Module 2 Quality and Quality Measures Definition of

- Slides: 14
Module 2: Quality and Quality Measures Definition of Quality The degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge. Source: Crossing the Quality Chasm: A New Health System for the 21 st Century. Institute of Medicine, 2001.
Types of Measures in Health Care Quality (Donabedian) • Structure • Process • Outcome

Dimensions of Quality • • • Safety Effectiveness Patient-Centeredness Timeliness Efficiency Equity
Criteria for a Good Quality Measure (National Quality Forum) • • Importance Scientific Acceptability Useable Feasible
Let’s walk one of your examples down the trail and visit these criteria.
Importance to Measure and Report • Addresses – 1) accepted health goal, or – 2) high impact area • • Large numbers, leading cause of morbidity or mortality. Significant resource utilization. High severity. Patient/societal consequences. • Associated with Quality Problems and Opportunities for Improvement
Importance to Measure & Report (Continued) • Focus is – An outcome (morbidity, mortality, function, Qo. L); or – An intermediate outcome (Hb. A 1 c) with causal linkage to outcome; or – A process with evidence; or – A structure consistent delivery of effective care or access; or – A patient experience linked to outcomes, values or preferences; or – Access to effective care; or – Efficiency
Scientific Acceptability of Measure Properties • Potential for consistent implementation. • Reliable (Test-retest at population level). • Valid (measures what it is supposed to). – criterion, construct, predictive, content, and face. • Exclusions specified and justified. • Risk adjusted as appropriate. • Ability to detect statistically and clinically significant differences over time, between sites. • Ability to identify disparities.
Usability • Understandable and useful to intended audiences. • Aligned or in harmony with other measures in use. • Adds value to existing measures.
Feasible • Routinely generated as part of care process. • Available electronically. • Exclusions should not require additional data sources. • Minimum but understood susceptibility to errors. • Data collection strategy feasible.
What makes for a good list of indicators? • Pareto Principle: Law of the Vital Few • Comprehensive Measurement—List of indicators tap into all of the required dimensions. – Structure – Process – Outcome Donabedian
What about combining individual indicators? Composites and Bundles • All-or-none scoring. – Patient meets all indicators in the list (yes, no, NA). • Patient average method. – Number of indicators in the list that the patient meets. • Indicator average. – The average of indicators calculated separately. Notes: see Reeves DR et al. Combining multiple indicators of clinical quality: An evaluation of different analytic approaches. Medical Care 2007; 45(6): 489 -496.
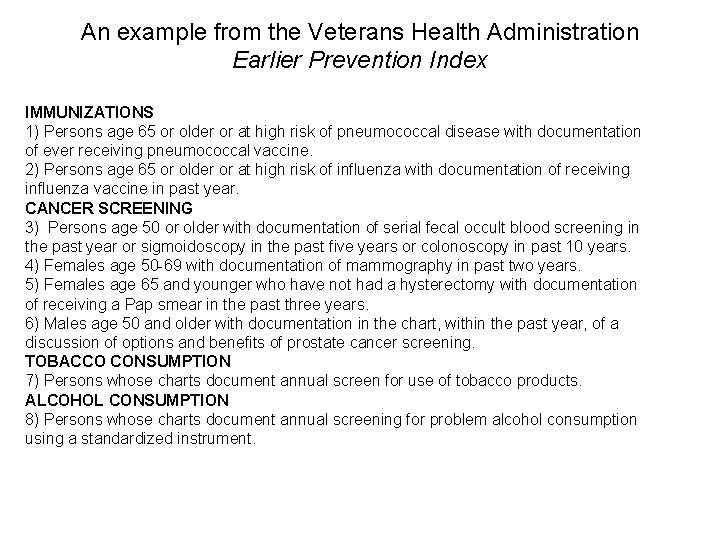
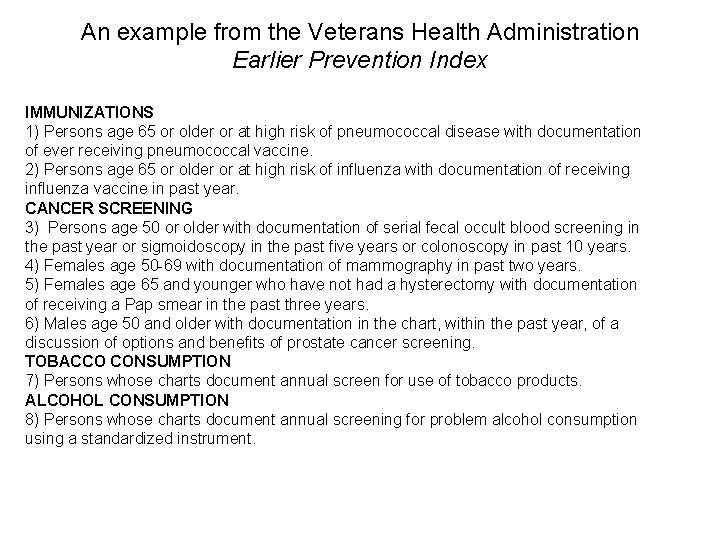
An example from the Veterans Health Administration Earlier Prevention Index IMMUNIZATIONS 1) Persons age 65 or older or at high risk of pneumococcal disease with documentation of ever receiving pneumococcal vaccine. 2) Persons age 65 or older or at high risk of influenza with documentation of receiving influenza vaccine in past year. CANCER SCREENING 3) Persons age 50 or older with documentation of serial fecal occult blood screening in the past year or sigmoidoscopy in the past five years or colonoscopy in past 10 years. 4) Females age 50 -69 with documentation of mammography in past two years. 5) Females age 65 and younger who have not had a hysterectomy with documentation of receiving a Pap smear in the past three years. 6) Males age 50 and older with documentation in the chart, within the past year, of a discussion of options and benefits of prostate cancer screening. TOBACCO CONSUMPTION 7) Persons whose charts document annual screen for use of tobacco products. ALCOHOL CONSUMPTION 8) Persons whose charts document annual screening for problem alcohol consumption using a standardized instrument.
Think—Pair—Share Questions • How can you combine these indicators? a. All or none? b. Patient Average? c. Indicator Average? • Name two advantages of the indicator average method or the all-or-none method.