Multiple Fetal Pregnancy ELAHE ZAREAN Incidence and epidemiology





- Slides: 34
Multiple Fetal Pregnancy ELAHE. ZAREAN
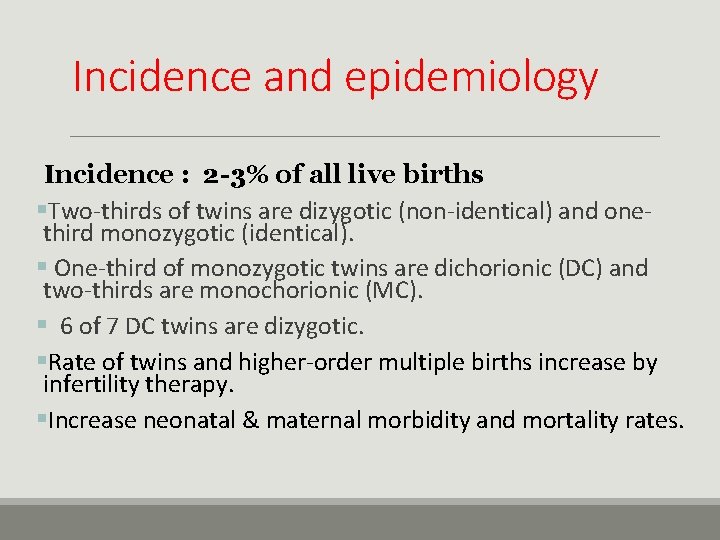
Incidence and epidemiology Incidence : 2 -3% of all live births §Two-thirds of twins are dizygotic (non-identical) and onethird monozygotic (identical). § One-third of monozygotic twins are dichorionic (DC) and two-thirds are monochorionic (MC). § 6 of 7 DC twins are dizygotic. §Rate of twins and higher-order multiple births increase by infertility therapy. §Increase neonatal & maternal morbidity and mortality rates.
Incidence and epidemiology Frequency of twins: a- Monozygotic: 1: 250 b- Dizygotic: ? Depend on race, hereditary, age, parity and fertility drugs. Hereditary mother important than father. Age peak at 37 years of age. Parity increase more than six times.
Etiology Dizygotic: It is a fertilization of two separate ovum. Monozygotic = Identical twins: It is a single fertilized ovum that subsequently divides into two similar structures.
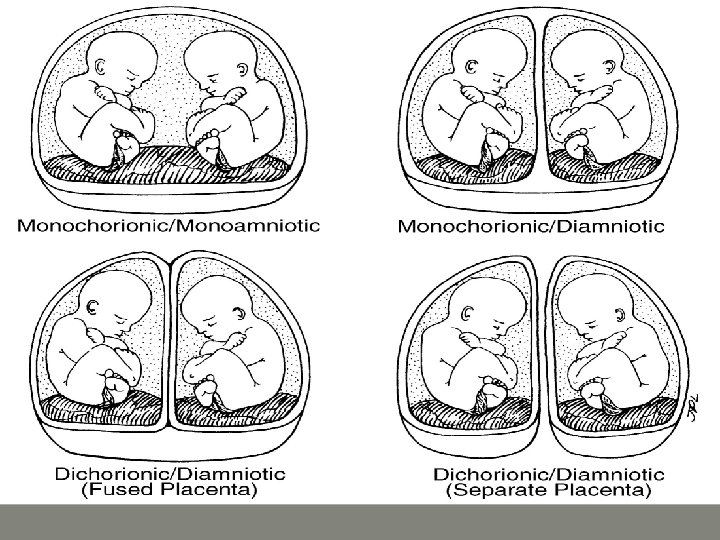
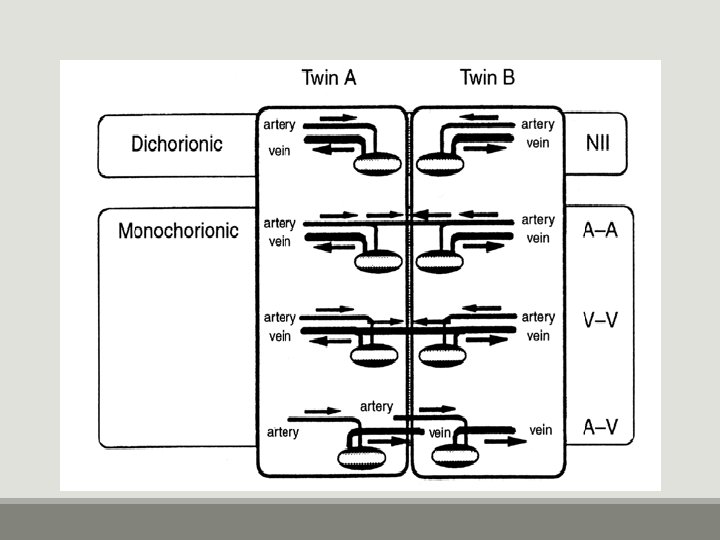
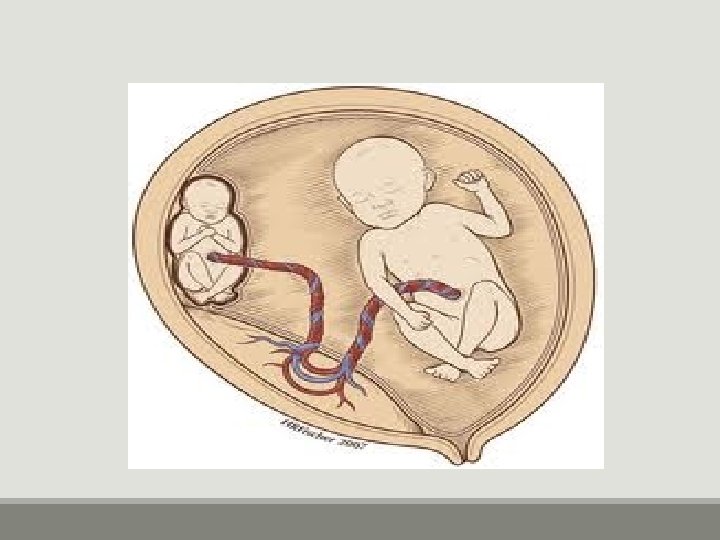
Divisions First 72 H two embryos, diamniotic, dichorionic and two placenta or single fused placenta. 4 -8 days two embryos, diamniotic, monochorionic. About 8 days after fertilization two embryos, monoamniotic and monochorionic.
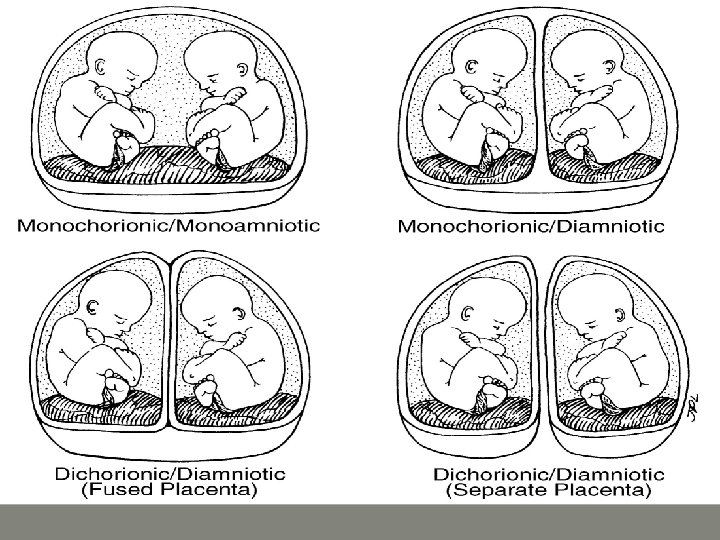
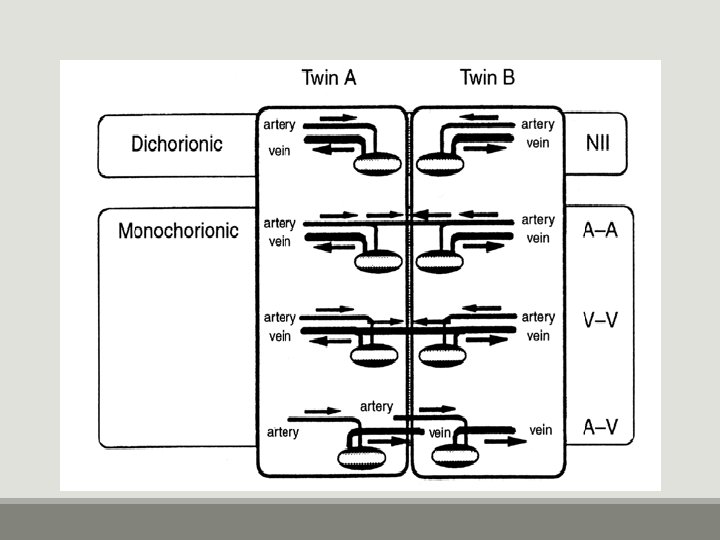
Types of twins zygosity refers to genetic work up of the pregnancy. Chorionicity indicate the membrane composition of the pregnancy (the chorion and amnion)
chorionicicity Increase risk of perinatal mortality and morbidity. The effect of the zygosity on the outcome is less clear. The outcome of dichorionic monozygotic seem to have the same outcome of dizygotic twins.
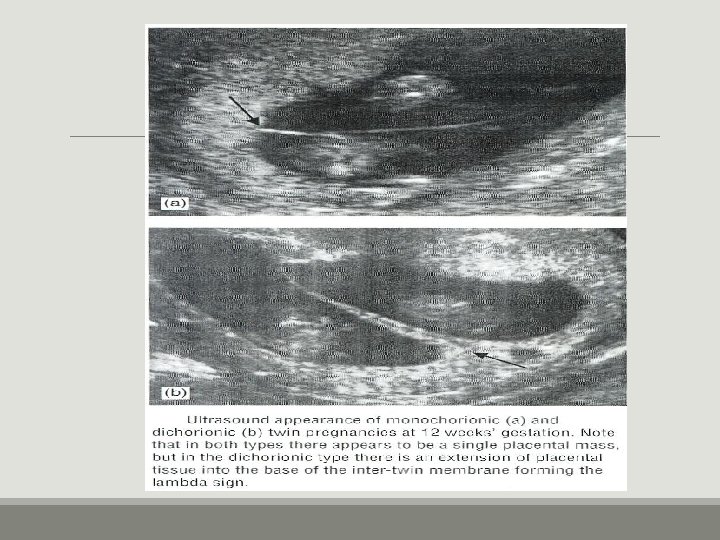
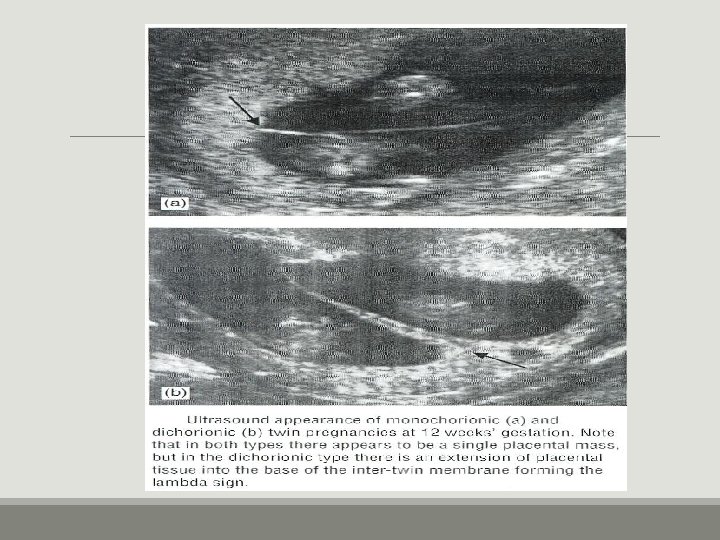
Determination of chorionicity The best way to determine chorionicity by ultrasound at 11 -13 weeks’ gestation. In DC pregnancies there is a triangular placental tissue projection (λ sign) into the base of the membranes. With advancing gestation, there is regression of the chorion laeve and the ‘lambda’ sign becomes progressively more difficult to identify. Thus by 20 weeks only 85% of DC pregnancies demonstrate the λ sign.
Diagnosis of Multiple Fetuses 1. History : Family history, Advanced age, High parity, Large maternal size, Medication. 1. Clinical Examination. 2. Investigations.
Pregnancy dating Spontaneous conception: use the crown-rump length of the longest fetus at 11 -13 weeks. IVF conception: use the embryonic age from fertilization.
Complications Maternal ◦ Pregnancy ◦ Labour ◦ Puerperium Fetal
Maternal complication During pregnancy: miscarriages Hyperemesis gravidorum Anaemia Pre-eclampsia (25%) Hydramnios ( 10 % )
GDM ( 2 – 3 times) Acute fatty liver Antepartum hemorrhage – placenta previa and placental abruption Cholestasis of pregnancy Malpresentations Preterm labour (50%) twins – 37 weeks, triplets – 34 weeks, quadruplets – 30 weeks Mechanical distress such as palpitation, dyspnea, varicosities and haemorrhoids
Obstructive uropathy , UTI Intervertebral discitis Amniotic fluid volume abnormalities
During Labour: Prelabour rupture of the membranes Cord prolapse Incoordinate uterine contractions Increased operative interference Placental abruption after delivery of 1 st baby Postpartum haemorrhage During puerperium: Subinvolution , Infection, Lactation failure
Fetal complication more with monochorionic Spontaneous abortion Single fetal demise Vanishing twin – before 10 weeks Fetus papyraceous/compressus – 2 nd trim Complications in 2 nd twin (depend on chorionicity) – neurological, renal lesions - anaemia, DIC - hypotension and death
Low birth weight ( 90%) Prematurity – spontaneous or iatrogenic Fetal growth restriction - in 3 rd trimester, asymmetrical, in both fetus Discordant growth - Difference of >20% in weight , >20 mm in AC, abnormal doppler waveforms
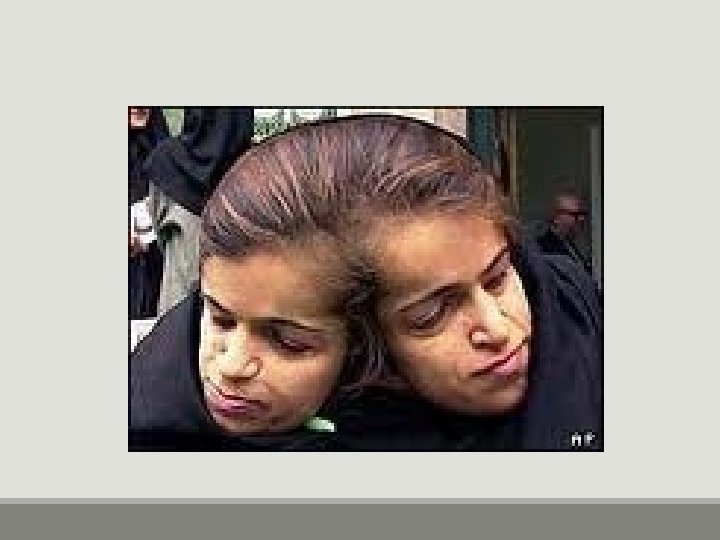
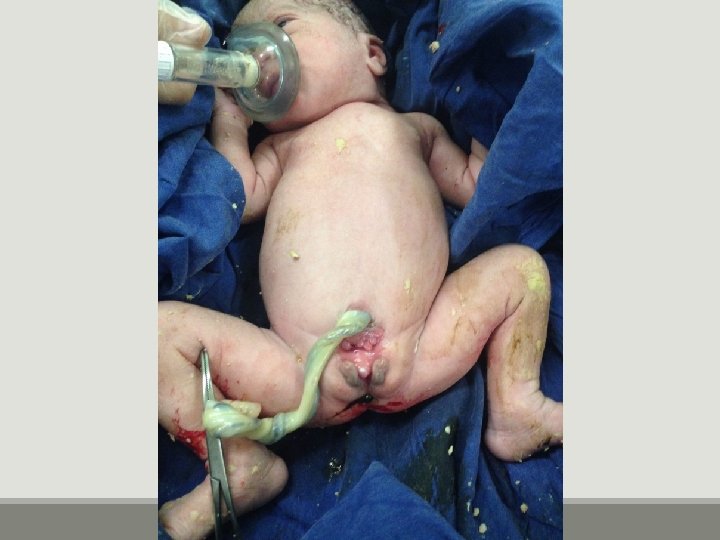
TRAP -Twin reversed arterial perfusion syndrome or Acardiac twin - absent heart in one fetus with arterioarterial communication in placenta, donor twin also dies Cord entanglement and compression – more in monoamniotic twins Locked twins Asphyxia – cord complication, abruption Still birth – antepartum or intrapartum cause
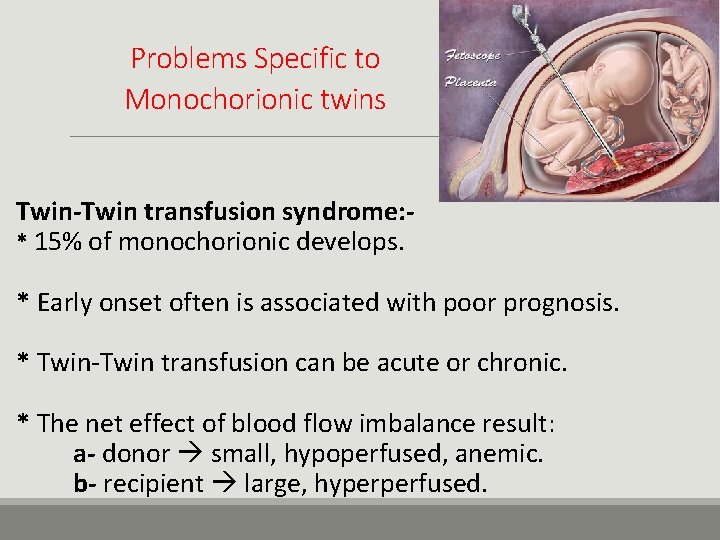
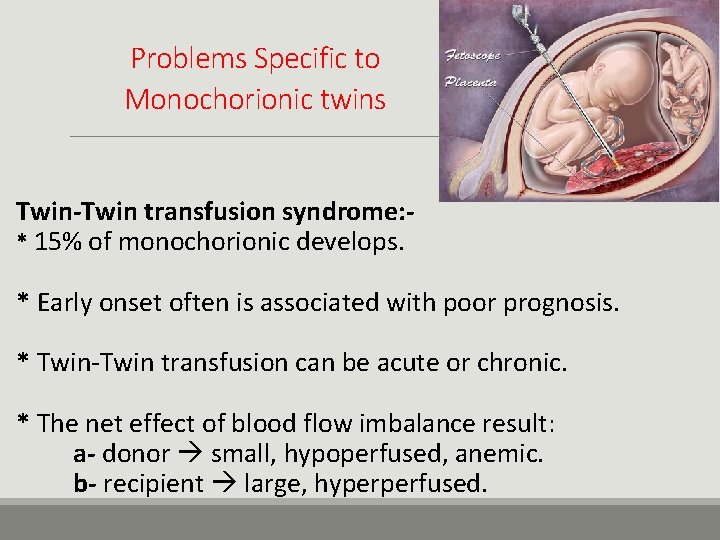
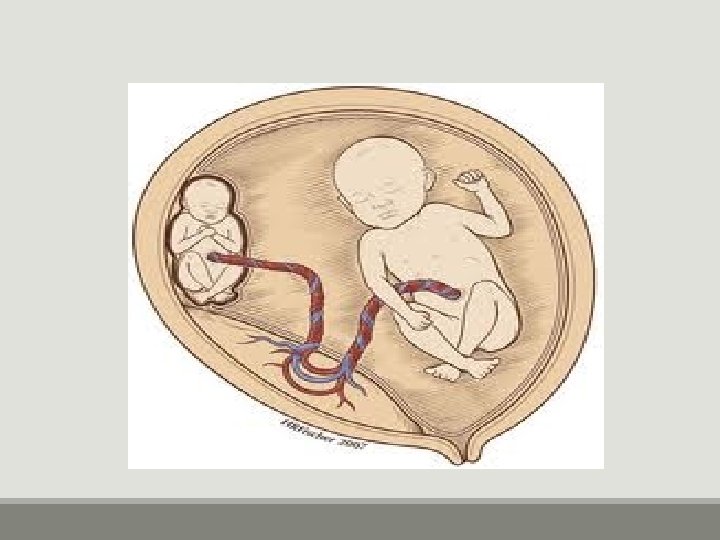
Problems Specific to Monochorionic twins Twin-Twin transfusion syndrome: * 15% of monochorionic develops. * Early onset often is associated with poor prognosis. * Twin-Twin transfusion can be acute or chronic. * The net effect of blood flow imbalance result: a- donor small, hypoperfused, anemic. b- recipient large, hyperperfused.




Antenatal Management Early diagnosis (mainly by ultra sound) Adequate nutrition: 1 - Caloric consumption increased by 300 Kcal per day. 2 - Iron 60 -100 mg per day. 3 - Folic acid 1 mg per day. Frequent prenatal visit: observe maternal and fetal complications 1 - Frequent ultrasound fetal growth, congenital anomalies, amniotic fluid. 2 - Doppler. 3 - BPP.
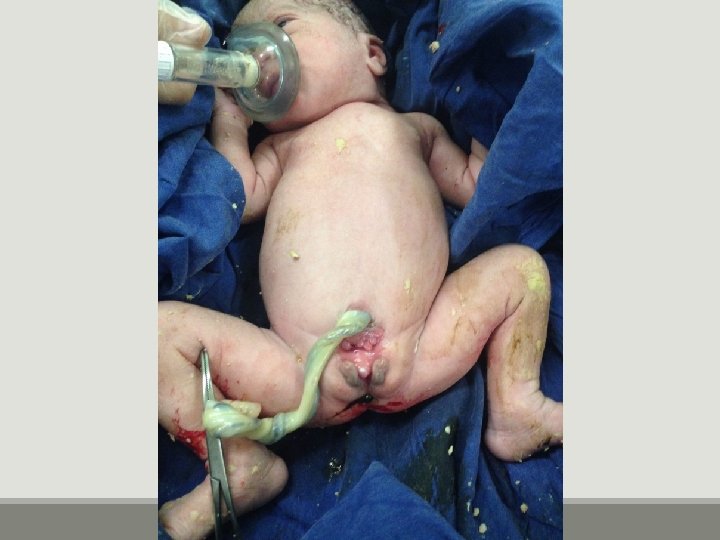
In Labor Management Trained obstetrical attendant. Available blood. Good access I. V live. CTG monitoring. Anesthetist Pediatrician for each fetus. Mode of delivery depend on presentation.
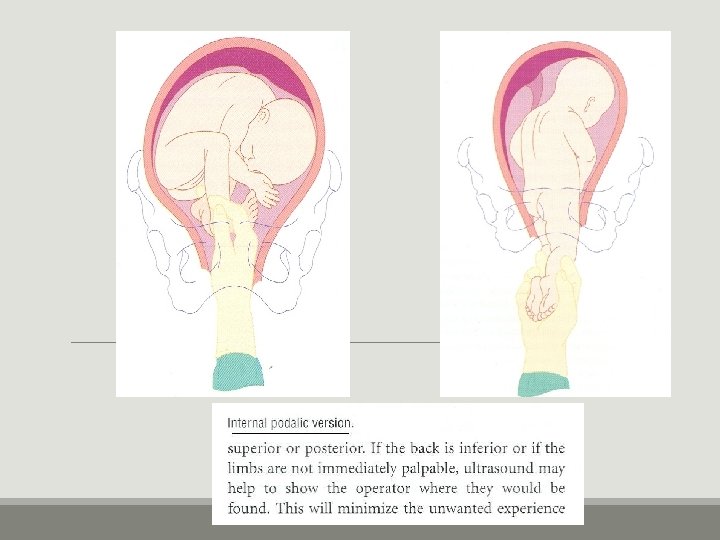
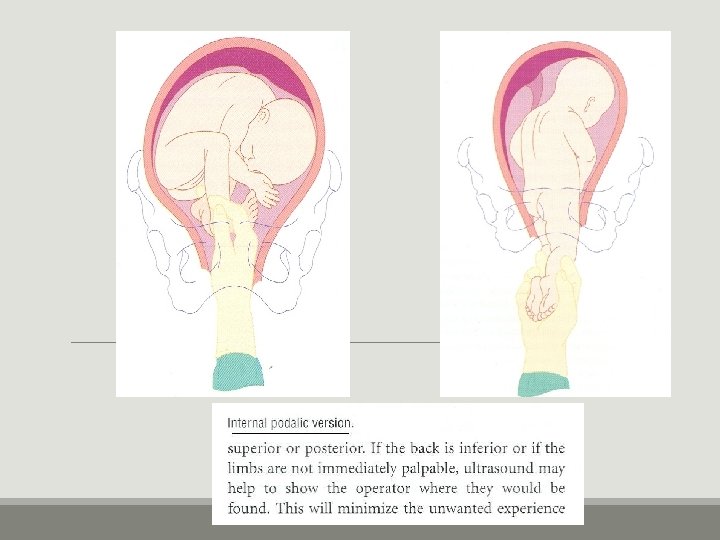
In Labor Management Ceph-ceph: NVD Ceph –non ceph: contraversy. Breech: cord prolaps, Head trappe, Locked twin: c/s. Second twin: 10 min and no contraction. Non fixed p. p : abdominal manipulation Second twin: internal pudalic version. Irregular FHR, VB, larger, Bx, Trans , contract Cx: C/S

 Prevalence calculation
Prevalence calculation Prevalence vs incidence
Prevalence vs incidence Pregnancy and fetal development brainpop answers
Pregnancy and fetal development brainpop answers Pregnancy and fetal development brainpop answers
Pregnancy and fetal development brainpop answers Molar pregnancy symptoms
Molar pregnancy symptoms Multiple pregnancy nursing diagnosis
Multiple pregnancy nursing diagnosis Thesourceagents
Thesourceagents Define nutritional epidemiology
Define nutritional epidemiology Descriptive vs analytical epidemiology
Descriptive vs analytical epidemiology Incidence and prevalence meaning
Incidence and prevalence meaning Certification board of infection control and epidemiology
Certification board of infection control and epidemiology Descriptive epidemiology
Descriptive epidemiology Incidence geometry proofs
Incidence geometry proofs Owasp cloud top 10
Owasp cloud top 10 Multiple baseline across settings
Multiple baseline across settings Disadvantages of mimd
Disadvantages of mimd Ukuran asosiasi epidemiologi
Ukuran asosiasi epidemiologi Logistic regression epidemiology
Logistic regression epidemiology Cross sectional study advantages and disadvantages
Cross sectional study advantages and disadvantages Attack rate calculation
Attack rate calculation Bibliography of epidemiology
Bibliography of epidemiology Example of recall bias
Example of recall bias Attack rate calculation
Attack rate calculation Ramboman
Ramboman Wheel of causation vs web of causation
Wheel of causation vs web of causation Defination of prevalence
Defination of prevalence Defination of epidemiology
Defination of epidemiology Distribution in epidemiology
Distribution in epidemiology What is descriptive study in epidemiology
What is descriptive study in epidemiology Spurious association
Spurious association Field epidemiology ppt
Field epidemiology ppt Bhisma murti
Bhisma murti Gordon epidemiology
Gordon epidemiology Epidemiology kept simple
Epidemiology kept simple Diabetic ketoacidosis epidemiology
Diabetic ketoacidosis epidemiology