National Emergency Laparotomy Audit Improving Patient Care www



- Slides: 39
National Emergency Laparotomy Audit Improving Patient Care www. nela. org. uk info@nela. org. uk
• Summary of year 3 results • Trends in national picture • How NELA might change in next few years
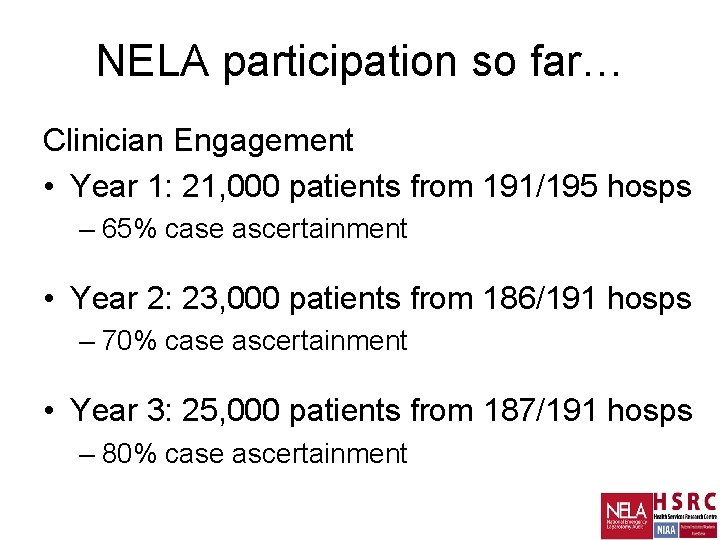
NELA participation so far… Clinician Engagement • Year 1: 21, 000 patients from 191/195 hosps – 65% case ascertainment • Year 2: 23, 000 patients from 186/191 hosps – 70% case ascertainment • Year 3: 25, 000 patients from 187/191 hosps – 80% case ascertainment
Year 3: 25, 000 patients (83%) from 187 hospitals • Personal practice still improving • Organisational change still challenging • Still considerable variation 4
i)Processes
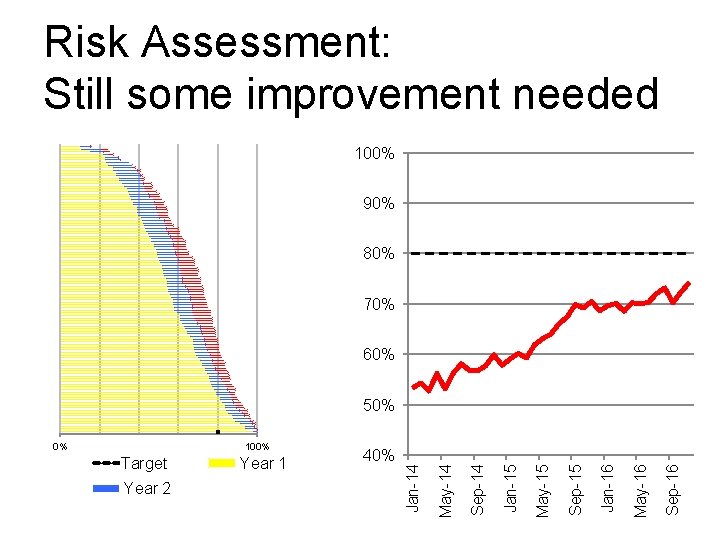
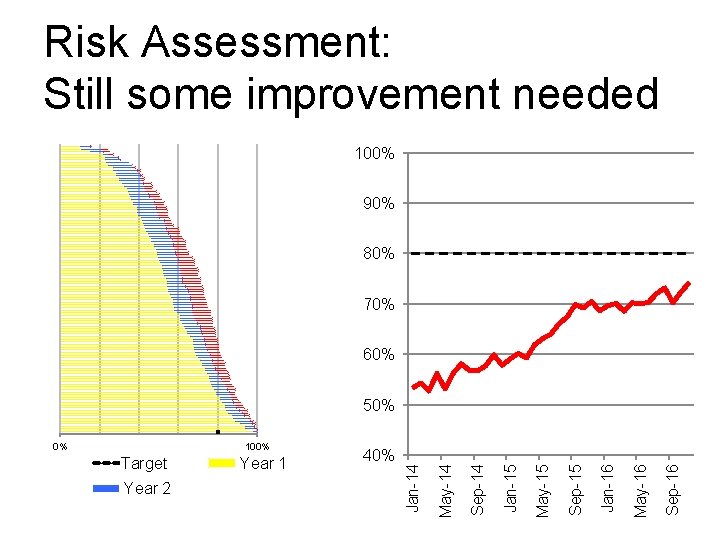
Risk Assessment: Still some improvement needed 100% 90% 80% 70% 60% 50% Sep-16 May-16 Jan-16 Sep-15 May-15 40% Jan-15 Year 2 Year 1 Sep-14 Target May-14 100% Jan-14 0%
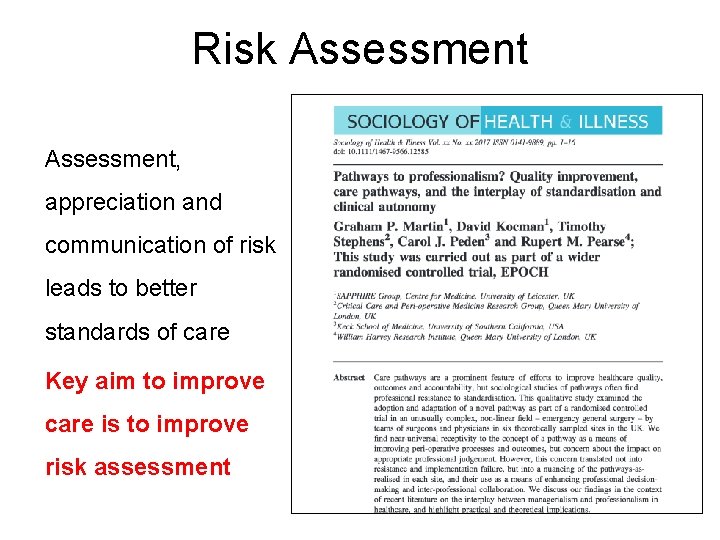
Risk Assessment, appreciation and communication of risk leads to better standards of care Key aim to improve care is to improve risk assessment
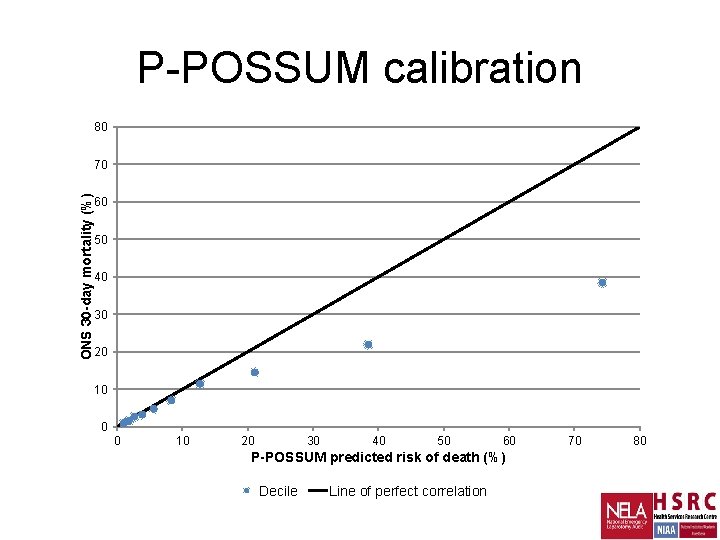
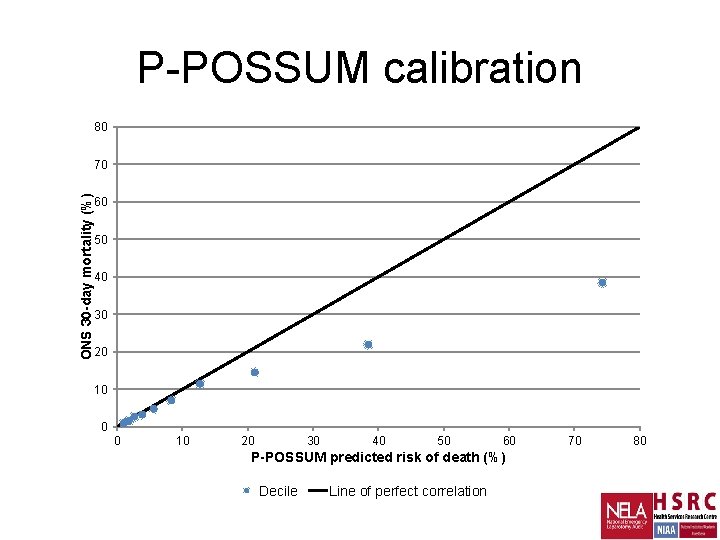
P-POSSUM calibration 80 ONS 30 -day mortality (%) 70 60 50 40 30 20 10 0 0 10 20 30 40 50 60 P-POSSUM predicted risk of death (%) Decile Line of perfect correlation 70 80
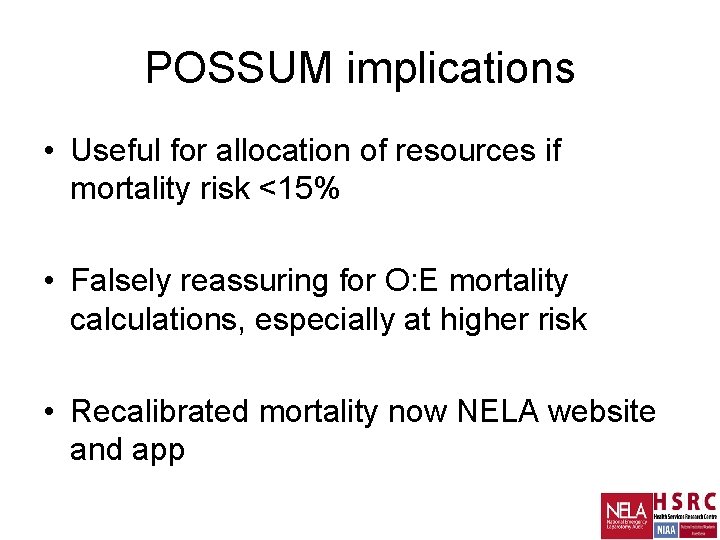
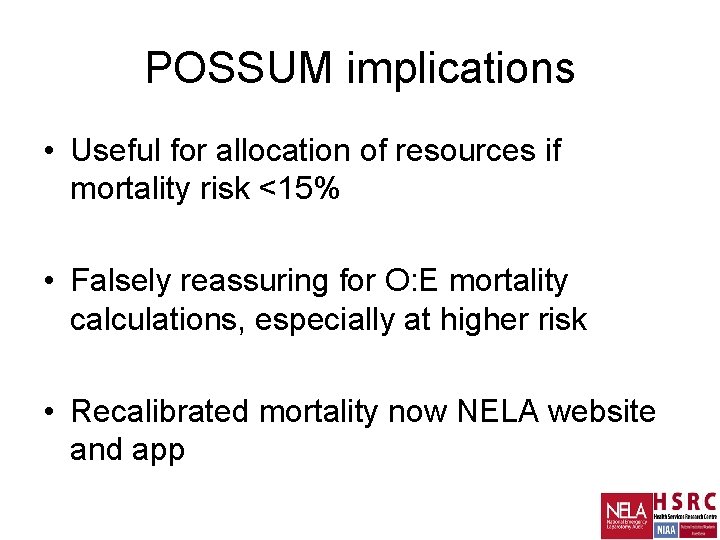
POSSUM implications • Useful for allocation of resources if mortality risk <15% • Falsely reassuring for O: E mortality calculations, especially at higher risk • Recalibrated mortality now NELA website and app
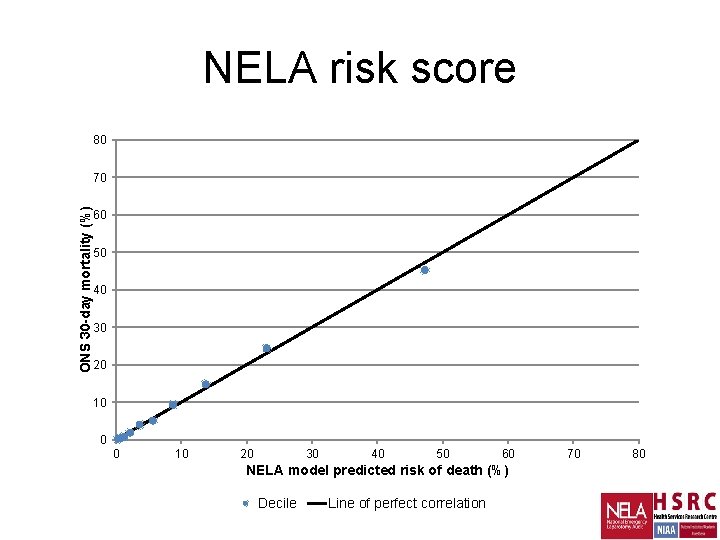
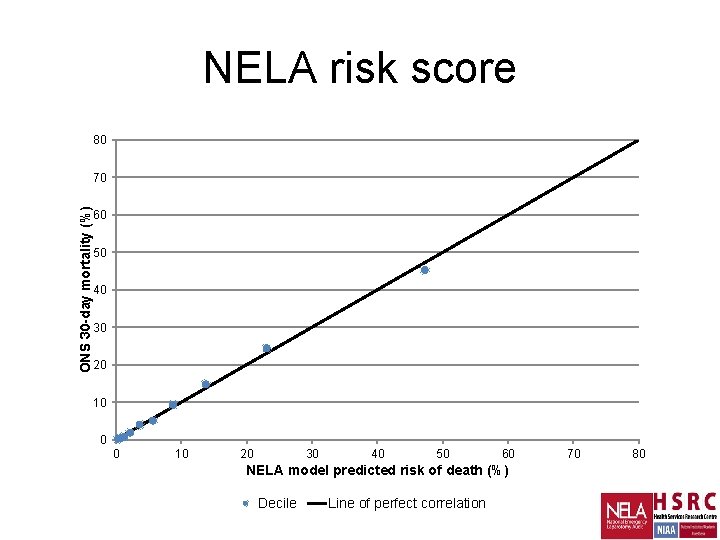
NELA risk score 80 ONS 30 -day mortality (%) 70 60 50 40 30 20 10 0 0 10 20 30 40 50 60 NELA model predicted risk of death (%) Decile Line of perfect correlation 70 80
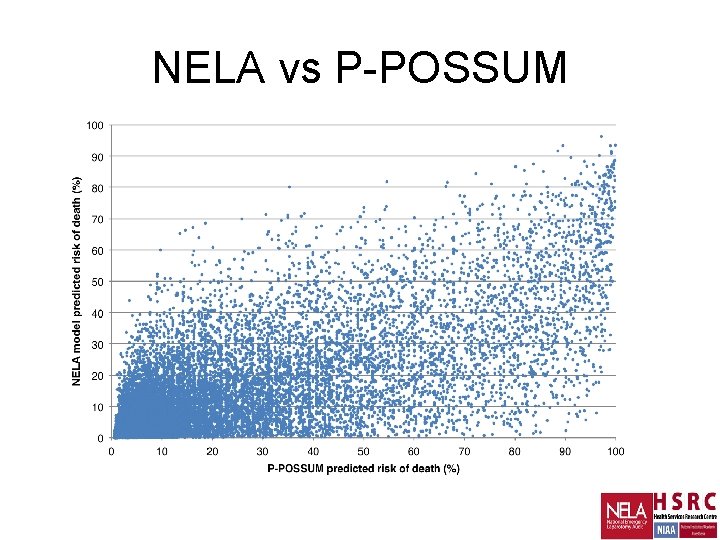
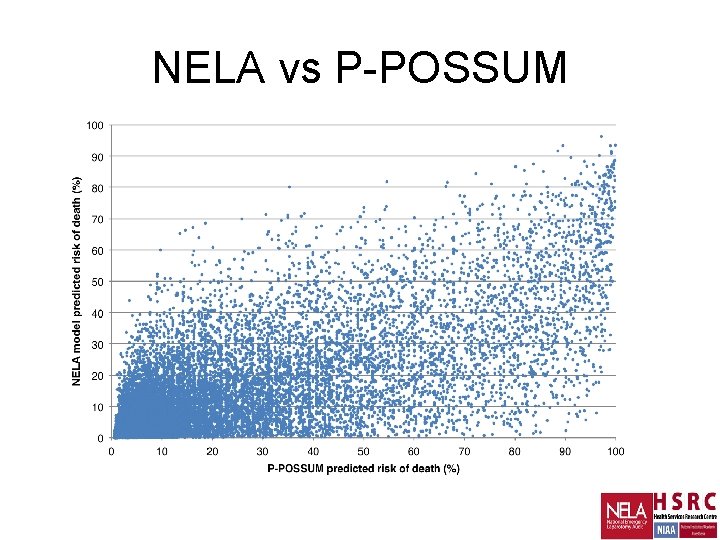
NELA vs P-POSSUM
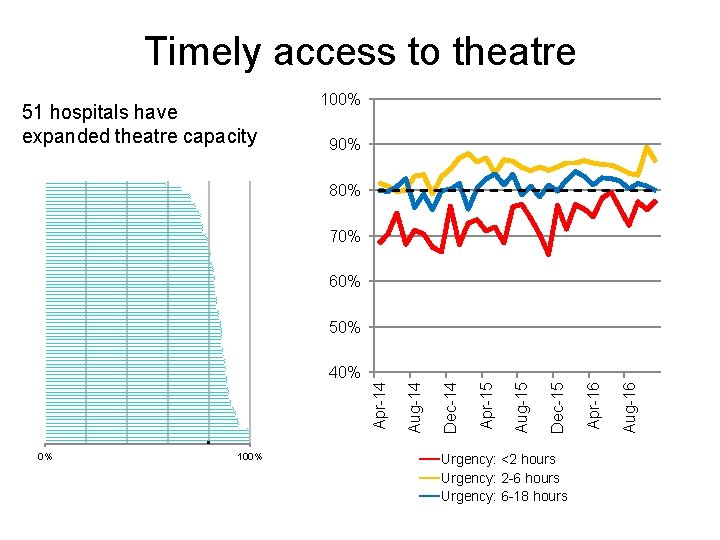
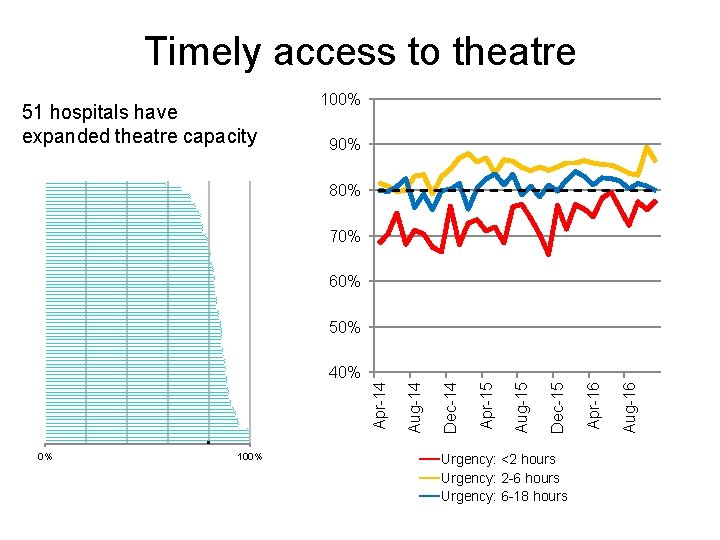
Timely access to theatre 51 hospitals have expanded theatre capacity 100% 90% 80% 70% 60% 50% 0% 100% Urgency: <2 hours Urgency: 2 -6 hours Urgency: 6 -18 hours Aug-16 Apr-16 Dec-15 Aug-15 Apr-15 Dec-14 Aug-14 Apr-14 40%
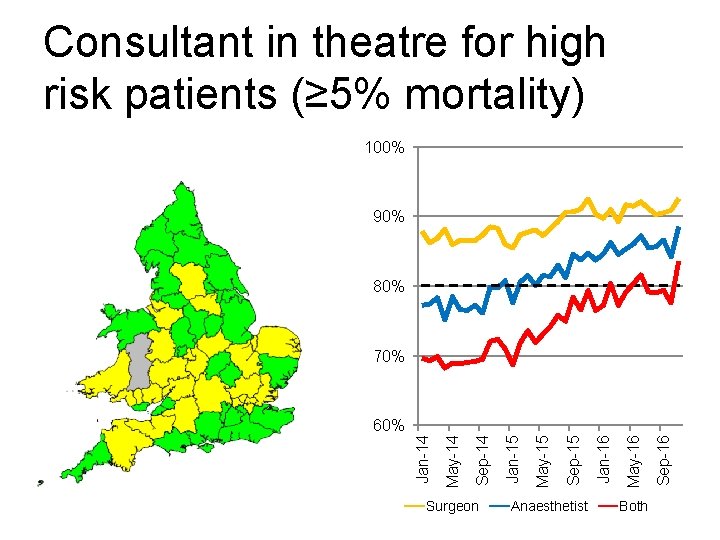
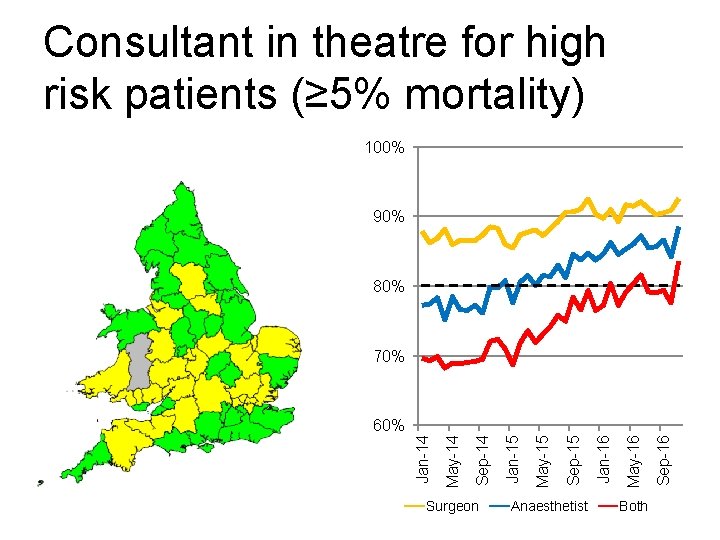
Consultant in theatre for high risk patients (≥ 5% mortality) 100% 90% 80% 70% Surgeon Anaesthetist Both Sep-16 May-16 Jan-16 Sep-15 May-15 Jan-15 Sep-14 May-14 Jan-14 60%
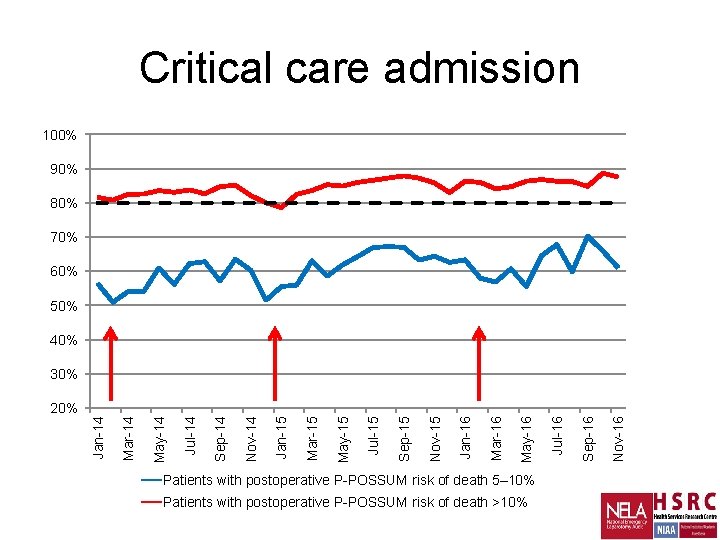
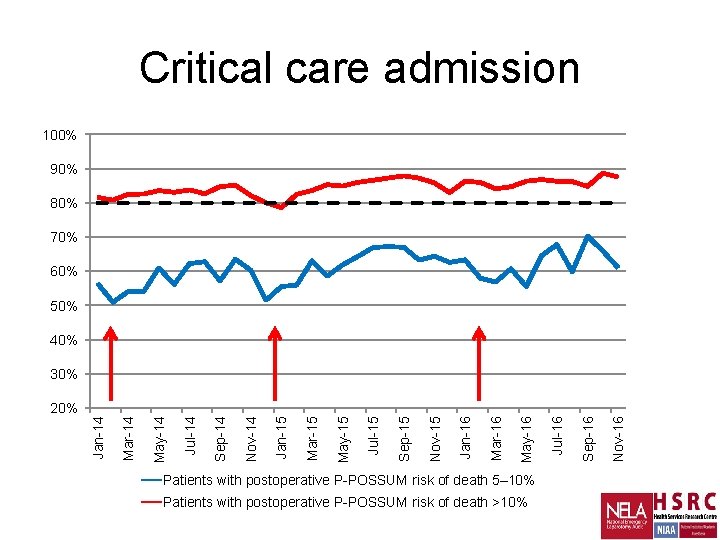
Critical care admission 100% 90% 80% 70% 60% 50% 40% 30% Patients with postoperative P-POSSUM risk of death 5– 10% Patients with postoperative P-POSSUM risk of death >10% Nov-16 Sep-16 Jul-16 May-16 Mar-16 Jan-16 Nov-15 Sep-15 Jul-15 May-15 Mar-15 Jan-15 Nov-14 Sep-14 Jul-14 May-14 Mar-14 Jan-14 20%
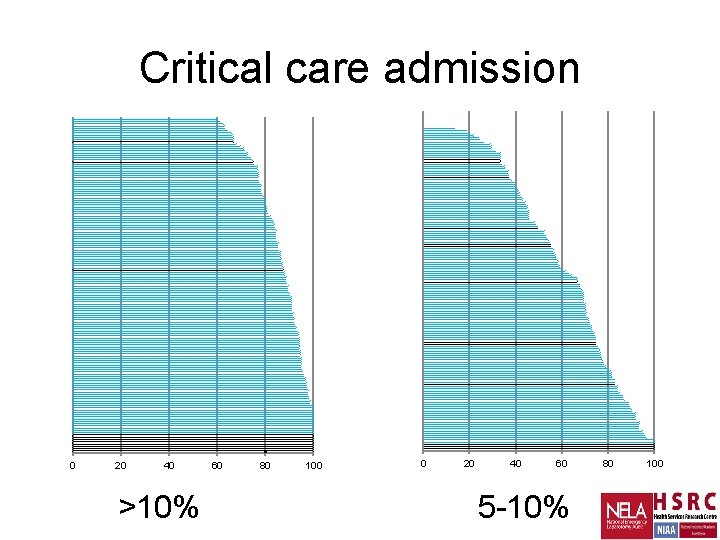
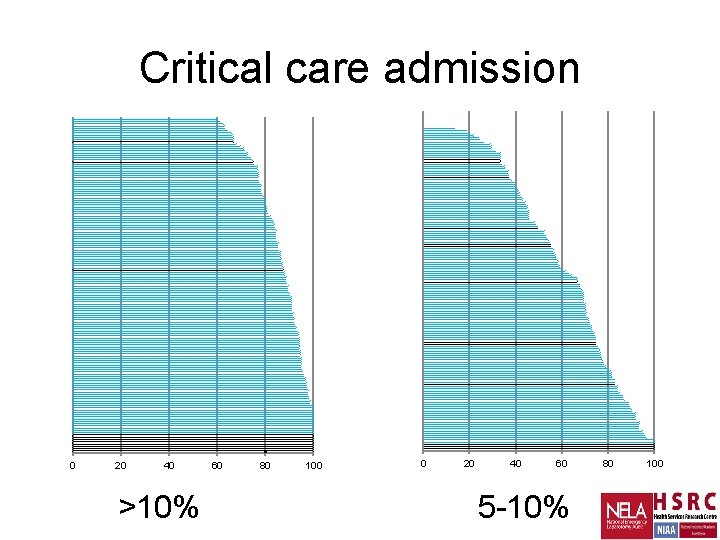
Critical care admission 0 20 40 >10% 60 80 100 0 20 40 60 5 -10% 80 100
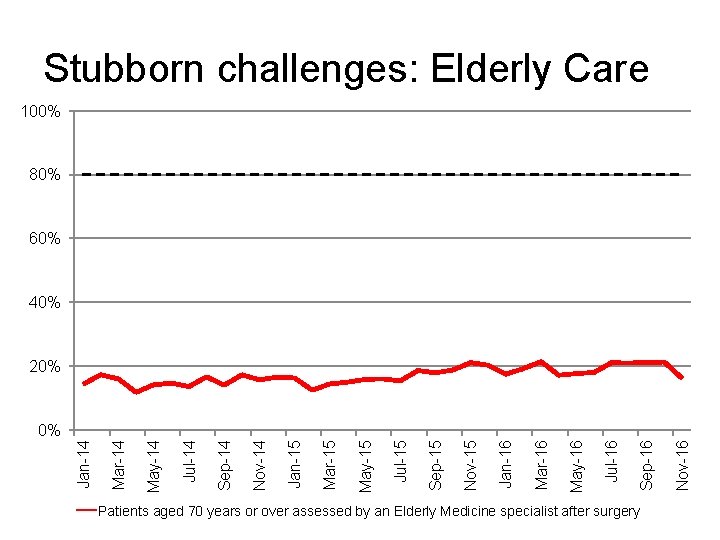
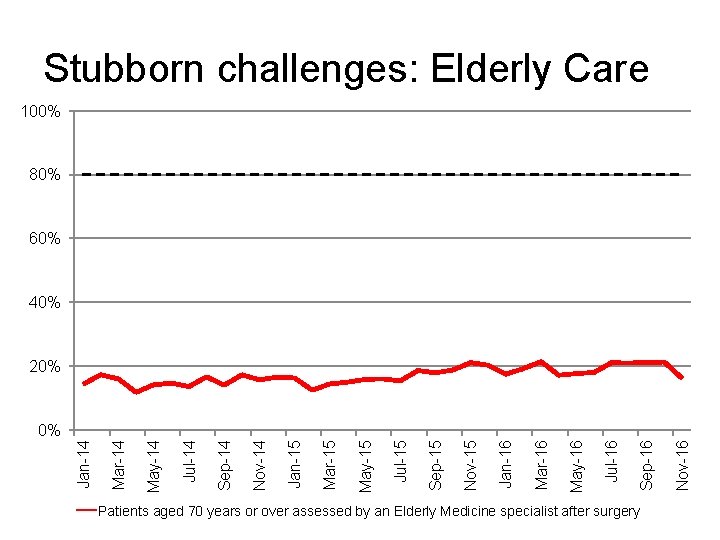
Stubborn challenges: Elderly Care 100% 80% 60% 40% 20% Patients aged 70 years or over assessed by an Elderly Medicine specialist after surgery Nov-16 Sep-16 Jul-16 May-16 Mar-16 Jan-16 Nov-15 Sep-15 Jul-15 May-15 Mar-15 Jan-15 Nov-14 Sep-14 Jul-14 May-14 Mar-14 Jan-14 0%
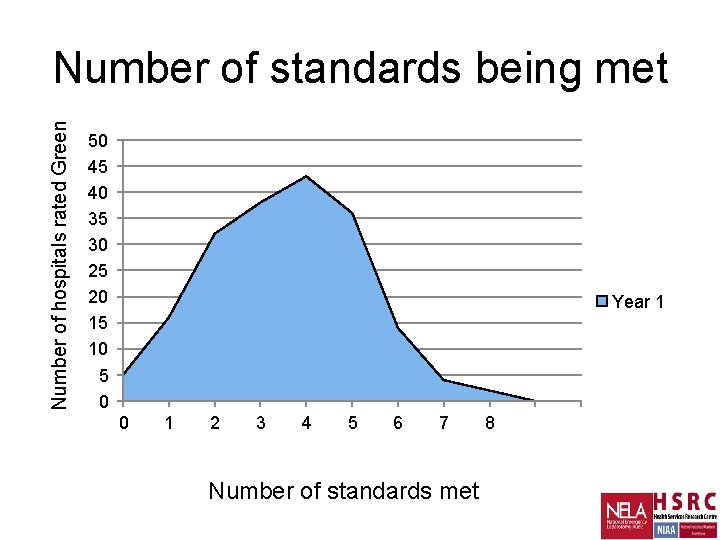
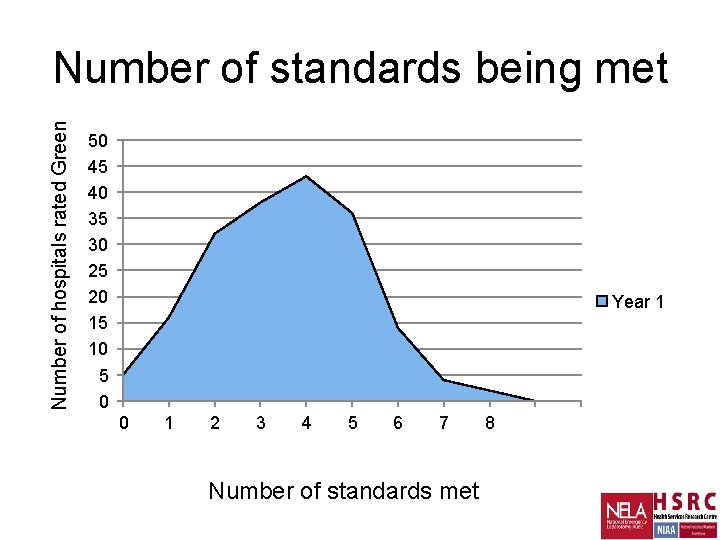
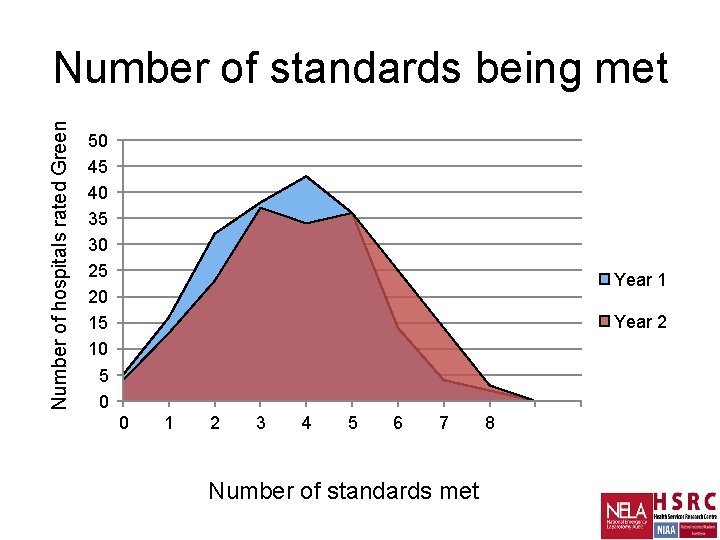
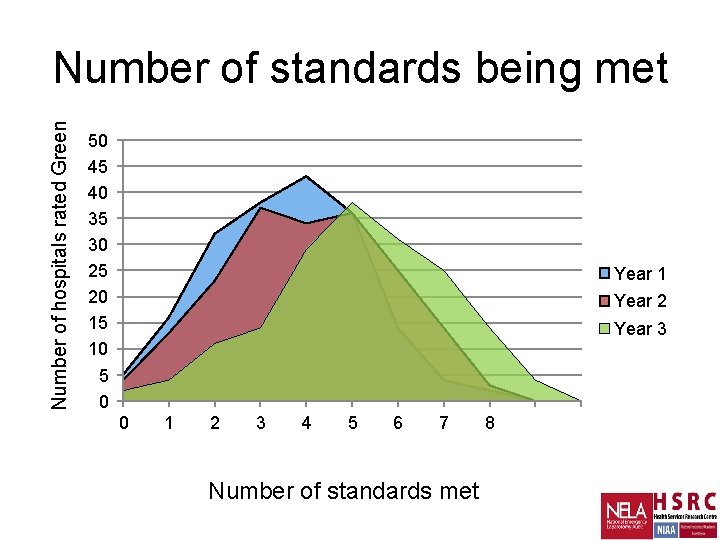
Number of hospitals rated Green Number of standards being met 50 45 40 35 30 25 20 15 10 5 0 Year 1 0 1 2 3 4 5 6 7 Number of standards met 8
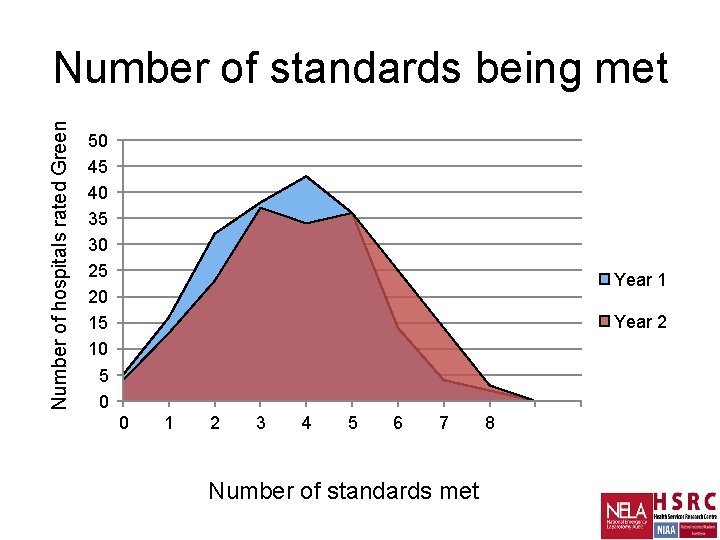
Number of hospitals rated Green Number of standards being met 50 45 40 35 30 25 20 15 10 5 0 Year 1 Year 2 0 1 2 3 4 5 6 7 Number of standards met 8
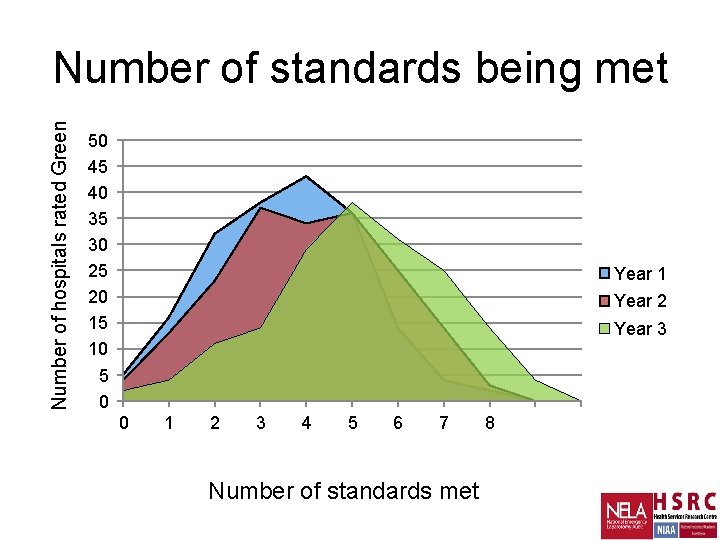
Number of hospitals rated Green Number of standards being met 50 45 40 35 30 25 20 15 10 5 0 Year 1 Year 2 Year 3 0 1 2 3 4 5 6 7 Number of standards met 8
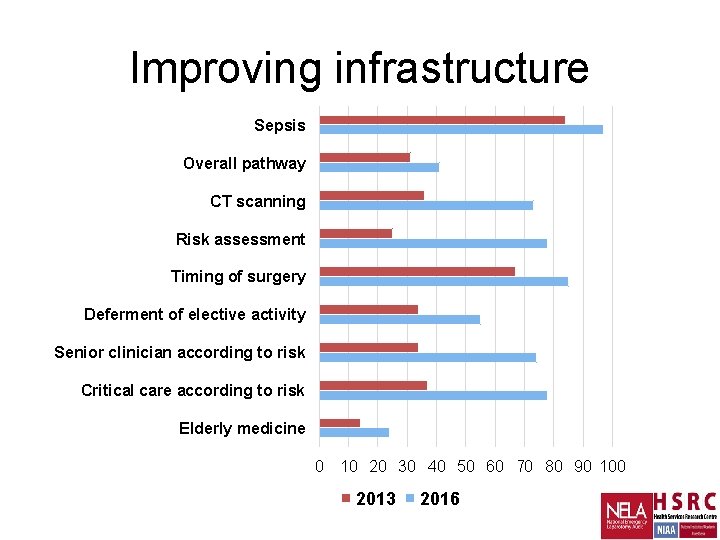
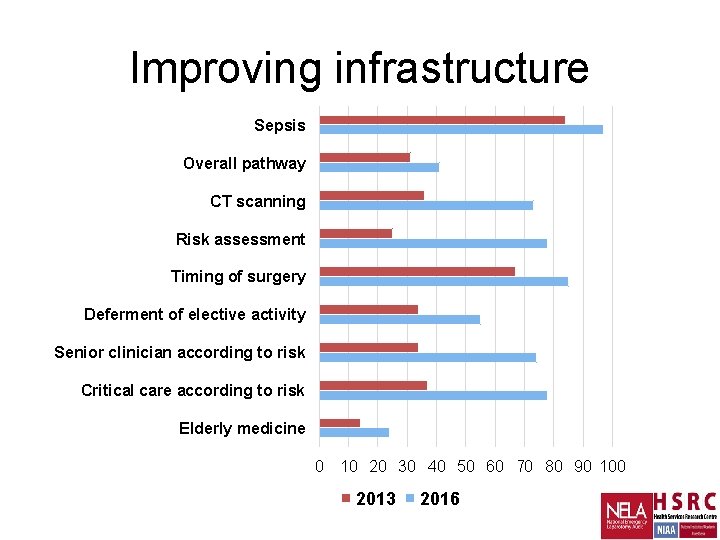
Improving infrastructure Sepsis Overall pathway CT scanning Risk assessment Timing of surgery Deferment of elective activity Senior clinician according to risk Critical care according to risk Elderly medicine 0 10 20 30 40 50 60 70 80 90 100 2013 2016

Outcomes
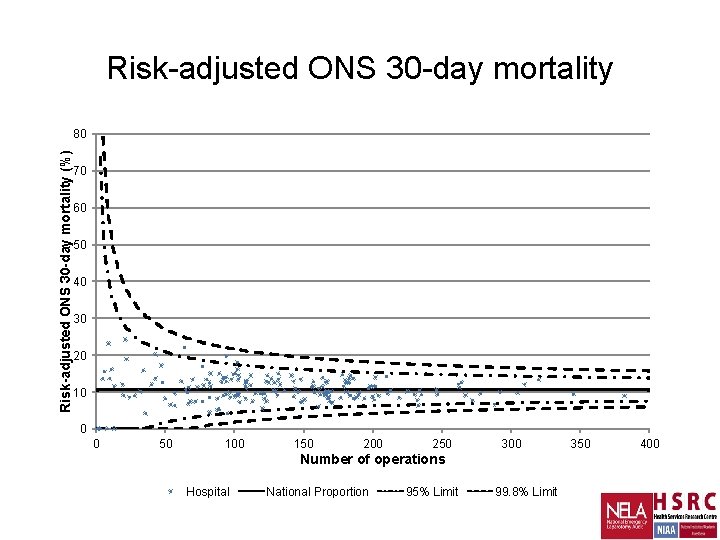
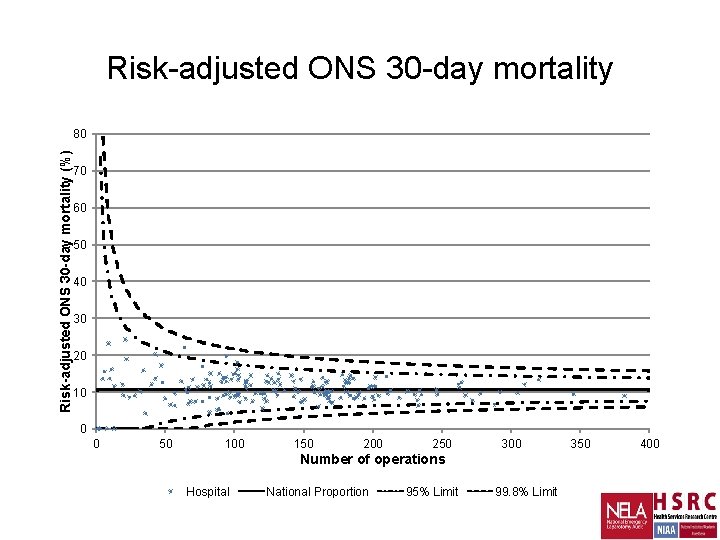
Risk-adjusted ONS 30 -day mortality (%) 80 70 60 50 40 30 20 10 0 0 50 100 150 200 250 300 Number of operations Hospital National Proportion 95% Limit 99. 8% Limit 350 400
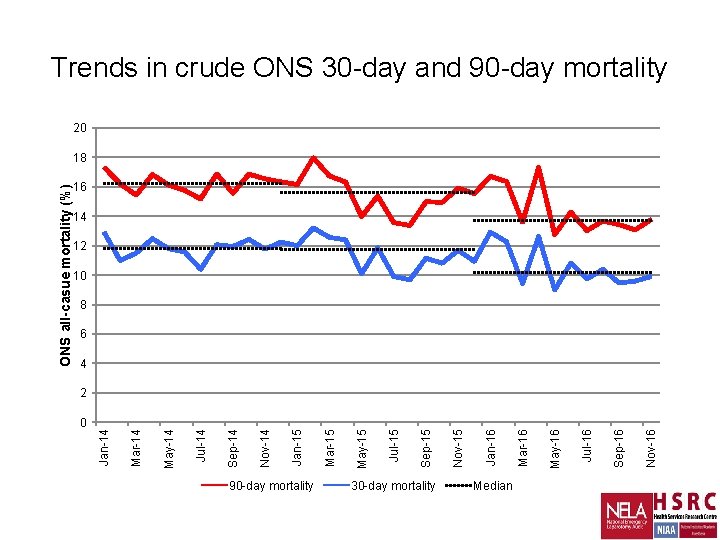
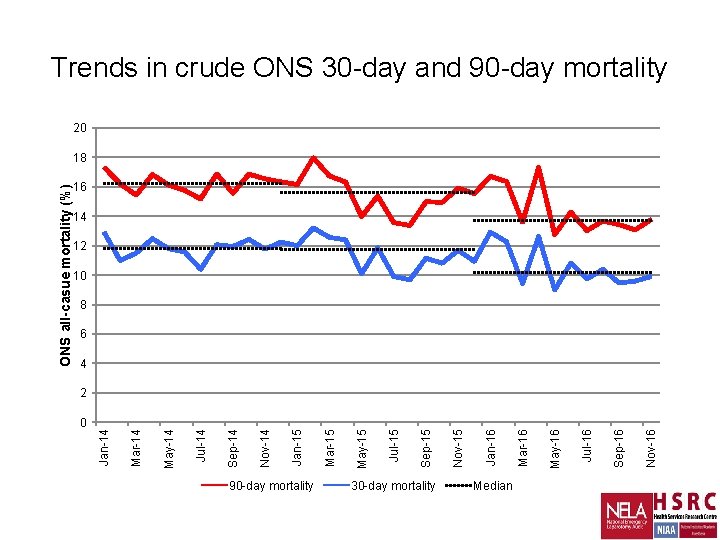
0 90 -day mortality 30 -day mortality Median Nov-16 Sep-16 Jul-16 May-16 Mar-16 Jan-16 Nov-15 Sep-15 Jul-15 May-15 Mar-15 Jan-15 Nov-14 Sep-14 Jul-14 May-14 Mar-14 Jan-14 ONS all-casue mortality (%) Trends in crude ONS 30 -day and 90 -day mortality 20 18 16 14 12 10 8 6 4 2
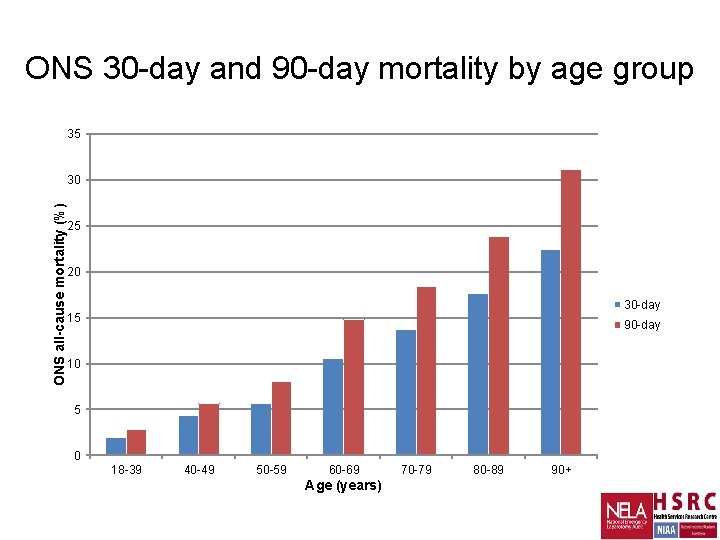
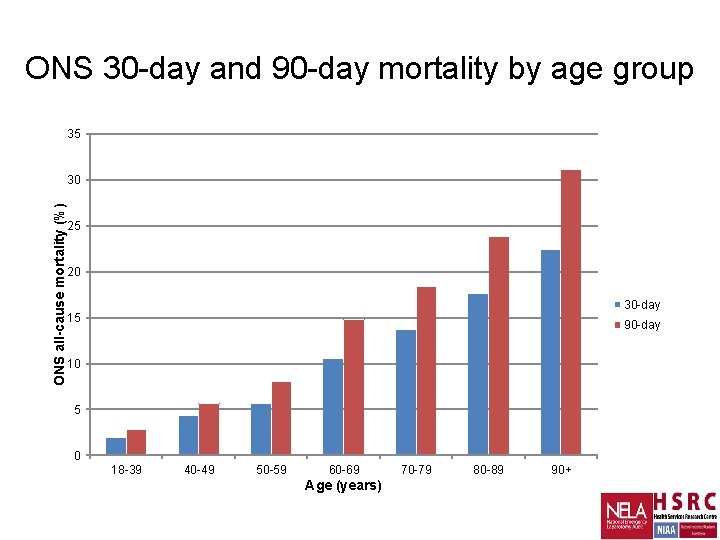
ONS 30 -day and 90 -day mortality by age group 35 ONS all-cause mortality (%) 30 25 20 30 -day 15 90 -day 10 5 0 18 -39 40 -49 50 -59 60 -69 Age (years) 70 -79 80 -89 90+
30 -day mortality Year 1 Year 2 Year 3 11. 8% 11. 5% 10. 6%
30 -day mortality Year 1 Year 2 Year 3 11. 8% 11. 5% 10. 6%
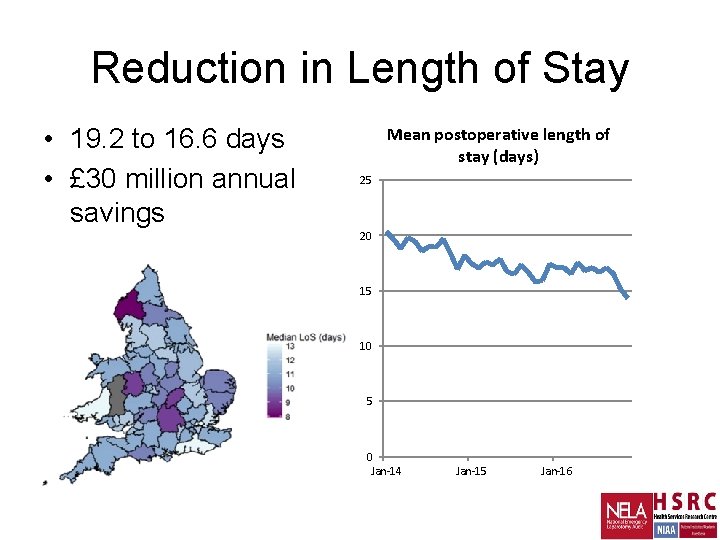
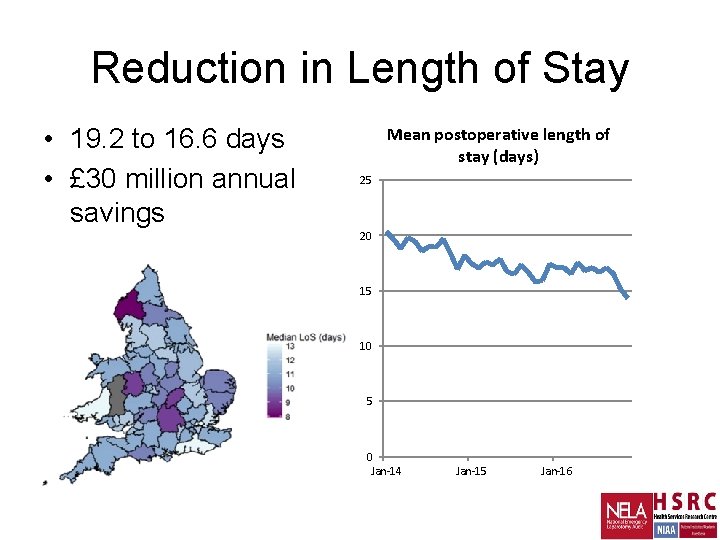
Reduction in Length of Stay • 19. 2 to 16. 6 days • £ 30 million annual savings Mean postoperative length of stay (days) 25 20 15 10 5 0 Jan-14 Jan-15 Jan-16

Going forwards… • Greater emphasis on QI • More frequent public reporting • RAG rating boundaries will increase • Mandatory and discretionary measures • Best Practice Tariff
What next for NELA/NELQIP? • Greater emphasis on QI • Targeted /themed reporting, eg commissioners • Secondary research • Parsimonious risk model
The Problem With Audit Data
The Problem With Audit Data Local QI
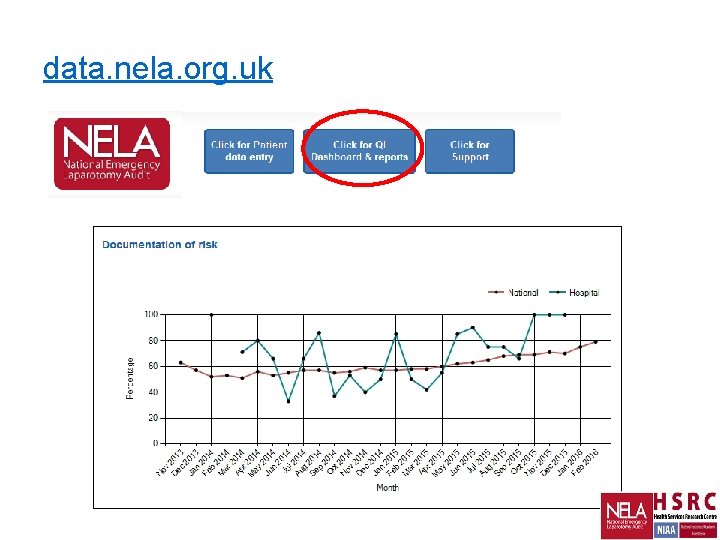
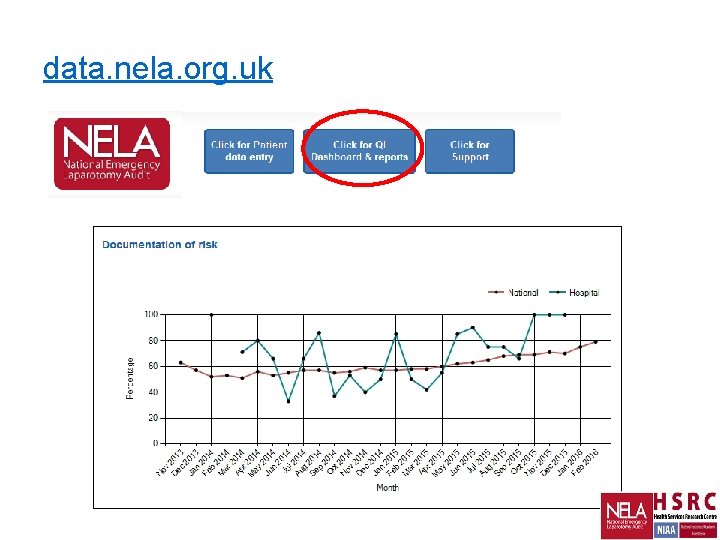
data. nela. org. uk
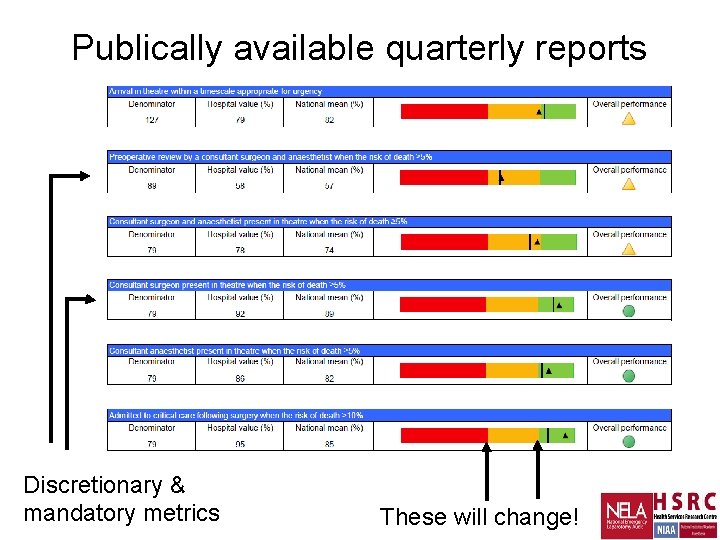
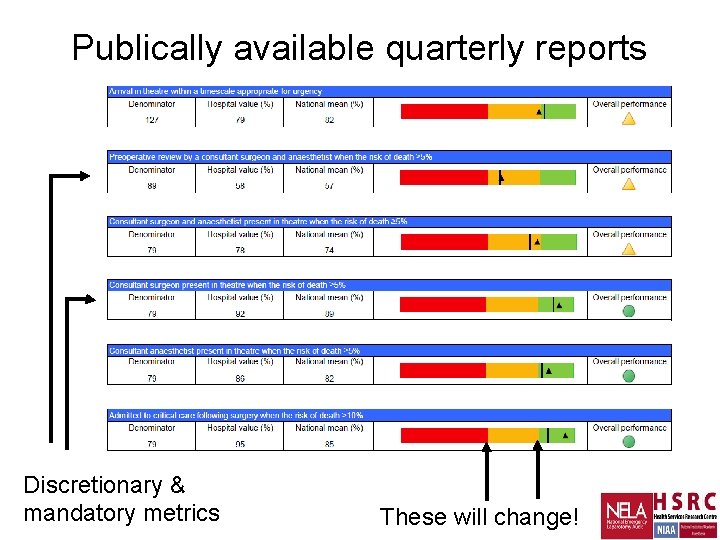
Publically available quarterly reports Discretionary & mandatory metrics These will change!

Best Practice Tariff • • Consultant presence? Theatre on time? Critical care? Elderly care?
Research… www. epochtrial. org www. floela. org
Ongoing projects • NELA Surgical sub-speciality analysis Perforated peptic ulcer (AUGIS) Subtotal colectomy for colitis (ACPGBI) Bowel Obstruction (ASGBI) Hartmann’s (ACPGBI) Bowel Cancer (ACPGBI) • NELA Risk Tool Replace / augment P-POSSUM
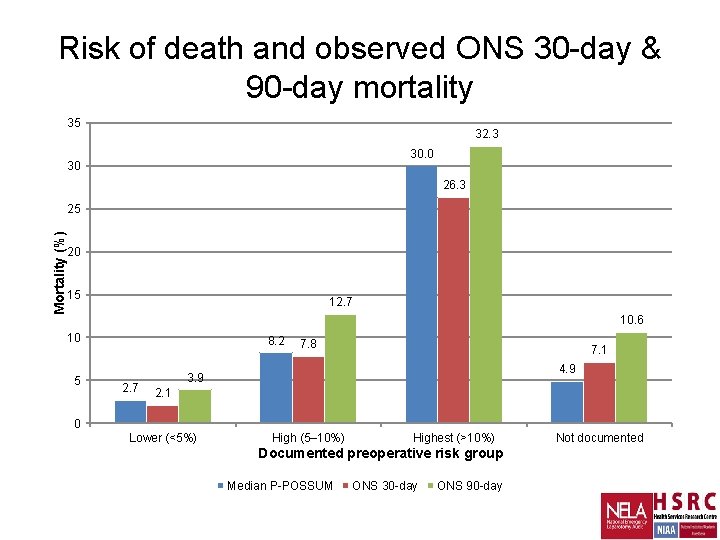
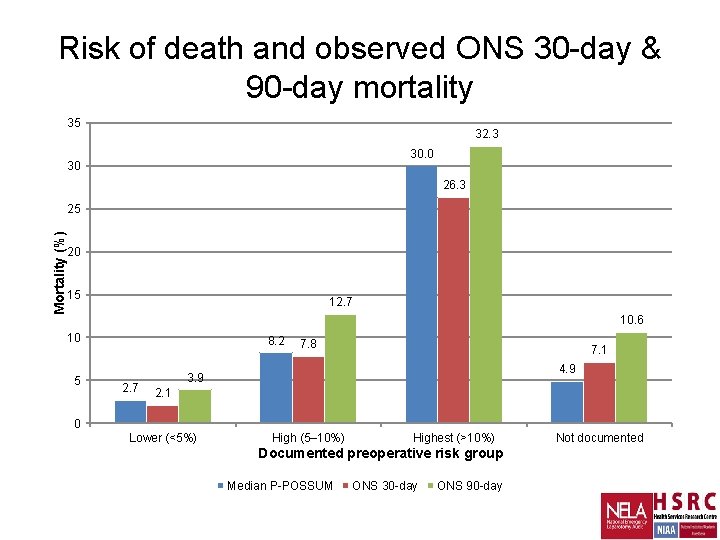
Risk of death and observed ONS 30 -day & 90 -day mortality 35 32. 3 30. 0 30 26. 3 Mortality (%) 25 20 15 12. 7 10. 6 10 5 8. 2 2. 7 7. 8 7. 1 4. 9 3. 9 2. 1 0 Lower (<5%) High (5– 10%) Highest (>10%) Documented preoperative risk group Median P-POSSUM ONS 30 -day ONS 90 -day Not documented
l a e t y l S s s e l e m a h S 38
Summary • Thank you for: 75, 000+ patients Improvement seen at personal level • Risk Assessment drives resources • Need organisational change • Not “National Audit”, but local Quality Improvement
 National emergency laparotomy audit
National emergency laparotomy audit National emergency laparotomy audit
National emergency laparotomy audit Nelson nec
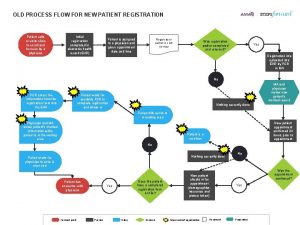
Nelson nec Patient registration process flowchart
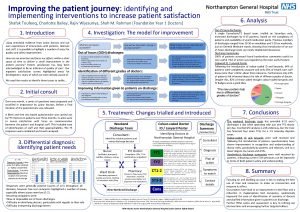
Patient registration process flowchart Improving the patient journey
Improving the patient journey Bronson intranet
Bronson intranet Improving chronic illness care model
Improving chronic illness care model Lifting and moving
Lifting and moving Health care levels primary secondary tertiary
Health care levels primary secondary tertiary Patient 2 patient
Patient 2 patient National emergency services academy
National emergency services academy National radiological emergency preparedness conference
National radiological emergency preparedness conference National emergency communications plan
National emergency communications plan Perbedaan audit konvensional dengan audit berbasis risiko
Perbedaan audit konvensional dengan audit berbasis risiko Audit informasi klinis
Audit informasi klinis Beda audit medis dan audit klinis
Beda audit medis dan audit klinis Penyelesaian audit dan tanggung jawab pasca audit
Penyelesaian audit dan tanggung jawab pasca audit Hubungan ekonomisasi efisiensi dan efektivitas
Hubungan ekonomisasi efisiensi dan efektivitas Prosedur audit bottom-up dan audit top-down!
Prosedur audit bottom-up dan audit top-down! Vouching in auditing
Vouching in auditing Perbedaan audit konvensional dengan audit berbasis risiko
Perbedaan audit konvensional dengan audit berbasis risiko Secondary objective of auditing
Secondary objective of auditing Audit universe
Audit universe Overall audit plan
Overall audit plan Emergency care system framework
Emergency care system framework Prehospital emergency care 10th edition
Prehospital emergency care 10th edition Therapeutic communication techniques
Therapeutic communication techniques Injuries first aid
Injuries first aid Enfield ems
Enfield ems Emergency care 13th edition
Emergency care 13th edition Emergency care and disaster preparation chapter 7
Emergency care and disaster preparation chapter 7 Chapter 54 basic emergency care
Chapter 54 basic emergency care Outdoor emergency care 6th edition
Outdoor emergency care 6th edition Care for a victim of an immunologic emergency
Care for a victim of an immunologic emergency Nhs 7 pillars
Nhs 7 pillars Chapter 8 emergency care first aid and disasters
Chapter 8 emergency care first aid and disasters Chapter 7 emergency care and disaster preparation
Chapter 7 emergency care and disaster preparation Prehospital care 11th edition
Prehospital care 11th edition Prehospital emergency care 11th edition study guide
Prehospital emergency care 11th edition study guide Prehospital emergency care 11th edition
Prehospital emergency care 11th edition