Module III Returning To School 1 Module III










- Slides: 56
Module III ___________________________ Returning To School 1
Module III Goal ___________________________ • To provide information that will facilitate the successful return of students with TBI to their schools 2
Module III Learning Outcomes ___________________________ • At the end of this module you will: – Understand the responsibilities of hospital and school in school re-entry planning – Be familiar with the IEP team process for students with TBI – Recognize common problems of students with TBI – Be able to plan an evaluation of a student with TBI 3
Transition to School ___________________________ • Preparing for transition to school begins at the time of injury 4
Transition to School ___________________________ • What can the medical facility do? • What can the educational facility do? 5
School Re-entry Planning: Whose responsibility is it? ____________________________ • Responsibilities of school staff and medical staff shift over time • Medical staff: assumes leadership for patient care in the hospital • Educational staff: takes more responsibility for school planning as needs are known and discharge nears • The family is involved throughout 6
Three Stages of School Re-entry Planning ___________________________ • At the time of injury • During the hospital/rehabilitation stay • Prior to discharge 7
Strategies for the Medical Facility ___________________________ • At the time of the injury – Identify a medical contact person (e. g. , care coordinator or social worker) • During hospitalization – Provide updates on progress and needs – Arrange for hospital visits for school staff – Educate family and school staff – Refer for special education if need is suspected 8
Strategies for the Medical Facility (cont. ) ___________________________ • Prior to discharge – Inform family and school of discharge date – Provide discharge summary – Participate in IEP team if possible – Establish and communicate follow-up and reevaluation schedule 9

Re-entry Strategies for Schools ___________________________ • At the time of the injury – As soon as you know a student has been injured, designate a school contact person to receive and provide information – Identify the medical contact person 10
Role of the School Contact Person ___________________________ • Be a support to the family • Get appropriate releases signed to share information • Gather information from hospital personnel as it becomes available • Inform others (such as teachers, peers, and siblings’ teachers) as needed 11

Re-entry Strategies for Schools (cont. ) ___________________________ • During hospitalization – Obtain parent’s permission to release/receive information – Request updates from medical contact – Visit student in the hospital – Share information with school staff 12
Re-entry Strategies for Schools (cont. ) ____________________________ • During hospitalization (cont. ) – Refer for special education if appropriate – Educate parents about special education process – Arrange for staff training 13
Re-entry Strategies for Schools (cont. ) ___________________________ • Prior to discharge – Obtain current hospital records – Complete IEP team process before discharge, if possible, but within statutory timeframes. – Collaborate with medical facility to obtain consultation and in-service training 14
Strategies For Successful School Re-entry of Students With TBI ____________________________ • Summary of strategies used by medical and school facilities appears on pages 15 a-15 b. • Which strategies have participants used? • Are there other strategies participants have found helpful in the transition from hospital to school? 15
Transition to School Checklist ____________________________ • The Transition to School Checklist is designed to help school personnel monitor completion of transition activities • Please refer to the Checklist on page 16 a. 16
Transitions also include ___________________________ • • • Transitions between classes Transition to new schools Transition to post school settings Other students See Transition Checklist on p. 17 a 17
The IEP Team Process ____________________________ 1. Refer the student to the LEA 2. Identify IEP Team members 3. Evaluate the student’s eligibility and determine needs 4. Develop the IEP 5. Offer placement 18
1. Refer the student to the LEA ___________________________ • In moderate and severe brain injuries referrals usually occur while the student is hospitalized • As soon as you suspect a student is a child with a disability, inform the parent of your intent to refer, and refer in writing to the LEA 19
2. Identify IEP team members ____________________________ • The IEP Team must include members designated in Chapter 115. 78 • These requirements are reproduced on the next page of your manual • Others with special expertise or knowledge may be included at the discretion of parent or school 20

2. Identify IEP Team Members (cont. ) ___________________________ • Who would you want on Serena’s IEP team? • Who would you want on Monty’s IEP team? 21
3. Evaluate the student’s needs ____________________________ • As part of the evaluation the IEP team: – Reviews existing evaluation data • evaluations and information provided by parents • previous interventions and their effects • current classroom-based assessments and observations • observations by teachers and related services providers 22
3. Evaluate the student’s needs (cont. ) ___________________________ • After review of data the IEP team determines – if additional data are needed, and if so, who should gather it – if child has an impairment – present levels of performance – if child needs SE and related services 23
4. Develop the IEP ___________________________ • If the IEP team determines that the student has an impairment (TBI) and needs special education and related services, the team prepares the Individualized Education Program 24
5. Offer placement ____________________________ • An educational placement is developed to implement the child’s IEP • To the maximum extent appropriate, a child with a disability is educated with nondisabled children (Chapter 115. 79) 25
Designate a case manager ____________________________ • It is best practice to appoint a case manager who coordinates communication among IEP team members 26
What types of problems can the school anticipate? ____________________________ • Serena • Monty • Mike 27
Common Problems of Students with TBI ___________________________ • Certain types of difficulties are common in students with TBI • Anticipating these difficulties can facilitate successful re-entry to school • Problems can be physical/medical, cognitive, sensory, motor, social, emotional, and behavioral 28

Physical/Medical Problems ____________________________ • Problems – – – • • Seizures Fatigue Headaches Swallowing/Eating Self-care activities Medication issues (see p. 29 a) Is an Individualized Health Care Plan (IHCP) needed? (see p. 29 c-d) 29

Common Motor Problems ___________________________ • Apraxia • Ataxia • Coordination problems • Paresis or paralysis • Orthopedic problems • Spasticity • Balance problems • Impaired speed of movement • Fatigue • See p. 30 a 30
Sensory/Perceptual Problems ___________________________ • Visual deficits – field cuts – tracking (moving and stationary objects) – spatial relationships – double vision (diplopia) • Neglect • Auditory deficits • Tactile deficits 31
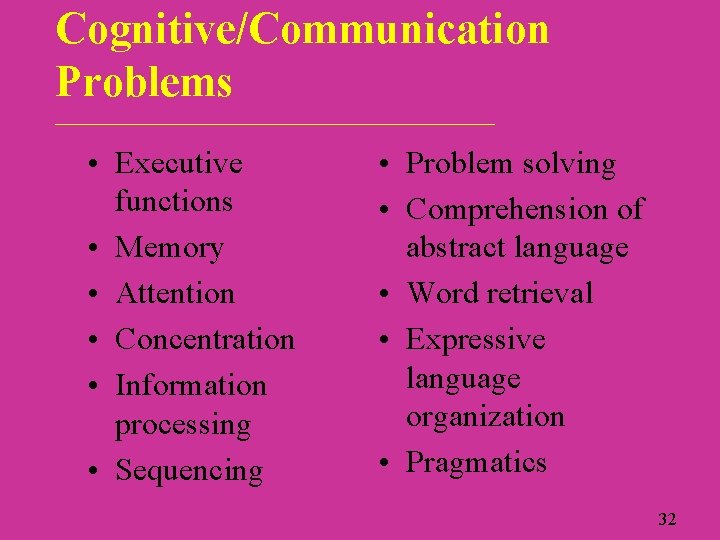
Cognitive/Communication Problems ____________________________ • Executive functions • Memory • Attention • Concentration • Information processing • Sequencing • Problem solving • Comprehension of abstract language • Word retrieval • Expressive language organization • Pragmatics 32

Executive Functions ___________________________ • Planning, prioritizing, sequencing, selfmonitoring, self-correcting, inhibiting, initiating, controlling or altering behavior (Savage & Wolcott, 1995, p. 150) 33
Cognitive/Communication Deficits ____________________________ • See p. 34 a for additional information regarding cognitive/communication problems • See p. 34 b for an example of Monty’s difficulties at school 34
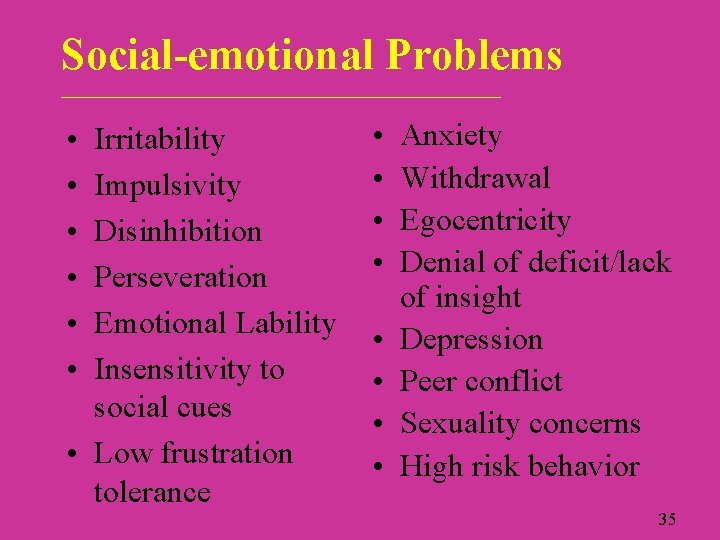
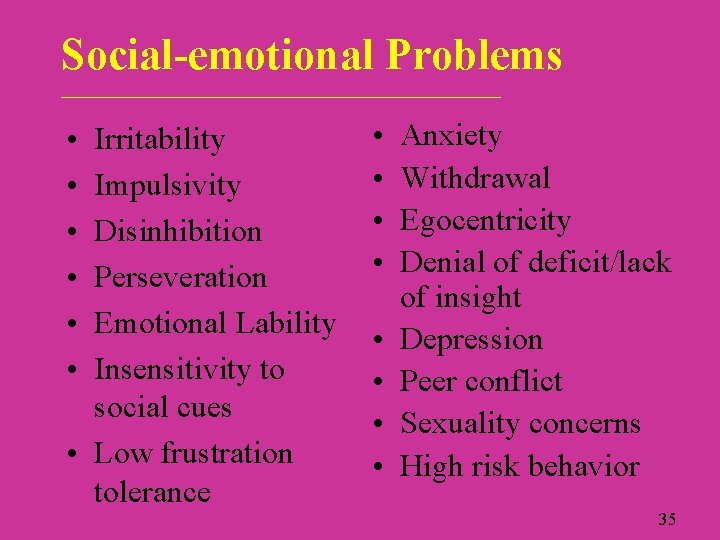
Social-emotional Problems ____________________________ • • • Irritability Impulsivity Disinhibition Perseveration Emotional Lability Insensitivity to social cues • Low frustration tolerance • • Anxiety Withdrawal Egocentricity Denial of deficit/lack of insight Depression Peer conflict Sexuality concerns High risk behavior 35
Social-emotional Problems _______________________________ • See p. 36 a for descriptions of socialemotional deficits • See p. 36 b for an example of Serena’s difficulties at school 36

Behavioral Problems ___________________________ • Deficits (all types) may lead to challenging behaviors – non-compliance – aggression – confrontational behavior – lack of initiative – withdrawal 37
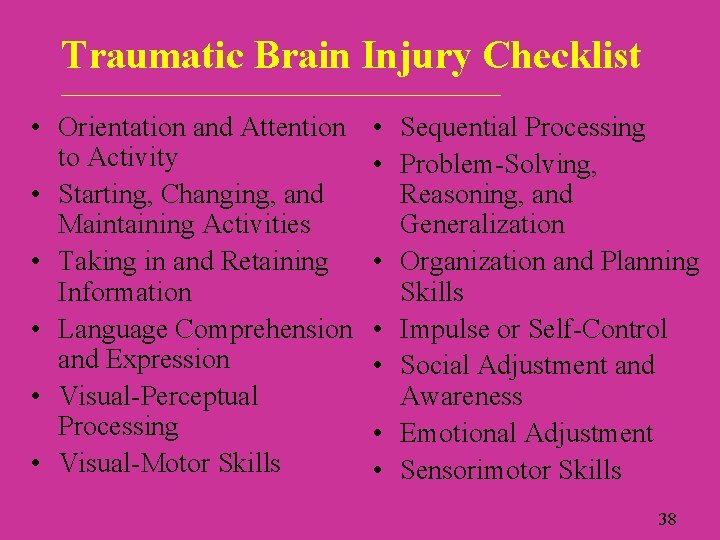
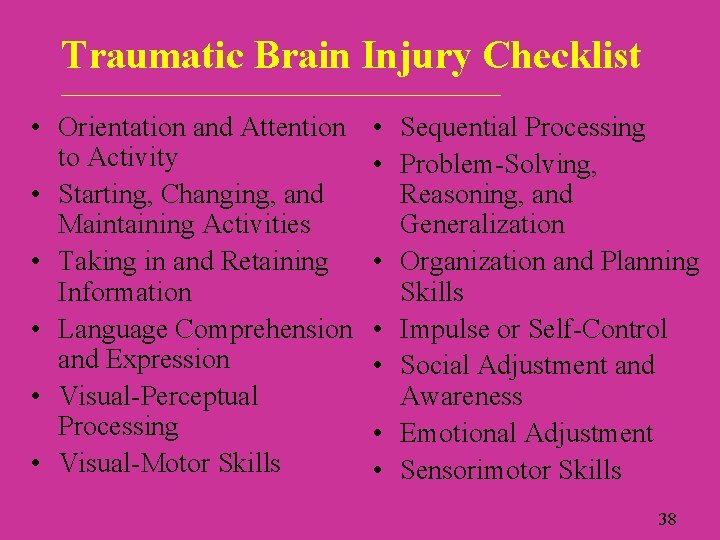
Traumatic Brain Injury Checklist ____________________________ • Orientation and Attention to Activity • Starting, Changing, and Maintaining Activities • Taking in and Retaining Information • Language Comprehension and Expression • Visual-Perceptual Processing • Visual-Motor Skills • Sequential Processing • Problem-Solving, Reasoning, and Generalization • Organization and Planning Skills • Impulse or Self-Control • Social Adjustment and Awareness • Emotional Adjustment • Sensorimotor Skills 38

Manifestations of TBI by Age _____________________________ • Preschool – Irritability and crying – Temper tantrums – Frustration – Fearfulness – Disabilities become evident over time as higher level skills are expected to develop 39
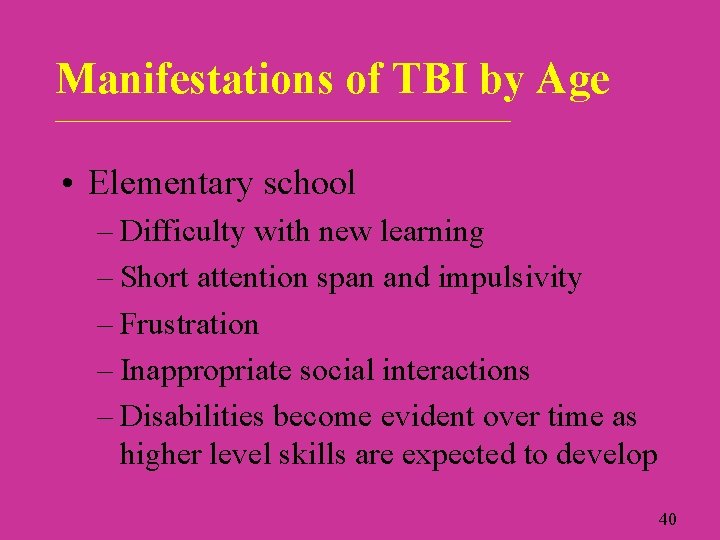
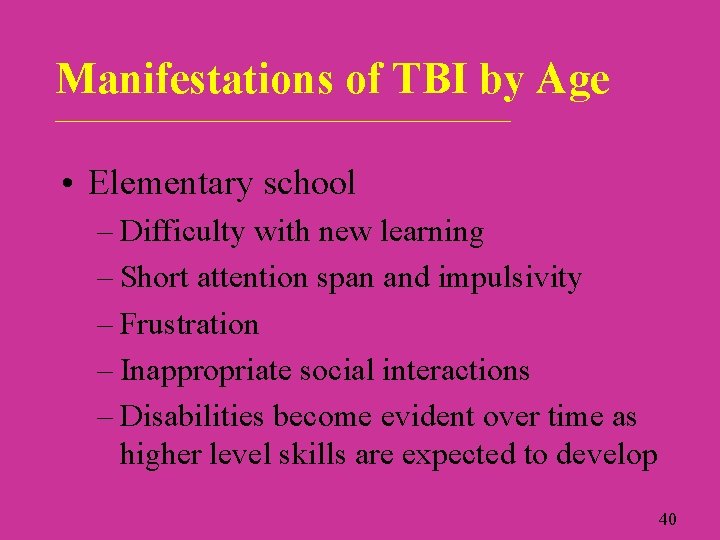
Manifestations of TBI by Age _____________________________ • Elementary school – Difficulty with new learning – Short attention span and impulsivity – Frustration – Inappropriate social interactions – Disabilities become evident over time as higher level skills are expected to develop 40

Manifestations of TBI by Age ____________________________ • Middle school and high school – Difficulty with new learning – Short attention span and impulsivity – Frustration over skill losses – Decreased social judgment – Risk-taking – Depression and anxiety – Sexuality concerns – Effects of earlier injury become evident 41
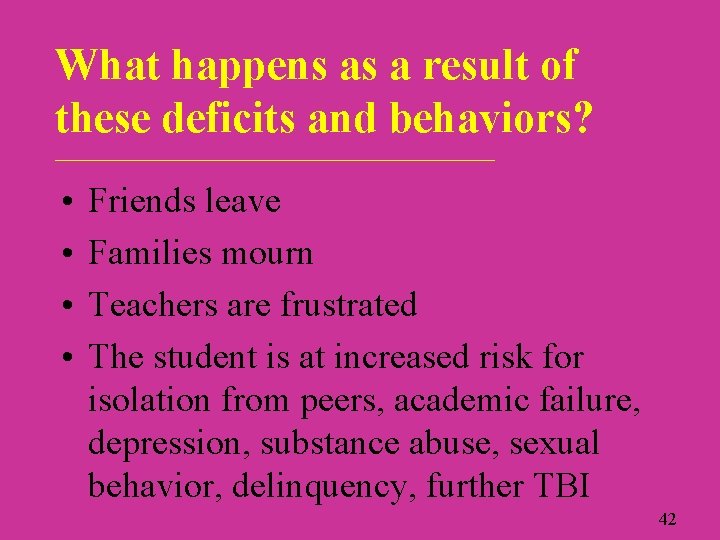
What happens as a result of these deficits and behaviors? ____________________________ • • Friends leave Families mourn Teachers are frustrated The student is at increased risk for isolation from peers, academic failure, depression, substance abuse, sexual behavior, delinquency, further TBI 42
Evaluation of students with TBI ____________________________ Two purposes: • Identification of a student as a student with a disability • Program planning 43
Evaluation Planning ___________________________ • Where do you begin after a referral is made? • What do you need to know about the student to determine eligibility for special education and related services and to develop an IEP? 44
Information to Determine Needs ____________________________ • TBI information • Information about areas of functioning – Cognition and memory – Speech and language; communication – Sensory and perceptual abilities – Motor abilities – Psychosocial impairments – Physical functions/safety – Academic skills 45
Challenges to Evaluation for Programming ___________________________ • What factors make evaluation of the programming needs of students with TBI challenging? 46
Challenges to Evaluation for Programming: Student Factors ___________________________ • Rapidly changing skills (especially during first 6 -12 months) • Communication, physical, sensory, motor, emotional, and behavioral difficulties may interfere with assessment • Uneven skill profile (some higher skills preserved with lower skills lost) • Performance influenced by state and situation • Problems may emerge later 47
Challenges to Evaluation for Programming: Other Factors ___________________________ • The family is probably in distress • Initial assessment is probably conducted outside school in a setting unlike the classroom • Much assessment information is needed from other professionals (who are busy) • Medical reports may be difficult to interpret • Assessment requires IEP team coordination and planning 48
What can be done to address these challenges? ____________________________ • Use classroom data to inform instruction • Use observation, curriculum-based measures, work samples, trial teaching • Assess across content, time, settings • Invite parents to provide information • Ask medical personnel for assistance • Plan team evaluations • Share information 49
Teamwork: The Family and the School Staff ___________________________ • Parent(s) and educators work together • Educators recognize and respect the expertise, values, and concerns of the family • The family recognizes and respects the skills of educators • Communication is frequent and honest 50
TBI Evaluation Planning: Group Activity ___________________________ • Refer to the TBI Evaluation Planning worksheet on pages 51 a and b • Monty and Serena have been referred for evaluation for special education. What do you know? What do you need to find out? 51

How Can I Gather Additional Information? ____________________________ • • Record review (school and medical) Direct observation (school or hospital) Student interview (if possible) Teachers/service provider interviews Criterion-referenced assessment Curriculum-based assessment Rating scales and checklists Neuropsychological assessment (if available) 52
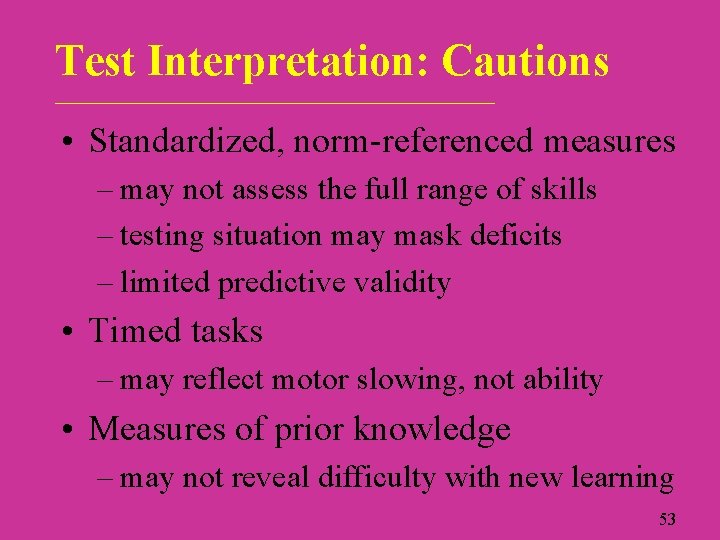
Test Interpretation: Cautions ____________________________ • Standardized, norm-referenced measures – may not assess the full range of skills – testing situation may mask deficits – limited predictive validity • Timed tasks – may reflect motor slowing, not ability • Measures of prior knowledge – may not reveal difficulty with new learning 53
What does Wisconsin law require in evaluations for special education? ___________________________ • See Chapter 115. 782 on pages 54 a and 54 b 54
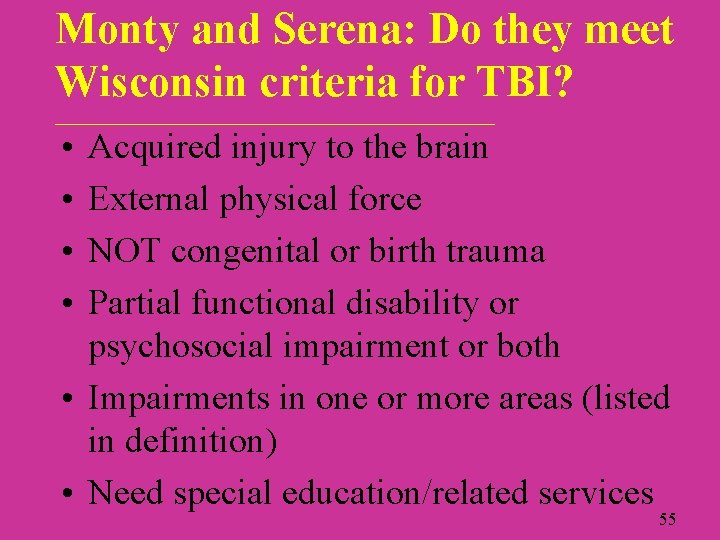
Monty and Serena: Do they meet Wisconsin criteria for TBI? ____________________________ • • Acquired injury to the brain External physical force NOT congenital or birth trauma Partial functional disability or psychosocial impairment or both • Impairments in one or more areas (listed in definition) • Need special education/related services 55
End of Module III 56