Nontoxic goitre Dr Madhukar Mittal Medical Endocrinology Goitre
- Slides: 51
Nontoxic goitre Dr Madhukar Mittal Medical Endocrinology
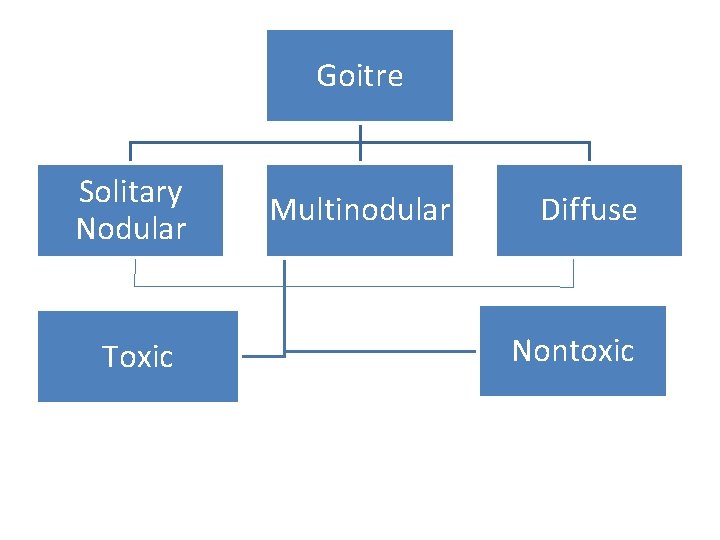
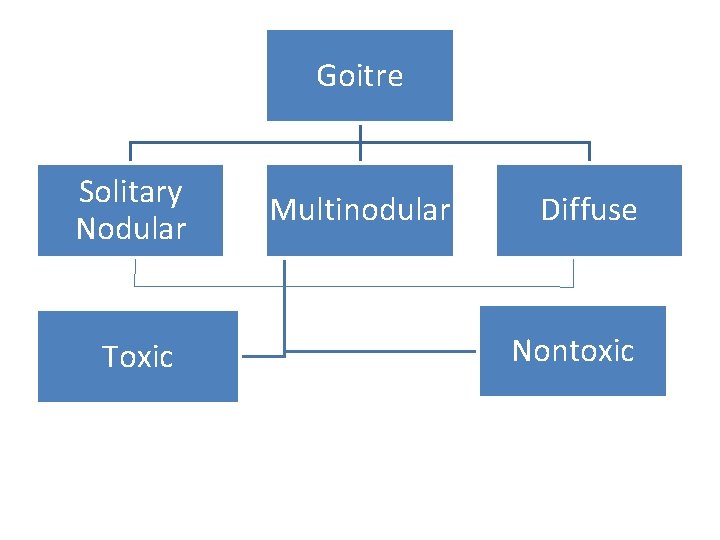
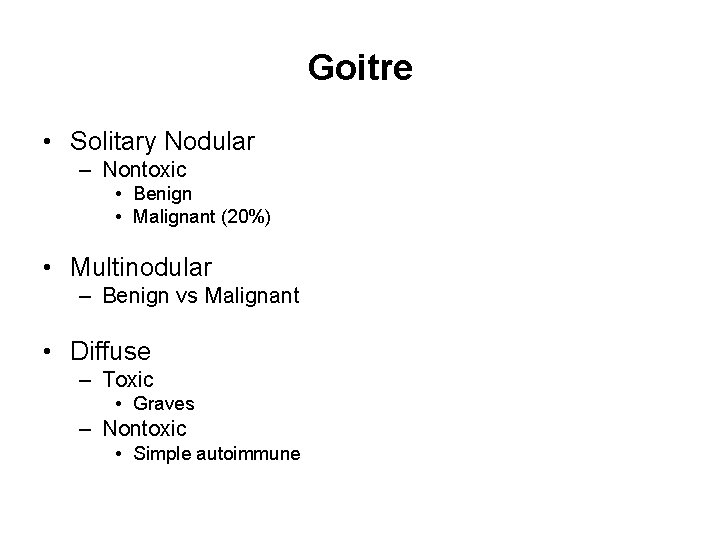
Goitre Solitary Nodular Toxic Multinodular Diffuse Nontoxic
Goitre • Solitary Nodular – Nontoxic • Benign • Malignant (20%) • Multinodular – Benign vs Malignant • Diffuse – Toxic • Graves – Nontoxic • Simple autoimmune
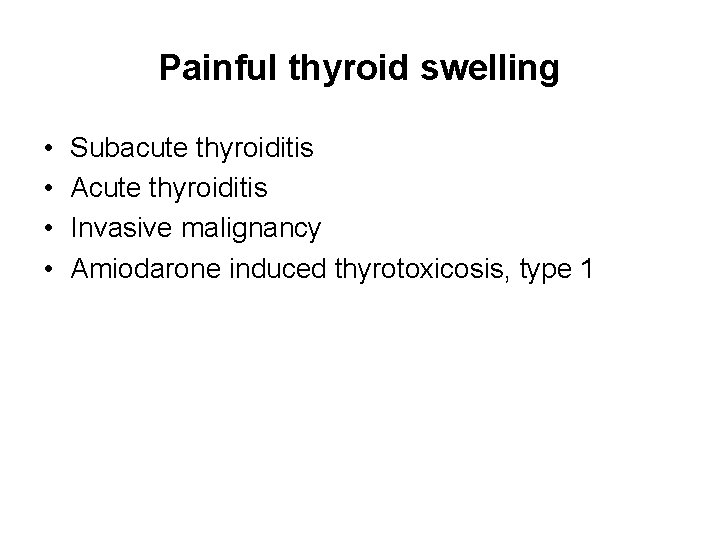
Painful thyroid swelling • • Subacute thyroiditis Acute thyroiditis Invasive malignancy Amiodarone induced thyrotoxicosis, type 1
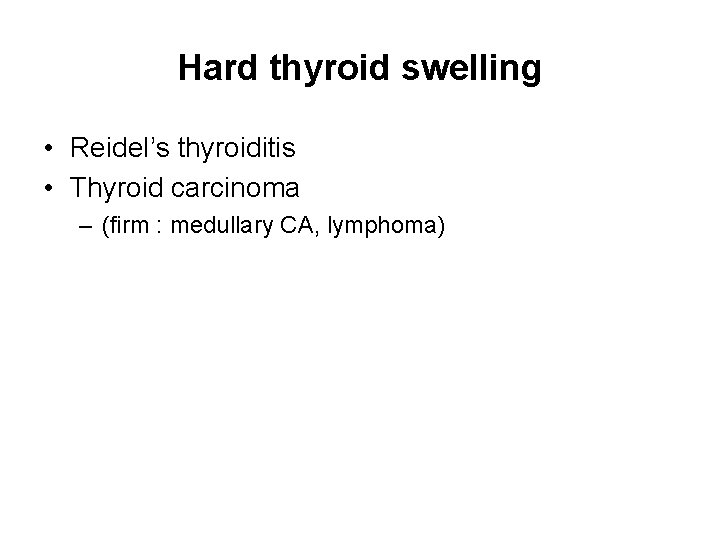
Hard thyroid swelling • Reidel’s thyroiditis • Thyroid carcinoma – (firm : medullary CA, lymphoma)
Thyroid examination • From behind with neck flexed slightly forward • Rt lobe is 25% larger than left lobe • Palpable and smooth normally
Midline neck swellings • Goitre of thyroid isthmus & pyramidal lobe • Thyroglossal cyst • Suprasternal LN, lipoma • Ludwig’s angina • Submental LN • Sublingual dermoid, lipoma
Lateral neck swellings • Carotid triangle – – Thyroid Branchial cyst Carotid body tumor Carotid artery aneurysm • Submandibular triangle – LN – Enlarged submandibular salivary gland • Post triangle – – – LN Cystic hygroma Pharyngeal pouch Subclavian aneurysm Cervical rib
Thyroid • 12 -20 g • Between cricoid cartilage & suprasternal notch • Develops during 3 rd week of GA from floor of primitive pharynx • Hormone synthesis begins at 11 weeks GA • Parathyroid glands located in posterior region of each pole of thyroid • C cells : interspersed throughout thyrod gland
Thyroid examination • Normally • Pizillo’s method – Hands clasped behind head and push • On swallowing – – Thyroid moves up Thyroglossal cysts Subhyoid bursitis Fixed prelaryngeal/pretracheal LN • For retrosternal goitre – Raise both arms till they touch ears – Pemberton’s sign
Thyroid examination • From behind with neck flexed • Lahey’s method – With both hands • Crile’s method – With thumb • Kocher’s test – Slight push on lat lobes produces stridor • To exclude retrosternal prolongation
History • Age – Young – colloid goitre, STN – Middle age – hashimoto’s, follicular CA • • • Residence Pain Sleep Compressive symp Others – – Respiratory Myopathy Cardiac Neurologic • Family H/O
Examination • • • Anemia BP Pulse rate Skin of hands (moist, hot/cold) Tremors – hand, tongue LN Facies Eye signs Dermopathy Acropachy Vitiligo
Malignancy • Hard swelling • Local signs – Dyspnea, dysphagia, hoarseness of voice – Carotid pulsations cannot be felt • • • LN – papillary, anaplastic Metastases – follicular (bone, lungs) Recent increase in size of swelling with pain Diarrhea – medullary CA Prior h/o irradiation STN – – Male Solid nodule Large nodule >4 cm Cold nodule (least imp sign)
Treatment
• Hypothyroidism – Levothyroxine • Hyperthyroidism of Graves disease – Antithyroid drugs (Europe, Japan) – Radioiodine (USA)
Acute thyroiditis • Antibiotics • Drainage of abscess
Subacute thyroiditis • • Aspirin – large doses 600 mg 4 -6 hrly Prednisolone 40 -60 mg/d Thyrotoxic phase – β-blockers Hypothyroid phase – low dose levothyroxine
Silent thyroiditis • Thyrotoxic phase – propranolol 20 -40 mg TDS/QID • Hypothyroid phase – LT 4 for 6 -9 months • Annual followup for permanent hypothyroidism
Reidel’s thyroidits • Surgery • + tamoxifen
Amiodarone induced • Hypothyroidism – LT 4 • Thyrotoxicosis type 1 – Stop amiodarone if possible – High doses of ATD • Thyrotoxicosis type 2 – – – Oral contrast agents (Na ipodoate, Na tyropanoate) K perchlorate Glucocorticoids Lithium Near total thyroidectomy
Simple goitre 1. I 2 or suppressive thyroxine therapy (young patients with soft goitre for 3 -6 months) 2. Radioiodine (decreases goitre size by 50%) 3. Sx – for tracheal compression
MNG - toxic 1. Sx 2. Radioiodine in elderly 3. Antithyroid drugs – often stimulate growth of goitre
MNG nontoxic 1. Radioiodine 2. Sx 3. T 4 suppressive therapy (rarely effective for decreasing goitre size)
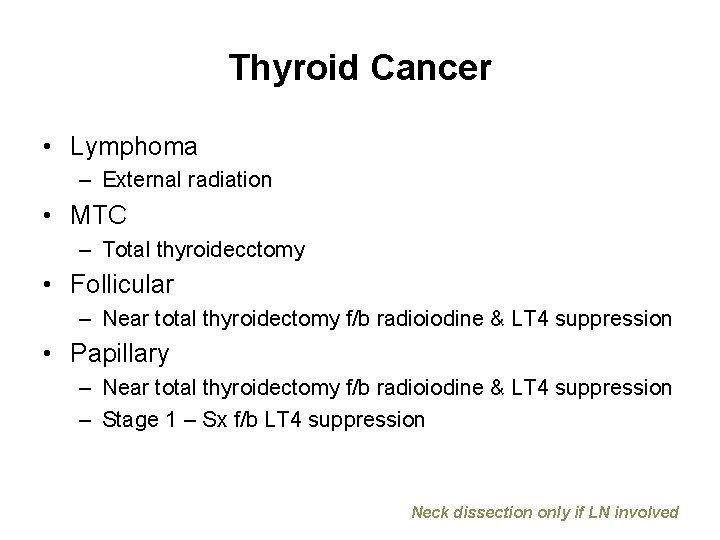
Thyroid Cancer • Lymphoma – External radiation • MTC – Total thyroidecctomy • Follicular – Near total thyroidectomy f/b radioiodine & LT 4 suppression • Papillary – Near total thyroidectomy f/b radioiodine & LT 4 suppression – Stage 1 – Sx f/b LT 4 suppression Neck dissection only if LN involved
STN Hyperfunctioning 1. Radioiodine ablation – esp >45 yr 2. Sx resection – esp <45 yr – Enucleation – Lobectomy 3. Ethanol injection
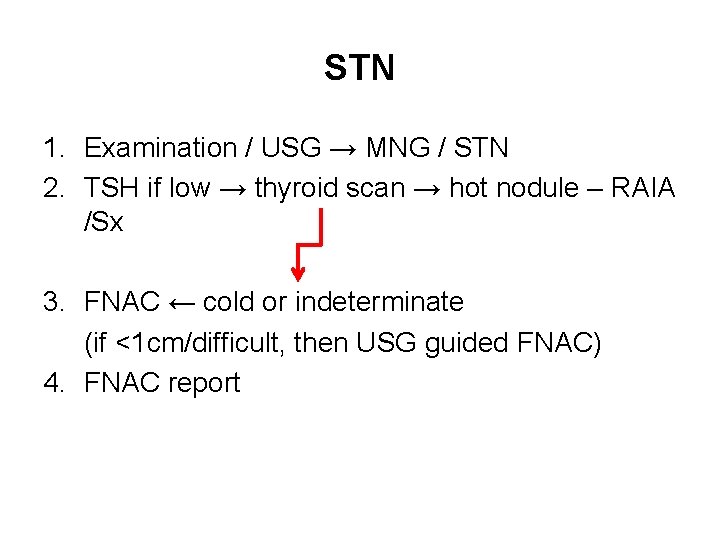
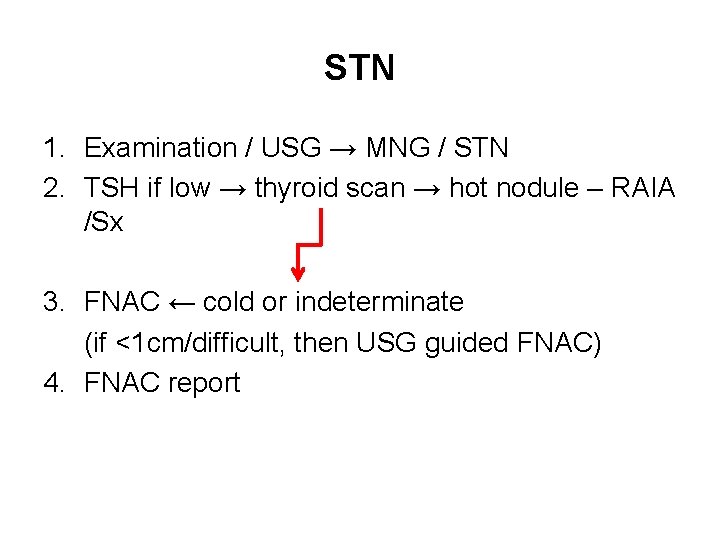
STN 1. Examination / USG → MNG / STN 2. TSH if low → thyroid scan → hot nodule – RAIA /Sx 3. FNAC ← cold or indeterminate (if <1 cm/difficult, then USG guided FNAC) 4. FNAC report
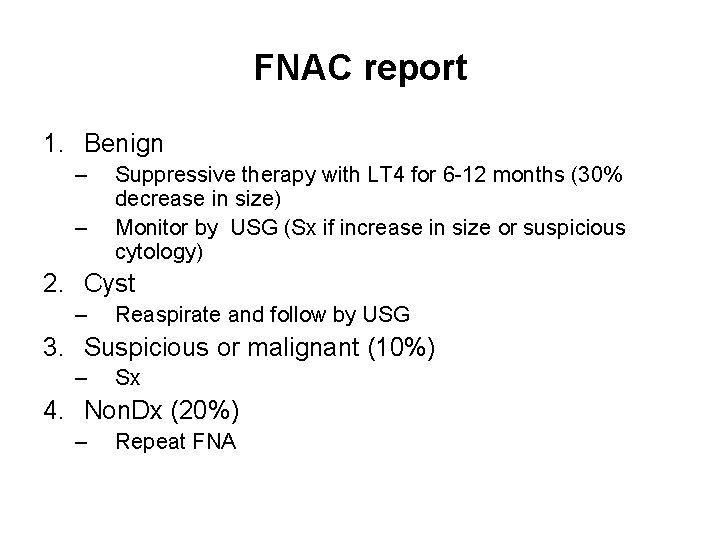
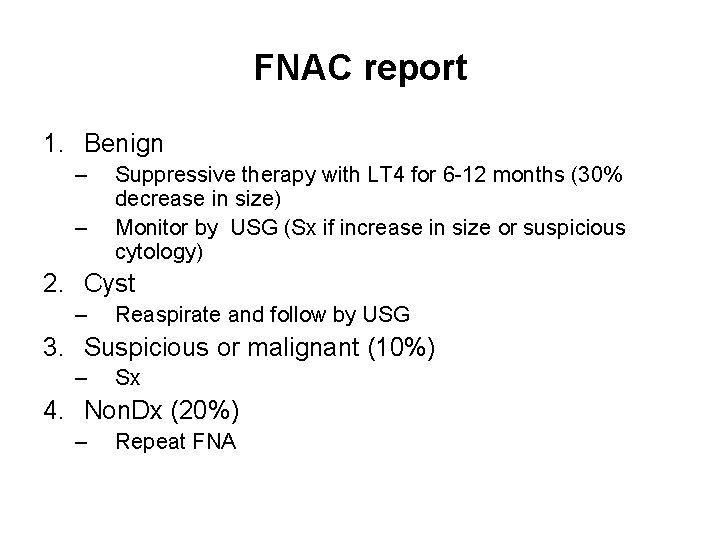
FNAC report 1. Benign – – Suppressive therapy with LT 4 for 6 -12 months (30% decrease in size) Monitor by USG (Sx if increase in size or suspicious cytology) 2. Cyst – Reaspirate and follow by USG 3. Suspicious or malignant (10%) – Sx 4. Non. Dx (20%) – Repeat FNA
MNG
Nontoxic MNG • • • Occurs in up to 12% of adults More common in females Increased prevalence with age More common in iodine deficient regions Most nodules are polyclonal in origin
Risk Factors • Iodine deficiency • Radiation exposure • Exposure to iodine from contrast dyes or other sources may precipitate or exacerbate thyrotoxicosis in MNG
Etiology • Pathogenesis of MNG is multifactorial. – Genetic – Autoimmune – Environmental • Major difference between toxic and nontoxic MNG – Toxic MNG evolves from nontoxic MNG as part of the natural history of the disease • Stages of nodular transformation of the thyroid – Goitrogenic stimuli (iodine deficiency, autoimmunity, or nutritional goitrogens) cause diffuse thyroid hyperplasia – In the proliferating thyroid, growth factor expression is increased, stimulating cellular division and formation of independent clones – Most nodules in MNG are polyclonal in origin, but monoclonal nodules also occur
Diagnosis • Detection of MNG by physical examination depends on goiter and nodule size, location, and anatomy of the patient’s neck • Laboratory evaluation – Determination of serum TSH will distinguish nontoxic MNG from toxic MNG • Diagnostic imaging is indicated in following situations: – To verify hyperfunctioning nodules in a patient with a MNG and concomitant clinical and/or laboratory evidence of hyperthyroidism – To evaluate the degree of obstruction in large MNG • Fine-needle aspiration (FNA) biopsy – A dominant or enlarging nodule within MNG – Nonfunctioning (cold) nodules ≥ 1– 1. 5 cm in diameter – Nodules found to have microcalcifications, hypoechogenicity, complex architecture, or increased vascularity on ultrasonography – FNA should not be used to evaluate autonomous (warm/hot) nodules
Imaging • X-ray, CT, or MRI of the neck/chest indicated only when necessary for: – Goiter anatomy – Substernal extension – Extent of tracheal compression • Iodinated contrast agents should be administered cautiously to persons with a low TSH level – May precipitate or exacerbate underlying hyperthyroidism – Consider pretreatment with antithyroid drug therapy before imaging with contrast agents
Imaging • Thyroid scintigraphy (123 iodine or 99 mtechnetium) – Limited to patients with a low TSH level to verify the clinical diagnosis of toxic MNG – Unnecessary in the setting of a normal TSH level. – Toxic MNG shows heterogeneous iodine uptake with multiple regions of increased and decreased uptake • Ultrasonography – Recommended for all patients with known or suspected thyroid nodules – Useful for accurate monitoring of nodule size or for guiding FNA biopsy of suspicious nodules
Endemic goitre • More common in mountainous regions • Diffuse goitre caused by I 2 deficiency affecting >5% of population comprising children
Thank You
Iodine Deficiency
Iodine Deficiency • Iodine is an essential micronutrient – T 4 synthesis – Brain growth and development • Daily requirement (adult) 150 ug/day – 1 teaspoonful of iodine is sufficient for lifetime • Iodine deficiency causes a wide spectrum of illness collectively termed iodine deficiency disorders (IDD)
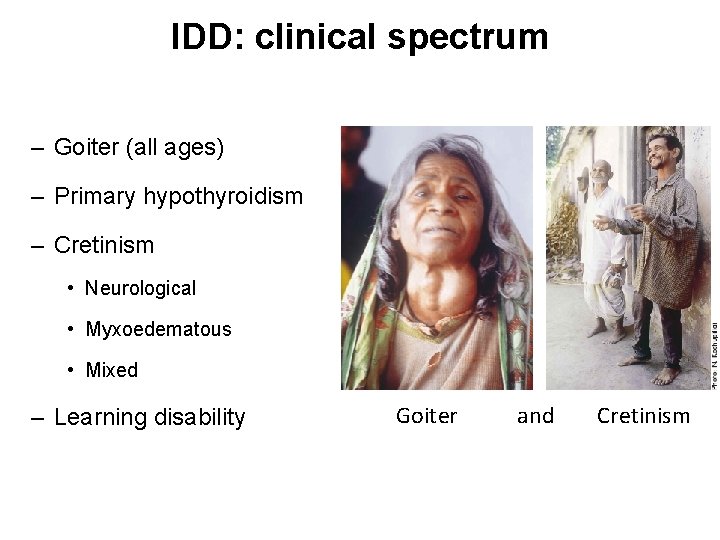
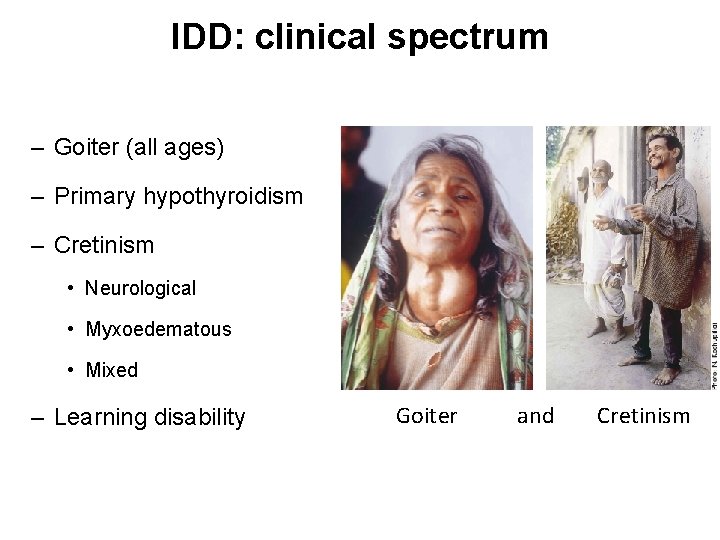
IDD: clinical spectrum – Goiter (all ages) – Primary hypothyroidism – Cretinism • Neurological • Myxoedematous • Mixed – Learning disability Goiter and Cretinism
IDD • Mild iodine deficiency causes, in children, poor school performance, reduced intellectual ability and impaired work capacity 1, 2 • Results – Compromised human potential – Poor socio-economic development • On a worldwide basis, iodine deficiency is the single most important preventable cause of brain damage 1. 2. Tiwari BD, Godbole MM, et al. Learning disabilities and poor motivation to achieve due to prolonged iodine deficiency. Am J Clin Nutr 1996; 63: 782– 6. Kochupillai N. , The impact of iodine deficiency on human resource development. Prog Food Nutr Sci. 1989; 13(1): 1 -15. Review.
IDD: Causes • Low dietary iodine contents – Soil with low iodine content due to past glaciations or the repeated leaching effects of snow, water (floods) and heavy rainfall • Crops grown in this soil, therefore, do not provide adequate amounts of iodine when consumed
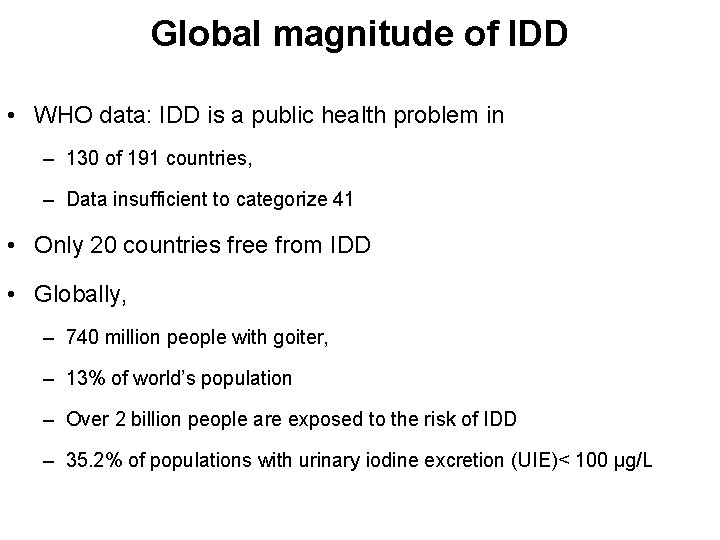
Global magnitude of IDD • WHO data: IDD is a public health problem in – 130 of 191 countries, – Data insufficient to categorize 41 • Only 20 countries free from IDD • Globally, – 740 million people with goiter, – 13% of world’s population – Over 2 billion people are exposed to the risk of IDD – 35. 2% of populations with urinary iodine excretion (UIE)< 100 µg/L
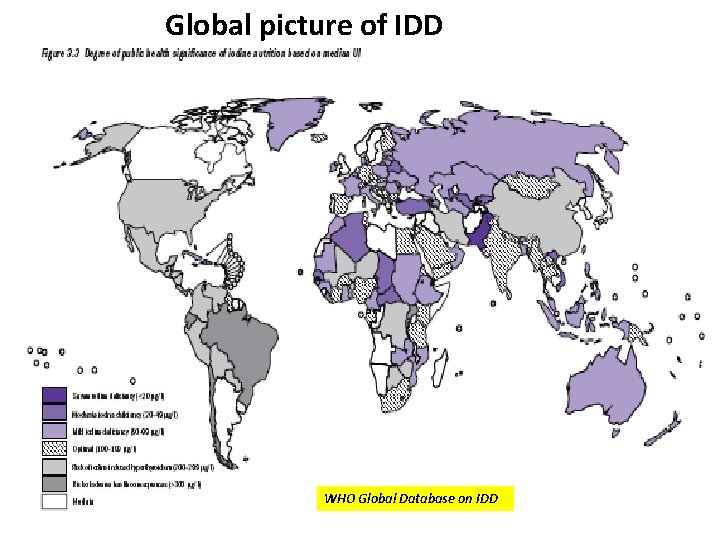
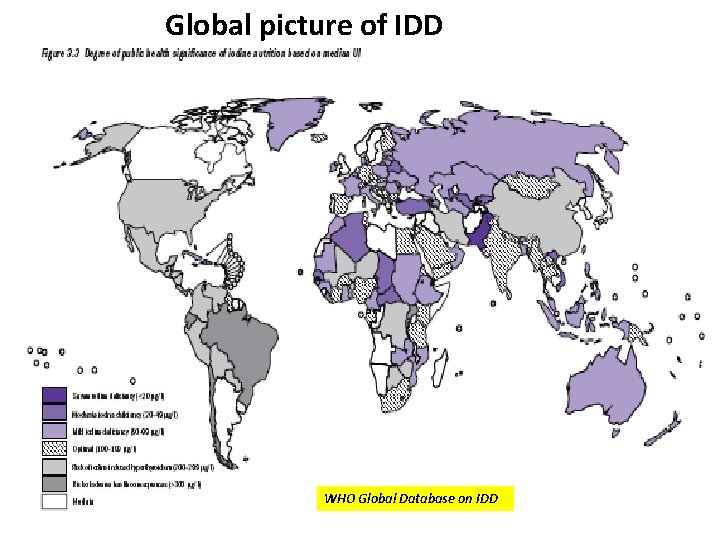
Global picture of IDD WHO Global Database on IDD
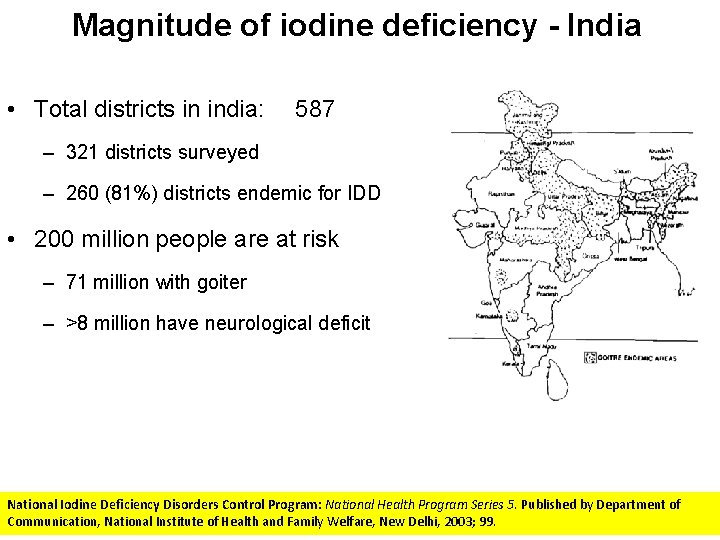
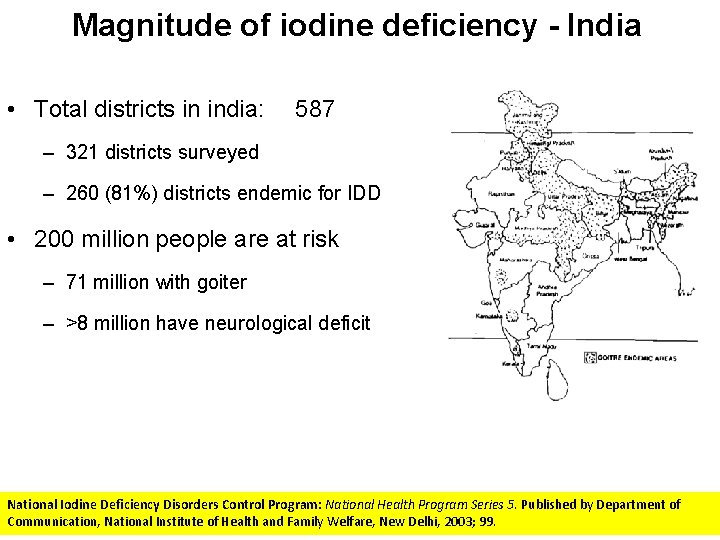
Magnitude of iodine deficiency - India • Total districts in india: 587 – 321 districts surveyed – 260 (81%) districts endemic for IDD • 200 million people are at risk – 71 million with goiter – >8 million have neurological deficit National Iodine Deficiency Disorders Control Program: National Health Program Series 5. Published by Department of Communication, National Institute of Health and Family Welfare, New Delhi, 2003; 99.
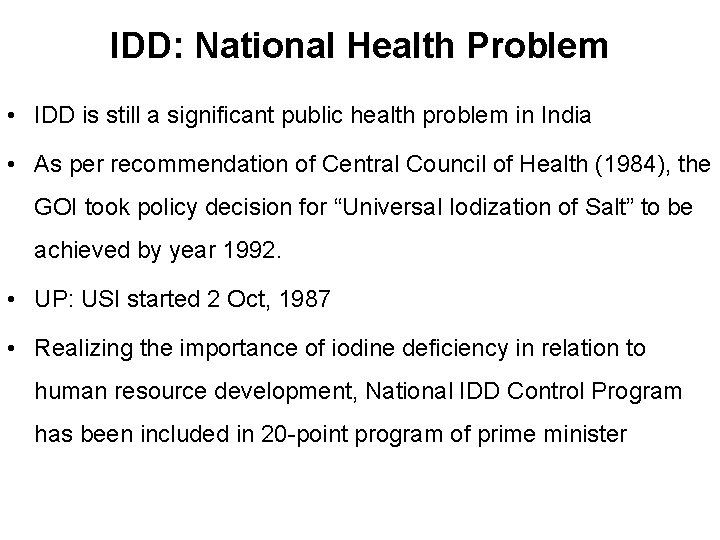
IDD: National Health Problem • IDD is still a significant public health problem in India • As per recommendation of Central Council of Health (1984), the GOI took policy decision for “Universal Iodization of Salt” to be achieved by year 1992. • UP: USI started 2 Oct, 1987 • Realizing the importance of iodine deficiency in relation to human resource development, National IDD Control Program has been included in 20 -point program of prime minister
Shift in policies in salt iodination • 1992: sale of non-iodized salt declared as punishable offence • 2000: Punitive clause removed through Central notification • 2005, Nov: Punitive clause restored
Non-uniform Iodized salt distribution in India • The use of iodized salt varies dramatically from one state to another • Why: number of factors – scale of salt production, – transportation requirements, – enforcement efforts, – differences in state regulations, – the pricing structure, and – storage patterns
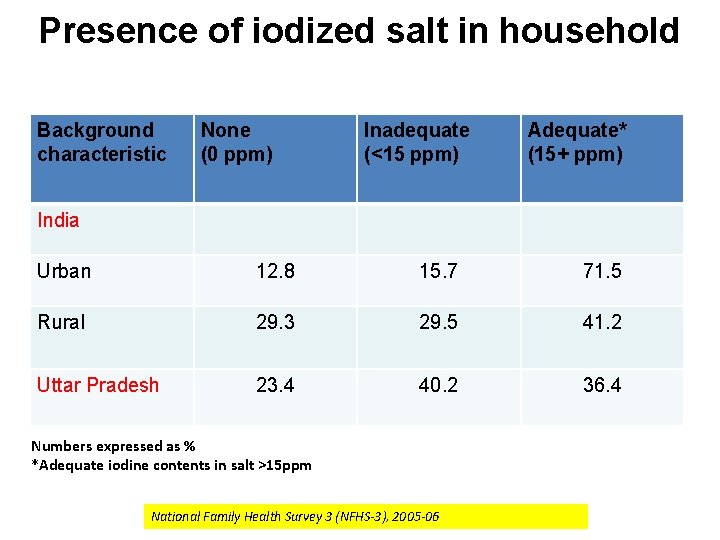
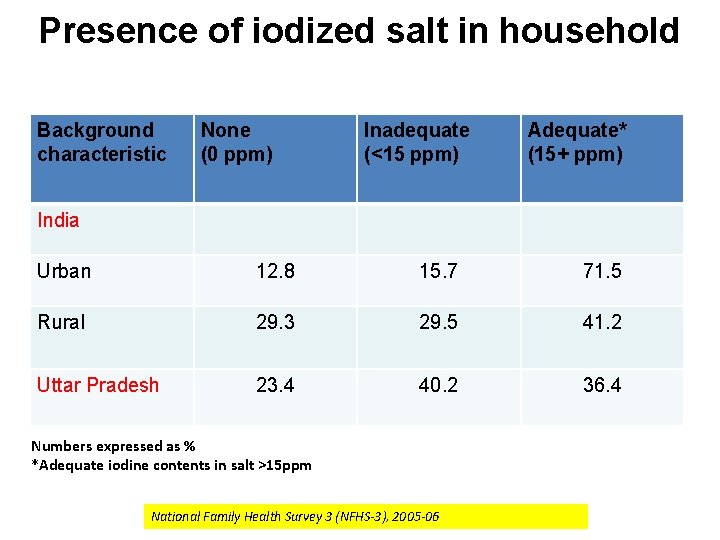
Presence of iodized salt in household Background characteristic None (0 ppm) Inadequate (<15 ppm) Adequate* (15+ ppm) India Urban 12. 8 15. 7 71. 5 Rural 29. 3 29. 5 41. 2 Uttar Pradesh 23. 4 40. 2 36. 4 Numbers expressed as % *Adequate iodine contents in salt >15 ppm National Family Health Survey 3 (NFHS-3), 2005 -06
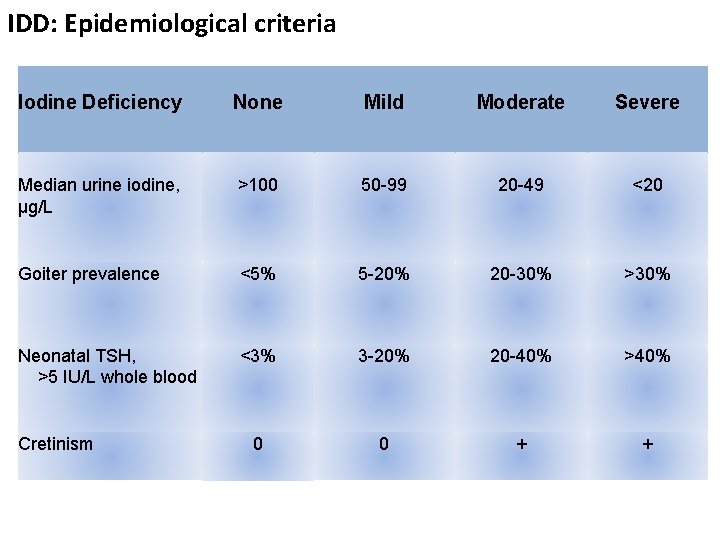
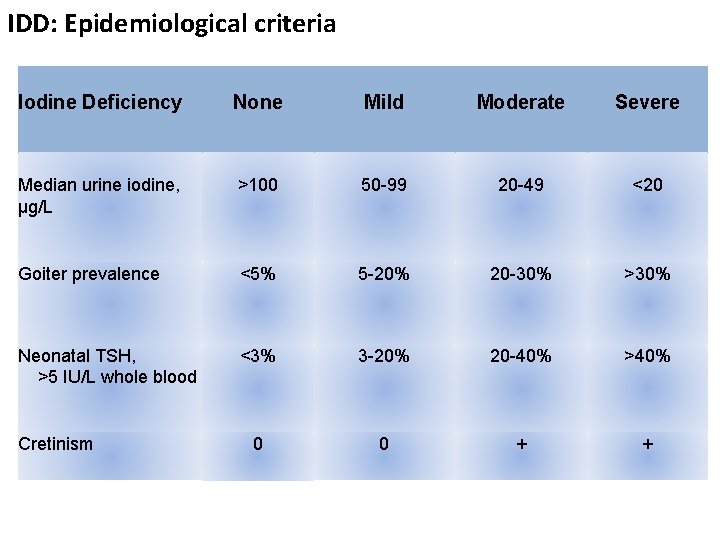
IDD: Epidemiological criteria Iodine Deficiency None Mild Moderate Severe Median urine iodine, µg/L >100 50 -99 20 -49 <20 Goiter prevalence <5% 5 -20% 20 -30% >30% Neonatal TSH, >5 IU/L whole blood <3% 3 -20% 20 -40% >40% 0 0 + + Cretinism
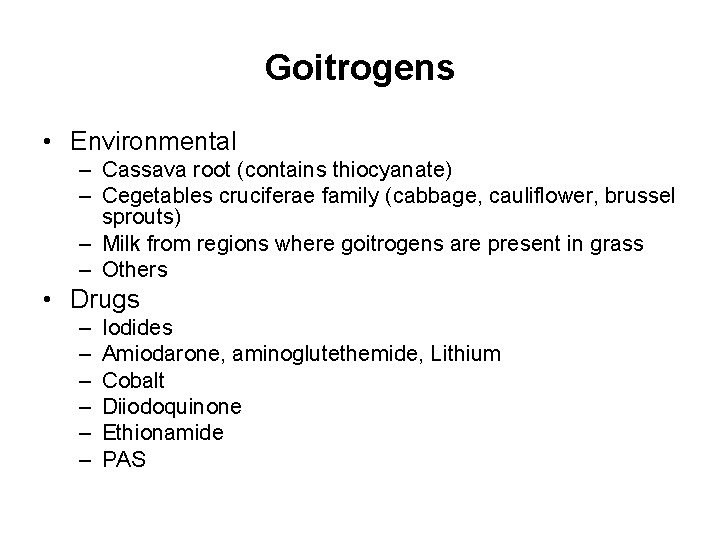
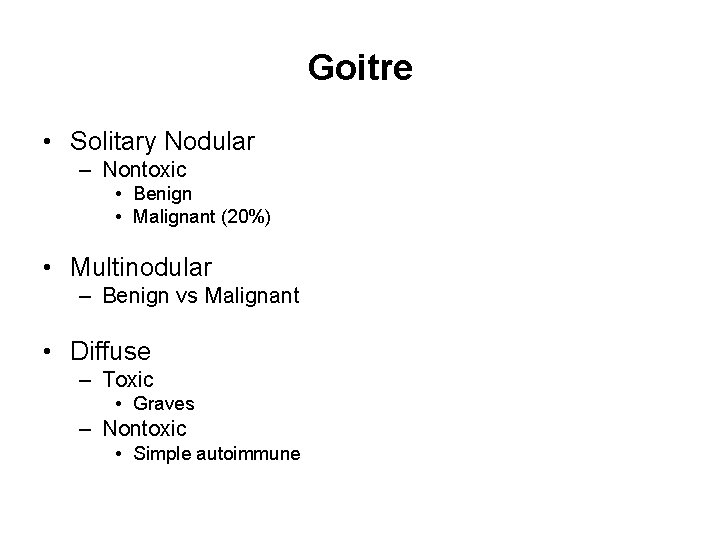
Goitrogens • Environmental – Cassava root (contains thiocyanate) – Cegetables cruciferae family (cabbage, cauliflower, brussel sprouts) – Milk from regions where goitrogens are present in grass – Others • Drugs – – – Iodides Amiodarone, aminoglutethemide, Lithium Cobalt Diiodoquinone Ethionamide PAS
 Synthesis and secretion of thyroid hormones
Synthesis and secretion of thyroid hormones Pizillo method
Pizillo method Primary aldo
Primary aldo Root prefix suffix sistem endokrin
Root prefix suffix sistem endokrin Reproductive biology and endocrinology
Reproductive biology and endocrinology 2232021
2232021 Reproductive endocrinology near campbell
Reproductive endocrinology near campbell Endocrinology of pregnancy
Endocrinology of pregnancy Endocrinology
Endocrinology Park nicollet pediatric endocrinology
Park nicollet pediatric endocrinology Goitre plongeant photo
Goitre plongeant photo Goitre
Goitre Classification of goitre
Classification of goitre Goitre classification
Goitre classification Endocrine disorder
Endocrine disorder Goitre
Goitre Dr madhukar bhide
Dr madhukar bhide 4 types of trust
4 types of trust Rowena mittal
Rowena mittal Arcelormittal net
Arcelormittal net Bhumika mittal
Bhumika mittal Rajat mittal
Rajat mittal Leena mittal
Leena mittal Prateek mittal
Prateek mittal Ipo readiness roadmap
Ipo readiness roadmap Lga to pie
Lga to pie Torrance memorial outpatient lab
Torrance memorial outpatient lab Doctors license number
Doctors license number Gbmc infoweb
Gbmc infoweb Cartersville medical center medical records
Cartersville medical center medical records Difference between medical report and medical certificate
Difference between medical report and medical certificate Toronto medical
Toronto medical Michigan medical school
Michigan medical school Conclusion of medical surgical nursing
Conclusion of medical surgical nursing Basic medical ethics
Basic medical ethics Servier medical art
Servier medical art Megan lammers
Megan lammers Plural formation of medical terms
Plural formation of medical terms Medical terminology aden
Medical terminology aden Medical manuscript writing
Medical manuscript writing Sihd medical abbreviation
Sihd medical abbreviation Kenyatta lee md
Kenyatta lee md Medical law and ethics 5th edition
Medical law and ethics 5th edition Polio vaccine acronym
Polio vaccine acronym Mercer medical library
Mercer medical library Past medical history
Past medical history Common veterinary medical equipment vocabulary
Common veterinary medical equipment vocabulary Dorsal prefix root combining vowel and suffix
Dorsal prefix root combining vowel and suffix Twitter share abbr
Twitter share abbr Function
Function Adssc al ain mall
Adssc al ain mall Mcbis
Mcbis