MOOD DISORDERS Part I Depressive Disorders Major Depressive



- Slides: 39
MOOD DISORDERS
Part I: Depressive Disorders
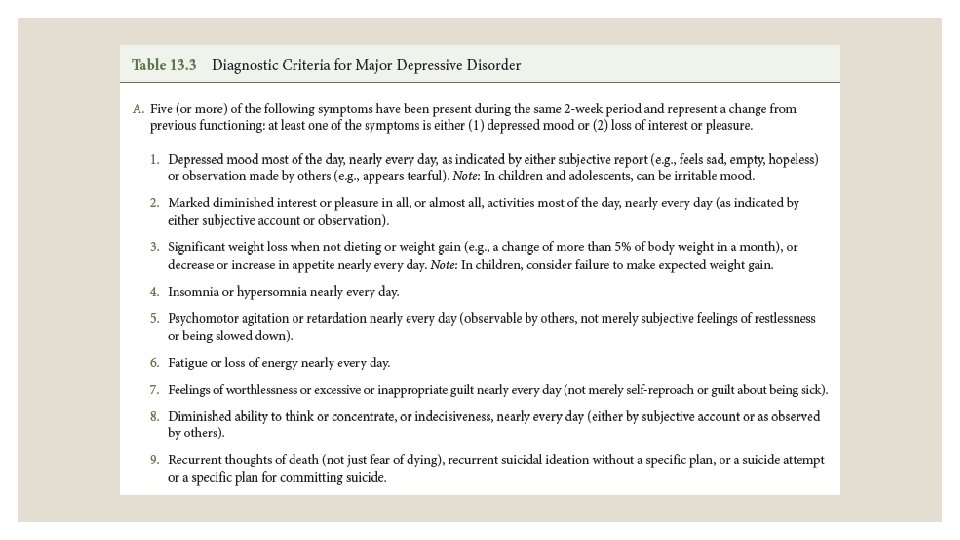
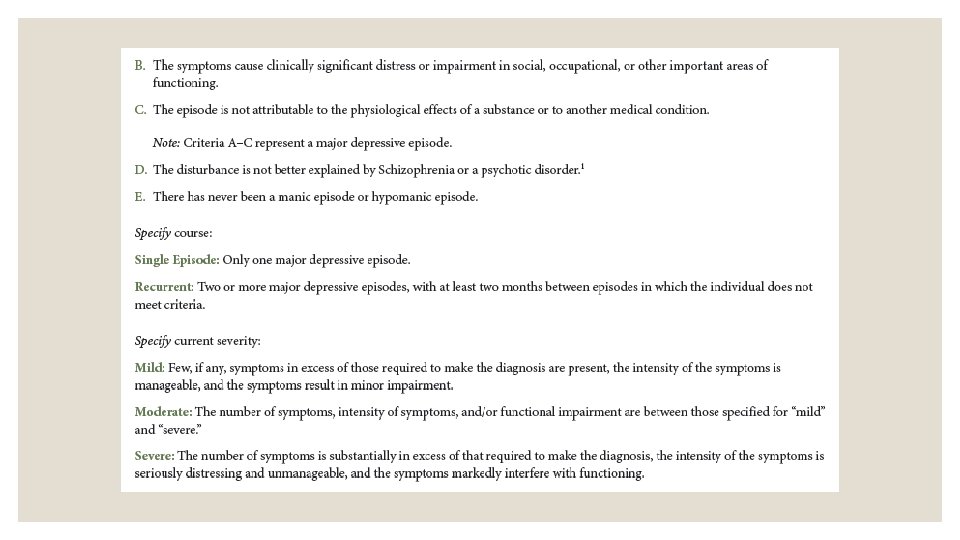
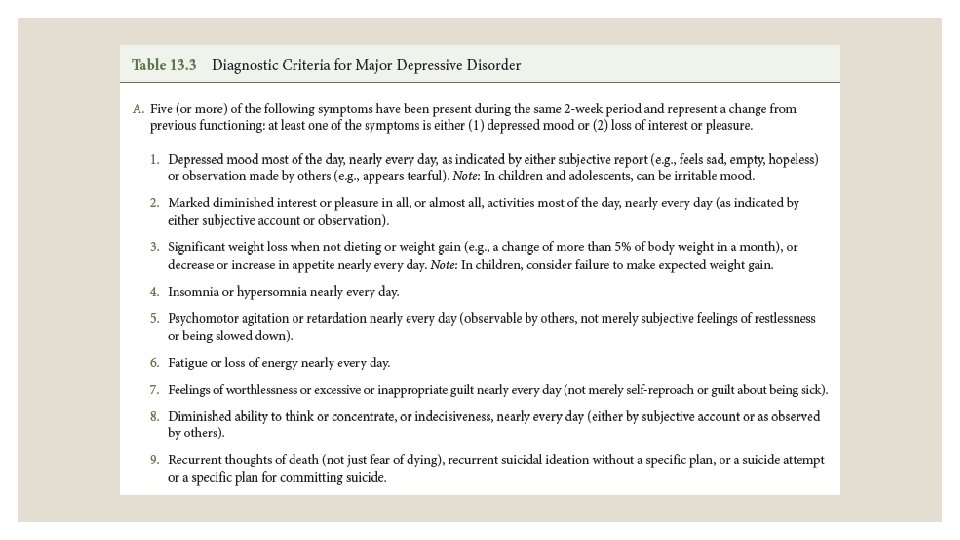
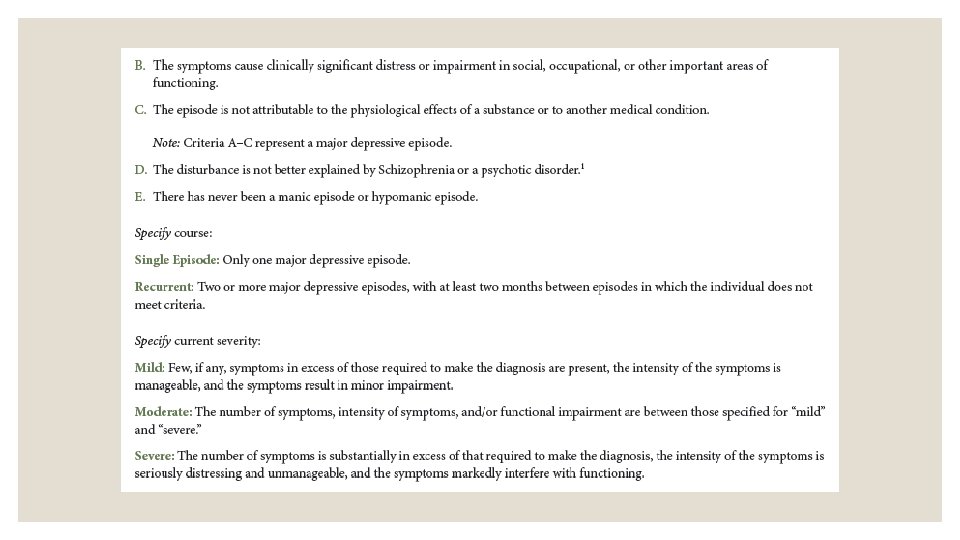
Major Depressive Disorder ◦ Core Features (diagnosis requires at least 1 of the following): ◦ Depressed, sad, or irritable mood ◦ Loss of interest in most activities (anhedonia) ◦ As with adults 5 of 9 DSM-5 symptoms needed (see DSM-5 criteria next slide)
Diagnostic uncertainty ◦ Distinct episode or general unhappiness? ◦ Difficulty with self-expression ◦ Comorbidity & co-occurrence ◦ Anxiety 25 -50% ◦ Disruptive behavior disorder 33 -60%
Estimated Prevalence ◦ 1 -2% of preschool children ◦ 2% of school-aged children ◦ 4% late childhood/early-adolescence ◦ 15% of late adolescence & young adults
Course of MDD ◦ Median length = 7 to 9 months ◦ Most children will have a subsequent episodes ◦ Early onset is a negative prognostic sign ◦ Adolescents who have two or more major depressive episodes will likely experience depression as adults
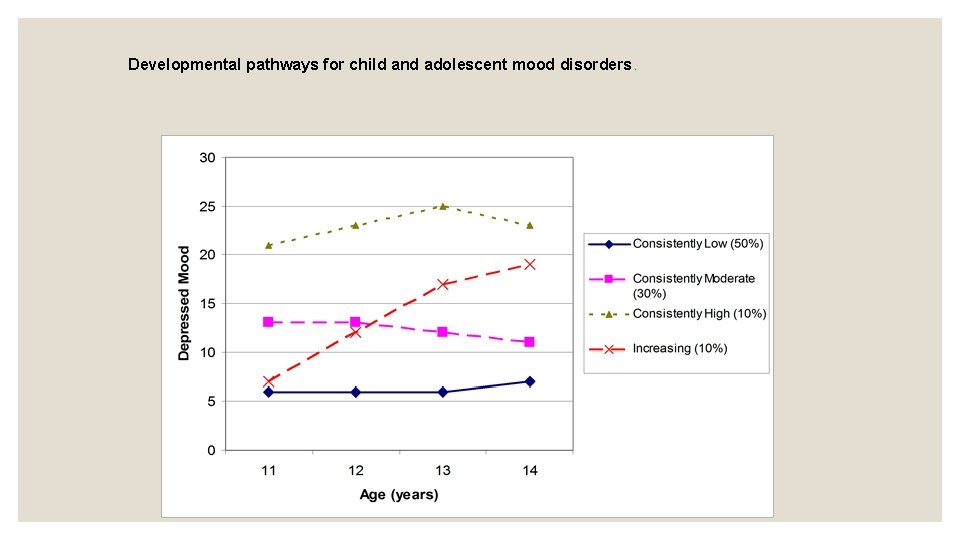
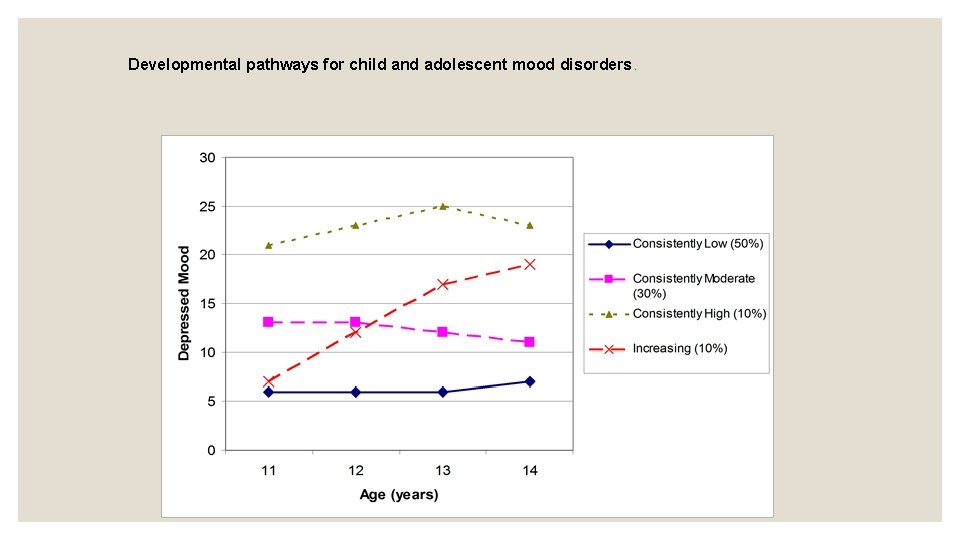
Developmental pathways for child and adolescent mood disorders.
COURSE ◦ Children and adolescents with depressive disorder are at elevated risk for: ◦ Bipolar disorder ◦ Eating disorders ◦ Substance use disorders ◦ Suicide ◦ Anxiety Disorders
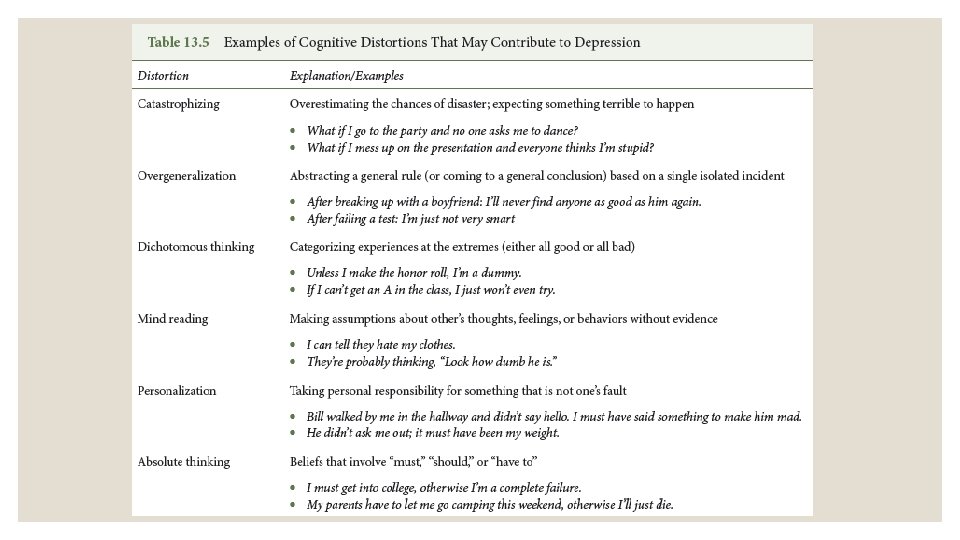
Etiology ◦ Genetics- depression has a moderate heritability estimate. ◦ Biological factors ◦ Neurological abnormalities ◦ Decreased blood flow and reduced activity in left frontal regions ◦ Amygdala dysregulation- amygdala important for arousal and mood regulation. ◦ Directionality- early environment characterized by abuse and neglect may affect neurological functioning (remember environment may impact biology).
Etiology ◦ Maternal Depression ◦ Other familial factors ◦ Even without parental depression, families of children with depression have higher levels of stress, marital discord, & negativity ◦ Directionality?
Treatment ◦ Adults: ◦ Evidence-based psychotherapy ◦ Behavioral/Cognitive behavioral therapy ◦ Interpersonal psychotherapy ◦ Medication: ◦ Antidepressants including SSRIs, tricyclic antidepressants, and monoamine oxidase inhibitors
Treatment ◦ Medication: ◦ There are probably over 20 medications approved for the treatment of adult depression at this point. ◦ What about children and adolescents? ◦ Much less evidence for the effectiveness of antidepressant medications in children and adolescents (especially children). Prozac is one of the only medications approved. ◦ Concerns exist related to increased suicidal ideation. This led to a black box warning: ◦ http: //www. fda. gov/Drugs/Drug. Safety/Informationby. Drug. Class/ucm 096352. htm#
TADS study ◦ For youth, what works best-- medications or psychotherapy? TADS (Treatment of Adolescents with Depression Study) sought to address this. ◦ 4 groups: ◦ Combined treatment (med & CBT) ◦ Meds only ◦ Placebo ◦ CBT only
TADS ◦ Results ◦ Combination and medication initially more effective ◦ CBT eventually catches up ◦ Suicidal thinking and behaviors reduced in all group, greatest reduction when CBT is included
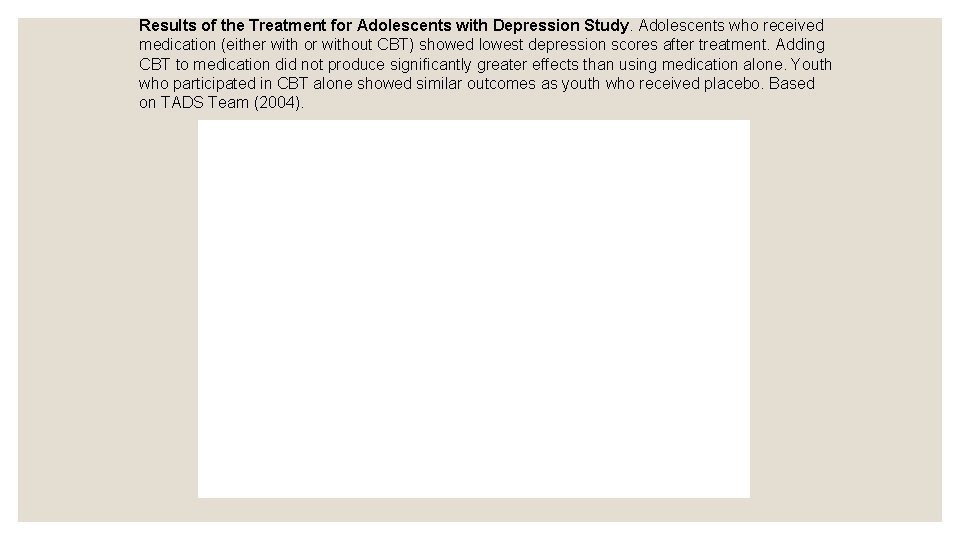
Results of the Treatment for Adolescents with Depression Study. Adolescents who received medication (either with or without CBT) showed lowest depression scores after treatment. Adding CBT to medication did not produce significantly greater effects than using medication alone. Youth who participated in CBT alone showed similar outcomes as youth who received placebo. Based on TADS Team (2004).
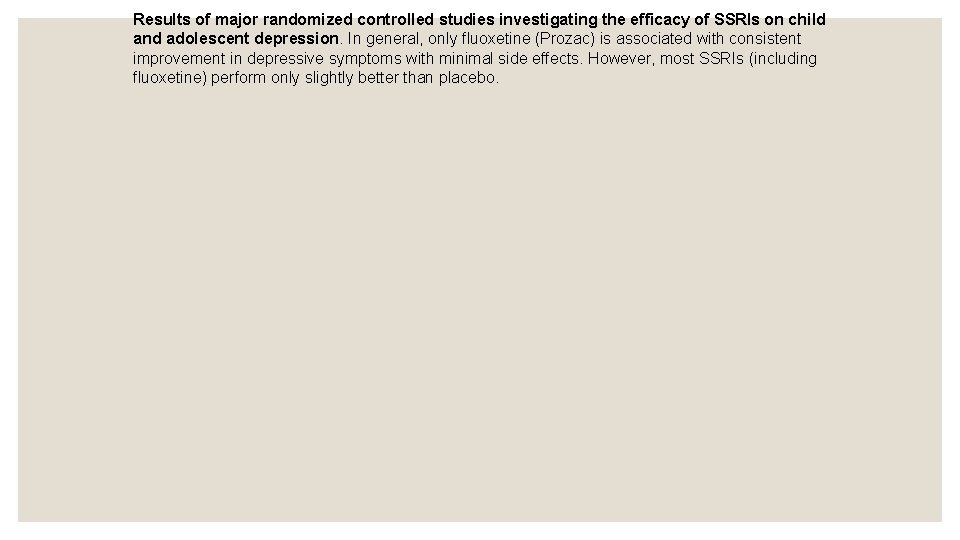
Results of major randomized controlled studies investigating the efficacy of SSRIs on child and adolescent depression. In general, only fluoxetine (Prozac) is associated with consistent improvement in depressive symptoms with minimal side effects. However, most SSRIs (including fluoxetine) perform only slightly better than placebo.
Persistent Depressive Disorder Chronic symptoms ◦ 1 year in children, 2 years in adults ◦ Former diagnoses (DSM-IV) ◦ Major depression- with a chronic symptoms (more severe forms) ◦ Dysthymic disorder- chronic low-grade depression
Part II: Bipolar Disorder
Bipolar disorder in children & adolescents ◦ Remember from Abnormal- the diagnosis of bipolar disorder requires at least 1 manic episode (1 week of intense manic symptoms). ◦ Adolescents: the pattern in adolescents seems very similar to the pattern seen in adults. Adult diagnostic criteria seems to apply. ◦ Children: this is a controversial diagnosis in children. ◦ Considered difficult to recognize and accurately diagnose. ◦ Historically, it has probably been over-diagnosed in children.
Mania in children & adolescents ◦ Frequent mood shifts, mixed moods, chronic difficulty regulating mood (episodes less distinct) ◦ Irritability (less euphoria) ◦ Psychotic features more likely ◦ Distinct disorder? ◦ Severe mood dysregulation ◦ Extreme ADHD
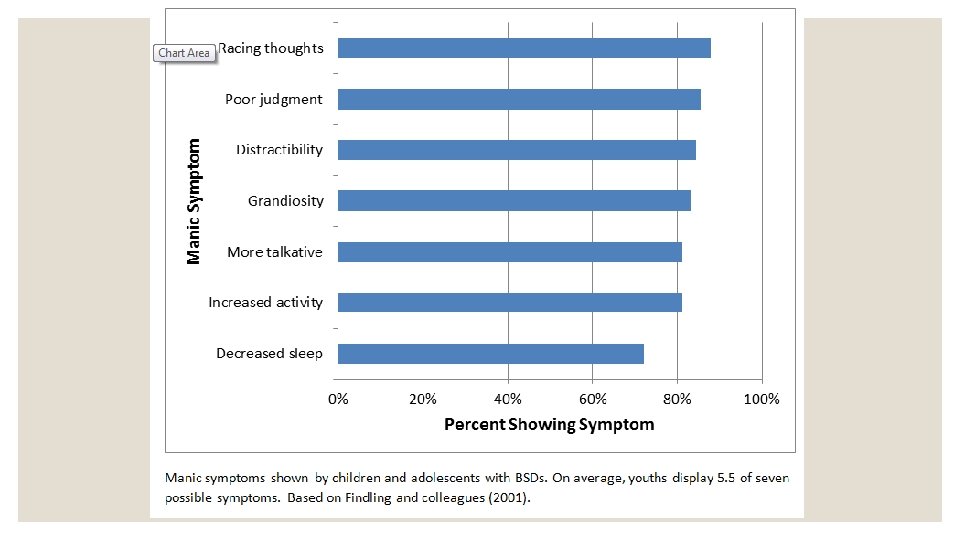
OTHER CHARACTERISTICS & COMMON EXPERIENCES ◦ Children and adolescents with bipolar disorder are at higher risk for: ◦ Substance abuse ◦ Suicide ◦ 44% of those diagnosed with bipolar attempt suicide, compared to 1. 2% in all adolescents
Prevalence ◦ Little known about prevalence ◦ About 1% of children and teens appear to experience bipolar disorder. ◦ During adolescence, equal numbers of males & females ◦ Prior to puberty, more boys than girls
Course ◦ Little is known about the course ◦ The disorders are often chronic ◦ Estimated 90% of children with bipolar disorder will have the disorder in adulthood
Etiology ◦ Neurological abnormalities believed to be associated with bipolar disorder ◦ E. g. Norepinephrine, dopamine ◦ Genetic influences ◦ Strong genetic influence ◦ Heritability estimate is around 80%
Etiology (continued) ◦ Environmental Stress ◦ May impact neurological development ◦ Influential but not causal. ◦ Diathesis-Stress Model
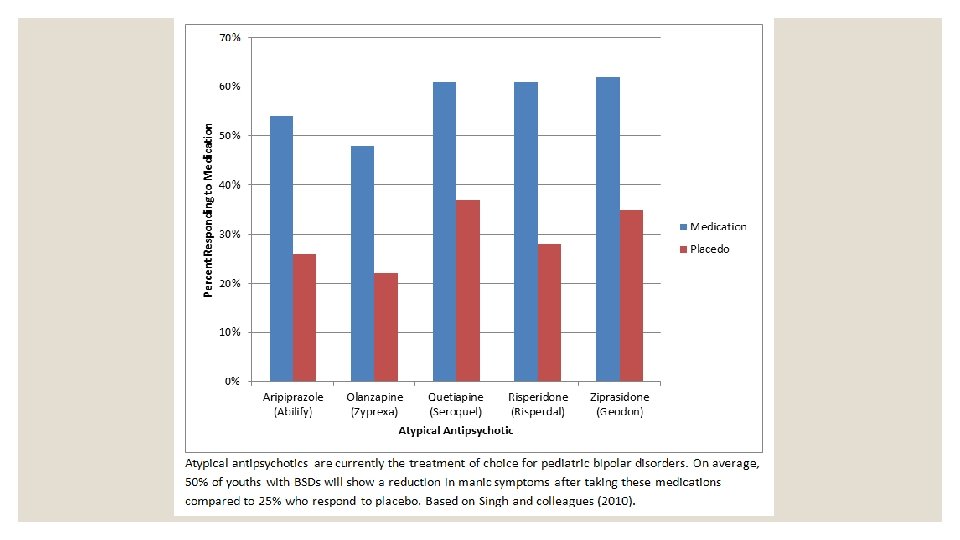
Therapeutic Interventions ◦ Medication ◦ Lithium ◦ Anticonvulsants- Depakote, Tegretol ◦ Atypical antipsychotics- Zyprexa, Risperdal ◦ Side effects common, some serious & long-term (e. g. kidney and heart problems) ◦ Hospitalization
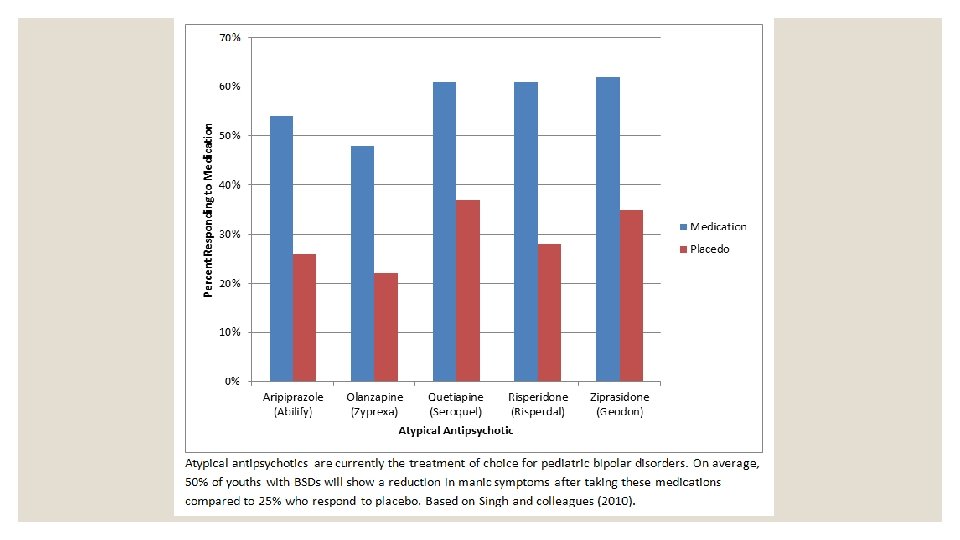
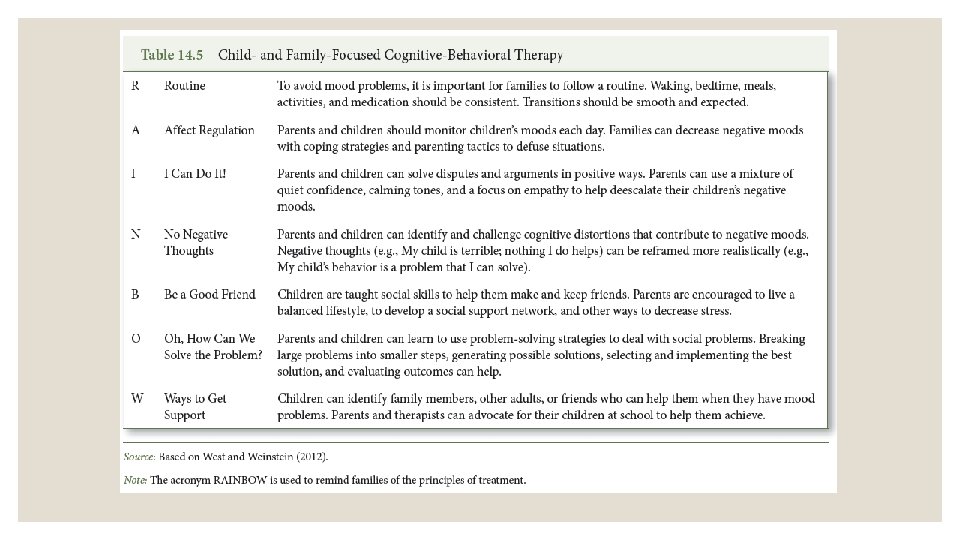
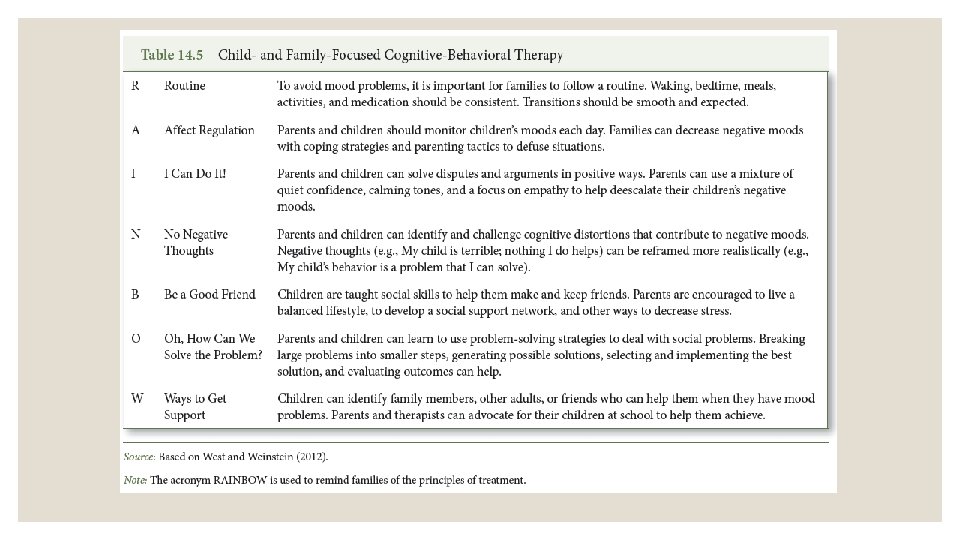
THERAPEUTIC INTERVENTIONS ◦ Psychosocial interventions: ◦ Children can benefit from therapy that focuses on social skills ◦ Family therapy

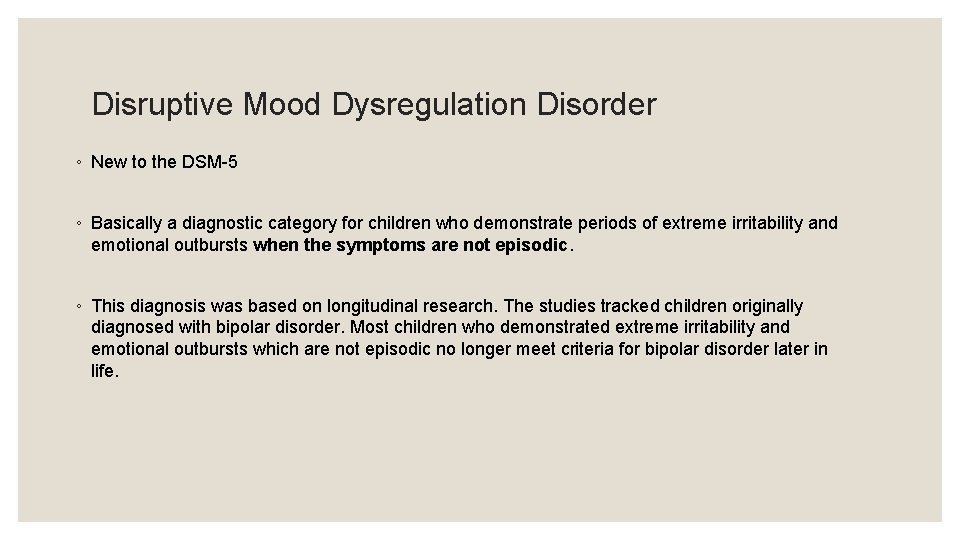
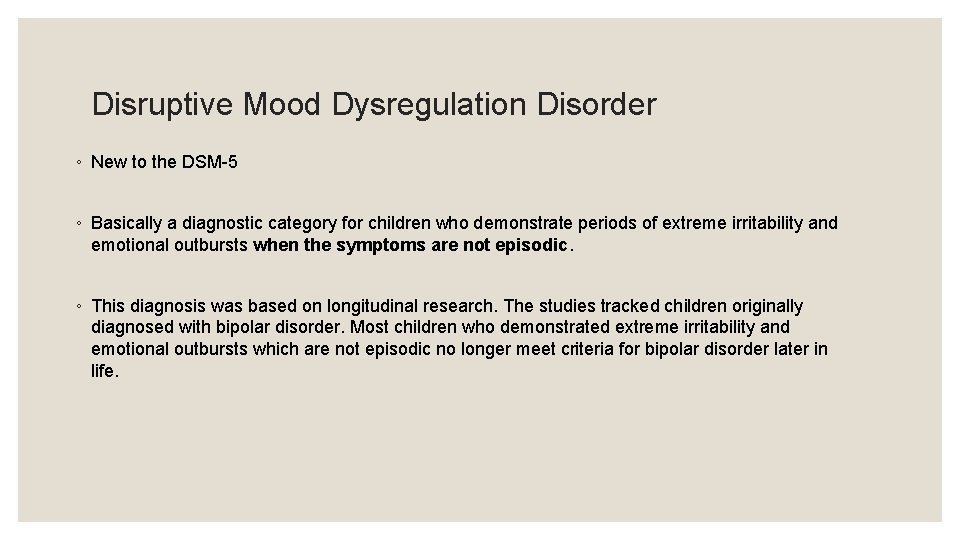
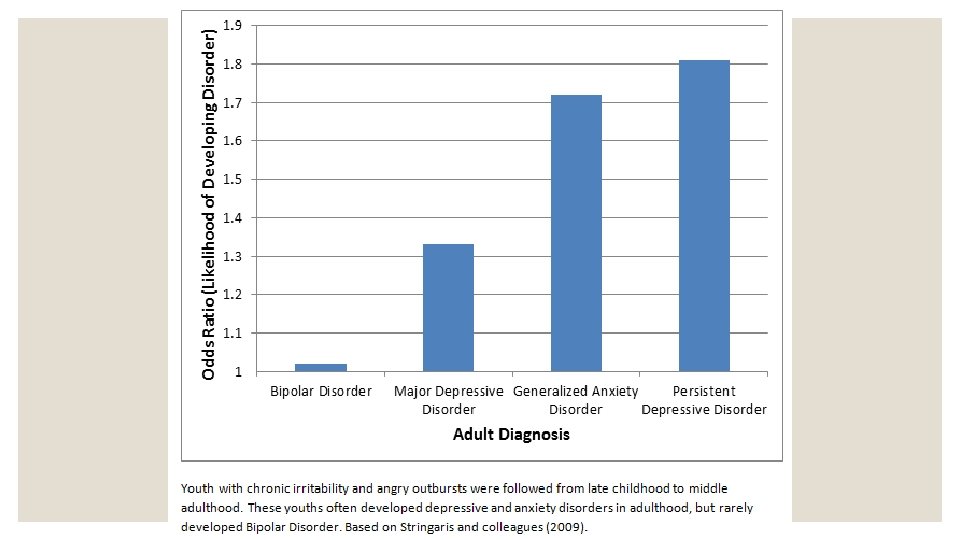
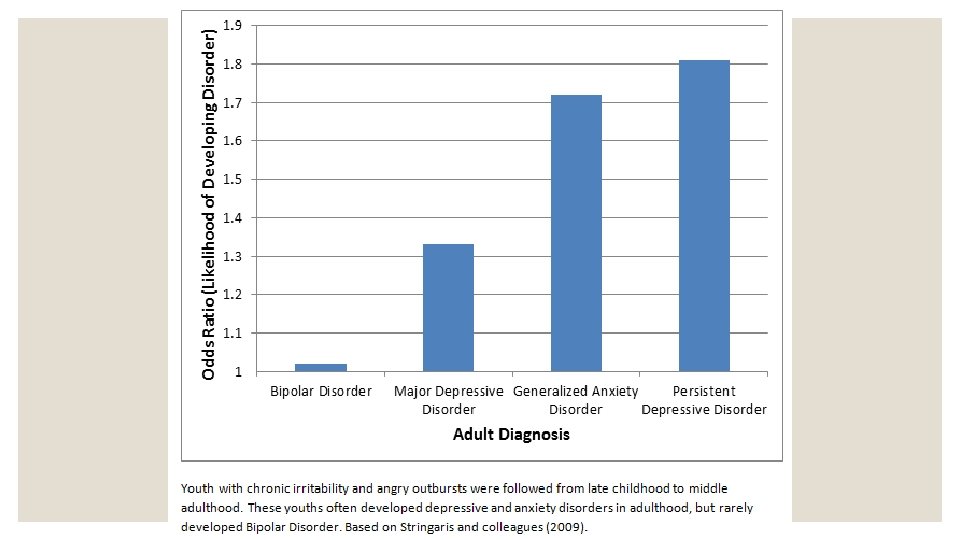
Disruptive Mood Dysregulation Disorder ◦ New to the DSM-5 ◦ Basically a diagnostic category for children who demonstrate periods of extreme irritability and emotional outbursts when the symptoms are not episodic. ◦ This diagnosis was based on longitudinal research. The studies tracked children originally diagnosed with bipolar disorder. Most children who demonstrated extreme irritability and emotional outbursts which are not episodic no longer meet criteria for bipolar disorder later in life.

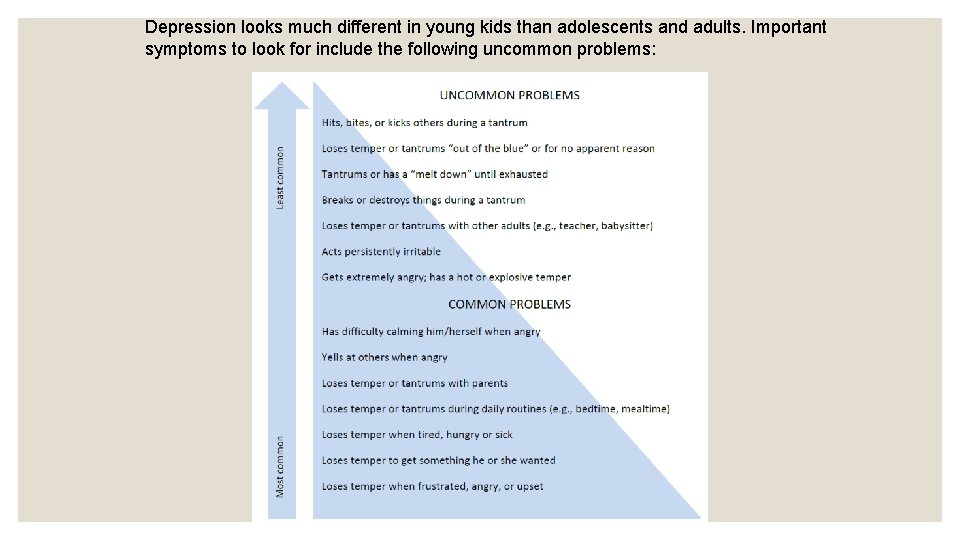
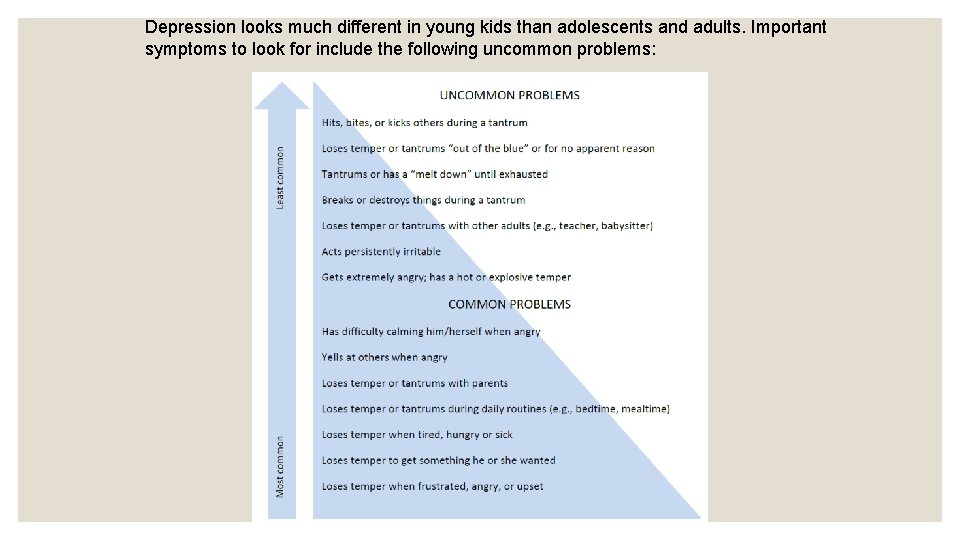
Depression looks much different in young kids than adolescents and adults. Important symptoms to look for include the following uncommon problems:
