Chapter 18 Mood Disorders Depression Depressive Disorders Major




- Slides: 29
Chapter 18 Mood Disorders: Depression
Depressive Disorders • Major depressive disorder (MDD) – Potential for pain and suffering in all aspects of life – Fourth leading cause of disability in the U. S. – Affects children, teenagers, adults, elderly – Symptoms may include psychotic, catatonic, melancholic, postpartum, and seasonal features • Dysthymic disorder (DD) – Chronic depressed mood • > 1 year for children and adolescents • > 2 years for adults and elderly • At risk for developing major depressive episodes and other psychiatric disorders
Theories • Depression may result from a complex interaction of causes as evidenced by high variability of: – Symptoms – Response to treatment – Course of illness • Four common theories – – Biological Psychodynamic influences and life events Cognitive theories Learned helplessness
Biological Theories • Genetics – Genetic factors must interact with environmental factors for depression to develop • Biochemical – Neurotransmitters • Serotonin, norepinephrine, dopamine, acetylcholine, GABA • Basis of effectiveness of antidepressants
Psychodynamic Theory • Psychosocial stressors and interpersonal events trigger neurophysical and neurochemical changes in the brain that result in exaggerated stress response • Forms the basis for anxiety and mood disorders
Cognitive Theory • Aaron Beck: Early life experiences lead to negative, illogical thought processes that predispose the individual to depression. • Beck’s Cognitive Triad: – Negative view of self – Negative view of the world – Negative view of the future

Cognitive-Behavioral Therapy (CBT) • Premise: Negative thinking leads to negative feelings • Goal: Change the way client thinks about self, the world, and his/her future • Three steps – Identify and test negative thoughts – Develop alternative ways of thinking – Rehearse new ways of thinking and behaving
Learned Helplessness • Martin Seligman’s theory of learned helplessness • Initial anxiety is replaced by depression if the individual feels that he/she has no control over the outcome of the situation. • In part explains high rate of depression in the elderly, minority groups, and women
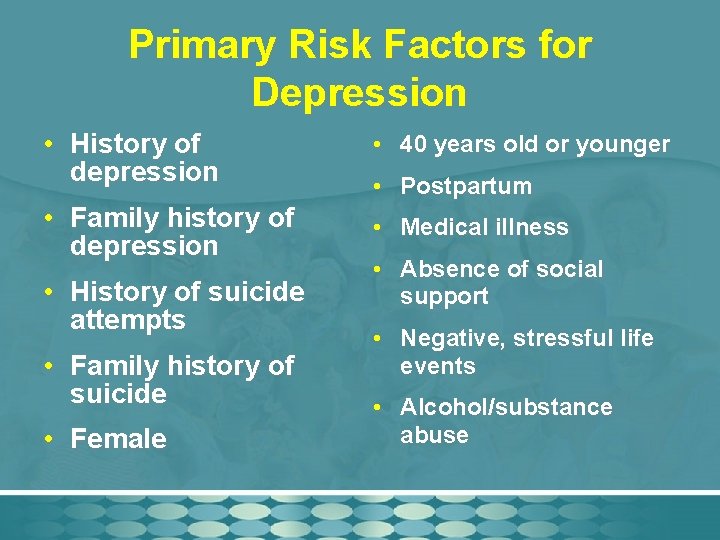
Primary Risk Factors for Depression • History of depression • 40 years old or younger • Family history of depression • Medical illness • History of suicide attempts • Family history of suicide • Female • Postpartum • Absence of social support • Negative, stressful life events • Alcohol/substance abuse
Untreated Depression • “Undiagnosed and untreated depression is often associated with more severe presentation of depression, greater suicidality, somatic problems, and severe anxiety or anxiety disorders” (text, p. 333).
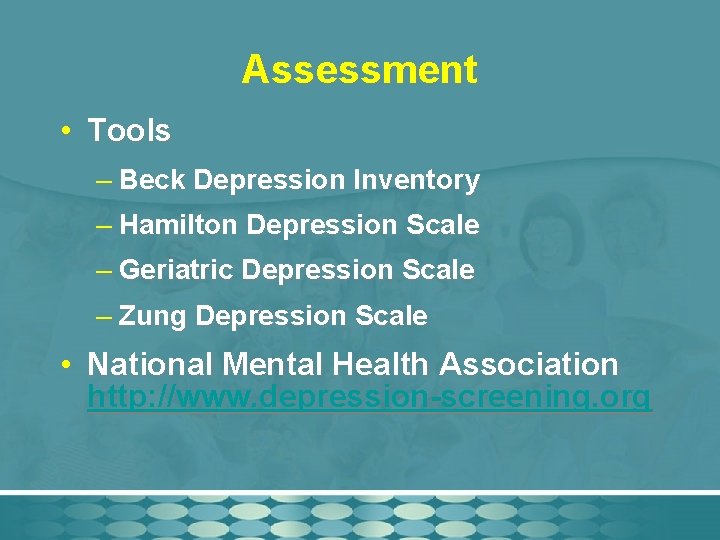
Assessment • Tools – Beck Depression Inventory – Hamilton Depression Scale – Geriatric Depression Scale – Zung Depression Scale • National Mental Health Association http: //www. depression-screening. org
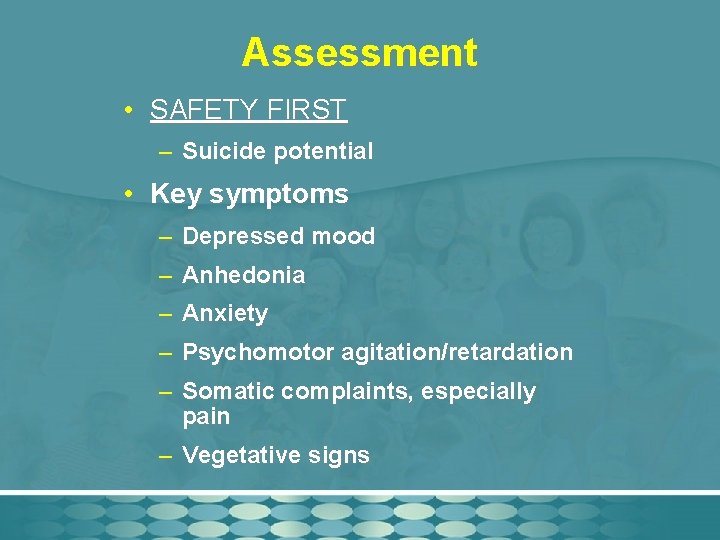
Assessment • SAFETY FIRST – Suicide potential • Key symptoms – Depressed mood – Anhedonia – Anxiety – Psychomotor agitation/retardation – Somatic complaints, especially pain – Vegetative signs
Areas to Assess • Affect: hopelessness, despair • Thought processes: suicidality • Feelings: anxiety, anger • Guilt • Physical behavior • Communication: slowed
Self-Assessment of the Nurse • Unrealistic expectations for the client and oneself • Feeling what the client is feeling • Alter problematic response to client by understanding depression as a systemic illness with a complex etiology
Potential Nursing Diagnoses • Risk for suicide • Hopelessness • Powerlessness • Disturbed thought process • Ineffective coping
Outcome Criteria: Concrete and Measurable • Remains safe • Reports hope for future • Identifies precursors of depression • Reports improved mood • Plans strategies to reduce effects of precursors of depression
Interventions • Acute phase: 6 -12 weeks – Reduction of symptoms – Resumption of psychosocial functioning • Continuation phase: 4 -9 months – Prevention of relapse • Maintenance phase: 1 or more years – Prevention of future episodes

Basic Level Interventions • Communication • Counseling • Encourage self-care activities • Maintain therapeutic milieu • Health teaching • Administer medications per physician/ advanced practice nurse • Assess effects of medications

Advanced Practice Interventions • Psychotherapy – Cognitive-behavioral therapy • As effective as medication – Interpersonal therapy • Social skills training – Assertiveness, coping skills • Group therapy
Best Treatment • “The combination of specific psychotherapies (e. g. , CBT, IPT, behavioral) and antidepressant therapy is superior to either psychotherapy or psychopharmacological treatment alone” (text, p. 342).
Psychopharmacology • Classes of antidepressants – First-line agents • Selective serotonin reuptake inhibitors (SSRIs) • Newer atypical antidepressants • Tricyclic antidepressants (TCAs) – Second-line interventions • Monoamine oxidase inhibitors (MAOIs) • Electroconvulsive therapy (ECT)
Antidepressants • Improvement in mood may take 1 -3 weeks or longer • New FDA warning in 2004 RE: possibility of worsening depression and suicidality • Because all antidepressants work equally well, chosen medication based on side effects, ease of administration, past response, safety & medical factors, and subtype of depression. • May precipitate manic episode in person with bipolar disorder

SSRIs • Selectively block neuronal reuptake of serotonin • First-line therapy for most types of depression • Reduced anticholinergic and cardiac effects • Side effects: agitation, anxiety, sleep and sexual disturbance, tremor, headache • Potential toxic effect: Central Serotonin Syndrome
Newer Atypical Antidepressants • Neurotransmitters – Selective serotonin-norepinephrine reuptake inhibitors (SNRIs) • Effexor, Remeron, Cymbalta – Selective norepinephrine reuptake inhibitors (NRI) • None approved yet in the U. S. • Advantages: target unique subtypes of depression
Tricyclic Antidepressants (TCAs) • Inhibit the reuptake of norepinephrine and serotonin by presynaptic neurons • May take 4 -8 weeks to work – Early improvement in sleep and appetite • Adverse effects: anticholinergic and cardiac effects • “Start low, go slow”
Monoamine Oxidase Inhibitors • Increase norepinephrine, serotonin, dopamine, tyramine • Particularly effective for atypical depression • Require special diet low in tyramine • Numerous adverse effects – Most serious: Hypertensive Crisis – See table 18 -5 on page 350.
ECT • High rate of effectiveness yet underutilized • Used for depression, bipolar disorder, schizophrenia • Usually 2 -3 treatments per week for 3 weeks • Can cause temporary confusion or memory loss • Maintenance ECT once weekly or once monthly
Integrative Approaches • Light therapy – Seasonal affective disorder (SAD) • St. John’s Wort – Can interact with other antidepressants, causing Central Serotonin Syndrome – Avoid tyramine-containing foods • Exercise • Transcranial magnetic stimulation (TMS) – Serious, relapsing medication-resistant depression
Evaluation • Evaluate outcomes related to suicidality, thought processes, selfesteem, and social interaction • Reassess and modify care plan as indicated