INTRAPARTUM FETAL MONITORING ELAHE ZAREAN Suggestion to improve

- Slides: 83

INTRAPARTUM FETAL MONITORING ELAHE ZAREAN
Suggestion to improve • • CTG training courses CTG weekly meeting to discuss interesting cases Make the definition of the CTG as standard. Make the speed of the machine standard When in doubt ask for the second opinion. Practice , practice Good documentation Legal cases to be judged by CTG experts in interpretation and labor management
Fetal Surveillance • The goal of antepartum fetal surveillance is to prevent fetal death. • The goal of intrapartum fetal heart rate monitoring is to prevent fetal death and neurologic injury.
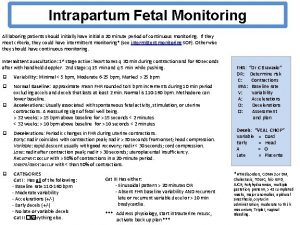
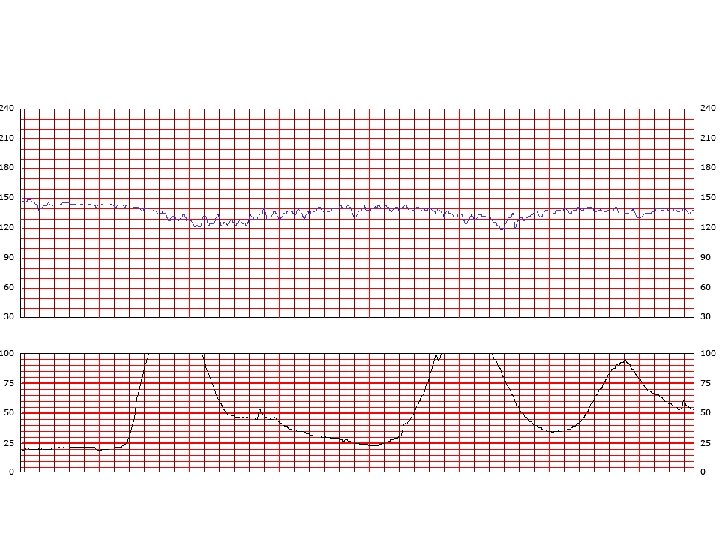
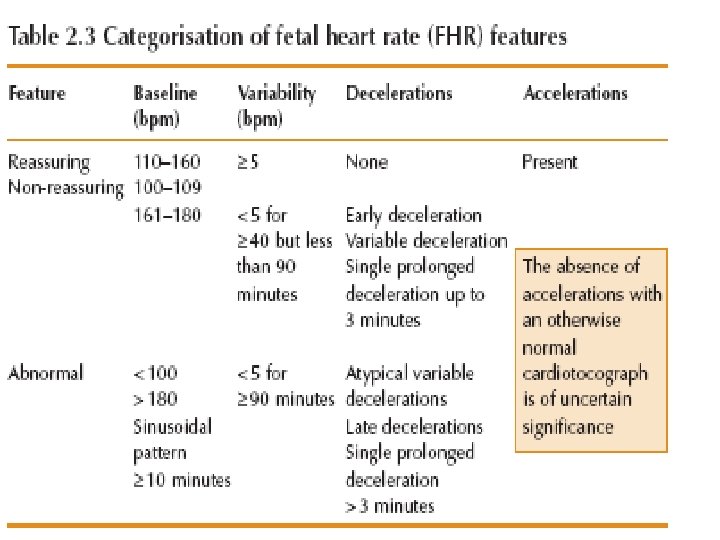
Interpretation of the Fetal Heart Tracing The interpretation of the fetal heart rate tracing should follow a systematic approach with a full qualitative and quantitative description of the following: • Baseline FHR rate variability • Periodic changes accelerations decelerations • Frequency and intensity of uterine contractions
DR C BRAVADO DR = determine risk C=contractions BRA = baseline rate V = variability A = accelerations D = decelerations O = overall assessment
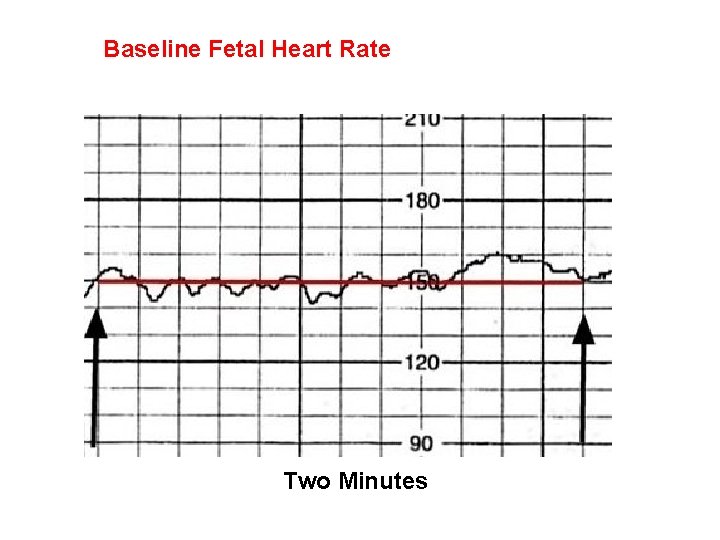
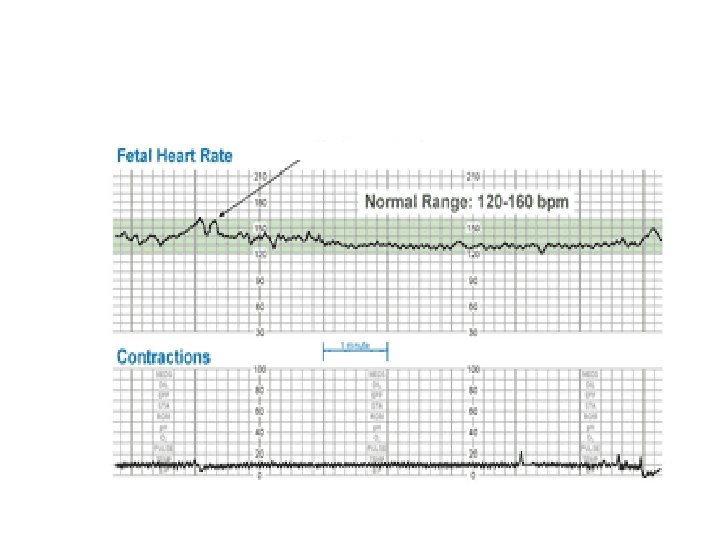
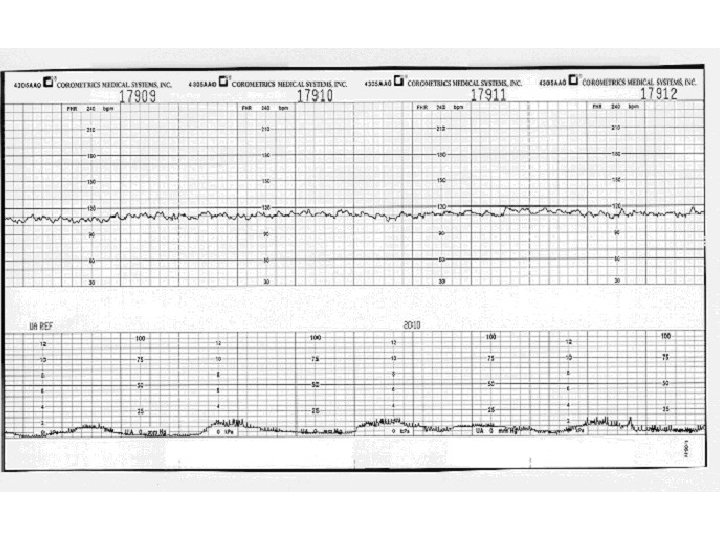
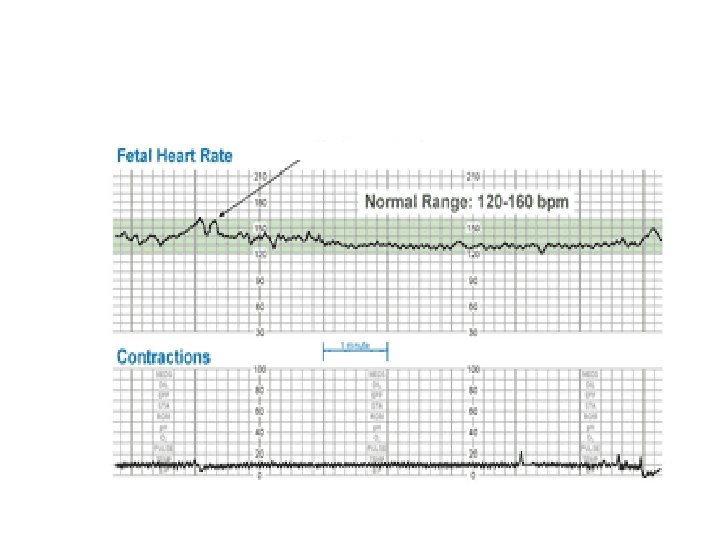
Baseline Fetal Heart Rate The baseline FHR is the heart rate during a 10 minute segment rounded to the nearest 5 beat per minute increment excluding periods of marked FHR variability, periodic or episodic changes, and segments of baseline that differ by more than 25 beats per minute. • The minimum baseline duration must be at least 2 minutes. • If minimum baseline duration is < 2 minutes then the baseline is indeterminate. • Normal baseline = 110 -160 bpm
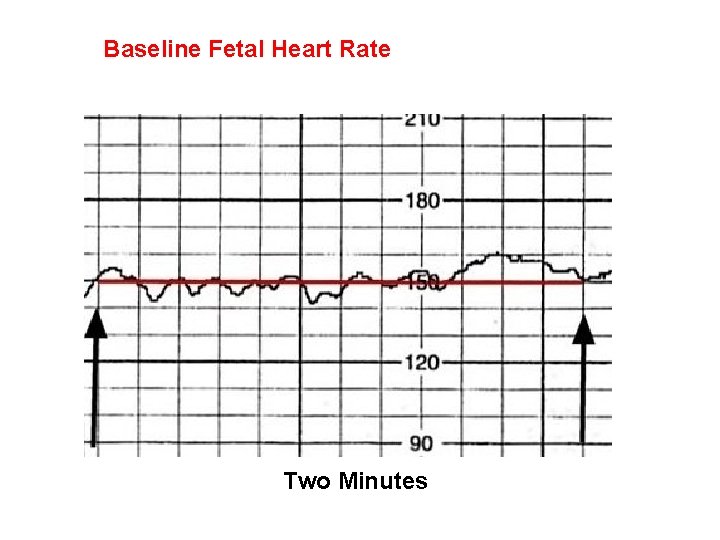
Baseline Fetal Heart Rate Two Minutes
bradycardia • Distinguish between bradycardia & prolonged deceleration • Drug , hypothermia , hypoglycemia • Complete heart block
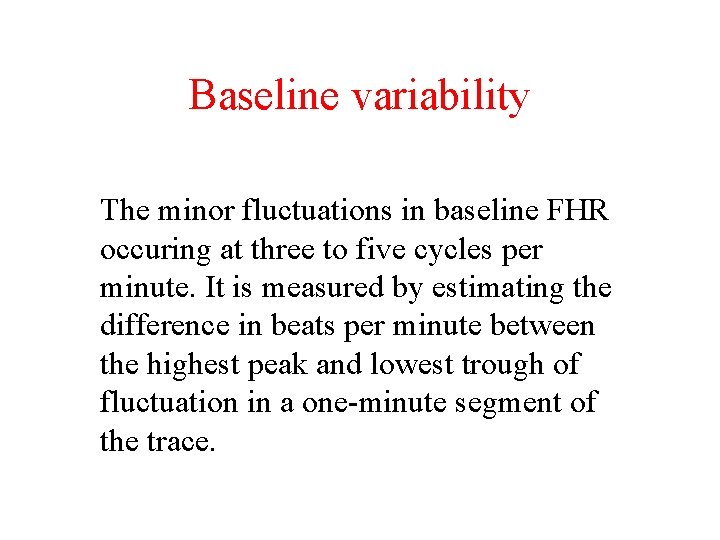
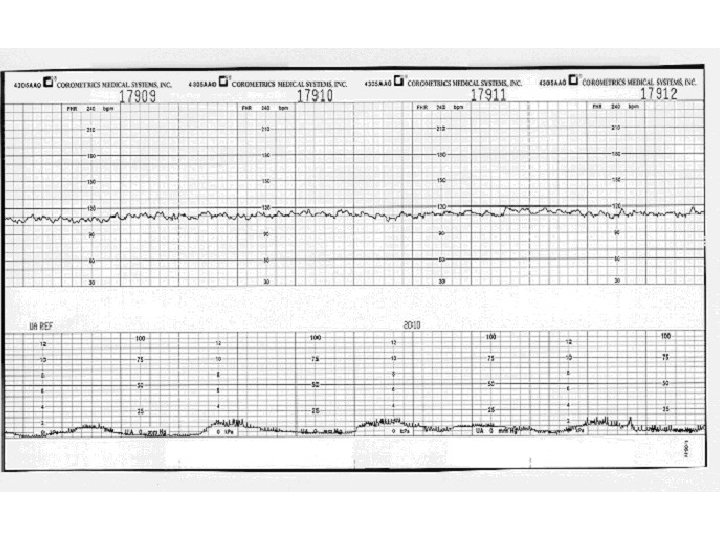
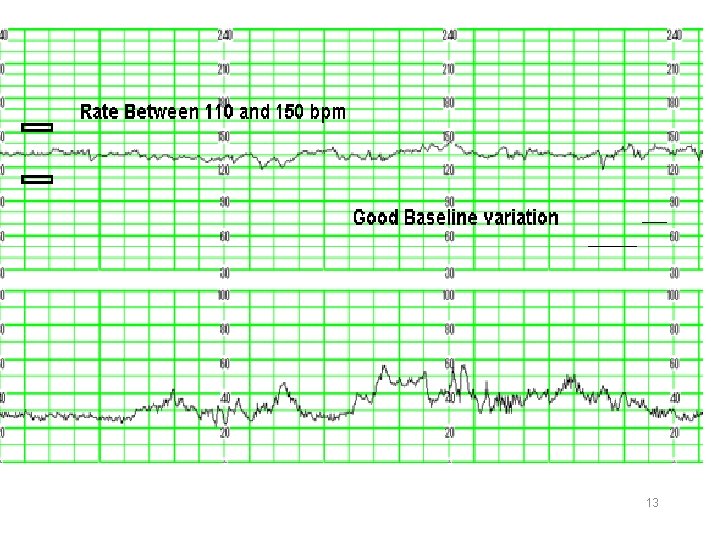
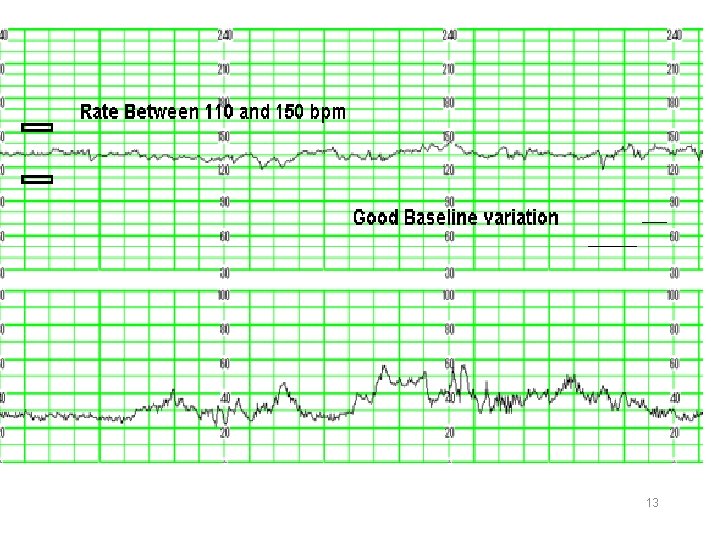
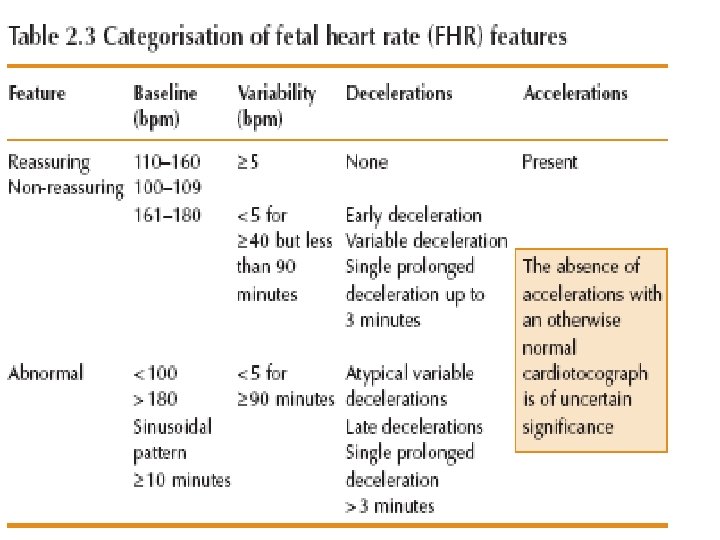
Baseline variability The minor fluctuations in baseline FHR occuring at three to five cycles per minute. It is measured by estimating the difference in beats per minute between the highest peak and lowest trough of fluctuation in a one-minute segment of the trace.
13
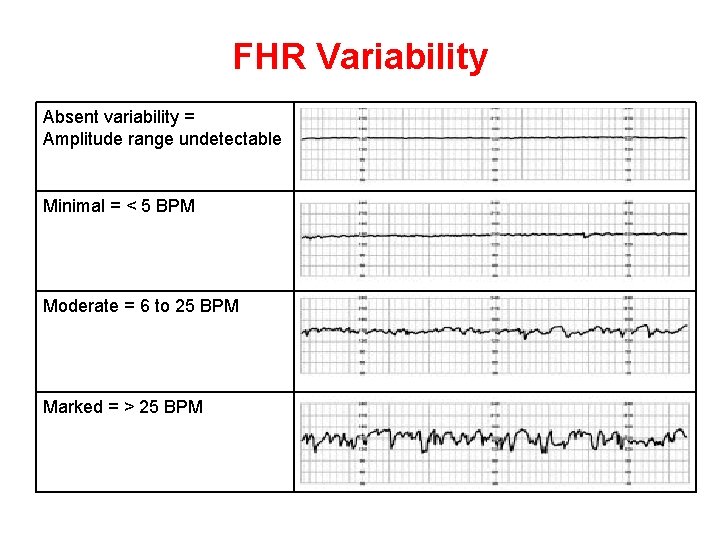
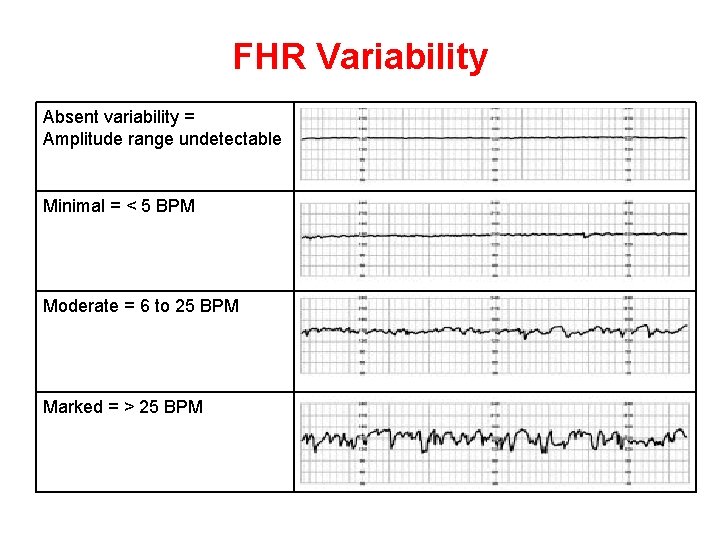
FHR Variability Absent variability = Amplitude range undetectable Minimal = < 5 BPM Moderate = 6 to 25 BPM Marked = > 25 BPM
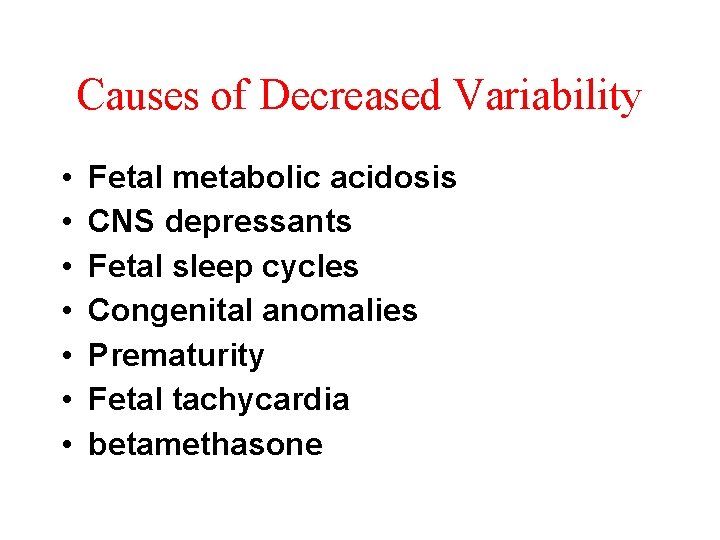
Causes of Decreased Variability • • Fetal metabolic acidosis CNS depressants Fetal sleep cycles Congenital anomalies Prematurity Fetal tachycardia betamethasone
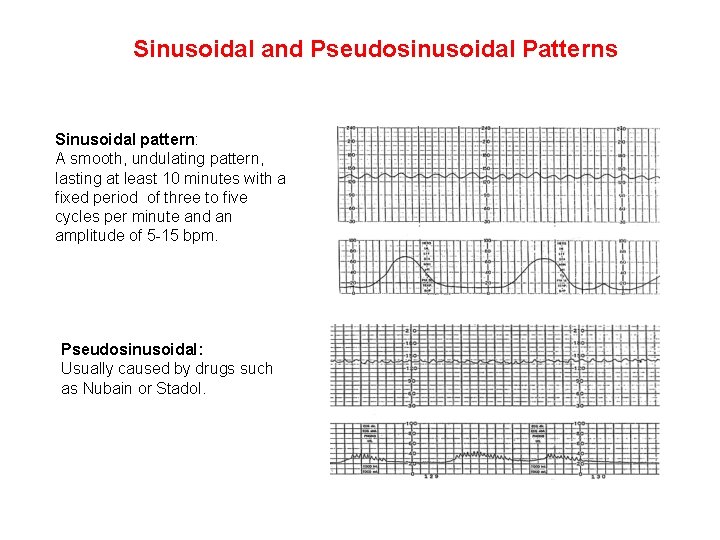
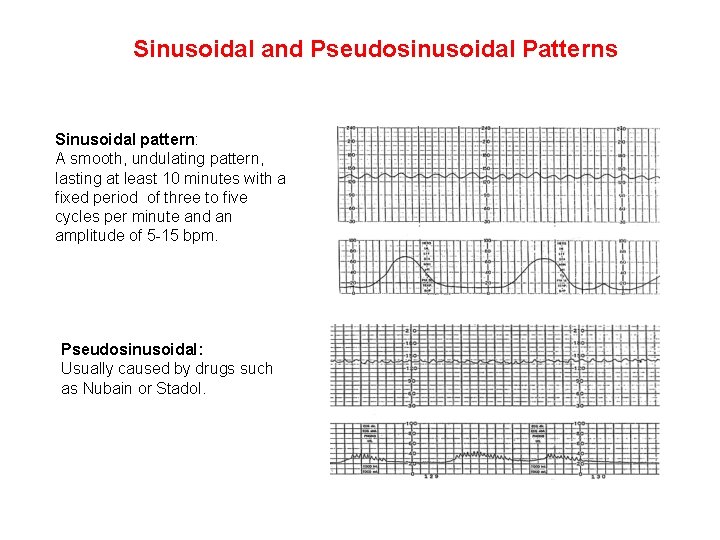
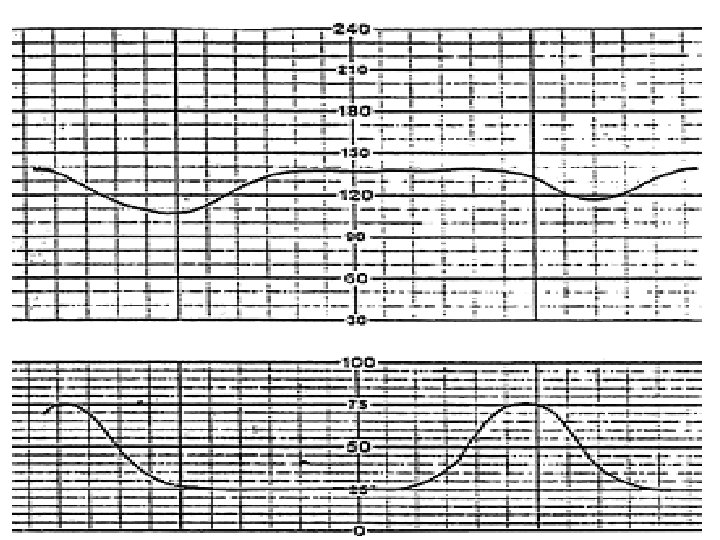
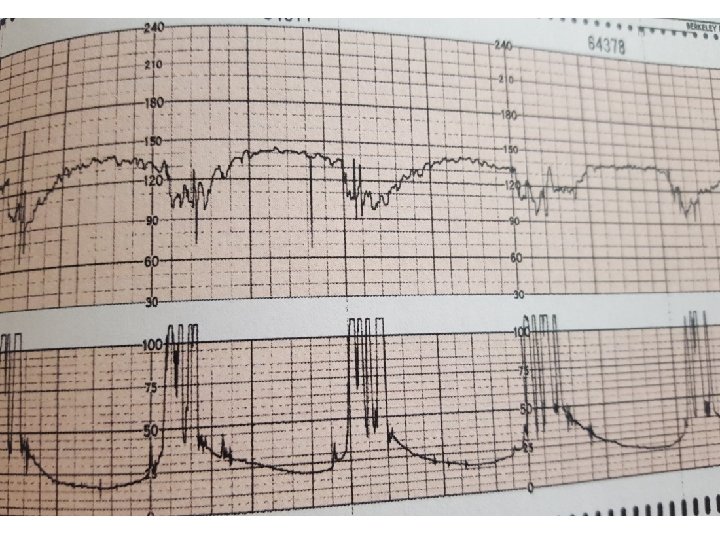
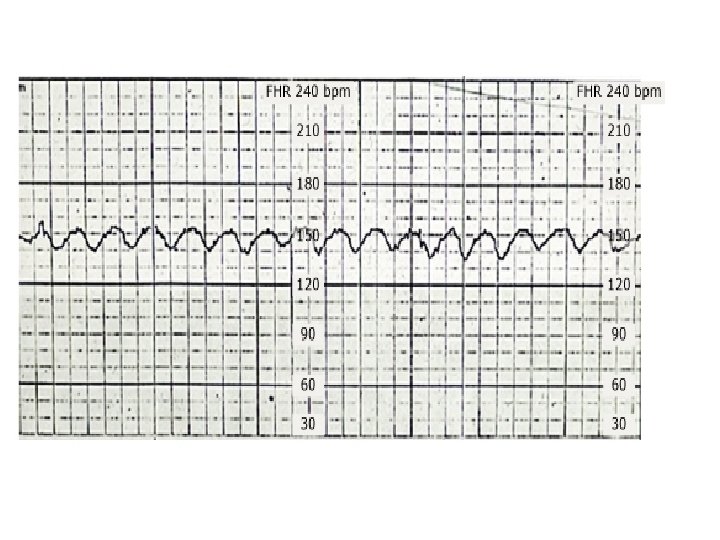
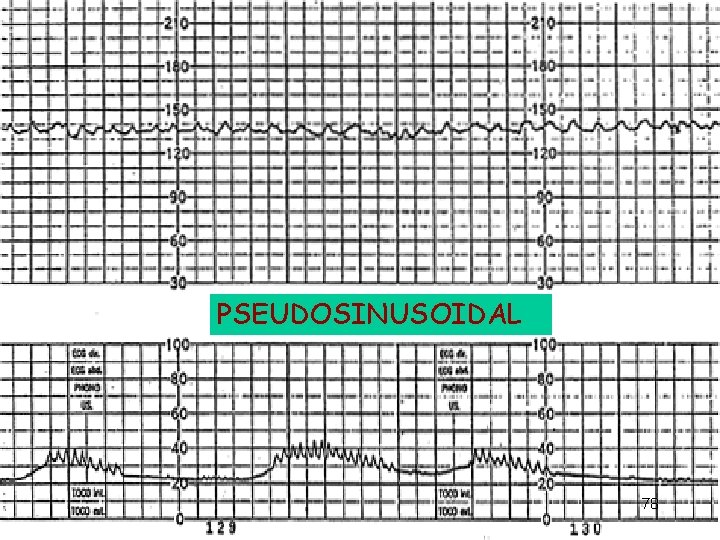
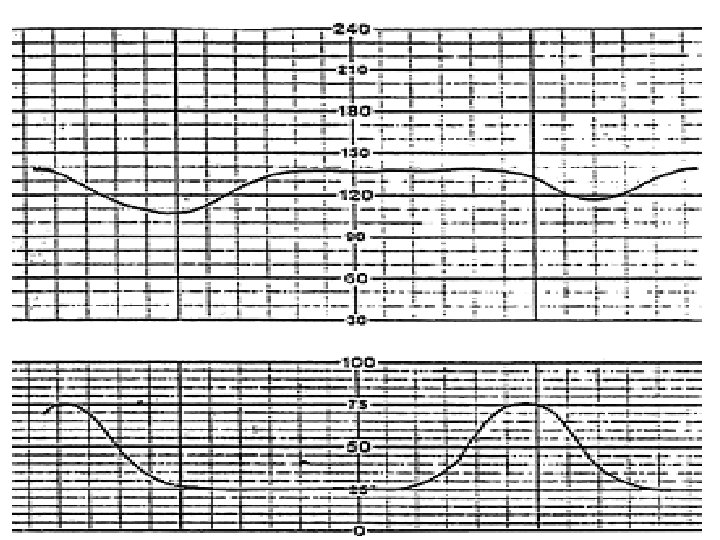
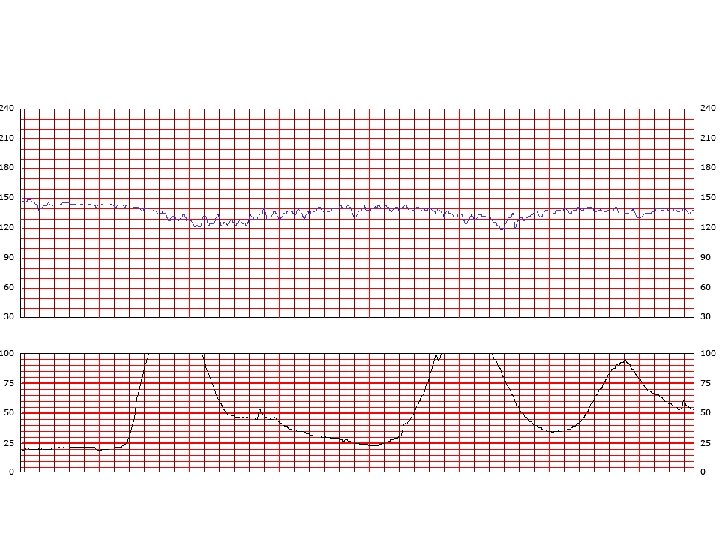
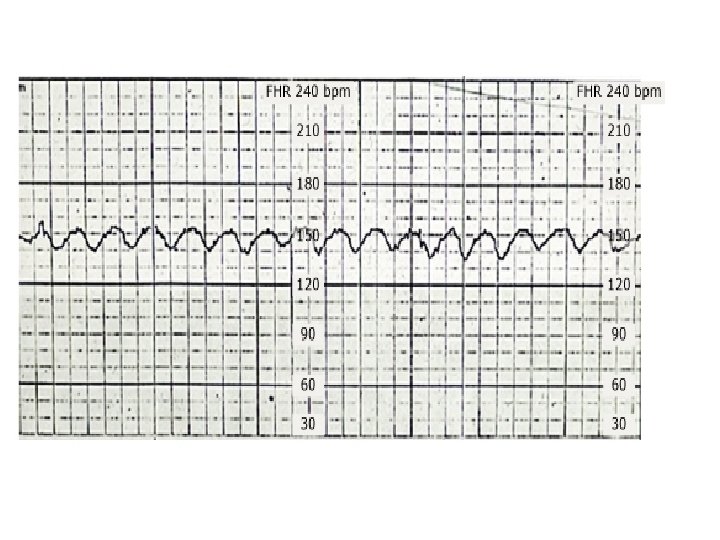
Sinusoidal and Pseudosinusoidal Patterns Sinusoidal pattern: A smooth, undulating pattern, lasting at least 10 minutes with a fixed period of three to five cycles per minute and an amplitude of 5 -15 bpm. Pseudosinusoidal: Usually caused by drugs such as Nubain or Stadol.
Accelerations An acceleration is an abrupt increase in FHR above baseline with onset to peak of the acceleration less than < 30 seconds and less than 2 minutes in duration. The duration of the acceleration is defined as the time from the initial change in heart rate from the baseline to the time of return to the FHR to baseline. • <32 weeks' : >10 BPM above baseline for >10 seconds. • >32 weeks' : >15 BPM above baseline for > 15 seconds. • Prolonged acceleration: Increase in heart rate lasts for 2 to 10 minutes. • The absence of accelerations for more than 80 minutes correlates with increased neonatal morbidity.
DECCELERATIONS • EARLY : Head compression • LATE : U-P Insufficiency • VARIABLE : Cord compression & Cord stretch
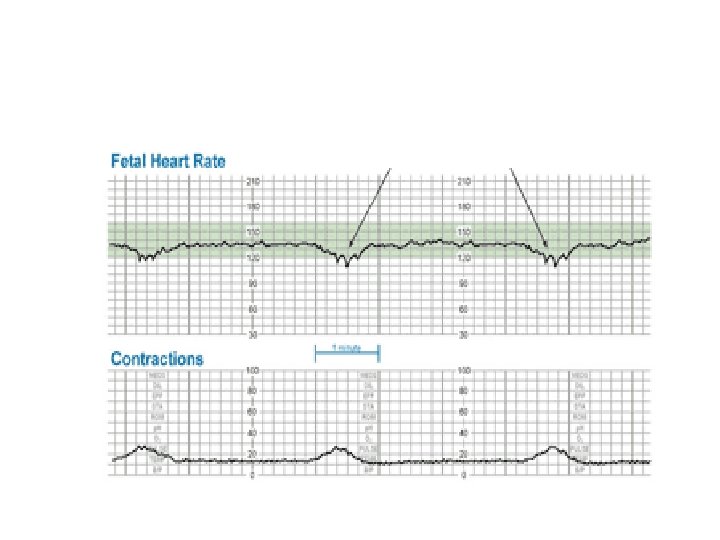
Decelerations The type of the deceleration is distinguished on the basis of its waveform : · Abrupt (variables) decrease in FHR below baseline with onset to nadir < 30 seconds. · Gradual decrease and return to baseline with time from onset of the deceleration to nadir >30 seconds.
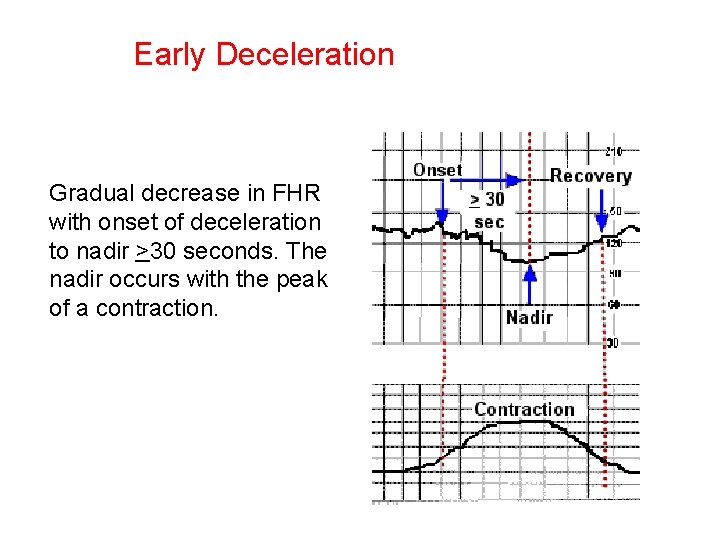
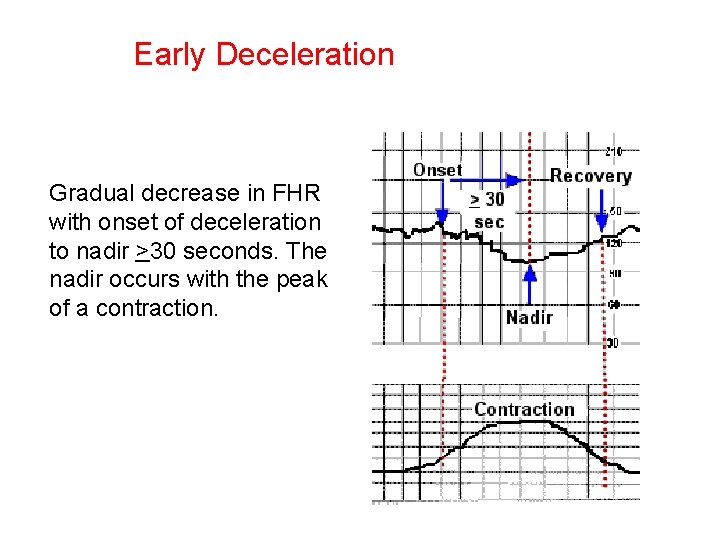
Early Deceleration Gradual decrease in FHR with onset of deceleration to nadir >30 seconds. The nadir occurs with the peak of a contraction.
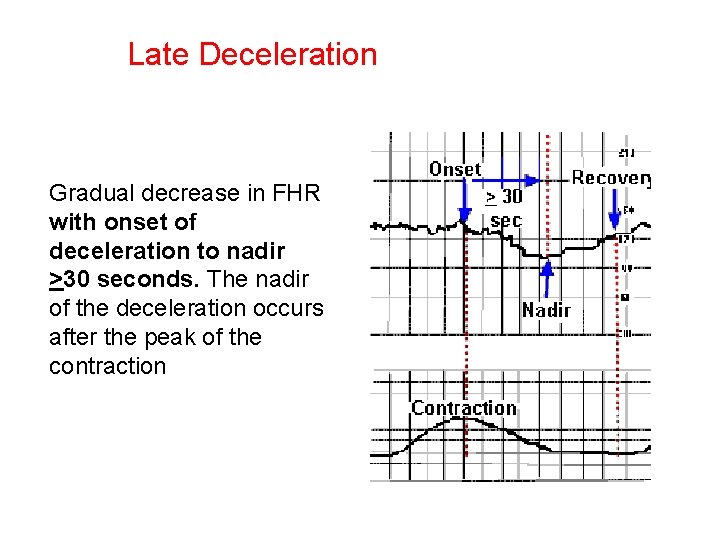
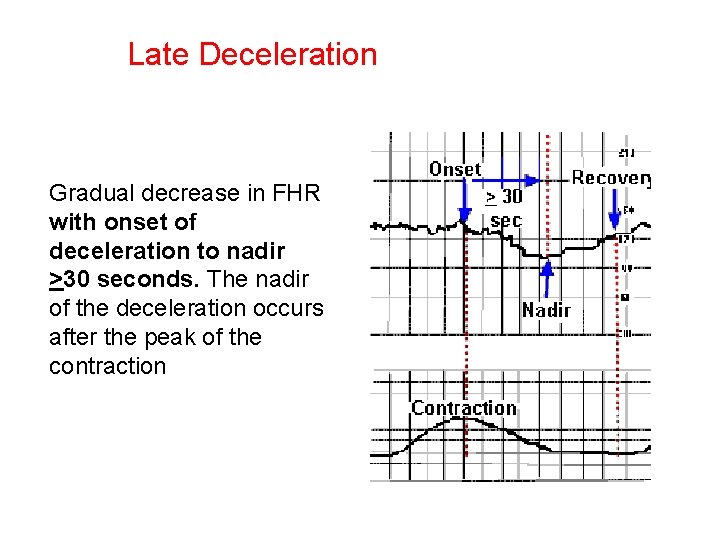
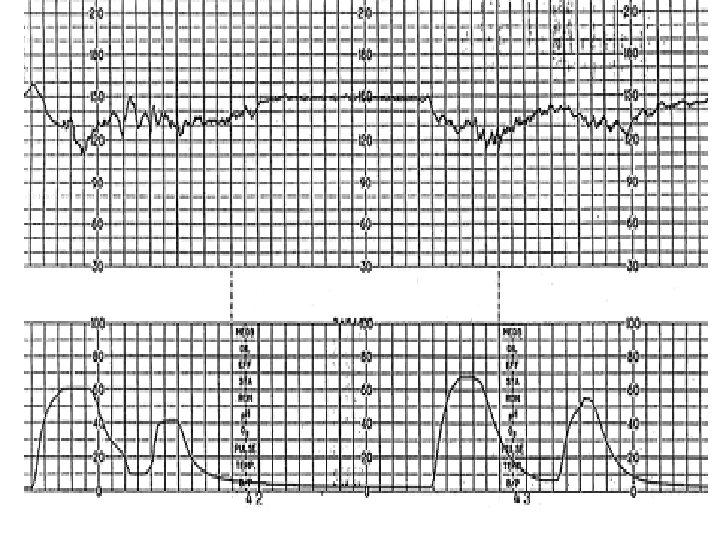
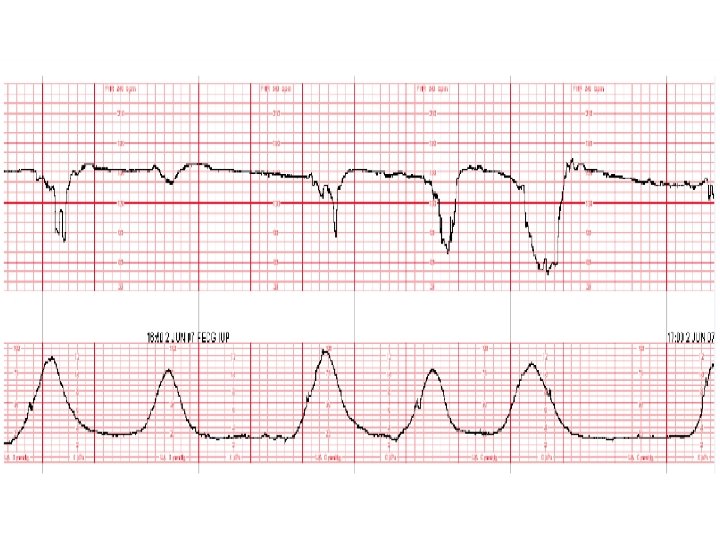
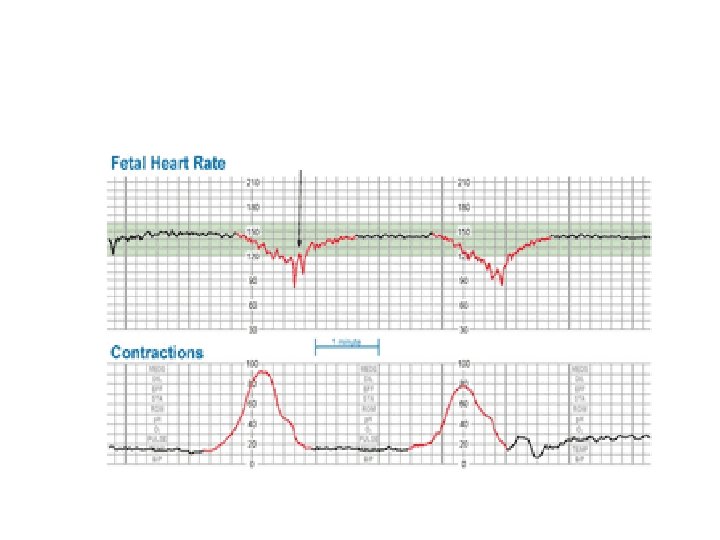
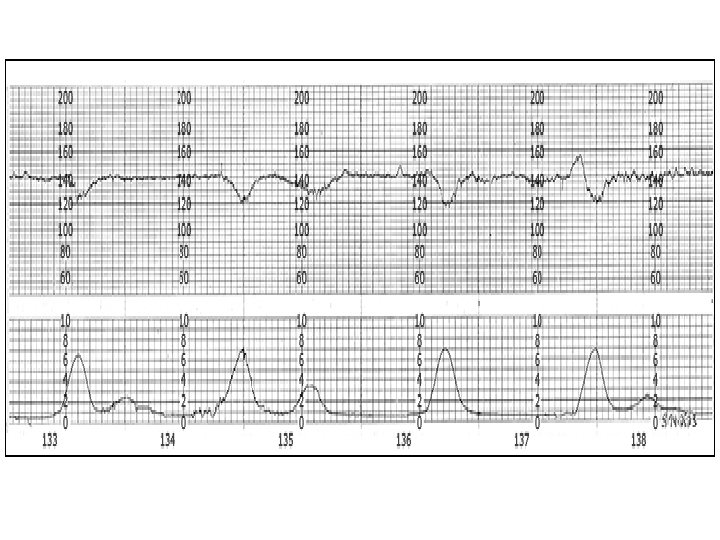
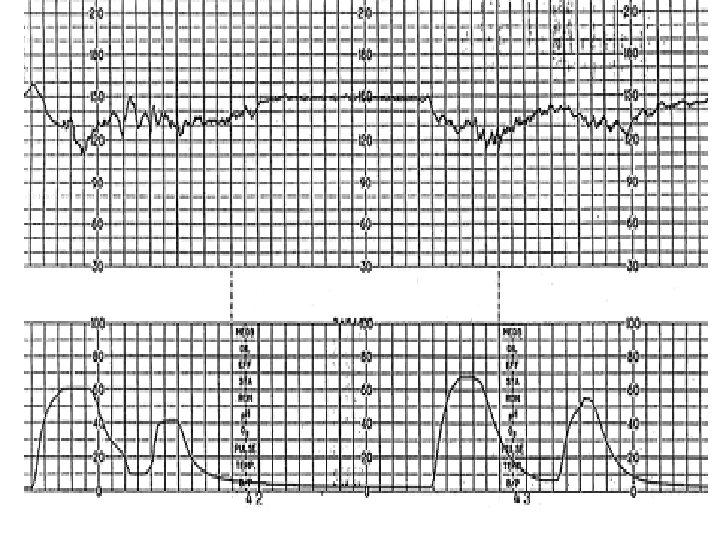
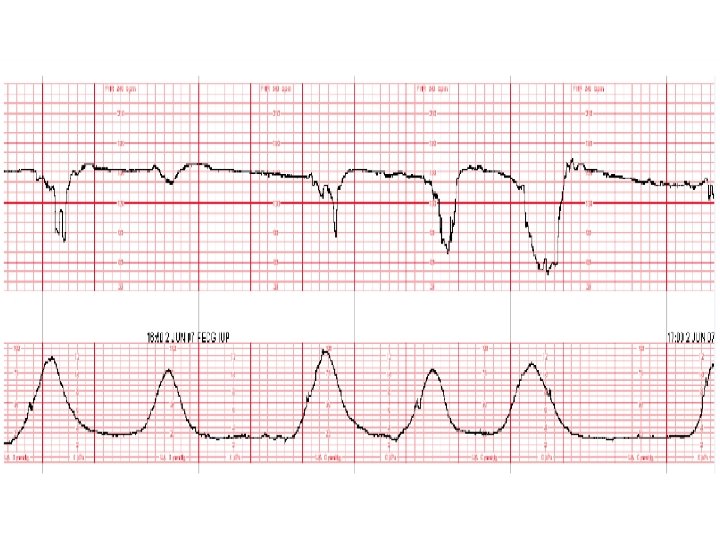
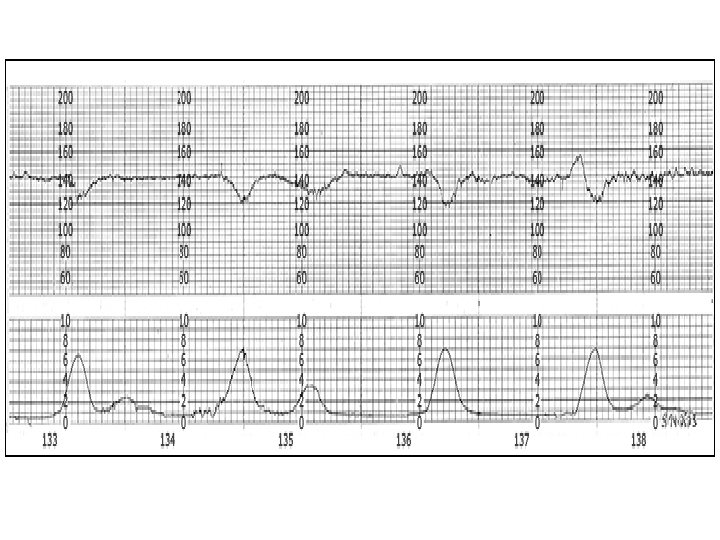
Late Deceleration Gradual decrease in FHR with onset of deceleration to nadir >30 seconds. The nadir of the deceleration occurs after the peak of the contraction
Late Deceleration • Reflex • Myocardial depression
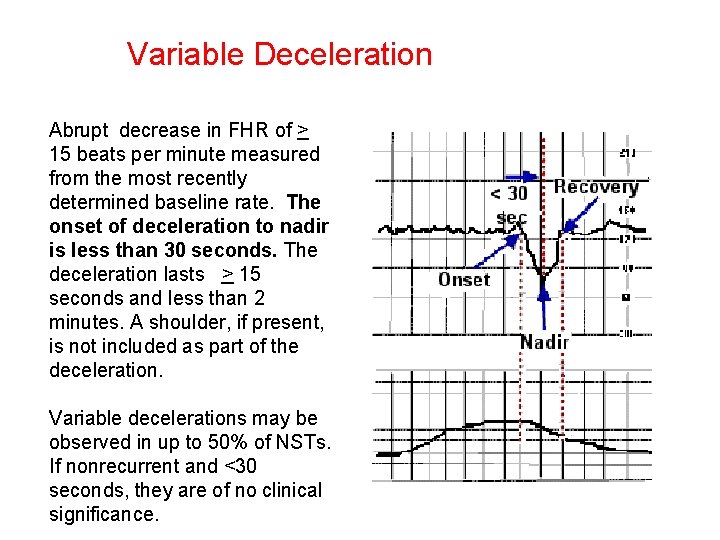
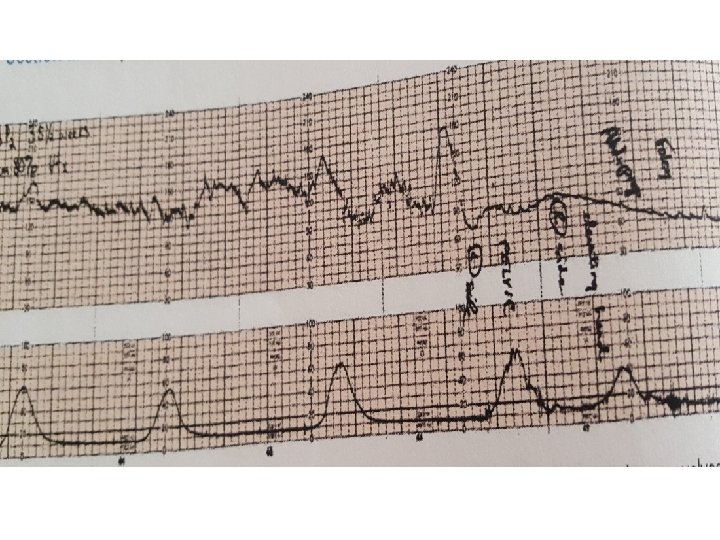
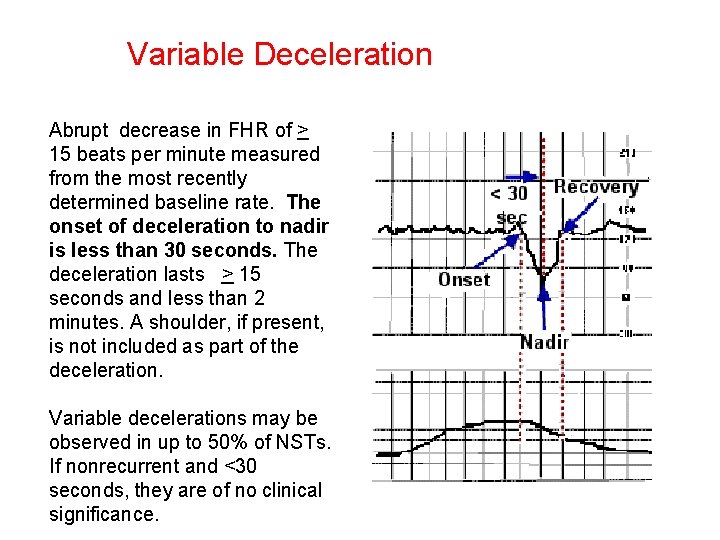
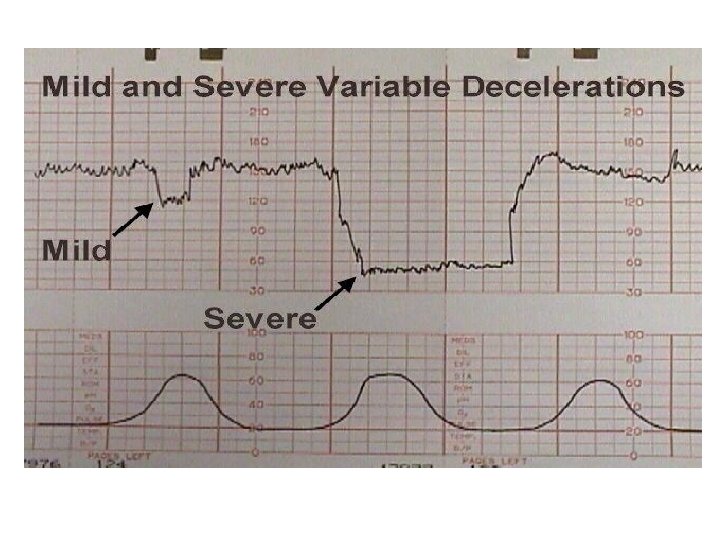
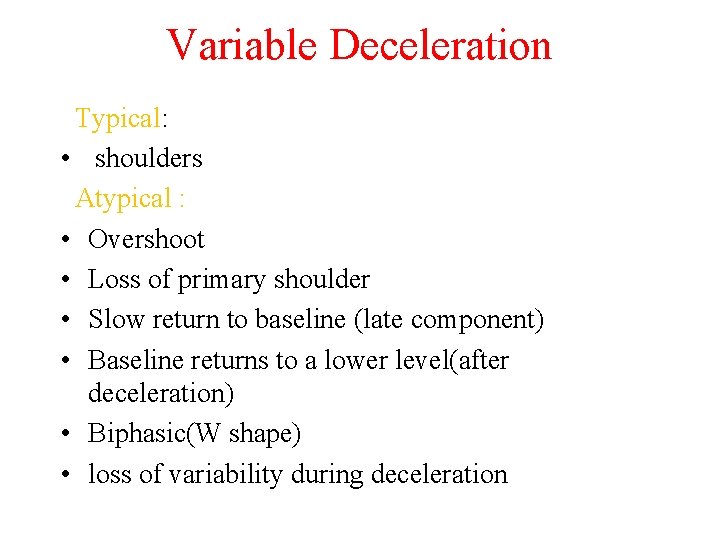
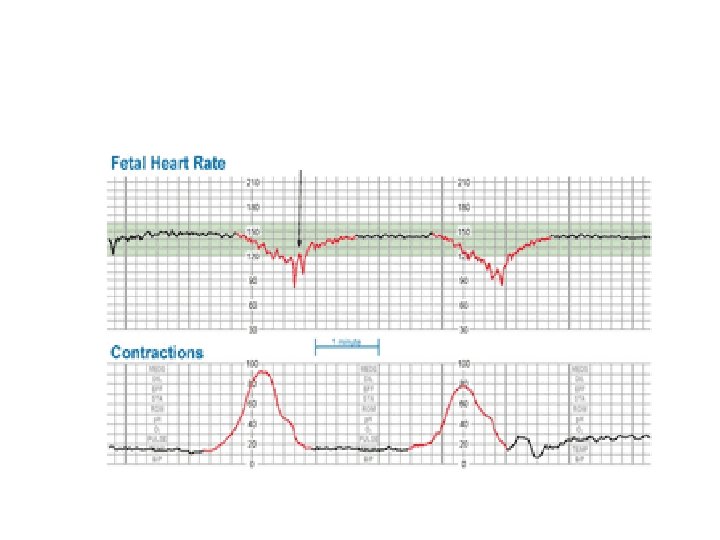
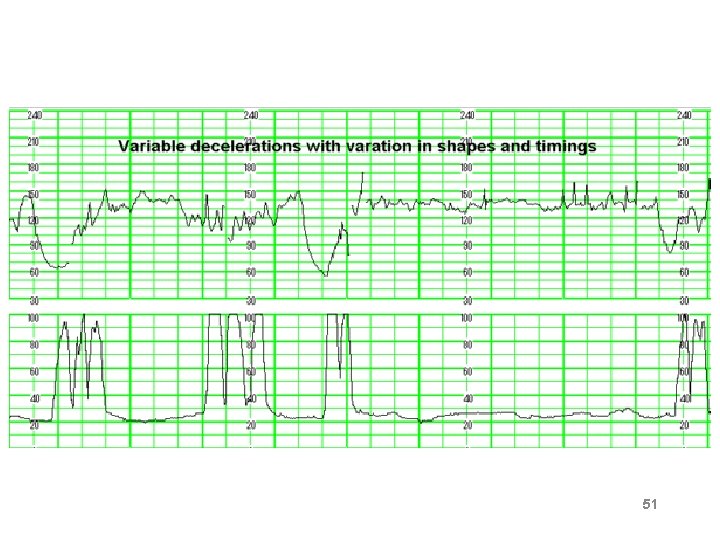
Variable Deceleration Abrupt decrease in FHR of > 15 beats per minute measured from the most recently determined baseline rate. The onset of deceleration to nadir is less than 30 seconds. The deceleration lasts > 15 seconds and less than 2 minutes. A shoulder, if present, is not included as part of the deceleration. Variable decelerations may be observed in up to 50% of NSTs. If nonrecurrent and <30 seconds, they are of no clinical significance.
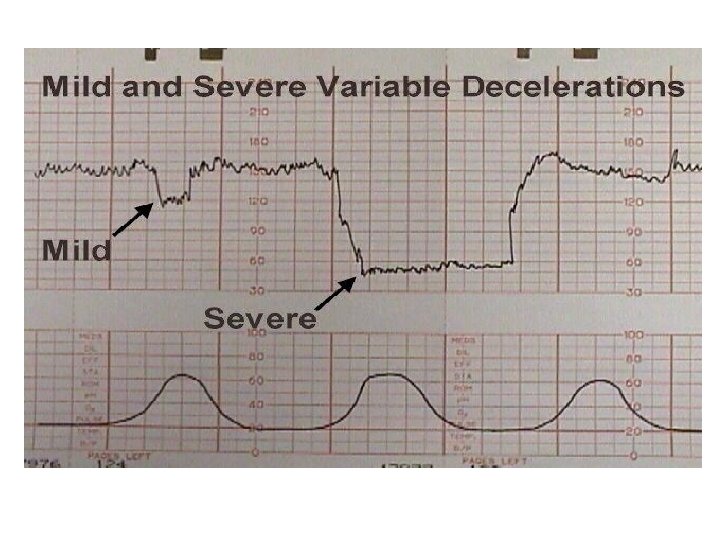
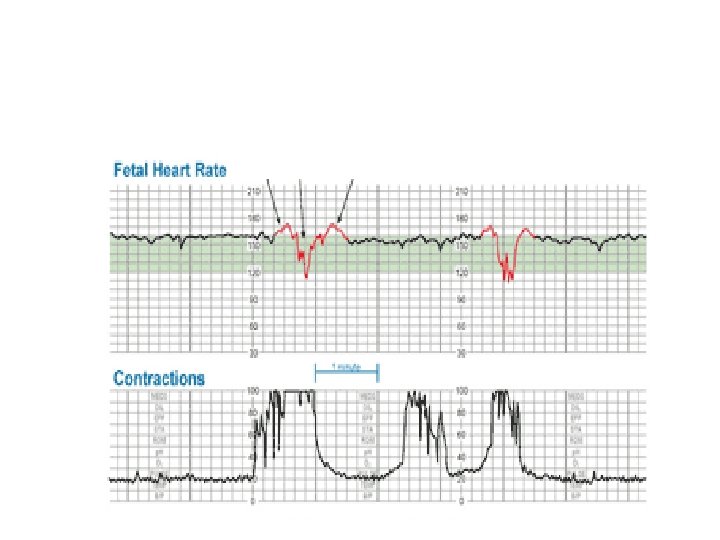
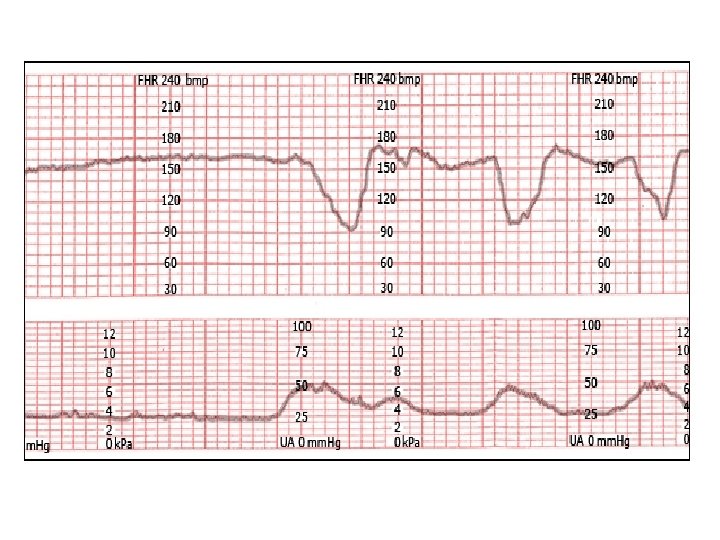
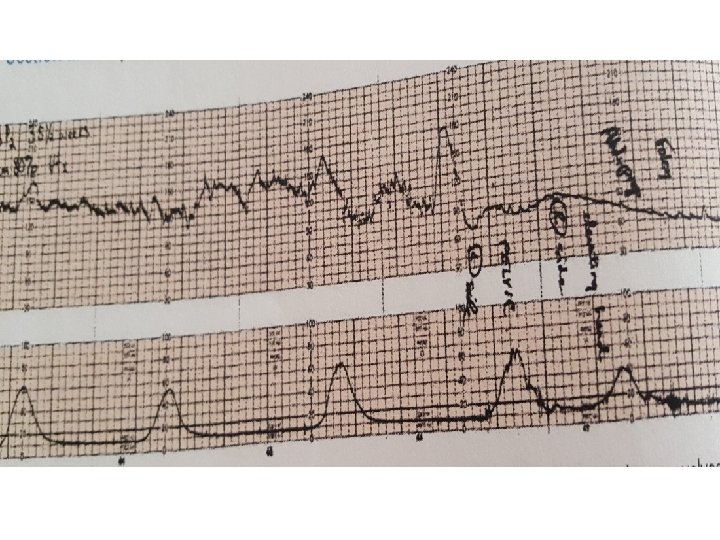
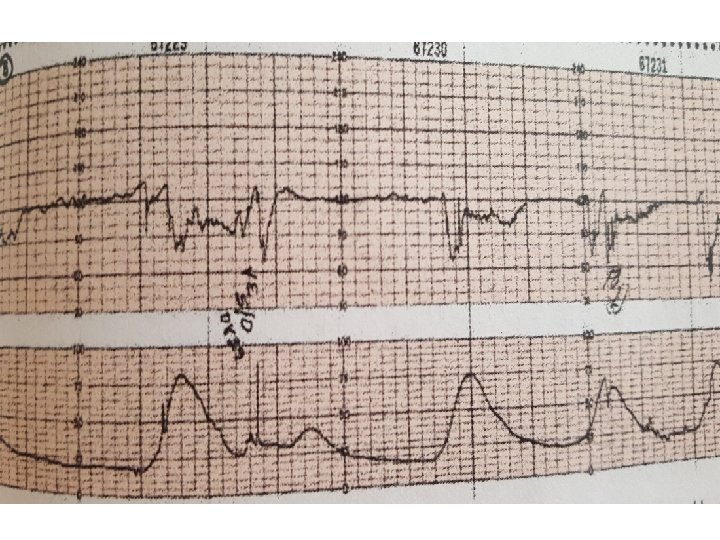
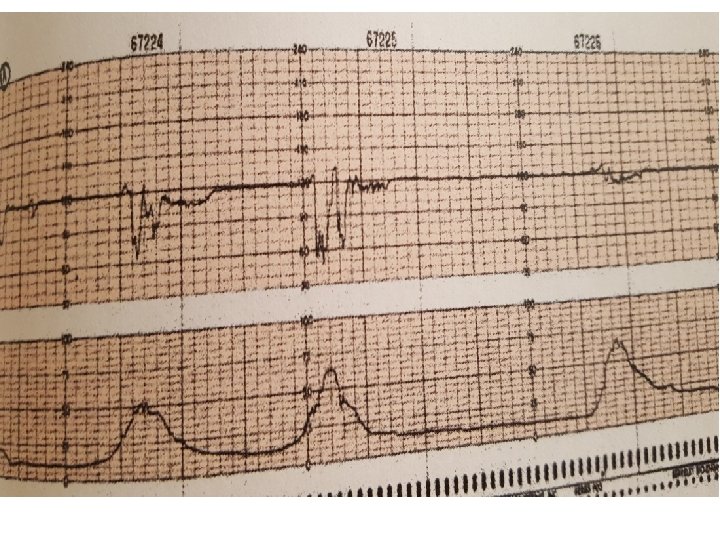
Variable Deceleration Typical: • shoulders Atypical : • Overshoot • Loss of primary shoulder • Slow return to baseline (late component) • Baseline returns to a lower level(after deceleration) • Biphasic(W shape) • loss of variability during deceleration
Classification severity of variable deceleration • Mild: duration < 30 second or depth up to 80 bpm • Moderate : deceleration < 80 bpm • Severe : deceleration < 70 bpm for more than 60 second
Red flags • Loss of variability • Complicated tachycardia
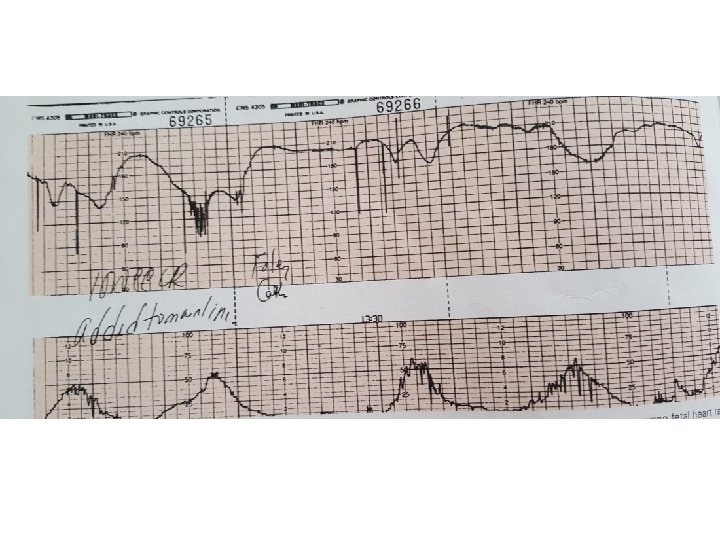
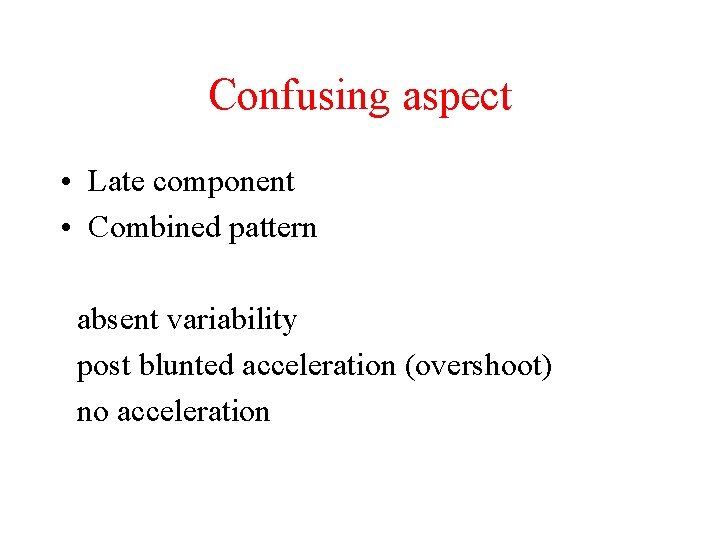
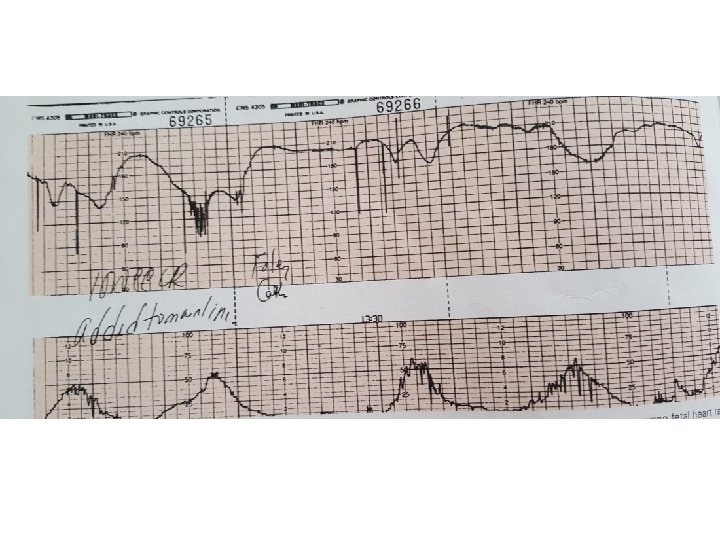
Confusing aspect • Late component • Combined pattern absent variability post blunted acceleration (overshoot) no acceleration
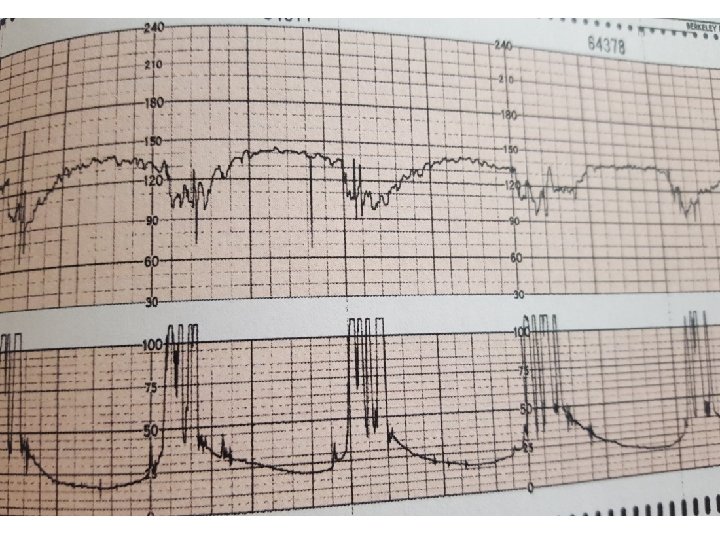
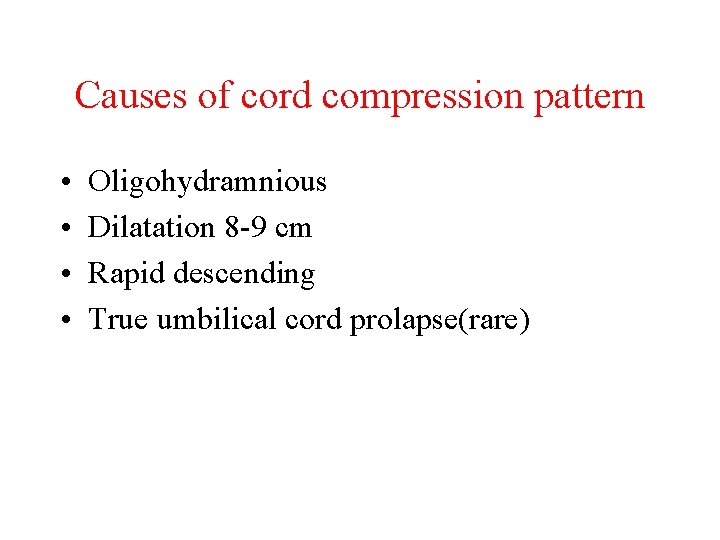
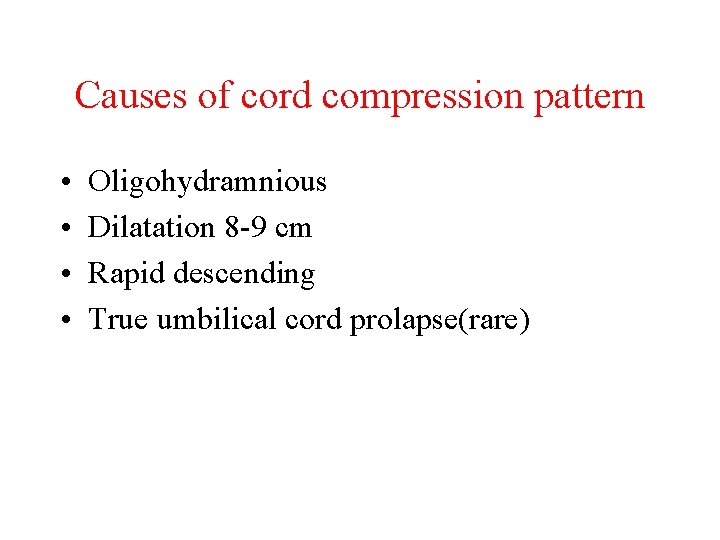
Causes of cord compression pattern • • Oligohydramnious Dilatation 8 -9 cm Rapid descending True umbilical cord prolapse(rare)
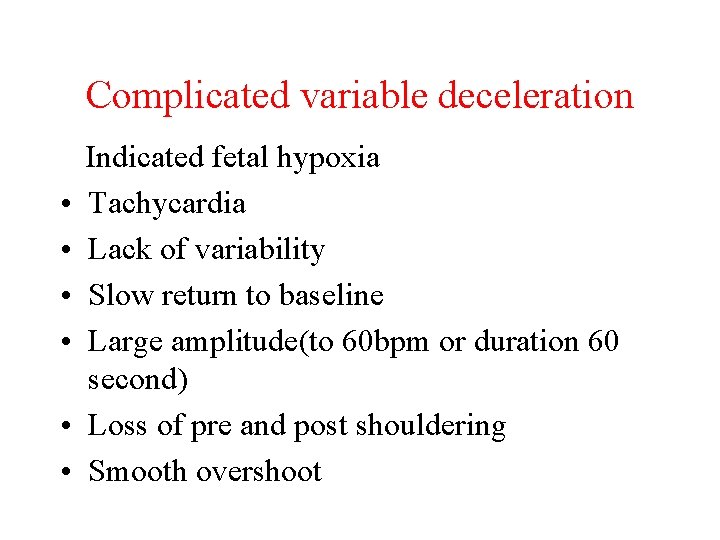
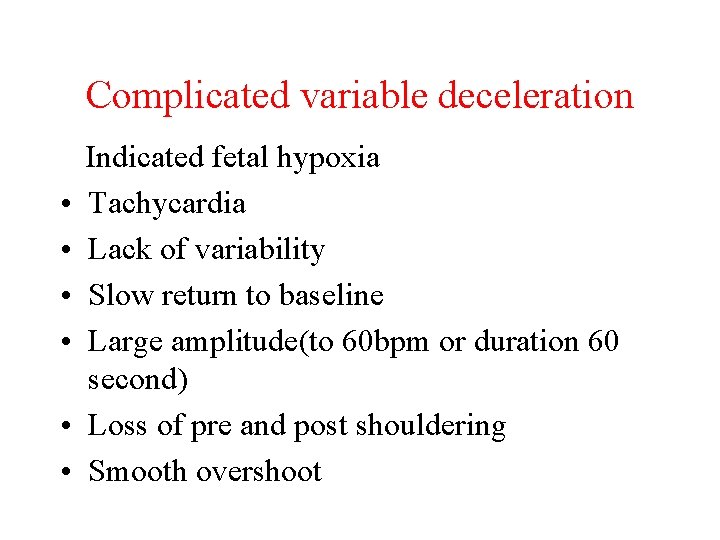
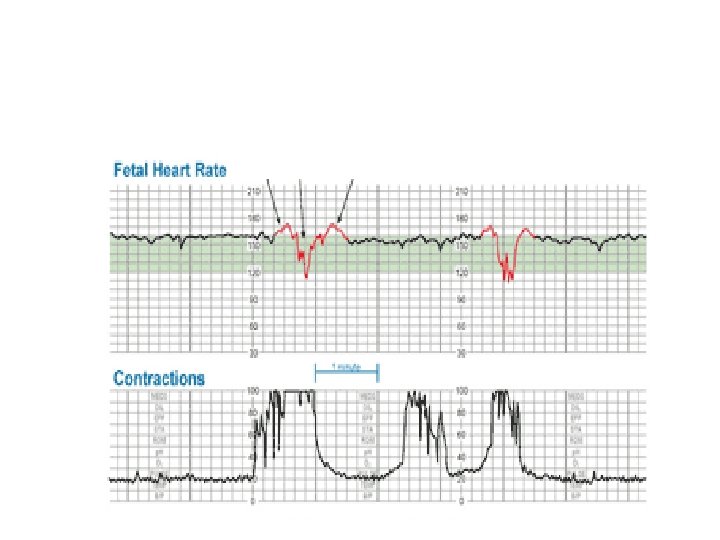
Complicated variable deceleration Indicated fetal hypoxia • Tachycardia • Lack of variability • Slow return to baseline • Large amplitude(to 60 bpm or duration 60 second) • Loss of pre and post shouldering • Smooth overshoot
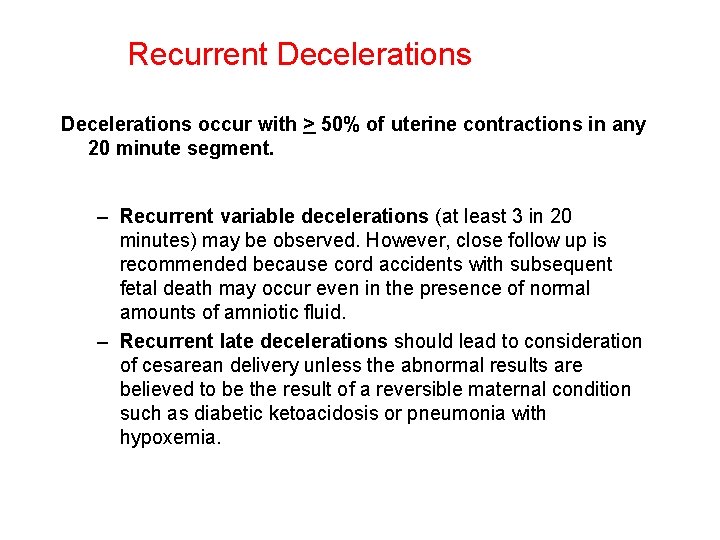
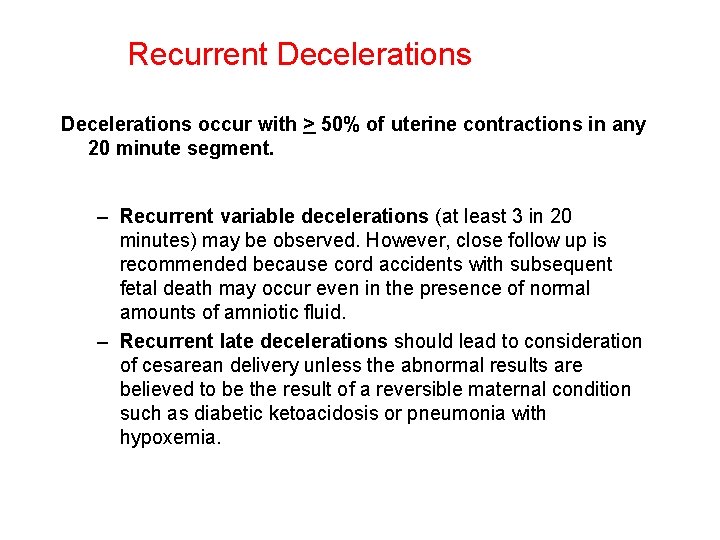
Recurrent Decelerations occur with > 50% of uterine contractions in any 20 minute segment. – Recurrent variable decelerations (at least 3 in 20 minutes) may be observed. However, close follow up is recommended because cord accidents with subsequent fetal death may occur even in the presence of normal amounts of amniotic fluid. – Recurrent late decelerations should lead to consideration of cesarean delivery unless the abnormal results are believed to be the result of a reversible maternal condition such as diabetic ketoacidosis or pneumonia with hypoxemia.
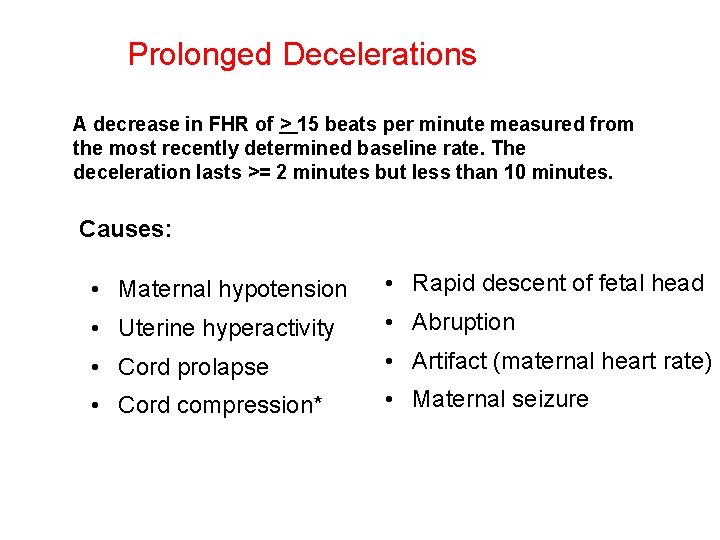
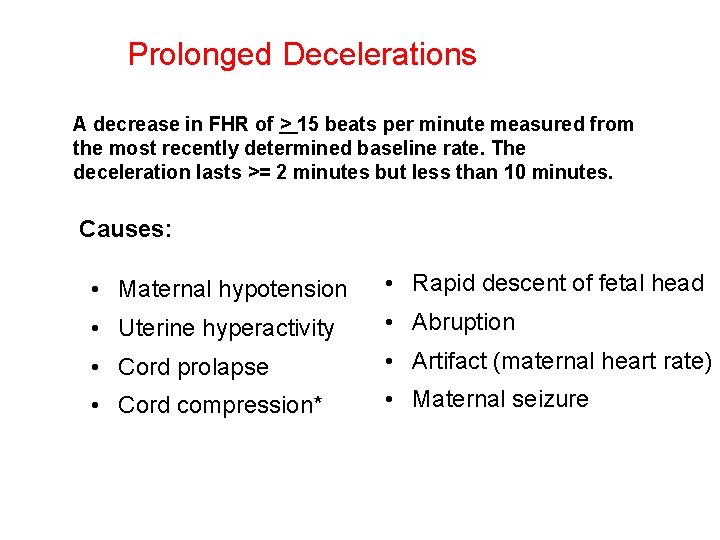
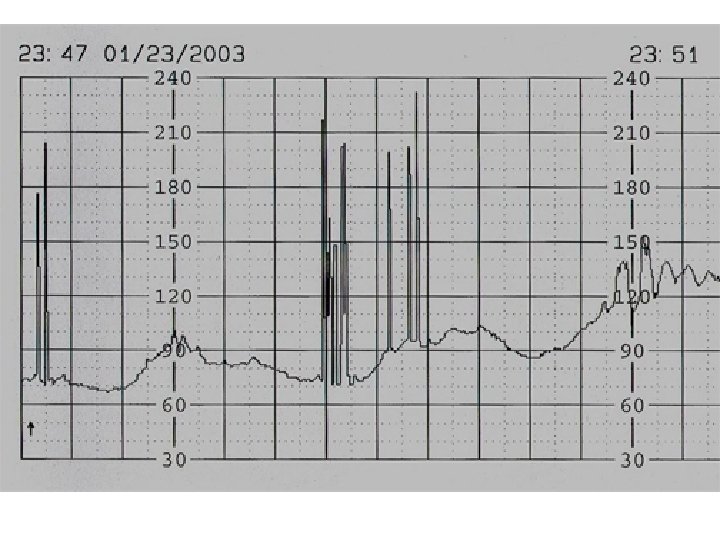
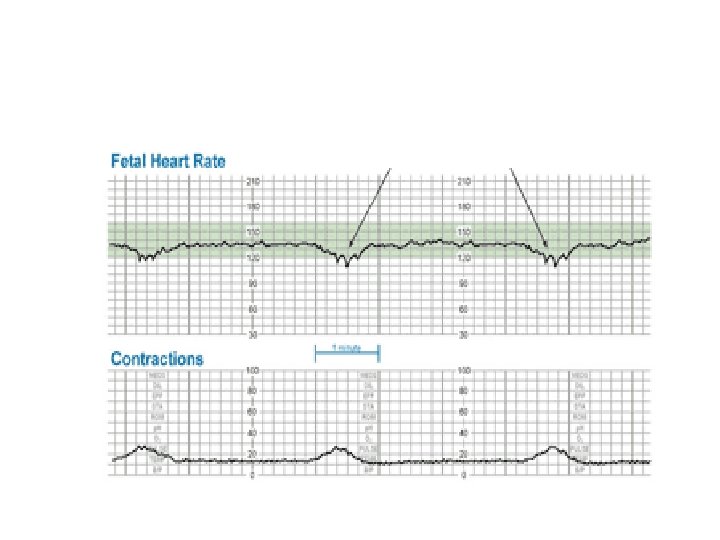
Prolonged Decelerations A decrease in FHR of > 15 beats per minute measured from the most recently determined baseline rate. The deceleration lasts >= 2 minutes but less than 10 minutes. Causes: • Maternal hypotension • Rapid descent of fetal head • Uterine hyperactivity • Abruption • Cord prolapse • Artifact (maternal heart rate) • Cord compression* • Maternal seizure
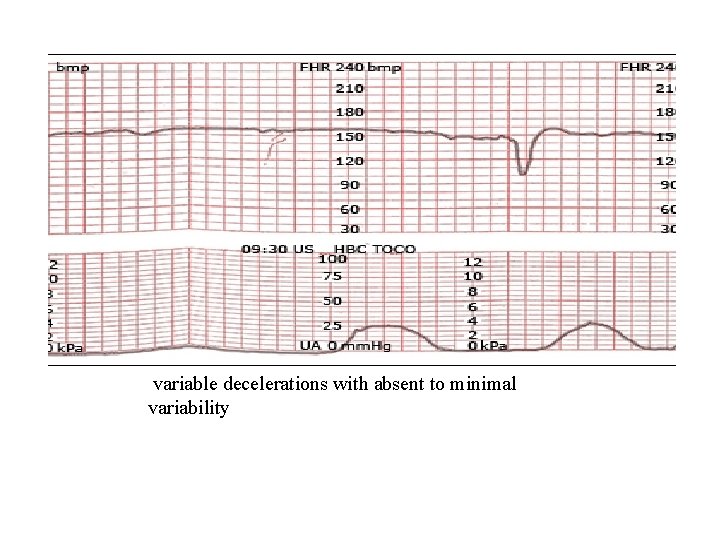
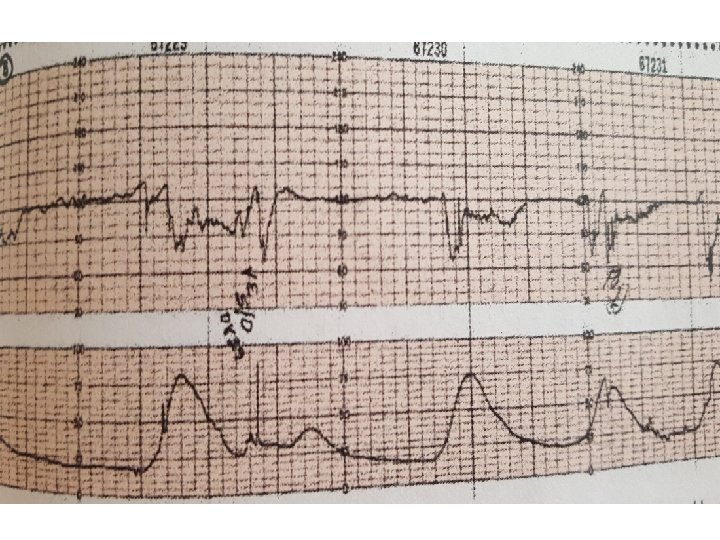
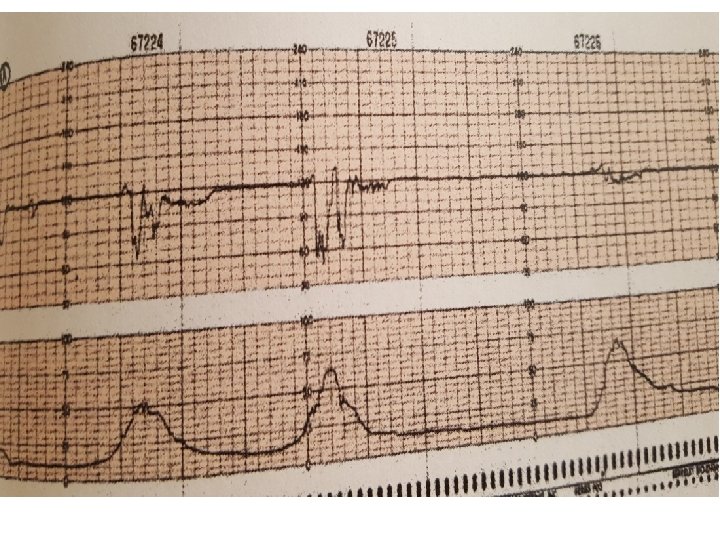
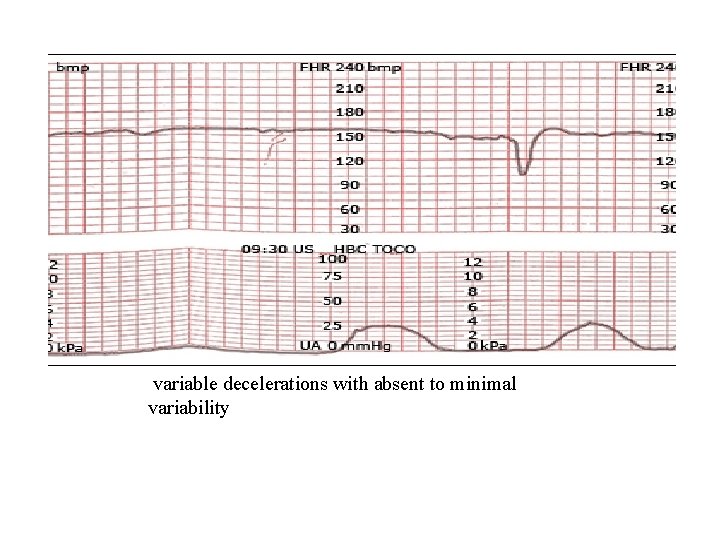
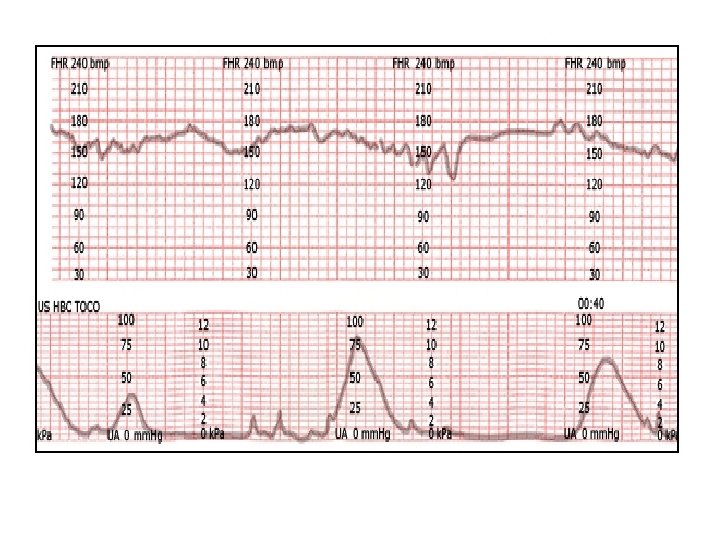
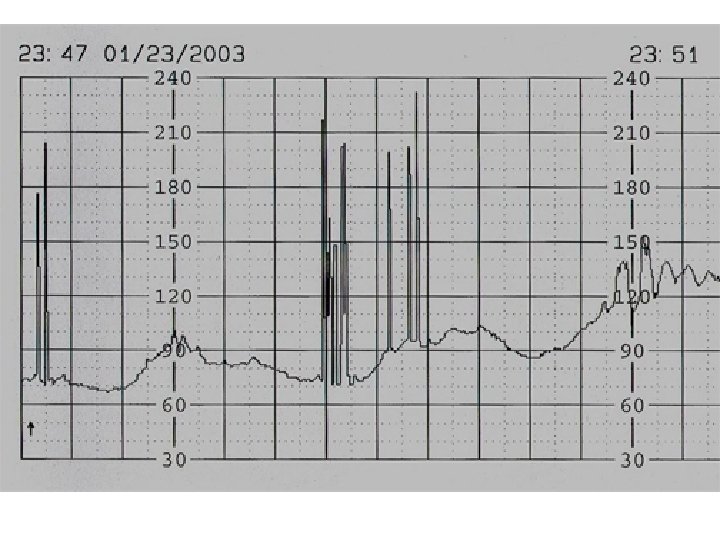
variable decelerations with absent to minimal variability
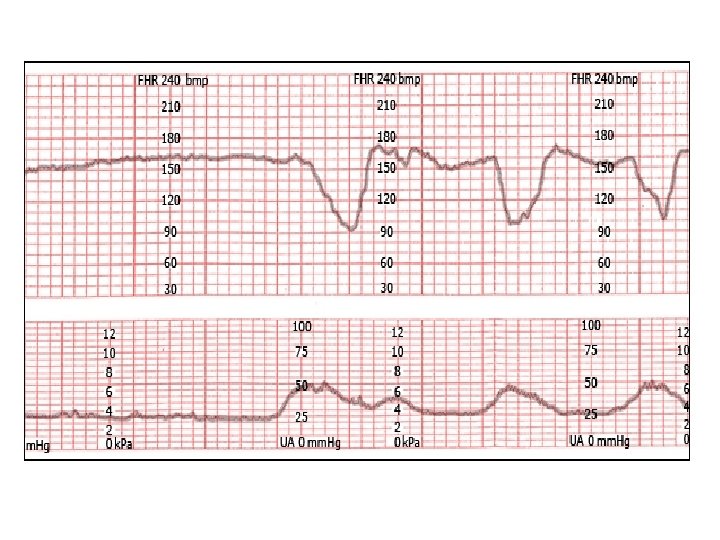
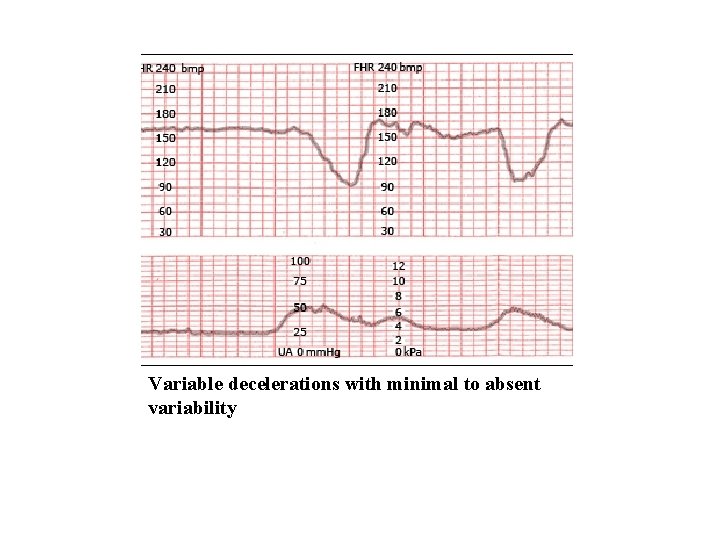
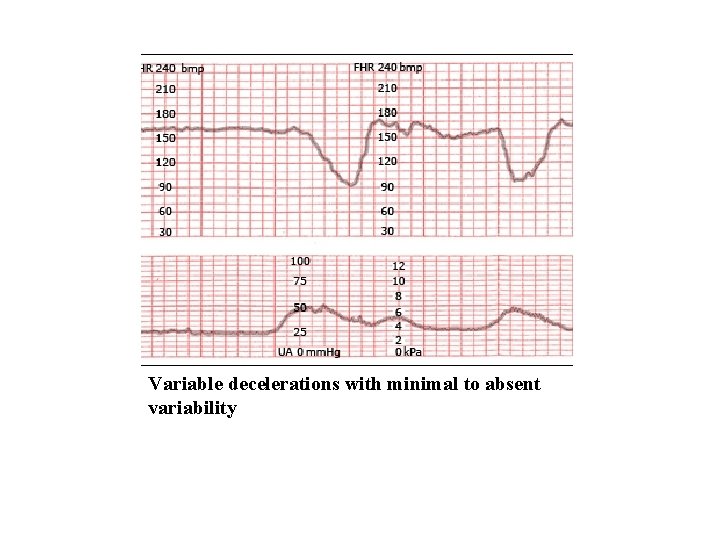
Variable decelerations with minimal to absent variability
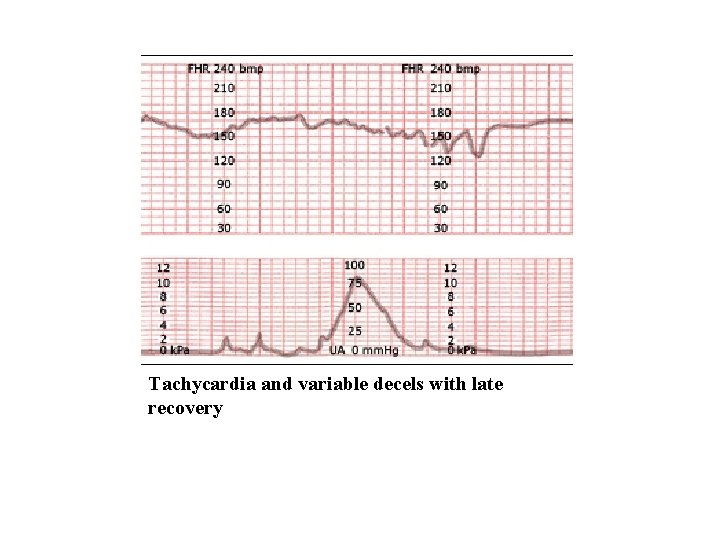
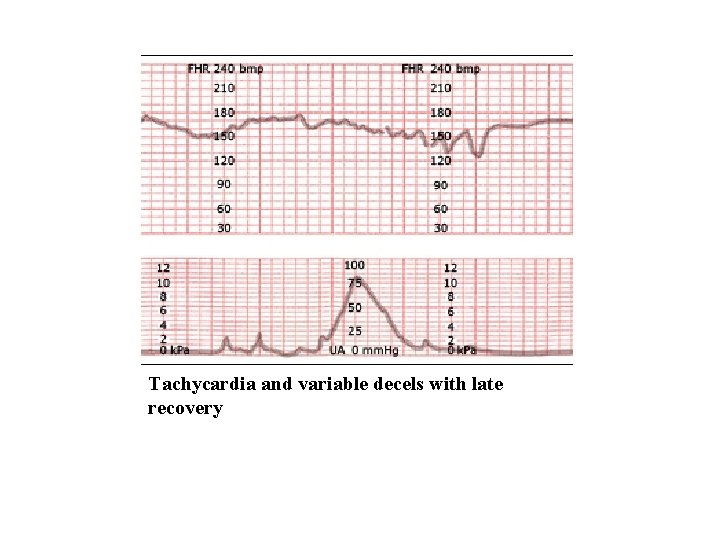
Tachycardia and variable decels with late recovery
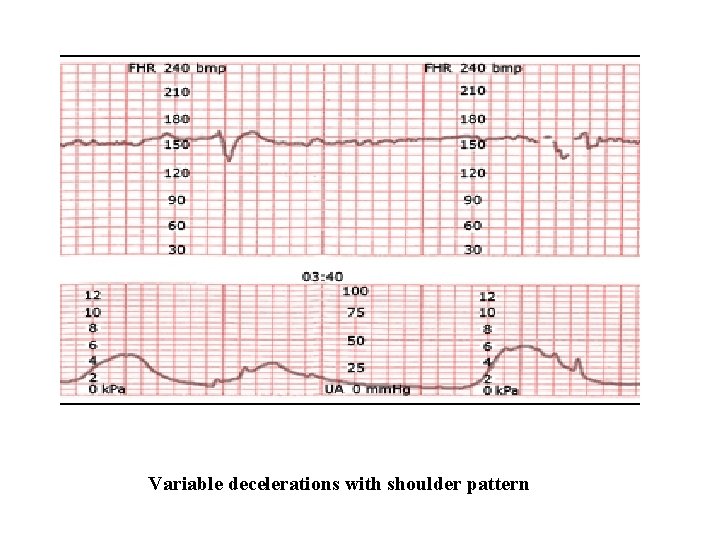
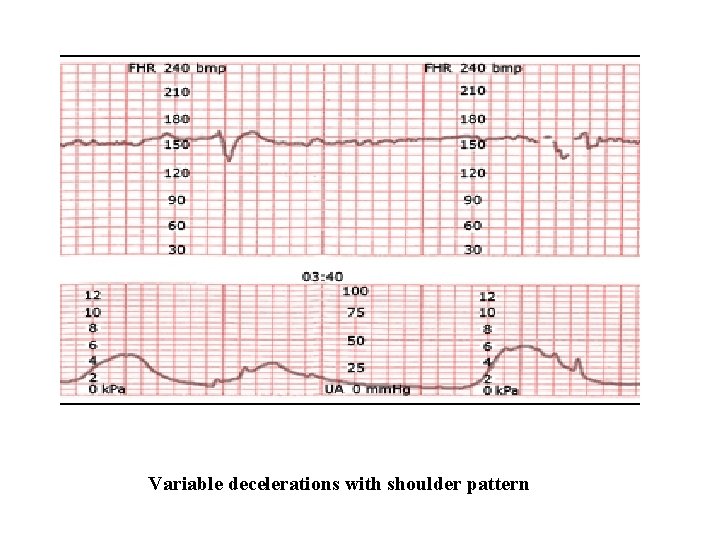
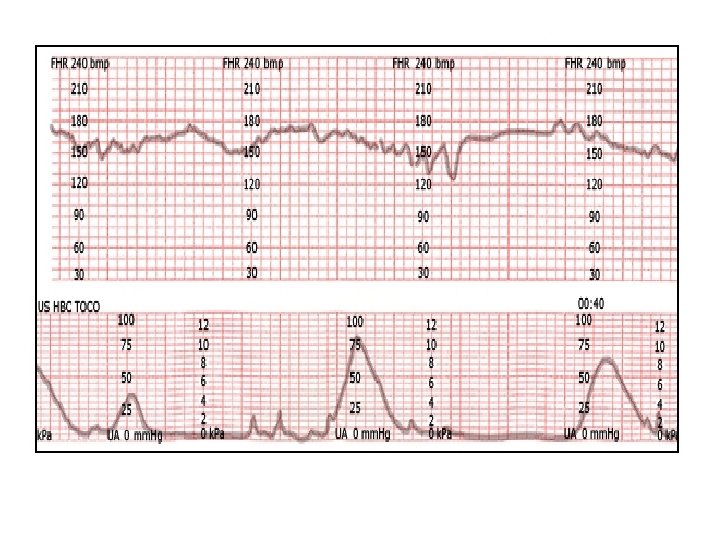
Variable decelerations with shoulder pattern
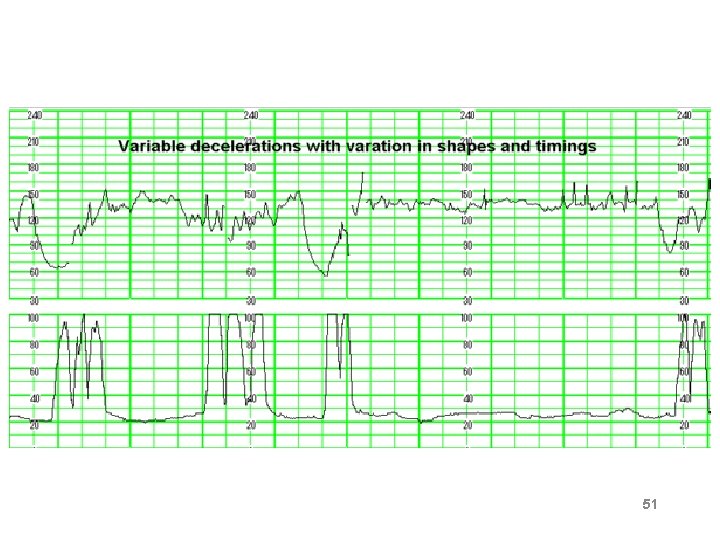
51
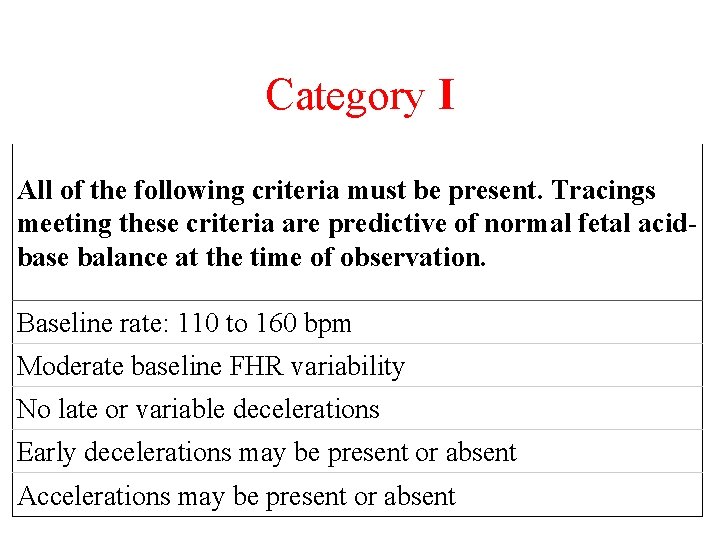
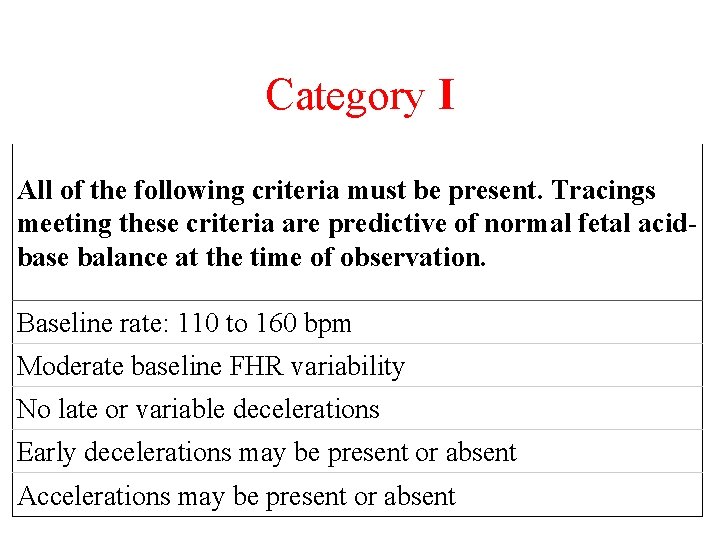
Category I All of the following criteria must be present. Tracings meeting these criteria are predictive of normal fetal acidbase balance at the time of observation. Baseline rate: 110 to 160 bpm Moderate baseline FHR variability No late or variable decelerations Early decelerations may be present or absent Accelerations may be present or absent
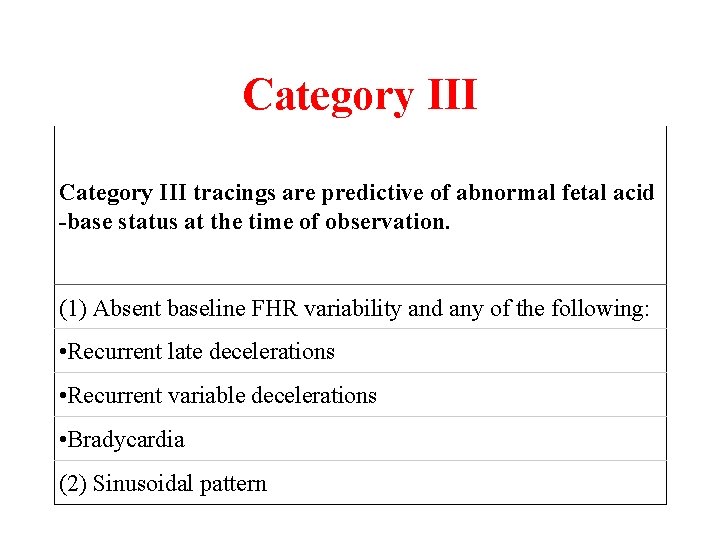
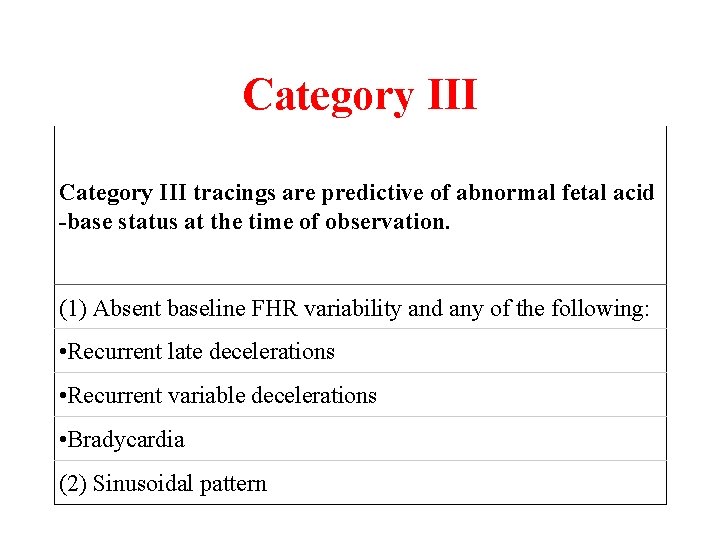
Category III tracings are predictive of abnormal fetal acid -base status at the time of observation. (1) Absent baseline FHR variability and any of the following: • Recurrent late decelerations • Recurrent variable decelerations • Bradycardia (2) Sinusoidal pattern
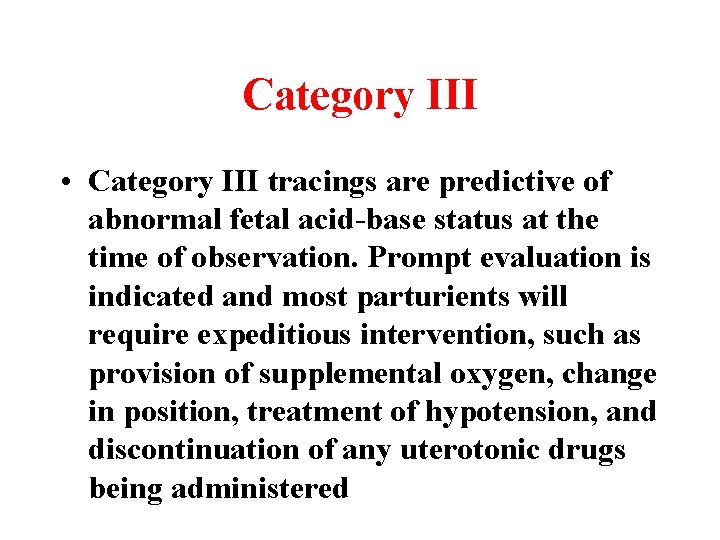
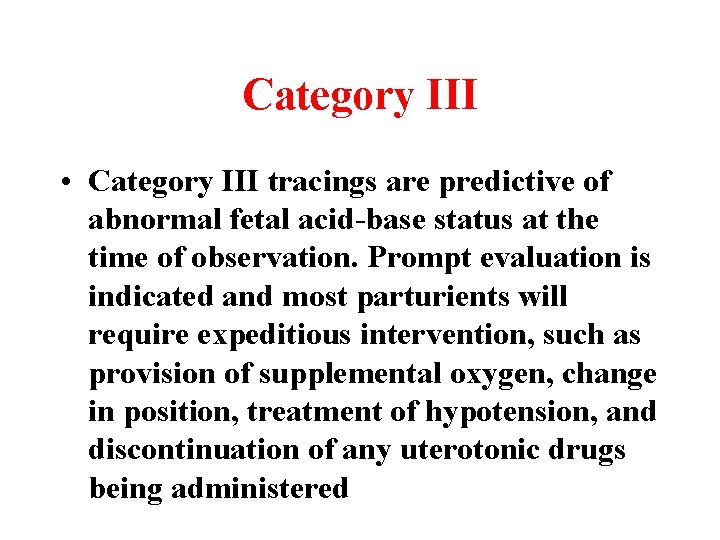
Category III • Category III tracings are predictive of abnormal fetal acid-base status at the time of observation. Prompt evaluation is indicated and most parturients will require expeditious intervention, such as provision of supplemental oxygen, change in position, treatment of hypotension, and discontinuation of any uterotonic drugs being administered
Category II • FHR tracing does not meet criteria for either category I or III and is considered indeterminate.
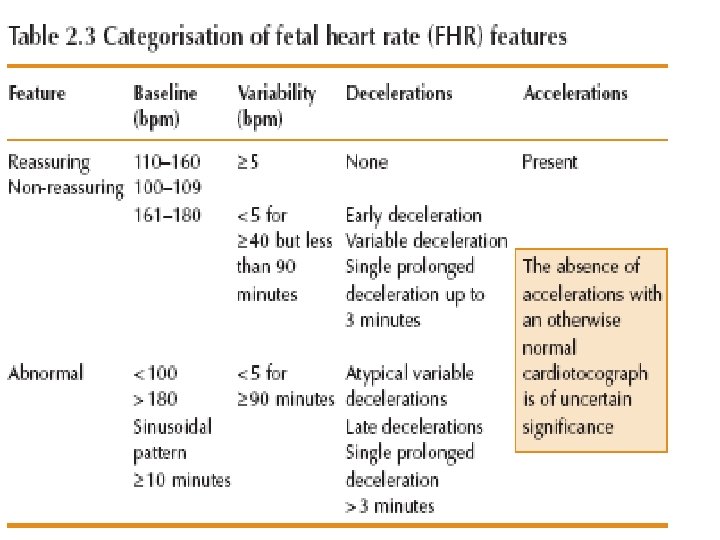
Cardio. Toco. Graphy • Normal • Suspicious • pathological
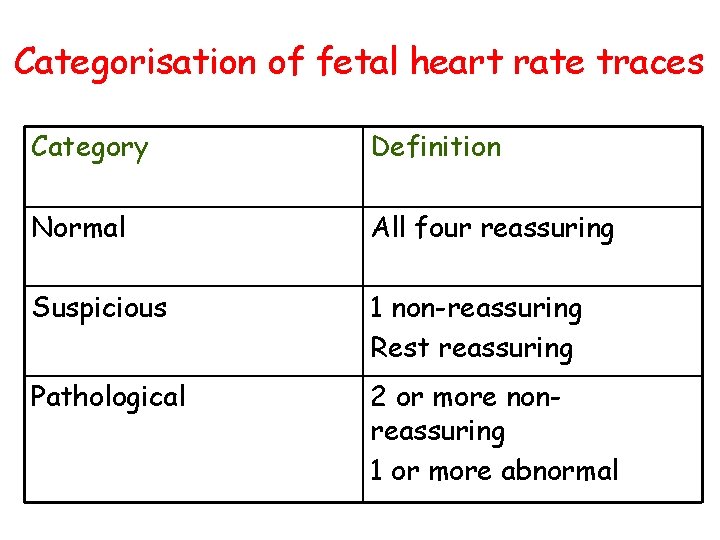
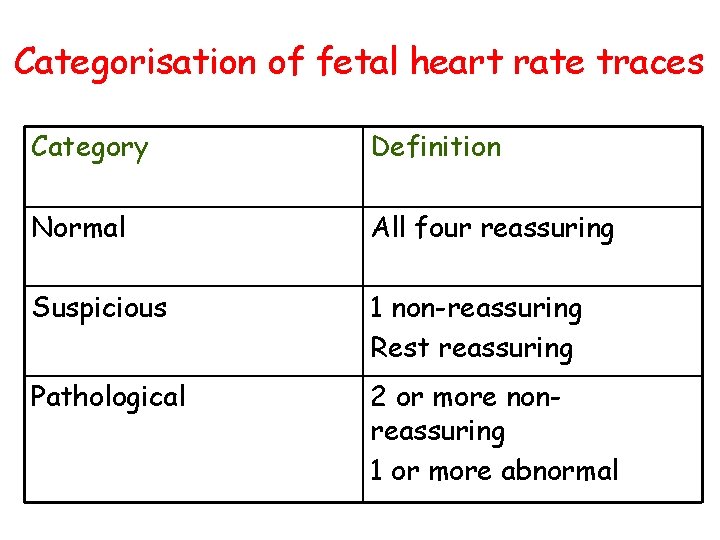
Categorisation of fetal heart rate traces Category Definition Normal All four reassuring Suspicious 1 non-reassuring Rest reassuring Pathological 2 or more nonreassuring 1 or more abnormal
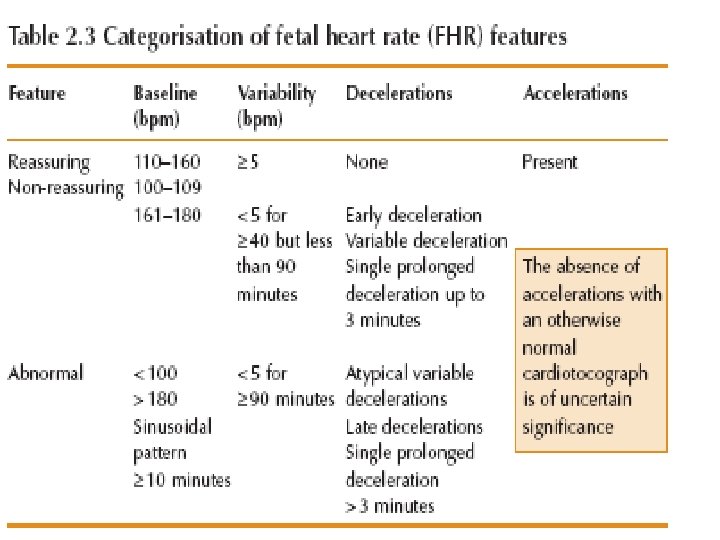
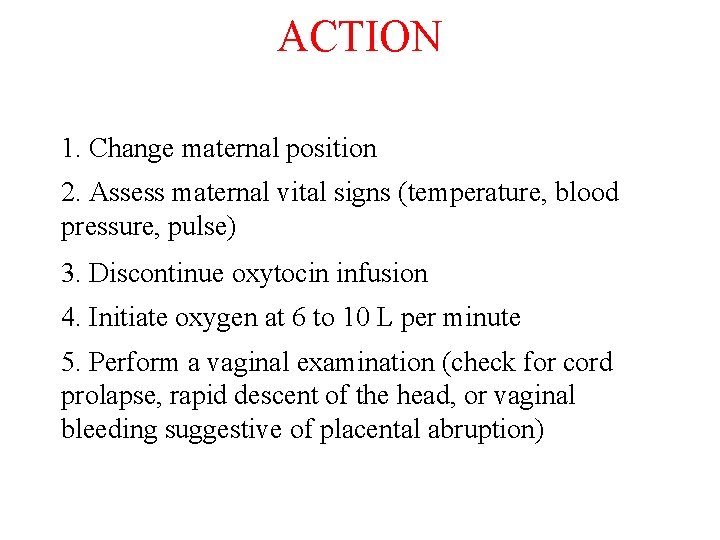
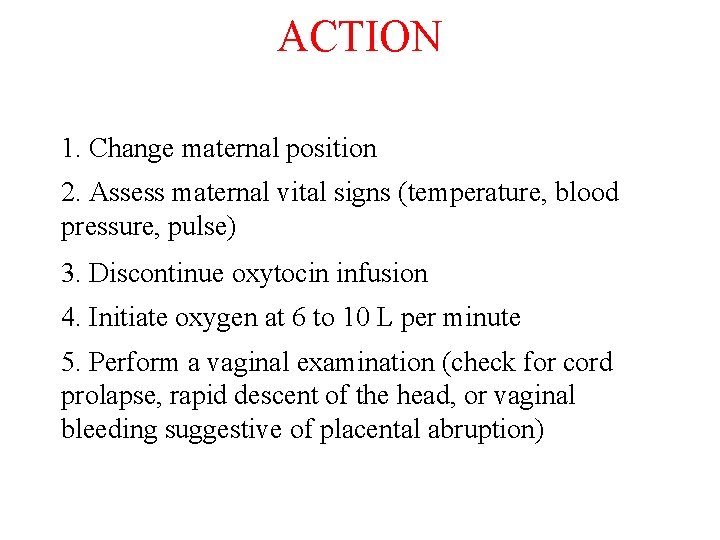
ACTION 1. Change maternal position 2. Assess maternal vital signs (temperature, blood pressure, pulse) 3. Discontinue oxytocin infusion 4. Initiate oxygen at 6 to 10 L per minute 5. Perform a vaginal examination (check for cord prolapse, rapid descent of the head, or vaginal bleeding suggestive of placental abruption)
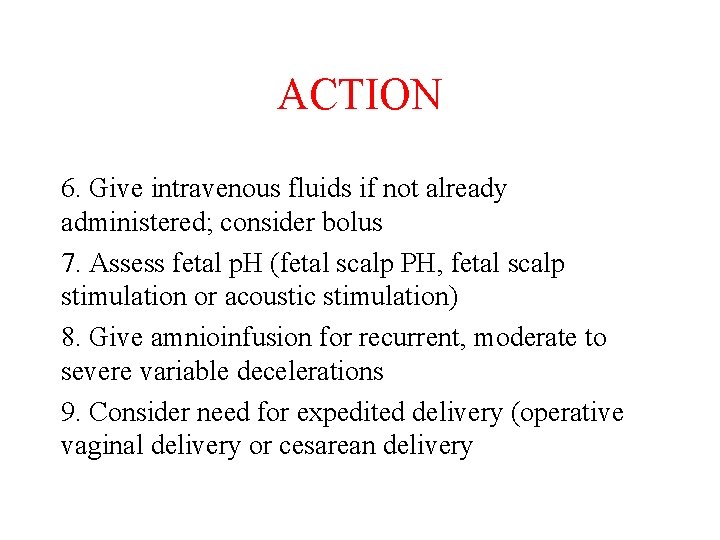
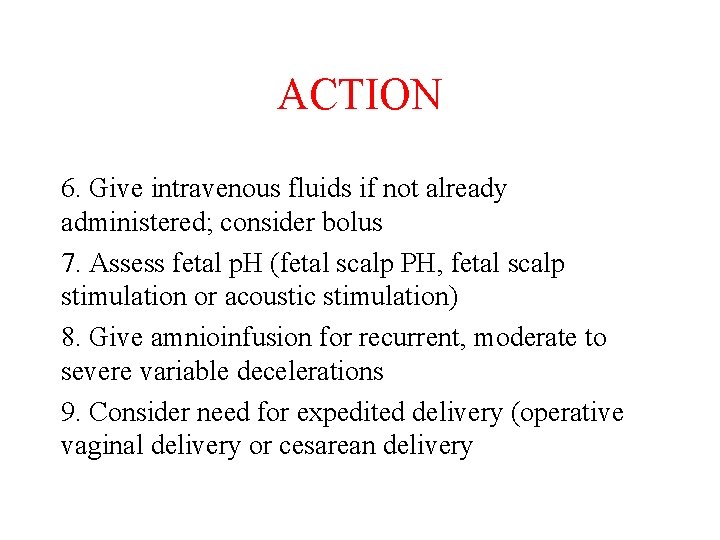
ACTION 6. Give intravenous fluids if not already administered; consider bolus 7. Assess fetal p. H (fetal scalp PH, fetal scalp stimulation or acoustic stimulation) 8. Give amnioinfusion for recurrent, moderate to severe variable decelerations 9. Consider need for expedited delivery (operative vaginal delivery or cesarean delivery
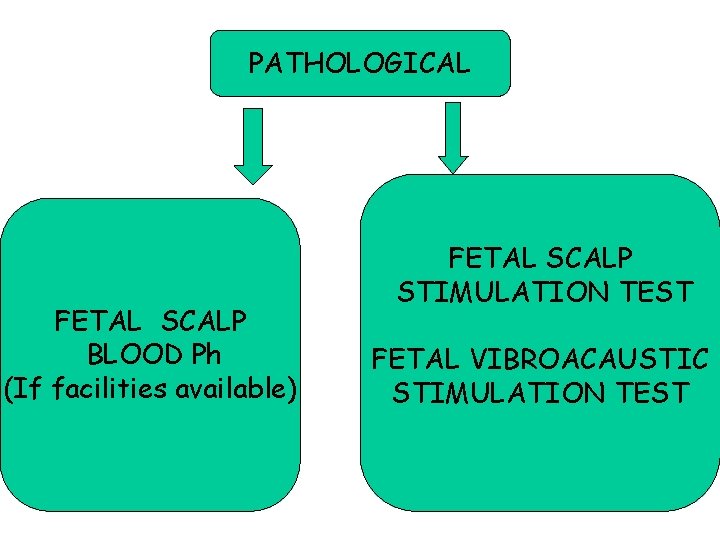
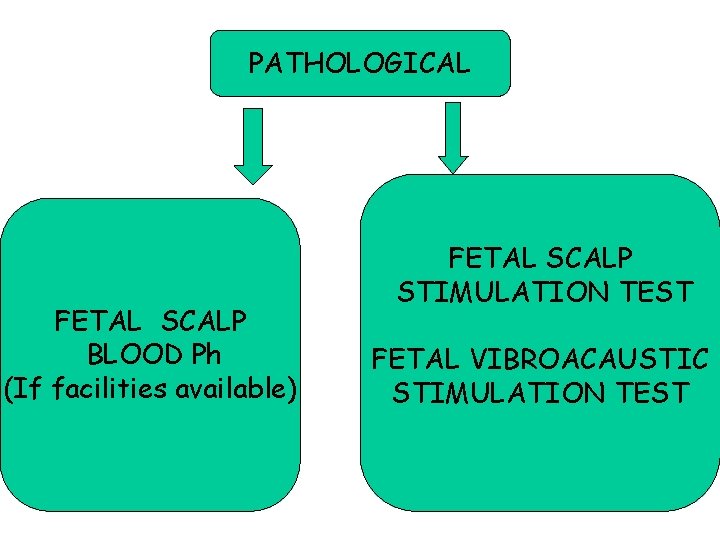
PATHOLOGICAL FETAL SCALP BLOOD Ph (If facilities available) FETAL SCALP STIMULATION TEST FETAL VIBROACAUSTIC STIMULATION TEST 65
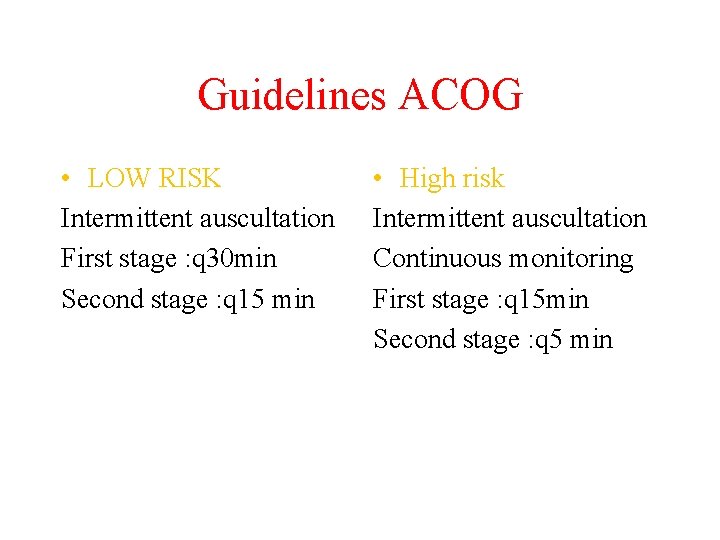
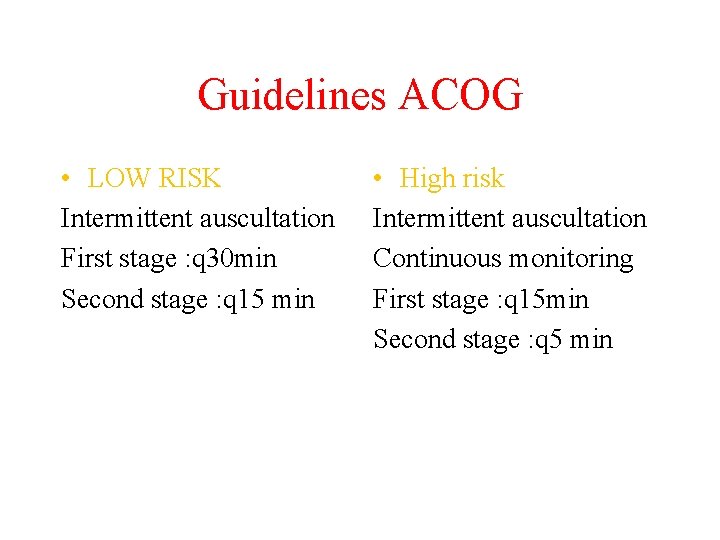
Guidelines ACOG • LOW RISK Intermittent auscultation First stage : q 30 min Second stage : q 15 min • High risk Intermittent auscultation Continuous monitoring First stage : q 15 min Second stage : q 5 min
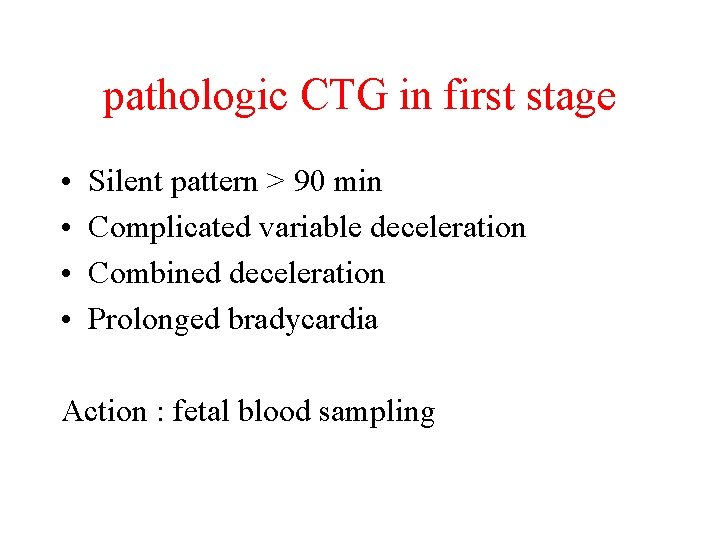
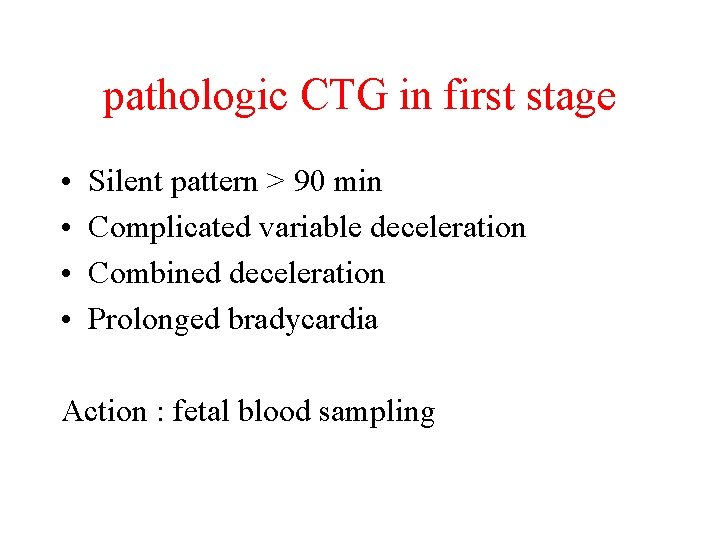
pathologic CTG in first stage • • Silent pattern > 90 min Complicated variable deceleration Combined deceleration Prolonged bradycardia Action : fetal blood sampling
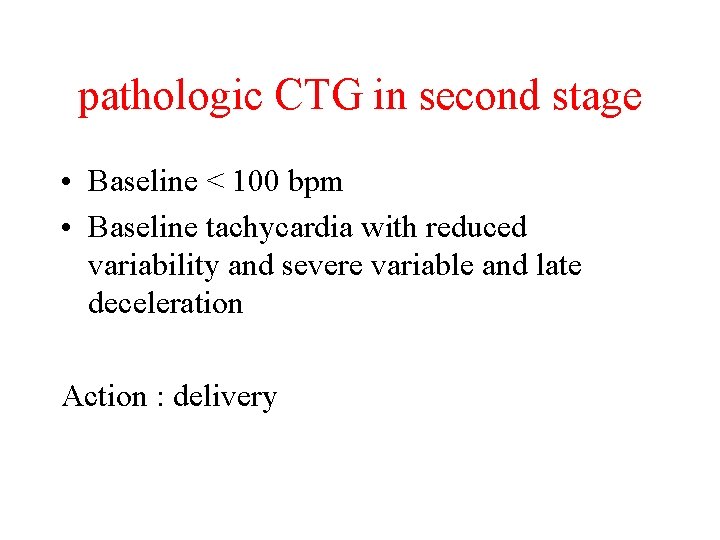
pathologic CTG in second stage • Baseline < 100 bpm • Baseline tachycardia with reduced variability and severe variable and late deceleration Action : delivery
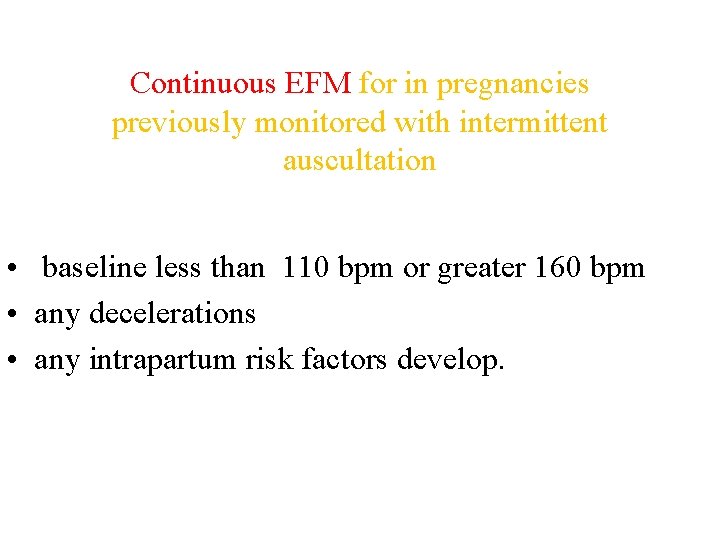
Continuous EFM for in pregnancies previously monitored with intermittent auscultation • baseline less than 110 bpm or greater 160 bpm • any decelerations • any intrapartum risk factors develop.
conditions not forgot • Meconium • Infection • abruption
RECORD KEEPING IN CTG • check date and time clocks on the EFM. (how reliable is the clock in the labor? ) • Lable FHR traces with mother’s name, date and hospital number. • Sign trace & record date , time and mode of birth. • Note any intrapartum events (e. g. vaginal examination, fetal blood sample, siting of an epidural). • Store trace securely.
Risk management • Consider the time taken for instrument vaginal birth and C/S. • Keep FHR traces for 25 years. • If the baby may suffer developmental delay , photocopy and store FHR traces indefinitely. • Don’t forget ABG.
• Absent acceleration in category I: rare acidosis. • Absent acceleration in category II : acidosis.
• Fetal blood sampling • Acceleration • variability
How long wait for recovery ? Determinate by • depth of deceleration • loss of variability during deceleration • heart rate returning toward baseline • evidence hypoxia preceded deceleration
• Asphyxiation for 7 -12 min resulted in transient motor and behavioral changes.
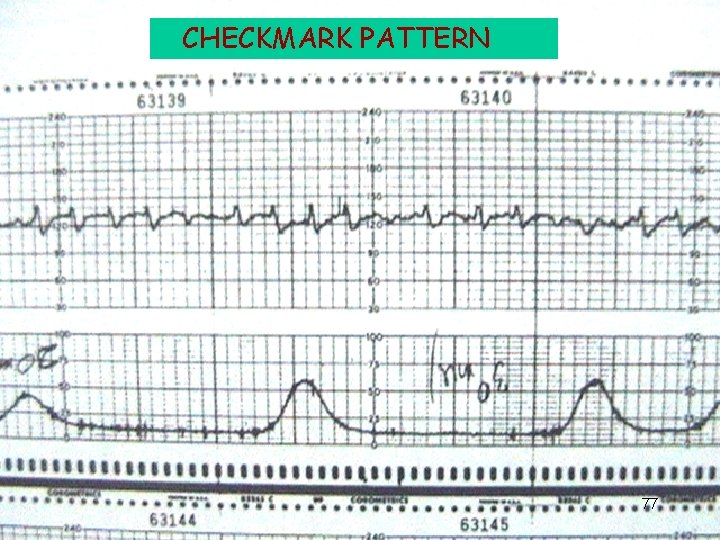
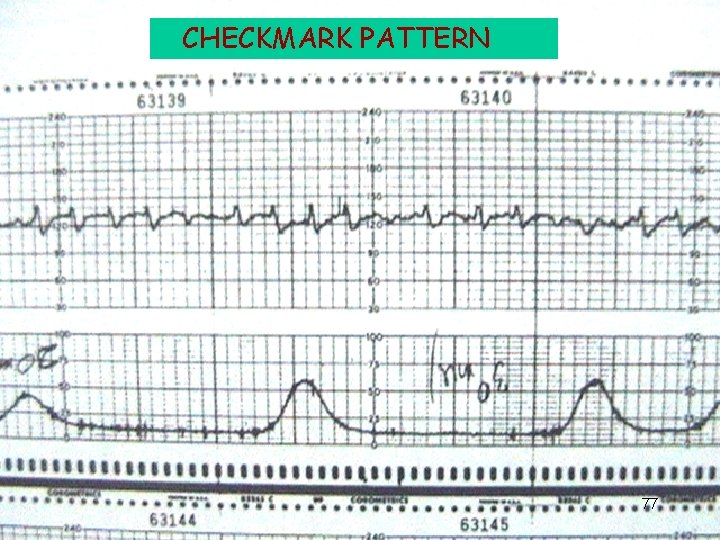
CHECKMARK PATTERN 77
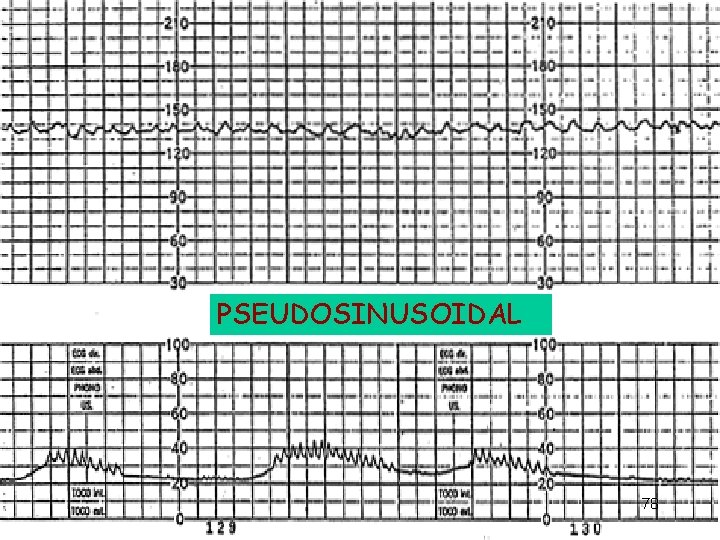
PSEUDOSINUSOIDAL 78
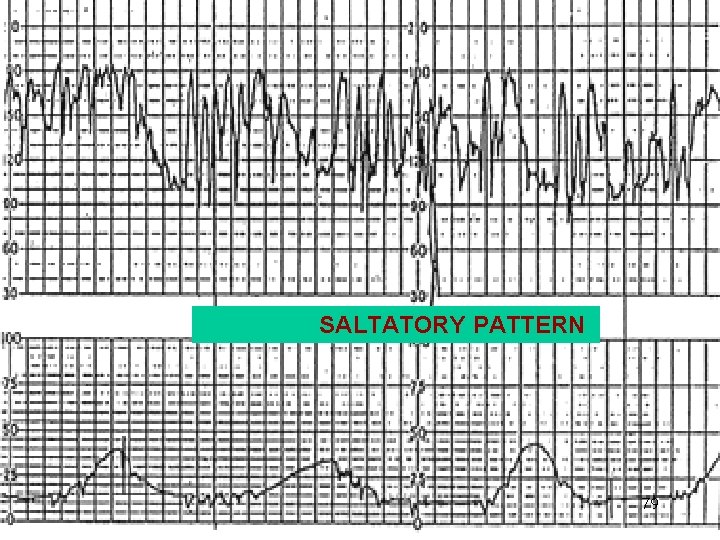
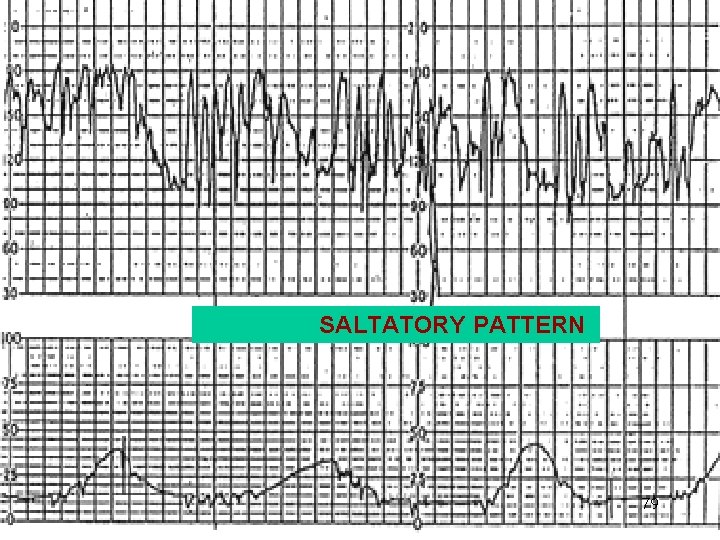
SALTATORY PATTERN 79
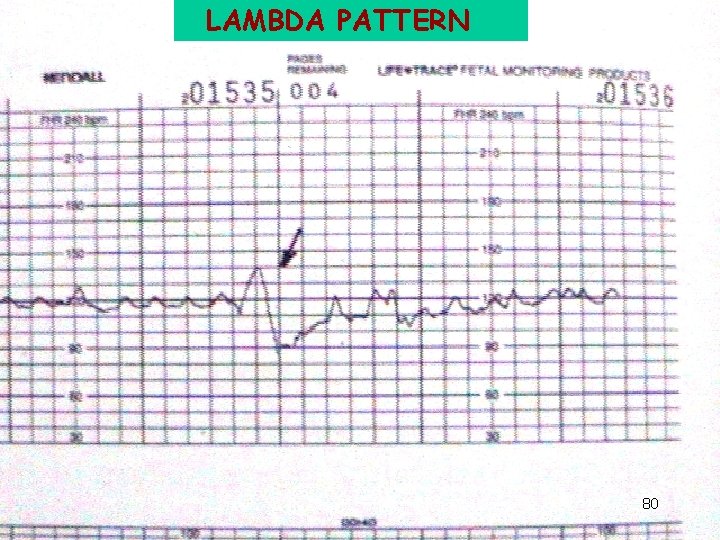
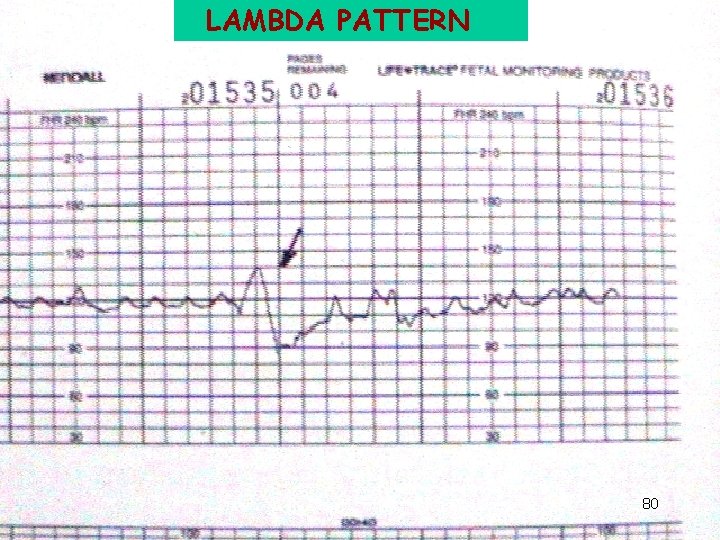
LAMBDA PATTERN 80
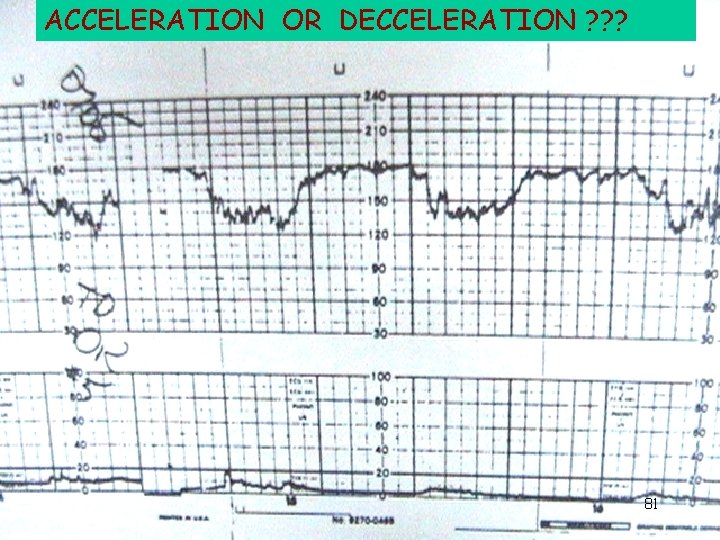
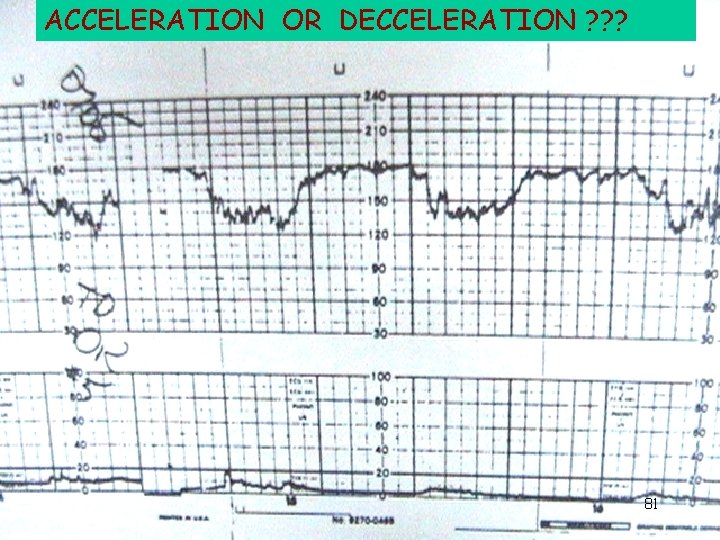
ACCELERATION OR DECCELERATION ? ? ? 81
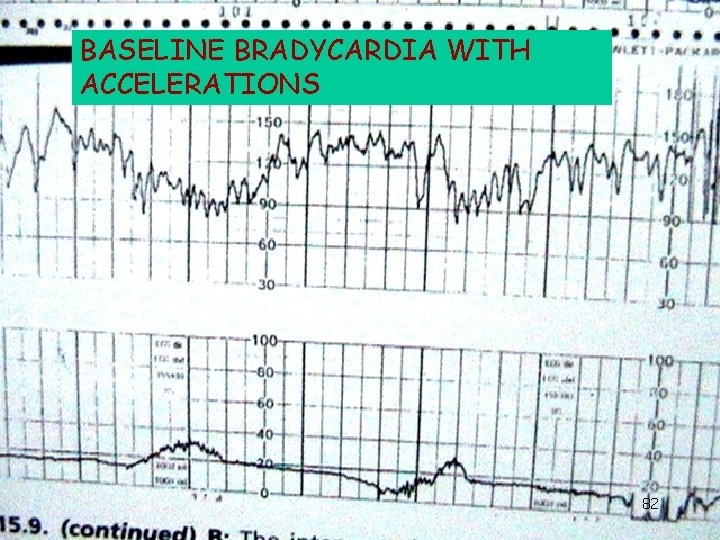
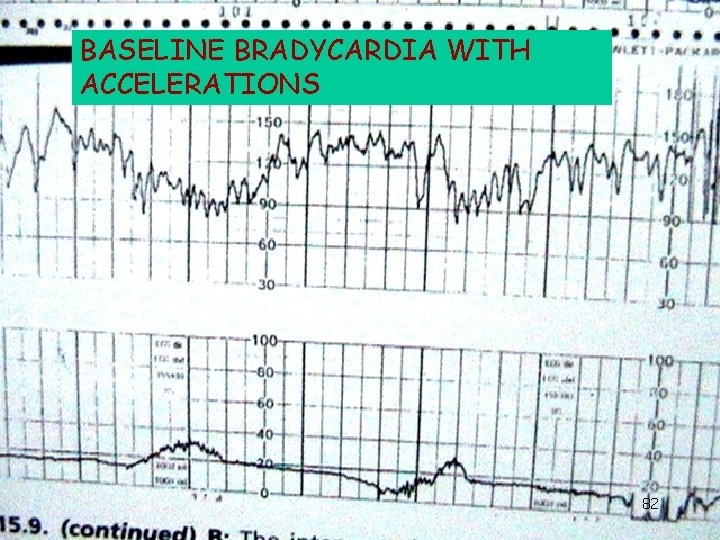
BASELINE BRADYCARDIA WITH ACCELERATIONS 82
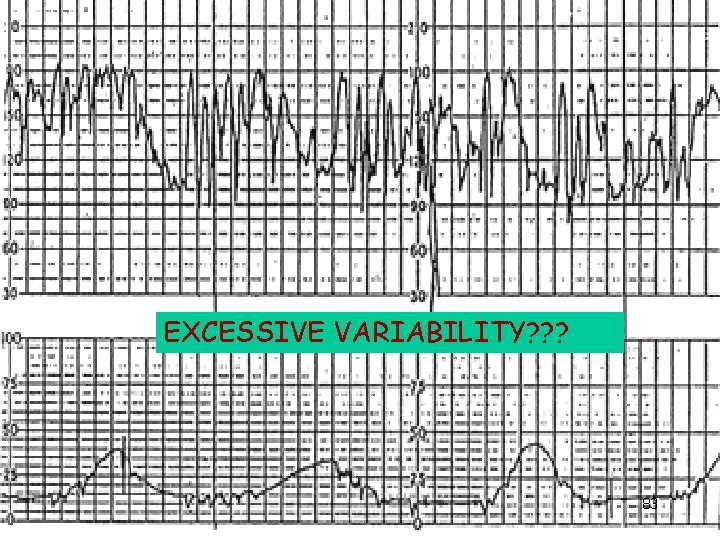
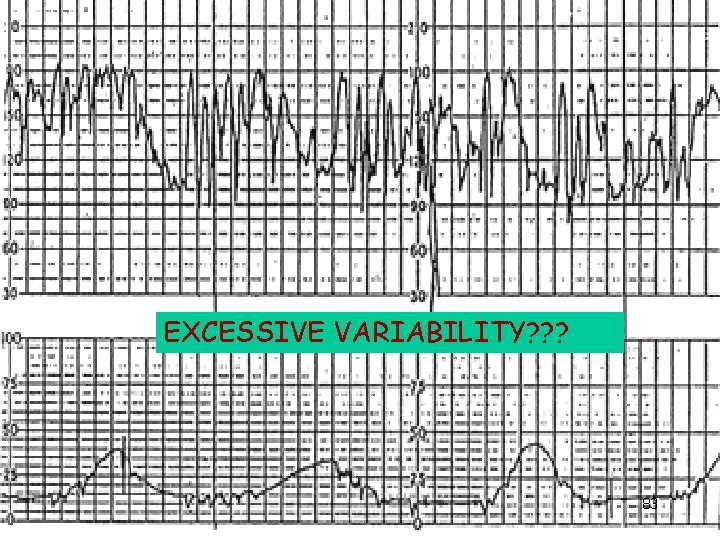
EXCESSIVE VARIABILITY? ? ? 83
 Wandering fetal heart rate baseline
Wandering fetal heart rate baseline Intrapartum meaning
Intrapartum meaning Intrapartum meaning
Intrapartum meaning Antenatal intrapartum and postnatal
Antenatal intrapartum and postnatal Advanced fetal monitoring test answers
Advanced fetal monitoring test answers Ctg dr c bravado
Ctg dr c bravado Nichd fetal monitoring
Nichd fetal monitoring Importance of types of claims
Importance of types of claims Pour toute suggestion
Pour toute suggestion Scopus title suggestion
Scopus title suggestion Perfect modals ejemplos
Perfect modals ejemplos What is the purpose of giving suggestion
What is the purpose of giving suggestion Conversation giving advice
Conversation giving advice Social function asking and giving opinion
Social function asking and giving opinion Direct speech.
Direct speech. Business english conversation
Business english conversation Suggestion and offering
Suggestion and offering Teaching syllable rules
Teaching syllable rules Desuggestopedia and suggestopedia
Desuggestopedia and suggestopedia Meetplan lean
Meetplan lean Efisiensi pompa
Efisiensi pompa Decision making unit example
Decision making unit example Wckcs
Wckcs How to monitor and improve workplace operations
How to monitor and improve workplace operations How did john smith improve conditions in jamestown
How did john smith improve conditions in jamestown How to improve current ratio
How to improve current ratio Oral fixation personality
Oral fixation personality Gearing investopedia
Gearing investopedia Asset management cmdb
Asset management cmdb Chosen synoynm
Chosen synoynm Action plan to improve listening skills
Action plan to improve listening skills Terminal server performance tuning
Terminal server performance tuning Improving sentences
Improving sentences If you can’t measure it, you can’t manage it
If you can’t measure it, you can’t manage it If you don't measure it it doesn't exist
If you don't measure it it doesn't exist Improve memory latency
Improve memory latency Cash flow options
Cash flow options The universe is sacred you cannot improve it
The universe is sacred you cannot improve it What did spallanzani do to improve upon redi's
What did spallanzani do to improve upon redi's How to improve yourself spiritually
How to improve yourself spiritually Rerandomization to improve covariate balance in experiments
Rerandomization to improve covariate balance in experiments Fm 6 22
Fm 6 22 Can far memory improve job throughput
Can far memory improve job throughput Suffix of educate
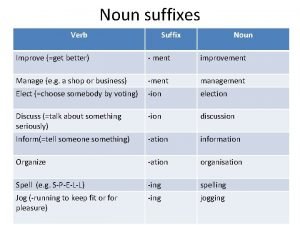
Suffix of educate Government can sometimes improve market outcomes
Government can sometimes improve market outcomes Open source assessment
Open source assessment Difference between spirituality and religion
Difference between spirituality and religion Kiss method keep improve start stop
Kiss method keep improve start stop Die 3. hali
Die 3. hali We improve lives
We improve lives 15 intrapersonal skills
15 intrapersonal skills How to improve organisational performance
How to improve organisational performance Improve resolution of image online
Improve resolution of image online Accurate cutting facilitates sewing and improve garment
Accurate cutting facilitates sewing and improve garment Lodi unified school district board meeting live
Lodi unified school district board meeting live How did the panama canal help improve trade
How did the panama canal help improve trade How did the hongwu emperor improve life for the peasants?
How did the hongwu emperor improve life for the peasants? Image restoration is to improve the dash of the image
Image restoration is to improve the dash of the image Noun suffixes advertise
Noun suffixes advertise Escore de improve
Escore de improve Lactate inflection point graph
Lactate inflection point graph Contoh aktiviti pembangunan profesionalisme berterusan
Contoh aktiviti pembangunan profesionalisme berterusan Improve software economics
Improve software economics To improve america's business ethics:
To improve america's business ethics: Protect, promote, and improve the health of all people
Protect, promote, and improve the health of all people Ways to improve urban infrastructure
Ways to improve urban infrastructure Settings for a story
Settings for a story How to improve cash flow gcse business
How to improve cash flow gcse business Improve website usability
Improve website usability Badminton drills
Badminton drills Joining together as a team to improve the quality
Joining together as a team to improve the quality If you cant measure it you can't manage it
If you cant measure it you can't manage it How to improve psychomotor skills
How to improve psychomotor skills Mesenterio ventral y dorsal
Mesenterio ventral y dorsal Fetal alcohol syndrome face
Fetal alcohol syndrome face Kleihauer betke test
Kleihauer betke test Occipito iliaco izquierdo anterior
Occipito iliaco izquierdo anterior Folhetos embrionarios
Folhetos embrionarios Smallest anteroposterior diameter of the pelvic inlet
Smallest anteroposterior diameter of the pelvic inlet Prenatal development
Prenatal development Fetal hemoglobin
Fetal hemoglobin Ominous periodic change in the fetal heart rate
Ominous periodic change in the fetal heart rate Lipolise
Lipolise Engatillamiento fetal
Engatillamiento fetal