Medical Informatics Practice Education the challenges solutions Syed
- Slides: 30
Medical Informatics Practice & Education -the challenges & solutions Syed Tirmizi, MD Medical Informatician Health Tech. Net November 15, 2008
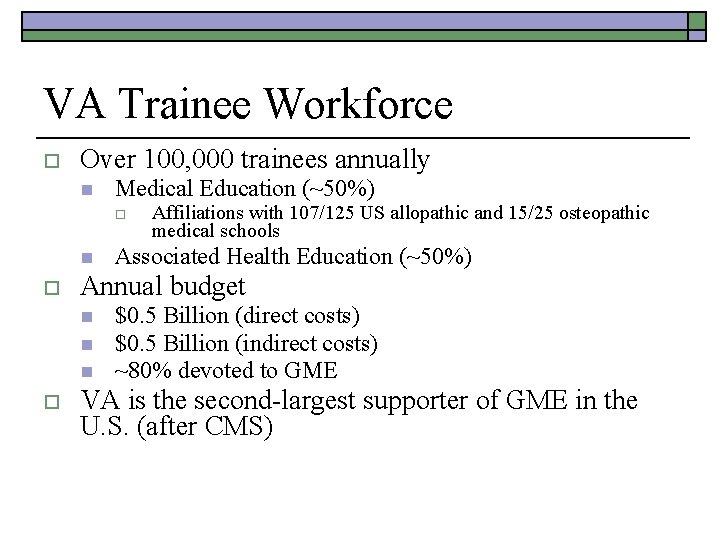
VA Trainee Workforce o Over 100, 000 trainees annually n Medical Education (~50%) o n o Associated Health Education (~50%) Annual budget n n n o Affiliations with 107/125 US allopathic and 15/25 osteopathic medical schools $0. 5 Billion (direct costs) $0. 5 Billion (indirect costs) ~80% devoted to GME VA is the second-largest supporter of GME in the U. S. (after CMS)
Academic Affiliation o o o draws expert clinicians and researchers to the VA affiliations allow VA to provide veterans “a much higher standard of medical care mutually beneficial by affording each party access to resources that would otherwise be unavailable o o o medical schools gain access to invaluable undergraduate and graduate medical education opportunities faculty with joint VA appointments are afforded opportunities for research funding (restricted to VA employees) 70 percent of VA physicians hold joint medical school faculty positions
Academic Affiliation o o o 130 VA medical centers have affiliations with 107 of the 126 allopathic medical schools Physician education represents half of the over 100, 000 VA health professions trainees Medical residents contribute approximately 1/3 of the VA physician workforce 2007 Learners Perception Survey o o Before training 21 percent of medical students and 27 percent of medical residents likely to consider VA employment After training 57 percent of medical students and 49 percent of medical residents.
Goals o o o Expand resident positions in specialties of greatest need to veterans Address uneven geographic distribution of residents and improve access to care Foster innovative models of resident education Assume VA’s proportionate share in addressing the physician workforce shortage Enhance VA’s leadership role in GME
Scope o o Restore VA-funded GME positions to 10 -11% of U. S. total First expansion of VA GME in over 15 years n 2, 000 new positions over 5 years o o o n o Critical Needs (CN) & Emerging Specialties (ES) New Affiliations (NA) and New Sites of Care (NS) Educational Innovation (ED INN) Estimated incremental cost: $250 million VA is presently the only GME payer increasing support for education
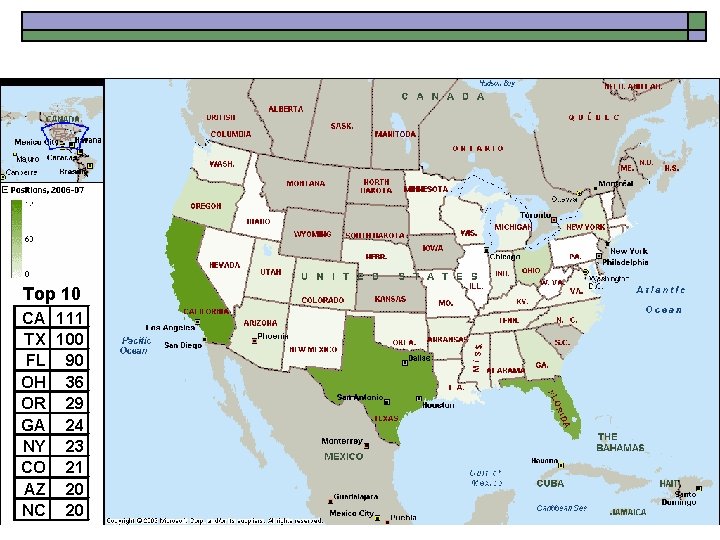
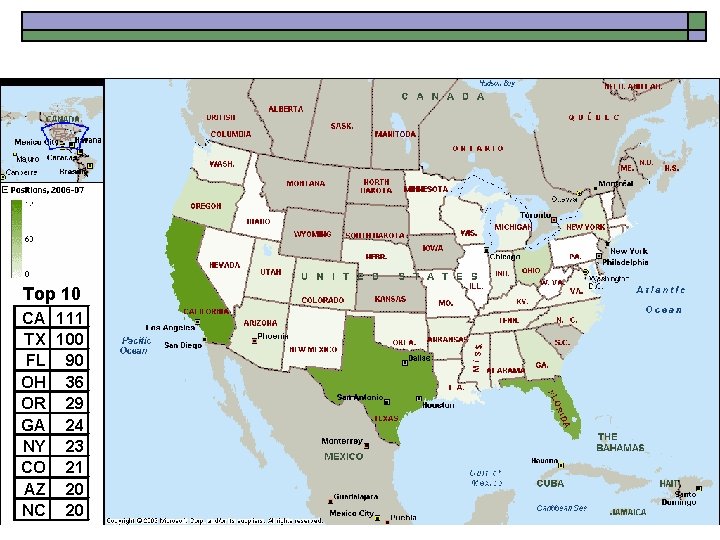
Approved Positions by State Top 10 CA 111 TX 100 FL 90 OH 36 OR 29 GA 24 NY 23 CO 21 AZ 20 NC 20
Institutional Eligibility o Innovation n n o Commitment n n o Transform educational processes Redesign clinical care models Protect teaching time Support professional development Assessment n n Measure educational and care outcomes Participate in cross-site program evaluation
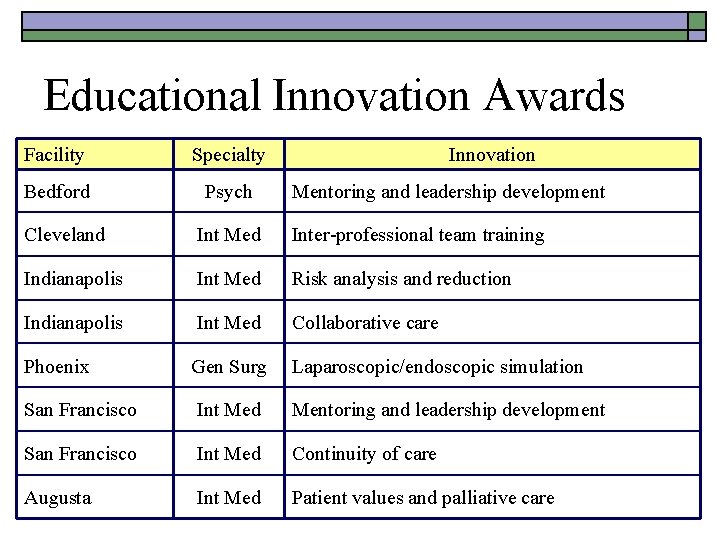
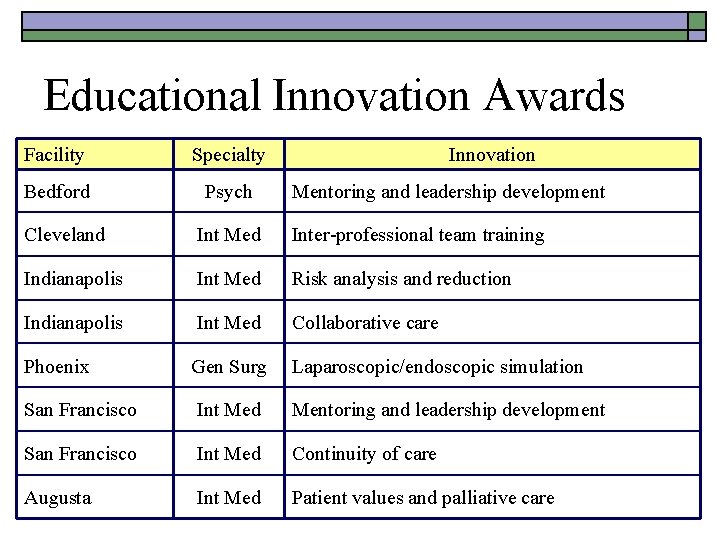
Educational Innovation Awards Facility Specialty Bedford Psych Innovation Mentoring and leadership development Cleveland Int Med Inter-professional team training Indianapolis Int Med Risk analysis and reduction Indianapolis Int Med Collaborative care Phoenix Gen Surg Laparoscopic/endoscopic simulation San Francisco Int Med Mentoring and leadership development San Francisco Int Med Continuity of care Augusta Int Med Patient values and palliative care
Summary o VA is expanding residency training positions in ways that will: n n Address specialty and geographic needs Expand veterans’ access to care Enhance residents’ clinical training experiences Contribute to reform and innovation in medical education, while improving care delivery
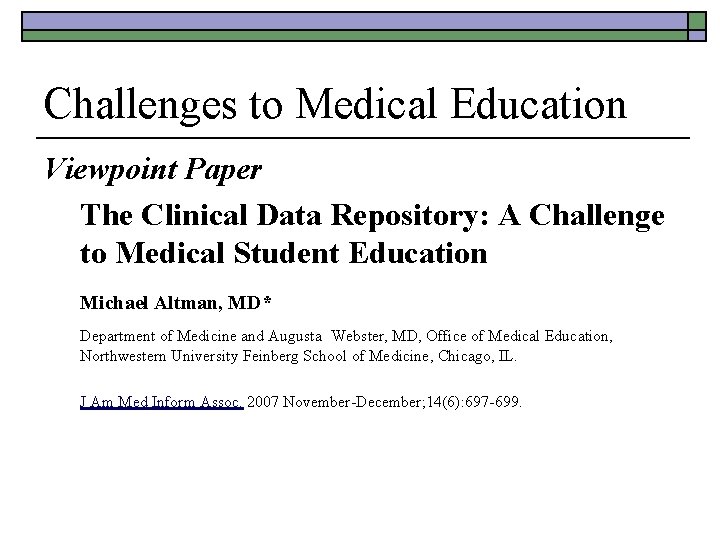
Challenges to Medical Education Viewpoint Paper The Clinical Data Repository: A Challenge to Medical Student Education Michael Altman, MD* Department of Medicine and Augusta Webster, MD, Office of Medical Education, Northwestern University Feinberg School of Medicine, Chicago, IL. J Am Med Inform Assoc. 2007 November-December; 14(6): 697 -699.
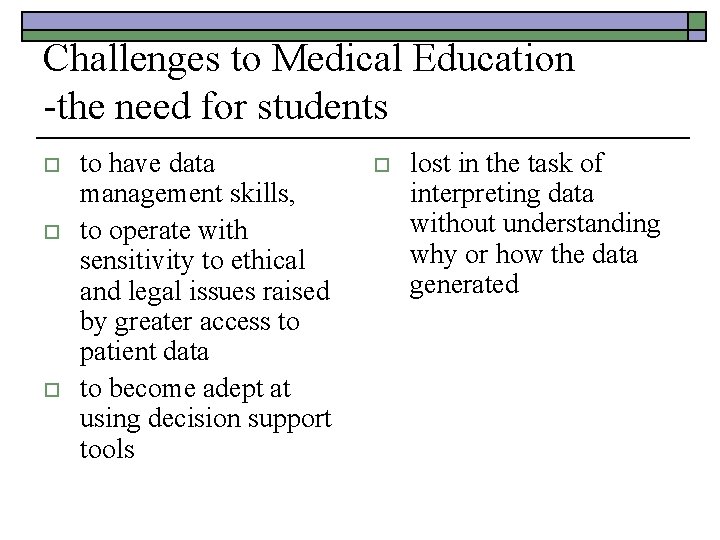
Challenges to Medical Education -the need for students o o o to have data management skills, to operate with sensitivity to ethical and legal issues raised by greater access to patient data to become adept at using decision support tools o lost in the task of interpreting data without understanding why or how the data generated
Challenges to Medical Education -solutions o o technological advances applied to improve medical student clinical education partnerships can produce educational tools to support the acquisition and reinforcement of some very basic physician skills o tools to prepare medical students to operate in information-rich clinical environment
Challenges to Informatics Education -solutions o o o AMIA 10 x 10 AAMC NLM Medical Informatics fellowships Public Health Informatics Fellowships AMIA academic forum Nursing informatics board certification o o Student & Resident Orientation Informatics projects Ve. HU VHA 5 -tiered approach n n n Online open courseware CME/CE Heath IT certification Graduate degree Medical informatics fellowships
Towards a “Virtual Health System” o o Electronic Health Records (EHRs) n Widespread Use of High Performance, Robust Electronic Health Records (EHRs) Personal Health Records (PHRs) n Full copy of one’s own health information along with personalized services based on that information Standards n Health Data & Communication Standards Health Information Exchange n Connectivity Among the EHRs, PHRs, and related health entities
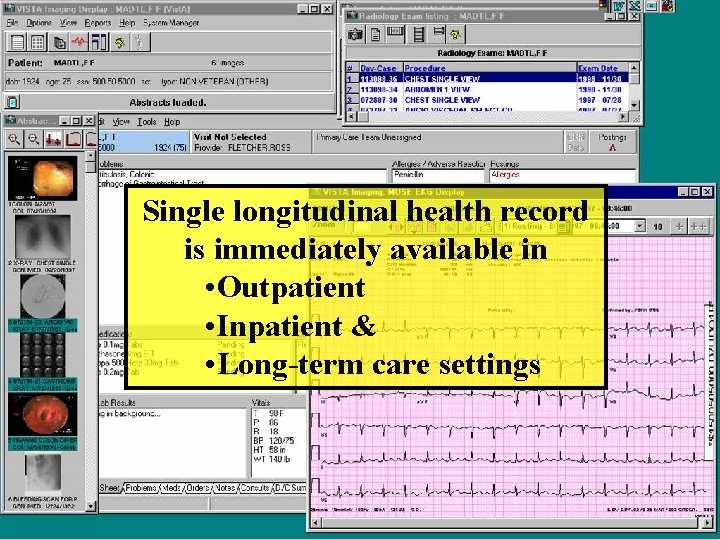
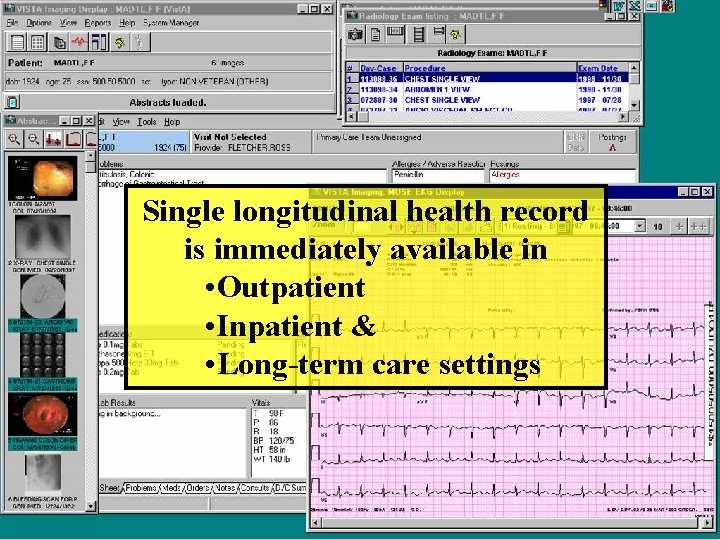
Single longitudinal health record is immediately available in • Outpatient • Inpatient & • Long-term care settings
Links Reminder With Actions With Documentation
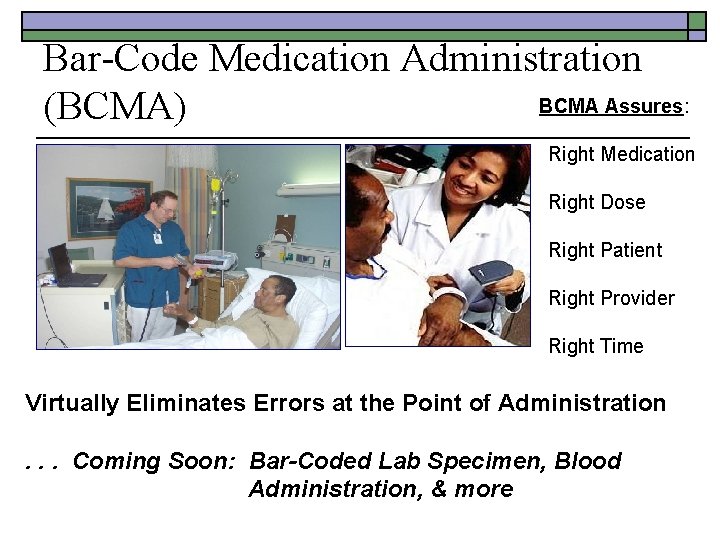
Bar-Code Medication Administration BCMA Assures: (BCMA) Right Medication Right Dose Right Patient Right Provider Right Time Virtually Eliminates Errors at the Point of Administration. . . Coming Soon: Bar-Coded Lab Specimen, Blood Administration, & more
PHR Personal Health Record
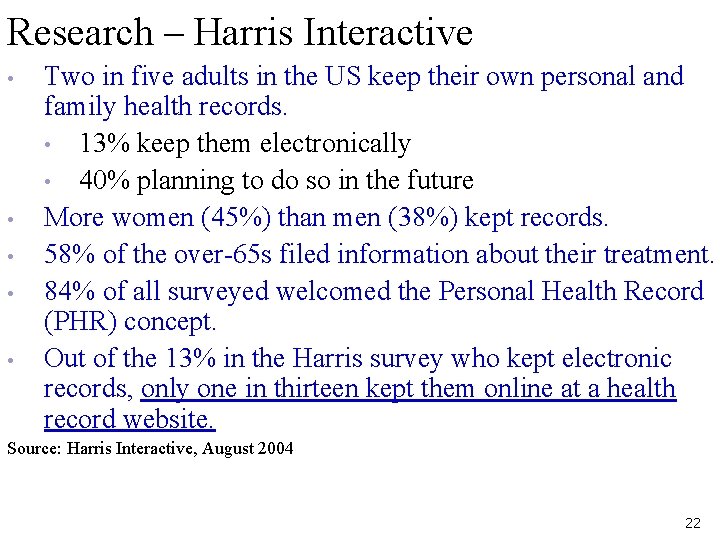
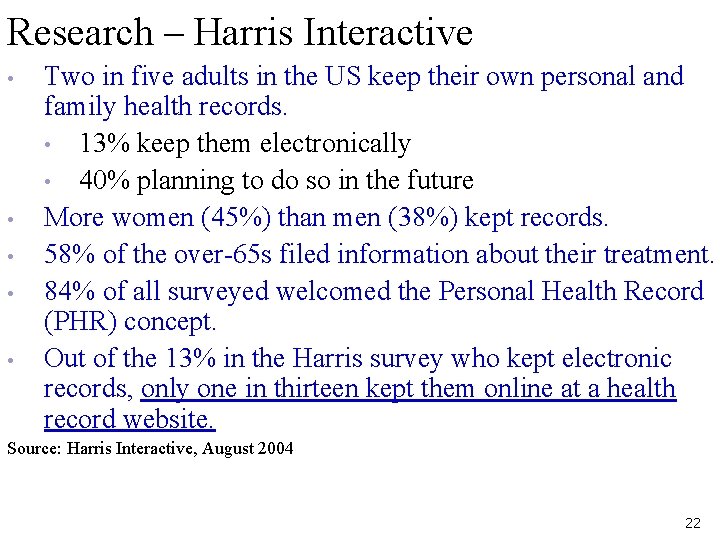
Research – Harris Interactive • • • Two in five adults in the US keep their own personal and family health records. • 13% keep them electronically • 40% planning to do so in the future More women (45%) than men (38%) kept records. 58% of the over-65 s filed information about their treatment. 84% of all surveyed welcomed the Personal Health Record (PHR) concept. Out of the 13% in the Harris survey who kept electronic records, only one in thirteen kept them online at a health record website. Source: Harris Interactive, August 2004 22
How comfortable would you be if an PHR was provided, sponsored, and/or maintained by: 23
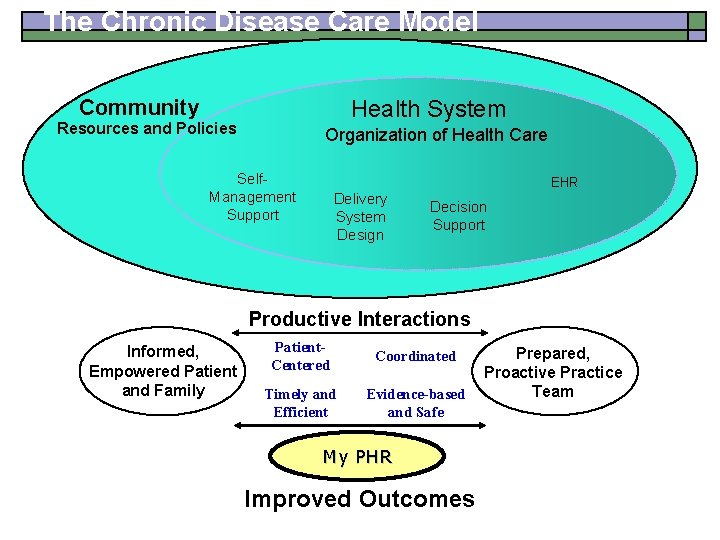
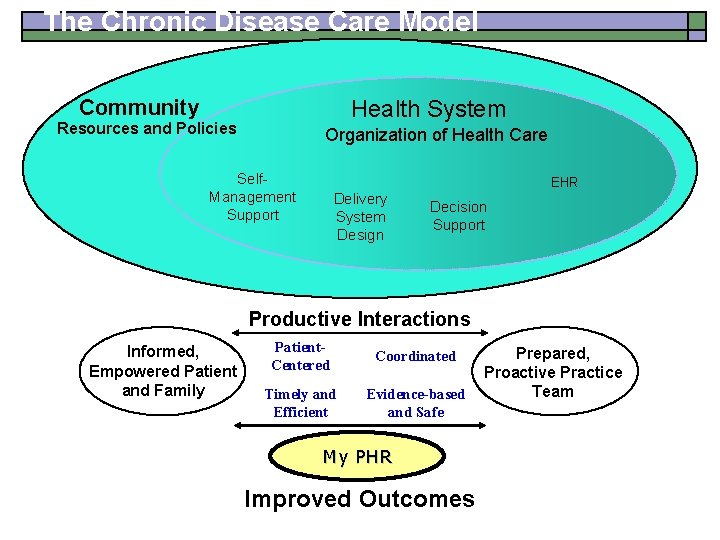
The Chronic Disease Care Model Community Health System Resources and Policies Organization of Health Care Self. Management Support EHR Delivery System Design Decision Support Productive Interactions Informed, Empowered Patient and Family Patient. Centered Coordinated Timely and Efficient Evidence-based and Safe My PHR Improved Outcomes Prepared, Proactive Practice Team
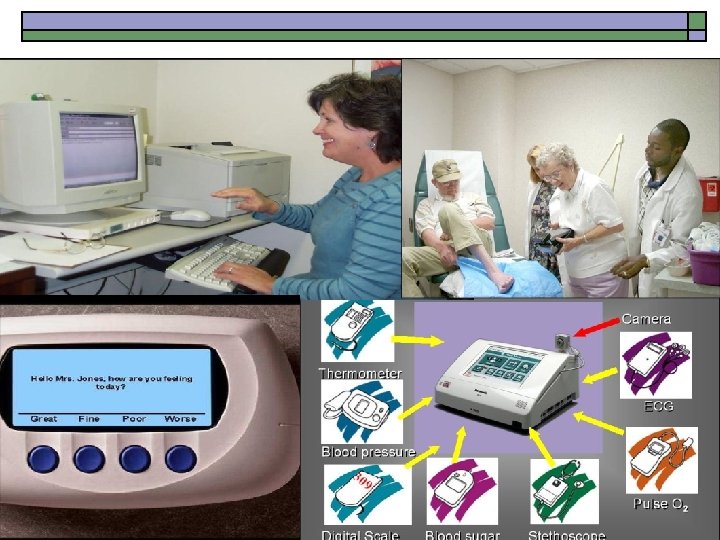
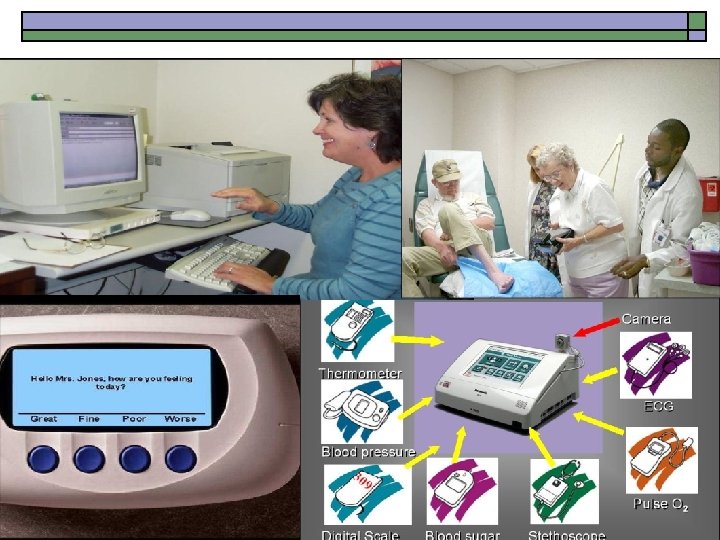
Home Telehealth Technologies
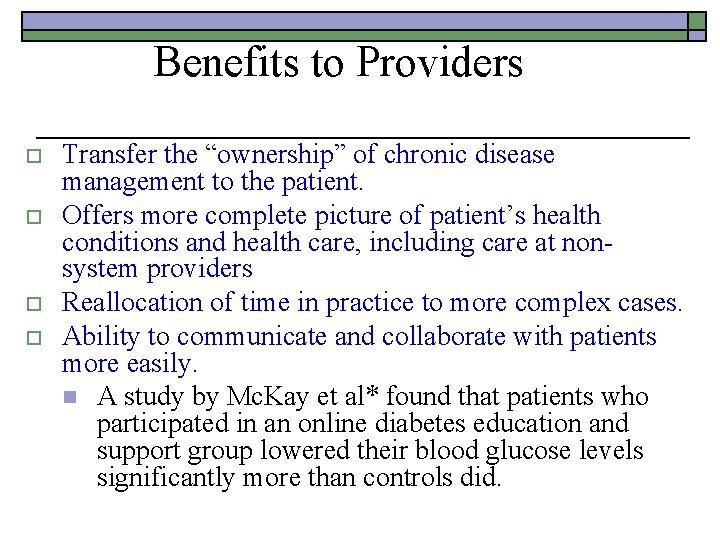
Benefits to Providers o o Transfer the “ownership” of chronic disease management to the patient. Offers more complete picture of patient’s health conditions and health care, including care at nonsystem providers Reallocation of time in practice to more complex cases. Ability to communicate and collaborate with patients more easily. n A study by Mc. Kay et al* found that patients who participated in an online diabetes education and support group lowered their blood glucose levels significantly more than controls did.
However This is NOT about technology… It is about RESULTS: o Improved Health Care Quality o Improved Health Outcomes
Clinical Decision Support Rationale - 1 o o CDS demonstrated to be effective in a number of settings over the past 30 -40 years Impact n n n n o best practices error reduction pay for performance cost effectiveness chronic disease management prevention Bio-surveillance etc. Yet slow dissemination and adoption
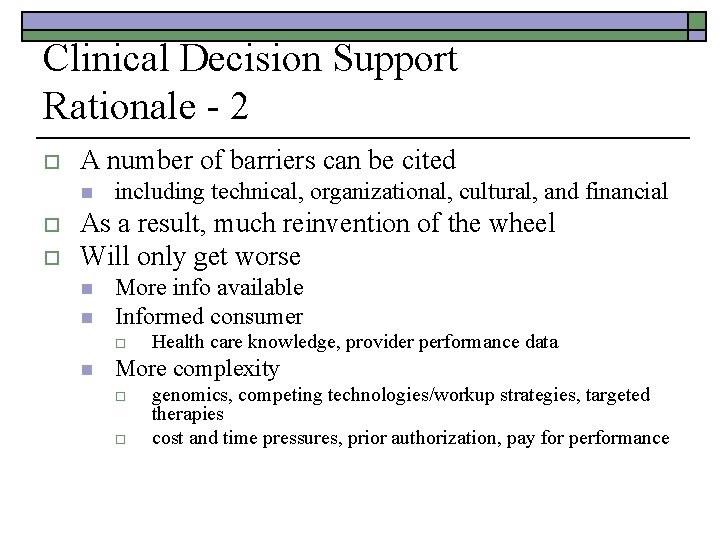
Clinical Decision Support Rationale - 2 o A number of barriers can be cited n o o including technical, organizational, cultural, and financial As a result, much reinvention of the wheel Will only get worse n n More info available Informed consumer o n Health care knowledge, provider performance data More complexity o o genomics, competing technologies/workup strategies, targeted therapies cost and time pressures, prior authorization, pay for performance
A Roadmap for National Action on Clinical Decision Support AMIA White paper, June 13, 2006 Prepared by: Jerome A. Osheroff, MD, Jonathan M. Teich, MD, Ph. D, Blackford F. Middleton, MD, MPH, MSc, Elaine B. Steen, MA, Adam Wright, Don E. Detmer, MD, MA
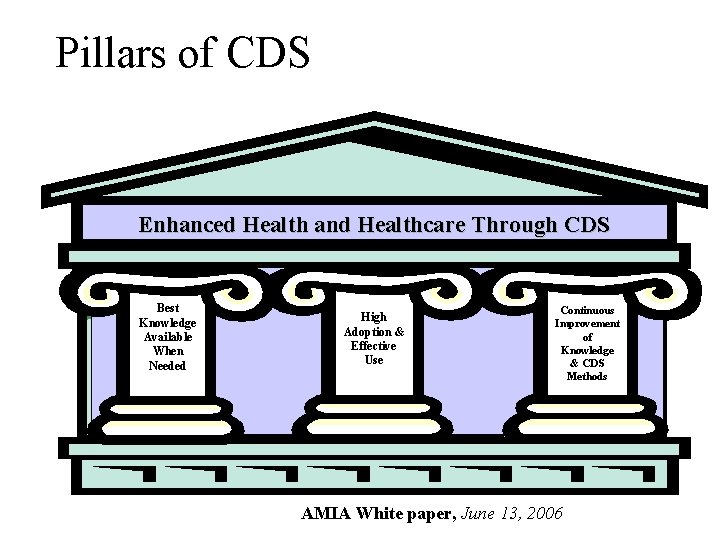
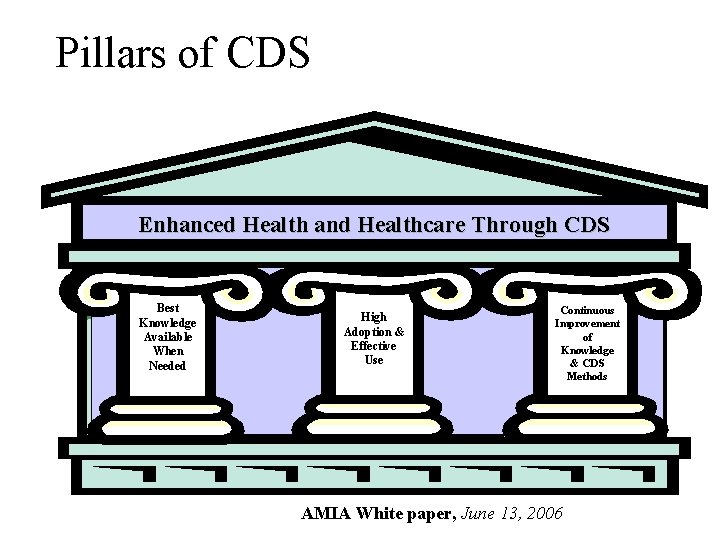
Pillars of CDS Enhanced Health and Healthcare Through CDS Best Knowledge Available When Needed High Adoption & Effective Use Continuous Improvement of Knowledge & CDS Methods AMIA White paper, June 13, 2006
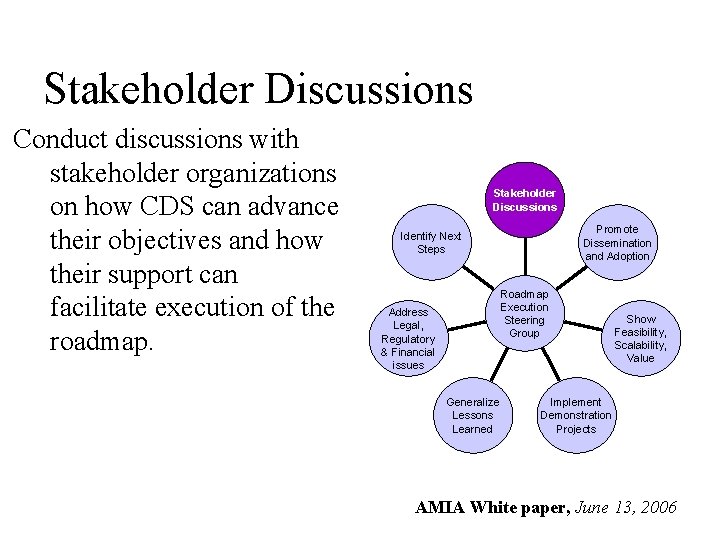
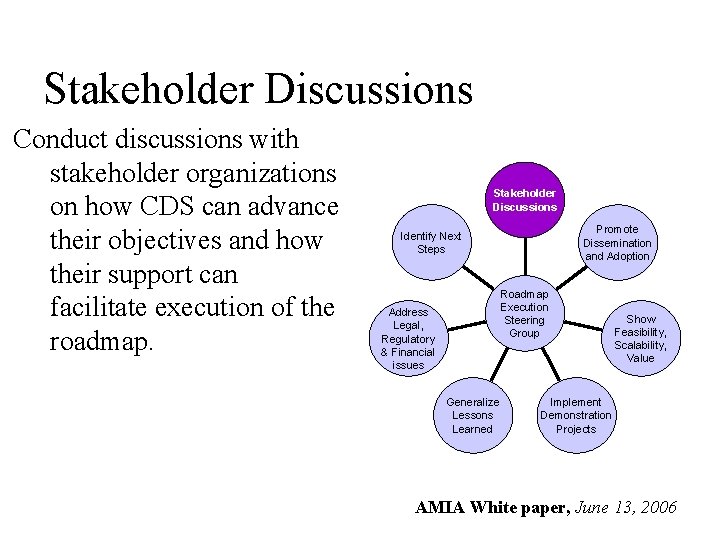
Stakeholder Discussions Conduct discussions with stakeholder organizations on how CDS can advance their objectives and how their support can facilitate execution of the roadmap. Stakeholder Discussions Promote Dissemination and Adoption Identify Next Steps Roadmap Execution Steering Group Address Legal, Regulatory & Financial issues Generalize Lessons Learned Show Feasibility, Scalability, Value Implement Demonstration Projects AMIA White paper, June 13, 2006