Medical Incident Report Form Education Module for 2009

- Slides: 29
Medical Incident Report Form Education Module for 2009 BLS Basic Training Course (Complete Dataset) Prepared by the Division of Emergency Medical Services
Education Module Goals • Train new EMS personnel • Provide a review for experienced EMS personnel
Education Module Contents • Basic information & general instructions • Cardiac arrest highlight (yes, again) • 2009 MIRF dataset • SPHERE questions
Basic Information & General Instructions
Why the MIRF is Important • Medical – The MIRF (both electronic and paper) is part of the patient’s medical file. – The paper MIRF transfers information between patient care providers. • Legal – Confidentiality – Patient Refusal – MIRF Signature
Why the MIRF is Important (continued) • Quality Review – Agency and systemwide • Planning/Funding – Medic unit placement, levy funding • Research – Resuscitation Outcome Consortium (ROC) – Supporting Public Health with Emergency Responders (SPHERE)
Components of a Good Report • Completeness – All available information regarding the incident or patient care should be recorded. • Accuracy – Describe exactly what happened. • Correct spelling • Legibility (on paper forms)
Components of a Good Report (continued) • Narrative: use S. O. A. P format: – Subjective – Objective – Assessment – Plan
Basic Instructions • An electronic recordis created by CAD/Dispatch for every call/incident. • When completing the paper (short) form in the field, use a ball point pen and press hard enough to mark through all copies. • Complete the electronic record verifying that the CAD information is accurate. • Refer to your agency protocols regarding exceptions to completing the paper (short) form. ******* • Agencies using the paper (long) formshould complete a form for every call/incident.
Paper MIRF Pages • Agency copy • EMS copy • Medical Review copy • Patient copy • Cardiac worksheet (Short Form Only): A reminder sheet to assist EMS personnel in collecting CPR data in the field, and paramedics in assessing Acute Coronary Syndrome (ACS). Worksheet may be discarded.
Completing the MIRF The person who provided primary care should: • Sign your name • Printyour name • Write your EMS number
Patient Refusal • Follow the instructions on the back of the MIRF. • Fill in patient’s name, and the date. • Read the statement slowly & clearly to the patient. Ask if they understand what it says. • Have the patient/guardian sign in the appropriate spots. • If patient/guardian refuses or you are unable to obtain a signature, make a note to that effect. • Obtain a signature from a witness and note their EMS agency affiliation or address.

Cardiac Arrest. Highlight
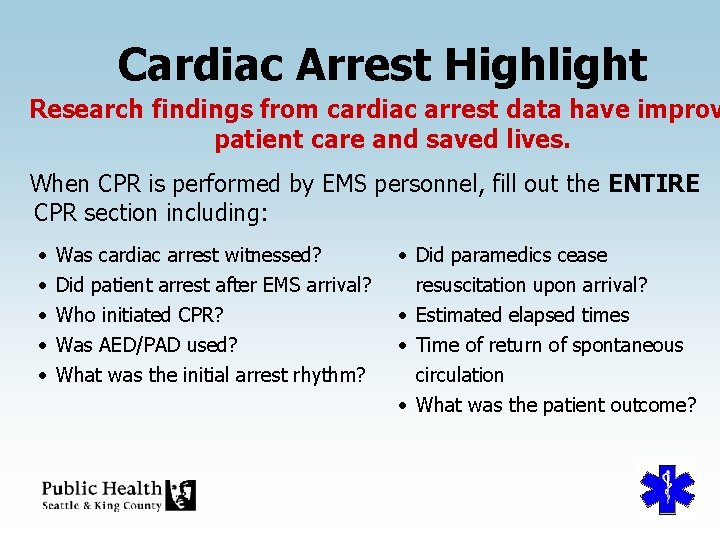
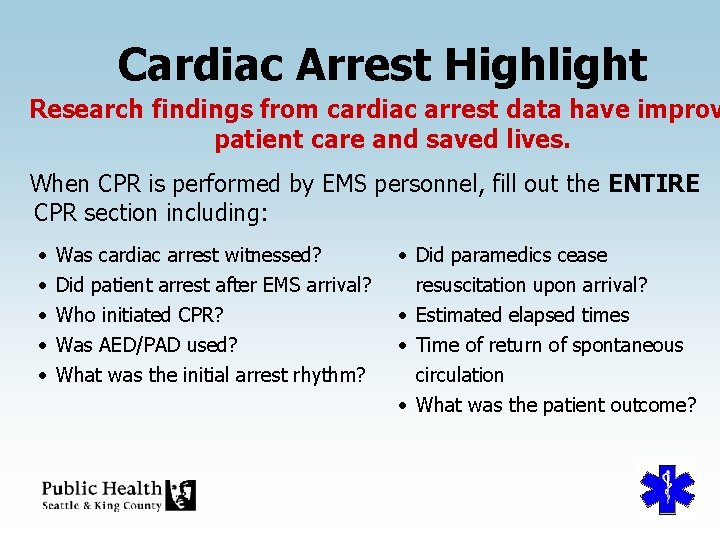
Cardiac Arrest Highlight Research findings from cardiac arrest data have improv patient care and saved lives. When CPR is performed by EMS personnel, fill out the ENTIRE CPR section including: • • • Was cardiac arrest witnessed? Did patient arrest after EMS arrival? Who initiated CPR? Was AED/PAD used? What was the initial arrest rhythm? • Did paramedics cease resuscitation upon arrival? • Estimated elapsed times • Time of return of spontaneous circulation • What was the patient outcome?
Cardiac Arrest Highlight (cont. ) • Cardiac Arrest Witnessed If someone directly saw or heard the patient collapse, then the arrest is considered witnessed and you should mark “Yes. ” If the patient’s collapse was not seen or heard, but found after an unknown length of time, it is considered unwitnessed and you should mark “No. ” • Arrest After Arrival of EMS Personnel Did the arrest occur after the arrival of emergency personnel?
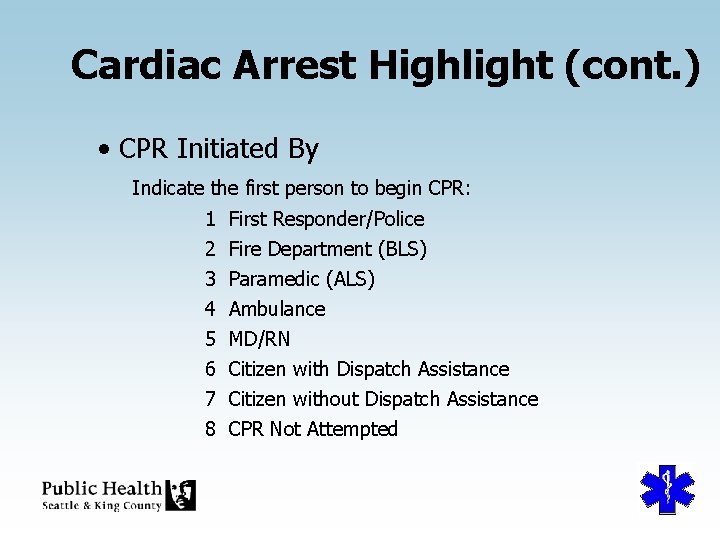
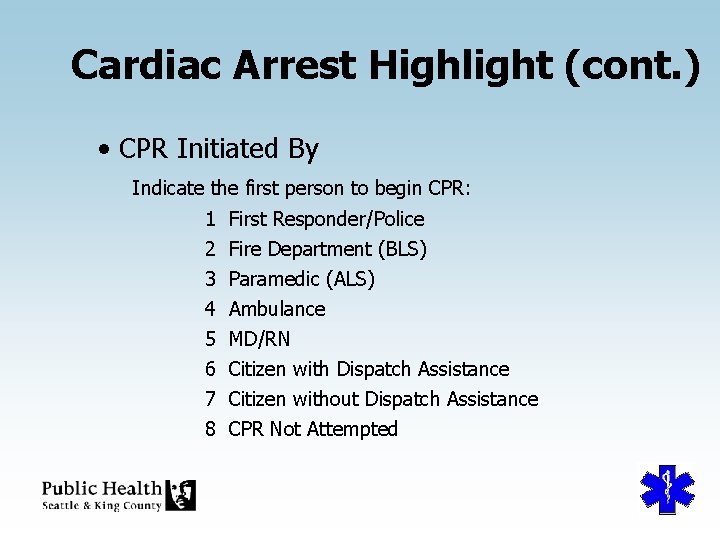
Cardiac Arrest Highlight (cont. ) • CPR Initiated By Indicate the first person to begin CPR: 1 2 3 4 5 6 7 8 First Responder/Police Fire Department (BLS) Paramedic (ALS) Ambulance MD/RN Citizen with Dispatch Assistance Citizen without Dispatch Assistance CPR Not Attempted
Cardiac Arrest Highlight (cont. ) • AED/PAD Used Was AED/PAD used? 1 Citizen – No Shock 2 Citizen – Shock 3 First Responder/Police – Shock 4 First Responder/Police – No Shock
Cardiac Arrest Highlight (cont. ) • Initial ECG Rhythm First observed cardiac rhythm by EMT: 01 Sinus Rhythm 02 04 11 U 0 Asystole Other Ventricular Fibrillation Unknown
Cardiac Arrest Highlight (cont. ) • Paramedics Cease Resuscitation On Arrival Indicate if resuscitation was ceased by paramedics within the first few minutes of arrival on scene due to DNR orders, compelling reasons, or conditions not compatible with life. • Estimated Elapsed Time (minutes) from Collapse to Call For witnessed arrest only; the estimated number of minutes between collapse of the patient and the reporting party reaching the correct agency by phone. If the collapse was unwitnessed or you cannot estimate the time, do not enter anything.
Cardiac Arrest Highlight (cont. ) • Estimated Time (minutes) from Collapse to CPR For witnessed arrests only, the estimated number of minutes from the patient’s collapse to the time CPR was initiated. • Time Return of Spontaneous Circulation Time of the return of any palpable pulse. A palpable pulse would be one detectable by manual palpation of a major artery, usually the carotid.
Cardiac Arrest Highlight (cont. ) • Patient Outcome Complete for all cardiac arrest patients. 01 DOA 02 03 04 05 06 Expired at Scene (including during transport) Admitted to ER Expired at ER Admitted to Hospital Unknown
Cardiac Arrest Highlight (cont. ) • When CPR is performed… – Mail the red copy of the MIRF and a printout of your electronic record and a copy of the defibrillation reading to the EMS Division within 4 days of the event.
2009 MIRF Dataset • Procedures • Short Form Backer
Procedures • Mask • Gown/Apron If a mask or gown/apron is used at the scene, please check the appropriate box.
Short Form Backer • Acute Coronary Syndrome (ACS) Algorithm: The new acute coronary guide on the back cover is intended primarily for paramedics to help identify patients who could benefit from immediate coronary catheterization.
SPHERE Questions
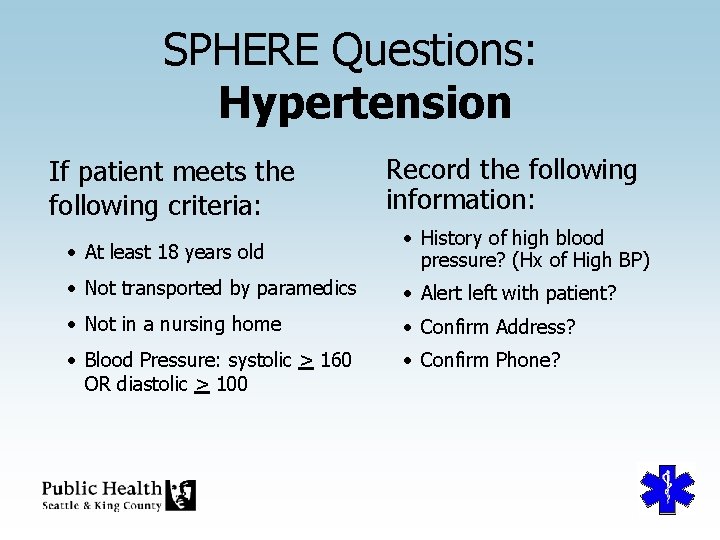
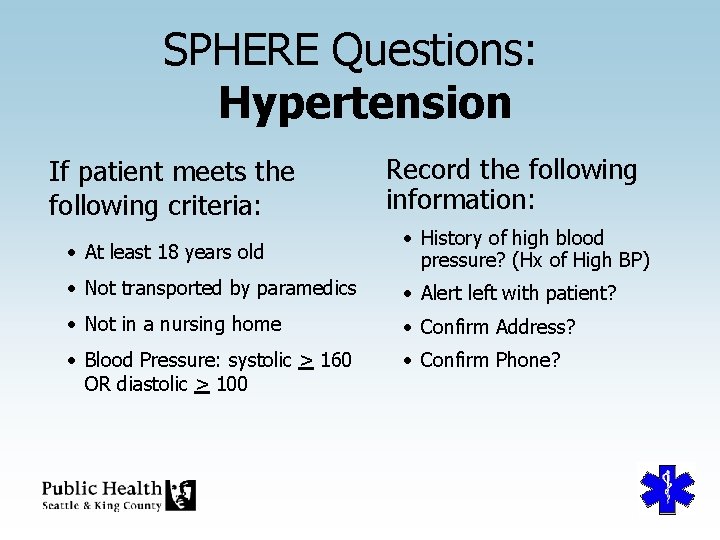
SPHERE Questions: Hypertension If patient meets the following criteria: Record the following information: • At least 18 years old • History of high blood pressure? (Hx of High BP) • Not transported by paramedics • Alert left with patient? • Not in a nursing home • Confirm Address? • Blood Pressure: systolic > 160 OR diastolic > 100 • Confirm Phone?
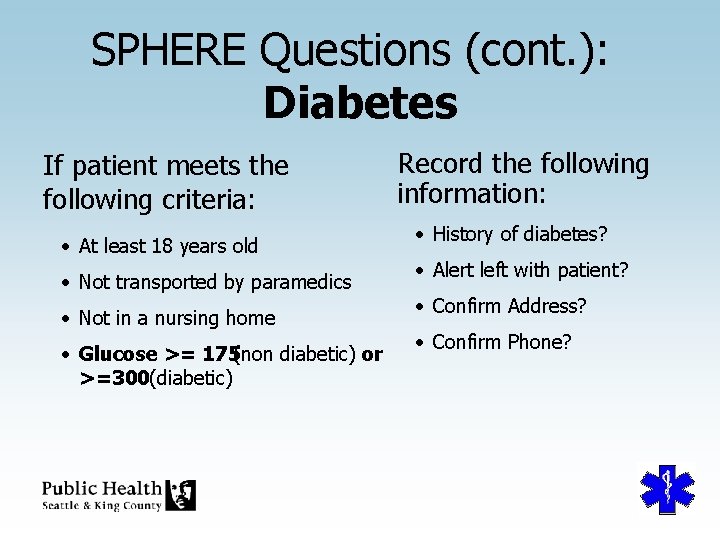
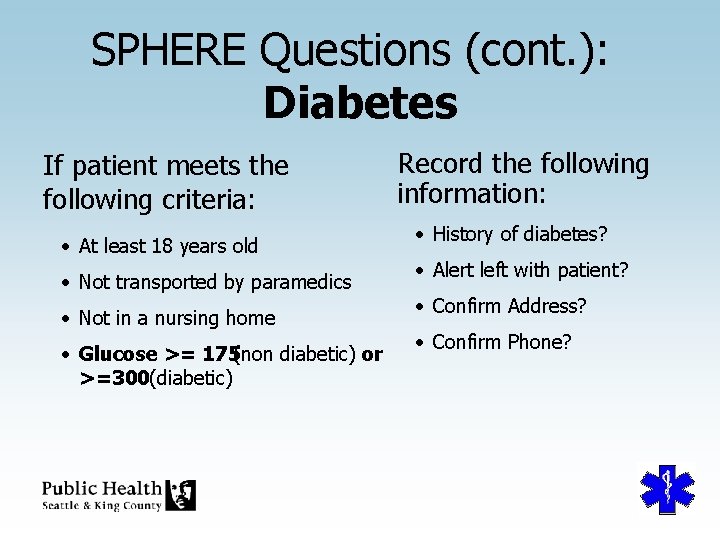
SPHERE Questions (cont. ): Diabetes If patient meets the following criteria: • At least 18 years old • Not transported by paramedics • Not in a nursing home • Glucose >= 175(non diabetic) or >=300(diabetic) Record the following information: • History of diabetes? • Alert left with patient? • Confirm Address? • Confirm Phone?
Medical Incident Report Form Education Module for 2009 BLS THE END Prepared by the Division of Emergency Medical Services
 Riskman incident reporting
Riskman incident reporting When a serious customer injury occurs
When a serious customer injury occurs Ahca airs login
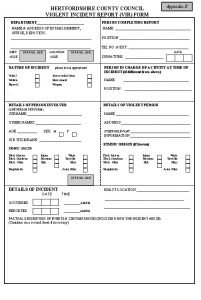
Ahca airs login Violent incident report form
Violent incident report form Patient safety incident reporting form
Patient safety incident reporting form Incident objectives that drive incident operations
Incident objectives that drive incident operations Difference between medical report and medical certificate
Difference between medical report and medical certificate Access vr phone number
Access vr phone number Education without burden
Education without burden Aeis report 2009
Aeis report 2009 2009 pearson education inc
2009 pearson education inc 2009 pearson education inc
2009 pearson education inc 2009 pearson education inc
2009 pearson education inc Copyright 2009 pearson education inc
Copyright 2009 pearson education inc Copyright 2009 pearson education inc
Copyright 2009 pearson education inc Pearson education 2009
Pearson education 2009 2009 pearson education inc
2009 pearson education inc Copyright 2009 pearson education inc
Copyright 2009 pearson education inc Punjab free and compulsory education act 2014
Punjab free and compulsory education act 2014 2009 pearson education inc
2009 pearson education inc Copyright 2009 pearson education inc
Copyright 2009 pearson education inc 2009 pearson education inc
2009 pearson education inc Copyright 2009 pearson education inc
Copyright 2009 pearson education inc Bus incident report
Bus incident report Grays harbor incident report
Grays harbor incident report ققق4
ققق4 Sit report fire
Sit report fire Incident report uncc
Incident report uncc Special incident report
Special incident report Hazardous materials incident report
Hazardous materials incident report