Managing Common Dental Health Concerns Thomas Hahn MD


- Slides: 62
Managing Common Dental Health Concerns Thomas Hahn, MD & Ildi Martonffy, MD Family Medicine Midwest October 11, 2014
Disclosures - none

Objectives • The participant will be able to discuss appropriate screening and treatment recommendations for preventive dental care, commonly encountered dental traumas and infections, and edentulism.
Overview • 878 visits to our 4 residency clinics for dental health concern in previous 12 months • 689 unique patients (189 repeat visits) • 589 of those to our 2 clinics which serve most ininsured/underinsured
Cases This is a cool case! And yes, you may use electronic resources as you discuss these cases!
Preventive Care
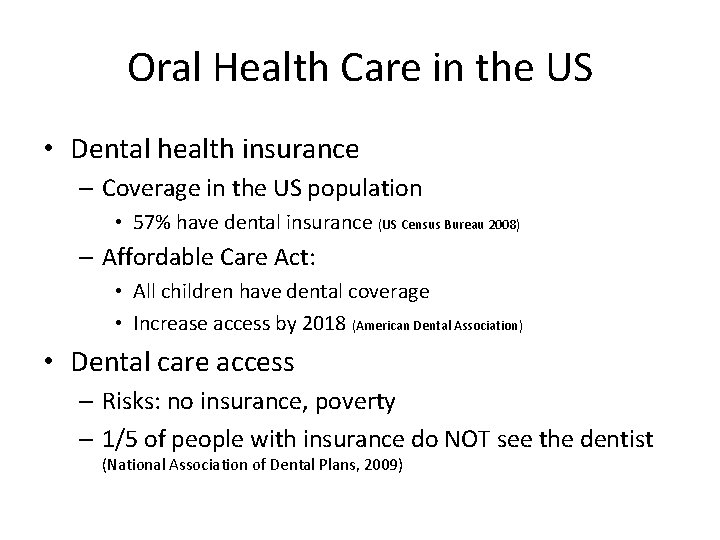
Oral Health Care in the US • Dental health insurance – Coverage in the US population • 57% have dental insurance (US Census Bureau 2008) – Affordable Care Act: • All children have dental coverage • Increase access by 2018 (American Dental Association) • Dental care access – Risks: no insurance, poverty – 1/5 of people with insurance do NOT see the dentist (National Association of Dental Plans, 2009)

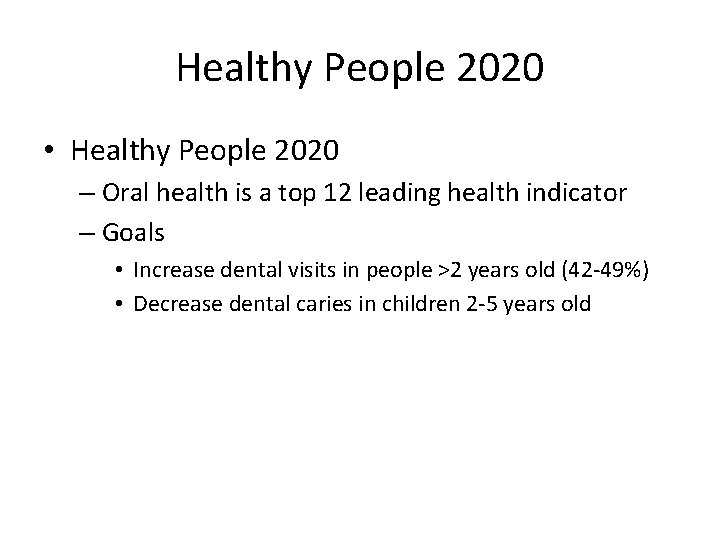
Healthy People 2020 • Healthy People 2020 – Oral health is a top 12 leading health indicator – Goals • Increase dental visits in people >2 years old (42 -49%) • Decrease dental caries in children 2 -5 years old
Case 1 • A 2 -year-old uninsured boy presents to your office for a routine well child examination. He lives in the city with his mother, who is pregnant, and she has some questions: – When should children brush and floss? – When should children see a dentist? – Does he need fluoride supplementation? • On examination of the oral cavity, the teeth appear to be in good condition. – What preventive oral care you can provide for the patient in the office? – Is there any preventive oral health advice in pregnancy?
Preventive Oral Care in Children • PCP is dental home until age 1 • Dental visits starting at age 1 • Brushing and flossing – Brush once daily 6 -24 mo – Floss with 2 teeth – Parent-assisted brushing 2 -5 year old • Adults: brush twice daily and floss once daily
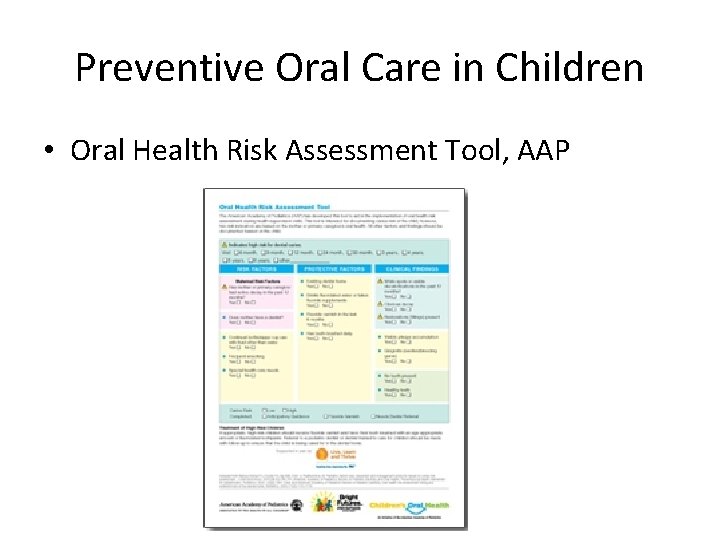
Preventive Oral Care in Children • Oral Health Risk Assessment Tool, AAP
Fluoride: How It Works • Fluoride: mineral found in the earth • Functions – Protective barrier, resists acid – Remineralization of damaged teeth • Types – Systemic • Fortified city water • Supplements like drops – Topical • Toothpaste • Varnish • Mouth rinse • Recommendations: fluoride in water and toothpaste
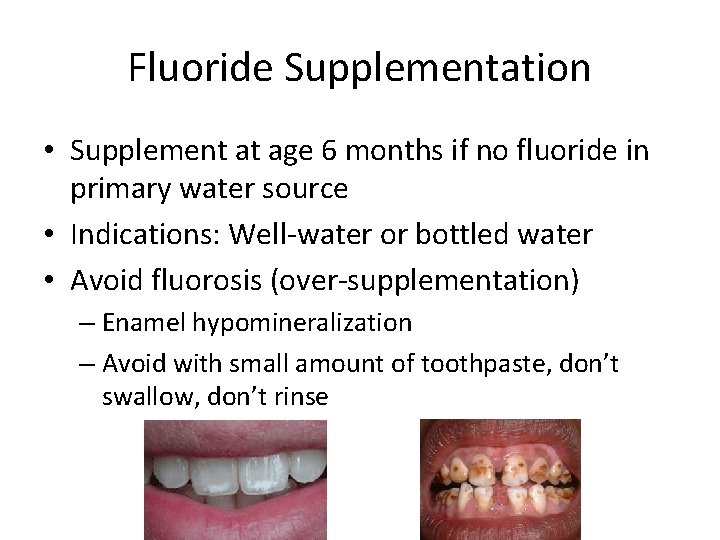
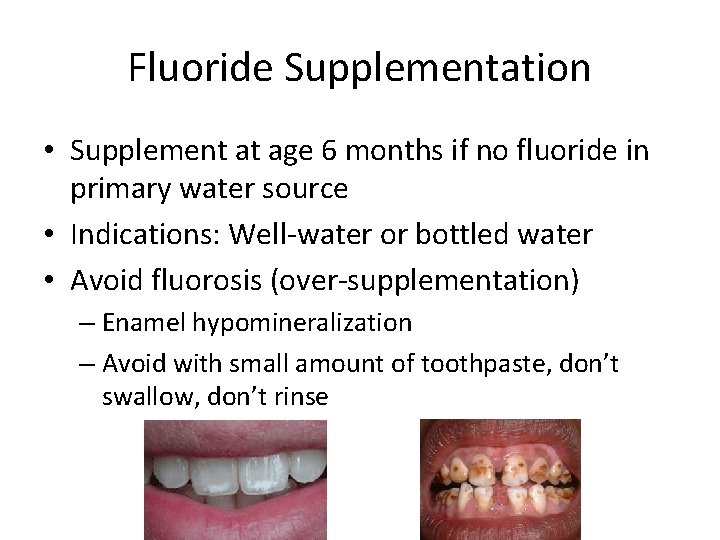
Fluoride Supplementation • Supplement at age 6 months if no fluoride in primary water source • Indications: Well-water or bottled water • Avoid fluorosis (over-supplementation) – Enamel hypomineralization – Avoid with small amount of toothpaste, don’t swallow, don’t rinse
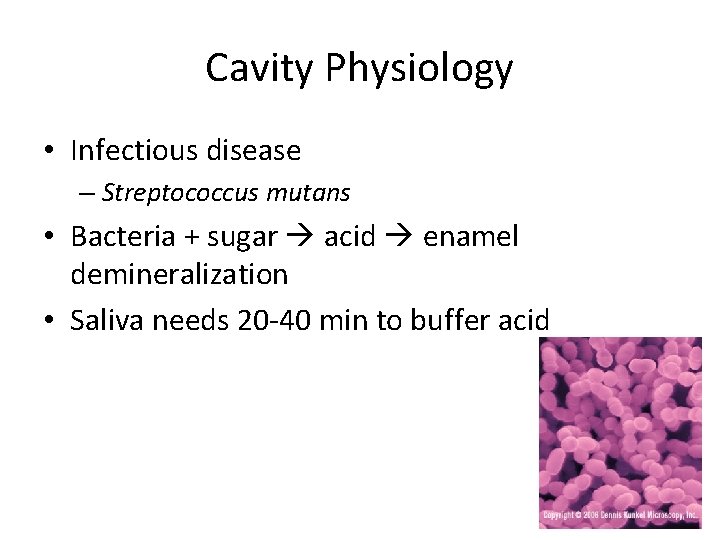
Cavity Physiology • Infectious disease – Streptococcus mutans • Bacteria + sugar acid enamel demineralization • Saliva needs 20 -40 min to buffer acid
Early Childhood Carries • Most common chronic childhood disease (more common than asthma and obesity) • Increased incidence from 24 -28% in past decade • Risks: low socioeconomic status, bottle in bed, lack of fluoride • Treatment: Dietary counseling, oral hygiene, fluoride varnish
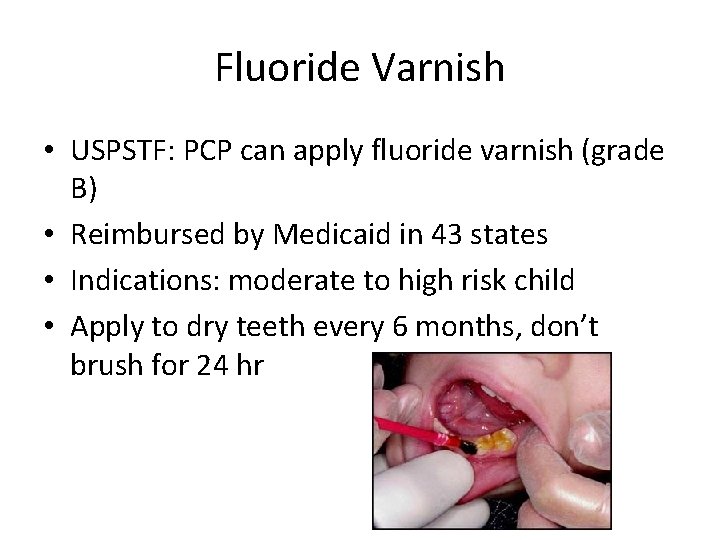
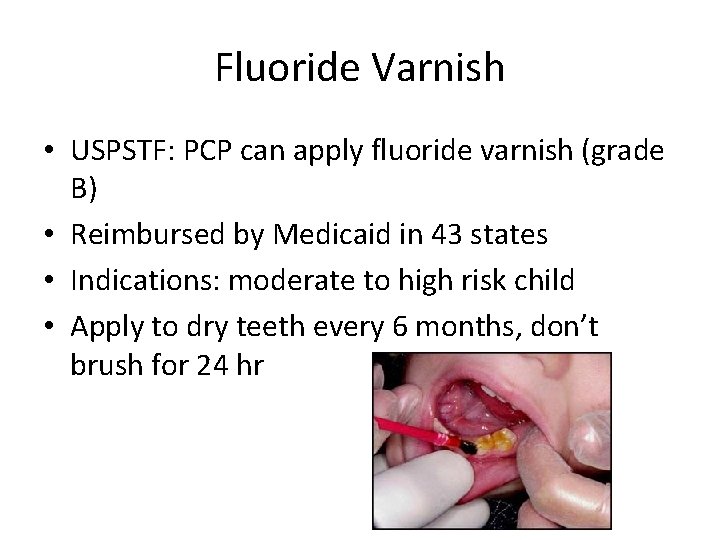
Fluoride Varnish • USPSTF: PCP can apply fluoride varnish (grade B) • Reimbursed by Medicaid in 43 states • Indications: moderate to high risk child • Apply to dry teeth every 6 months, don’t brush for 24 hr
Oral Care in Pregnancy • Only 35% of pregnant women get dental care (ACOG 2013) • Recommended oral exam at all OB intake visits • Okay to have dental care during pregnancy – Procedures during 2 nd trimester • Dental caries are infectious disease – Strep mutans – Transmitted from mothers to infants
Why should we care about prevention? • Poor dentition can lead to: – Pain – Other infections (pulmonary) – Possible worsening of T 2 DM and CVD • Keeps health care costs down • Remember: simple brushing with fluoride toothpaste and flossing can prevent dental infections and systemic disease!
Dental Trauma
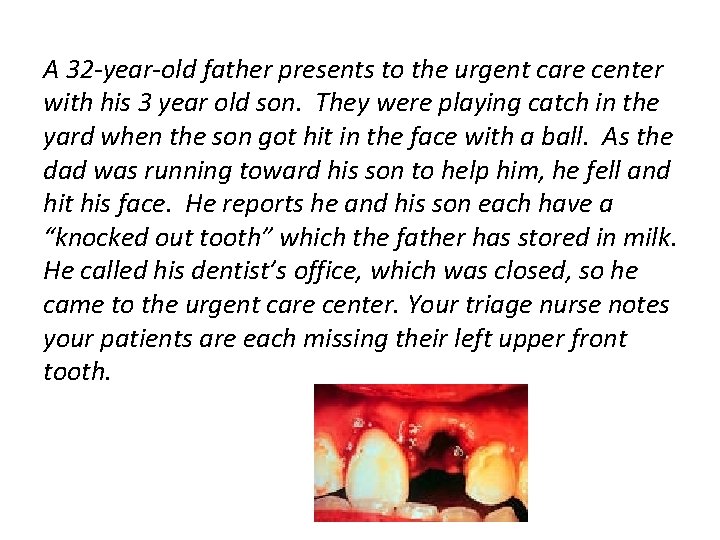
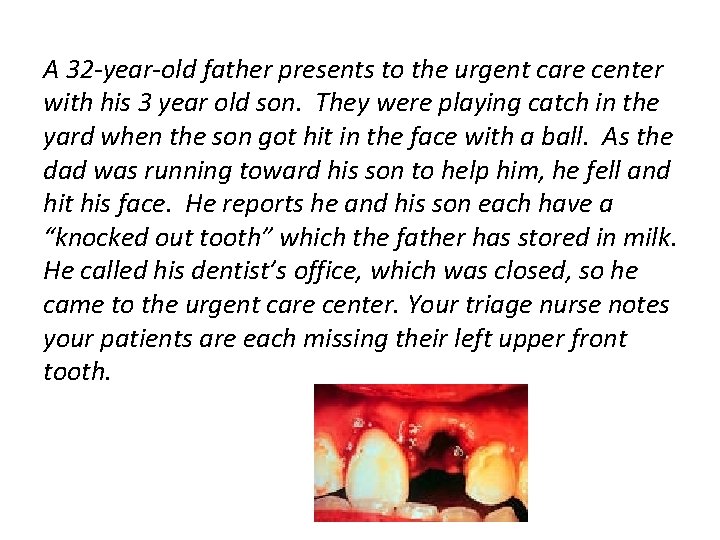
A 32 -year-old father presents to the urgent care center with his 3 year old son. They were playing catch in the yard when the son got hit in the face with a ball. As the dad was running toward his son to help him, he fell and hit his face. He reports he and his son each have a “knocked out tooth” which the father has stored in milk. He called his dentist’s office, which was closed, so he came to the urgent care center. Your triage nurse notes your patients are each missing their left upper front tooth.
Who? • Everyone! – 1/3 of preschool children and 1/4 of all school aged children have had a traumatic injury to their primary dentition – Almost 1/3 of adults have suffered trauma to their permanent dentition
When? • Primary teeth: ages 2 -3, as motor coordination is developing • Permanent teeth: falls, motor vehicle accidents, sports, violence • About 80% of lifetime dental injuries occur before age 19 (Glendor, 2008)
Where? • Maxillary central incisors and any protruding teeth are most commonly injured • Trauma can affect tooth enamel, dentin, pulp, root, periodontal ligament, gum, alveolar socket, or a combination of these • Trauma is defined by which components are affected
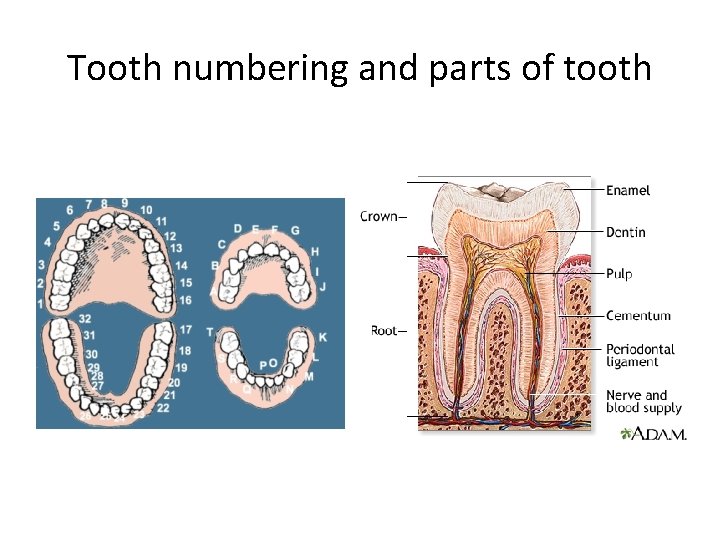
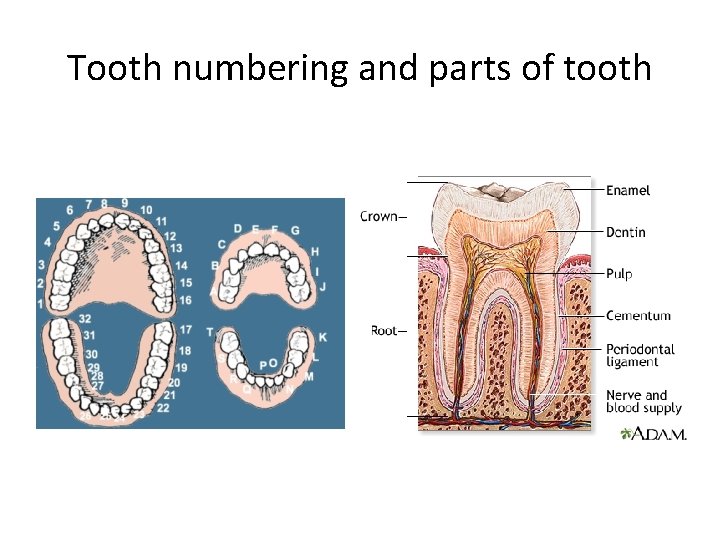
Tooth numbering and parts of tooth
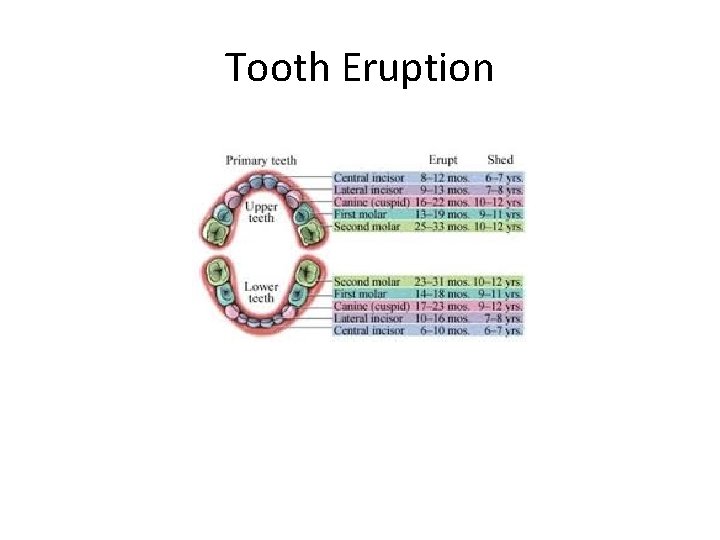
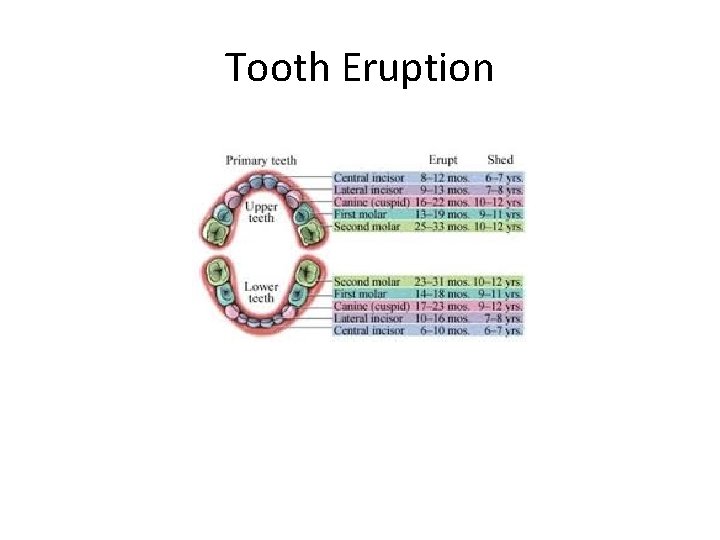
Tooth Eruption
What? • What are the types of injury? • What do we do about it? • What kind of collaboration and follow up do we need?
Types of trauma • Dental Trauma Guide – http: //www. dentaltraumaguide. org/Permanent_teeth. aspx
Treatment of dental trauma • ABCs: airway, breathing, circulation, other injuries • History: mechanism of injury, loss of consciousness, bite disturbance? • Exam: type and severity of injury – injury of multiple teeth more severe
Primary Teeth - Intrusion • Should be allowed to re-erupt spontaneously unless displaced toward germ of the developing secondary tooth. • The tooth should be extracted if displaced toward the germ of the developing secondary tooth • When indicated to allow re-eruption, 90% of intruded teeth will re-erupt within 2 -6 months • IADT and AAPD concur on these recommendations http: //www. dentaltraumaguide. org/Primary_Intrusion_Description. aspx
Primary Teeth - Avulsion • Leave it out! • An avulsed primary tooth should NOT be replanted
Permanent Teeth - Intrusion • Treatment options: – Awaiting spontaneous re-eruption (non-active) – Orthodontic repositioning (active treatment) – Surgical repositioning (active treatment) • Consider: severity, root stage, number of intruded teeth, ability to follow up
Permanent Teeth - Intrusion • 2007 Norwegian study, 51 intruded permanent incisors in 6 – 17 year olds (Wigen, 2008) – Higher rates of pulp necrosis, inflammatory root resorption, and replacement resorption (ankylosis) in active treatment group – Of 37 teeth in non-active group, 35 re-erupted and 2 became ankylosed – 9 of the 35 had been completely intruded and only 6 were intruded < 2 mm – NO mature, completely intruded teeth retained pulp vitality
Permanent Teeth - Intrusion • 2006 prospective study of 140 intruded teeth recommends surgical repositioning if: – Multiple intrusions – Nasal sinus invasion And prefers active repositioning if > age 17 with completed root formation (Andreasen, 2006)
Permanent Teeth: Intrusion Guidelines • AAPD: – Spontaneous re-eruption if roots 1/2 to 2/3 formed – Active repositioning of mature teeth with prompt (within 3 weeks) endodontic treatment – Intrusion of 7 mm or more has a negative influence on healing
Permanent Teeth: Intrusion Guidelines • IADT: – Surgical repositioning if mature tooth intruded > 7 mm – Surgical or orthodontic if immature tooth > 7 mm – Orthodontic repositioning if immature tooth does not move after “a few weeks” of waiting or mature tooth intruded < 3 mm does not move after 2 -4 weeks of expectant managment
Permanent Teeth - Avulsion • Time = tooth! • Prognosis depends on “pre-replantation extraoral dry time” and root development stage • Optimal = less than 5 minutes • Want to optimize neurovascular supply of tooth and periodontal ligament UNLESS: • poor alveolar bone integrity, uncontrolled seizure disorder, or immunocompromised state
Permanent Teeth - Avulsion • First person capable of doing so should replant the tooth • Rinse under cold water ONLY if visibly soiled • Store in cold animal milk or saliva if needed • Risk of akylosis increases with extra-oral dry time 20 minutes or more • PDL unlikely to survive if extra-oral dry time 60 minutes or more
Permanent Teeth - Avulsion • If 1 mm or more of apical opening, full pulp revascularization in 18% of cases • Systemic antibiotics improve revascularization rates • Systemic antibiotics and updating Tetanus vaccines recommended if avulsed tooth exposed to soil (Kling, 1986)
Permanent Teeth - Avulsion • For teeth less likely to revascularize, goal is to delay ankylosis as long as possible • Remaining PDL is removed by physical scraping or chemical methods and tooth is soaked in sodium fluoride prior to replantation, thought to decrease inflammation • Reduces 5 year resorption rates
Permanent Teeth - Avulsion Replanted tooth splinted in place x 2 weeks Soft diet, gentle brushing Chlorhexidine rinses Root canal for avulsed mature teeth 7 -10 days after injury • For immature teeth, no root canal unless evidence of pulp necrosis • •
Why should we (as docs) care? • Risks for ongoing pain and malocclusion in our patients • We can counsel about protective sports gear, general home safety, safe alcohol use
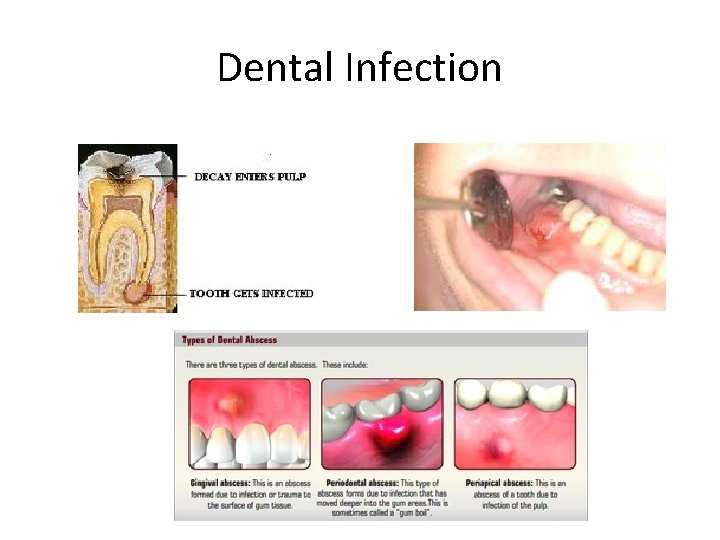
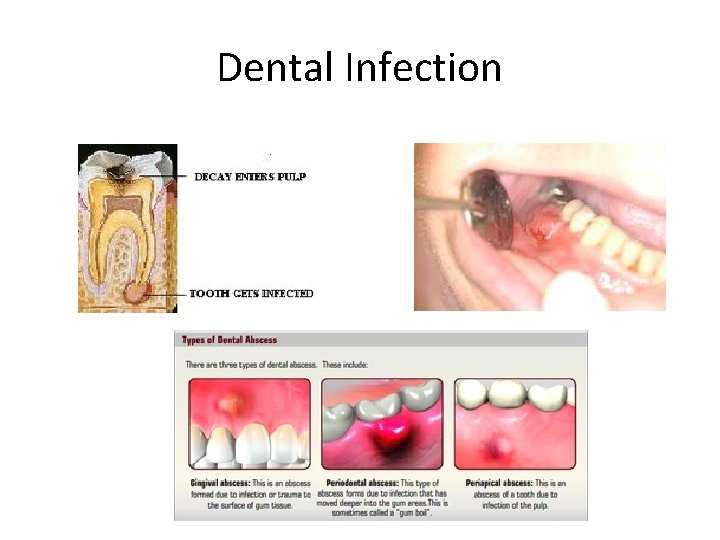
Dental Infection
Case 3 • A 39 year-old-woman presents to the office with pain in her left lower molar. You notice redness and swelling of her gum line. She is afebrile but you notice mild swelling in the left lower face. – What are the different types of dental infections, and what type does the patient likely have? – What are signs and symptoms of a dental emergency? – What are the major oral bacteria? – Which antibiotics are used to treat dental infections?
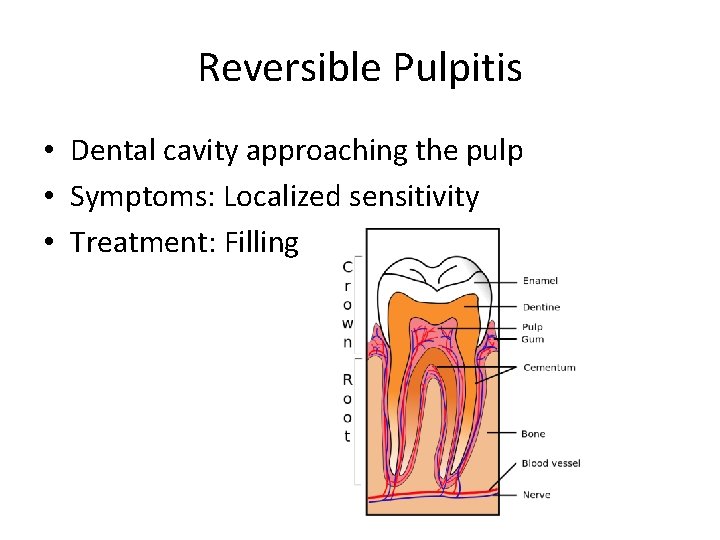
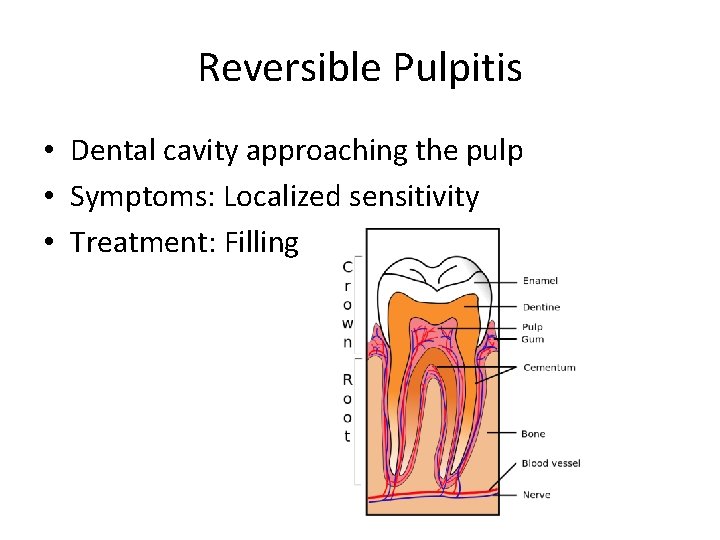
Reversible Pulpitis • Dental cavity approaching the pulp • Symptoms: Localized sensitivity • Treatment: Filling
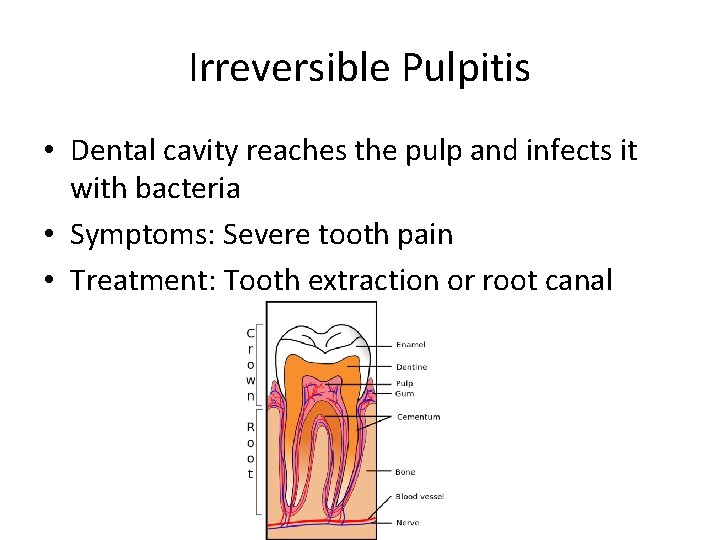
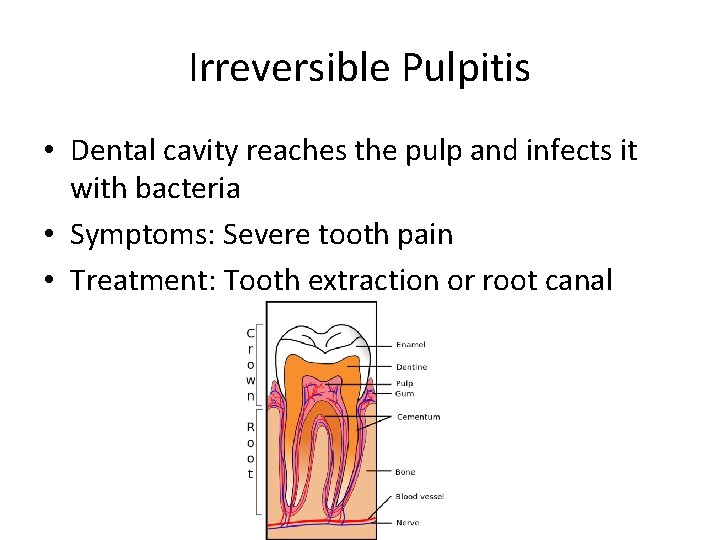
Irreversible Pulpitis • Dental cavity reaches the pulp and infects it with bacteria • Symptoms: Severe tooth pain • Treatment: Tooth extraction or root canal
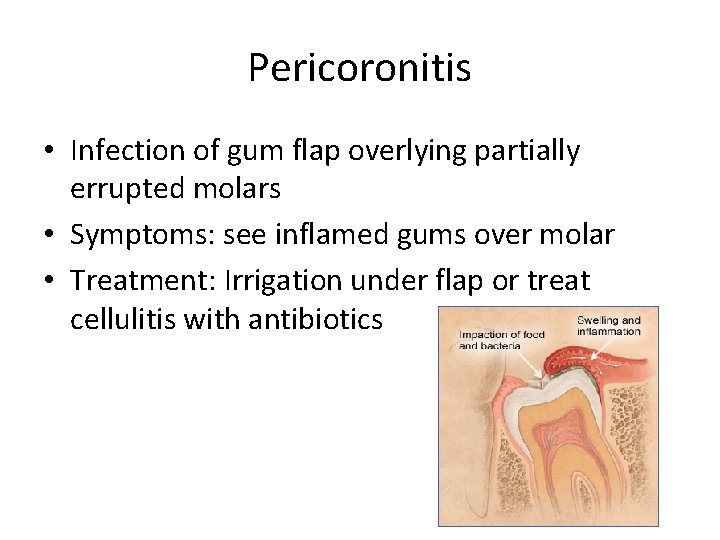
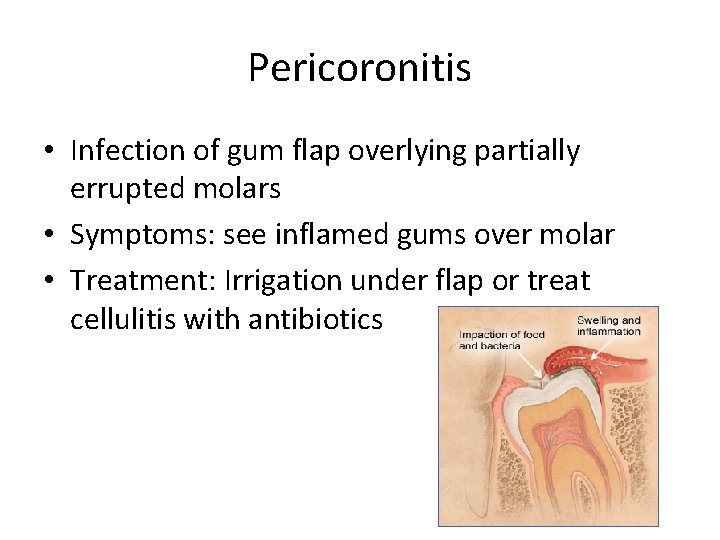
Pericoronitis • Infection of gum flap overlying partially errupted molars • Symptoms: see inflamed gums over molar • Treatment: Irrigation under flap or treat cellulitis with antibiotics
Periapical/Periodontal Abscess • Infected in the root of the tooth and in the surrounding tooth structures pulp causes an abscess under the root of the tooth and in the surrounding tooth structures • Symptoms: Localized swelling and pain, loose tooth, cellulitis • Treatment: Drain abscess, referral for root canal/extraction. Only use antibiotics if systemic symptoms or cellulitis present
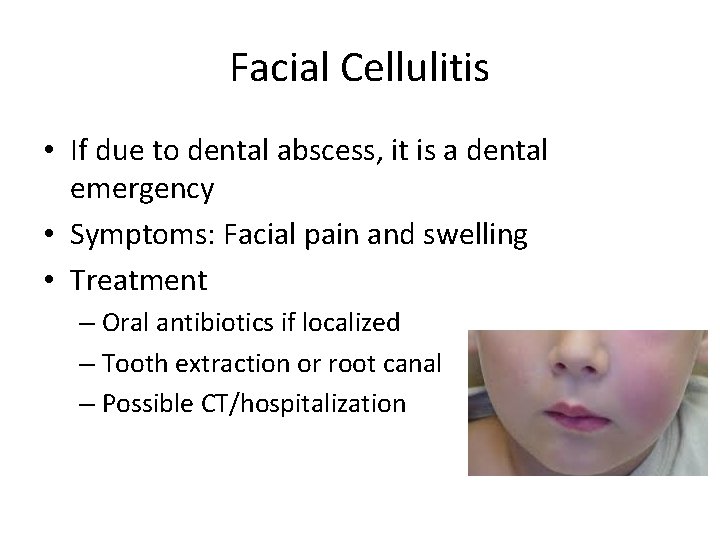
Facial Cellulitis • If due to dental abscess, it is a dental emergency • Symptoms: Facial pain and swelling • Treatment – Oral antibiotics if localized – Tooth extraction or root canal – Possible CT/hospitalization
Common Oral Bacteria • Gram-positive cocci – Streptococcus mutans (cause of dental caries) – Streptococcus sanguis – Staphylococci • Lactobacillus • Gram-negative cocci • Anaerobes – Bacteroides
Antibiotics • First-line – Penicillin VK 25 -50 mg/kg/day divided 4 times daily – Amoxicillin 35 -50 mg/kg/day divided 3 times daily – Amoxicillin-clavulanate 35 -50 mg/kg/day amox divided three times daily • Penicillin-allergic – Clindamycin 10 -25 mg/kg/day divided TID • Severe infections – Ampicillin-sulbactam – Piparicillin-tazobactam – Cefotaxime
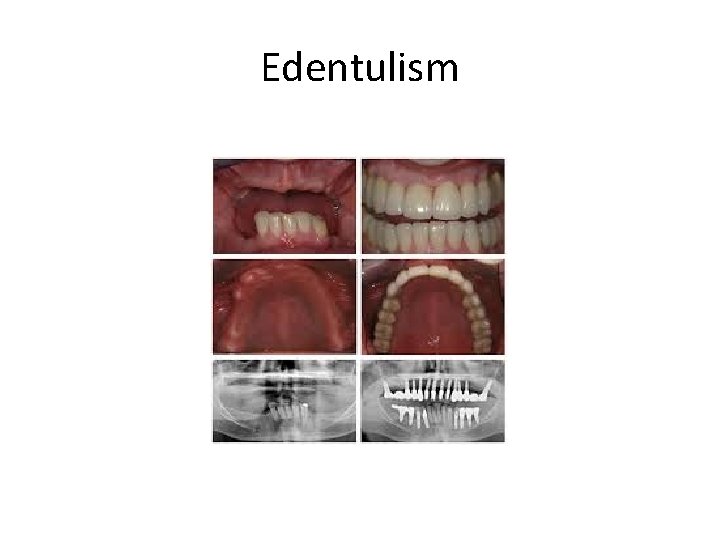
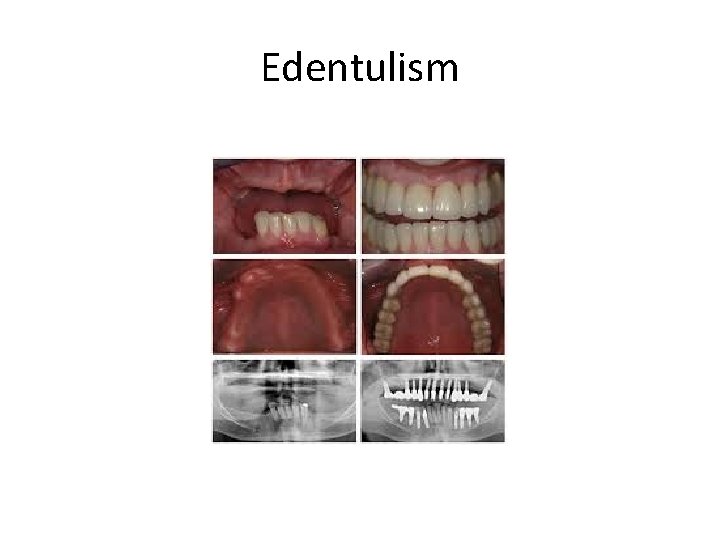
Edentulism
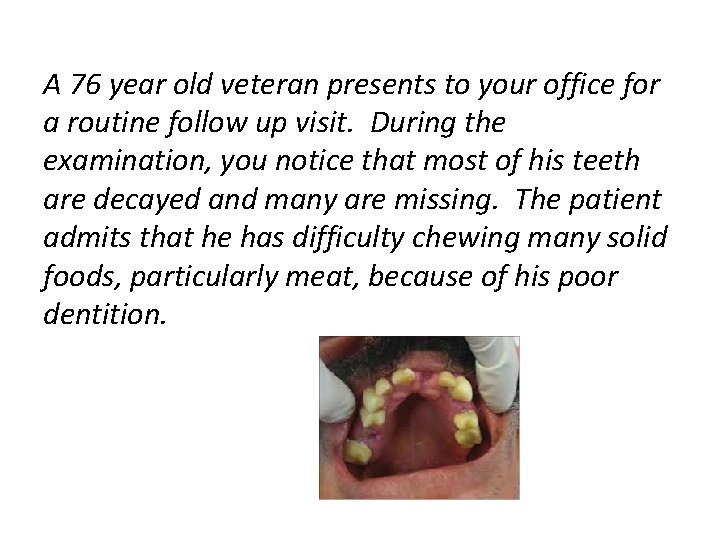
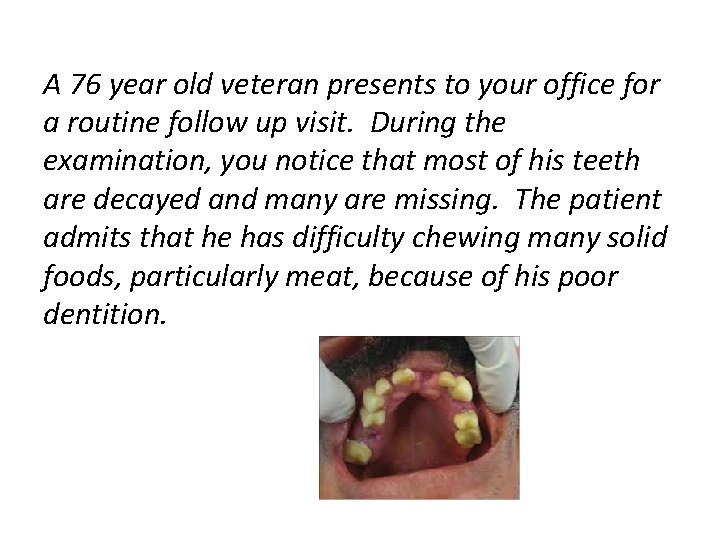
A 76 year old veteran presents to your office for a routine follow up visit. During the examination, you notice that most of his teeth are decayed and many are missing. The patient admits that he has difficulty chewing many solid foods, particularly meat, because of his poor dentition.
Scope of the problem • Over 35 million Americans are edentulous • 178 million are missing at least one tooth (from decay, injury, gum disease, wear, cancer treatment) • Effects: – – Nutritional deficiencies Oral pain Poorer psychosocial functioning Higher DM risk (Clearly, 1995)
Replacement indications Dentures Implants • Partial or full • About 15% of edentulous US adults have dentures made each year • Series of visits • Full if remaining teeth can’t support a removable partial • Denture intolerance • Can replace single tooth or anchor an over-denture • Poor healing in smokers, DM, tooth grinders, or Hx of radiation
Considerations – complete edentulism • 2 implants into mandible to hold over-denture is optimal for complete edentulism – improved function, satisfaction, QOL • Titanium root implanted into bone socked, allowed to heal for 6 -12 weeks, then connector post and crown are attached
Considerations – partial edentulism • 2012 Cochrane review: insufficient evidence to recommend particular replacement method • 2013 retrospective study: natural teeth did better with implants than with partials • Mean denture survival time is about 8 years
Complications - dentures • • • Soft tissue irritation – denture stomatitis Infection Bone loss Discomfort Caries Poor fit -> alveolar bone loss
Complications – implants (Mc. Dermott, 20013) • Inflammatory – mobility, infection, pain – 10. 2% • Prosthetic – recementation, ajustment – 2. 7% • Operative – incorrect placement, paresthesia > 1 week – 1%
Care Rinse oral tissues at least daily Clean all surfaces of denture – no toothpaste Store in moist, airtight container Brush any remaining teeth regularly Need for excess adhesive can indication poor fit • Check your patients for stomatitis • • •
Questions ?
References • • • • • Healthy People 2020. www. healthpeople. gov National association of dental providers, 2009. The Haves and the Have-Nots: Consumers With and Without Dental Benefits Preventive Dental Care and Counseling for Infants and Young Children, 2013. Up. To. Date. Silk, H. , 2013. Family Physicians Are in Perfect Position of Address Oral Health. AAFP. Smiles for Life. STFM. www. smilesorlifeoralhealth. org Amereican Academy of Pediatric Dentistry (AAPD), "Guideline on management of acute dental trauma, " in AAPD, Chicago, IL, 2011. "The Dental Trauma Guide, " [Online]. Available: http: //www. dentaltraumaguide. org. [Accessed 26 Nov 2013]. Facts & Figures. (2014, January 27). Retrieved from American College of Prosthodontists: http: //www. gotoapro. org/news/facts--figures/ Clearly, T. , & Hutton, J. (1995, July). An assessment of the association between functional edentulism, obesity, and NIDDM. Diabetes Care, 18(7), 1007 -9. Brown DW. Complete edentulism prior to the age of 65 years is associated with all-cause mortality. J Public Health Dent. 2009; 69(4): 260 -6. doi: 10. 1111/j. 1752 -7325. 2009. 00132. x. Alani, A. , Bishop, K. , Djemal, S. , & Renton, T. (2012). Guidelines for Selecting Appropriate Patients to Receive Treatment with Dental Implants: Priorities for the NHS. Royal College of Surgeons, Faculty of Dental Surgery. London: National Health Service. Mc. Dermott, N. , Chuang, S. , Woo, V. , & Dodson, T. (2003). Complications of dental implants: identification, frequency, and associated risk factors. The International Journal of Oral & Maxillofacial Implants, 18(6), 848 -855. Felton, D. , Cooper, L. , Duqum, I. , Minsley, G. , Guckes, A. , Haug, S. , . . . Deal Chandler, N. (2011). Evidence-based guidelines for the care and maintenance of complete dentures: A publication of the American College of Prosthodontists. Journal of the American Dental Association, 142, Suppl 1.
 Thomas hahn siemens
Thomas hahn siemens Health concerns
Health concerns Health concerns
Health concerns Health concerns
Health concerns Blood supply of pituitary gland
Blood supply of pituitary gland Health concerns
Health concerns Thomas mocker and thomas stewart
Thomas mocker and thomas stewart In common sense, thomas paine argued that
In common sense, thomas paine argued that Java9s
Java9s Software design separation of concerns
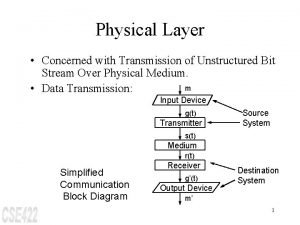
Software design separation of concerns The network layer is concerned with
The network layer is concerned with Addressing concerns and earning commitment
Addressing concerns and earning commitment What are the concerns of the constitutions?
What are the concerns of the constitutions? Product +concerns
Product +concerns Concerns-based adoption model
Concerns-based adoption model Southwest airlines code of ethics
Southwest airlines code of ethics A traditional method of earning commitment is the
A traditional method of earning commitment is the Joys and concerns images
Joys and concerns images Joys and concerns prayer
Joys and concerns prayer Flexible software design
Flexible software design Matzas
Matzas Chapter 6 process selection and facility layout
Chapter 6 process selection and facility layout Pietro molla
Pietro molla Closeness rating examples
Closeness rating examples The physical layer concerns with
The physical layer concerns with Identify concerns
Identify concerns Taiga environmental concerns
Taiga environmental concerns When a choice concerns matters of personal value or taste
When a choice concerns matters of personal value or taste Joys and concerns images
Joys and concerns images Adult career concerns inventory
Adult career concerns inventory Escalating concerns
Escalating concerns It concerns many sociologists
It concerns many sociologists Design concerns
Design concerns Thematic concerns
Thematic concerns How does banquo describe the witches
How does banquo describe the witches Dr smith
Dr smith What are banquo's concerns about the witches prophecy
What are banquo's concerns about the witches prophecy Whos ghost does macbeth see
Whos ghost does macbeth see Macmillan concerns checklist
Macmillan concerns checklist Father of public health dentistry in world
Father of public health dentistry in world Texas health steps check up
Texas health steps check up Define dental public health
Define dental public health Borrego urgent care cathedral city
Borrego urgent care cathedral city Objectives of school health programme
Objectives of school health programme Tattletooth program
Tattletooth program Albany area primary health care rural clinic
Albany area primary health care rural clinic Dental health aide therapist
Dental health aide therapist Greatest common factor of 20 and 36
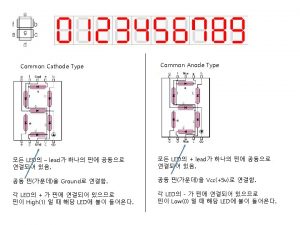
Greatest common factor of 20 and 36 Common anode and common cathode
Common anode and common cathode Common factors and common multiples
Common factors and common multiples Highest common factors and lowest common multiples
Highest common factors and lowest common multiples Factors of 12 and 42
Factors of 12 and 42 Multiples of 9 and 21
Multiples of 9 and 21 Nie mehr von ulla hahn
Nie mehr von ulla hahn Ulla hahn gedichte liebe
Ulla hahn gedichte liebe Tino hahn
Tino hahn Martin georg hahn
Martin georg hahn Retrazione ischemica di volkmann
Retrazione ischemica di volkmann Krokodilstränen weinen redewendung
Krokodilstränen weinen redewendung Closed for the season mary downing hahn
Closed for the season mary downing hahn Hahn banach theorem applications
Hahn banach theorem applications Emelie hahn
Emelie hahn Janos hahn
Janos hahn