Needlestick Regulations and Injury Prevention Chet Smith CSP
- Slides: 45
Needlestick Regulations and Injury Prevention Chet Smith, CSP Copyright © 2012 American Safety Management Inc.
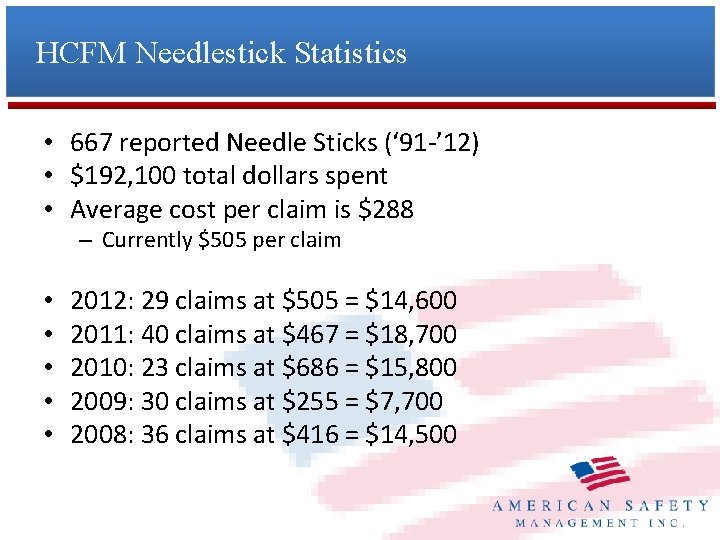
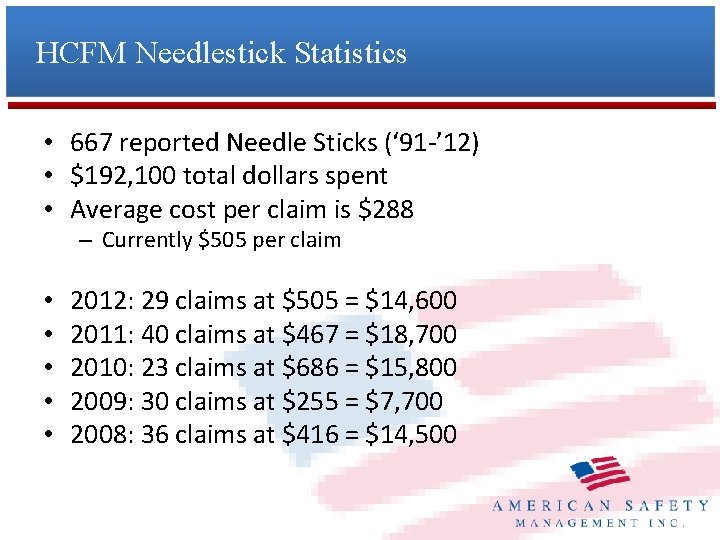
HCFM Needlestick Statistics • 667 reported Needle Sticks (‘ 91 -’ 12) • $192, 100 total dollars spent • Average cost per claim is $288 – Currently $505 per claim • • • 2012: 29 claims at $505 = $14, 600 2011: 40 claims at $467 = $18, 700 2010: 23 claims at $686 = $15, 800 2009: 30 claims at $255 = $7, 700 2008: 36 claims at $416 = $14, 500
Who is at risk? • How are these people exposed? – Nurses – CNA – Housekeeping – Maintenance – Dietary – Visitors
Bloodborne Pathogens
What is it? • A Bloodborne pathogen is a microorganism present in human blood or other infectious body fluid – i. e. Vaginal secretions, semen, amniotic fluid, etc. • Pathogens are spread through blood to blood or other bodily fluid contact • Some will die as soon as they are in open air, others can live up to a week outside of the body
Why Important? • 385, 000 Sharps Injuries Annually in Hospitalbased healthcare (CDC) – Many more in nursing homes! • Each year, approximately 75, 000 people infected with HBV (Hepatitis B) • 27% of people with HIV don’t know they have it • OSHA says approximately 8, 700 workers infected with HBV each year • Contracting a Bloodborne changes lives!
Areas of Most Concern • • HBV – Hepatitis B HCV – Hepatitis C HIV – Human Immunodeficiency Virus Also of concern – Malaria – Syphilis – Relapsing Fever
HBV – Hepatitis B Hepatitis means inflammation of the liver HBV attacks liver and can lead to cirrhosis and death Most common serious liver infection in world Only 10% of adults develop chronic infections, but 90% of children will • Virus can live up to a week outside of body • Symptoms: • • – Fever, fatigue, muscle pain – Loss of appetite, nausea, vomiting (severe flu symptoms) – However, you may feel no symptoms at all but can still infect others
HCV – Hepatitis C • Also works by attacking and destroying the liver • Most common chronic Bloodborne infection in US (3. 9 million infected) • 80% of people will have no symptoms at first • 70% of people develop chronic liver disease • Symptoms: – Jaundice, fatigue, dark urine – Abdominal pain, loss of appetite, nausea
HIV – Human Immunodeficiency Virus • Works by weakening the immune system over time • Makes you more susceptible to normal infections • HIV is not AIDS, it can slowly develop into AIDS over times • Time between HIV infection and AIDS symptoms can be 811 years • Virus dies quickly outside of body unless kept in lab conditions
Myths of Transmission • Can not contract a Bloodborne pathogen from: – Water fountain – Bathroom – Sharing food • Does not spread through air from: – Sneezing – Coughing • Can’t get from mosquitoes
Methods of Transmission • Bloodborne Pathogens can only spread when infected blood or body fluid enters body through cut or mucous membranes • Most common method is through sharing needles • Unprotected sexual activity 2 nd leading method • Occupational contraction is 2 nd lowest method • Indirect transmission – touching contaminated object or surface and then touching eyes, nose, mouth
How to Reduce Your Risk • Assume ALL blood or body fluids are contaminated • Always dispose of any kind of sharp into sharps container • Do not handle broken glass with bare hands, use a broom if at all possible
How to Reduce Your Risk • Thoroughly wash hands with non abrasive soap and water after contact with any potentially contaminated material • Also wash anytime you take off latex gloves • Bandage any cuts or sores • Never eat, smoke, or drink in areas where contamination could occur
Hepatitis B Vaccine • We shall make available the hepatitis B vaccine to all employees who have occupational exposure, and post-exposure evaluation and follow-up to all employees who have had an exposure incident. – Within 10 days of initial assignment (unless already vaccinated) – If declined, Appendix A – Titer Testing • Employees may decline the vaccine. • Other employees may voluntarily pay for the vaccine.
Post Exposure • Following the report of an exposure – Confidential medical evaluation & follow-up – Document route(s) of expsure – Document the source – Source blood tested after consent & results made available to the exposed employee – Exposed employee’s blood tested after consent – Counseling offered to exposed employee
Personal Protective Equipment - PPE • Wear latex or nitrile when dealing with any kind of blood or bodily fluid • May also be necessary to wear safety glasses or goggles, mask, and apron
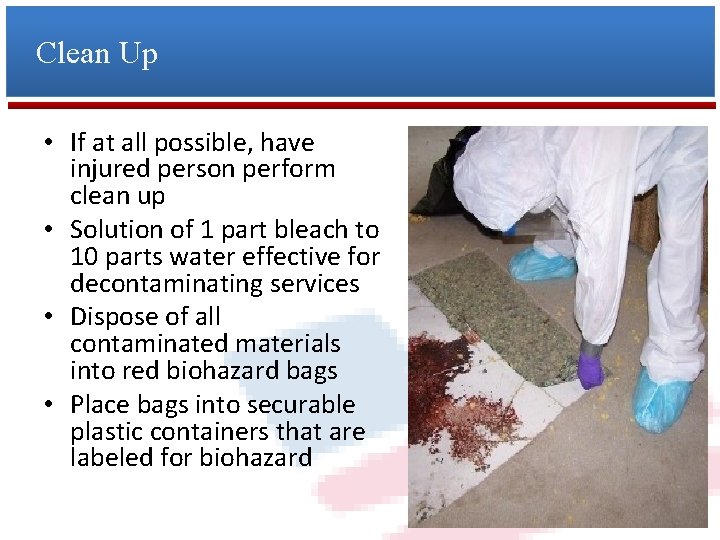
Clean Up • If at all possible, have injured person perform clean up • Solution of 1 part bleach to 10 parts water effective for decontaminating services • Dispose of all contaminated materials into red biohazard bags • Place bags into securable plastic containers that are labeled for biohazard
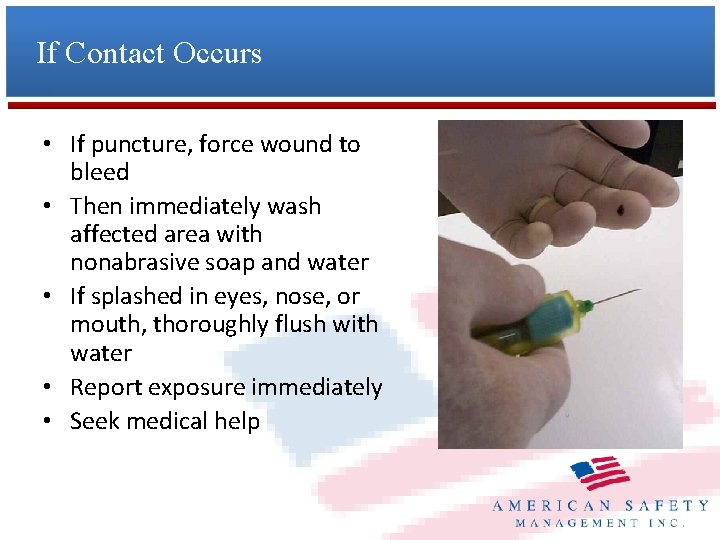
If Contact Occurs • If puncture, force wound to bleed • Then immediately wash affected area with nonabrasive soap and water • If splashed in eyes, nose, or mouth, thoroughly flush with water • Report exposure immediately • Seek medical help
Exposure Control Plan • Exposure Control Plan: – 1910. 1030(c)(1)(i) Each employer having an employee(s) with occupational exposure shall establish a written Exposure Control Plan designed to eliminate or minimize employee exposure”. – (b) Occupational Exposure: Means reasonably anticipated skin, eye, mucous membrane, or parenteral contact with blood or other potentially infectious materials that may result from the performance of an employee’s duties.
Exposure Control Plan • Exposure Control Plan – Must be accessible to employees – Reviewed and updated annually – Updated to reflect new or modified tasks – Updated to reflect new or revised employee positions
Exposure Determination • Exposure Determination – A list of all job classifications in which all employees in those jobs classifications have occupational exposure – A list of job classifications in which some employees have occupational exposure – A list of all tasks & procedures or groups of closely related tasks and procedures in which occupational exposure occurs and that are performed by employees in job classifications listed in “which some employees have occupational exposure. – Note: determination shall be made without regard to PPE.
Methods of Compliance Universal Precautions Engineering & Work Practice Controls Handwashing Needle Handling Sharps Containers Eating, Drinking, Smoking, Applying Cosmetics or Lip Balm, and Handling Contact Lenses is prohibited. • PPE • Decontamination Procedures • Waste Disposal • • •
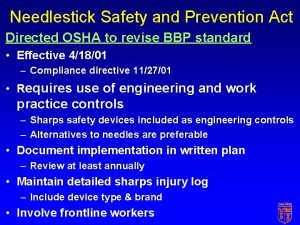
New Additions to the Exposure Control Plan • In addition to what is already required by the 1991 standard, the revised standard requires the documentation of… • (1) annual consideration and implementation of appropriate engineering controls, and • (2) solicitation of non-managerial healthcare workers in evaluating and choosing devices. The plan must be reviewed and updated at least annually. • ***Refer to Attachment***
National Emphasis Program Exp: 4 -5 -15 • Evaluate the employer’s written Exposure Control Plan (ECP) to determine if it contains all the elements required by the standard. • Assess the implementation of appropriate engineering and work practice controls. – Determine which procedures require the use of a sharp medical device (e. g. , use of a syringe for the administration of insulin) and determine whether the employer has evaluated, selected, and is using sharps with engineered sharps injury protection (SESIPs) or needleless systems.
NEP – Confirm that all tasks involving sharps have been evaluated for the implementation of safer devices. For example, determine whether the employer has implemented a policy requiring use of safety engineered needles for prefilled syringes and single-use blood tube holders. – Determine whether the employer solicited feedback from nonmanagerial employees responsible for direct resident care who are potentially exposed to injuries from contaminated sharps in the identification, evaluation, and selection of effective engineering and work practice controls and whether the employer documented solicitation in the ECP.
NEP • Ensure that proper work practices and personal protective equipment are in place. • Assess whether containment of regulated waste is performed properly. • Evaluate and document the availability of handwashing facilities. If immediate access to handwashing facilities is not feasible, ascertain whether skin cleansers are used (e. g. , alcohol gels).
NEP • Assess the use of appropriate personal protective equipment (e. g. , masks, eye protection, face shields, gowns and disposable gloves, including latex free gloves, where appropriate). • Ensure that a program is in place for immediate and proper clean-up of spills, and disposal of contaminated materials, specifically for spills of blood or other body fluids.
NEP • Ensure that the employer has chosen an appropriate EPA-approved disinfectant to clean contaminated work surfaces and that the product is being used in accordance with the manufacturer’s recommendations. • Determine that the employer has made available to all employees with occupational exposure to blood or OPIM the hepatitis B virus (HBV) vaccination series within 10 working days of initial assignment at no cost to the employee and that any declinations are documented.
NEP • Ensure that healthcare workers who have contact with residents or blood and are at ongoing risk for percutaneous injuries are offered a test for 20 antibody to the HBV surface antigen in accordance with the U. S. Public Health Service guidelines. (See CPL 02 -02 -069, Section XIII. F. ) • Investigate procedures implemented for postexposure evaluation and follow-up following an exposure incident:
NEP – Determine if establishment-specific post-exposure protocols are in place (i. e. , where and when to report immediately after an exposure incident). – Determine if medical attention is immediately available, including administration of a rapid HIV test, in accordance with current U. S. Public Health Service guidelines.
NEP • Observe whether appropriate warning labels and signs are present. • Determine whether employees receive training in accordance with the standard. • Evaluate the employer’s sharps injury log. Ensure that all injuries that appear on the sharps injury log are also recorded on the OSHA-300 log. • Determine whether the log includes the required fields.
NEP • Ensure that employees’ names are not on the log, but that a case or report number indicates an exposure incident. • Determine whether the employer uses the information on the sharps injury log when reviewing and updating its ECP. Failure to use this information is not a violation, but the CSHO should recommend that the information be used for these purposes.
Needlestick Safety & Prevention Act • Signed into law November 2000 and became effective April 2001. • Plan by the American Nurses Association (ANA) and other health care advocates to achieve an amendment to the BBP standard. http: //www. nursingworld. org
Needlestick Safety & Prevention Act • Numerous studies have demonstrated that the use of safer medical devices, such as needleless systems and sharps with engineered sharps injury protections, when they are part of an overall bloodborne pathogens risk-reduction program, can be extremely effective in reducing accidental sharps injuries.
Hierarchy of Controls • • • Elimination of Hazard Engineering Controls Administrative Controls Work Practice Controls Personal Protective Equipment (PPE)
Major Provisions • • • Engineering Controls – Safer Devices Involvement of frontline employees Annual Review and Update Administrative, Work Practice and PPE controls Enhanced Recordkeeping
Indications that a Device is Advantageous • Device is needleless • If device uses needles, it performs reliably with all needle sizes • Safety device in built-in • Safety device works passively (you don’t have to activate it) • It is evident that the safety device is activated • Safety feature can’t be deactivated • Device is easy to use and practical • Device is safe & effective in resident care
Flex Pens • Flex pens are not safety devices – What if a medicine only comes in a flex pen?
Sharps Injury Log • Required, Separate from OSHA 300 log. • Record: – Date/Time – Type, Brand, Model of Device – Department or Work Area – Describe How the Incident Occurred
Sharps Log Should be Used to… • Analyze injury frequencies by specific attributes like work units, devices, and procedures. • Identify high-risk devices and procedures. • Identify injuries that could be prevented. • Evaluate the efficacy of newly implemented devices. • Share and compare information and successes with other institutions.
Annual Assessment of Safer Sharps • • • Review Sharps Injury log Inform Staff of evaluation and selection process Create assessment team Review Resources Select improved work practices & new devices Train assessment team Gather feedback Make final decision & document Train all staff Ask for feedback at 30 days ***Refer to attachment***
Sharps Containers • Locate strategically throughout the facility – Rooms – Shower Rooms – Med Rooms – Treatment Rooms – Do not sit on floor – Do not set on sinks – Do not set on desks – Never overfilled (3/4 full or at the “full” line) – Never emptied
Common Sense • Needles should never be – Bent – Broken – Re-capped – Left on beds – Placed on tables – Put in pockets – Disposed immediately at site of use
Common Sense Being Respectful of sharps Keeping fingers out of sharps containers Not Carrying needles down the hall Not Sheathing a safety needle Not Re-capping both safety and non-safety type needles • Tubing in Sharps containers • Sharps containers lids • Not Re-capping shaving razors • • •
 Needlestick safety and prevention act
Needlestick safety and prevention act Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Example of intentional injury
Example of intentional injury Injuries first aid
Injuries first aid Workplace fatality prevention
Workplace fatality prevention Serious injury and fatality prevention
Serious injury and fatality prevention Needle stick injury prevention images
Needle stick injury prevention images Back injury prevention quiz answers
Back injury prevention quiz answers Hand injury prevention
Hand injury prevention Sharps injury prevention program
Sharps injury prevention program Atlas injury prevention
Atlas injury prevention Diagnosis
Diagnosis Turli mamlakatlarda talim tizimi
Turli mamlakatlarda talim tizimi Thần chết mang tên 7 sắc cầu vòng
Thần chết mang tên 7 sắc cầu vòng đám ma bác giun
đám ma bác giun Chet haegel
Chet haegel Chet haegel
Chet haegel Genre of a separate peace
Genre of a separate peace đêm đêm tôi vừa chợp mắt
đêm đêm tôi vừa chợp mắt Sonoma interconnect
Sonoma interconnect Ilg'or pedagogik texnologiyalar
Ilg'or pedagogik texnologiyalar Chaf sofit
Chaf sofit Disadvantages of act of parliament
Disadvantages of act of parliament Ap csp sequencing
Ap csp sequencing Csp mentoring
Csp mentoring Csp problem in ai
Csp problem in ai Csp checker
Csp checker Viairas
Viairas Azure csp migration
Azure csp migration Csp legacy migration
Csp legacy migration Csp yammer
Csp yammer Surface hub setup
Surface hub setup Csp office 365 business
Csp office 365 business Pip install python-constraint
Pip install python-constraint Backtracking search algorithm for csp
Backtracking search algorithm for csp Constraint graph
Constraint graph Constrained crossword
Constrained crossword Constraint graph
Constraint graph Csp problem in ai
Csp problem in ai Microsoft csp program
Microsoft csp program Csp outline
Csp outline Azure erdrich
Azure erdrich Csp planning
Csp planning Sms vs csp
Sms vs csp Csp cpd portfolio
Csp cpd portfolio 1000000 soudokou
1000000 soudokou