Mental Health Awareness Dr Sheila Hardy Senior Research





- Slides: 63

Mental Health Awareness Dr Sheila Hardy , Senior Research Fellow, Northamptonshire Healthcare NHS Foundation Trust, Post graduate educator, The Charlie Waller Memorial Trust
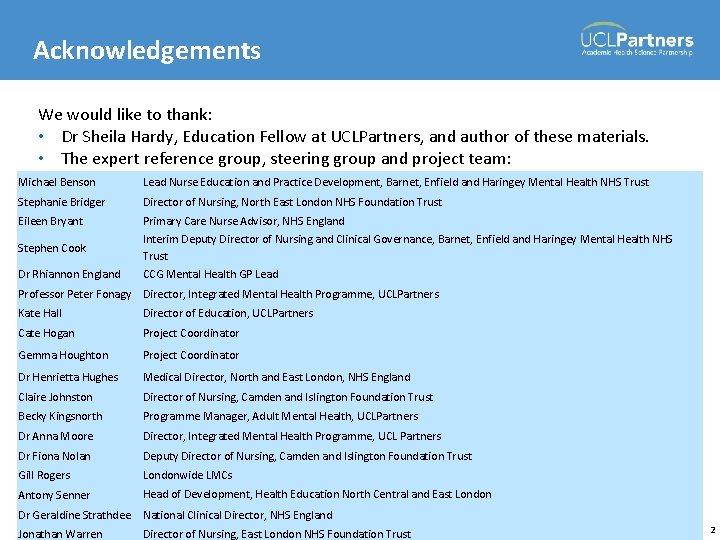
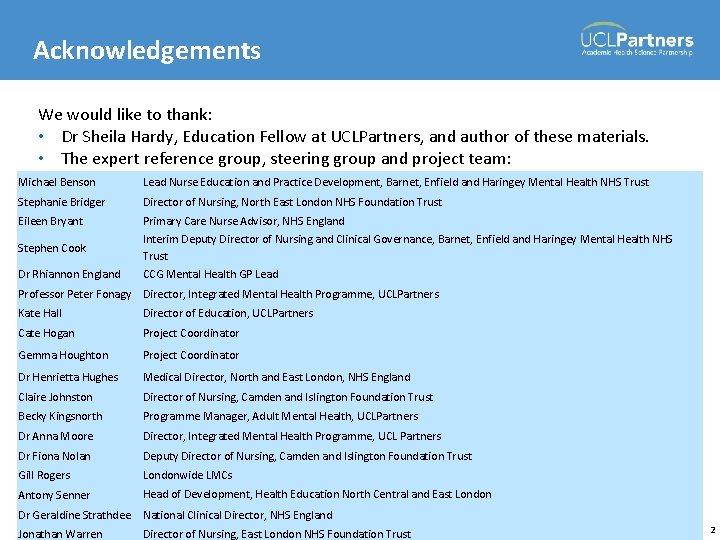
Acknowledgements We would like to thank: • Dr Sheila Hardy, Education Fellow at UCLPartners, and author of these materials. • The expert reference group, steering group and project team: Michael Benson Lead Nurse Education and Practice Development, Barnet, Enfield and Haringey Mental Health NHS Trust Stephanie Bridger Director of Nursing, North East London NHS Foundation Trust Eileen Bryant Primary Care Nurse Advisor, NHS England Stephen Cook Interim Deputy Director of Nursing and Clinical Governance, Barnet, Enfield and Haringey Mental Health NHS Trust Dr Rhiannon England CCG Mental Health GP Lead Professor Peter Fonagy Director, Integrated Mental Health Programme, UCLPartners Kate Hall Director of Education, UCLPartners Cate Hogan Project Coordinator Gemma Houghton Project Coordinator Dr Henrietta Hughes Medical Director, North and East London, NHS England Claire Johnston Director of Nursing, Camden and Islington Foundation Trust Becky Kingsnorth Programme Manager, Adult Mental Health, UCLPartners Dr Anna Moore Director, Integrated Mental Health Programme, UCL Partners Dr Fiona Nolan Deputy Director of Nursing, Camden and Islington Foundation Trust Gill Rogers Londonwide LMCs Antony Senner Head of Development, Health Education North Central and East London Dr Geraldine Strathdee National Clinical Director, NHS England Jonathan Warren Director of Nursing, East London NHS Foundation Trust 2

Introductions 3
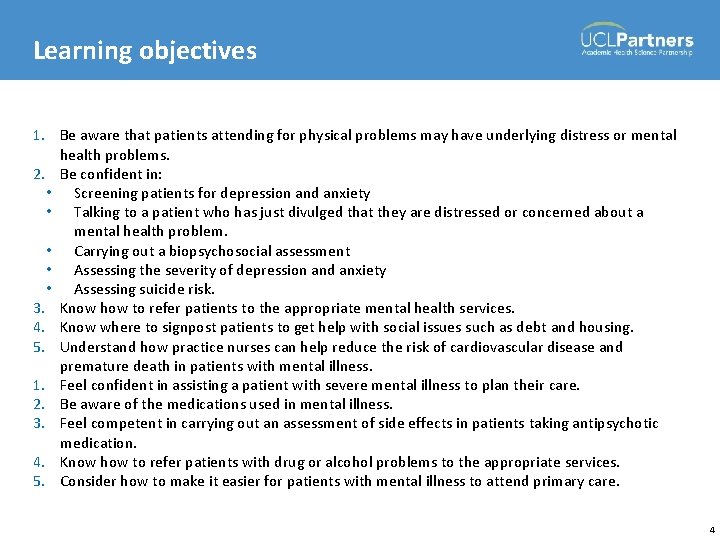
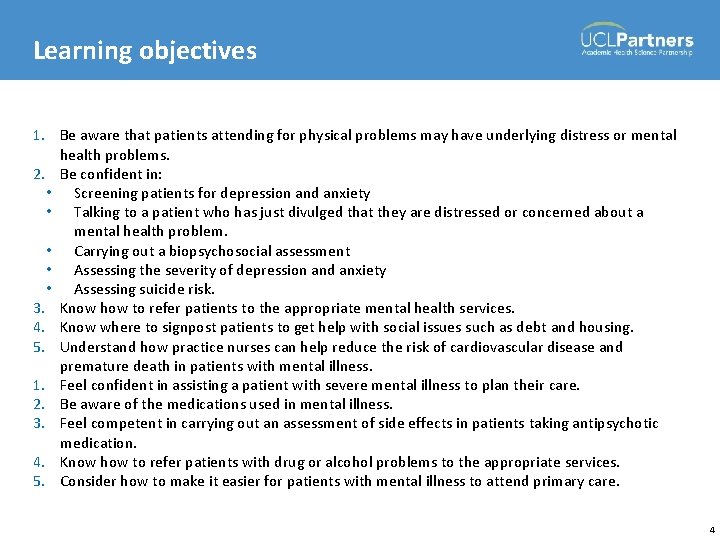
Learning objectives 1. Be aware that patients attending for physical problems may have underlying distress or mental health problems. 2. Be confident in: • Screening patients for depression and anxiety • Talking to a patient who has just divulged that they are distressed or concerned about a mental health problem. • Carrying out a biopsychosocial assessment • Assessing the severity of depression and anxiety • Assessing suicide risk. 3. Know how to refer patients to the appropriate mental health services. 4. Know where to signpost patients to get help with social issues such as debt and housing. 5. Understand how practice nurses can help reduce the risk of cardiovascular disease and premature death in patients with mental illness. 1. Feel confident in assisting a patient with severe mental illness to plan their care. 2. Be aware of the medications used in mental illness. 3. Feel competent in carrying out an assessment of side effects in patients taking antipsychotic medication. 4. Know how to refer patients with drug or alcohol problems to the appropriate services. 5. Consider how to make it easier for patients with mental illness to attend primary care. 4
Underlying distress or mental health problems 5
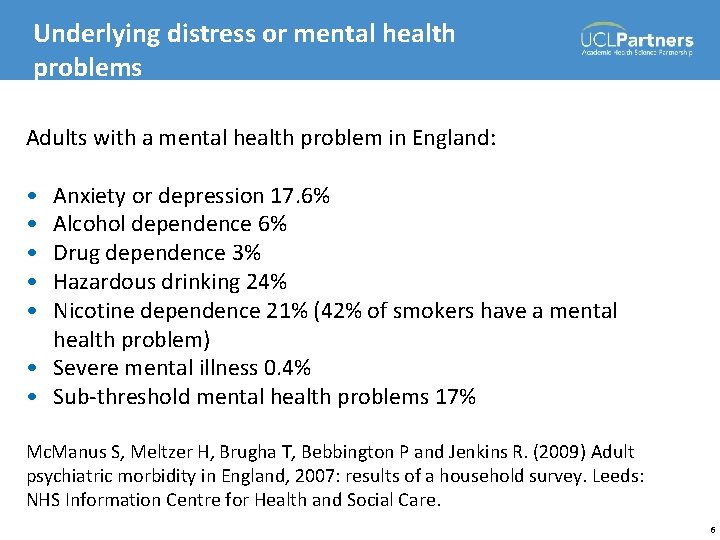
Underlying distress or mental health problems Adults with a mental health problem in England: • • • Anxiety or depression 17. 6% Alcohol dependence 6% Drug dependence 3% Hazardous drinking 24% Nicotine dependence 21% (42% of smokers have a mental health problem) • Severe mental illness 0. 4% • Sub-threshold mental health problems 17% Mc. Manus S, Meltzer H, Brugha T, Bebbington P and Jenkins R. (2009) Adult psychiatric morbidity in England, 2007: results of a household survey. Leeds: NHS Information Centre for Health and Social Care. 6
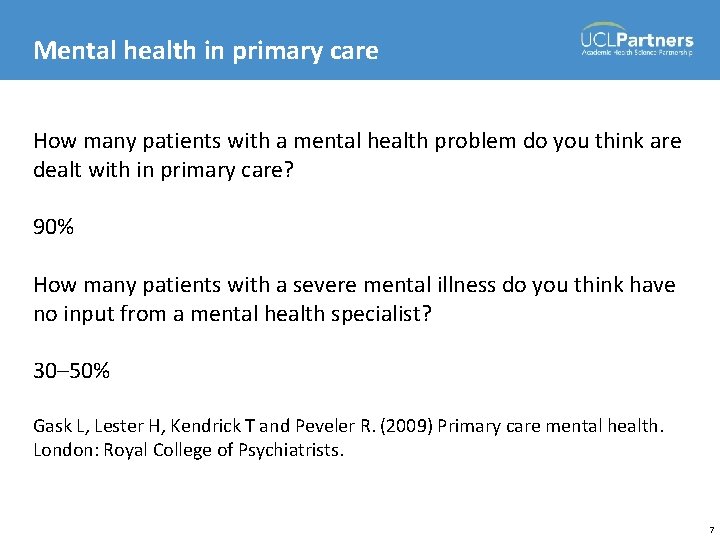
Mental health in primary care How many patients with a mental health problem do you think are dealt with in primary care? 90% How many patients with a severe mental illness do you think have no input from a mental health specialist? 30– 50% Gask L, Lester H, Kendrick T and Peveler R. (2009) Primary care mental health. London: Royal College of Psychiatrists. 7
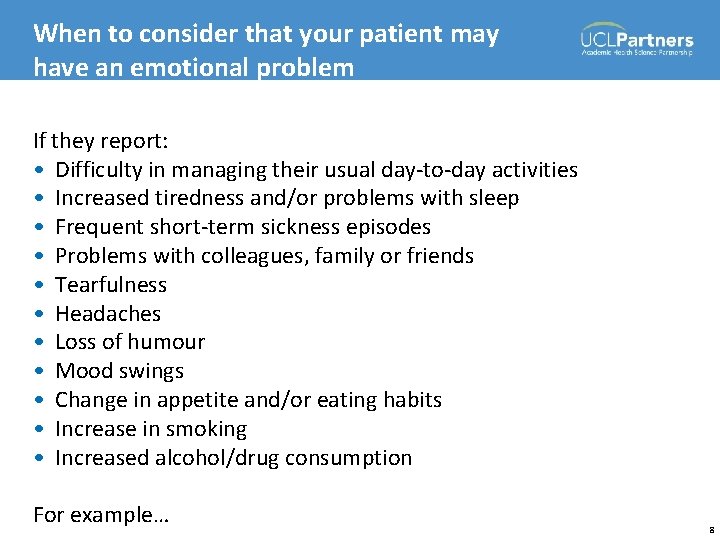
When to consider that your patient may have an emotional problem If they report: • Difficulty in managing their usual day-to-day activities • Increased tiredness and/or problems with sleep • Frequent short-term sickness episodes • Problems with colleagues, family or friends • Tearfulness • Headaches • Loss of humour • Mood swings • Change in appetite and/or eating habits • Increase in smoking • Increased alcohol/drug consumption For example… 8
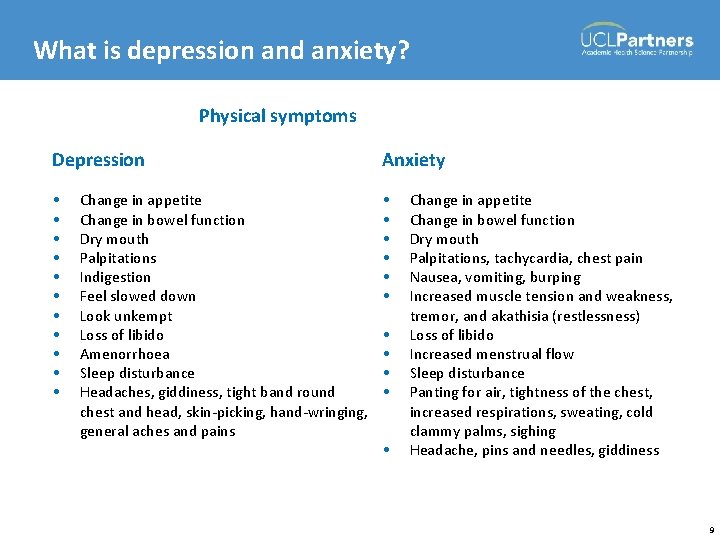
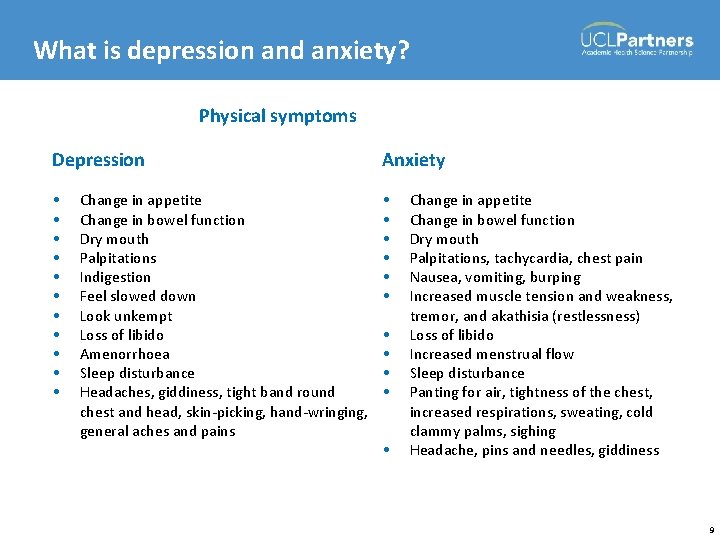
What is depression and anxiety? Physical symptoms Depression Anxiety • • • • • Change in appetite Change in bowel function Dry mouth Palpitations Indigestion Feel slowed down Look unkempt Loss of libido Amenorrhoea Sleep disturbance Headaches, giddiness, tight band round chest and head, skin-picking, hand-wringing, general aches and pains • • • Change in appetite Change in bowel function Dry mouth Palpitations, tachycardia, chest pain Nausea, vomiting, burping Increased muscle tension and weakness, tremor, and akathisia (restlessness) Loss of libido Increased menstrual flow Sleep disturbance Panting for air, tightness of the chest, increased respirations, sweating, cold clammy palms, sighing Headache, pins and needles, giddiness 9
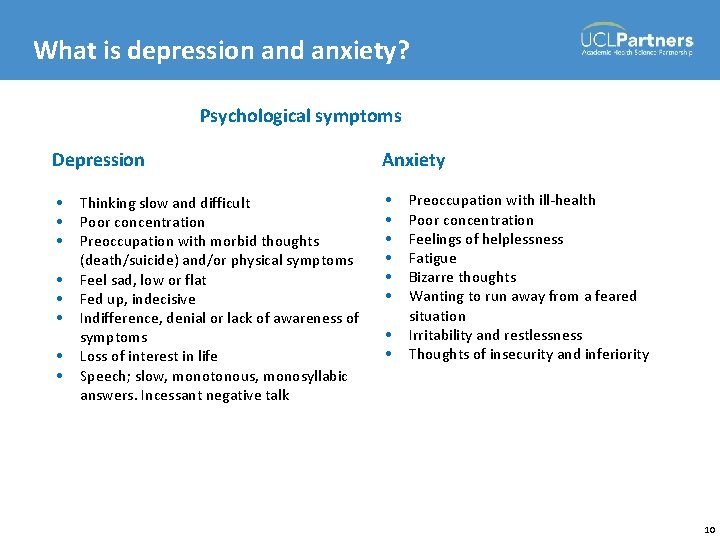
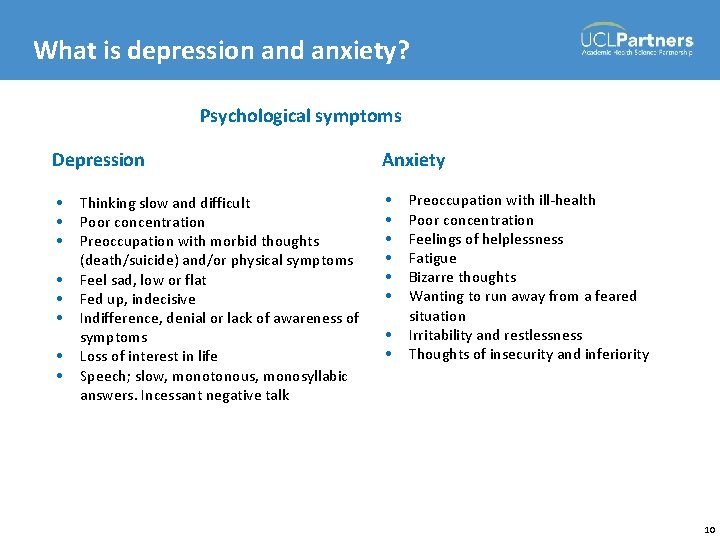
What is depression and anxiety? Psychological symptoms Depression Anxiety • • • • Thinking slow and difficult Poor concentration Preoccupation with morbid thoughts (death/suicide) and/or physical symptoms Feel sad, low or flat Fed up, indecisive Indifference, denial or lack of awareness of symptoms Loss of interest in life Speech; slow, monotonous, monosyllabic answers. Incessant negative talk • • Preoccupation with ill-health Poor concentration Feelings of helplessness Fatigue Bizarre thoughts Wanting to run away from a feared situation Irritability and restlessness Thoughts of insecurity and inferiority 10
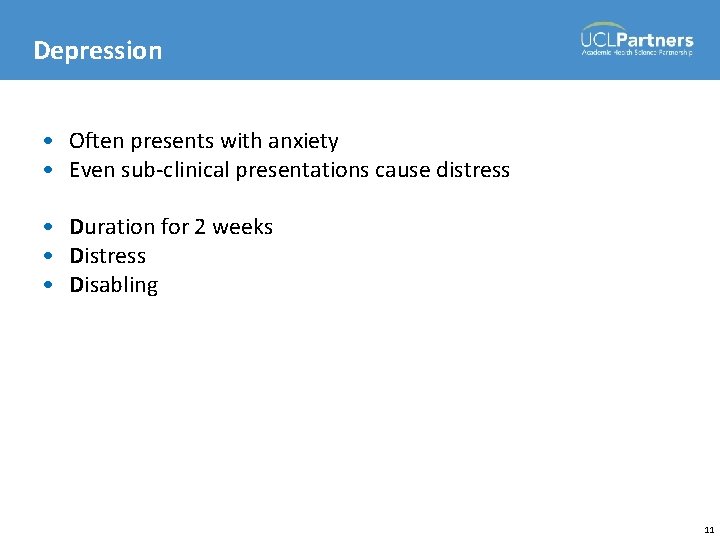
Depression • Often presents with anxiety • Even sub-clinical presentations cause distress • Duration for 2 weeks • Distress • Disabling 11
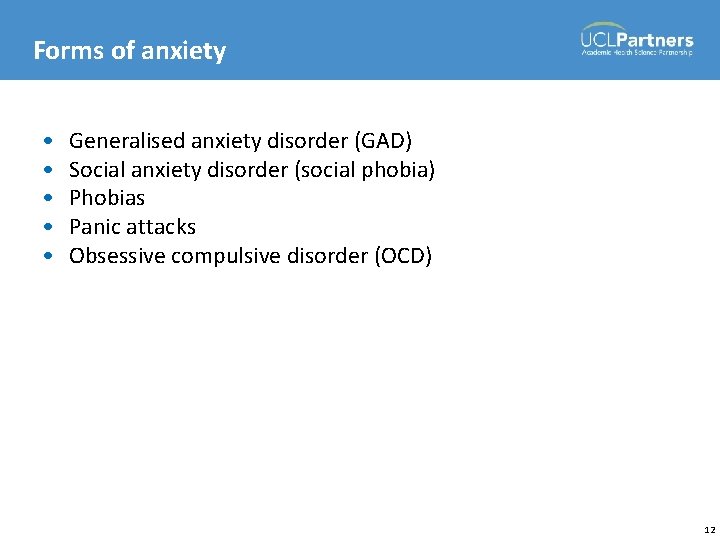
Forms of anxiety • • • Generalised anxiety disorder (GAD) Social anxiety disorder (social phobia) Phobias Panic attacks Obsessive compulsive disorder (OCD) 12
Related modules • Comorbidities: using a psychological approach • Wellbeing 13
Screening for depression and anxiety and supporting patients 14
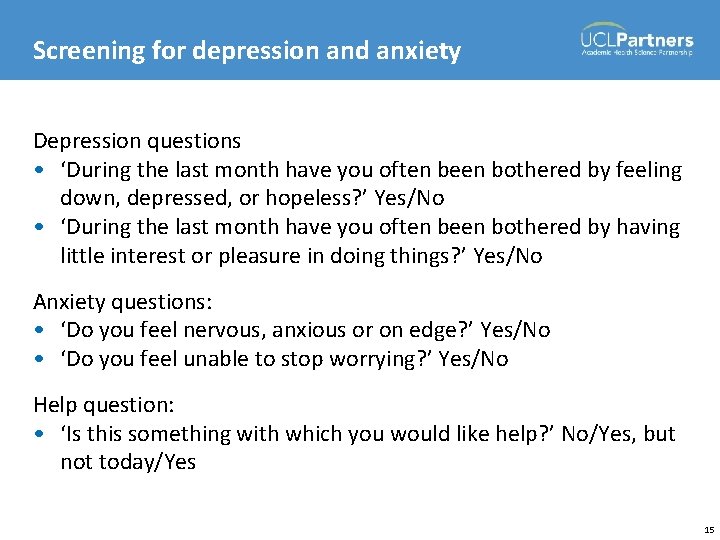
Screening for depression and anxiety Depression questions • ‘During the last month have you often been bothered by feeling down, depressed, or hopeless? ’ Yes/No • ‘During the last month have you often been bothered by having little interest or pleasure in doing things? ’ Yes/No Anxiety questions: • ‘Do you feel nervous, anxious or on edge? ’ Yes/No • ‘Do you feel unable to stop worrying? ’ Yes/No Help question: • ‘Is this something with which you would like help? ’ No/Yes, but not today/Yes 15
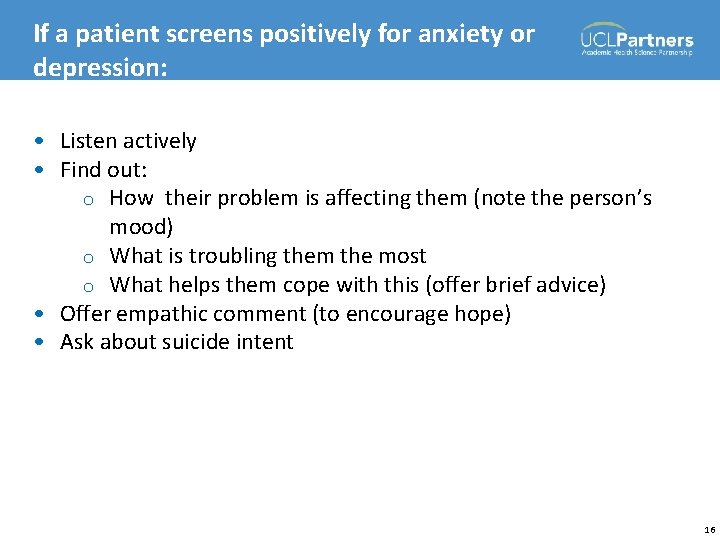
If a patient screens positively for anxiety or depression: • Listen actively • Find out: o How their problem is affecting them (note the person’s mood) o What is troubling them the most o What helps them cope with this (offer brief advice) • Offer empathic comment (to encourage hope) • Ask about suicide intent 16
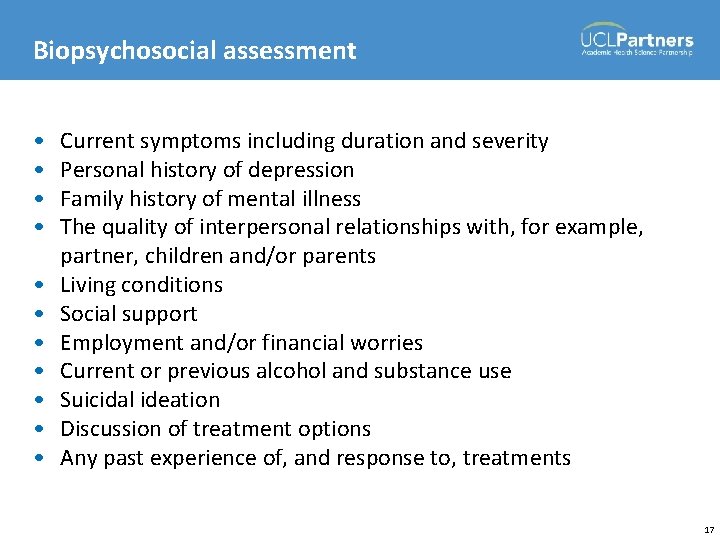
Biopsychosocial assessment • • • Current symptoms including duration and severity Personal history of depression Family history of mental illness The quality of interpersonal relationships with, for example, partner, children and/or parents Living conditions Social support Employment and/or financial worries Current or previous alcohol and substance use Suicidal ideation Discussion of treatment options Any past experience of, and response to, treatments 17
Tools used to make a detailed assessment of depression and/or anxiety Tools validated for primary care: • PHQ-9 (depression) • GAD-7 (anxiety) • HADs (depression and anxiety) • Beck Depression Inventory (depression) 18
People most at risk of suicide • • Family history Previous attempt Underlying mental disorder Long-term physical condition (or pain) Male Young adult or elderly Alcohol or drug abuse Under extreme distress 19
Suicide questions 1. 2. 3. 4. 5. 6. Have you made a suicide attempt in the past? Do you think that life is not worth living? Do you think about harming or killing yourself? Have you got a plan to kill yourself? How would you do it? Do you aim to carry out this plan? Have you got access to (the necessary tools) to carry out the plan? 7. What would stop (or is stopping) you from carrying out your plan? 20
Self-harm Prevalence: • >11% of girls and 3% of boys aged 15– 16 years self-harmed in the previous year (Hawton 2002) • 4. 9% of adults have self-harmed (Mc. Manus et al 2009) Self-harm is intentional damage or injury to the body. It is a way of coping with or expressing overwhelming emotional distress. Causes: • Social factors • Trauma • Mental health conditions Hawton K. (2002) Deliberate self harm in adolescents: Self report survey in schools in England. British Medical Journal 325 (7374): 1207. Mc. Manus S, Meltzer H, Brugha T, Bebbington P and Jenkins R. (2009) Adult psychiatric morbidity in England, 2007: results of a household survey. Leeds: NHS Information Centre for Health and Social Care. 21
Self-harm What to look out for: • • • Cutting or burning their skin Bruising (e. g. from punching themselves) Poisoning themselves with tablets Misusing alcohol or drugs Deliberately starving themselves (anorexia nervosa) or binge eating (bulimia nervosa) • Unexplained injuries • Depression • Low self-esteem Respond as you would when identifying depression and anxiety 22
Services for people with mental health problems 23
Services for people with mental health problems • Primary care • Counselling services • Improving Access to Psychological Therapy (IAPT) • Third sector organisations • Secondary care mental health services 24
Local services 25
National resources Relevant services for people with mental health problems are listed in your manual 26
Related modules • Your patient’s journey (e-learning) 27
Tea break! 28
Severe mental illness (SMI) 29
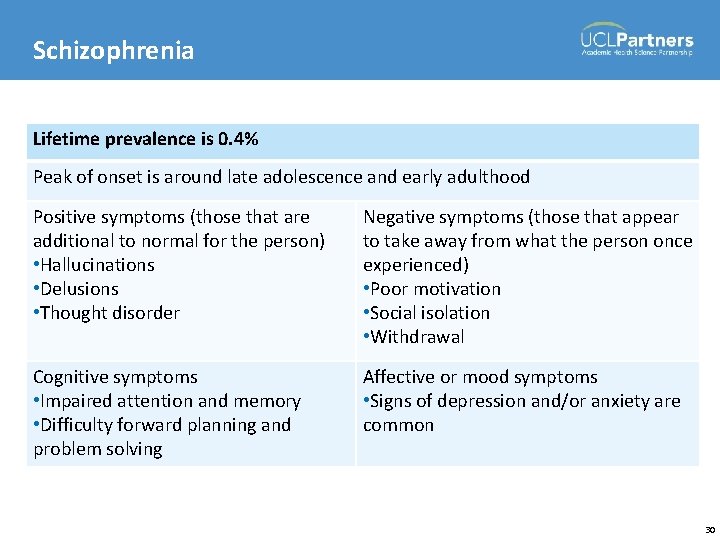
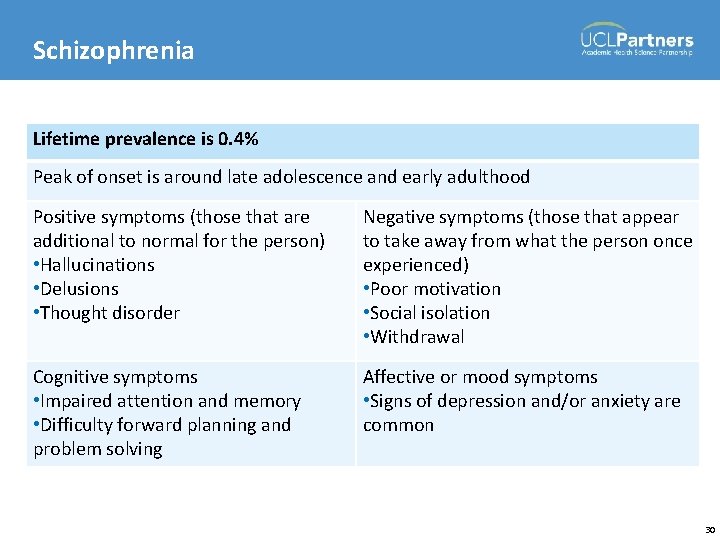
Schizophrenia Lifetime prevalence is 0. 4% Peak of onset is around late adolescence and early adulthood Positive symptoms (those that are additional to normal for the person) • Hallucinations • Delusions • Thought disorder Negative symptoms (those that appear to take away from what the person once experienced) • Poor motivation • Social isolation • Withdrawal Cognitive symptoms • Impaired attention and memory • Difficulty forward planning and problem solving Affective or mood symptoms • Signs of depression and/or anxiety are common 30
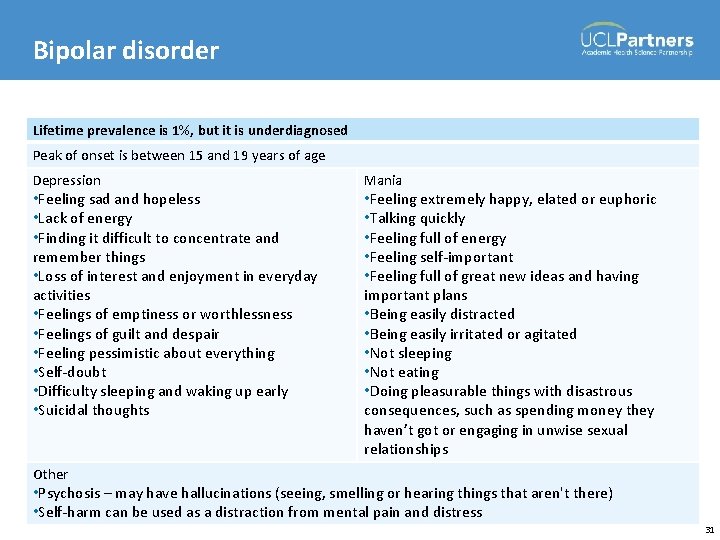
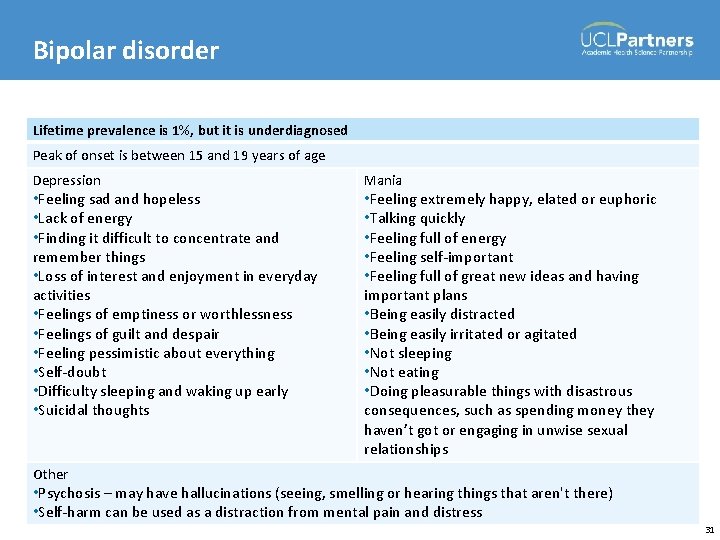
Bipolar disorder Lifetime prevalence is 1%, but it is underdiagnosed Peak of onset is between 15 and 19 years of age Depression • Feeling sad and hopeless • Lack of energy • Finding it difficult to concentrate and remember things • Loss of interest and enjoyment in everyday activities • Feelings of emptiness or worthlessness • Feelings of guilt and despair • Feeling pessimistic about everything • Self-doubt • Difficulty sleeping and waking up early • Suicidal thoughts Mania • Feeling extremely happy, elated or euphoric • Talking quickly • Feeling full of energy • Feeling self-important • Feeling full of great new ideas and having important plans • Being easily distracted • Being easily irritated or agitated • Not sleeping • Not eating • Doing pleasurable things with disastrous consequences, such as spending money they haven’t got or engaging in unwise sexual relationships Other • Psychosis – may have hallucinations (seeing, smelling or hearing things that aren't there) • Self-harm can be used as a distraction from mental pain and distress 31
Reducing the risk of premature death from cardiovascular disease in people with SMI • Life expectancy is reduced by 12– 19 years • Many comorbidities but most common cause of premature death is cardiovascular disease (CVD) • Caused by smoking (50% smoke), unhealthy diets, low levels of physical activity, some antipsychotic medication 32
Reducing the risk of premature death from cardiovascular disease in people with SMI Offer patients an annual physical health check A website has been created specifically for practice nurses. It has a best practice manual – The Health Improvement Profile for Primary Care (HIP-PC) – and other useful tools. These can all be downloaded free: http: //physicalsmi. webeden. co. uk/ Attend the module ‘Physical health in mental illness’ 33
Making it easier for patients with SMI to attend primary care Late morning or afternoon appointments Invitation letter: • Uncomplicated • Make clear patient can refuse treatment offered • Date and time (be flexible if patient cannot attend) • Named practitioner • Not sent out too early Telephone reminders before appointment and if does not attend to • Patient • Carer • Mental health worker 34

Basic care planning Key questions: 1. Do you see a doctor, nurse or social worker at (name of secondary care centre)? 2. Have you got housing difficulties, money or employment problems? 3. Do you have help from anyone else? 4. What is it that keeps you well? 5. What are your main symptoms when you are unwell? 6. Can we discuss what to do if you become unwell? 7. What signs are there that you could be becoming unwell again? 8. Can we make/review a plan for when you feel you are becoming unwell? 9. Do you have any plans for the future? 35
Related modules • Physical health in mental illness (classroom) • Changing patients’ behaviour (classroom) • Care planning (e-learning) 36
Medications used in mental illness 37
Medications used in mental illness Common medicines you will see in primary care Treatment for depression and/or anxiety: • Selective serotonin reuptake inhibitors or SSRIs (fluoxetine, citalopram, sertraline, paroxetine), Others (mirtazepine, venlafaxine) Drugs used for psychotic disorder: • Antipsychotics (e. g. olanzapine, risperidone, aripiprazole, quetiapine, clozapine) Drugs used for bipolar disorder: • Antipsychotics, antidepressants, ‘mood stabilisers’ (lithium, valproate, lamotrigine, carbamazepine) 38
Giving depot injections in primary care Giving an antipsychotic depot injections is not very different from giving a long-acting injection for a physical illness or contraception Follow the neuroleptic injection protocol Some of the most common drug names are: • Flupentixol Decanoate (Psytixol®/Depixol®) • Zuclopentixol Decanoate (Clopixol®) • Fluphenazine (Modecate®) • Pipothiazine (Piportil®) • Haloperidol Decanoate (Haldol®) • Risperidone (Risperdal Consta®) 39
Monitoring side effects • Glasgow Antipsychotic Side-effect Scale (GASS) 40
Related modules • Medications used in mental illness (e-learning) 41
Specific conditions 42
Alcohol problems Alcohol use is measured in units 1 unit = 1/2 a standard glass (175 ml) of wine (ABV 12%) or 1/3 of a pint of beer (ABV 5– 6%) Screening tools: AUDIT-C Misuse: • >28 units per week (men) or 21 (women) • Associated with increased risk of: o Liver disease o Gastrointestinal bleeding o Depression and/or anxiety o Negative social consequences (e. g. loss of job) 43
Alcohol problems Alcohol dependence is defined by the presence of three or more of the following: • A strong craving to use alcohol • Trouble in controlling alcohol use • Withdrawal (anxiety, tremors, sweating) when drinking is stopped • Tolerance (able to drink large amounts of alcohol without becoming drunk) • Continual alcohol use despite damaging consequences The consequences of alcohol dependence are considerable and include CVD and stroke. 44

Drug misuse • No proactive screening in primary care • Patients often will deny problem • May be recognised when patients want: o A prescription for drugs o Help to withdraw or stabilise their drug use o Treatment for the physical complications of drug use, such as abscesses o Medical acknowledgement of a drug problem because of debt or prosecution 45
Treatment of alcohol and drug problems • Dependent on whether patient wants to stop or reduce • Pass no judgement if they wish to continue • Advise on the benefits of stopping (physical health, mental health, ability to sort out social problems) • Refer to local NHS service • Provide self-help information 46
Eating disorders Most common: • Anorexia • Bulimia Often present with a physical complaint: • Palpitations • Amenorrhoea • Fits OR Brought in by member of family (worried about weight loss, refusal to eat, vomiting) 47
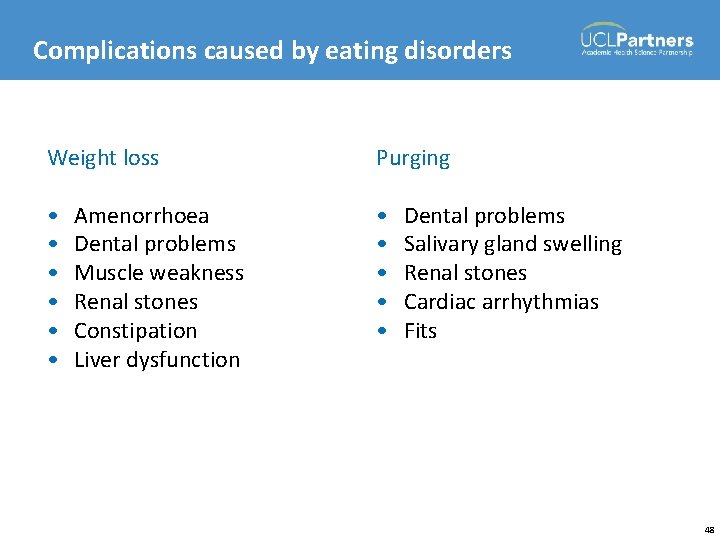
Complications caused by eating disorders Weight loss Purging • • • Amenorrhoea Dental problems Muscle weakness Renal stones Constipation Liver dysfunction Dental problems Salivary gland swelling Renal stones Cardiac arrhythmias Fits 48
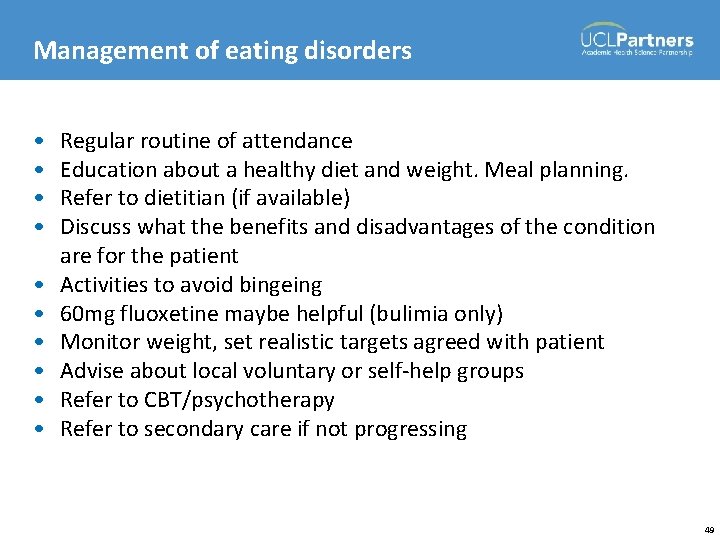
Management of eating disorders • • • Regular routine of attendance Education about a healthy diet and weight. Meal planning. Refer to dietitian (if available) Discuss what the benefits and disadvantages of the condition are for the patient Activities to avoid bingeing 60 mg fluoxetine maybe helpful (bulimia only) Monitor weight, set realistic targets agreed with patient Advise about local voluntary or self-help groups Refer to CBT/psychotherapy Refer to secondary care if not progressing 49
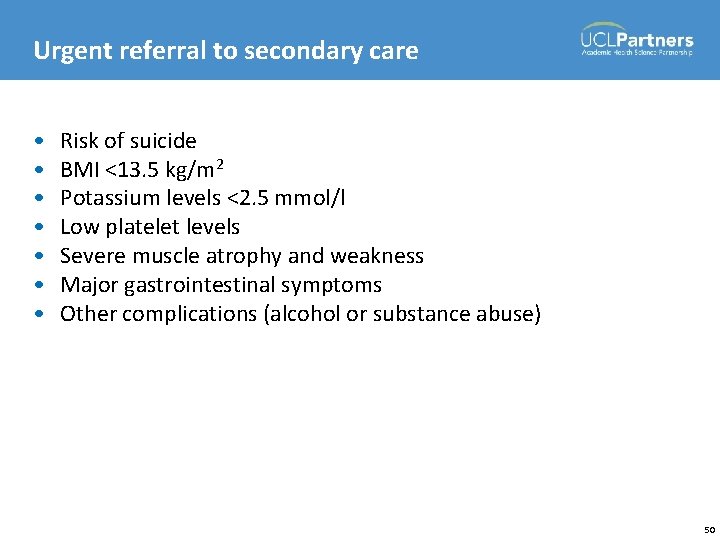
Urgent referral to secondary care • • Risk of suicide BMI <13. 5 kg/m 2 Potassium levels <2. 5 mmol/l Low platelet levels Severe muscle atrophy and weakness Major gastrointestinal symptoms Other complications (alcohol or substance abuse) 50
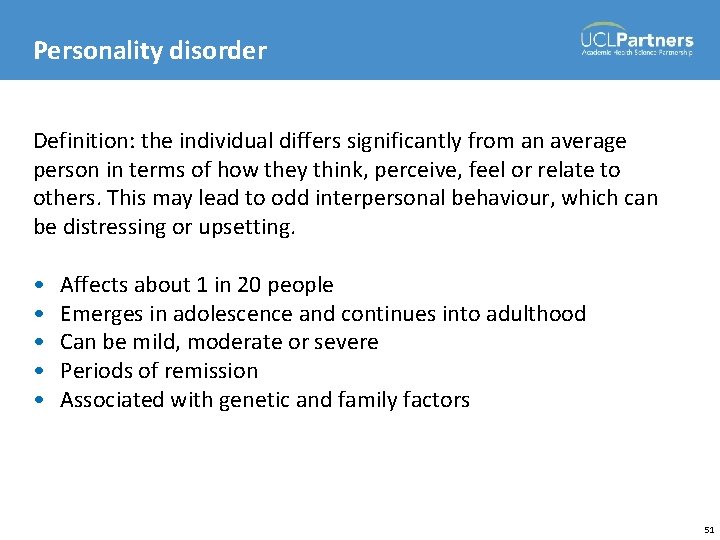
Personality disorder Definition: the individual differs significantly from an average person in terms of how they think, perceive, feel or relate to others. This may lead to odd interpersonal behaviour, which can be distressing or upsetting. • • • Affects about 1 in 20 people Emerges in adolescence and continues into adulthood Can be mild, moderate or severe Periods of remission Associated with genetic and family factors 51
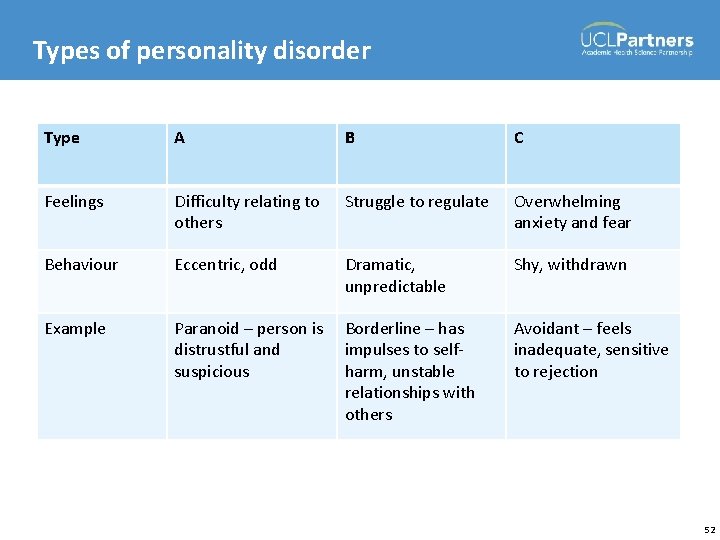
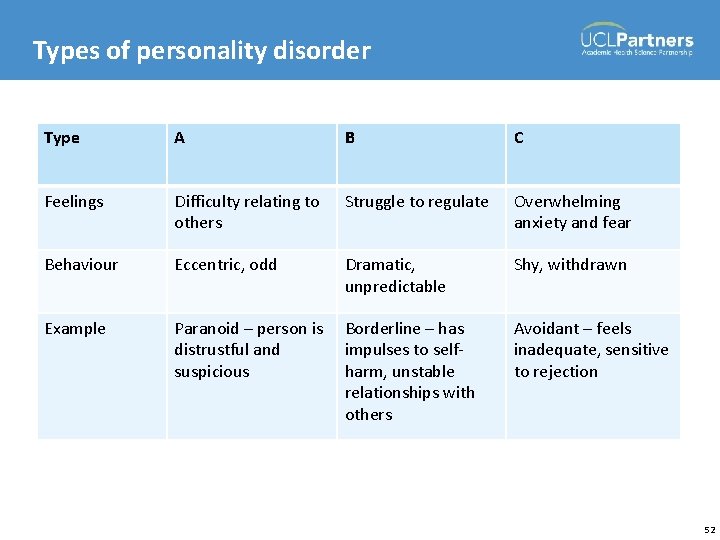
Types of personality disorder Type A B C Feelings Difficulty relating to others Struggle to regulate Overwhelming anxiety and fear Behaviour Eccentric, odd Dramatic, unpredictable Shy, withdrawn Example Paranoid – person is distrustful and suspicious Borderline – has impulses to selfharm, unstable relationships with others Avoidant – feels inadequate, sensitive to rejection 52
Management of personality disorder Most people recover time Psychological therapies include • Psychodynamic • Cognitive behavioural therapy • Interpersonal Therapeutic communities Medication – none licensed for personality disorder 53
Postnatal depression Occurs 4 to 6 weeks after birth but may be later Affects 10– 15% of women Causes: • Stress of looking after the baby • Hormonal changes • Money worries, poor social support or relationship problems Higher risk if: • Previous history of depression, bipolar disorder or postnatal depression • Depression or anxiety during pregnancy Treatment as for depression described earlier 54
Postpartum psychosis Occurs within 2 weeks of birth Affects one in every 1000 A severe episode of mental illness Symptoms: • Mania • Depression • Confusion • Hallucinations • Delusions Postpartum psychosis is a psychiatric emergency 55
Bereavement Grief following: • Death of someone close • Significant event (loss of job or limb, breakdown of relationship) There are four stages: • Accepting the loss (may feel numb) • Feeling the pain • Becoming accustomed to the loss • Letting go and moving on 56
Bereavement What the practice nurse can do: • Provide the opportunity for the patient to talk • Ask about feelings regarding the loss • Explain it will take time to come to terms with the loss, pain will fade slowly • Advise to take time out if needed • Consider depression and treat appropriately • Refer for counselling if at risk of developing an abnormal reaction 57
Abuse is a violation of an individual's human and civil rights by any other person or persons (DOH 2000) • • Physical abuse Sexual abuse Psychological abuse Financial or material abuse Neglect and acts of omission Discriminatory abuse Institutional abuse Department of Health. (2000) No secrets: Guidance on developing and implementing multi-agency policies and procedures to protect vulnerable adults from abuse. London: DOH. 58
Abuse Your role is that of a supportive listener How to respond: • Maintain a calm appearance • Listen actively • Don’t make promises you can’t keep • Reassure them it is right to tell • Recognise the bravery/strength needed to divulge the problem • Tell them what you plan to do next 59
Related modules • Specific conditions (e-learning) 60
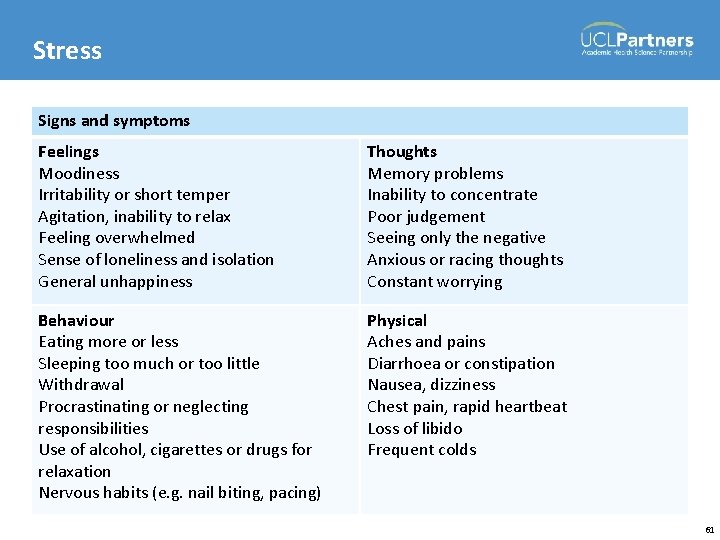
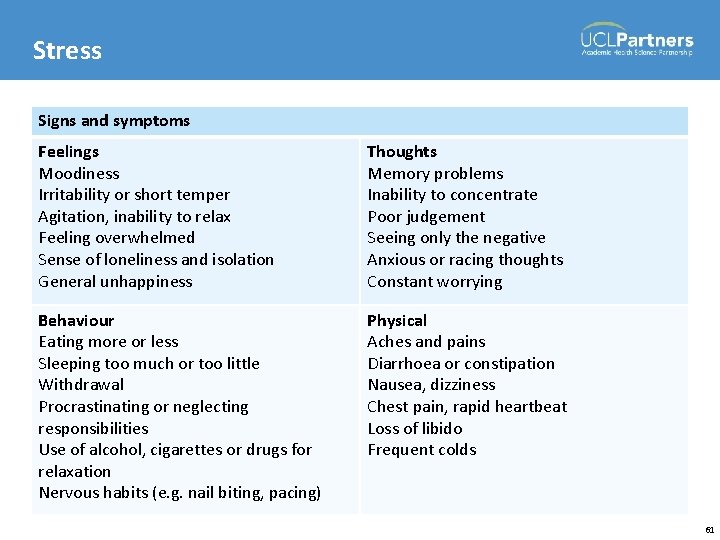
Stress Signs and symptoms Feelings Moodiness Irritability or short temper Agitation, inability to relax Feeling overwhelmed Sense of loneliness and isolation General unhappiness Thoughts Memory problems Inability to concentrate Poor judgement Seeing only the negative Anxious or racing thoughts Constant worrying Behaviour Eating more or less Sleeping too much or too little Withdrawal Procrastinating or neglecting responsibilities Use of alcohol, cigarettes or drugs for relaxation Nervous habits (e. g. nail biting, pacing) Physical Aches and pains Diarrhoea or constipation Nausea, dizziness Chest pain, rapid heartbeat Loss of libido Frequent colds 61
Related modules • Wellbeing (classroom) 62

 Objective for mental health awareness
Objective for mental health awareness Poem on mental health awareness day
Poem on mental health awareness day Titles for mental health presentations
Titles for mental health presentations Mental health and mental illness chapter 20
Mental health and mental illness chapter 20 Jeopardy mental health
Jeopardy mental health Privacy awareness and hipaa privacy training cvs answers
Privacy awareness and hipaa privacy training cvs answers Overlake senior health clinic
Overlake senior health clinic Senior health clinic
Senior health clinic Department of health and senior services missouri
Department of health and senior services missouri Men's health awareness ball
Men's health awareness ball The bass the river and sheila mant text
The bass the river and sheila mant text Dr sheila crowe
Dr sheila crowe El novio de la muerte acordes
El novio de la muerte acordes Sheila eyberg
Sheila eyberg Sheila greibach
Sheila greibach Sheila greibach
Sheila greibach Sheila ortega nacimiento
Sheila ortega nacimiento Gaby borglund partner
Gaby borglund partner Greibach
Greibach An inspector calls summary
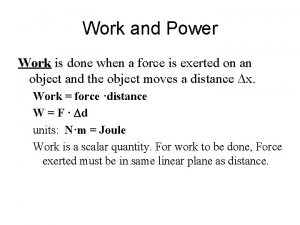
An inspector calls summary Hans full is pulling on a rope to drag
Hans full is pulling on a rope to drag Mr birling irresponsible quotes
Mr birling irresponsible quotes How does sheila change in an inspector calls
How does sheila change in an inspector calls Dr sheila crowe
Dr sheila crowe Hans full is pulling on a rope to drag
Hans full is pulling on a rope to drag Sheila gupta
Sheila gupta Sheila embleton
Sheila embleton Sheila bouman
Sheila bouman Meet kevin henkes
Meet kevin henkes Sheila tormey
Sheila tormey Wesley bad boy boone
Wesley bad boy boone Secondlive bsc
Secondlive bsc Sheila ostrander and lynn schroeder
Sheila ostrander and lynn schroeder Sheila harshey
Sheila harshey Sheila
Sheila Sheila is writing a persuasive message
Sheila is writing a persuasive message Sheila birling
Sheila birling Searching for sheila
Searching for sheila Frances baillon
Frances baillon Sheila crowe
Sheila crowe Kerrie has paid the bill.
Kerrie has paid the bill. Sheila birling character profile
Sheila birling character profile Sheila birling
Sheila birling Sheila tarrant
Sheila tarrant Sheila ortega sola
Sheila ortega sola Sheila barb
Sheila barb Sheila cussons
Sheila cussons Sheila hoffman phd
Sheila hoffman phd Food poisoning
Food poisoning Sheila adjectives
Sheila adjectives Junius hardy
Junius hardy The ruined maid analysis
The ruined maid analysis When is population in hardy weinberg equilibrium
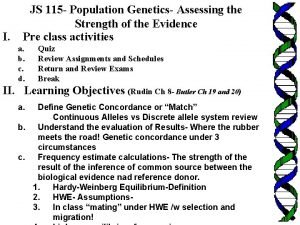
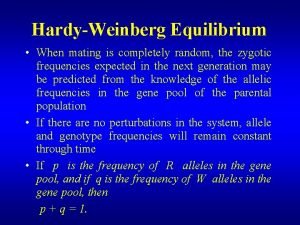
When is population in hardy weinberg equilibrium Allelfrekvens beregning
Allelfrekvens beregning Five conditions for hardy weinberg
Five conditions for hardy weinberg Hardy weinburg assumptions
Hardy weinburg assumptions Hardy weinberg assumptions
Hardy weinberg assumptions Hardy weinberg equation
Hardy weinberg equation Hardy-weinberg equilibrium conditions
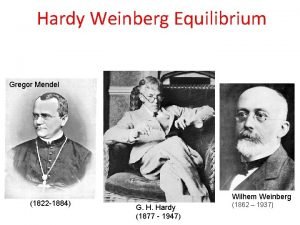
Hardy-weinberg equilibrium conditions Gregor mendel
Gregor mendel Hardy matematik
Hardy matematik M
M Eritroblastose fetal
Eritroblastose fetal Ken hardy tasks of the privileged
Ken hardy tasks of the privileged