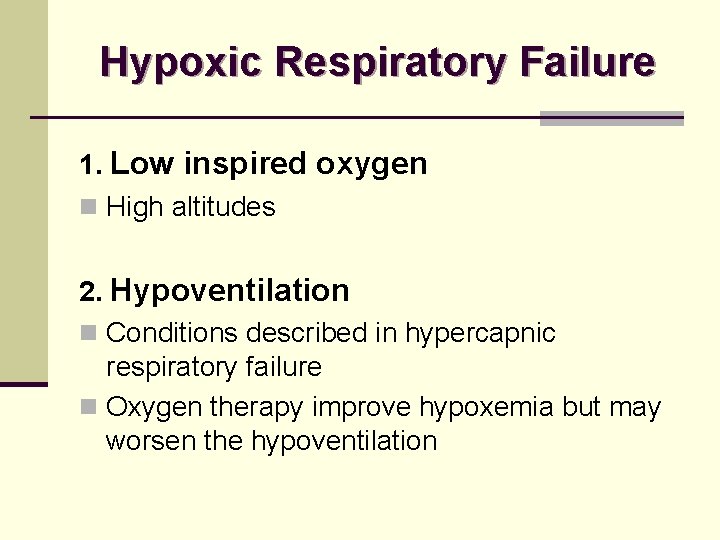
Hypoxic Respiratory Failure 1. Low inspired oxygen n High altitudes 2. Hypoventilation n Conditions described in hypercapnic respiratory failure n Oxygen therapy improve hypoxemia but may worsen the hypoventilation
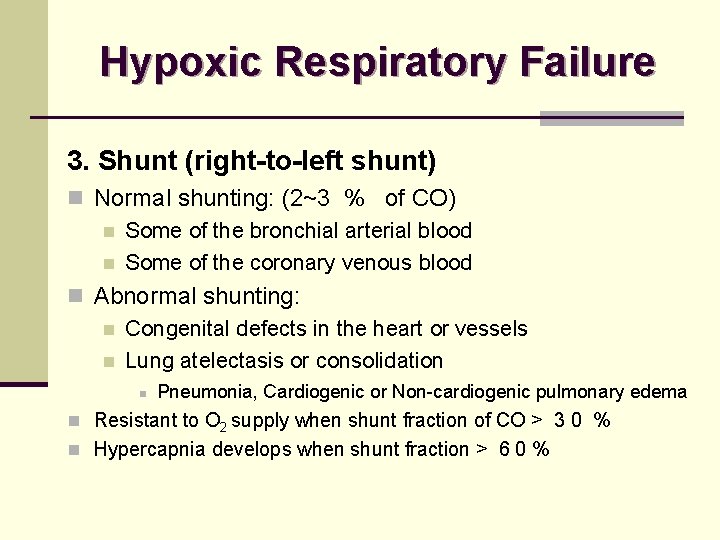
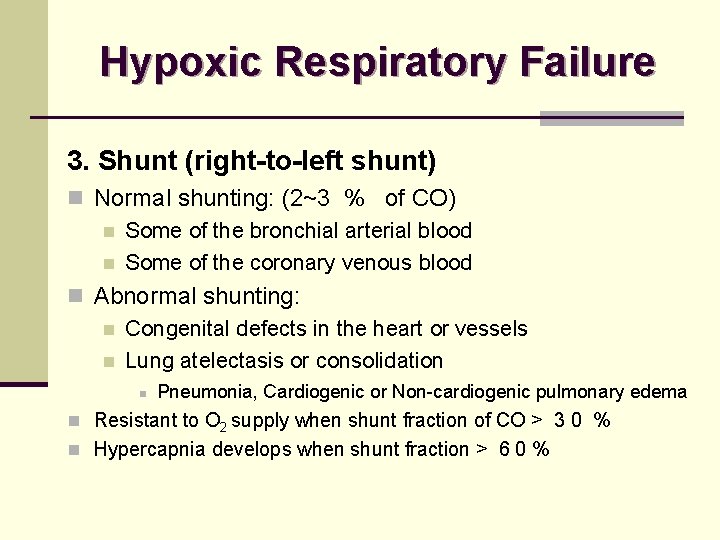
Hypoxic Respiratory Failure 3. Shunt (right-to-left shunt) n Normal shunting: (2~3 % of CO) n Some of the bronchial arterial blood n Some of the coronary venous blood n Abnormal shunting: n Congenital defects in the heart or vessels n Lung atelectasis or consolidation n Pneumonia, Cardiogenic or Non-cardiogenic pulmonary edema n Resistant to O 2 supply when shunt fraction of CO > 3 0 % n Hypercapnia develops when shunt fraction > 6 0 %
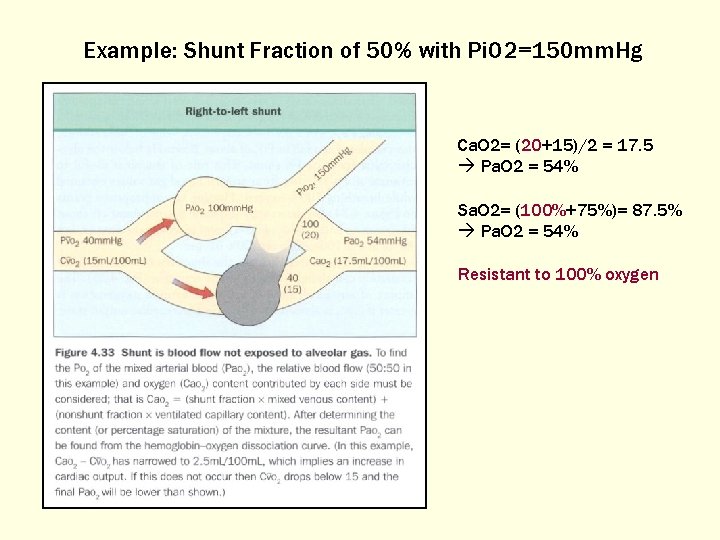
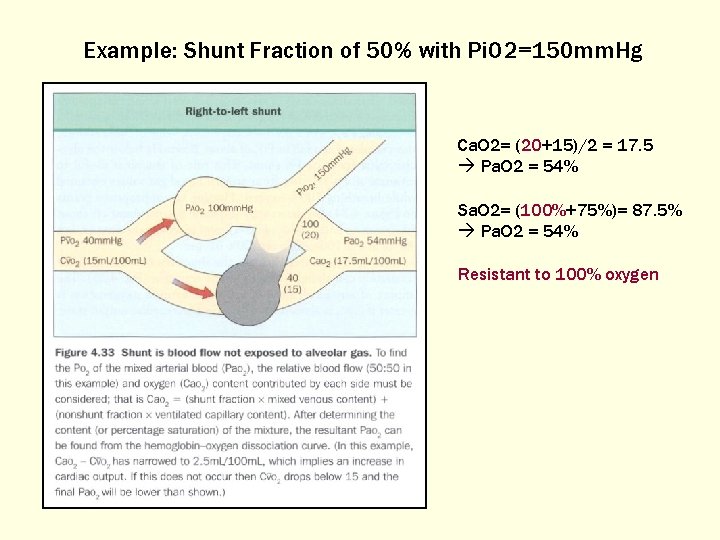
Example: Shunt Fraction of 50% with Pi. O 2=150 mm. Hg Ca. O 2= (20+15)/2 = 17. 5 Pa. O 2 = 54% Sa. O 2= (100%+75%)= 87. 5% Pa. O 2 = 54% Resistant to 100% oxygen
Hypoxic Respiratory Failure 4. Ventilation-Perfusion Mismatch (V-Q) n Vascular obstruction n Pulmonary embolism n Air-space consolidation n Pneumonia, Pulmonary edema
Hypoxic Respiratory Failure 5. Diffusion Impairment n Interstitial lung disease n Pulmonary fibrosis, Connective tissue disease, Interstitial pneumonia, interstitial pulmonary edema n ARDS. RDS n Obstructive lung disease n Emphysema, Asthma
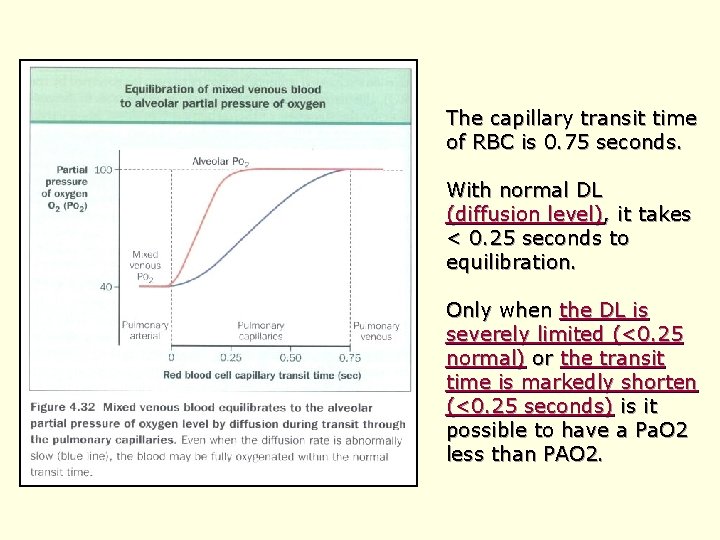
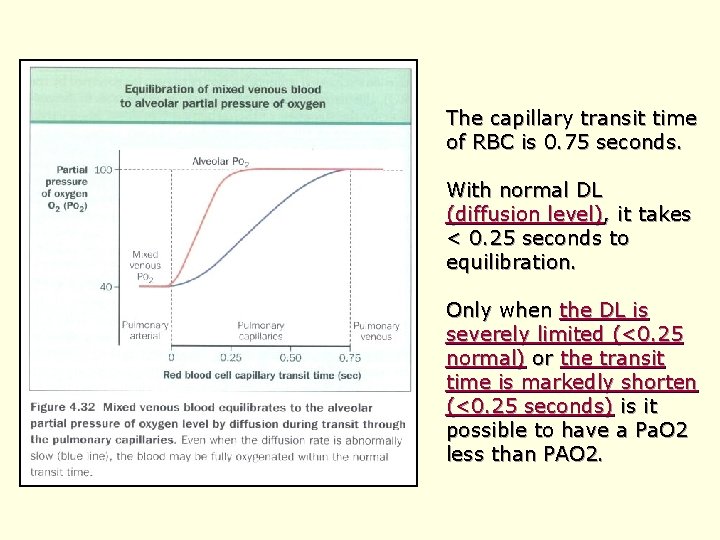
The capillary transit time of RBC is 0. 75 seconds. With normal DL (diffusion level), it takes < 0. 25 seconds to equilibration. Only when the DL is severely limited (<0. 25 normal) or the transit time is markedly shorten (<0. 25 seconds) is it possible to have a Pa. O 2 less than PAO 2.
Approaching a Patient with Respiratory Failure
History & Physical Examination n Acute or Chronic n Underlying ( heart / lung ) diseases n Drugs history n Wheezing? Rhonchus? Diminish breath sound? Air-space consolidation? n Symptoms of heart failure n Clubbing finger
Clinical Presentations of Acute Respiratory Failure n B reath pattern: n rapid-deep rapid-shallow slow-shallow n Accessory respiratory muscles used: n Paradoxical respiration: n Hypoxemia n dizziness, irritable, conscious change, tachycardia, cyanosis, peripheral vasodilatation, pulmonary vasoconstrition. n Hypercapnia n Headache, somnolence, conscious change
Workup n LAB: n Arterial blood gas; Pulse oxymeter n complete blood count (CBC), differential count (DC), Creactive protein n Cardiac enzyme n Electrolytes: K, Pi, Mg… Ca, Na…. n B iochemistry data, n EKG (cardiac echo) n Chest X-ray (chest CT, lung scan) n Lung function test n Pulmonary artery catheter n Neurological exam (Brain CT, EEG……)
Dyspnea n Short of breath n Abnormally uncomfortable awareness of breathing subjectively n Increased work of breath n
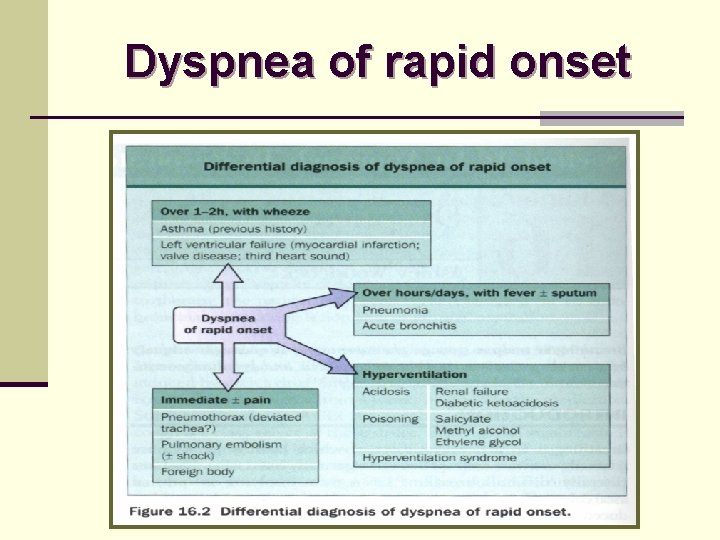
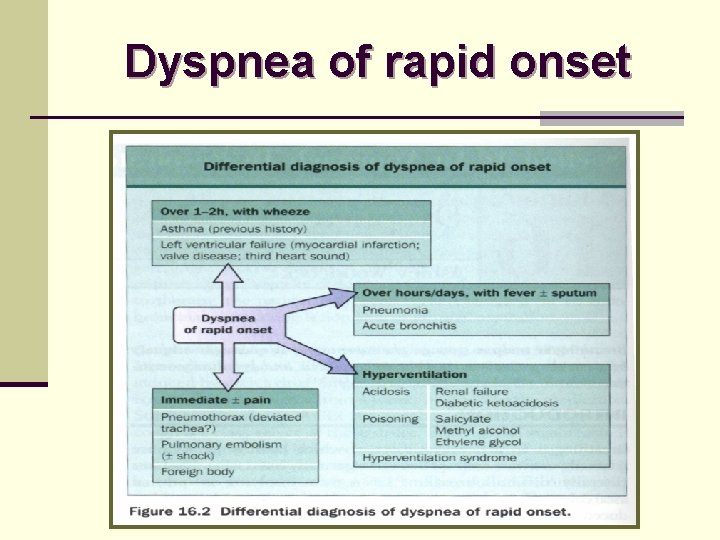
Dyspnea of rapid onset
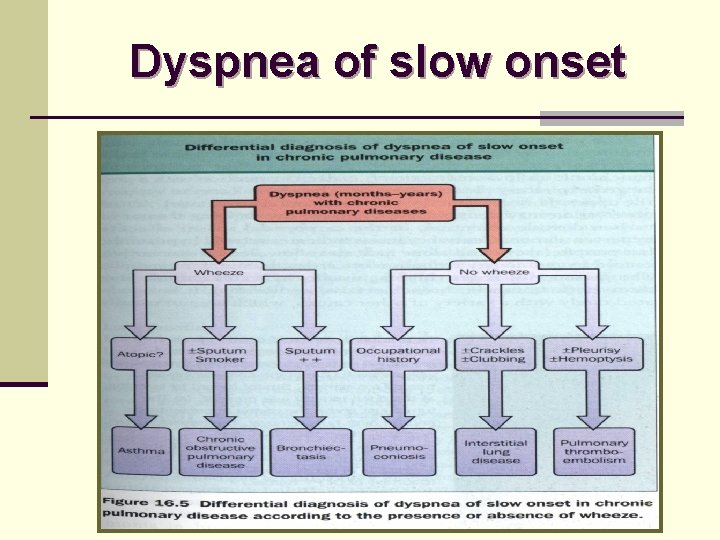
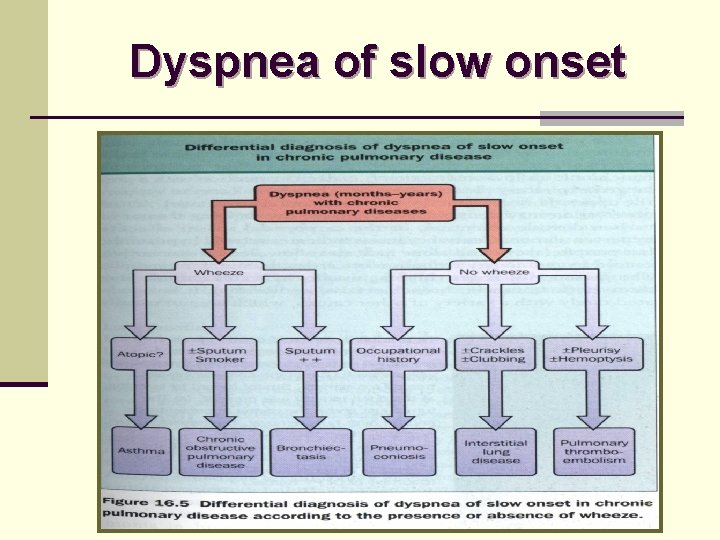
Dyspnea of slow onset
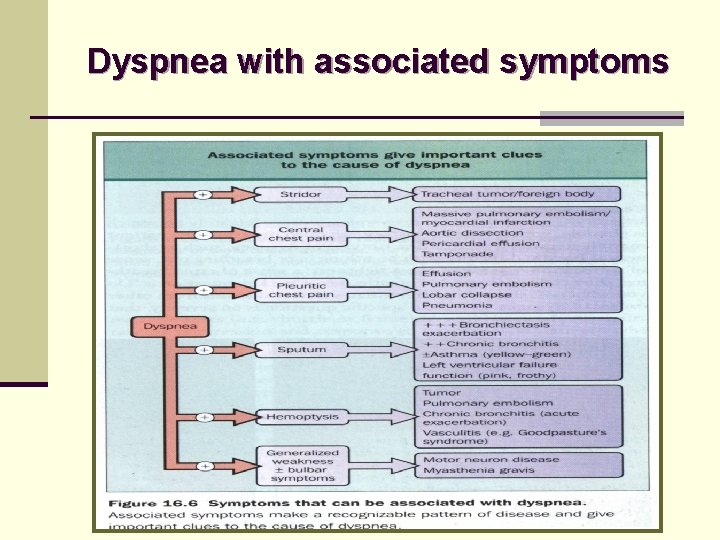
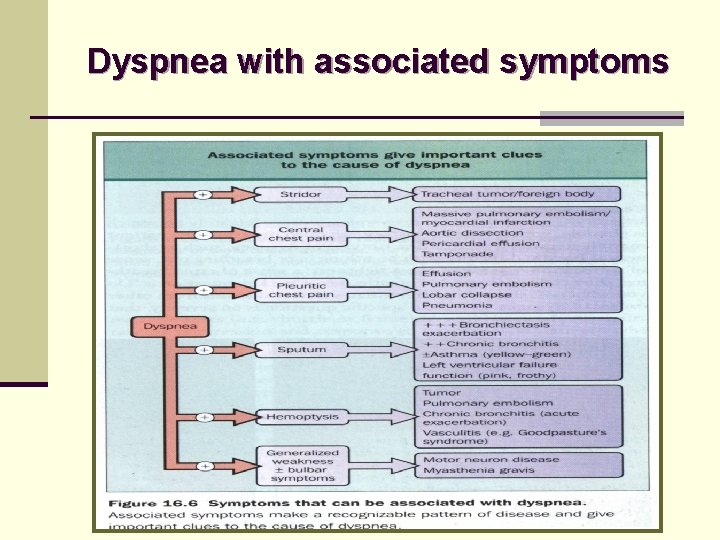
Dyspnea with associated symptoms
Treatment
A…B… C n Establish Airway n Establish Ventilation n Oxygen Therapy n Treat the circulatory failure n Oxygen delivery = {(Sa. O 2·Hb· 1. 3 9) + (0. 0 0 3 ·Pa. O 2)} X Cardiac Output
Airway Management n Head tilt-chin lift / Jaw-thrust maneuver n Artificial airway (Oral or Nasal airway) n Laryngeal Mask Airway n Endo-Tracheal intubation n Emergent Cricothyroidotomy n Tracheostomy




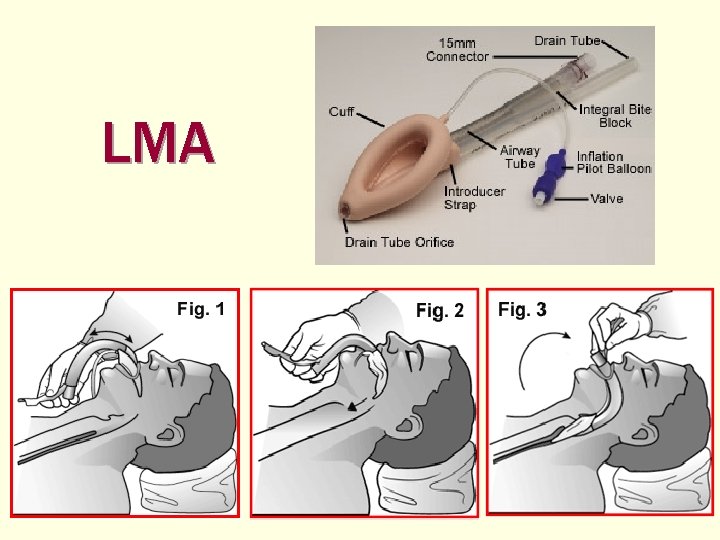
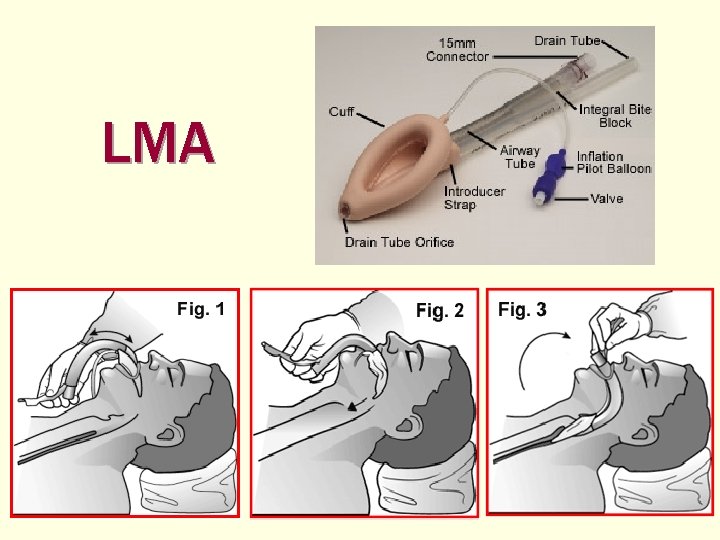
LMA
Endotracheal intubation n Direct oratracheal intubation n B lind nasotracheal intubation n Flexible fiberoptically guided intubation
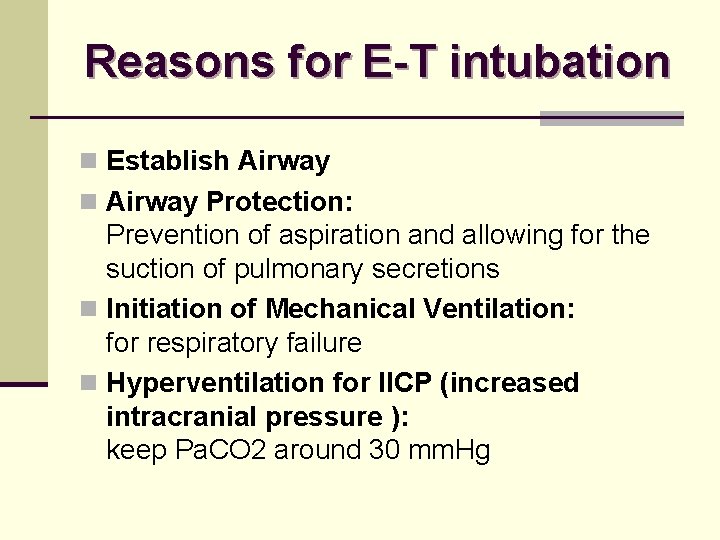
Reasons for E-T intubation n Establish Airway n Airway Protection: Prevention of aspiration and allowing for the suction of pulmonary secretions n Initiation of Mechanical Ventilation: for respiratory failure n Hyperventilation for IICP (increased intracranial pressure ): keep Pa. CO 2 around 30 mm. Hg


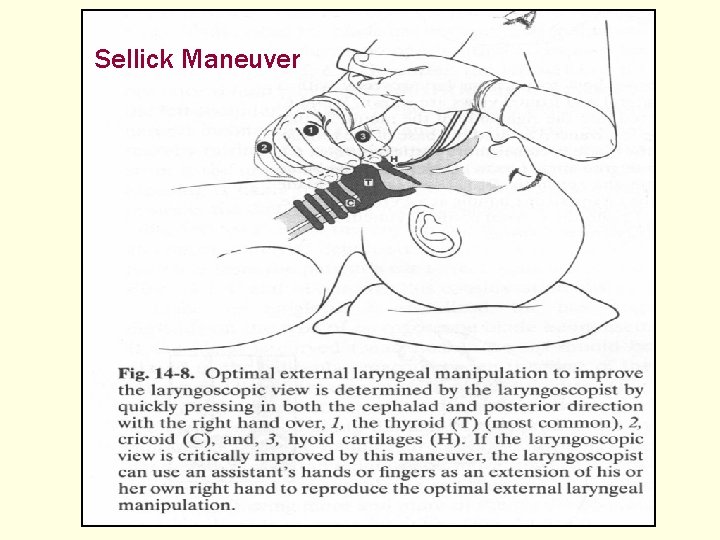
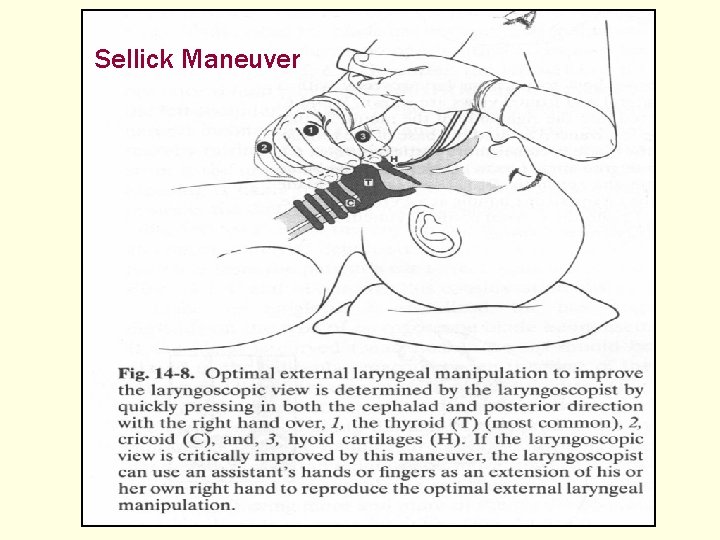
Sellick Maneuver





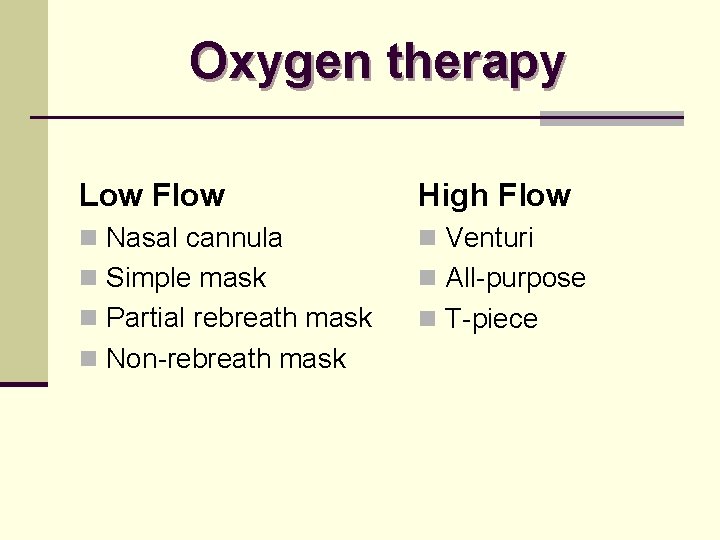
Oxygen therapy Low Flow High Flow n Nasal cannula n Venturi n Simple mask n All-purpose n Partial rebreath mask n T-piece n Non-rebreath mask
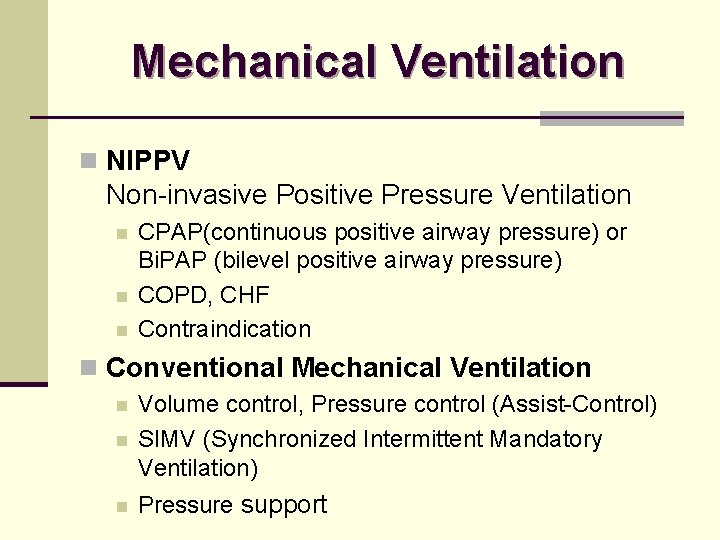
Mechanical Ventilation n NIPPV Non-invasive Positive Pressure Ventilation n CPAP(continuous positive airway pressure) or Bi. PAP (bilevel positive airway pressure) COPD, CHF Contraindication n Conventional Mechanical Ventilation n Volume control, Pressure control (Assist-Control) SIMV (Synchronized Intermittent Mandatory Ventilation) n Pressure support n
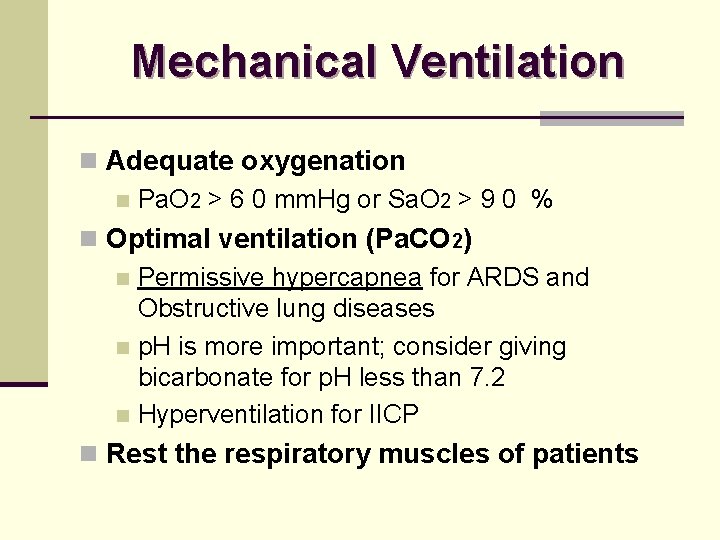
Mechanical Ventilation n Adequate oxygenation n Pa. O 2 > 6 0 mm. Hg or Sa. O 2 > 9 0 % n Optimal ventilation (Pa. CO 2) n Permissive hypercapnea for ARDS and Obstructive lung diseases n p. H is more important; consider giving bicarbonate for p. H less than 7. 2 n Hyperventilation for IICP n Rest the respiratory muscles of patients
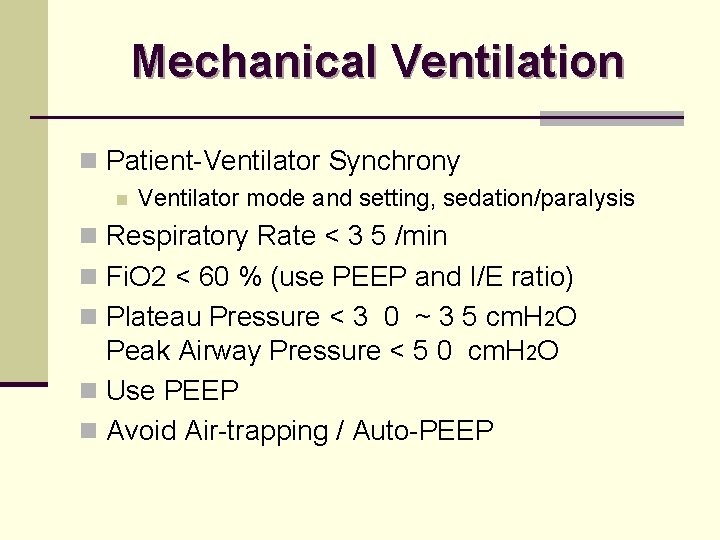
Mechanical Ventilation n Patient-Ventilator Synchrony n Ventilator mode and setting, sedation/paralysis n Respiratory Rate < 3 5 /min n Fi. O 2 < 60 % (use PEEP and I/E ratio) n Plateau Pressure < 3 0 ~ 3 5 cm. H 2 O Peak Airway Pressure < 5 0 cm. H 2 O n Use PEEP n Avoid Air-trapping / Auto-PEEP

Thank you for your attention!!!
 Lahey clinic anesthesiology residency
Lahey clinic anesthesiology residency Odessa state environmental university
Odessa state environmental university Odessa state environmental university
Odessa state environmental university Umass memorial pharmacy
Umass memorial pharmacy Oc techs
Oc techs Coding bootcamps odessa
Coding bootcamps odessa Kiev odessa
Kiev odessa Brenntag lachine
Brenntag lachine What are the central plains
What are the central plains Jobsindice.com odessa tx
Jobsindice.com odessa tx Odessa commercial sea port
Odessa commercial sea port M.gorky donetsk national medical university
M.gorky donetsk national medical university Seoul national university history
Seoul national university history Mongolian national university of medical sciences
Mongolian national university of medical sciences Intensive intervention definition
Intensive intervention definition National center on intensive intervention
National center on intensive intervention Indiana university intensive english program
Indiana university intensive english program Tracer card medical record
Tracer card medical record Medical education and drugs department
Medical education and drugs department National risk and resilience unit
National risk and resilience unit National core standards assessment tools
National core standards assessment tools Function of national audit department in malaysia
Function of national audit department in malaysia Department of law university of jammu
Department of law university of jammu Department of geology university of dhaka
Department of geology university of dhaka University of padova psychology department
University of padova psychology department University of bridgeport it department
University of bridgeport it department Iowa state math department
Iowa state math department Department of physics university of tokyo
Department of physics university of tokyo Texas state university psychology department
Texas state university psychology department Department of information engineering university of padova
Department of information engineering university of padova Information engineering padova
Information engineering padova Manipal university chemistry department
Manipal university chemistry department Syracuse university pool
Syracuse university pool Jackson state university finance department
Jackson state university finance department Mice.cs.columbia
Mice.cs.columbia Michigan state physics
Michigan state physics Columbia university cs department
Columbia university cs department University of sargodha engineering department
University of sargodha engineering department Stanford university philosophy department
Stanford university philosophy department California medical license application
California medical license application Gbmc infoweb
Gbmc infoweb Hepburn osteometric board
Hepburn osteometric board Torrance memorial map
Torrance memorial map Cartersville medical center medical records
Cartersville medical center medical records National board certification for medical interpreters
National board certification for medical interpreters National ambulatory medical care survey
National ambulatory medical care survey Ibn sina national college for medical studies
Ibn sina national college for medical studies University medical centre maribor
University medical centre maribor Liaoning medical university
Liaoning medical university Vietnam military medical university
Vietnam military medical university Masaryk university medical faculty
Masaryk university medical faculty Ibn sina university of medical and pharmaceutical sciences
Ibn sina university of medical and pharmaceutical sciences Kirovohrad medical university
Kirovohrad medical university