Marylands AllPayer Model and Future Enhanced Total Cost

- Slides: 55
Maryland’s All-Payer Model and Future Enhanced Total Cost of Care Model North Carolina HFMA Annual Conference Brett Mc. Cone, Maryland Hospital Association March 12, 2018
Maryland All-Payer Model (Waiver) § All-payer system § All pay the same price for same service in each hospital (Medicare, Medicaid, self-pay and commercial) § Rate setting system § Health Service Cost Review Commission (HSCRC) sets hospital rates § Federal Medicare payment rules had to be “waived” § Brings over $2 billion annually into Maryland § Medicare and Medicaid pay higher hospital rates than they would outside of Maryland, because they pay for the cost of hospital care 2
Maryland All-Payer Model (Waiver) § Hospitals shift to global budgets § Entered into new agreement with CMS in 2014; We are in year five of the five-year agreement § Next phase focused on “Total Cost of Care” § Negotiation underway with CMS 3
Discussion Topics I. HSCRC and early rate setting II. System Redesign and Charge Per Case III. The Second Medicare Waver and Global Budgets IV. The Future 4

Maryland Health Services Cost Review Commission (HSCRC) & early years of rate setting 5
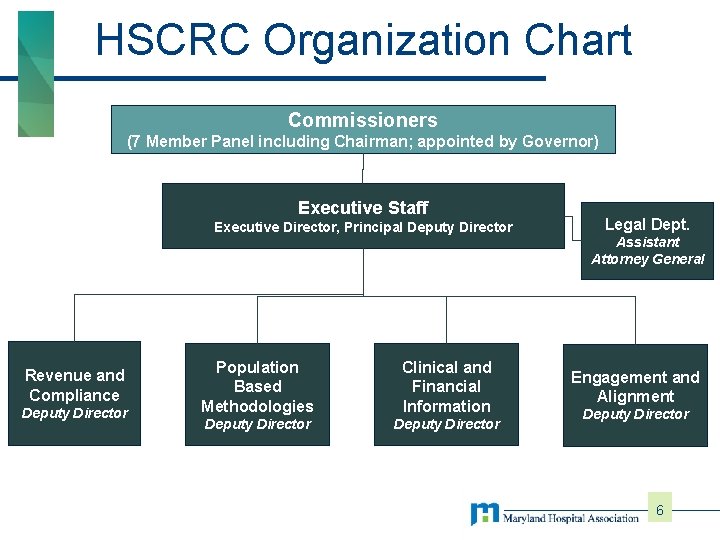
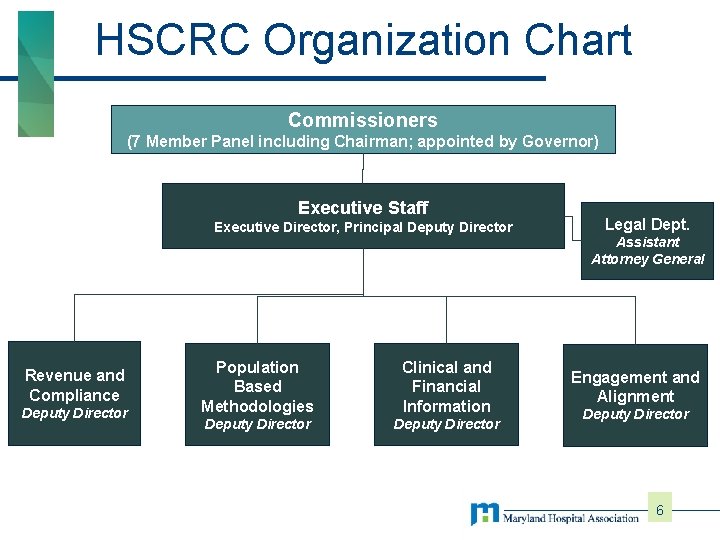
HSCRC Organization Chart Commissioners (7 Member Panel including Chairman; appointed by Governor) Executive Staff Executive Director, Principal Deputy Director Revenue and Compliance Deputy Director Population Based Methodologies Clinical and Financial Information Deputy Director Legal Dept. Assistant Attorney General Engagement and Alignment Deputy Director 6
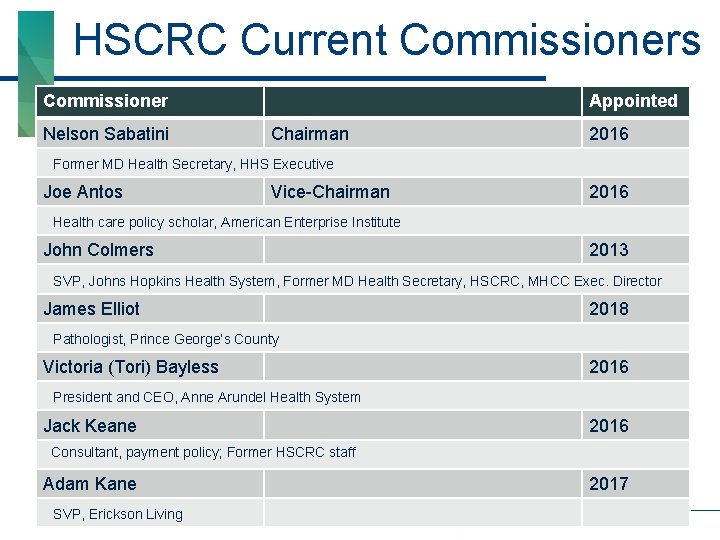
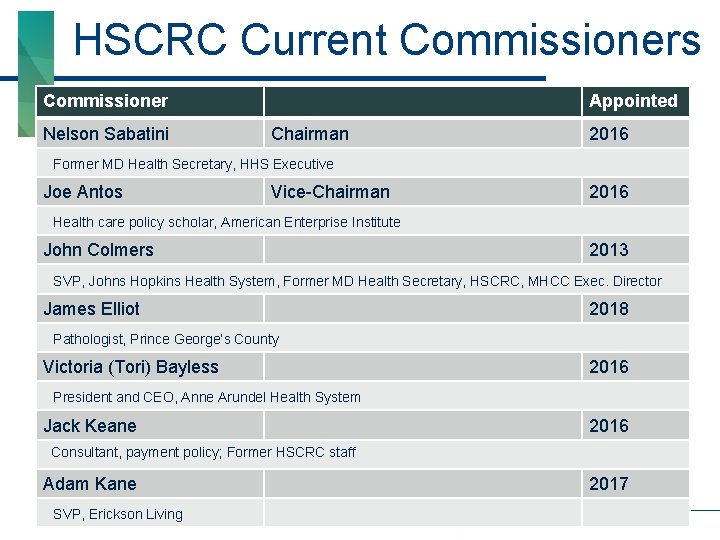
HSCRC Current Commissioners Commissioner Nelson Sabatini Appointed Chairman 2016 Former MD Health Secretary, HHS Executive Joe Antos Vice-Chairman 2016 Health care policy scholar, American Enterprise Institute John Colmers 2013 SVP, Johns Hopkins Health System, Former MD Health Secretary, HSCRC, MHCC Exec. Director James Elliot 2018 Pathologist, Prince George’s County Victoria (Tori) Bayless 2016 President and CEO, Anne Arundel Health System Jack Keane 2016 Consultant, payment policy; Former HSCRC staff Adam Kane SVP, Erickson Living 2017 7
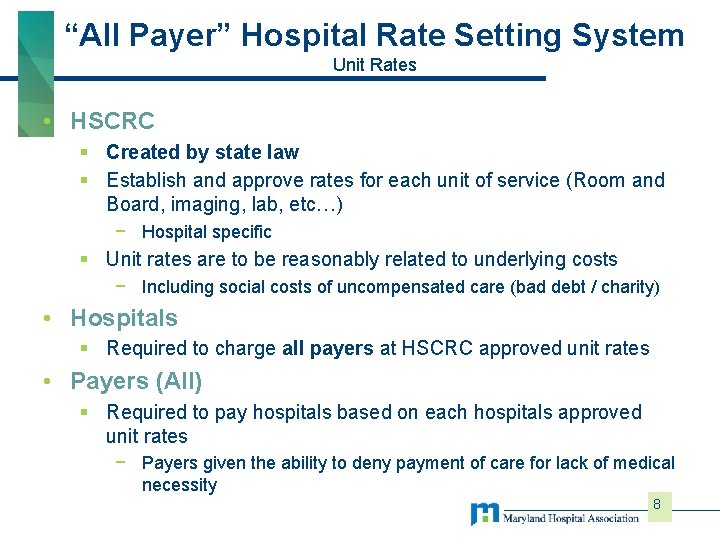
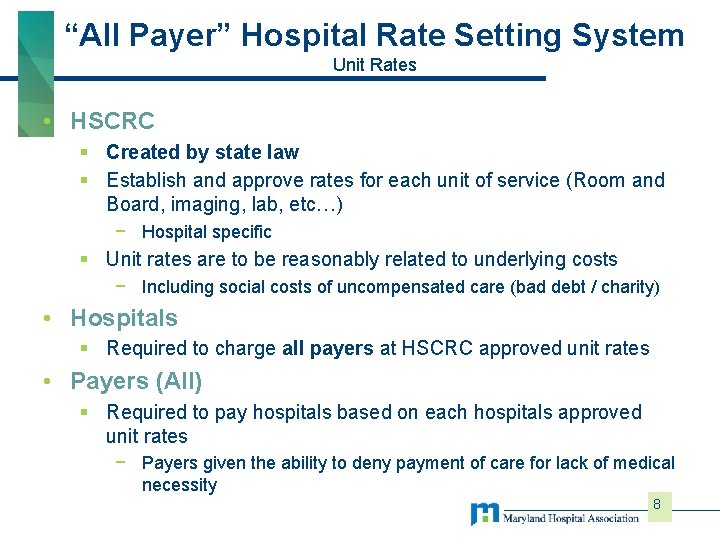
“All Payer” Hospital Rate Setting System Unit Rates • HSCRC § Created by state law § Establish and approve rates for each unit of service (Room and Board, imaging, lab, etc…) − Hospital specific § Unit rates are to be reasonably related to underlying costs − Including social costs of uncompensated care (bad debt / charity) • Hospitals § Required to charge all payers at HSCRC approved unit rates • Payers (All) § Required to pay hospitals based on each hospitals approved unit rates − Payers given the ability to deny payment of care for lack of medical necessity 8
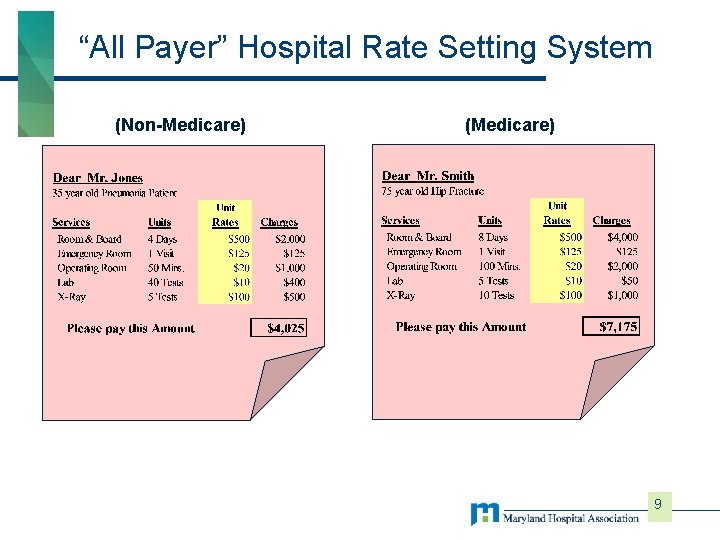
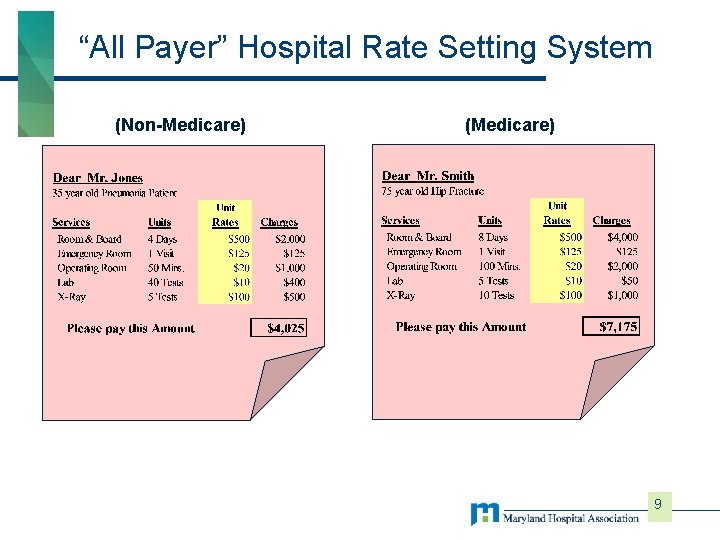
“All Payer” Hospital Rate Setting System (Non-Medicare) (Medicare) 9
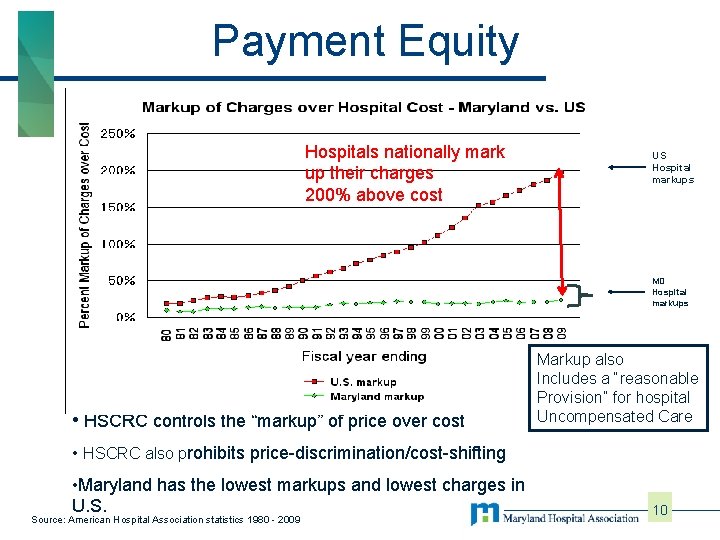
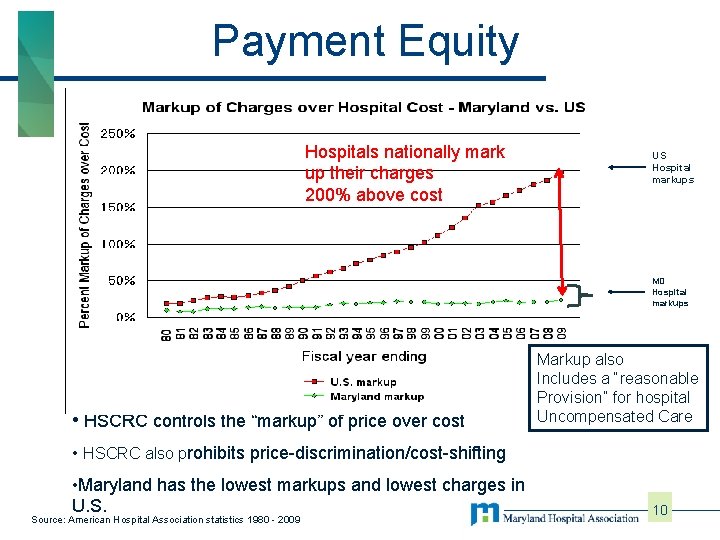
Payment Equity Hospitals nationally mark up their charges 200% above cost US Hospital markups MD Hospital markups • HSCRC controls the “markup” of price over cost Markup also Includes a “reasonable Provision” for hospital Uncompensated Care • HSCRC also prohibits price-discrimination/cost-shifting • Maryland has the lowest markups and lowest charges in U. S. Source: American Hospital Association statistics 1980 - 2009 10
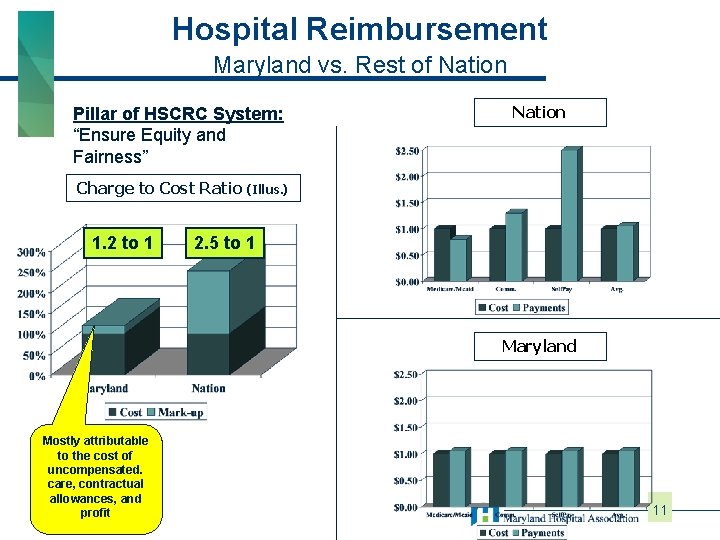
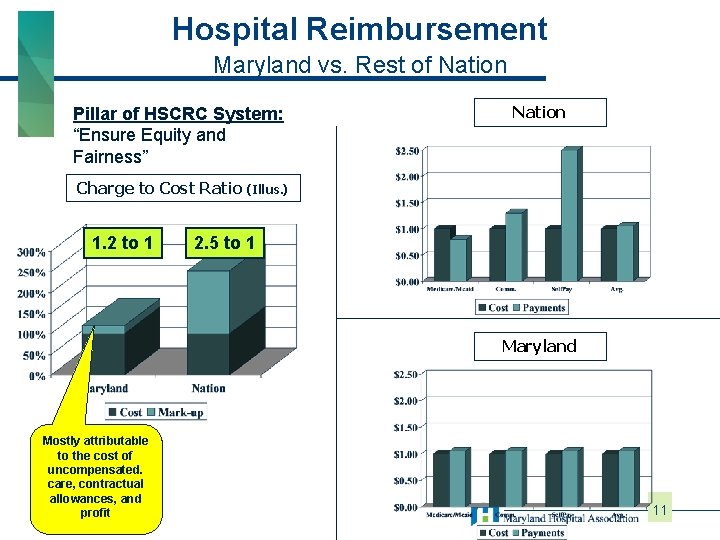
Hospital Reimbursement Maryland vs. Rest of Nation Pillar of HSCRC System: “Ensure Equity and Fairness” Charge to Cost Ratio 1. 2 to 1 Nation (Illus. ) 2. 5 to 1 Maryland Mostly attributable to the cost of uncompensated. care, contractual allowances, and profit 11
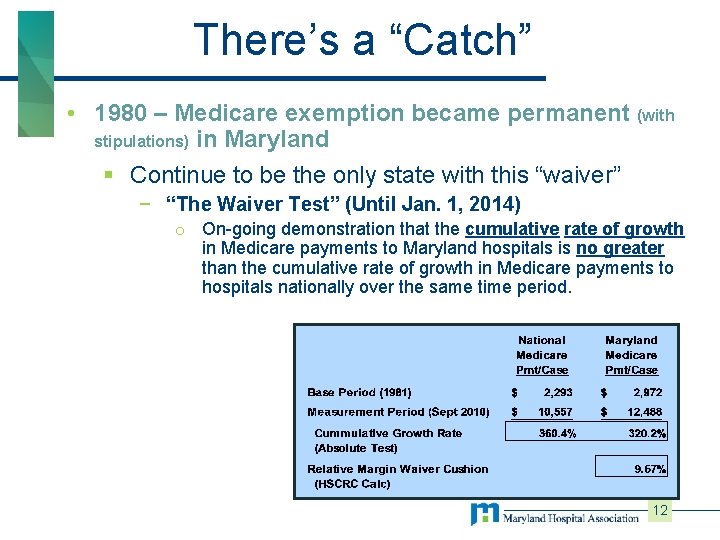
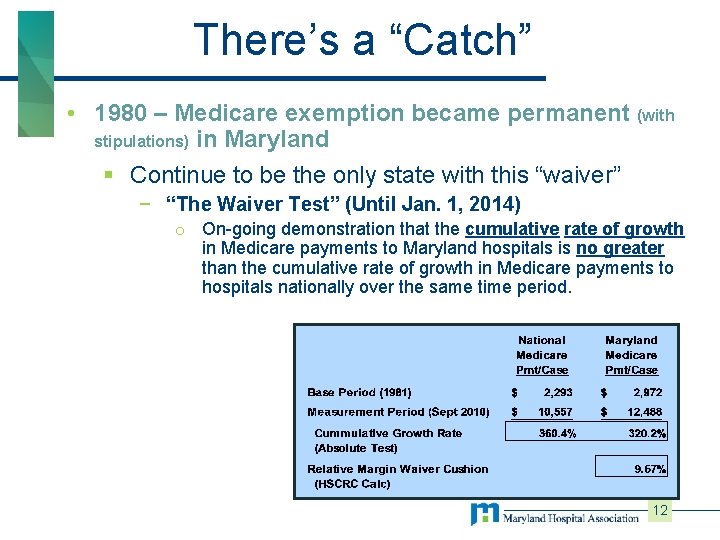
There’s a “Catch” • 1980 – Medicare exemption became permanent (with stipulations) in Maryland § Continue to be the only state with this “waiver” − “The Waiver Test” (Until Jan. 1, 2014) o On-going demonstration that the cumulative rate of growth in Medicare payments to Maryland hospitals is no greater than the cumulative rate of growth in Medicare payments to hospitals nationally over the same time period. 12
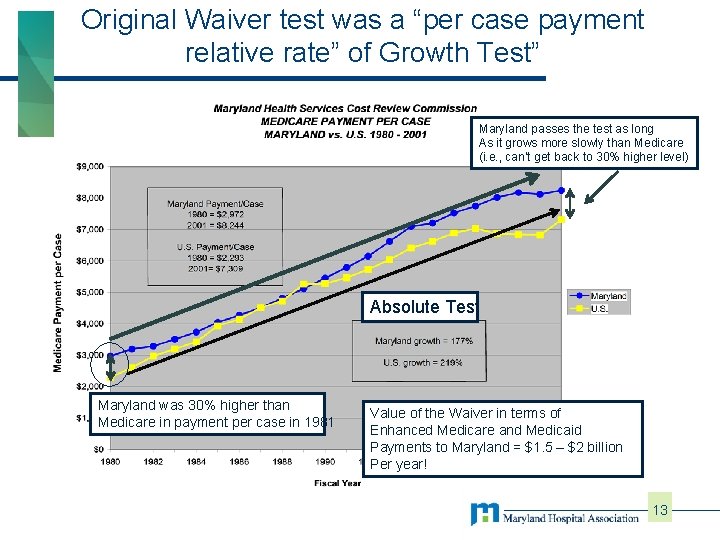
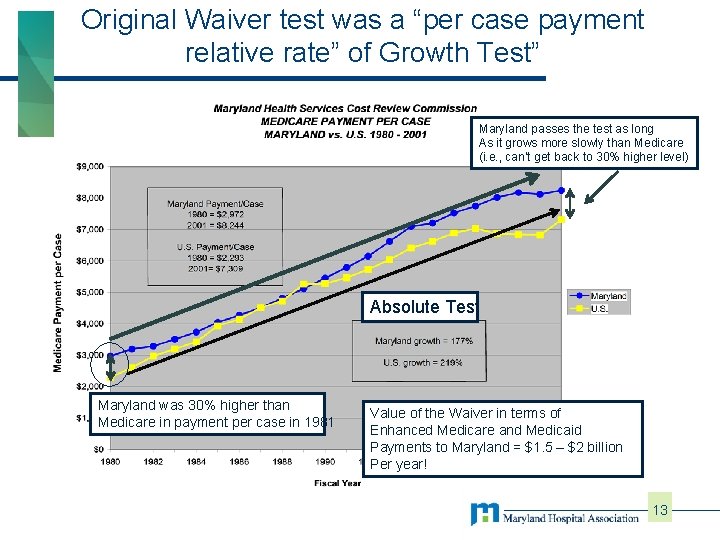
Original Waiver test was a “per case payment relative rate” of Growth Test” Maryland passes the test as long As it grows more slowly than Medicare (i. e. , can’t get back to 30% higher level) Absolute Test Maryland was 30% higher than Medicare in payment per case in 1981 Value of the Waiver in terms of Enhanced Medicare and Medicaid Payments to Maryland = $1. 5 – $2 billion Per year! 13
System Redesign and Charge per Case 14
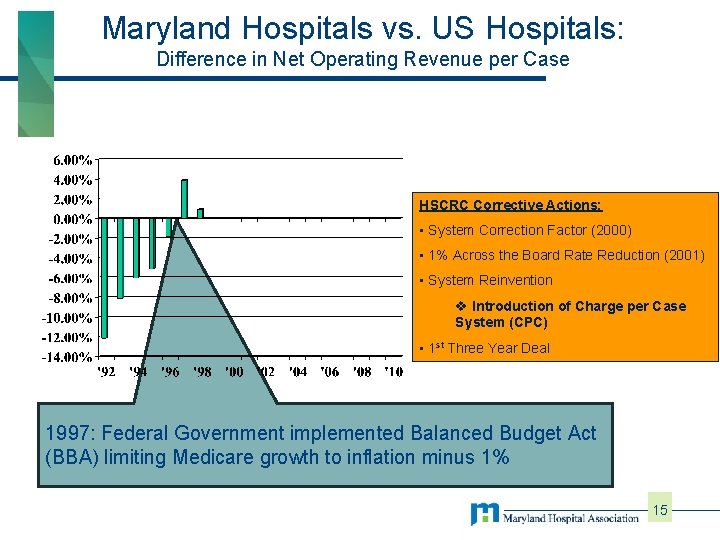
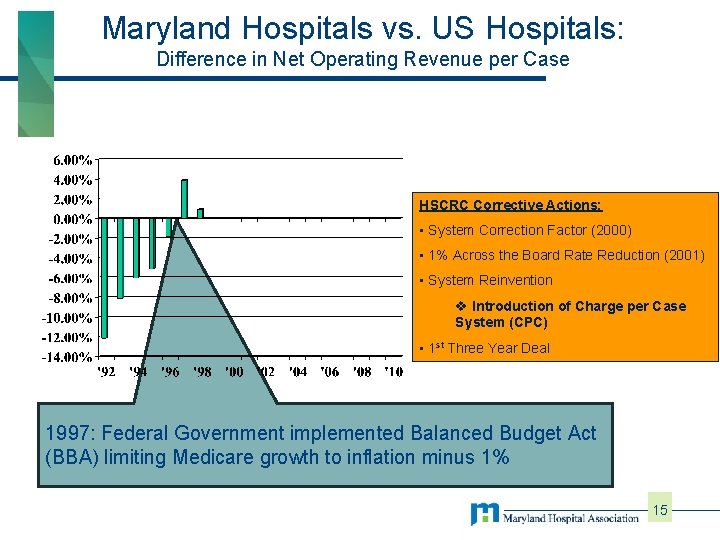
Maryland Hospitals vs. US Hospitals: Difference in Net Operating Revenue per Case HSCRC Corrective Actions: • System Correction Factor (2000) • 1% Across the Board Rate Reduction (2001) • System Reinvention v Introduction of Charge per Case System (CPC) • 1 st Three Year Deal 1997: Federal Government implemented Balanced Budget Act (BBA) limiting Medicare growth to inflation minus 1% 15
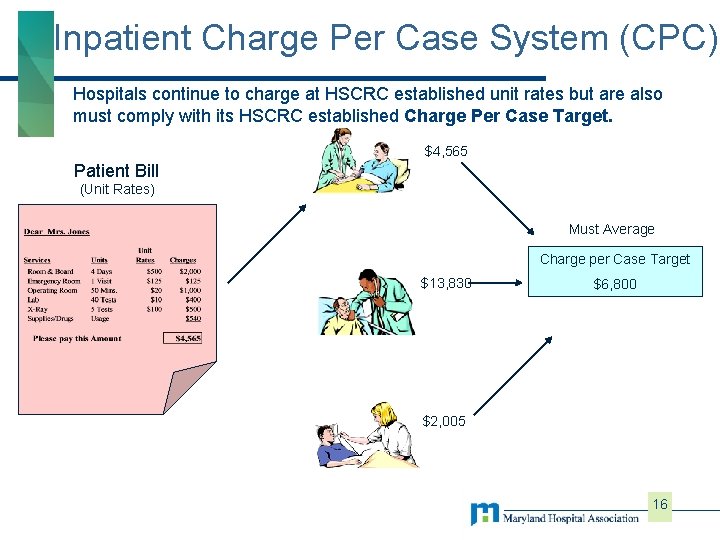
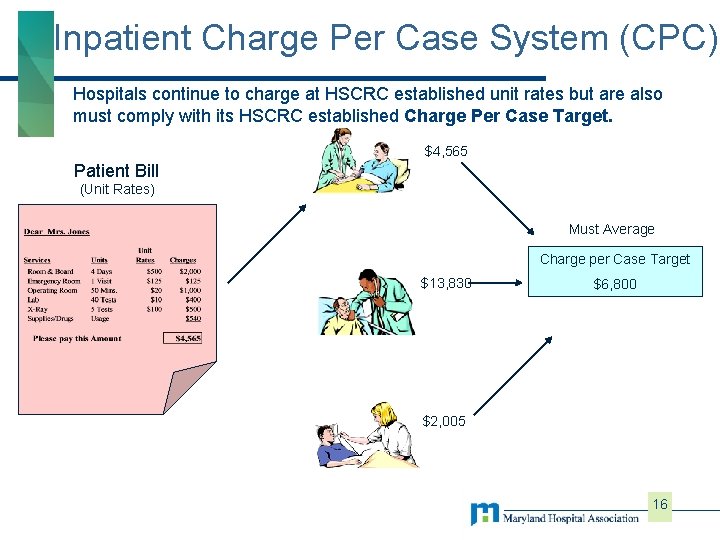
Inpatient Charge Per Case System (CPC) Hospitals continue to charge at HSCRC established unit rates but are also must comply with its HSCRC established Charge Per Case Target. $4, 565 Patient Bill (Unit Rates) Must Average Charge per Case Target $13, 830 $6, 800 $2, 005 16
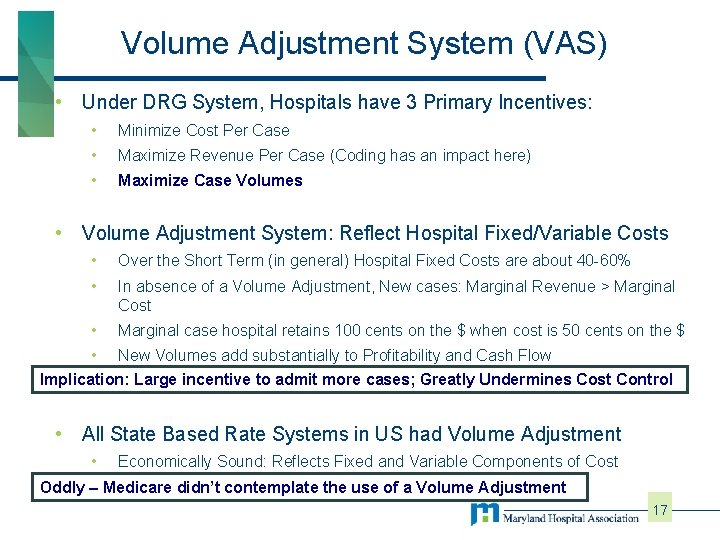
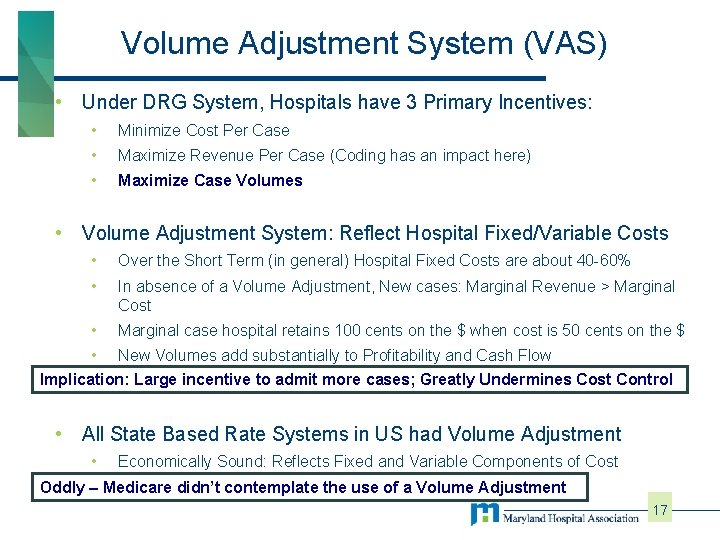
Volume Adjustment System (VAS) • Under DRG System, Hospitals have 3 Primary Incentives: • Minimize Cost Per Case • Maximize Revenue Per Case (Coding has an impact here) • Maximize Case Volumes • Volume Adjustment System: Reflect Hospital Fixed/Variable Costs • Over the Short Term (in general) Hospital Fixed Costs are about 40 -60% • In absence of a Volume Adjustment, New cases: Marginal Revenue > Marginal Cost • Marginal case hospital retains 100 cents on the $ when cost is 50 cents on the $ • New Volumes add substantially to Profitability and Cash Flow Implication: Large incentive to admit more cases; Greatly Undermines Cost Control • All State Based Rate Systems in US had Volume Adjustment • Economically Sound: Reflects Fixed and Variable Components of Cost Acts as adidn’t “Break” on incentivethe to use do unnecessary Oddly – • Medicare contemplate of a Volumevolume Adjustment 17
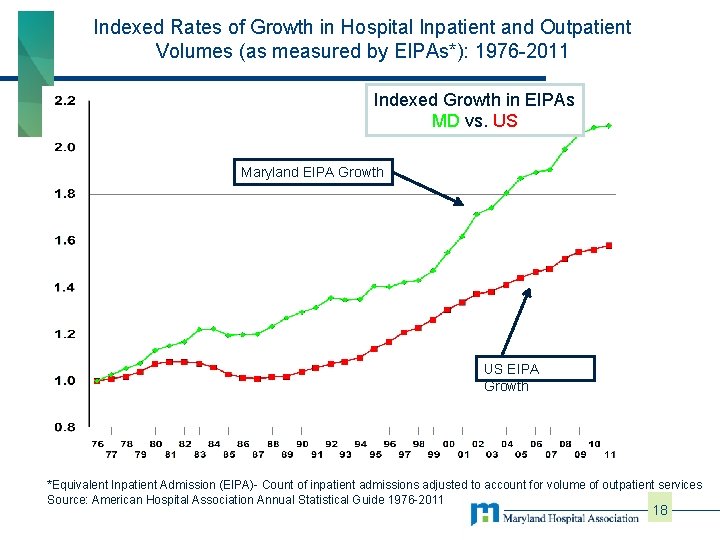
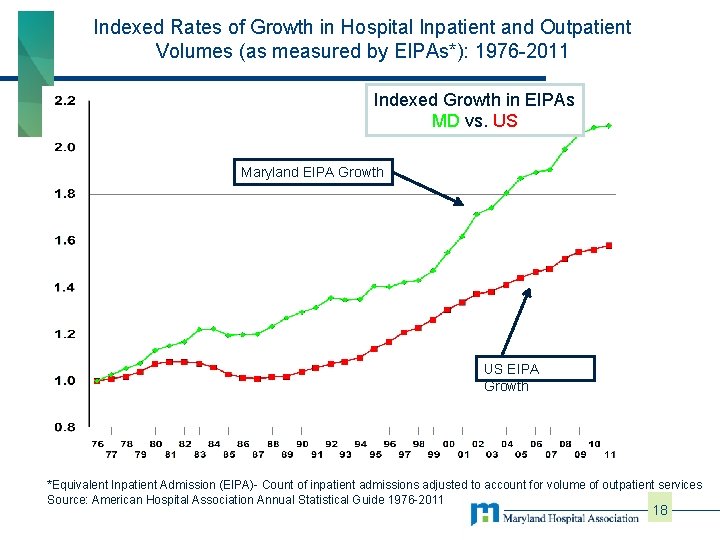
Indexed Rates of Growth in Hospital Inpatient and Outpatient Volumes (as measured by EIPAs*): 1976 -2011 Indexed Growth in EIPAs MD vs. US Maryland EIPA Growth US EIPA Growth *Equivalent Inpatient Admission (EIPA)- Count of inpatient admissions adjusted to account for volume of outpatient services Source: American Hospital Association Annual Statistical Guide 1976 -2011 18
The Second Waiver Test and Move to Value 19
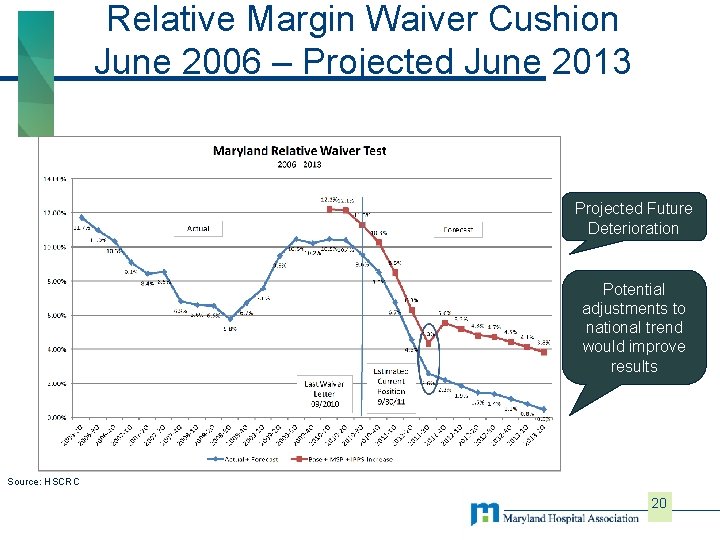
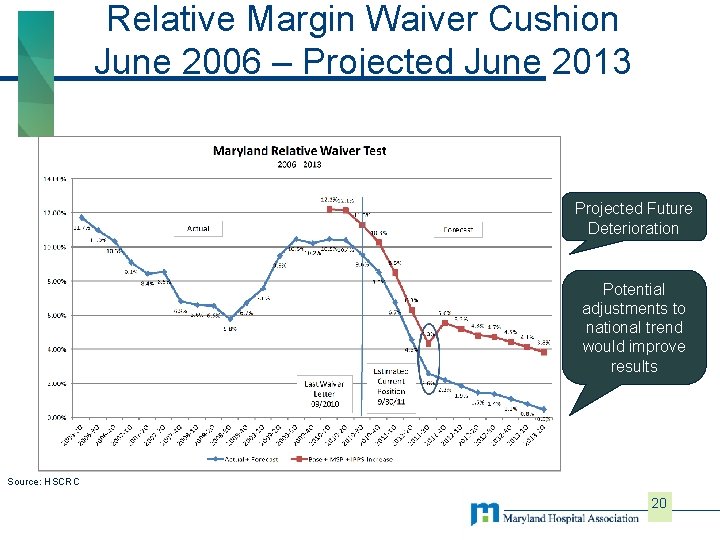
Relative Margin Waiver Cushion June 2006 – Projected June 2013 Projected Future Deterioration Potential adjustments to national trend would improve results Source: HSCRC 20
Overarching Concern for Maryland Hospitals • Changes to the healthcare delivery system will challenge the current waiver test: • Shift of cases to Observation increases the average charge per admission in Maryland • Impact of 2 -midnight rule • New payment initiatives (first generation of global budgets, readmission programs, etc. ) provide incentives to reduce utilization, increasing the average charge per admission • Medicaid budget issues 21
Background • On October 10, 2013, the State of Maryland applied to the Center for Medicare and Medicaid Innovation (CMMI) for a demonstration project to improve outcomes, to enhance patient experience and to control costs. • The application was approved on January 10, 2014 • The resulting All-Payer Model (“the Model”) shifts the focus from historic price per encounter controls to a focus on overall revenue growth, including price and use. 22
Background • The New Model includes the following provisions: § Annual all-payer, per capita, total hospital cost growth limited to 3. 58% § Maryland’s Medicare per beneficiary total hospital cost growth rate must be below the national Medicare per beneficiary average, resulting in $330 m of Medicare savings over five years − 80% of Maryland hospital revenue shifted into global payment models by year 5 § Maryland’s Medicare per beneficiary total cost growth rate cannot exceed the national average by more than 1 percentage point in year 1, and must be “break even” with the national average by year 3. 23
Background • The New Model includes the following provisions (cont. ): § Maryland will reduce its 30 -day Medicare readmission rate to the national average in five years § Annual Potentially Preventable Complication (PPC) reduction of 6. 89%, for a cumulative 5 year reduction of 30%. § Maryland will propose a model extension at the start of Year 4 § Maryland elects to no longer be paid under Section 1814(b)(3) of the SSA: Maryland’s historic Waiver Test − If the Model is not extended, or terminated early, Maryland hospitals will transition to the national Medicare payment systems. 24
Financial Targets: All-Payer Test • All-payer per capita growth rate of 3. 58% is the ten year average annual growth rate in Maryland Gross State Product (GSP) per capita (2002 – 2012) • 3. 58% is fixed cap for years 1 -3. In years 4 and 5, Maryland may adjust the all-payer cap for more recently available GSP data. • The all-payer per capita growth rate is expected to be calculated using: § Regulated, inpatient and outpatient hospital charges, from Maryland hospitals for Maryland residents receiving services. § Population growth from the Maryland Department of Planning. 25
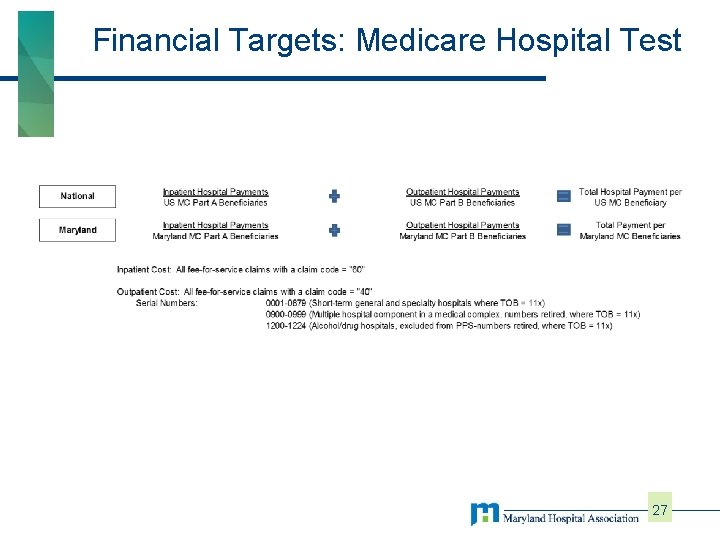
Financial Targets: Medicare Hospital Test • Baseline = CY 2013 Medicare hospital payments for Maryland Medicare beneficiaries • Maryland Medicare beneficiaries = All Maryland residents who are (Medicare) fee-for-service beneficiaries enrolled in Part A and/or Part B • Includes Medicare payments, regardless of georaphic service locations: in-state and out-ofstate 26
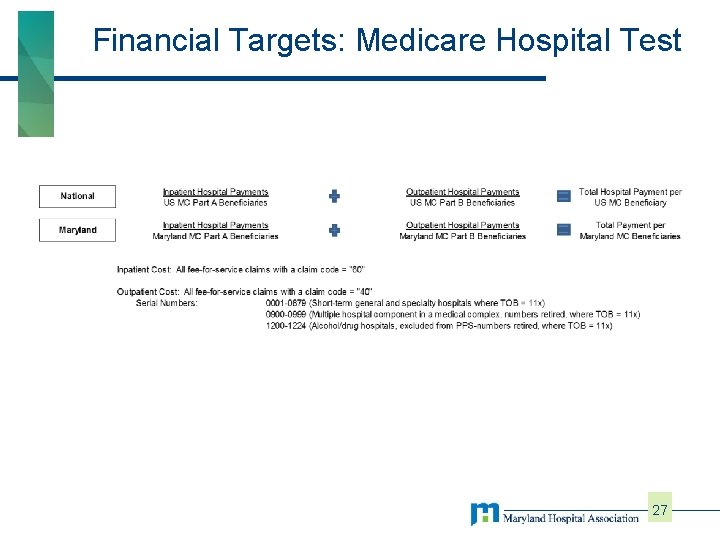
Financial Targets: Medicare Hospital Test 27
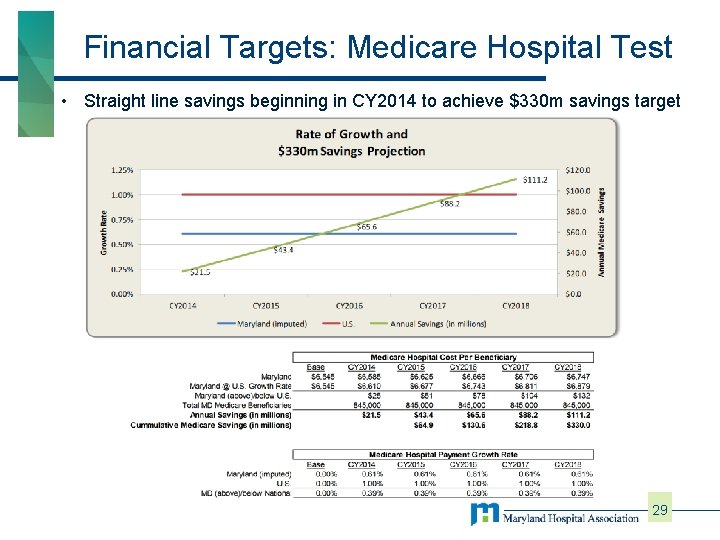
Financial Targets: Medicare Hospital Test • A CY 2013 baseline will also be established for the national average • The savings test will compare the actual growth rate of the Maryland hospital payment per beneficiary versus the applied national (actual) growth rate to the baseline Maryland hospital payment per beneficiary. § § The growth rate differential applied to the Maryland beneficiary total will compute the annual savings The agreement reflects a savings targets that assumes no savings in year 1 and approximately 0. 5% below the national trend in years 2 -5. • The assumptions and chart on the next page is an illustrative, example calculations. (Here’s what we thought going into the new Waiver…) 28
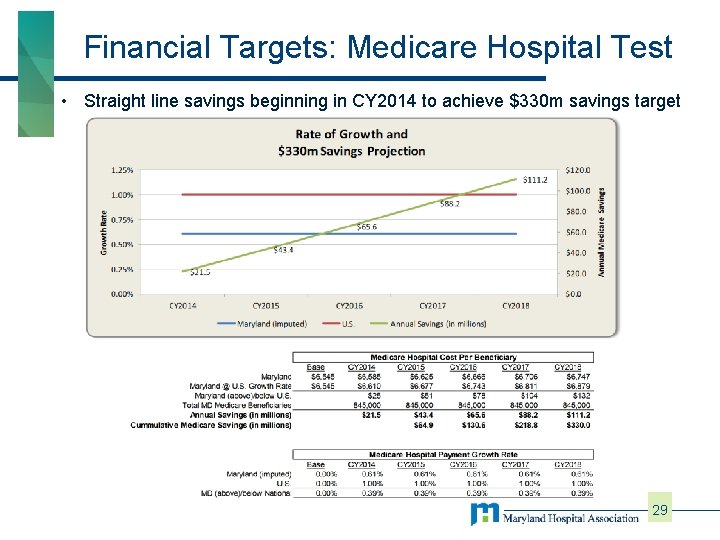
Financial Targets: Medicare Hospital Test • Straight line savings beginning in CY 2014 to achieve $330 m savings target 29
Financial Targets: Medicare Total Payment Test • The Medicare “Total” Payment per beneficiary test is similar to the Hospital Payment per beneficiary test § Compares Maryland’s growth rate to the national growth rate • Rather than defined savings, Maryland’s Medicare per beneficiary total cost growth rate cannot exceed the national average by more than 1 percentage point in year 1, and cannot exceed the national average in any two consecutive years § CMS concerned with shifts to unregulated or other services • Total payments include SNF, Home Health, Physician Services, Hospitals, etc. 30
Quality Test: Readmissions • Maryland maintains its waiver from the CMS Hospital Readmission Reduction Program. • To do so, Maryland will reduce 30 -day Medicare readmission rate to the national average in five years 31
Quality Test: Potentially Preventable Complication’s (PPC’s) • Maryland maintains its waiver from the CMS Hospital Acquired Conditions (HAC) Program. • Maryland will achieve an annual, aggregate reduction of 6. 89% in 65 PPC’s • 30% reduction over 5 years 32
Proposed Terms • During the five year period, there are specific events that will lead to further review by CMS and potentially early termination: § § Failure to achieve (Medicare) savings for two consecutive years Failure to meet the cumulative (Medicare) savings target by $100 m or more at any point during the life of the model Annual growth in Maryland Medicare per beneficiary total cost that is more than 1% point greater than the national average Determination of significant quality of care deterioration • Should any of these occur, CMS will provide notice to Maryland. § § Maryland has 90 days to respond, with CMS having 90 days to accept the response or request a corrective action plan, due in 30 days. If the corrective action plan is not implemented successfully within 1 year of notification, CMS may terminate the agreement. 33
HSCRC Policy Impacts • To achieve success under the Model, HSCRC Staff have taken several actions, including: § Negotiating either a Global Budgeted Revenue (GBR) agreement with almost every hospital in the State. § Implementing a series of workgroups and committees to assist with implementation − Overall Advisory Council that identified guiding principles − Other workgroups to address critical success factors (physician alignment, performance improvement, etc. ) − Sub-workgroups to address certain technical issue's (transfer policy, demographic adjustment, etc. ) § Establishing policies to address the non-financial measures (PPC’s and readmissions) 34
HSCRC Policy Impacts: GBR • Consistent with the Model’s provision to shift 80% of Maryland hospital revenue into global payment models by year 5, Staff established new GBR agreements with all hspitals § 95% of revenue is under a global model at the end of year 1 • The GBR agreements establish a fixed amount of regulated charges for each hospital. The cap/floor was based on FY 2013 experience, with certain adjustments and allowances for infrastructure 35
HSCRC Policy Impacts: GBR • Under GBR, hospitals receive annual adjustments for: § Inflation § Change in markup (payer mix and UCC via the UCC pool) § Population/Demographics • There are no explicit adjustments for changes in: § Volume (I/P or O/P) § Case Mix/Severity 36
HSCRC Policy Impacts: GBR and TPR • GBR arrangements are designed to encourage efficient and effective service delivery § Right patient, right time, right setting § Reduce or eliminate “potentially avoidable utilization” or PAU − PAU’s include several types of volumes: Readmissions, PPC’s and AHRQ’s Prevention Quality Indicators (PQI; Patients admitted for ambulatory sensitive conditions), 30 day observation and ED re-encounters, etc. § Deliver care in the lowest cost setting § Monitor and emphasize quality measures to prevent quality decline § Hospital billing: Fee for service, unit rates are adjusted up or down based on ability to change PAUs within total global budget 37
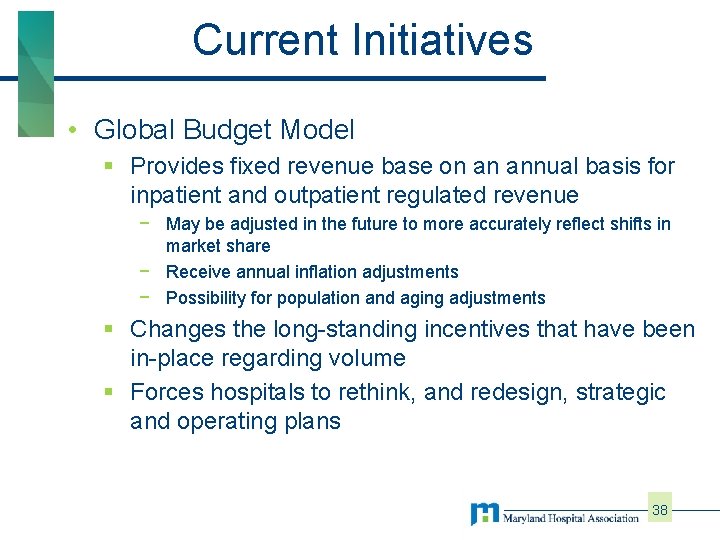
Current Initiatives • Global Budget Model § Provides fixed revenue base on an annual basis for inpatient and outpatient regulated revenue − May be adjusted in the future to more accurately reflect shifts in market share − Receive annual inflation adjustments − Possibility for population and aging adjustments § Changes the long-standing incentives that have been in-place regarding volume § Forces hospitals to rethink, and redesign, strategic and operating plans 38
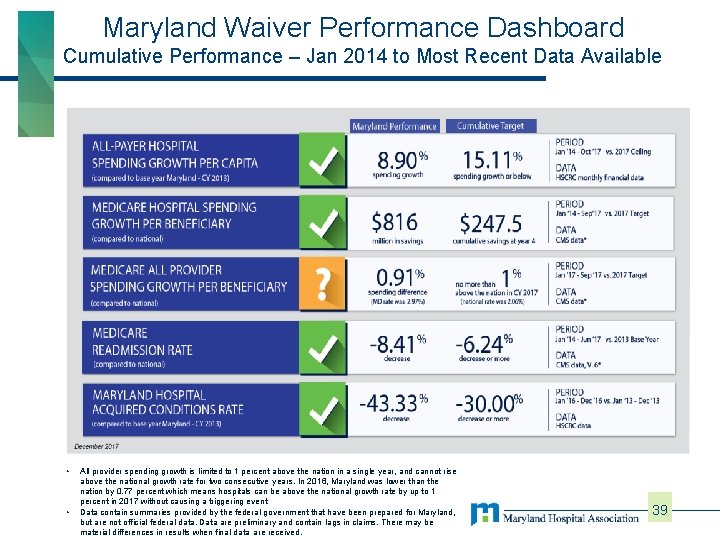
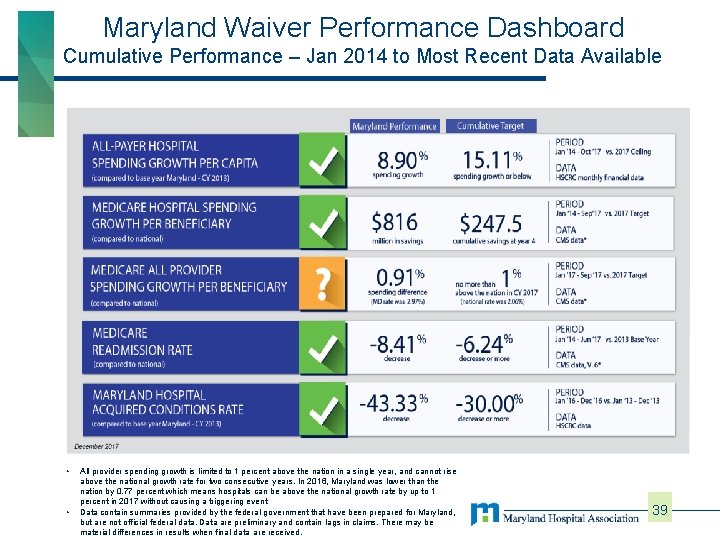
Maryland Waiver Performance Dashboard Cumulative Performance – Jan 2014 to Most Recent Data Available • • All provider spending growth is limited to 1 percent above the nation in a single year, and cannot rise above the national growth rate for two consecutive years. In 2016, Maryland was lower than the nation by 0. 77 percent which means hospitals can be above the national growth rate by up to 1 percent in 2017 without causing a triggering event Data contain summaries provided by the federal government that have been prepared for Maryland, but are not official federal data. Data are preliminary and contain lags in claims. There may be material differences in results when final data are received. 39
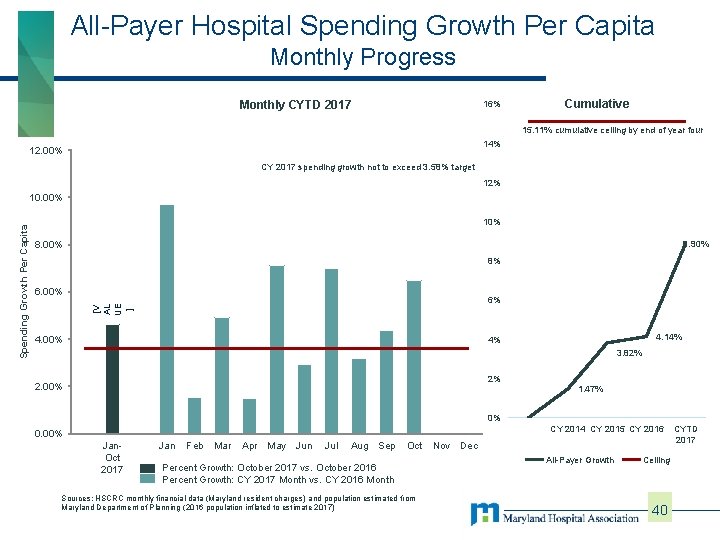
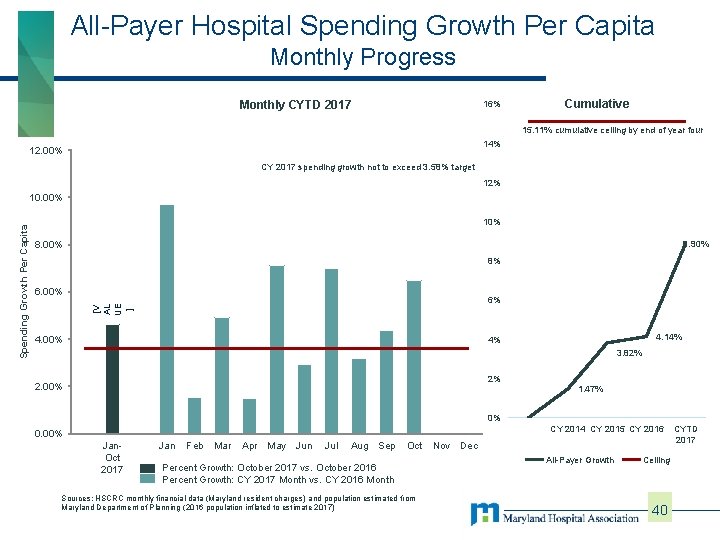
All-Payer Hospital Spending Growth Per Capita Monthly Progress Monthly CYTD 2017 16% Cumulative 15. 11% cumulative ceiling by end of year four 14% 12. 00% CY 2017 spending growth not to exceed 3. 58% target 12% 10% 8. 90% 8. 00% 8% 6. 00% 6% [V AL UE ] Spending Growth Per Capita 10. 00% 4. 14% 4% 3. 82% 2% 2. 00% 1. 47% 0% CY 2014 CY 2015 CY 2016 0. 00% Jan. Oct 2017 Jan Feb Mar Apr May Jun Jul Aug Sep Oct Percent Growth: October 2017 vs. October 2016 Percent Growth: CY 2017 Month vs. CY 2016 Month Sources: HSCRC monthly financial data (Maryland resident charges) and population estimated from Maryland Department of Planning (2016 population inflated to estimate 2017) Nov Dec All-Payer Growth Ceiling 40 CYTD 2017
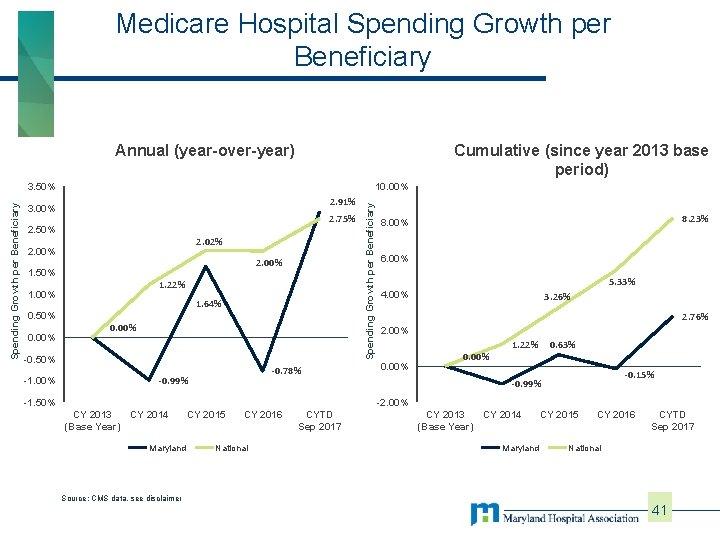
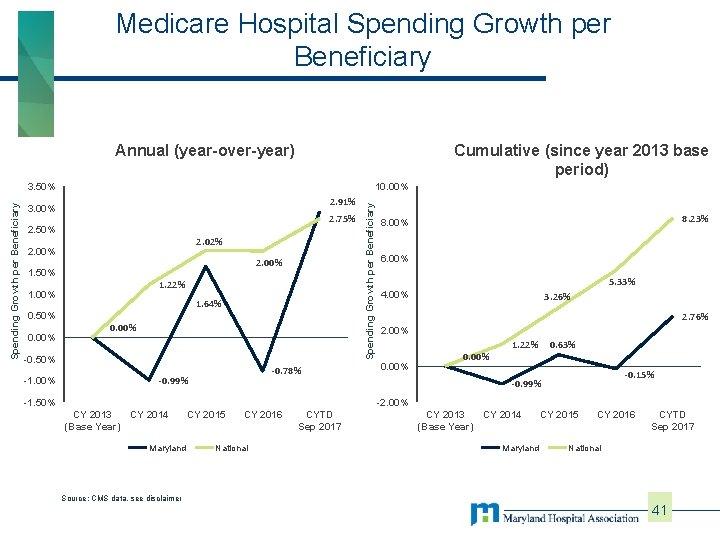
Medicare Hospital Spending Growth per Beneficiary Cumulative (since year 2013 base period) Annual (year-over-year) 10. 00% 2. 91% 3. 00% 2. 75% 2. 50% 2. 02% 2. 00% 1. 50% 1. 22% 1. 00% 0. 50% 0. 00% 1. 64% 0. 00% -0. 50% -1. 00% -0. 78% -0. 99% Spending Growth per Beneficiary 3. 50% 8. 23% 8. 00% 6. 00% 5. 33% 4. 00% 3. 26% 2. 76% 2. 00% 0. 00% 1. 22% 0. 63% -0. 15% -0. 99% -1. 50% -2. 00% CY 2013 CY 2014 (Base Year) Maryland CY 2015 CY 2016 National CYTD Sep 2017 CY 2013 CY 2014 (Base Year) Maryland CY 2015 CY 2016 CYTD Sep 2017 National Source: CMS data, see disclaimer 41
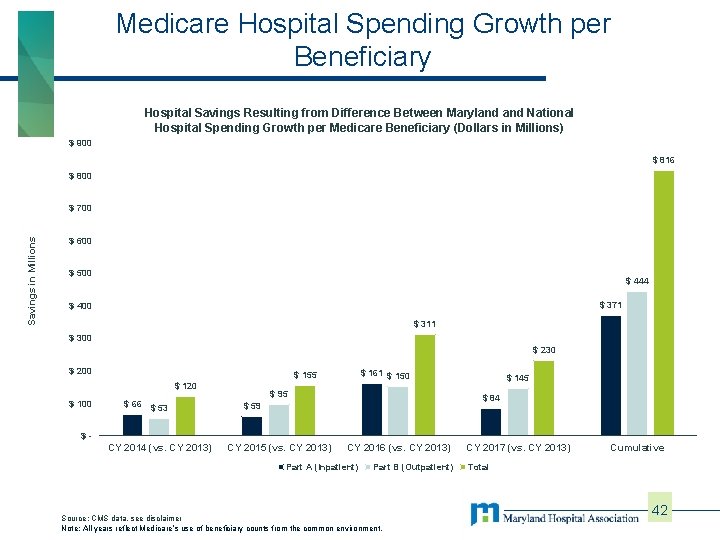
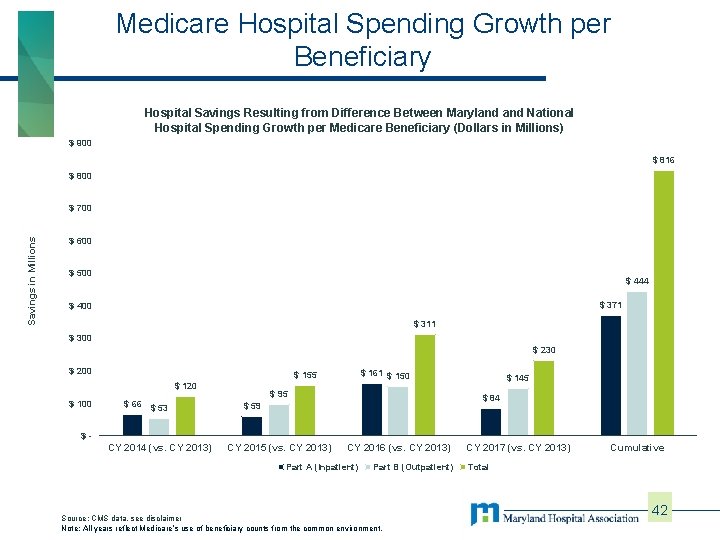
Medicare Hospital Spending Growth per Beneficiary Hospital Savings Resulting from Difference Between Maryland National Hospital Spending Growth per Medicare Beneficiary (Dollars in Millions) $ 900 $ 816 $ 800 Savings in Millions $ 700 $ 600 $ 500 $ 444 $ 371 $ 400 $ 311 $ 300 $ 230 $ 200 $ 120 $ 100 $ 161 $ 150 $ 155 $ 66 $ 53 $ 95 $ 145 $ 84 $ 59 $- CY 2014 (vs. CY 2013) CY 2015 (vs. CY 2013) CY 2016 (vs. CY 2013) Part A (Inpatient) Part B (Outpatient) Source: CMS data, see disclaimer Note: All years reflect Medicare’s use of beneficiary counts from the common environment. CY 2017 (vs. CY 2013) Cumulative Total 42
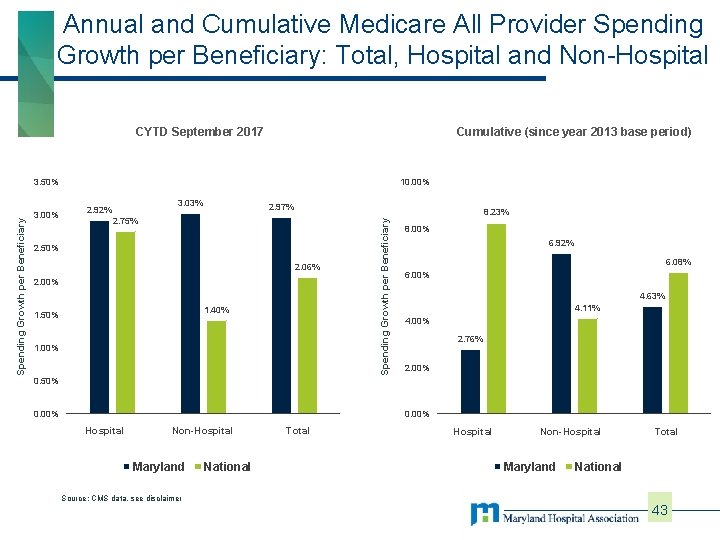
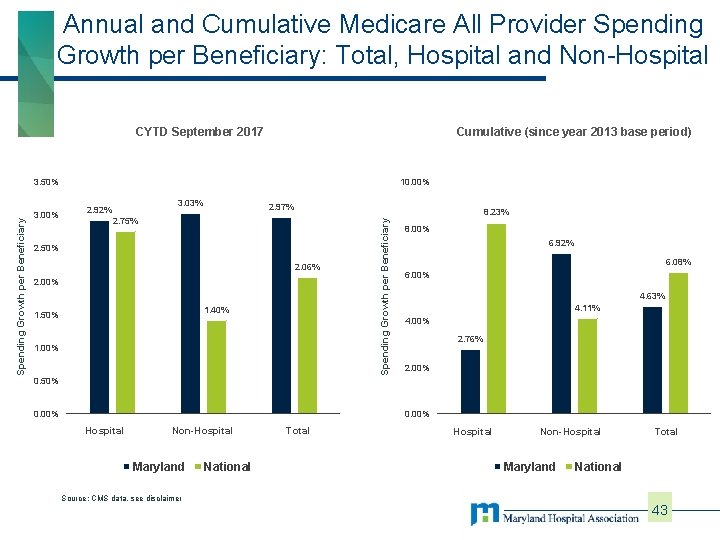
Annual and Cumulative Medicare All Provider Spending Growth per Beneficiary: Total, Hospital and Non-Hospital CYTD September 2017 Cumulative (since year 2013 base period) 3. 00% 10. 00% 3. 03% 2. 92% 2. 97% 8. 23% 2. 75% 2. 50% 2. 06% 2. 00% 1. 40% 1. 50% 1. 00% 0. 50% 0. 00% Spending Growth per Beneficiary 3. 50% 8. 00% 6. 92% 6. 08% 6. 00% 4. 63% 4. 11% 4. 00% 2. 76% 2. 00% 0. 00% hospital Hospital non Non-Hospital Maryland National total Total Hospital Non-Hospital Maryland Total National Source: CMS data, see disclaimer 43
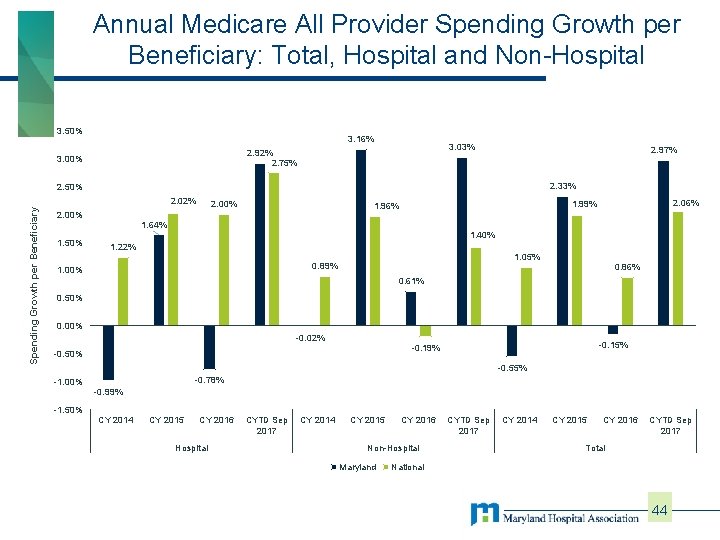
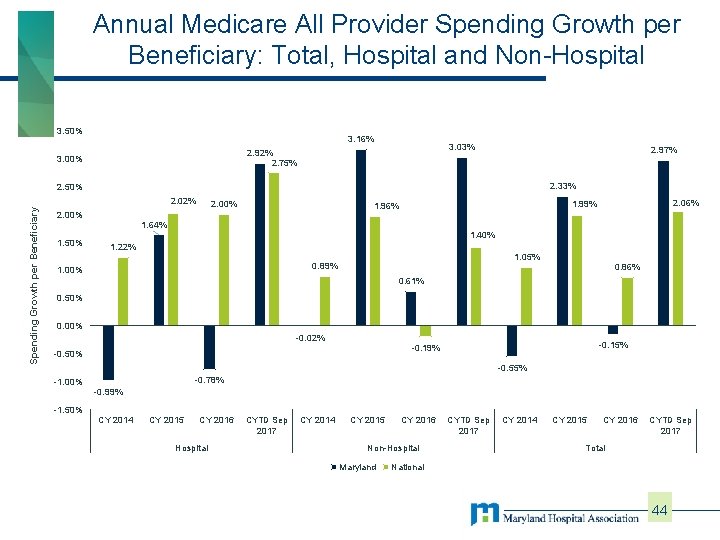
Annual Medicare All Provider Spending Growth per Beneficiary: Total, Hospital and Non-Hospital 3. 50% 3. 16% 3. 03% 2. 92% 2. 75% 3. 00% 2. 97% 2. 33% 2. 50% Spending Growth per Beneficiary 2. 02% 2. 00% 2. 06% 1. 99% 1. 96% 2. 00% 1. 64% 1. 50% 1. 40% 1. 22% 1. 05% 0. 89% 1. 00% 0. 86% 0. 61% 0. 50% 0. 00% -0. 02% -0. 15% -0. 19% -0. 50% -0. 55% -0. 78% -1. 00% -0. 99% -1. 50% CY 2014 CY 2015 CY 2016 Hospital CYTD Sep 2017 CY 2014 CY 2015 CY 2016 Non-Hospital Maryland CYTD Sep 2017 CY 2014 CY 2015 CY 2016 CYTD Sep 2017 Total National 44
Hospital Views Environment: • Support for demo concept; progress to date • Frustration with implementation • No acknowledgement of investments to date • CMS slow to approve/overly prescriptive with needed policy changes 45
Future Model 46
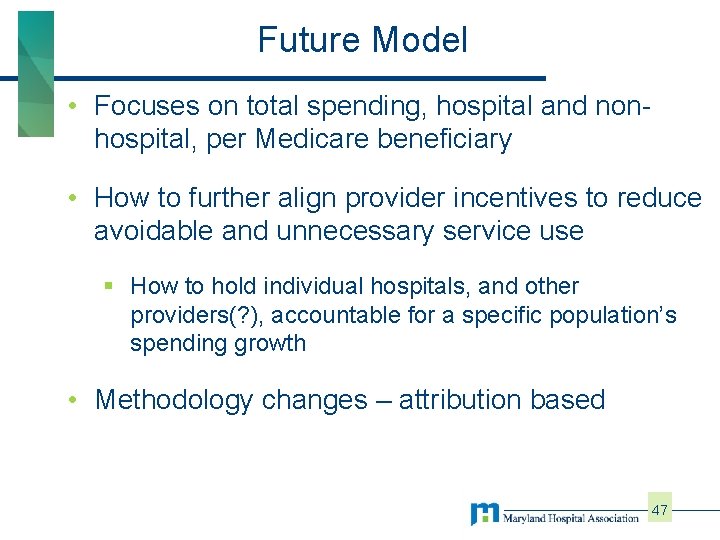
Future Model • Focuses on total spending, hospital and nonhospital, per Medicare beneficiary • How to further align provider incentives to reduce avoidable and unnecessary service use § How to hold individual hospitals, and other providers(? ), accountable for a specific population’s spending growth • Methodology changes – attribution based 47
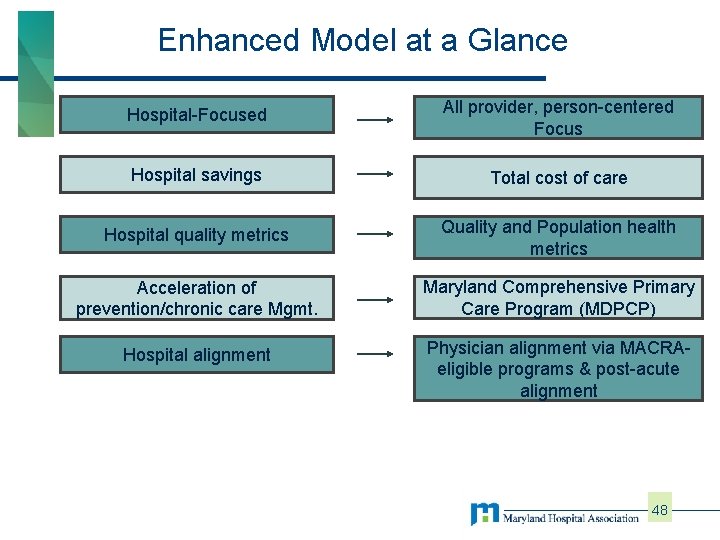
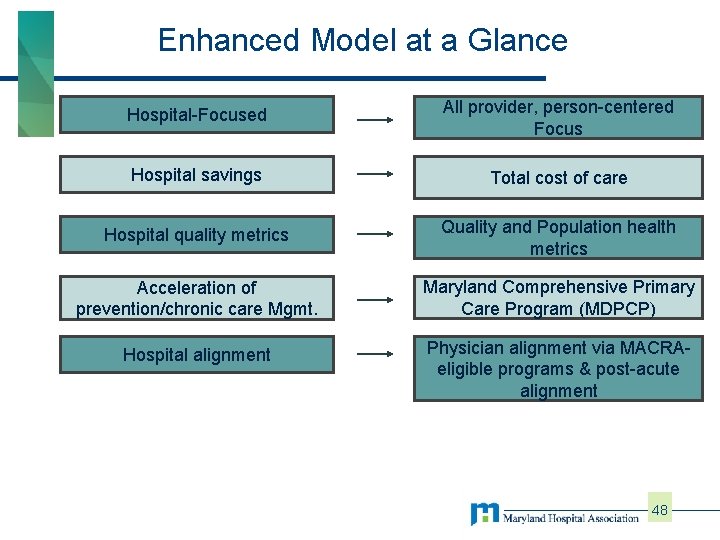
Enhanced Model at a Glance Hospital-Focused All provider, person-centered Focus Hospital savings Total cost of care Hospital quality metrics Quality and Population health metrics Acceleration of prevention/chronic care Mgmt. Maryland Comprehensive Primary Care Program (MDPCP) Hospital alignment Physician alignment via MACRAeligible programs & post-acute alignment 48
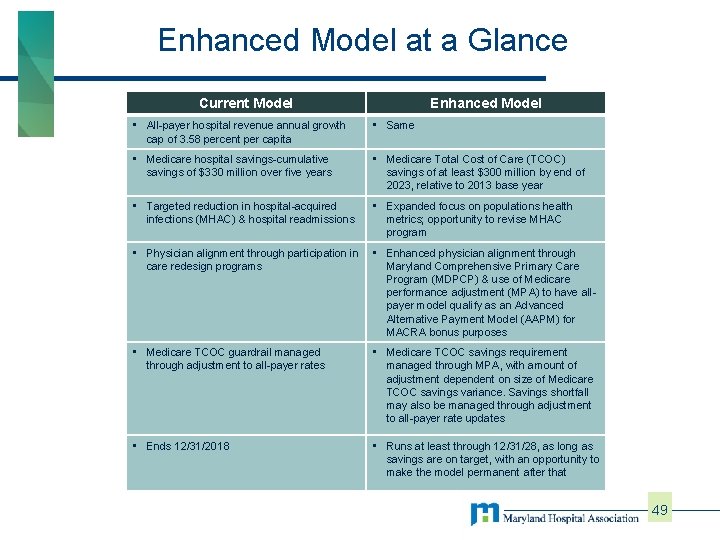
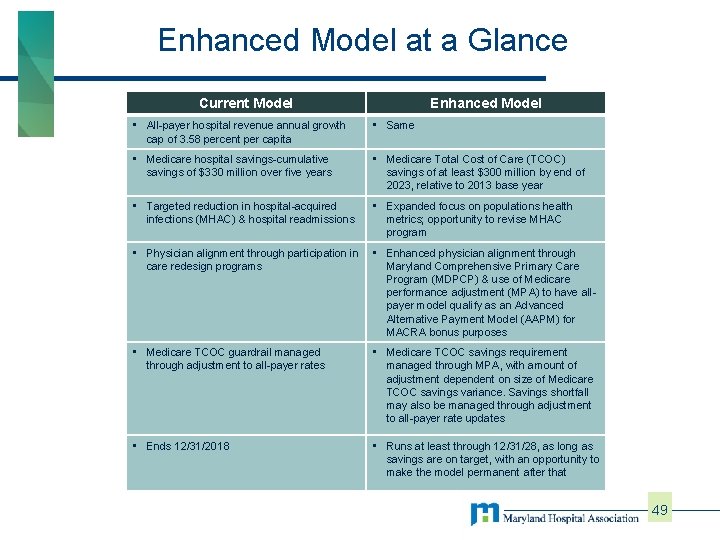
Enhanced Model at a Glance Current Model Enhanced Model • All-payer hospital revenue annual growth cap of 3. 58 percent per capita • Same • Medicare hospital savings-cumulative savings of $330 million over five years • Medicare Total Cost of Care (TCOC) savings of at least $300 million by end of 2023, relative to 2013 base year • Targeted reduction in hospital-acquired infections (MHAC) & hospital readmissions • Expanded focus on populations health metrics; opportunity to revise MHAC program • Physician alignment through participation in care redesign programs • Enhanced physician alignment through Maryland Comprehensive Primary Care Program (MDPCP) & use of Medicare performance adjustment (MPA) to have allpayer model qualify as an Advanced Alternative Payment Model (AAPM) for MACRA bonus purposes • Medicare TCOC guardrail managed through adjustment to all-payer rates • Medicare TCOC savings requirement managed through MPA, with amount of adjustment dependent on size of Medicare TCOC savings variance. Savings shortfall may also be managed through adjustment to all-payer rate updates • Ends 12/31/2018 • Runs at least through 12/31/28, as long as savings are on target, with an opportunity to make the model permanent after that 49
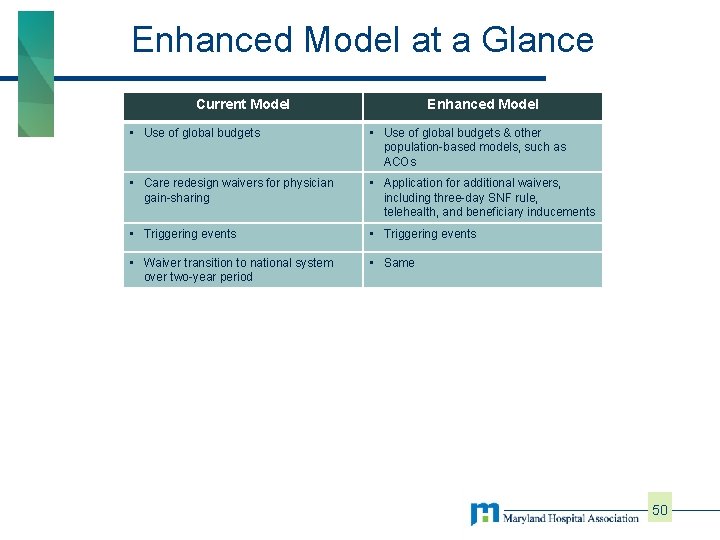
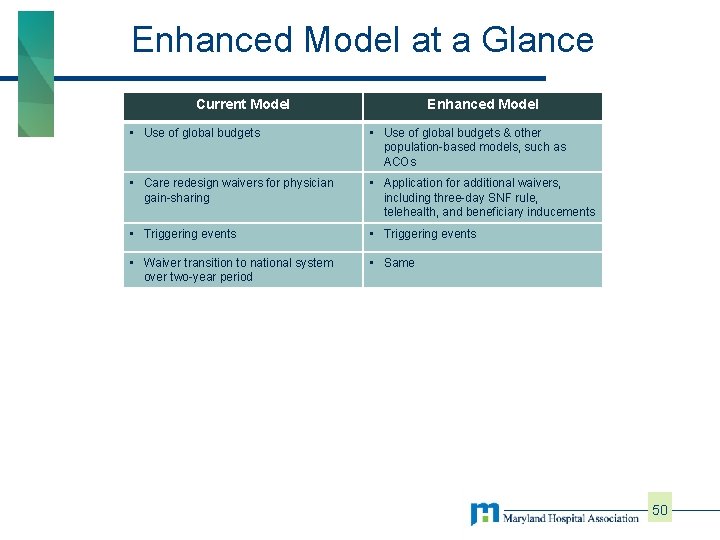
Enhanced Model at a Glance Current Model Enhanced Model • Use of global budgets & other population-based models, such as ACOs • Care redesign waivers for physician gain-sharing • Application for additional waivers, including three-day SNF rule, telehealth, and beneficiary inducements • Triggering events • Waiver transition to national system over two-year period • Same 50
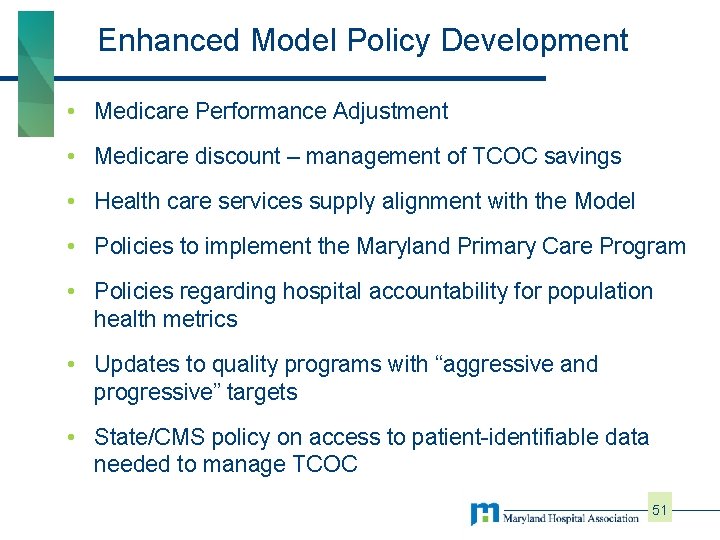
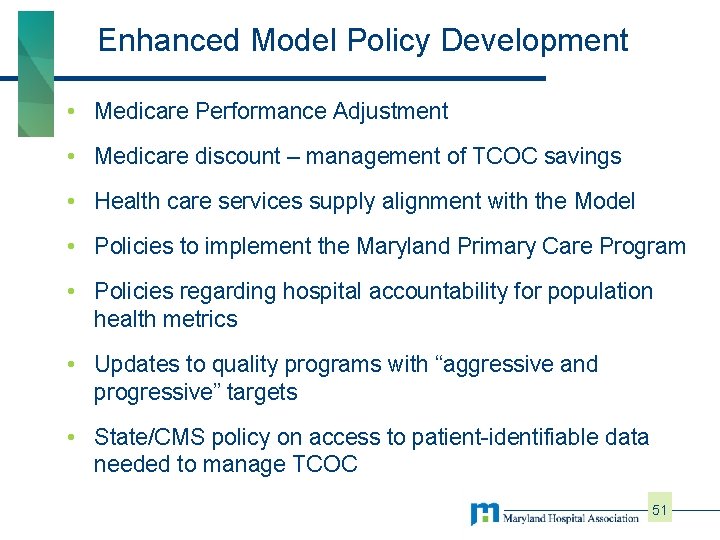
Enhanced Model Policy Development • Medicare Performance Adjustment • Medicare discount – management of TCOC savings • Health care services supply alignment with the Model • Policies to implement the Maryland Primary Care Program • Policies regarding hospital accountability for population health metrics • Updates to quality programs with “aggressive and progressive” targets • State/CMS policy on access to patient-identifiable data needed to manage TCOC 51
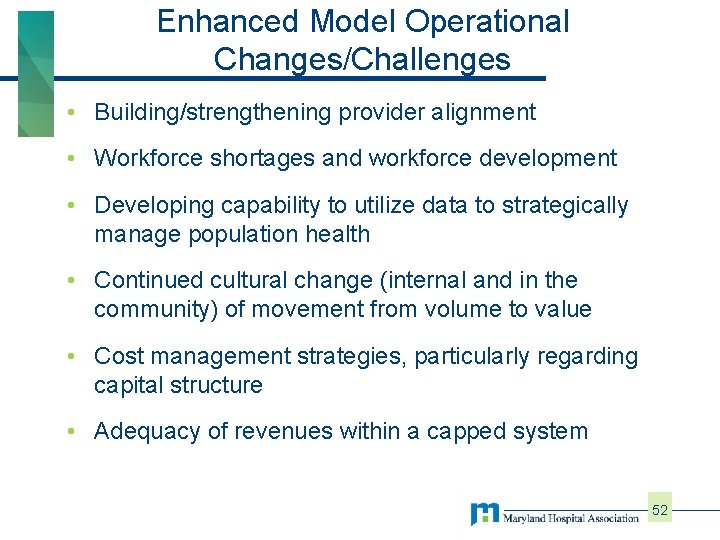
Enhanced Model Operational Changes/Challenges • Building/strengthening provider alignment • Workforce shortages and workforce development • Developing capability to utilize data to strategically manage population health • Continued cultural change (internal and in the community) of movement from volume to value • Cost management strategies, particularly regarding capital structure • Adequacy of revenues within a capped system 52
Hospital Views Future proposal: • Risk shift to hospitals; savings targets may be unrealistic without new tools • Key issues undefined; need clarity to support • Limited hospital resources/bandwidth • But, MARYLAND’S HOSPITALS SUPPORT KEEPING MARYLAND’S MEDICARE WAIVER!! 53
HSCRC Impact: Accountability • Disclosure of Information and Performance § High degree of availability − Maryland system is based on most comprehensive and timely information available § Multiple reporting requirements of Hospitals − − − Monthly revenue and utilization Annual filings Community Benefit Reporting by payer and in-state vs. out-of-state New data tape submission requirements – now monthly § Public Disclosure Report prepared annually by the HSCRC 54
Contact Information Brett Mc. Cone Vice President, Rate Setting bmccone@mhaonline. org 410 540 5060 Maryland Hospital Association 6820 Deerpath Road, Elkridge, MD 21075 410 -379 -6200