MultiAgency Perinatal and Infant Mental Health Awareness Training








- Slides: 63
Multi-Agency Perinatal and Infant Mental Health Awareness Training This presentation has been provided for the sole use of the Champion who received direct Champions training from the i. HV, for the purpose of providing cascade training to their colleagues. The slideset remains the intellectual property of the i. HV and its use in activities leading to commercial gain either by the Champion or others is therefore not permitted. The slides should not be amended without permission of the i. HV and are considered accurate at the point of production in March 2020. ©Institute of Health Visiting
Welcome & Housekeeping Fire Alarms & Exit Photos Toilets Engagement Mobiles Breaks Tweeting @i. Health. Visiting #i. HVPIMHChampion © Institute of Health Visiting 2020
What is the i. HV? The Institute of Health Visiting is a charity and centre of excellence for practice The i. HV’s charitable objectives are to improve outcomes for children and families and reduce health inequalities Much in common with a royal college in terms of philosophy © Institute of Health Visiting 2020
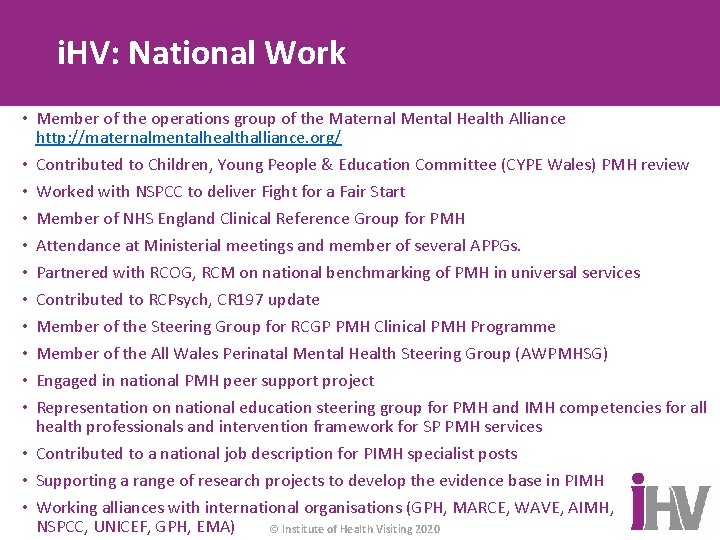
i. HV: National Work • Member of the operations group of the Maternal Mental Health Alliance http: //maternalmentalhealthalliance. org/ • Contributed to Children, Young People & Education Committee (CYPE Wales) PMH review • Worked with NSPCC to deliver Fight for a Fair Start • Member of NHS England Clinical Reference Group for PMH • Attendance at Ministerial meetings and member of several APPGs. • Partnered with RCOG, RCM on national benchmarking of PMH in universal services • Contributed to RCPsych, CR 197 update • Member of the Steering Group for RCGP PMH Clinical PMH Programme • Member of the All Wales Perinatal Mental Health Steering Group (AWPMHSG) • Engaged in national PMH peer support project • Representation on national education steering group for PMH and IMH competencies for all health professionals and intervention framework for SP PMH services • Contributed to a national job description for PIMH specialist posts • Supporting a range of research projects to develop the evidence base in PIMH • Working alliances with international organisations (GPH, MARCE, WAVE, AIMH, NSPCC, UNICEF, GPH, EMA) © Institute of Health Visiting 2020
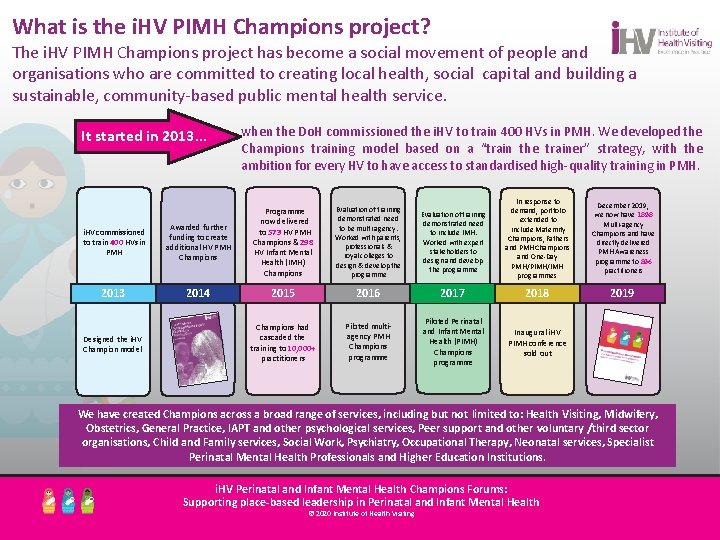
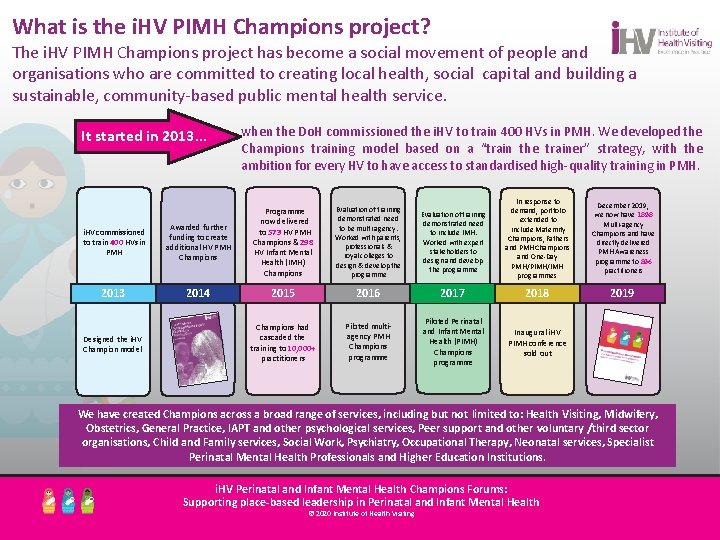
What is the i. HV PIMH Champions project? The i. HV PIMH Champions project has become a social movement of people and organisations who are committed to creating local health, social capital and building a sustainable, community-based public mental health service. It started in 2013. . . when the Do. H commissioned the i. HV to train 400 HVs in PMH. We developed the Champions training model based on a “train the trainer” strategy, with the ambition for every HV to have access to standardised high-quality training in PMH. Evaluation of training demonstrated need to be multi-agency. Worked with parents, professionals & royal colleges to design & develop the programme Evaluation of training demonstrated need to include IMH. Worked with expert stakeholders to design and develop the programme In response to demand, portfolio extended to include Maternity Champions, Fathers and PMH Champions and One-Day PMH/PIMH/IMH programmes December 2019, we now have 1898 Multi-agency Champions and have directly delivered PMH Awareness programme to 896 practitioners 2019 i. HV commissioned to train 400 HVs in PMH Awarded further funding to create additional HV PMH Champions Programme now delivered to 573 HV PMH Champions & 298 HV Infant Mental Health (IMH) Champions 2013 2014 2015 2016 2017 2018 Champions had cascaded the training to 10, 000+ practitioners Piloted multiagency PMH Champions programme Piloted Perinatal and Infant Mental Health (PIMH) Champions programme Inaugural i. HV PIMH conference sold out Designed the i. HV Champion model We have created Champions across a broad range of services, including but not limited to: Health Visiting, Midwifery, Obstetrics, General Practice, IAPT and other psychological services, Peer support and other voluntary /third sector organisations, Child and Family services, Social Work, Psychiatry, Occupational Therapy, Neonatal services, Specialist Perinatal Mental Health Professionals and Higher Education Institutions. i. HV Perinatal and Infant Mental Health Champions Forums: Supporting place-based leadership in Perinatal and Infant Mental Health © 2020 Institute of Health Visiting © Institute of Health Visiting 2020
The Role of an Institute of Health Visiting Perinatal and Infant Mental Health Champion As a Champion you will be an ambassador for perinatal and infant mental health within “A Champion is role someone wholeheartedly your local area, taking an active in leading these very important agendas through: • cascading the training to your colleagues: increasing awareness and knowledge of embraces a cause (PIMH) goes above and beyond to perinatal and infant mental health within teams, enabling them to signpost effectively to the rightdefend service at theand right timesupport that cause with passion, fight, • ensuring families who are experts by experience are partners in the planning and shaping energy, enthusiasm and tenacity. Driving forward of local services • beingforcing the voice of organisational the child and changes even when there • making certain that services are inclusive and developed to meet the needs of its is population resistance (oftowhich I have encountered plenty in with respect diversity, equality and equity • improving access to services for those affected by or at risk of perinatal and infant mental my time). At least that’s my experience of being a illness • progressing local-integrated perinatal and infant mental Ihealth pathways. PIMH to Champion at every opportunity talkcareabout • empowering colleagues to raise parity of esteem for perinatal and infant mental health everyone I meet, whether they are professional or • promoting evidenced based information at all levels not. Being ancapacity i. HVthrough Champion makes you feel that • building community working in partnership with local citizens • dispelling myths and proactively working to challenge and reduce stigma urging the cause is essential”. © Institute of Health Visiting 2020

i. HV Champions: A social movement September 2018 Awarded 1 st Place for best Perinatal Education Programme by International Marce Society http: //www. marce 2018. com/swan. php © Institute of Health Visiting 2020

Aim: Day One By the end of day one, practitioners will understand the concepts of perinatal and infant mental health and the impact it can have for the developing foetus, infant, mother, father/partner, wider family and society. “What it is and why it matters” © Institute of Health Visiting 2020
Learning Outcomes By the end of day one, practitioners will: • be able to *articulate the importance of good perinatal and infant mental health • have reviewed and be able to appreciate contemporary policy and research related to perinatal and infant mental health, understanding how it applies to practice at a local level • appreciate the effects and impact of perinatal mental illness on: the mother, father/partner; the developing foetus-infant-child; across the life course and the wider family • understand the key concepts relating to infant mental health, appreciating what an infant needs from care givers to help them build strong and secure foundations for emotional wellbeing • recognise how perinatal mental illness can affect the parent-child and wider family relationships • know the range of perinatal mental health conditions and be able to recognise the clinical features of the most common perinatal mental health conditions • appreciate the benefits of developing resilience in practice and feel confident to promote this concept to colleagues © Institute of Health Visiting 2020
PIMH: Clarification of the Terminology Perinatal Mental Health • As more evidence emerges about the effects of PMI on the mother, developing foetus/infant and family, the term perinatal mental health, is now commonly used to describe mental health in the period from conception to 1 year following the birth of the child • PMH in the context of this training is about the emotional wellbeing of mothers, fathers/partners, their children and families from conception to 1 year following the child’s birth © Institute of Health Visiting 2020
PIMH: Clarification of the Terminology Infant Mental Health • The young child’s capacity to experience, regulate and express emotions, form close and secure relationships, and explore the environment and learn. All of these capacities will be best accomplished within the context of the caregiving environment that includes family, community and cultural expectations. Developing these capacities is synonymous with healthy social and emotional development. (Zero to three 2001, cited Zeanah 2009) © Institute of Health Visiting 2020
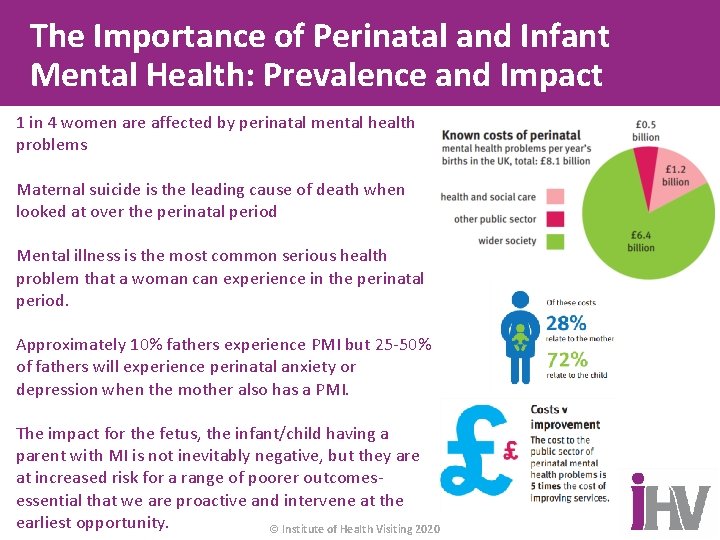
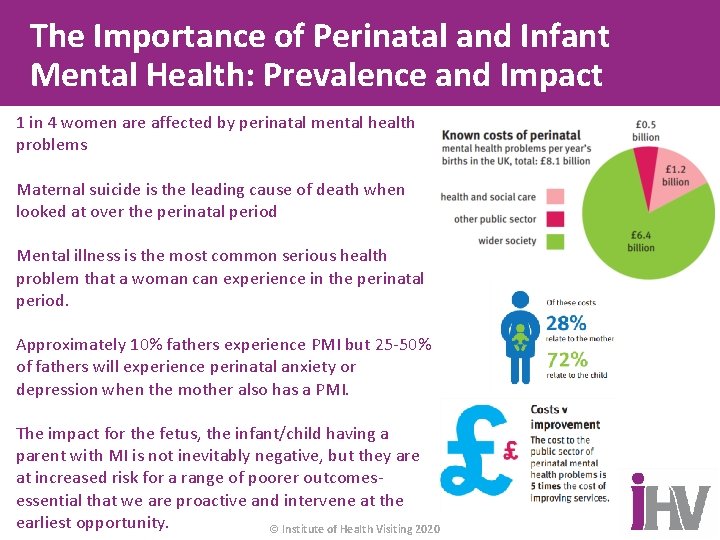
The Importance of Perinatal and Infant Mental Health: Prevalence and Impact 1 in 4 women are affected by perinatal mental health problems Maternal suicide is the leading cause of death when looked at over the perinatal period Mental illness is the most common serious health problem that a woman can experience in the perinatal period. Approximately 10% fathers experience PMI but 25 -50% of fathers will experience perinatal anxiety or depression when the mother also has a PMI. The impact for the fetus, the infant/child having a parent with MI is not inevitably negative, but they are at increased risk for a range of poorer outcomesessential that we are proactive and intervene at the earliest opportunity. © Institute of Health Visiting 2020

Policy and Research © Institute of Health Visiting 2020
Policy and Research • Adverse childhood experiences: What we know, what we don't know, and what should happen next (2020) • Mental Health and the Journey to Parenthood (2019) • Infant Mental Health Competencies Framework (IMHCF) (2019) • Fight for a Fair Start (2019) • PMH Curricular Framework: A framework for maternal and IMH (2019) • The NHS Long Term Plan (2019) • WHO's Nurturing Care Framework (2018) • From bumps to babies: PMH care in Wales (2018) • The Perinatal Mental Health Care Pathways (2018) • MBRRACE-UK Saving Lives, Improving Mothers’ Care (2015, 2017, 2018, 2019) • Every mother must get the help they need (2017) • Womens Voices (2017) • Specialist Health Visitors in PIMH: What they do and why they matter (2016) • Associations between maternal-foetal attachment and infant dev. outcomes (2016) • National Maternity Review (2016) • NICE QS 115 (2016) © Institute of Health Visiting 2020

Policy and Current Research • Falling Through the Gaps Practical implications for primary care of the NICE CG 192 (2015) • Building Great Britons (2015) • NICE CG 192 (2014) • Cost of Perinatal Mental Health Problems (2014) • Psychological adversity in pregnancy (2014) • Cross Party Manifesto, The 1001 Critical Days (2013) • NSPCC - Prevention In Mind (2013) • Wave Trust - Conception to Two (2013) • Boots Family Trust - Wellbeing Plan (2013) • Joint Commissioning Panel for MH: Guidance for Commissioners of PMH Services (2012) • Management of Women with Mental Health Issues during Pregnancy and the Postnatal Period (2011) • No Health without Mental Health (2011) © Institute of Health Visiting 2020
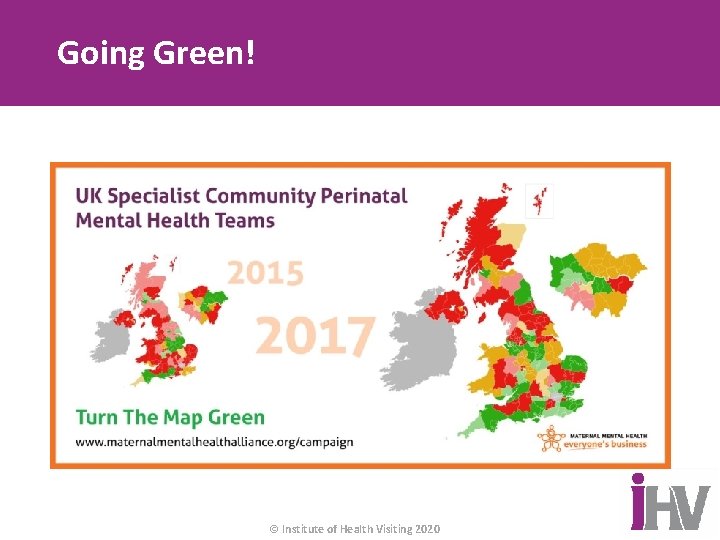
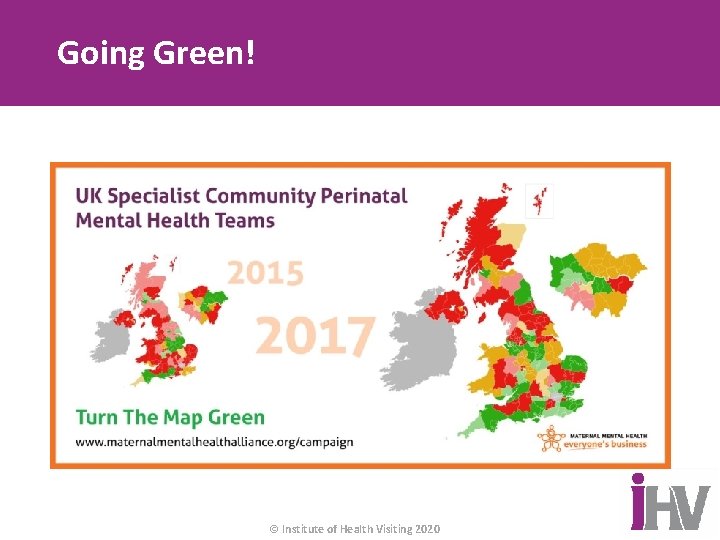
Going Green! © Institute of Health Visiting 2020
The Building Blocks: Infant Mental Health “The environment in the womb, during different sensitive periods for specific outcomes, can alter the development of the fetus, with a permanent effect on the child. We are now beginning to understand this at the molecular level” (V. Glover, oral evidence to Marce Society, 2016). https: //www. albertafamilywellness. org/resources/video/thecore-story-of-brain-development © Institute of Health Visiting 2020
Epigenetics: The opportunity to develop weapons of mass construction! https: //www. youtub e. com/watch? v=9 Af. B s. TAQ 8 zs#t=38 © Institute of Health Visiting 2020
Emotional Wellbeing in Pregnancy www. beginbeforebirth. org https: //youtu. be/TSWX 3 n-Rys © Institute of Health Visiting 2020
Trauma-informed approaches in the antenatal period to support mental health across the life-course Trauma-informed care - changing the narrative from: What’s wrong with you? To……. What happened to you? “To understand how to really care for women, we must first understand where she came from“ © Institute of Health Visiting 2020
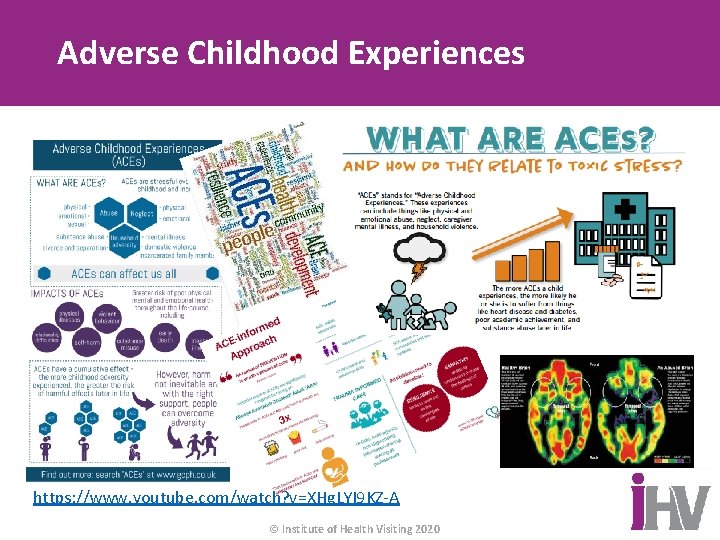
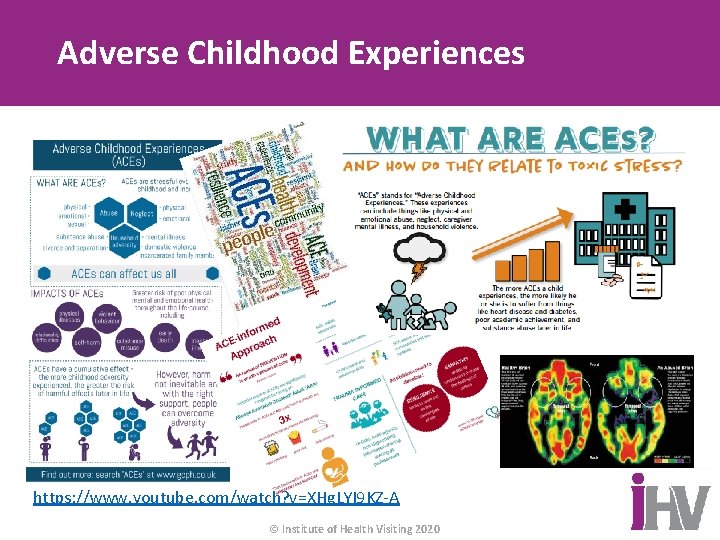
Adverse Childhood Experiences https: //www. youtube. com/watch? v=XHg. LYI 9 KZ-A © Institute of Health Visiting 2020
Seeing the woman - holding the child History of childhood abuse or trauma is associated with increased risk of perinatal mental illness. . Practitioners should take into account the potential experience and impact of trauma during perinatal period. Pregnancy, maternity care, birth and transition to parenting and postnatal period can be extremely triggering, particularly for women who have experienced childhood sexual abuse (1 in 4 women). © Institute of Health Visiting 2020
Antenatal Stress and Anxiety • Stress and anxiety are different but often occur together and can be in the absence of depression • Pregnancy is a time of increased vulnerability for the development of anxiety (and depression) anxiety disorders are present in significant numbers in perinatal period *(15%) • Anxiety disorder is a strong predictor of PND, general anxiety disorder in the antenatal period predicts depression at all time points after delivery • Symptoms of anxiety and depression often occur together • NICE (2014) recognises the need to identify and support women who do not necessarily meet diagnostic criteria for mental illness but do experience a range of symptoms that cause distress • Essential that stress and anxiety are detected during pregnancy and appropriate interventions offered © Institute of Health Visiting 2020
Obstetric Consequences of PMI Antenatal identification of women with a mental illness and / or a history of mental illness is important to protect the health of the mother and may also impact upon the health of the neonate. PMIs in pregnancy have been associated with adverse obstetric and neonatal outcomes, for example: • • Pre-term birth Low birth weight Small-for-gestational-age births Increased likelihood of caesarean / instrumental delivery However, it is important to bear in mind co-morbidity and the factors that may influence the association between maternal mental disorder and adverse neonatal outcomes © Institute of Health Visiting 2020
Causes and impact: Importance of early intervention Advances in research are highlighting the multiple biological, psychological and social aetiological pathways that are known to influence the associations between mental illness and the factors that may increase adverse obstetric, neonatal and infant outcomes Discussion Groups: 1. Why do you think that women experiencing PMI might be at increased risk of adverse obstetric/neonatal outcomes? 2. What are the implications for practice? https: //bmcpregnancychildbirth. biomedcentral. com/articles/10. 1186/s 12884 -019 -2572 -4 © Institute of Health Visiting 2020
Differential diagnosis: Challenges for assessment and identification of mental health problems in antenatal period • Physical symptoms of pregnancy • Minor disorders • Effective assessment must unpick those overlapping symptoms to determine what they represent Misdiagnosis can work both ways round • it is not just failure to identify PMI because it is perceived to be a physical symptom of pregnancy • symptoms of medical conditions such as eclampsia, infection or pulmonary embolus have been misattributed in women with an identified mental health problem and this has led to deaths in new mothers © Institute of Health Visiting 2020
Impact of Adverse Prenatal Mental Health • Adverse prenatal mental health has been shown to be associated with a wide range of outcomes both in the short (i. e. immediately following birth) and longer term (i. e. through to adolescence and adulthood). • Children of women who are experiencing adverse pre natal mental health during pregnancy have an increased risk of adverse neurodevelopmental, physical, social, emotional, behavioural and cognitive outcomes. • Important to emphasise this is not inevitable, there is opportunity to ameliorate effects, and most children born to mothers with PMI will be ok. © Institute of Health Visiting 2020
Supporting Parental Emotional Wellbeing and Infant Development in Your Practice • Support mothers and fathers to negotiate the emotional, as well as the physical transition to parenthood • Nurture healthy couple relationships • Encourage the development of sensitive, reflective parent-child relationships, starting in the antenatal period • Help mothers and their partners to begin to relate to their baby as a person through informing them of the research • Explore with the mother how they imagine their baby to be. • Encourage positive images of the baby. Explorations that identify extremely negative images or that suggest the mother is very ‘disengaged’ should involve referral to a psychologist • Integrate the emotional wellbeing alongside physical wellbeing at all opportunities. For example; asking a mother/father during listening for the heartbeat, “how does hearing your baby’s heartbeat make you feel? ” © Institute of Health Visiting 2020
Bonding Before Birth https: //youtu. be/OD TY-i. YYJNU © Institute of Health Visiting 2020
Infant Development • Nature AND nurture • Brain is not mature at birth • Brain is changed by experience • Timing of experiences is important • Relationships influence social and emotional functioning © Institute of Health Visiting 2020
Supporting the Parent/Infant Relationship: Family Mental Health PMI can influence the way in which a parent thinks about, interprets, describes, cares for and interacts with their baby. This can affect the way a parent feels about their ability to care for their baby, their enjoyment of parenting, their parenting styles and their developing relationship with their baby. Children with 2 depressed parents = higher risk of poor development outcomes Interaction with caregivers is the most important element of a child’s early experience and lays the foundations for his or her social and emotional development It is through these early interactions that babies learn how to recognise and regulate their own emotions, and build the foundations for later relationships. Support for the affected parent, and for the rest of the family, can make a really positive difference to the outcome for everyone in the family. © Institute of Health Visiting 2020
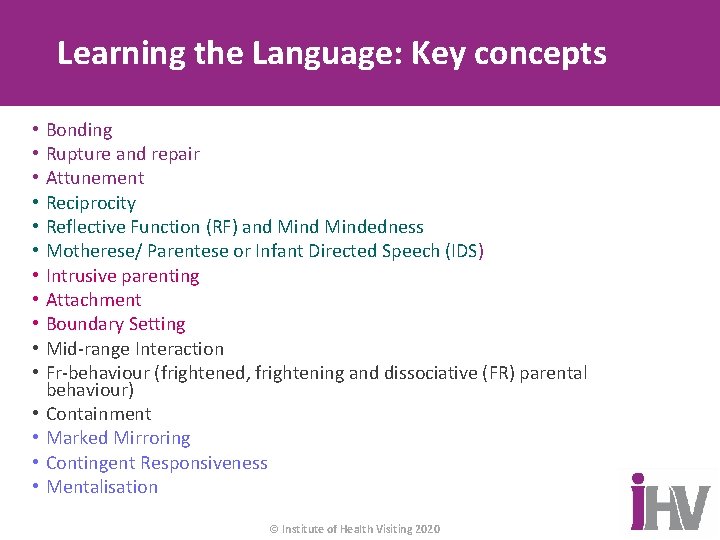
Learning the Language: Key concepts • • • • Bonding Rupture and repair Attunement Reciprocity Reflective Function (RF) and Mindedness Motherese/ Parentese or Infant Directed Speech (IDS) Intrusive parenting Attachment Boundary Setting Mid-range Interaction Fr-behaviour (frightened, frightening and dissociative (FR) parental behaviour) Containment Marked Mirroring Contingent Responsiveness Mentalisation © Institute of Health Visiting 2020

Still Face Experiment http: //bit. ly/1 m. EZ 3 Y 8 © Institute of Health Visiting 2020

Getting to Know your Baby https: //aimh. org. uk/getting-to-know-your-baby/ © Institute of Health Visiting 2020
Observing the Parent–Infant Relationship https: //youtu. be/ PZcd. Ph. Qp 2 W 8 © Institute of Health Visiting 2020
Observing the Parent–Infant Relationship https: //youtu. be/ 4 TYjzxpz 0 c. A © Institute of Health Visiting 2020

Observing the Parent–Infant Relationship: Father involvement © Institute of Health Visiting 2020
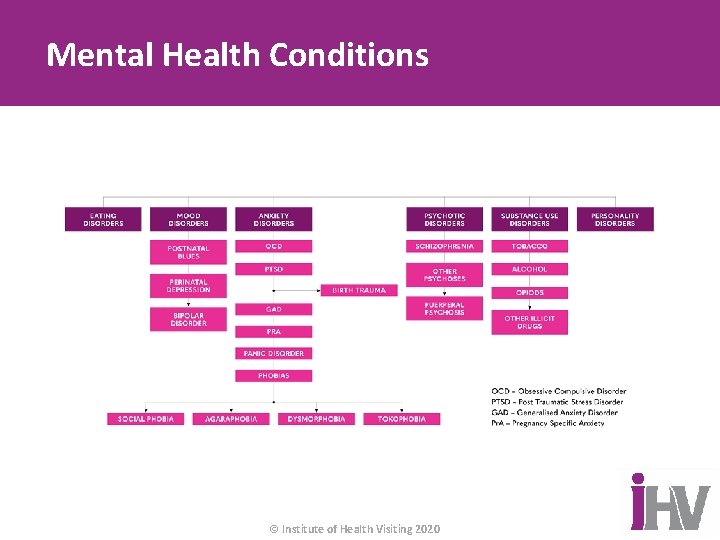
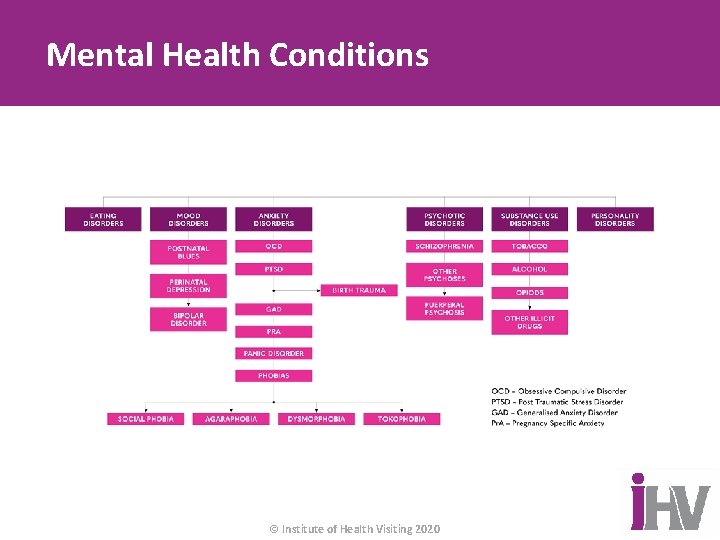
Mental Health Conditions © Institute of Health Visiting 2020
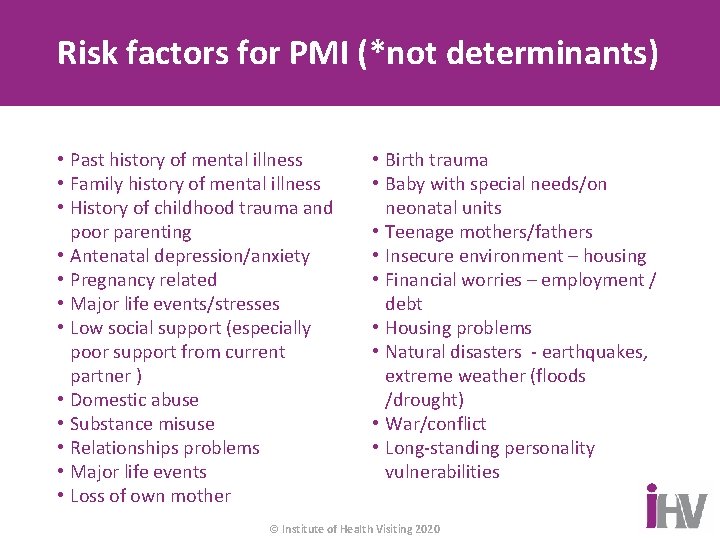
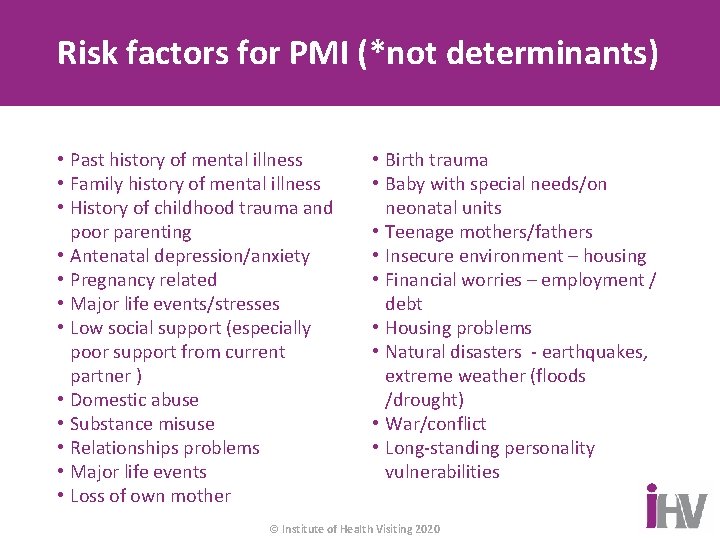
Risk factors for PMI (*not determinants) • Past history of mental illness • Family history of mental illness • History of childhood trauma and poor parenting • Antenatal depression/anxiety • Pregnancy related • Major life events/stresses • Low social support (especially poor support from current partner ) • Domestic abuse • Substance misuse • Relationships problems • Major life events • Loss of own mother • Birth trauma • Baby with special needs/on neonatal units • Teenage mothers/fathers • Insecure environment – housing • Financial worries – employment / debt • Housing problems • Natural disasters - earthquakes, extreme weather (floods /drought) • War/conflict • Long-standing personality vulnerabilities © Institute of Health Visiting 2020
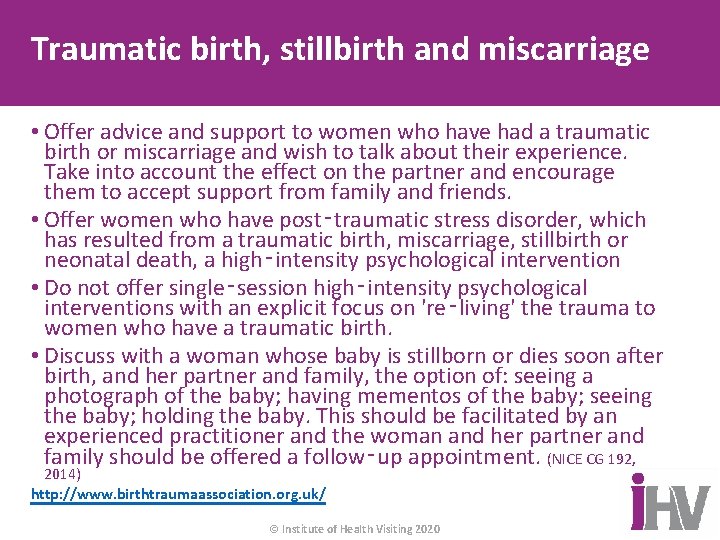
Traumatic birth, stillbirth and miscarriage • Offer advice and support to women who have had a traumatic birth or miscarriage and wish to talk about their experience. Take into account the effect on the partner and encourage them to accept support from family and friends. • Offer women who have post‑traumatic stress disorder, which has resulted from a traumatic birth, miscarriage, stillbirth or neonatal death, a high‑intensity psychological intervention • Do not offer single‑session high‑intensity psychological interventions with an explicit focus on 're‑living' the trauma to women who have a traumatic birth. • Discuss with a woman whose baby is stillborn or dies soon after birth, and her partner and family, the option of: seeing a photograph of the baby; having mementos of the baby; seeing the baby; holding the baby. This should be facilitated by an experienced practitioner and the woman and her partner and family should be offered a follow‑up appointment. (NICE CG 192, 2014) http: //www. birthtraumaassociation. org. uk/ © Institute of Health Visiting 2020

Bereavement Care Pathway www. nbcpathway. org. uk © Institute of Health Visiting 2020
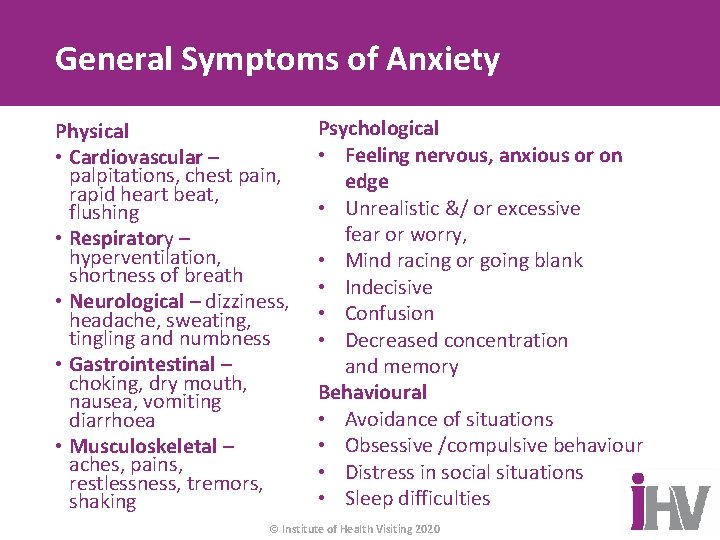
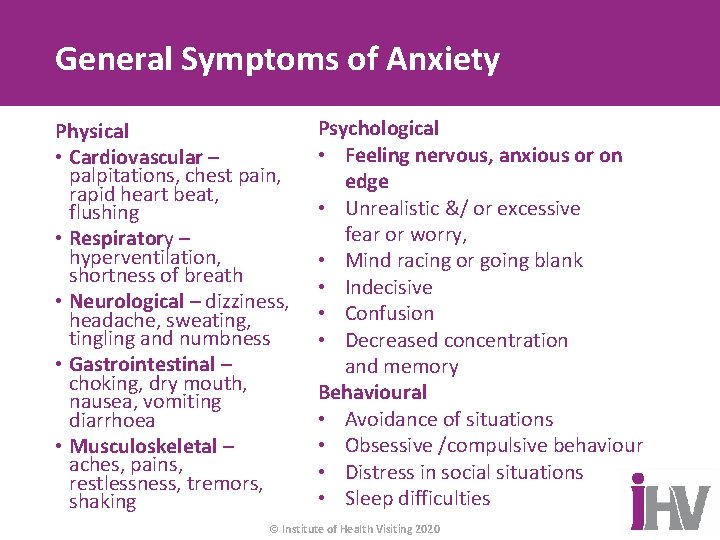
General Symptoms of Anxiety Physical • Cardiovascular – palpitations, chest pain, rapid heart beat, flushing • Respiratory – hyperventilation, shortness of breath • Neurological – dizziness, headache, sweating, tingling and numbness • Gastrointestinal – choking, dry mouth, nausea, vomiting diarrhoea • Musculoskeletal – aches, pains, restlessness, tremors, shaking Psychological • Feeling nervous, anxious or on edge • Unrealistic &/ or excessive fear or worry, • Mind racing or going blank • Indecisive • Confusion • Decreased concentration and memory Behavioural • Avoidance of situations • Obsessive /compulsive behaviour • Distress in social situations • Sleep difficulties © Institute of Health Visiting 2020
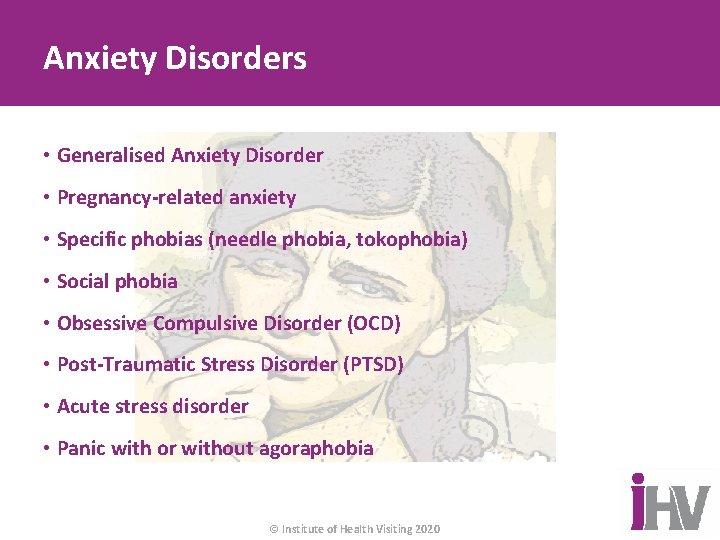
Anxiety Disorders • Generalised Anxiety Disorder • Pregnancy-related anxiety • Specific phobias (needle phobia, tokophobia) • Social phobia • Obsessive Compulsive Disorder (OCD) • Post-Traumatic Stress Disorder (PTSD) • Acute stress disorder • Panic with or without agoraphobia © Institute of Health Visiting 2020
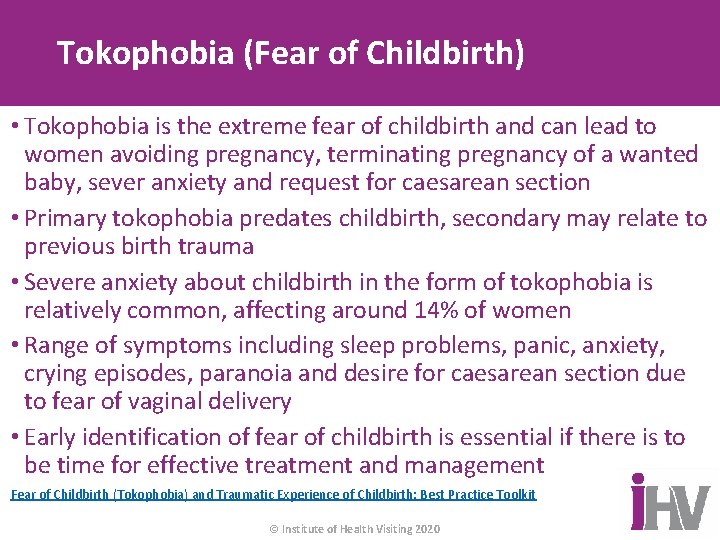
Tokophobia (Fear of Childbirth) • Tokophobia is the extreme fear of childbirth and can lead to women avoiding pregnancy, terminating pregnancy of a wanted baby, sever anxiety and request for caesarean section • Primary tokophobia predates childbirth, secondary may relate to previous birth trauma • Severe anxiety about childbirth in the form of tokophobia is relatively common, affecting around 14% of women • Range of symptoms including sleep problems, panic, anxiety, crying episodes, paranoia and desire for caesarean section due to fear of vaginal delivery • Early identification of fear of childbirth is essential if there is to be time for effective treatment and management Fear of Childbirth (Tokophobia) and Traumatic Experience of Childbirth: Best Practice Toolkit © Institute of Health Visiting 2020
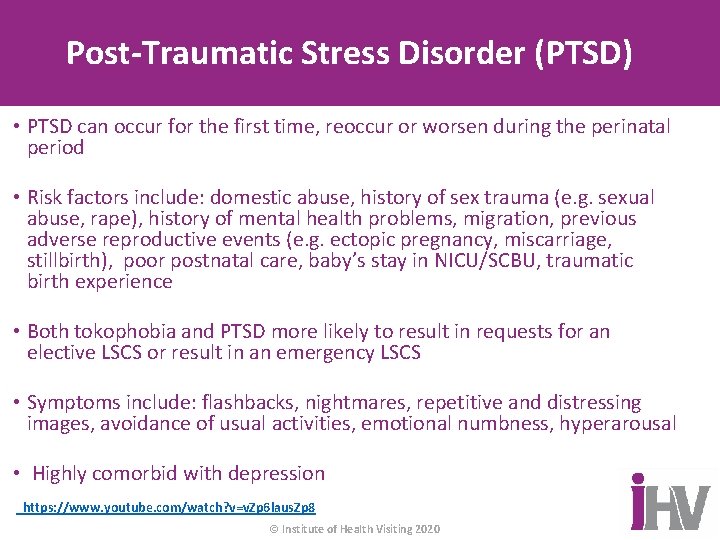
Post-Traumatic Stress Disorder (PTSD) • PTSD can occur for the first time, reoccur or worsen during the perinatal period • Risk factors include: domestic abuse, history of sex trauma (e. g. sexual abuse, rape), history of mental health problems, migration, previous adverse reproductive events (e. g. ectopic pregnancy, miscarriage, stillbirth), poor postnatal care, baby’s stay in NICU/SCBU, traumatic birth experience • Both tokophobia and PTSD more likely to result in requests for an elective LSCS or result in an emergency LSCS • Symptoms include: flashbacks, nightmares, repetitive and distressing images, avoidance of usual activities, emotional numbness, hyperarousal • Highly comorbid with depression https: //www. youtube. com/watch? v=v. Zp 6 laus. Zp 8 © Institute of Health Visiting 2020
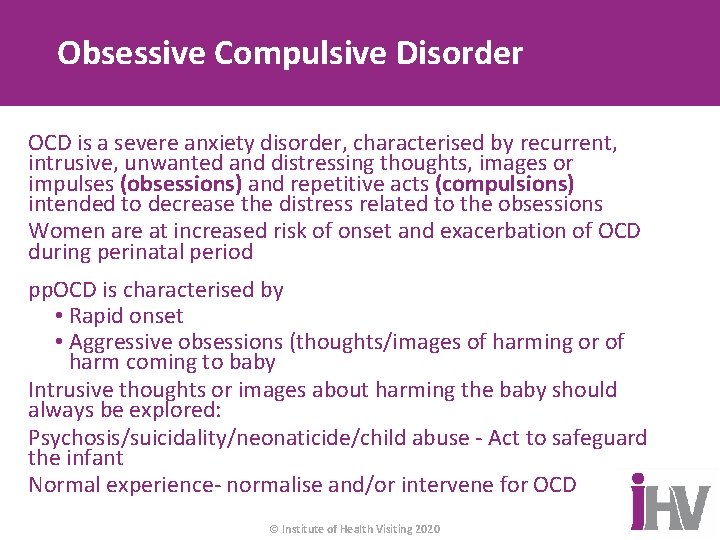
Obsessive Compulsive Disorder OCD is a severe anxiety disorder, characterised by recurrent, intrusive, unwanted and distressing thoughts, images or impulses (obsessions) and repetitive acts (compulsions) intended to decrease the distress related to the obsessions Women are at increased risk of onset and exacerbation of OCD during perinatal period pp. OCD is characterised by • Rapid onset • Aggressive obsessions (thoughts/images of harming or of harm coming to baby Intrusive thoughts or images about harming the baby should always be explored: Psychosis/suicidality/neonaticide/child abuse - Act to safeguard the infant Normal experience- normalise and/or intervene for OCD © Institute of Health Visiting 2020
NHS Choices – Mothers talking https: //www. youtube. com/watch? v=KBl. VBO P 7 TGc © Institute of Health Visiting 2020
Postpartum Psychosis • Affects 1 -2 in 1000 mothers – cases are rare, however, if a woman has a past history of postpartum psychosis or bipolar disorder, her risk rises to 25%-50%. This risk is increased if there is, in addition, a first-degree relative with either disorder • Rapid onset - the majority of those affected having an onset within the first three postnatal months. • Immediate hospitalisation © Institute of Health Visiting 2020
Symptoms of Postpartum Psychosis • Rapidly changing mood • Bizarre behaviour • Lack of inhibition • Hallucinations – distortion of the 5 senses • Delusions – thought disorder • Confusion • Agitation • Flight of ideas • Lack of insight • Risk to mother and infant © Institute of Health Visiting 2020
General Symptoms of Depression Physical • Tired all the time • Lack of energy • Crying, sad • Sleep disruption • Appetite disruption • Changes in weight • Pain • Loss of libido • Personal neglect • Psychomotor agitation or retardation Psychological • Self blame, criticism, guilt • Impaired concentration • Hopelessness • Depressed mood • Withdrawal from family and friends • Loss of motivation • Suicidal ideation • Anhedonia Behavioural • Self neglect/ avoidance • Insomnia/ hypersomnia © Institute of Health Visiting 2020
Perinatal Depression Baby Blues • Usually mild and transient low mood affecting between 30 -80% of new mothers in the first few days Perinatal Depression • Persistent and pervasive low mood of varying severity and duration. Frequently missed • Incidence of 10 -15% • Antenatal as common as postnatal • The most common complication of pregnancy • 40% of women are likely to experience subsequent postnatal or non postnatal relapse -with new research showing that women with persistent PND showed elevated depressive symptoms up to 11 years after childbirth. © Institute of Health Visiting 2020
Fathers and Perinatal Mental Health • Pregnancy is the most demanding period for the father’s psychological reorganisation of self • Labour and birth the most emotional moments • Postnatal period is the most challenging time The most common risk factors ( factual or perceptual): • Maternal depression • Poor social support • Low emotional support © Institute of Health Visiting 2020
Prevalence rates in Fathers Antenatal depression: 11 -12% Postnatal depression: 8 -26% Overall rates of perinatal mental illness in fathers 9% These rates rise to 50% if their partner is experiencing mental ill health in the perinatal period © Institute of Health Visiting 2020
Video to demonstrate the feelings around depression: Black Dog https: //www. youtub e. com/watch? v=Xi. Crn i. LQGYc © Institute of Health Visiting 2020
Join the Movement! i. HV Fellow, Sharin Baldwin, publishes Systematic Review on First Time Fathers’ Mental http: //www. newdadstudy. com Health and Wellbeing v @Mark. Williams. FMH v @dad_matters v @Ash. Curry. Ocd v @Dr. Andy. Mayers v @fatherhoodinst The Blues Boys d pa d da e /th / : s p htt © Institute of Health Visiting 2020 . uk o. c
Eating Disorders • May impact on a woman’s fertility, but does not preclude pregnancy • Between 2 -7. 5% of women may experience an eating disorder • For many women, eating disorder symptoms improve during pregnancy BUT, relapse of symptoms and postnatal depression is common following birth • Associated with adverse obstetric outcomes, difficulties with infant feeding and family mealtimes • Highlights the importance of preconception advice, and consistent antenatal and postnatal care © Institute of Health Visiting 2020 http: //www. eatingdisordersandpregnancy. co. uk
Bipolar Affective Disorder • Bipolar disorder is characterised by episodes of mania and episodes of depressed mood. • During periods of mania, symptoms may include increased energy, loss of inhibitions, delusions of grandeur, euphoric mood or irritability and rapid speech. • During bouts of depression, the usual symptoms associated with lowered mood are experienced and the individual may be at risk of suicide • Past history of bipolar disorder, increases risk of PP. © Institute of Health Visiting 2020
Schizophrenia Symptoms of schizophrenia include: • a lack of interest in things • Disassociation • Poor concentration • Hallucinations: visual, auditory, olfactory, gustatory, tactile • Delusions (including paranoid, persecutory, grandiose delusions) • Disorganised thinking and speech# • Ideas of reference • Made act • Thought interference • Lack of self care • Lack of motivation and interest in life • Emotional blunting © Institute of Health Visiting 2020
Personality Disorder Personality refers to the collection of characteristics or traits that we have developed as we have grown up and which make each of us an individual. Personality disorders are conditions in which an individual differs significantly in: • Thoughts – ways of looking at the world, thinking about self or others, and interacting • Emotions – appropriateness, intensity, and range of emotional functioning • Interpersonal Functioning – relationships and interpersonal skills. • Impulse Control – considering the outcome of actions Difficulties in thought patterns, emotions, interpersonal functioning and impulse control can be problematic in pregnancy, child-birth and the post-natal period. People with personality disorders have higher rates of: • substance misuse • Suicidality and deliberate self-harm • Depression, anxiety and emotional dysregulation • social services involvement • poor engagement with antenatal / postnatal care which can lead to poor outcomes for the individual and the infant © Institute of Health Visiting 2020
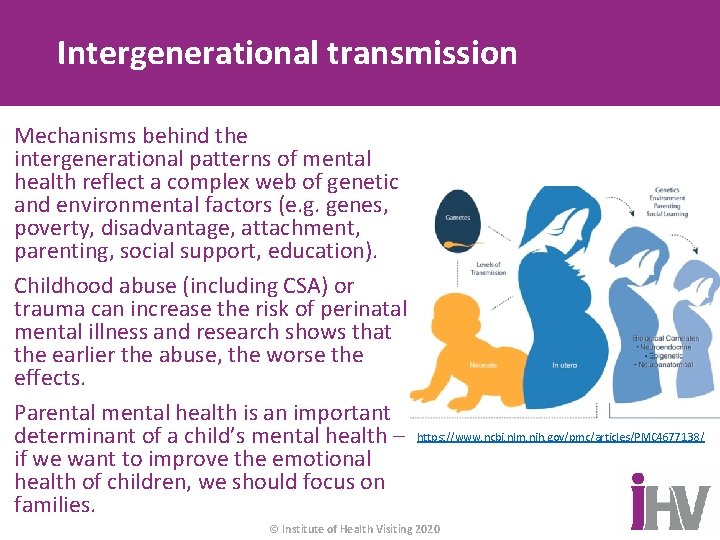
Intergenerational transmission Mechanisms behind the intergenerational patterns of mental health reflect a complex web of genetic and environmental factors (e. g. genes, poverty, disadvantage, attachment, parenting, social support, education). Childhood abuse (including CSA) or trauma can increase the risk of perinatal mental illness and research shows that the earlier the abuse, the worse the effects. Parental mental health is an important determinant of a child’s mental health – if we want to improve the emotional health of children, we should focus on families. https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 4677138/ © Institute of Health Visiting 2020
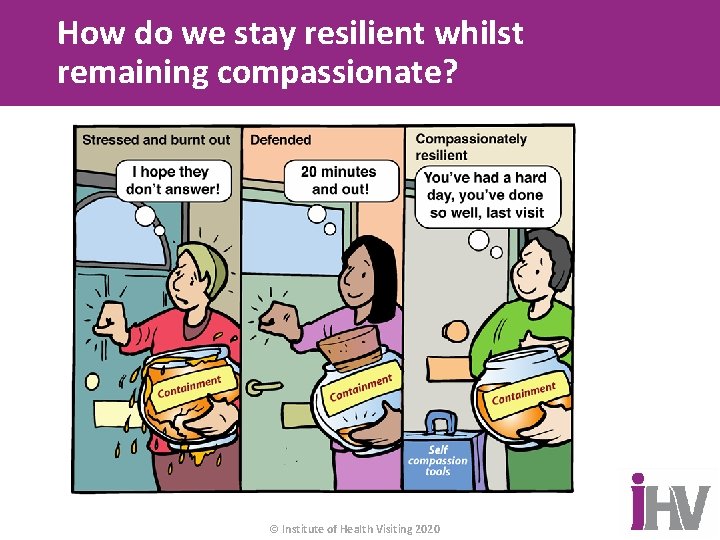
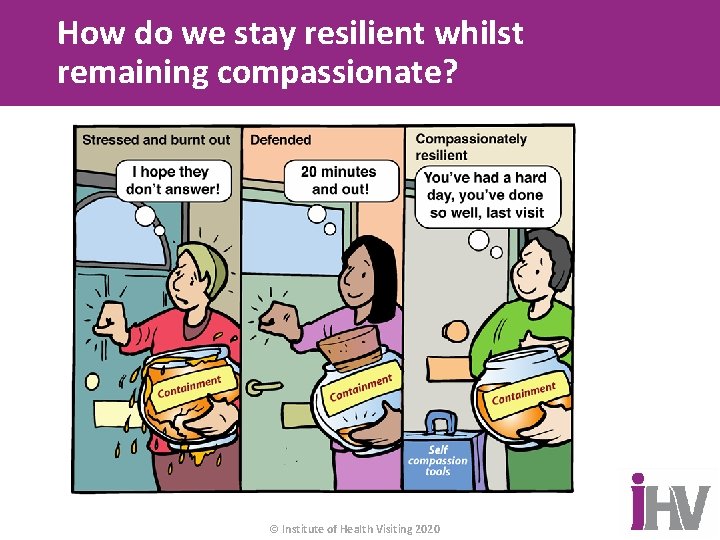
How do we stay resilient whilst remaining compassionate? © Institute of Health Visiting 2020
Wellbeing Factors that influence our wellbeing in work: • Control over our job • Clarity of what is expected of us After mental/physical health and personal relationships, our work/employment is the • Variety in what we do • Positive relationships with colleagues and 3 rd biggest factor associated with our families we work with wellbeing. • Belief that our workplace and pay are fair A supportive and effective workplace is key • A sense of personal purpose and of our for practitioner wellbeing. wider value to others • Opportunities to use and develop our skills Training leaders (Champions) to be effective • A safe and pleasant working environment and supportive can enhance the wellbeing • Supportive supervision of both leaders (Champions) and their colleagues. • A sense of job security and clear career prospects There is link between staff wellbeing and • Good work/life balance quality of patient care Wellbeing is about how we are doing as individuals, communities and as a society. https: //whatworkswellbeing. org/ © Institute of Health Visiting 2020
 Catherine maguire infant mental health
Catherine maguire infant mental health Privacy awareness and hipaa awareness training cvs
Privacy awareness and hipaa awareness training cvs Objective for mental health awareness
Objective for mental health awareness Mental health awareness poem
Mental health awareness poem Titles for mental health presentations
Titles for mental health presentations Chapter 20 mental health and mental illness
Chapter 20 mental health and mental illness Stress management jeopardy
Stress management jeopardy Maternal and infant health disparities
Maternal and infant health disparities Golden thread clinical documentation
Golden thread clinical documentation We can talk mental health training
We can talk mental health training Georgia mental health consumer network cps training
Georgia mental health consumer network cps training Promoting infant health section 7-2
Promoting infant health section 7-2 Hhs
Hhs Infant oral health care
Infant oral health care Seta security education training awareness
Seta security education training awareness Suspicious package awareness training
Suspicious package awareness training Hipaa privacy and security awareness training
Hipaa privacy and security awareness training Clear perinatal quality
Clear perinatal quality Coex grof
Coex grof Perinatal mortality rate
Perinatal mortality rate Classification of birth asphyxia
Classification of birth asphyxia Perinatal asphyxia
Perinatal asphyxia Perinatal audit
Perinatal audit Uyarıcı zenginliği ve yoksunluğu nedir
Uyarıcı zenginliği ve yoksunluğu nedir Indiana perinatal quality improvement collaborative
Indiana perinatal quality improvement collaborative Certain conditions originating in the perinatal period
Certain conditions originating in the perinatal period Ccqi perinatal standards
Ccqi perinatal standards South dakota perinatal association
South dakota perinatal association Standing around crying
Standing around crying Helen marlo
Helen marlo Ruta materno perinatal
Ruta materno perinatal Waiter's tip deformity
Waiter's tip deformity Hie
Hie Picme2.0
Picme2.0 Iso 9001:2015 presentation
Iso 9001:2015 presentation Cjis security levels
Cjis security levels Was i sexually abused as a child quiz
Was i sexually abused as a child quiz Ppe awareness training
Ppe awareness training Ppe awareness training
Ppe awareness training Sogedac
Sogedac Iso 9001:2015 management review meeting presentation ppt
Iso 9001:2015 management review meeting presentation ppt Iso 14001 awareness training
Iso 14001 awareness training Insider threat awareness training
Insider threat awareness training Environmental management system awareness training
Environmental management system awareness training Dynamic risk assessment training
Dynamic risk assessment training Mold awareness training
Mold awareness training Chemical sensitivity symptoms
Chemical sensitivity symptoms Dysphagia symptoms
Dysphagia symptoms Hand arm vibration awareness training
Hand arm vibration awareness training Ergonomics awareness training for supervisors
Ergonomics awareness training for supervisors Ergonomics awareness training for supervisors
Ergonomics awareness training for supervisors Sfar 73 awareness training
Sfar 73 awareness training Mold awareness training
Mold awareness training Insider threat training slides
Insider threat training slides 00-25-234
00-25-234 Webroot cyber security training
Webroot cyber security training Lgbt awareness training
Lgbt awareness training Find ergonomics awareness training
Find ergonomics awareness training Rf safety awareness training answers
Rf safety awareness training answers Bloodborne pathogens awareness training
Bloodborne pathogens awareness training Phonological awareness training program
Phonological awareness training program Child protection awareness training
Child protection awareness training Counterfeit material awareness training
Counterfeit material awareness training Ehs awareness training
Ehs awareness training